Abdominal muscle strain pregnancy
How to Tell if You Have Torn Abs During Pregnancy? Diastasis Recti
Diastasis Recti Surgery in Melbourne
Do you feel as though your abs have torn during pregnancy? If you’ve been struggling with a worsening abdominal bulge or back pain and muscle weakness after giving birth, then the chances are that yes, they may very well be. Find out more by reading our overview of Diastasis Recti (torn or split abdominal muscles) and how to tell if your ab muscles were torn during pregnancy.
URGENT UPDATE – The Australian Government has reinstated a Medicare Item Number for a Tummy Tuck for some post-pregnancy patients suffering from Diastasis Recti (Split Tummy Muscles) if you are eligible and meet the new criteria. This new Medicare Item Number -30175 is effective 1st July 2022. Read the 30175 Medicare Item Number factsheet
Download Our Tummy Tuck Guide
Have my abs split or torn during pregnancy?
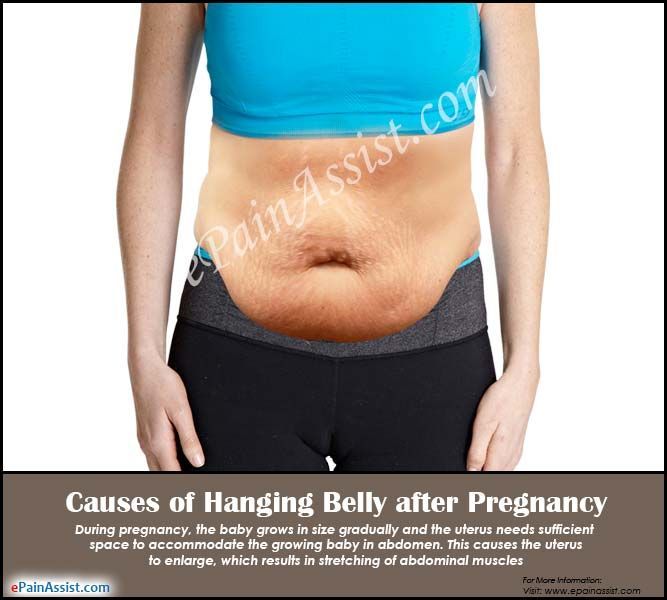
After pregnancy, many women are often eager to get their post-baby body back and feel great within their own skin again. Even if you exercise regularly and keep in shape during pregnancy, the extensive changes that your body goes through during this time can come as a shock.
It is no surprise that women can become dismayed when diet and exercise alone don’t seem to help restore their pre-pregnancy body shape. However, there is often another reason for this. Abdominal muscles can be torn, split and damaged during pregnancy and childbirth; this condition is known as diastasis recti.
Many mums remain unfamiliar with the condition of torn abs during or after pregnancy. They assume it is their fault that they can’t restore their belly to it’s ‘normal’ shape and size. In reality, diastasis recti can make that nearly impossible without surgical help.
What is the condition of torn abs, or Diastasis Recti?
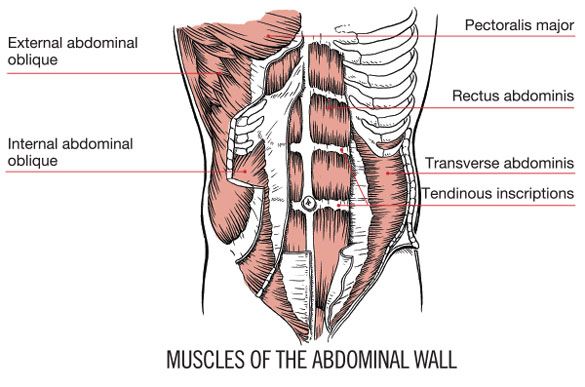
Diastasis recti is a disorder that is generally defined as the separation of the abdomen muscle into right and left halves. Basically, the abs split – or divide – into two, greatly reducing your core strength.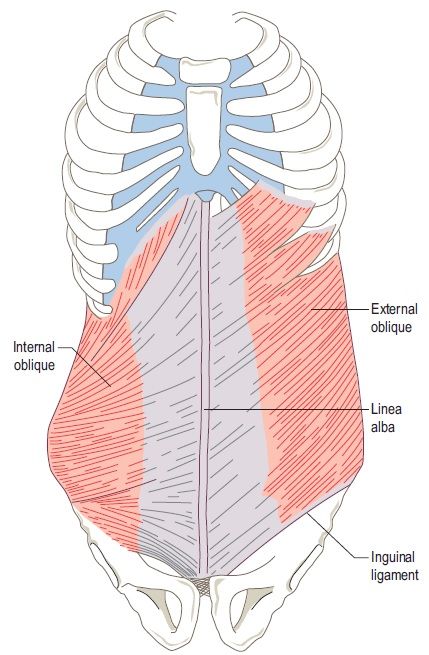
Typically when this condition happens, a pregnant woman’s uterus pushes against the muscles and separates them. Pregnancy hormones also weaken the tissues that hold these muscles together.
Diastasis recti as a result of pregnancy can lead to:
- Back pain
- Muscle weakness
- Incontinence
- Skin infection due to excess skin folds and loose skin
Many women don’t realise their “mummy pooch” isn’t due to lack of exercise or a poor diet; it’s due to abdominal separation. Though the words muscle separation may make you think “flabby, loose, and painful” – it’s actually quite common.
You can view what the latest research shows about torn abs and incontinence after pregnancy by reading the ASAPS press release.
Who is prone to diastasis recti?
It seems that nearly anyone who has had more than one child is highly likely to have torn abdominal muscles.
Women with the highest chances of having damaged abdominal muscles due to pregnancy include:
- Being over the age of 35
- Having experienced multiple pregnancies
- Delivering a high birth-weight baby
If you too have been struggling to remove your post-baby belly bulge after pregnancy, you’re not alone. As many as 1 in 3 mums eventually discover they have abdominal separation.
As many as 1 in 3 mums eventually discover they have abdominal separation.
Having split abs is something that many women either end up accepting or choosing to have surgery to repair (typically a Tummy Tuck). For people who care about how they look after pregnancy and want a firmer, tighter belly area; Abdominoplasty surgery can be life-changing.
How to tell if you have separated abdominal muscles due to pregnancy?
Self-assessment for the condition of Diastasis Recti is the first step. However, a professional medical evaluation can give you better advice. For example, you might have a hernia as well as torn abs or an entirely different condition that is causing the bulge.
- Firstly, you will need to allow an adequate period of time for your body to adjust post-pregnancy before you assess the situation.
- As pregnancy results in such a huge change for your body, this can take from several months, up to a year or two.
- If after exercising for a reasonable amount of time and eating healthy meals and your body still isn’t anywhere near the same condition that it was before childbirth, you might consider these self-assessment techniques.

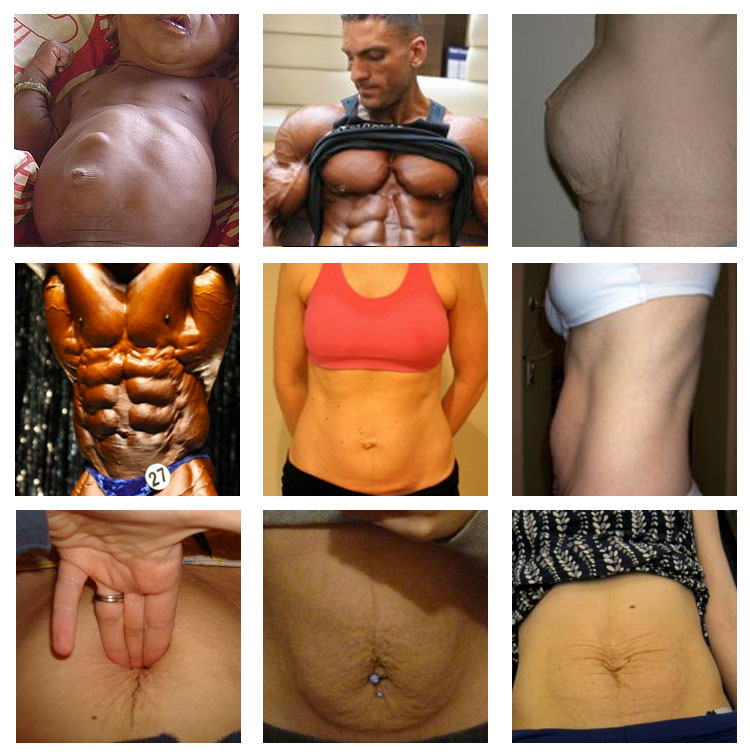
There are three ways to tell if your abdominal muscles were damaged or torn during pregnancy:
- A visible gap in the middle of your abdominal area (more than 2 1/2 finger-widths) when the abdomen is fully contracted.
