20 weeks pregnant miscarriage
Understanding Second Trimester Loss | Obstetrics and Gynecology
Pregnancy loss in the second trimester can be the result of a very preterm delivery (like a spontaneous miscarriage in the second trimester) or death of the fetus (called a fetal demise). About 2-3% of pregnancies will be lost in the second trimester, a rate that is much lower than in the first trimester. Once a pregnancy gets to about 20 weeks gestation, less than 0.5% will end in a fetal demise.
A loss at this time in pregnancy is most often a hard and sad experience. Many friends and family already know you are pregnant. What do you do? What do you say? For most women and their partners, the process of grieving is no different than losing a person who has been in your life for some time. You often have hopes and dreams about your child before that child is born, and losing the pregnancy in the second or third trimester is certainly a loss for a family.
Why see a UC Davis Health specialist?
Our specialists can evaluate you quickly in an office setting. Any laboratory testing or ultrasound examinations that need to be done can be performed easily and conveniently. We perform our own ultrasound examination in the office and can share the results with you immediately. Treatment of a second trimester loss is very different than early miscarriage, and our specialists can provide all options to you and your family. We understand that losses at this time require both emotional and medical support. We are happy to review all treatment options but also know that you may need some time. It is also important for you to know that a fetal demise in the second trimester is not a medical emergency so treatment is not immediately indicated.
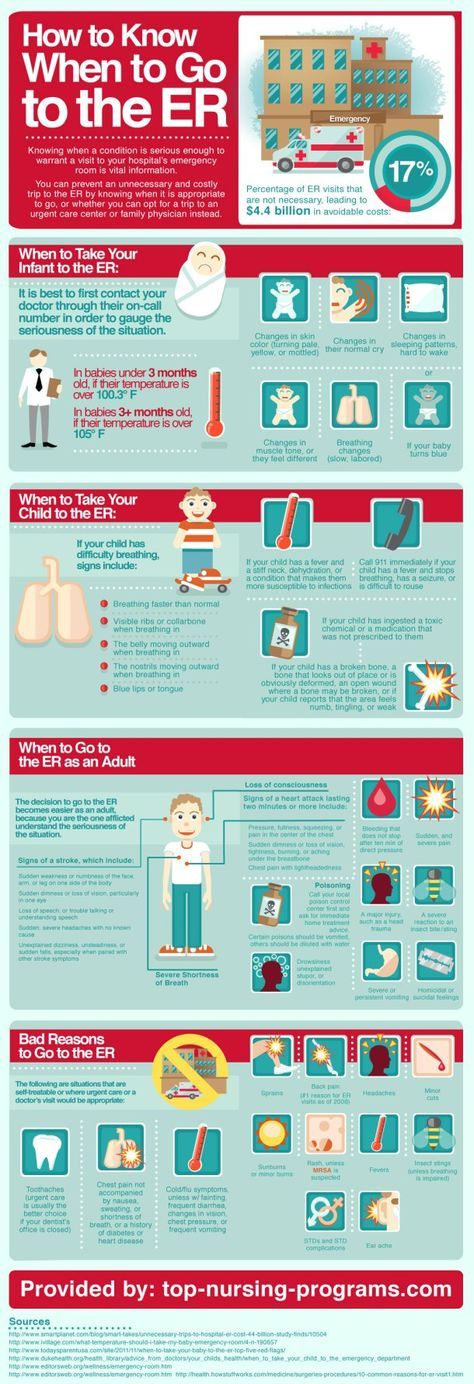
If you are having very heavy vaginal bleeding or are feeling very sick, you should go to the Emergency Room to see our physicians.
Symptoms of a second trimester loss
- Bleeding: Most commonly, bleeding is a sign of a problem with the placenta and does not indicate a fetal demise. But, bleeding can be a sign that the cervix is opening without labor (called cervical insufficiency).
 With cervical insufficiency, the cervix begins to open early without contractions; as the cervix opens more, contractions then follow.
With cervical insufficiency, the cervix begins to open early without contractions; as the cervix opens more, contractions then follow. - Cramping: Pregnancy losses in the second trimester can be due to early labor.