- The gap does not shrink as you contract your abdomen.
- You can see a small mound protruding along the length of your mid-line.
In addition, there is a simple test you can perform at home:
- Lie on your back with your knees bent, and the soles of your feet on the floor
- Place one hand behind your head, and the other hand on your abdomen. Ensure your fingertips are across your stomach at the level of your belly button
- With your abdominal wall relaxed, gently press your fingertips into your stomach
- Roll your upper body off the floor into a “crunch” position. Make sure that your ribcage moves closer to your pelvis
- Move your fingertips back and forth across your midline, feeling for the right and left sides of your abdominal muscle.

- Feel for separation at, above, and below your belly button. It’ll be a palpable division, although can be easier to feel on some belly areas than others.
Can exercise fix torn abs after pregnancy?
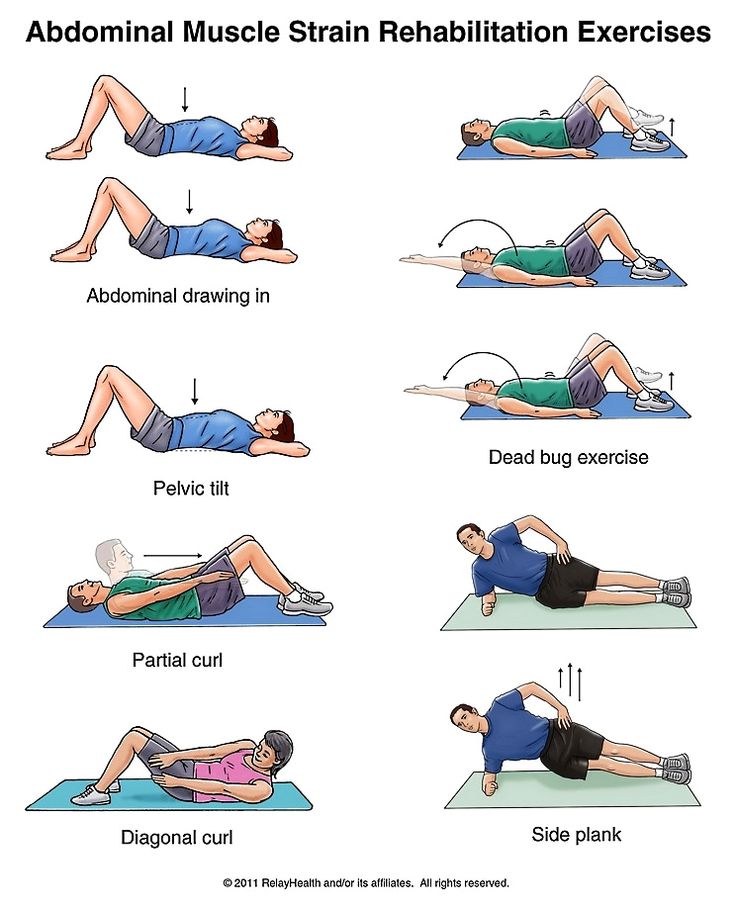
If you find you have abdominal separation, there are things you can do to help mitigate but not repair the condition. In fact, the wrong exercises can actually make the bulge of the split abdominal muscles appear even worse.
Some properly performed abdominal exercises, including many Pilates moves, may help:
- Cardio, strength training and yoga; Ideally under the direction of a physio or fitness trainer can be a great place to start if your condition of diastasis recti is somewhat mild.
- Some, but not all, abdominal exercises are also appropriate for a mild condition.
- In fact, some exercises can make belly bulges worse, such as crunches or improperly performed abdominal exercises.
Exercises for separated abdominal muscles
- Abdominal compressions, pelvic tilts, toe taps, bridges, etc.
 will help separated muscles.
will help separated muscles. - The stomach should remain pulled in, rather than pushed out while exercising.
- This explains why pilates instructors and physiotherapists are so adamant about keeping your navel pulled in during abdominal exercises.
Exercises can tighten the belly somewhat but exercises cannot, on their own, repair and rejoin torn abdominal muscles.
Despite all of the exercises you do, you may never again have a tummy that doesn’t significantly protrude. Furthermore, along with post-pregnancy hormonal changes and an altered Body Mass Index (BMI), you’ll probably also have areas of your body that have accumulated body fat or uneven body fat distribution. This can make the appearance of a bulging belly even worse.
Early recovery from muscle tears during pregnancy
If you’re suffering from; back pain, a lack of strength, or have bulges in the belly area that refuse to yield to consistent abdominal strengthening exercises or pilates, a professional consultation will help you to find out what’s really wrong.
See your Physician, Obstetrician/Gynaecologist or Plastic Surgeon if you suspect your abdominal area has suffered notable muscle damage during pregnancy. They will be able to confirm if you have separated abdominal muscles.
Your Medical Care providers will also be able to help you learn the best methods of; how to lift things properly, how to use good posture, how to get out of bed properly etc. These efforts can sometimes help prevent your separation from worsening. They can also give you a chance to recover as much as possible without surgery.
Next steps: Abdominoplasty Surgery to repair diastasis recti
Tummy Tuck and Abdominal Muscle Repair or Belt Lipectomy
If months or years have passed and your diastasis recti have not recovered, there are additional options for recovery:
- Surgery may be performed if the separation is larger than 2 centimetres.
- During a complete Tummy Tuck procedure (abdominal corrective surgery), a qualified Plastic Surgeon will tighten your abdominal muscles, remove additional skin and reduce excess body fat.
 This procedure will also help to bring the abdominal muscles back together.
This procedure will also help to bring the abdominal muscles back together. - After healing, Tummy Tuck surgery allows your abdominal muscles to work more effectively again.
- This means, all those pilates exercises or crunches will actually have a far better effect.
Some women may only need the muscle tightened, which can be done through a small incision in the bikini line. Patients with a large amount of excess skin will need a more involved surgery – a full tummy tuck. In this procedure, the muscle is tightened, extra skin is removed, and the belly button is relocated.
You Should Have Realistic Expectations
Surgery will not necessarily help you remove excess fat. It will, however, remove skin and the “pooch” of the stomach. If a tummy tuck or other body surgery is combined with liposuction, however, some excess fat can be removed for improved body contours.
What to Do If You Think Your Muscles Are Separated
- First and foremost, be sure you are exercising properly.
 This requires the advice of a physiotherapist or exercise professional with the right qualifications and background.
This requires the advice of a physiotherapist or exercise professional with the right qualifications and background. - You may also be able to get an ultrasound on your abdominal muscles by your Physiotherapist during exercises to see if you’re using the muscles correctly.
- Crunches and certain abdominal exercises, when done improperly, can actually potentially worsen diastasis recti – so be sure to get professional exercise advice from a qualified physiotherapist or exercise physician.
It takes time to get your ‘pre-pregnancy body’ back – and that’s okay. Keep your expectations realistic as pregnancy will permanently change your body.
However, if you are concerned about abdominal muscle separation and a noticeable ‘tummy pouch’ that won’t go away – send our team an enquiry form to discuss the possibility of Tummy Tuck or Belt Lipectomy surgery.
BOOK a Consultation Today at one of our convenient locations in Melbourne and Sydney.
BOOK a FREE 15-minute Phone Chat with our Patient Liaison Manager.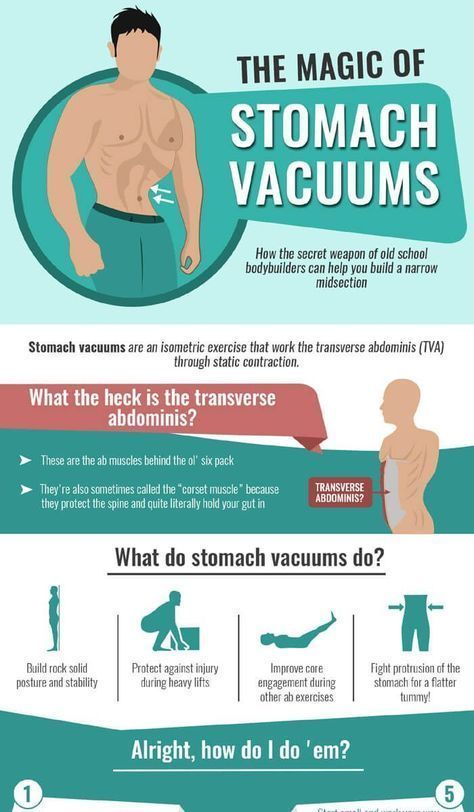
Further Reading about Mummy Makeover
- Find out more about:
- A Mummy Makeover Melbourne by Dr Craig Rubinstein,
- Mummy Makeover Surgery Melbourne by Dr Patrick Briggs,
- Mummy Makeover Melbourne by Dr Rebecca Wyten,
- Abdominal Muscles During Pregnancy Queensland and NSW,
How to Deal With a Pulled Muscle During Pregnancy
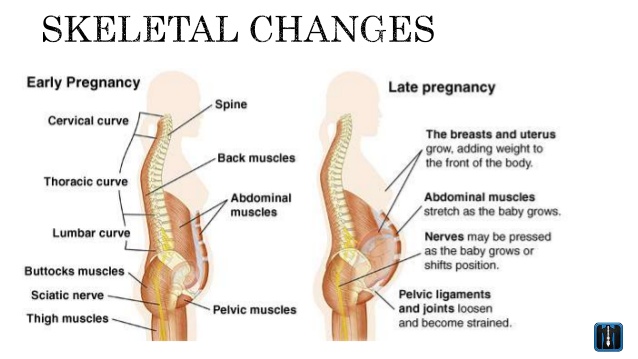
During pregnancy, your body changes a lot. Weight gain, shifting posture, loose joints, and an evolving shape can all contribute to aches and pains, along with stability issues or risk of injury. This is primarily because of relaxin.
It’s pregnancy hormone responsible for relaxing ligaments and arteries throughout the body in order to prepare for labor and delivery, as well as manage increased blood volume. As a pregnant woman, you may consequently experience things like a pulled hamstring, back or hip pain or acid reflux.
This is especially true if you’re working out. Our experts explain why pulled muscles are more common throughout pregnancy, and how to keep your muscles safe to avoid strain.
Why are pregnant women more susceptible to pulled muscles?
“There are a handful of reasons why being [pregnant] makes you more susceptible to pain, injury, and pulled muscles,” says Steve Washuta, a certified personal trainer in Savannah, Georgia. “Firstly, there are hormonal changes: hCG, prolactin, estrogen, progesterone, oxytocin, and relaxin. Relaxin will loosen up ligaments and joints around the pelvic region among other things in preparation for the pregnancy. It has also shown to actually widen feet, making women feel less stable, and clumsy when coupled with weight gain and change of body shape.”
Potassium levels are often lower during pregnancy. Without adequate potassium, muscle flexibility is limited.
A growing belly means that your body weight is distributed toward the front, too. This forces lower back and abdominal muscles to overwork. Plus, as the pelvis widens and shifts, says Washuta, a pregnant woman can experience sciatica in the lower back, hips, glutes or legs.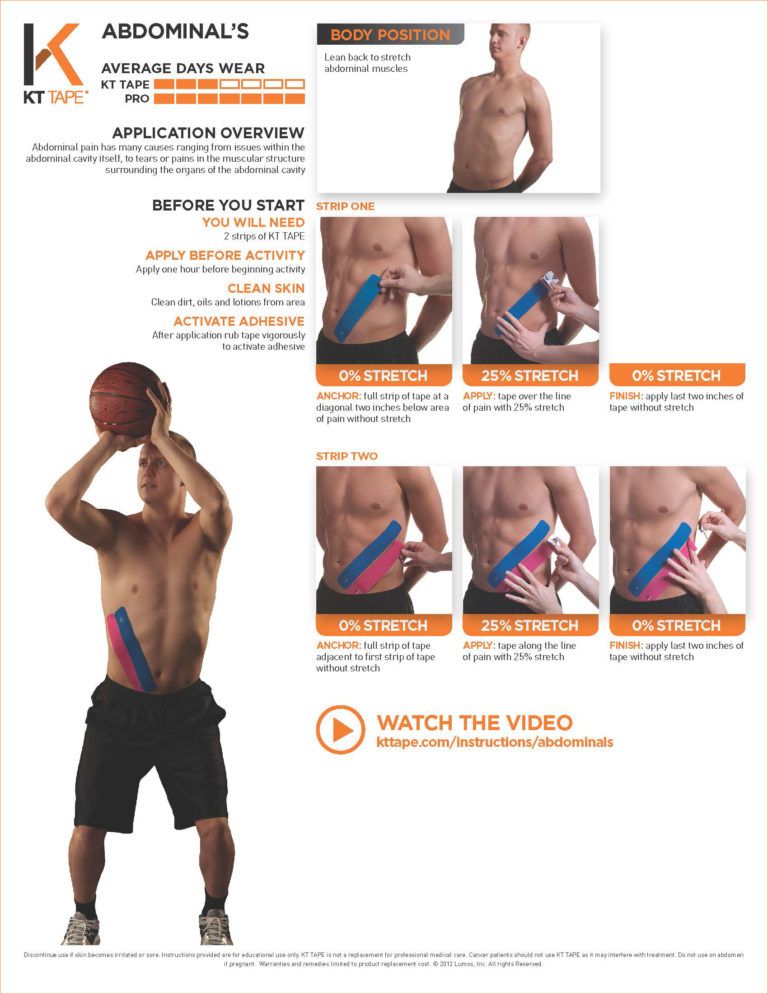 This is due to compression on the nerves.
This is due to compression on the nerves.
Additionally, potassium levels are often lower during pregnancy, adds Dr. Lisa Folden, a licensed physical therapist and naturopathic lifestyle coach. “Without adequate potassium, muscle flexibility is limited, meaning [that] activities that call upon muscle contractions or muscle lengthening can easily result in a muscle tear, pull, or strain,” she says.
What’s the difference between a pulled muscle and a strained muscle?