- Loss of fetal movement: This can indicate a fetal demise. Most women can feel the baby moving by the 20th week. If the baby has been moving and you no longer feel that same movement, it is important to contact the doctor’s office immediately to make sure the baby is fine. Decreased fetal movement is more commonly a sign that there is a problem with the pregnancy and only rarely does it mean the fetus has died.
Most women less than 20 weeks of pregnancy do not notice any symptoms of a fetal demise.
The test used to check for a fetal demise in the second trimester is an ultrasound examination to see if the baby is moving and growing. Fetal demise is diagnosed when the ultrasound examination shows no fetal heart activity.
What causes a second trimester loss?
The causes of a pregnancy loss in the second trimester are very different than early pregnancy loss. There are medical conditions that increase the risk for cervical insufficiency or preterm labor before viability which include:
There are medical conditions that increase the risk for cervical insufficiency or preterm labor before viability which include:
- Prior surgery to the cervix
- Use of illicit drugs, especially cocaine
- Fetal abnormalities (genetic or structural problems)
- Uterine infection (this is more common in developing countries and less common in the United States)
- Physical problems with the uterus, including fibroids or abnormalities in the shape of the uterus
There are also some medical conditions that are associated with fetal death in the second trimester which include:
- Fetal abnormalities (genetic or structural problems)
- Poorly controlled maternal cnoditions like thyroid disease, diabetes or hypertension
- Lupus (systemic lupus erythematosus)
- Autoimmune or genetic conditions that increase a woman’s risk of forming blood clots in her legs or her lungs (like antiphospholipid syndrome)
- Very early pre-eclampsia or eclampsia of pregnancy
- Trauma
The specialists at UC Davis Health will review with you what testing is indicated to help learn more about why a second trimester loss occurred. Despite the testing that is available, about half of the time there is no identifiable reason for a second trimester loss. We can work with you to figure out what may be helpful with a next pregnancy or to learn more about medical issues that are important for your future.
Despite the testing that is available, about half of the time there is no identifiable reason for a second trimester loss. We can work with you to figure out what may be helpful with a next pregnancy or to learn more about medical issues that are important for your future.
Treatment of a second trimester loss
It is typically not safe for a woman to wait for the pregnancy to deliver on its own with a second trimester loss. There is a high chance of having significant bleeding when a pregnancy in the second trimester delivers on its own at home. In the case of fetal demise, a dead fetus that has been in the uterus for 4 weeks can cause changes in the body’s clotting system. These changes can put a woman at a much higher chance of significant bleeding if she waits for a long time after the fetal demise to deliver the pregnancy.
Our doctors are committed to providing all available treatment options. Testing to figure out the cause of the pregnancy loss can be performed regardless of the method a woman chooses for termination.
We understand that a second trimester loss is an emotional and stressful time and we want to ensure that the emotional needs of you and your family are met as well. We understand this is a time that you need support and we are sensitive to your wishes for remembrances and religious preferences. We will discuss these issues with you before any treatment.
When a diagnosis of fetal demise in the second or third trimester is made, options include:
- Surgical evacuation: This procedure, called a dilation and evacuation, can be performed in the second trimester, typically up to about 24 weeks. Surgical evacuation is the most common treatment women choose and involves removing the pregnancy through the cervix in the operating room while you are asleep. The cervix needs to be opened about 1-2 inches in diameter. The doctors can use different ways to open the cervix based on how far along the pregnancy is and your individual circumstance. The goal is to provide the safest care for each patient.
 After a surgical evacuation, normal activity can typically be resumed the following day. Opening or preparing the cervix for surgical evacuation of the pregnancy may involve:
After a surgical evacuation, normal activity can typically be resumed the following day. Opening or preparing the cervix for surgical evacuation of the pregnancy may involve: - Medicines (tablets) that are put in the vagina a few hours to one day before the procedure.
- Medicine (tablets) that you hold between your cheek and gums for 30 minutes before swallowing. You would use this medicine a few hours before the procedure.
- Placing thin sticks in your cervix, called osmotic dilators, to absorb water from the cervix which causes the dilator sticks to swell slowly over 4-24 hours. Having the osmotic dilators placed is similar to getting a Pap test.