Many pregnant women are familiar with round ligament pain. It’s a sharp feeling near the low belly or groin area that normally occurs in the second trimester, due to ligaments that stretch as both baby and belly grow. But, pulled muscles are a little different. They’re more similar to a strained—not sprained—muscle than anything else. Aaptiv Trainer Amanda Butler says pulled muscles happen when a muscle, or the tissue connecting muscle to bone, is overstretched or torn. Conversely, sprains involve stretches or tears in ligaments, which connect bone to bone at your joints.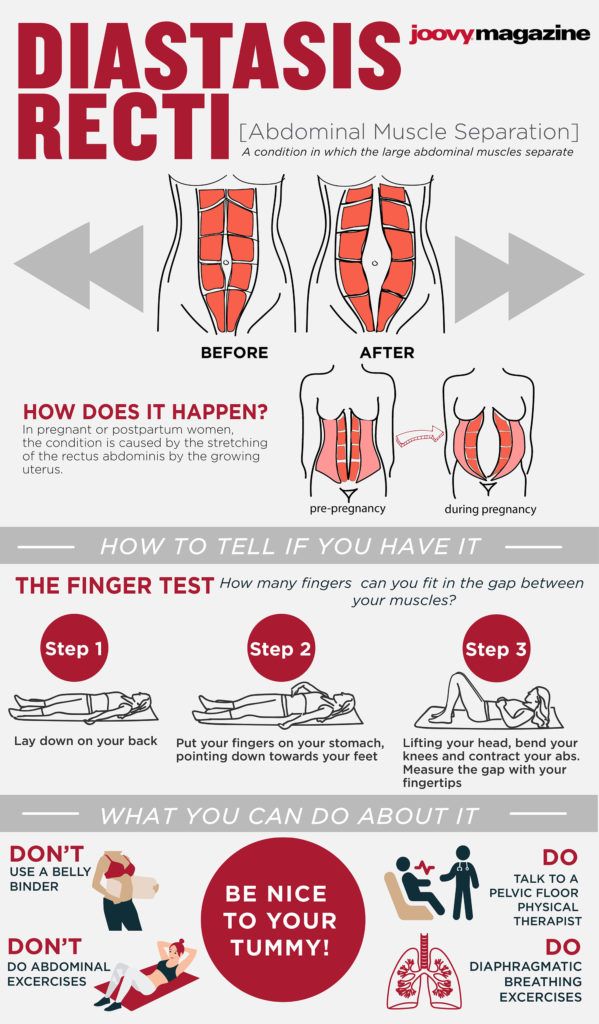
“A ‘pulled’ muscle typically means that the muscle was stretched beyond its ideal limit,” says Dr. Folden. “In this way, a ‘strained’ muscle can be the exact same as a ‘pulled’ muscle. However, ‘straining’ a muscle can also include injuries that result from an over-contraction of the muscle when the muscle is being used from the shortened position.”
All in all, there are three grades of pulled muscles, notes Washuta:
- Grade one is a slight strain with light swelling, hindered range of motion, minimal pain. It takes two to three weeks to full recovery.
- Grade two is when there’s damage to the muscle, but no rupture, with mild swelling. This one takes four to eight weeks before fully healing.
- Grade three results in severe pain. This is due to a complete rupture of the muscle or tendon, with dark bruising and heavy swelling. There’s no range of motion. You may need surgery for repair.
Where do pulled muscles commonly occur for pregnant women?
As mentioned, many women may feel pulling in the groin area related to round ligament pain.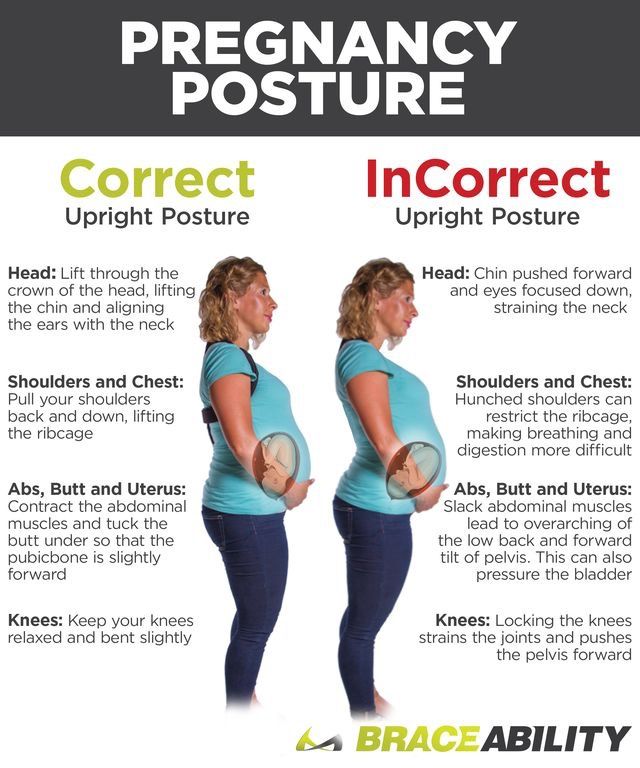 Pulled muscles tend to happen elsewhere, when pregnant women lose their balance, twist an ankle, or strain the lower back and knees. Abdominals and inner thigh muscles are also key targets, says Dr. Kellen Scantlebury of Fit Club Physical Therapy & Sports Performance.
Pulled muscles tend to happen elsewhere, when pregnant women lose their balance, twist an ankle, or strain the lower back and knees. Abdominals and inner thigh muscles are also key targets, says Dr. Kellen Scantlebury of Fit Club Physical Therapy & Sports Performance.
“Pregnant women tend to suffer from pulled muscles in many of the same places as non-pregnant people, like the hamstrings, quadriceps, calves, and low back,” agrees Dr. Folden. “However, one unique pulled muscle that happens often in pregnancy is that of the rectus abdominis (abs or six-pack muscles). This injury occurs when the muscles of the front abdominal wall spread and or split as the uterus grows larger, resulting in diastasis recti.”
How can you protect your body from pulled muscles, especially during exercise while pregnant?
Be mindful that your weight is now front-loaded, says Washuta, meaning that your back muscles are working in overdrive. He recommends seated exercises with back support to allow your back and core muscles to relax.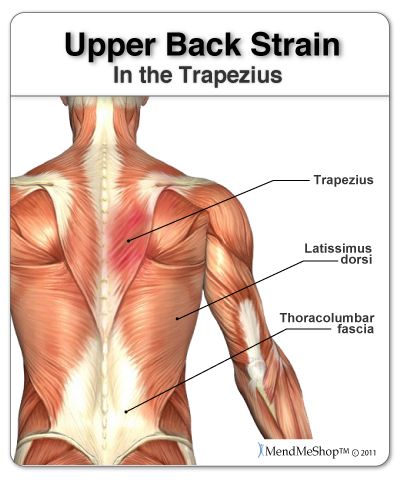 This way you can focus on strengthening specific muscle groups.
This way you can focus on strengthening specific muscle groups.
Also, it’s best to try to stick to the type of exercise that you’re used to doing pre-pregnancy, with proper modifications, rather than introducing something new or strenuous. Dr. Folden suggests stretching and moving as much as possible. If you think you’ve accidentally pulled a muscle, make an appointment with a physical therapist or your doctor.
“Make sure [that] you do a light warm-up, and avoid jumping into a workout cold,” says Butler. “Mild strains can use the ‘RICE’ approach: rest, ice, compress, and elevate. If it’s more severe, see a doctor to make sure [that] there’s not a fracture. Overall, be mindful of your movements. Just because your range of motion can increase during pregnancy doesn’t mean [that] you should push to your new range of motion. Avoid overstretching and work on strengthening exercises instead.”
Aaptiv has maternity-safe workouts that can be easily modified to meet your needs. View our maternity program here.
View our maternity program here.
Diastasis of the rectus abdominis muscles and diastasis of the womb. Solvable problems of pregnancy. Interview with Doctor of Medical Sciences, Professor M.A. Chechnevoy
— What is muscle diastasis and what is pubic symphysis diastasis?
— Pregnancy is an amazing and wonderful time, but it is also a period of additional loads, which undoubtedly becomes a test of strength for the female body.
The previously existing everyday point of view that pregnancy rejuvenates and gives strength is not confirmed by anything. During the bearing of a child, significant additional loads are placed on the mother's body, which often lead to the manifestation of problems that were invisible before pregnancy.
Diastasis of the rectus abdominis muscles is a divergence of the inner edges of the muscles along the white line of the abdomen (connective tissue structure) at a distance of more than 27 mm. Pubic diastasis is one of the manifestations of pregnancy-associated pelvic girdle pain. This pathology affects the entire pelvic ring, sacroiliac joints and symphysis. And they certainly have common causes for the appearance.
This pathology affects the entire pelvic ring, sacroiliac joints and symphysis. And they certainly have common causes for the appearance.