Labor induction: This treatment uses medicines to cause the uterus to go into labor. For women with pregnancies beyond 24 weeks, this is commonly the only option. If you choose this option, you will be in the Labor and Delivery Unit at UC Davis Medical Center and will have all of the same pain treatments available to you as a woman who is naturally in labor (like IV pain medications or an epidural). The treatment typically starts with swallowing a pill to make the uterus more sensitive to the medications to induce labor. About 24 hours later, you are admitted to the Labor and Delivery Unit and will have medicine (tablets) put in the vagina every few hours to cause labor. Sometimes, women need medicine through an IV to also help get labor started. It may take 1-2 days for the uterus to go into labor and for the delivery to be complete. Up to 5% of women in the second trimester do not go into labor and need a surgical evacuation.
The treatment typically starts with swallowing a pill to make the uterus more sensitive to the medications to induce labor. About 24 hours later, you are admitted to the Labor and Delivery Unit and will have medicine (tablets) put in the vagina every few hours to cause labor. Sometimes, women need medicine through an IV to also help get labor started. It may take 1-2 days for the uterus to go into labor and for the delivery to be complete. Up to 5% of women in the second trimester do not go into labor and need a surgical evacuation.
Your doctor will be able to explain more details about the pros and cons of each treatment.
After treatment of a second trimester loss
Bleeding may continue for several weeks after a labor induction but tends to be much lighter with a surgical evacuation. Any bleeding may change in color from bright red to pink or brown. Lower abdominal cramping in the few days after treatment is also common. You should contact a doctor right away if the bleeding gets heavier instead of lighter over time, if a fever develops, or if vaginal discharge or a strange or unpleasant vaginal odor occurs. Avoid intercourse, douching, or using tampons for one week. Regular activities can be resumed right away, based on how you feel. Importantly, if you want to delay getting pregnant, it will be very important to start an effective method of contraception.
Avoid intercourse, douching, or using tampons for one week. Regular activities can be resumed right away, based on how you feel. Importantly, if you want to delay getting pregnant, it will be very important to start an effective method of contraception.
FAQs about second trimester loss
Q: What is cervical insufficiency?
A: This diagnosis is made when a woman has dilation of the cervix during the second trimester without having any contractions or signs of a uterine infection. Some studies suggest that some types of surgeries performed when women have advanced pre-cancerous changes in the cervix can increase the risk of cervical insufficiency. These surgeries include cervical conization (also known as a “cone biopsy”) or if a patient has had multiple LEEP procedures. With these surgeries, part of the cervix is removed to get rid of the pre-cancerous changes. Having these procedures increases the risk of having a second trimester loss by about 1%. In women who have these types of procedures, the chance of having cervical insufficiency is about 1.5%.
In women who have these types of procedures, the chance of having cervical insufficiency is about 1.5%.
Q: What treatments are available if one of the tests shows I have a medical problem that increased the chance of a second trimester loss?
A: Our specialists will work with you to maximize your health status before you try to get pregnant again. For some women, this may mean treatment of a thyroid condition, improved control of diabetes, or changing medications being used for chronic illnesses. Some conditions may require blood thinners like aspirin or injectable medications that should be started early in the next pregnancy (after a normal pregnancy is seen with an early ultrasound exam).
Q: In my last pregnancy, I didn’t get any genetic testing and had a second trimester demise related to a genetic abnormality. What genetic testing is available for my next pregnancy to help figure out if the pregnancy is normal so I can learn earlier if the pregnancy is genetically normal?
A: It will be important to meet with a genetic counselor, if possible, before your next pregnancy, who can also review the details of the available tests. The counselor can also talk with you more about your history and your family history to make sure no genetic or familial medical problems are missed. There are a few different tests, all of which can be performed early in pregnancy, depending on what is right for you. Screening for some of the most common chromosomal abnormalities just from your blood (called NIPT or non-invasive prenatal testing). First trimester screening can be performed between 11 and 14 weeks which involves a blood test and an ultrasound examination. In some situations, chorionic villus sampling (a biopsy of the placenta) or expanded prenatal screening may be indicated. Our specialists and genetic counselors can work with you and your family to help you understand all of these tests and figure out what approach is right for you.