The formation of such problems is facilitated by a decrease in the strength of connective tissue collagen. One of the reasons is an innate predisposition, the so-called connective tissue dysplasia, when the tissues are very elastic, extensible. During pregnancy, the body of a woman increases the production of the hormone relaxin, which reduces the synthesis of collagen and enhances its breakdown. This is provided by nature to create maximum elasticity of the birth canal. However, other structures, such as the anterior abdominal wall and the pubic symphysis, also fall under the action of relaxin.
— How does diastasis of the muscles and diastasis of the pubis affect pregnancy and childbirth?
- The divergence of the rectus abdominis muscles is observed in about 40% of pregnant women. During pregnancy, it does not give serious complications that threaten the life of the mother or the condition of the fetus.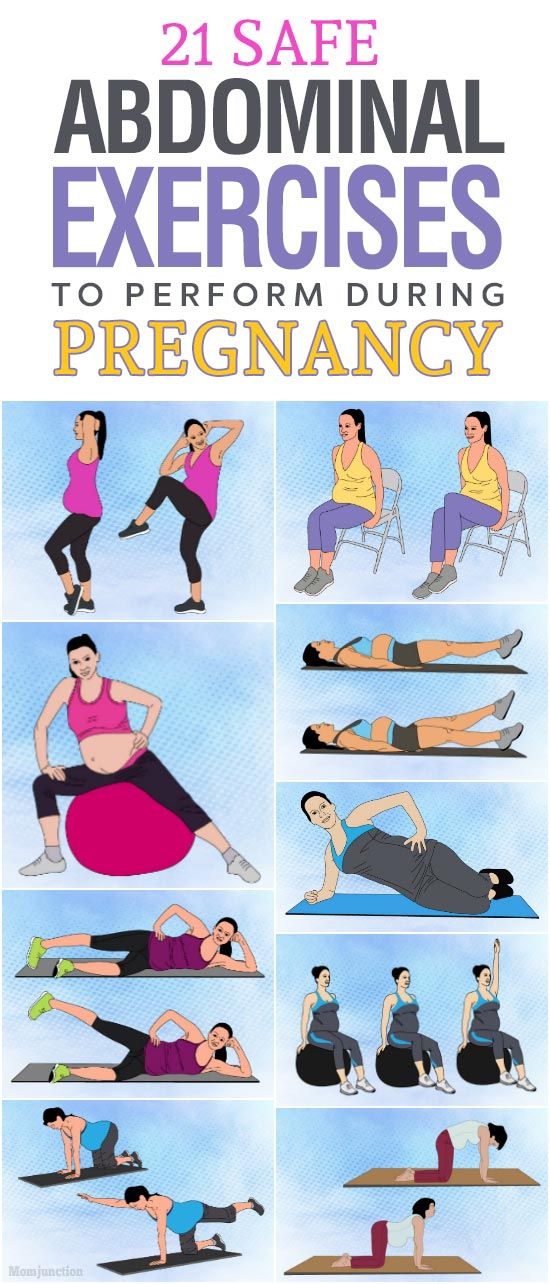 However, the inferiority of the work of the rectus abdominis muscles forces the redistribution of the load on the back muscles, which can lead to lumbar-pelvic pain and, accordingly, discomfort in the back. During childbirth, the abdominal muscles are involved in attempts, and the violation of their anatomy and function can affect the birth act.
However, the inferiority of the work of the rectus abdominis muscles forces the redistribution of the load on the back muscles, which can lead to lumbar-pelvic pain and, accordingly, discomfort in the back. During childbirth, the abdominal muscles are involved in attempts, and the violation of their anatomy and function can affect the birth act.
With diastasis of the pubis, things are more complicated. As already mentioned, this is only one of the manifestations of a violation of the structure and function of the pubic joint (symphysiopathy) during pregnancy. It occurs in about 50% of pregnant women in varying degrees of severity: in 25% of cases it leads to restriction of the mobility of the pregnant woman, in 8% - to severe disorders up to disability.
With symphysiopathy, the ligaments of the pubic articulation and the cartilages that connect the pubic bones are affected. All this leads to severe pain in the pubic joint, pelvic bones, lower back, as well as to a violation of gait and the inability to stand up or lie down without outside help.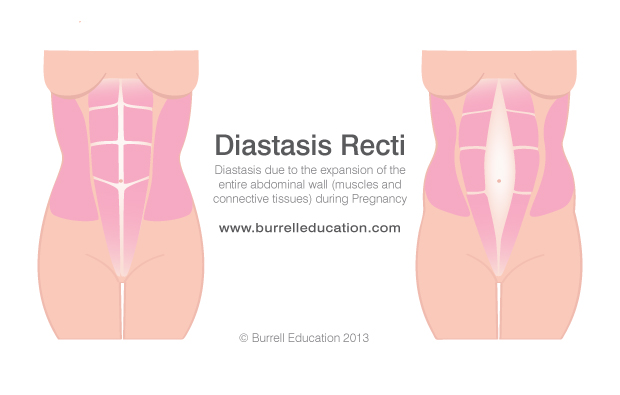 Women with pelvic girdle pain syndrome experience significant levels of discomfort, disability, and depression, with associated social and economic problems. These include impaired sexual activity during pregnancy, chronic pain syndrome, risk of venous thromboembolism due to prolonged immobility, and even seeking early induction of labor or caesarean section to stop pain.
Women with pelvic girdle pain syndrome experience significant levels of discomfort, disability, and depression, with associated social and economic problems. These include impaired sexual activity during pregnancy, chronic pain syndrome, risk of venous thromboembolism due to prolonged immobility, and even seeking early induction of labor or caesarean section to stop pain.
During childbirth, this patient may experience rupture of the pubic symphysis and may require surgery to repair it.
— How to prevent the development of muscle and pelvic diastasis during pregnancy and childbirth? What factors increase the likelihood of its development?
- There is no recipe that will be one hundred percent. There is a wonderful term in the medical literature called "lifestyle modification". Whatever diseases we study, be it symphysiopathy, diabetes mellitus or preeclampsia, the risk group for pathology is always overweight women. You need to prepare for pregnancy, you need to be in good physical shape. During pregnancy, weight gain should be monitored. The recommendation to "eat for two" is not just wrong, but extremely harmful. Pregnant women should maintain reasonable physical activity. Weak and flabby abdominal muscles, combined with the large size of the fetus, undoubtedly increase the risk of diastasis.
During pregnancy, weight gain should be monitored. The recommendation to "eat for two" is not just wrong, but extremely harmful. Pregnant women should maintain reasonable physical activity. Weak and flabby abdominal muscles, combined with the large size of the fetus, undoubtedly increase the risk of diastasis.
The risk factors for symphysiopathy in numerous studies are hard physical labor and previous injuries of the pelvic bones. Factors such as time elapsed from previous pregnancies, smoking, use of hormonal contraception, epidural anesthesia, mother's ethnicity, number of previous pregnancies, bone density, weight and gestational age of the fetus (post-term fetus) are not associated with an increased risk of symphysiopathy.
— How to diagnose diastasis recti and diastasis pubis?
— In most cases, diastasis rectus abdominis can be diagnosed clinically. It happens that inspection, palpation and simple measurements are enough.
In the standing position, you can see the divergence of the muscles when the woman does not have subcutaneous fat. In this case, diastasis is defined as a vertical defect between the rectus muscles.
In this case, diastasis is defined as a vertical defect between the rectus muscles.
With tension of the abdominal press, a longitudinal protrusion is observed in the diastasis zone. Such a protrusion is especially noticeable if the patient in the supine position is asked to raise her head and legs. If necessary, you can measure the width of the defect simply with a ruler.
Ultrasound may be the most accurate diagnostic method. With ultrasound, the inner edges of the rectus muscles are clearly visible and the distance between them at different levels can be measured.
Computed tomography is used in the diagnosis of diastasis extremely rarely, mainly in scientific research.
For the diagnosis of symphysiopathy and diastasis pubis there is no one test as a "gold standard".
The first place, of course, is the questioning and examination of the patient. We pay attention to the gait of the pregnant woman, to how she sits down, lies down and how she gets up. Symphysiopathy is characterized by a “duck gait”, when a pregnant woman rolls from foot to foot. On palpation in the area of the womb, pain and swelling are noted. The so-called pain provocative tests are used, for example, a mat-test (pulling up an imaginary rug, mat with your foot towards you).