The counselor can also talk with you more about your history and your family history to make sure no genetic or familial medical problems are missed. There are a few different tests, all of which can be performed early in pregnancy, depending on what is right for you. Screening for some of the most common chromosomal abnormalities just from your blood (called NIPT or non-invasive prenatal testing). First trimester screening can be performed between 11 and 14 weeks which involves a blood test and an ultrasound examination. In some situations, chorionic villus sampling (a biopsy of the placenta) or expanded prenatal screening may be indicated. Our specialists and genetic counselors can work with you and your family to help you understand all of these tests and figure out what approach is right for you.
Q: After a second trimester loss, how long should I wait before I try to conceive again?
A: There is really no good information available to show the absolute right answer to that question. First, it may take a month or two to have any testing completed to help figure out why you had a second trimester loss. We know that it takes some time for your uterus and your body to get back to normal. The specialists at UC Davis usually recommend waiting at least 3 months after a second trimester loss before trying again to get pregnant.
First, it may take a month or two to have any testing completed to help figure out why you had a second trimester loss. We know that it takes some time for your uterus and your body to get back to normal. The specialists at UC Davis usually recommend waiting at least 3 months after a second trimester loss before trying again to get pregnant.
Losing a baby at 20-24 weeks of pregnancy
Babies born showing no signs of life before 24 weeks of gestation cannot by law be officially registered as a stillbirth (for more information see Overview) and are referred to as a miscarriage. The effects of this legal limit impacted on parents in both practical and emotional ways. The parents that we spoke to felt extremely strongly that the word ‘miscarriage’ was completely inappropriate and did not in any way describe their lived experience. The reality of losing a baby after 20 weeks was very different to what they imagined, or had experienced, an earlier miscarriage as being. They reflected on the pain of labour and giving birth to a “formed, tiny, perfect” baby which felt more than a miscarriage. Many parents had held their baby in their arms, sung to them, washed and dressed them and had a funeral for them. Maxine felt very strongly that “we've gone through everything that you would for a normal baby”.
They reflected on the pain of labour and giving birth to a “formed, tiny, perfect” baby which felt more than a miscarriage. Many parents had held their baby in their arms, sung to them, washed and dressed them and had a funeral for them. Maxine felt very strongly that “we've gone through everything that you would for a normal baby”.
Mike and Emily were anxious about how their baby might look, but she was like a very tiny baby.
Mike and Emily were anxious about how their baby might look, but she was like a very tiny baby.
View full profile
SHOW TEXT VERSION
EMBED CODE
PRINT TRANSCRIPT
Mike: I remember the nurse saying that she looked great when she was born. And she was, she was - she was exactly what you'd expect a baby to look like, but just smaller, like everything was there in proportion, nothing –Emily: Perfectly formed, yeah.
Mike: Like I mean, it wasn't like a - like a fetus, you know, they're slightly still developing. Like she, she was ready. All she was going to do from there was get bigger.
Emily: Mmm.
Mike: She was perfectly formed. So, to –
Emily: I think we were even shocked at that. Because I –
Mike: Yeah.
Emily: -that was one of the things I was really anxious about, it's like, what is she going to look like? Is it going to be disgusting?
Mike: Fingernails, and little things like that, as well. Just these tiny details that - to me, that's - that wasn't a miscarriage. In no way, shape or form. Medically it was. But I don't, I don't think it was.
Emily: Because I - yeah, we were worried of what she'd look - I didn't know if she'd still look sort of like blobby, or - you know, be squid-, I don’t know. I just didn't know what to expect at all. So, I, we were both surprised, weren't we?
So, I, we were both surprised, weren't we?
Mike: Yeah.
Emily: And when we've shown people photos, they're like "Oh, my goodness - she is a, like just a tiny little baby." So, yeah. I think that terminology - I don't know how you’d, on earth you'd go around changing it. But I do feel like it doesn't do justice to what we went through.
Kelly hated the term miscarriage.
Kelly hated the term miscarriage.