Symphysiopathy is characterized by a “duck gait”, when a pregnant woman rolls from foot to foot. On palpation in the area of the womb, pain and swelling are noted. The so-called pain provocative tests are used, for example, a mat-test (pulling up an imaginary rug, mat with your foot towards you).
The following questionnaires are used to assess quality of life, pain and disability: Health-Related Quality of Life (HRQL), Oswestry Disability Index (ODI), Disability Rating Index (DRI), Edinburgh Postpartum Depression Scale (EPDS), Pregnancy Mobility Index (PMI), and Pelvic Ring Score (PGQ).
Of the instrumental methods, ultrasound is the most widely used, less often computed or magnetic resonance imaging. Ultrasound allows you to assess the condition of the ligaments of the pubic joint and the interpubic disc, the severity of the changes and the risk of natural childbirth.
— What is the treatment for diastasis recti or pubis?
— Primary prevention: when planning and during pregnancy, it is necessary to strengthen all muscle groups of the pelvic girdle, as well as the pelvic diaphragm.
More often, diastasis of the rectus muscles disappears on its own during the first months after childbirth. Special physical exercises to correct the work of muscles, to tone them and restore their basic functions should be performed under the guidance of a competent instructor. There are types of physical exercises that can, on the contrary, worsen the situation with diastasis of the rectus abdominis muscles. In some cases, when there is no effect from physiotherapy exercises, it is necessary to resort to surgical correction of the defect. Currently, both endoscopic and open surgery are practiced. The choice of method depends on the size and localization of the defect.
With symphysiopathy, therapeutic exercises reduce lumbar and pelvic pain. Acupuncture and wearing a pelvic bandage have a positive effect on symphysiopathy.
Initial treatment of pubic symphysis should be conservative even if symptoms are severe. Treatment includes bed rest and the use of a pelvic brace or corset that tightens the pelvis. Early appointment of physiotherapy with dosed therapeutic exercises will help to avoid complications associated with prolonged immobilization. Walking should be done with assistive devices such as walkers.
Early appointment of physiotherapy with dosed therapeutic exercises will help to avoid complications associated with prolonged immobilization. Walking should be done with assistive devices such as walkers.
In most cases (up to 93%), the symptoms of dysfunction of the pelvic ring, including the pubic joint, progressively subside and completely disappear six months after birth. In other cases, it persists, becoming chronic. However, if the diastasis exceeds 40 mm, then surgical treatment may be required. Most studies recommend surgery only after failure of conservative treatment, inadequate enlargement of diastasis, or its recurrence. Several procedures have been described, including external fixation and open reduction of the pubic bones with internal fixation.
The best advice for prevention, diagnosis and treatment: ask a competent doctor all the questions that worry you. Only the joint efforts of the doctor and the patient can overcome all problems and find the best solutions.
Diastasis of the rectus abdominis muscles - symptoms, signs, degrees, causes and treatment in men and women in Moscow in the "SM-Clinic"
The surgeon deals with the treatment of this disease
Book online Request a call
- What is diastasis rectus abdominis?
- About disease
- Species
- Symptoms of diastasis recti
- Causes of diastasis recti
- Diagnostics of diastasis of the rectus abdominis muscles
- Expert opinion
- Treatment of diastasis recti
- Surgical treatment of diastasis recti
- Prevention
- Rehabilitation after surgery
- Questions and Answers
- Sources
About the disease
The disease is based on stretching and expansion of the white line of the abdomen - a tendon that is located between the rectus muscles, connects and holds them. This is a strip of connective tissue, consisting of several layers, located in the middle of the abdomen vertically from the xiphoid process to the pubic joint.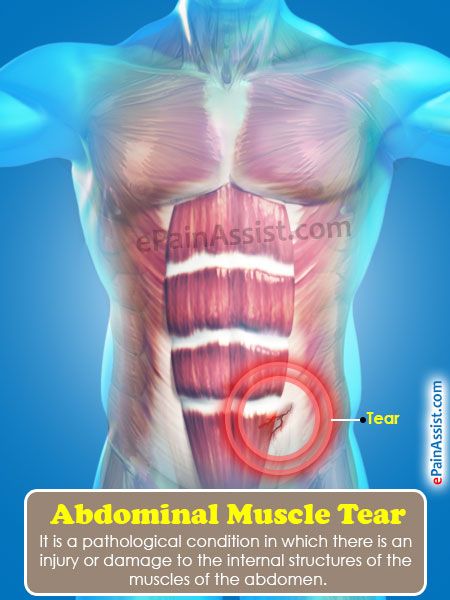
Due to an increase in intra-abdominal pressure or a violation of the properties of the connective fibers, the structure of the tendon changes, it weakens, becomes thinner and stretches. The trigger mechanism is prolonged pressure on the abdominal wall associated with pregnancy or visceral obesity. An aggravating factor is the loosening of the white line against the background of collagenopathy, the effects of relaxin, the immaturity of cellular structures, etc.
As a result, the white line becomes thinner and stretched. Normally, its dimensions are restored with a gradual decrease in the abdomen or as the properties of the connective tissue normalize. Thus, physiological diastasis is eliminated during the neonatal period or in women after childbirth.
If abdominal training is started early in the postpartum period, this leads to contraction of the rectus muscles and a simultaneous increase in intra-abdominal pressure, and the white line is fixed in a stretched position and does not hold the internal organs well. As a result, unaesthetic vertical folds form on the abdomen, a rounded protrusion appears, dysfunction of the digestive tract occurs and the risk of hernia formation increases.
Species
Depending on the magnitude of the stretching of the tendon ligament, there are 3 degrees of diastasis of the rectus abdominis muscles:
- first - the muscles move away from each other by 2.5-5 cm;
- second - ligaments diverge by 5-8 cm;
- third - the line is stretched more than 8 cm.
According to the localization of the place of maximum stretching, supra-umbilical, sub-umbilical and mixed forms of diastasis are distinguished.
According to the degree of involvement of other muscles of the anterior abdominal wall, the pathology is classified into types:
- A - classical divergence of muscles after natural childbirth;
- B - relaxation of the lower lateral sections of the muscles;
- C - expansion affects the region of the ribs and the xiphoid process;
- D - diastasis is combined with a curvature of the waist line.
Symptoms of diastasis of the rectus abdominis muscles
Manifestations of BPMD increase as the pathology progresses. In women, a vivid clinical picture manifests itself abruptly (shortly after childbirth), while in men the disease develops gradually.
At the onset of the disease, there may be no symptoms at all. The patient then notices a characteristic rounded vertical protrusion in the center of the abdomen. With deliberate tension of the press, the inner edges of the rectus muscles and the groove between them are clearly visible. Due to muscle dysfunction, pain in the spine, lower back, fatigue, and posture disorders are possible.
With the progression of the pathology, manifestations of dysfunction of the gastrointestinal tract join:
- heartburn;
- belching;
- flatulence;
- abdominal pain;
- constipation.