View full profile
SHOW TEXT VERSION
EMBED CODE
PRINT TRANSCRIPT
I found that really, really hard. Because Grace was born at twenty three weeks. And to me, she looked like a baby. And it upset me for them to call her like a miscarriage. Or like the - what they used as the terminology.Because to me, I've heard of babies surviving at twenty three weeks. And continuing. I just can't understand why they use that terminology.
And continuing. I just can't understand why they use that terminology.
I don't - yeah. I, the one I lost at fifteen weeks, I would say yes, a miscarriage. But not the one I lost at twenty three weeks. I hated the terminology, it really upset me.
I think there needs to be some other terminology used.
Many of the parents we spoke to were treated as if they were having a baby not a miscarriage by hospital staff caring for them. They really appreciated this level of care. Sarah felt “it was nice that they were treating him as a baby, a child that we had lost, rather than a miscarriage and I think these are all the kind of things that made a massive difference to how we dealt with it afterwards.” Some mothers talked about how using the term ‘miscarriage’ had failed to prepare them for the experience of going through labour, giving birth, seeing and spending time with their baby . Camille felt it would have helped if “instead of using that horrible word 'miscarriage', they should have said ‘you're about to have a baby’”.
Courtney felt she wasn’t prepared for giving birth to her son because everyone told her she was having a miscarriage.
Courtney felt she wasn’t prepared for giving birth to her son because everyone told her she was having a miscarriage.
View full profile
SHOW TEXT VERSION
EMBED CODE
PRINT TRANSCRIPT
And then labour happened. And, you know? The fact that I had to go through the whole process of giving birth and everything, actually like - I just didn't feel like that I was going to have to have him. I didn't realise how big he was going to be, and how formed he was. You know? I thought like - Because they kept saying to me, "Oh, it's a miscarriage. It's a miscarriage." Because obviously before twenty four weeks, they don't count it as a live baby.
But so in my head I was like 'it's not going to be like this, it's going to be like, like just blood or whatever'. But you know, I had to full on give birth, and. And they had to take the baby out. And then I had to give birth to the placenta.
Maxine felt an early miscarriage was very different to giving birth and holding her baby born at 21 weeks of pregnancy.
Maxine felt an early miscarriage was very different to giving birth and holding her baby born at 21 weeks of pregnancy.
View full profile
SHOW TEXT VERSION
EMBED CODE
PRINT TRANSCRIPT
And I think there's those two groups of people who talk about what's happened, the people who - you know - are very - have a very early miscarriage, before twelve weeks. Or people who will have a proper baby to hold, and to - you know - even if it is stillborn. And then there's that people in the middle, who - I didn't have a clue what I'd have to do. I kind of thought I might go to the toilet and the baby would go. And it, it doesn't work like that.
And then there's that people in the middle, who - I didn't have a clue what I'd have to do. I kind of thought I might go to the toilet and the baby would go. And it, it doesn't work like that. Parents felt losing a baby at any stage of pregnancy was devastating but that more consideration should be given to the impact of losing a baby so close to the 24 weeks cut off when the death would be considered a stillbirth and legally registered. Some parents we spoke to had experienced a miscarriage early in a different pregnancy and then also lost a baby between 20 and 24 weeks, and felt the “trauma was a lot different”. While extremely upset by their experiences of loss in early pregnancy, feeling a baby move or seeing them on an ultrasound scan and then giving birth to a formed baby rather than heavy bleeding made the experience very different. Some parents also felt that there should not be different rules based on whether or not a baby shows signs of life. Kelly felt that knowing that some babies who are born at 22 and 23 weeks of pregnancy survive made the word miscarriage even harder to accept, “I've heard of babies surviving at twenty three weeks... I just can't understand why they use that terminology.”
Kelly felt that knowing that some babies who are born at 22 and 23 weeks of pregnancy survive made the word miscarriage even harder to accept, “I've heard of babies surviving at twenty three weeks... I just can't understand why they use that terminology.”
Alison described the loss of her son at 21 weeks of pregnancy compared to an earlier loss at 12 weeks.
Alison described the loss of her son at 21 weeks of pregnancy compared to an earlier loss at 12 weeks.
View full profile
SHOW TEXT VERSION
EMBED CODE
PRINT TRANSCRIPT
I think [sigh]. It was because he was - The later pregnancy, you've felt them. I'd felt him move. He - Everybody knew. And a lot of people, like a lot of very close friends knew about my first pregnancy, but. Yeah. It was kind of like that was our accepted fact, that this was it.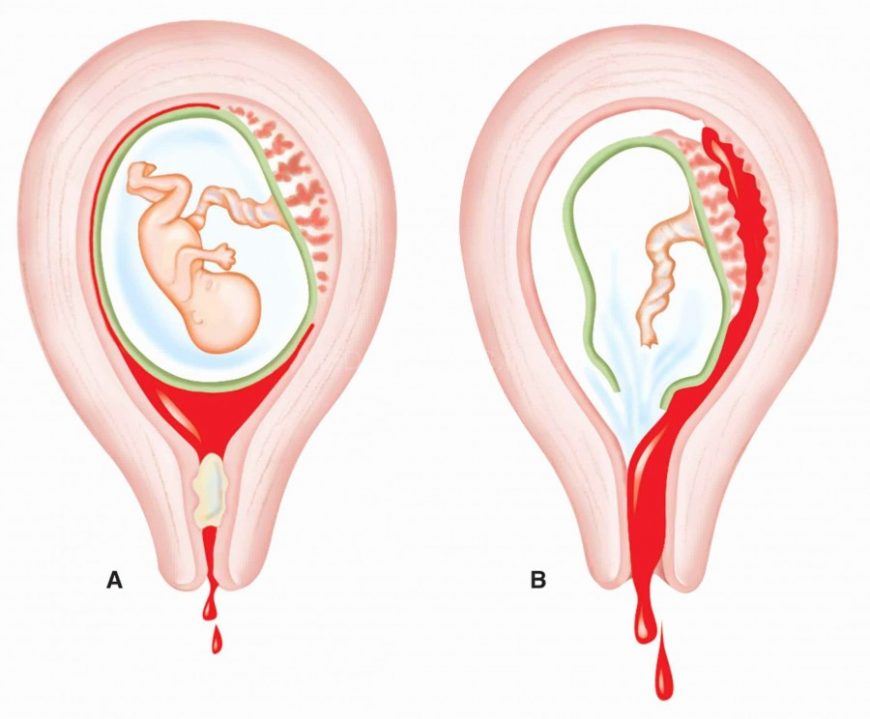 Whereas you - although we hadn't expected to have a miscarriage, it's - that's more common. And so [sigh] after a little while, it was kind of like 'right okay, well this is a normal thing that happens'. With the second pregnancy, it was like, 'well this is what our life is going to be', and then that was snatched away. And we'd bonded. And seen him on the ultrasound, so.
Whereas you - although we hadn't expected to have a miscarriage, it's - that's more common. And so [sigh] after a little while, it was kind of like 'right okay, well this is a normal thing that happens'. With the second pregnancy, it was like, 'well this is what our life is going to be', and then that was snatched away. And we'd bonded. And seen him on the ultrasound, so.With the first baby, we'd never seen - I think no, actually, I think I'd been in at seven weeks and had seen a tiny little - tiny little dot with the first pregnancy. But it wasn't kind of seeing a baby on there. So it was - And then the actual process of giving birth, the fact that you did actually - I did give birth to him. And I don't - I think a lot of people just don't - they don't either think or realise that that is something that you go through. And so that, that all still happened. Yeah. And I still - I mean, this all quite hard to talk about with anybody that I know.
Parents talked about how using the word ‘miscarriage’ to refer to their loss made them feel as if they were “making a mountain out of a molehill” and that it prevented friends and family fully understanding what they had been through. David felt that calling the loss of his baby a miscarriage meant that a lot of people couldn’t “read between the lines and experience the pain” he and his wife Elaine were feeling.
David felt that calling the loss of his baby a miscarriage meant that a lot of people couldn’t “read between the lines and experience the pain” he and his wife Elaine were feeling.
Matthew felt the term miscarriage prevented people understanding what they’d been through.
Matthew felt the term miscarriage prevented people understanding what they’d been through.