In the third stage of diastasis, patients are faced with the formation of hernias, which are formed due to structural defects in the white line.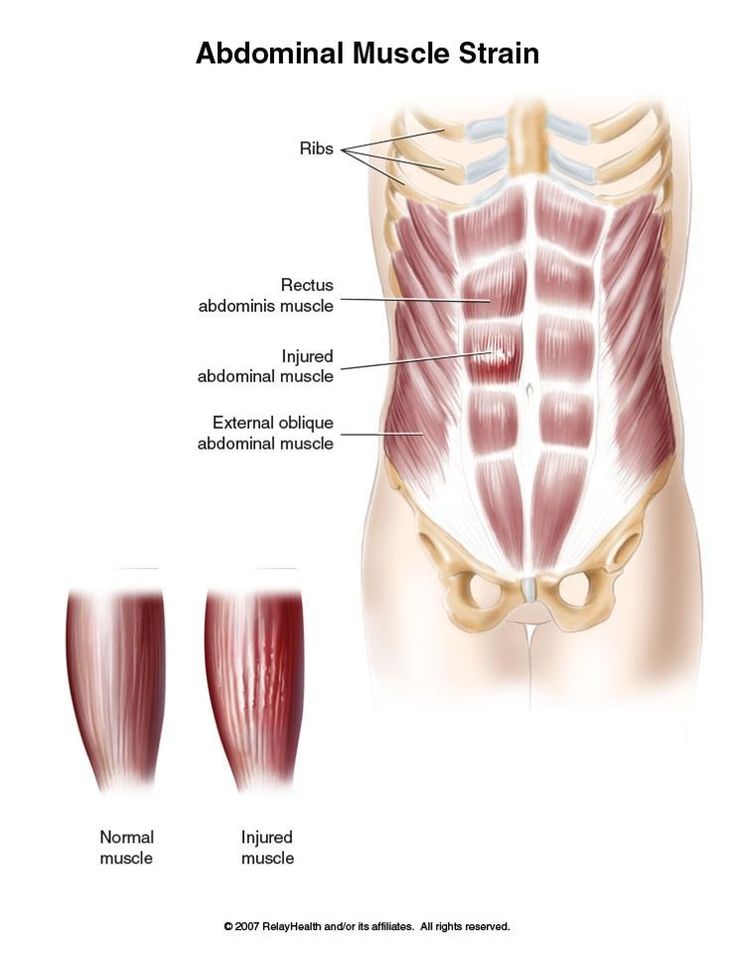 Possible ptosis (omission) of internal organs and serious disturbances in the work of the intestines (in severe cases, intestinal obstruction develops). Women often experience urinary incontinence, renal colic.
Possible ptosis (omission) of internal organs and serious disturbances in the work of the intestines (in severe cases, intestinal obstruction develops). Women often experience urinary incontinence, renal colic.
Causes of diastasis recti
Increase the risk of developing diastasis pathology of the connective tissue and increased pressure in the abdominal cavity. In different categories of patients, the causes of the development of PMSD are different.
Divergence of muscles in children is due to the failure of the musculature and tendons. After 2-12 months after birth, the muscles come into tone, the ligaments and tendons are strengthened - the process resolves itself. In premature babies and infants with intrauterine developmental pathologies, this may take longer. With Down syndrome, there is a risk of maintaining diastasis for life.
Pregnancy is the provocateur of diastasis of the rectus abdominis muscles in women. The growing uterus puts considerable pressure on the linea alba, stretching it. Under the action of hormones, the synthesis of collagen fibers is inhibited, the ligaments become looser. But a few months after the birth, the white line of the abdomen is normally restored.
Under the action of hormones, the synthesis of collagen fibers is inhibited, the ligaments become looser. But a few months after the birth, the white line of the abdomen is normally restored.
In men, BMD is often provoked by obesity, physical activity and hereditary collagenopathies. The risk of diastasis increases with a tendency to constipation, as well as with chronic respiratory diseases accompanied by coughing.
Treatment of pathology by conservative methods is possible with a small diastasis. At the later stages of development, the pathological divergence of muscles is eliminated with the help of abdominal plastic surgery.
Get advice
If you experience these symptoms, we recommend that you make an appointment with your doctor. Timely consultation will prevent negative consequences for your health.
You can find out more about the disease, prices for treatment and sign up for a consultation with a specialist by phone:
+7 (495) 292-39-72
Request a call back Book online
Why SM-Clinic?
1
Treatment is carried out in accordance with clinical recommendations
2
A comprehensive assessment of the nature of the disease and treatment prognosis
Modern diagnostic equipment and own laboratory
4
High level of service and a weighted price policy
Diagnosis of diastasis of the rectus abdominis muscles
Identification of BPMD is not difficult, since the disease has characteristic clinical manifestations.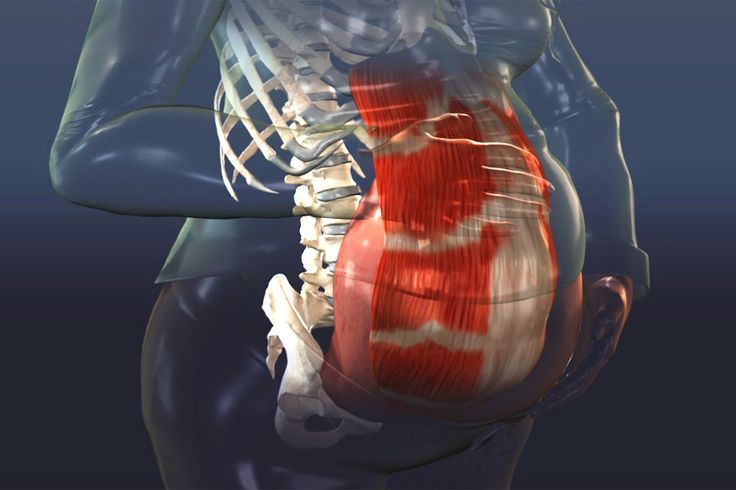 With signs of diastasis, you should contact the surgeon.
With signs of diastasis, you should contact the surgeon.
An increase in the space between the rectus muscles is determined during palpation of the abdomen. To conduct the test, the patient is asked to lie on his back, legs slightly bent at the knees, and then tighten the abdominal muscles, raising his head and shoulder blades. In patients with obesity, the doctor is not always able to fully explore the width of the white line.
The exact size of the sprain is determined by ultrasound. This diagnostic method also allows you to detect complications (hernia, displacement of internal organs). In order to differentiate the symptoms of diastasis and manifestations of chronic diseases of the gastrointestinal tract or the genitourinary system, consultations of specialized specialists are prescribed.
Expert opinion
Surgeons warn that diastasis rectus abdominis is asymptomatic for a long time. Therefore, in the presence of predisposing factors (recent pregnancy and childbirth, chronic constipation, obesity) or non-specific complaints, you should independently feel the white line of the abdomen in the navel. If the distance between the rectus muscles is more than 2.5 cm, contact the surgeon. Also, do not delay the visit in any doubtful cases. Only a doctor can establish the correct diagnosis, self-examination does not exclude the need for an in-person consultation.
If the distance between the rectus muscles is more than 2.5 cm, contact the surgeon. Also, do not delay the visit in any doubtful cases. Only a doctor can establish the correct diagnosis, self-examination does not exclude the need for an in-person consultation.
Egiev Valery Nikolaevich, surgeon, oncologist, doctor of medical sciences, professor, head of the department of surgery and oncology, FPC MR MI PFUR
Treatment of diastasis recti
Functional diastasis in newborns and puerperas does not require treatment. Doctors use expectant tactics, recommend adhering to the principles of rational nutrition, doing massages, and doing gymnastics. The observation period can last up to 12 months. If after this time the problem persists, the surgeon decides on an operative method of correction.
Conservative treatment
Patients are prescribed a diet to prevent constipation and excessive gas formation, as well as to gradually reduce weight. In the postpartum period, incl.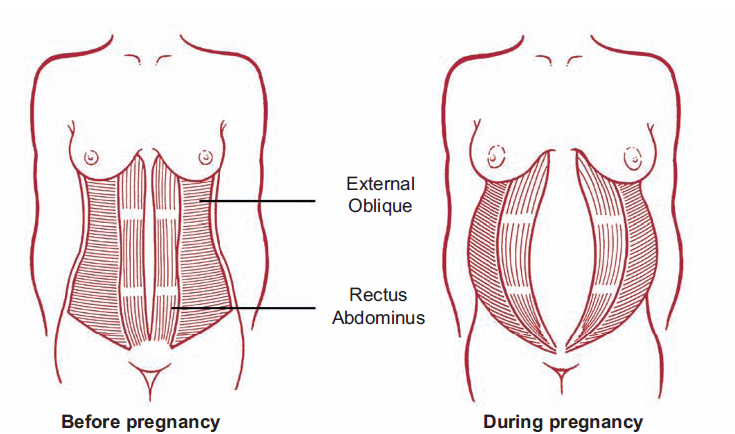 after a caesarean section, women are advised to wear a bandage, support the stomach during sneezing and coughing. The general strengthening of the muscles allows you to quickly restore the tone of the anterior abdominal wall, so patients are prescribed exercise therapy, swimming, yoga classes. It is important to exclude any training of the abdominal muscles. You can not perform exercises in the knee-elbow position, as well as in the emphasis (bar). Such loads can be resumed after the restoration of the size of the white line. Conservative treatment is effective only at the 1st stage of BPMD.
after a caesarean section, women are advised to wear a bandage, support the stomach during sneezing and coughing. The general strengthening of the muscles allows you to quickly restore the tone of the anterior abdominal wall, so patients are prescribed exercise therapy, swimming, yoga classes. It is important to exclude any training of the abdominal muscles. You can not perform exercises in the knee-elbow position, as well as in the emphasis (bar). Such loads can be resumed after the restoration of the size of the white line. Conservative treatment is effective only at the 1st stage of BPMD.
Surgical treatment of diastasis of the rectus abdominis muscles
In case of complicated and uncomplicated diastasis of the rectus abdominis muscles of the 2-3rd degree, surgical treatment is indicated. It is possible to use the following surgical techniques:
- Tension plastic using own tissues. It involves stitching the edges of the muscles with the removal of excess connective tissue.
 To date, it is not used due to the high risk of recurrence.
To date, it is not used due to the high risk of recurrence. - Tension-free repair with a mesh prosthesis. It implies the introduction of an endoprosthesis under the site of stretching.
- Tension plastic with prosthesis installation. It involves the removal of excess connective tissue, suturing the edges of the muscles and strengthening the zone with a polypropylene mesh.
- Combined technology. Includes muscle suturing, mesh strengthening, removal of excess adipose tissue and stretched skin.
Prevention
To reduce the risk of developing diastasis rectus abdominis, you should keep your body in shape - engage in regular exercise, train your muscles. However, do not overdo it: lifting weights can, on the contrary, become the main cause of muscle divergence.
It is also important to eat a nutritious and balanced diet - a lack of nutrients will lead to a decrease in the elasticity of the connective tissue.
It is necessary to control your weight - body mass index should not exceed 26 kg/m3.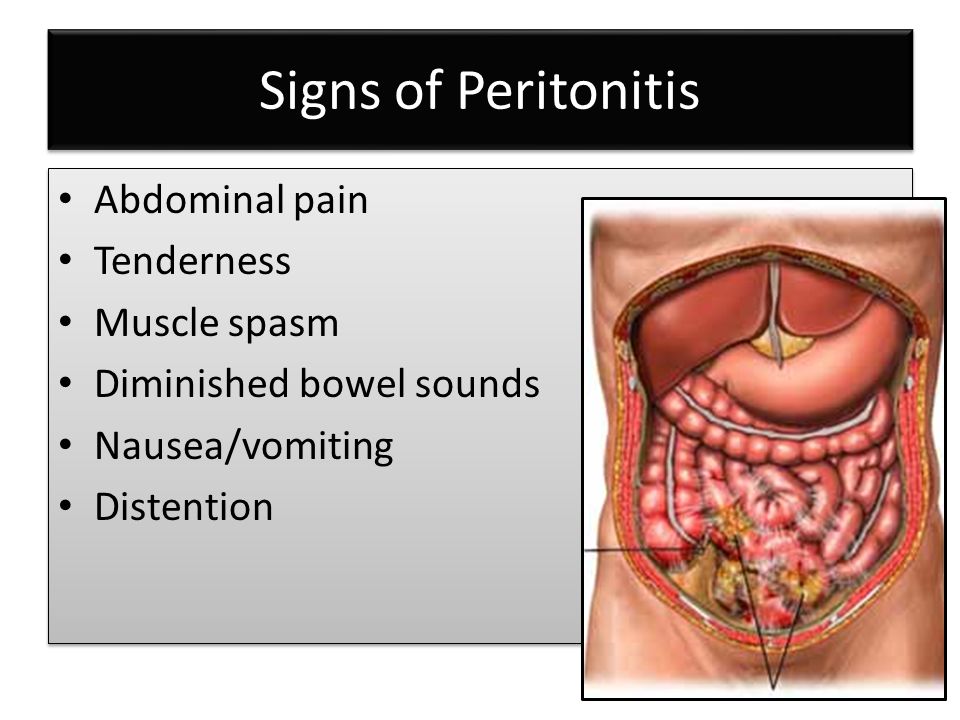 Obesity, especially of the abdominal type, is an important risk factor for BLV.
Obesity, especially of the abdominal type, is an important risk factor for BLV.
Prevention and timely treatment of chronic lung diseases accompanied by cough, pathologies of the digestive system, occurring with constipation, will reduce the possibility of increasing intra-abdominal pressure and, as a result, the likelihood of diastasis.
Rehabilitation after surgery
After surgery, the patient is under inpatient observation, receiving analgesic and antibiotic therapy. Full recovery lasts 1-3 months. During this period, the patient is prescribed a diet to normalize defecation, it is recommended to avoid significant physical exertion, weight lifting. To prevent excess tension, it is necessary to wear a bandage.
Questions and Answers
A surgeon deals with the treatment of pathology.
In the stronger sex, obesity and connective tissue dysplasia are considered to be the main cause of BMD. Sharp weight loss or weight gain, excessive passion for power loads are capable of provoking muscle divergence. If a man or close relatives have hernias, varicose veins, valgus flat feet, hemorrhoids, this is regarded as an increased tendency to PMSD.
If a man or close relatives have hernias, varicose veins, valgus flat feet, hemorrhoids, this is regarded as an increased tendency to PMSD.
There is no need to rush in this matter. Just the desire to quickly get in shape is the main reason for the progression of diastasis in women. Physical activity can be resumed 1-2 months after birth. You can start with hiking or yoga. Abdominal exercises can be performed soon after the white line is reduced to 2 cm. It is advisable to pay attention to the diet. A smooth decrease in weight and volume of visceral fat will ensure gradual and timely muscle contraction. Sharp weight loss, on the contrary, can increase diastasis.
You can lie on a hard surface on your back, tense your abs. With gentle movements of the fingers, you should begin to probe the stomach in the middle in the navel. With a normal width of the white line and with diastasis, a depression will be found - this is the median ligament. If its width is equal to or greater than the width of two fingers, you should contact the surgeon. Constipation, bloating and abdominal pain should be alarming. If there are such symptoms, it is necessary to get to the surgeon in the near future.
Constipation, bloating and abdominal pain should be alarming. If there are such symptoms, it is necessary to get to the surgeon in the near future.
Pathogenesis and treatment of ventral hernias and diastasis of the rectus abdominis muscles: Abstract of the thesis / Zagirov U.Z. - 1995.
Comparative aspects of methods for eliminating diastasis of the rectus abdominis muscles / Topchiev MA, Bondarev VA, Elderov S.Sh.// Astrakhan Medical Journal. - 2010.
Jessen M. L., Öberg S., Rosenberg J. Treatment Options for Abdominal Rectus Diastasis // Front Surg. - 2019. - No. 6. - R. 65
>
Diseases referred by the Surgeon
Appendicitis Ascites Atheroma femoral hernia Crohn's disease Bursitis Hernia Hernia of the white line of the abdomen hiatal hernia Cholelithiasis Keratoma salivary gland cyst Lipoma Bowel obstruction Oleogranuloma kidney tumor Acute pancreatitis Inguinal hernia Peritonitis Barrett's esophagus Polycystic kidney disease Postoperative hernia Umbilical hernia Heel spur Stomach cancer Reflux esophagitis (GERD) Thyroiditis Furuncle (boil) Furunculosis Cholecystitis Peptic ulcer of the stomach and duodenum
All doctors
VDNKh metro station
Belorusskaya metro station
Lesnaya, 57, pp.