View full profile
SHOW TEXT VERSION
EMBED CODE
PRINT TRANSCRIPT
I think it's almost like because she hadn't reached twenty four weeks, it wasn't legitimate, it was - Because it was still termed as a miscarriage.And because there hadn't been a birth certificate or a death certificate, it's almost like everyone - it's almost like it was minimised and wasn't that big of a deal.
Not just for the people who were involved at the hospital, but for like families as well. They didn't really seem to grasp what had happened, or how horrific it had been. Or that you know, a few days here and there shouldn't really make much difference. I mean, I think if she'd have been born at twenty four weeks, I think Kirsty would have been able to have like some maternity leave. Which I'm sure would have really helped her. She'd have very much appreciated that extra time off work. As it was, she was - she was back there herself after a couple of weeks. So. I don't know. I'm sure it wouldn't have helped the loss or the grief to have had the paperwork, but I think perhaps how other people dealt with it, they might have been a bit more sympathetic, I guess is the word. A bit more understanding, that we'd been through something quite, quite bad.
They didn't really seem to grasp what had happened, or how horrific it had been. Or that you know, a few days here and there shouldn't really make much difference. I mean, I think if she'd have been born at twenty four weeks, I think Kirsty would have been able to have like some maternity leave. Which I'm sure would have really helped her. She'd have very much appreciated that extra time off work. As it was, she was - she was back there herself after a couple of weeks. So. I don't know. I'm sure it wouldn't have helped the loss or the grief to have had the paperwork, but I think perhaps how other people dealt with it, they might have been a bit more sympathetic, I guess is the word. A bit more understanding, that we'd been through something quite, quite bad.
Babies born before 24 weeks of pregnancy showing no signs of life do not have their birth and death officially registered. Many parents found this very difficult, as if their baby’s life was not counted or validated.
Carly felt that having a birth and death certificate would give her baby more dignity and validate her grief.
Carly felt that having a birth and death certificate would give her baby more dignity and validate her grief.
View full profile
SHOW TEXT VERSION
EMBED CODE
PRINT TRANSCRIPT
So it's just like - it's just like insult to injury, isn't it. Same with the birth certificate. We got a little - was classed as a certificate of life. But really, it's just a printed out bit of paper that the hospital gives you, that's not formal, it's not recognised, and it's not official. Like a birth and death certificate, I think - they just give your baby that bit of, bit more dignity. Rather than - You wouldn't feel that you'd need to explain it so much, or like how you're feeling.
Kirsty found it particularly painful not receiving a birth or death certificate. Her baby was born two days before the official 24 weeks.
Kirsty found it particularly painful not receiving a birth or death certificate. Her baby was born two days before the official 24 weeks.
View full profile
SHOW TEXT VERSION
EMBED CODE
PRINT TRANSCRIPT
And then I remember saying to the midwife, "What do we do about a death certificate? What do I have to do about all of that?"And she said, "It's okay, it'll all be explained in the leaflets that we're going to give you. " And then the realisation hit me, that I knew somewhere in the back of my mind that it had to be twenty four weeks. And I said, "I've just had a miscarriage, haven't I?" And she says, "No, you've just had a baby." That is what I would say to anybody now that talks to me about late - late miscarriage. Or, what we had that night was a baby. We got to cuddle her, we got to put clothes on her. And that is not a miscarriage. And we did have a couple of family members refer to her as miscarriages. And I put - I said, "Please don't refer to her like that again. We had a baby." And I don't know if it helped particularly. A lot of our experience with Rebecca, I can see from two angles. I know why it was done. And I know why it would be seemingly to help us, but also, did it really? And when I'd asked about the birth certificate, we got given like a fake birth certificate. And I know that some people would probably love that. And I know that that was given to us because they wanted us to know that they recognised we'd just had a baby.
" And then the realisation hit me, that I knew somewhere in the back of my mind that it had to be twenty four weeks. And I said, "I've just had a miscarriage, haven't I?" And she says, "No, you've just had a baby." That is what I would say to anybody now that talks to me about late - late miscarriage. Or, what we had that night was a baby. We got to cuddle her, we got to put clothes on her. And that is not a miscarriage. And we did have a couple of family members refer to her as miscarriages. And I put - I said, "Please don't refer to her like that again. We had a baby." And I don't know if it helped particularly. A lot of our experience with Rebecca, I can see from two angles. I know why it was done. And I know why it would be seemingly to help us, but also, did it really? And when I'd asked about the birth certificate, we got given like a fake birth certificate. And I know that some people would probably love that. And I know that that was given to us because they wanted us to know that they recognised we'd just had a baby.
I don't want a fake birth certificate. And I think out of the whole experience, my hang-up has been the birth certificate. She was two days short. They had a crash team there. We had a baby, but she'll never be recognised by UK law. She'll never - she just didn't exist. And people treat you differently. People do treat it like you've had a miscarriage. And they'll tell you about their experiences of having a miscarriage. And I'm not going to take anybody's pain away, and say that my pain was worse than anybody else's. Because it's a very individual thing. But it's just a different experience. And I don't think you can put them in the same box. And having a loss of a baby at fewer weeks and having one where you have got a baby, they are different experiences. Same kind of pain, but different experiences. But I was all of a sudden in this other box that I didn't want to be in.
Many parents we spoke to found it extremely difficult when their baby was born so near to the legal definition of a stillbirth (24 weeks of pregnancy). Their babies were born a matter of a few weeks, days or even hours before the official time. While parents recognised the need to have some sort of legal cut-off they felt that the definition should be rethought. Nesta’s baby was born at 23 weeks and 6 days, she found it very strange to find out about the threshold, “if there's a baby and there's a coffin, then there's a person, but at the same time there’s a reason there has to be a threshold”. Michelle said people needed to realise “how painful it is to get so close to that line, and not get to that line… and actually offer some sort of support and practical help on that.” However whatever legal cut-off is used, there will be hurt for those who feel they and their babies are excluded from registration.
Their babies were born a matter of a few weeks, days or even hours before the official time. While parents recognised the need to have some sort of legal cut-off they felt that the definition should be rethought. Nesta’s baby was born at 23 weeks and 6 days, she found it very strange to find out about the threshold, “if there's a baby and there's a coffin, then there's a person, but at the same time there’s a reason there has to be a threshold”. Michelle said people needed to realise “how painful it is to get so close to that line, and not get to that line… and actually offer some sort of support and practical help on that.” However whatever legal cut-off is used, there will be hurt for those who feel they and their babies are excluded from registration.
Emily and Mike felt the word stillbirth much better described their experience than miscarriage.
Emily and Mike felt the word stillbirth much better described their experience than miscarriage.

View full profile
SHOW TEXT VERSION
EMBED CODE
PRINT TRANSCRIPT
Mike: I, I don't like - Miscarriage is obviously in common usage, everyone uses it. If you're pregnant and you don't have a baby, it's a miscarriage as well. But I think from like a - There has to be some better way of like categorising different stages of what a miscarriage can consist of.Emily: I feel she's more under the stillbirth bracket. Because I gave birth, and she was still [laugh]. You know? So I sort of feel like that actually fits the description much better.
Mike: Yeah.
Emily: I quite often say I had a stillborn daughter. Because I did. I gave birth, and she wasn't alive.
Mike: Yeah.
Emily: So actually, I think she falls under that bracket. I don't know why at twenty four weeks it is considered a stillbirth, I don't know. There's obviously a reason behind it, but I - I think if you have to go through a birth, and the baby doesn't survive, to me that is what –
There's obviously a reason behind it, but I - I think if you have to go through a birth, and the baby doesn't survive, to me that is what –
Mike: Yeah. I mean, the different - yeah.
Emily: Because I think sometimes when I'm trying to give someone a kind of quick version of it, saying I had a miscarriage just - again - brings back that sitting on the loo and bleeding. It doesn't tell people what we went through. Whereas if you say stillborn, people are like "Oh." And they get it. You know?
Carly described how losing a baby before 24 weeks made her loss feel less significant.
Carly described how losing a baby before 24 weeks made her loss feel less significant.
View full profile
SHOW TEXT VERSION
EMBED CODE
PRINT TRANSCRIPT
I do find it hard, just with - When she was born, specifically. Because you're not categorised as a stillbirth mother, I find that hard. I feel sometimes almost like I'm a fraud. Like my baby didn't matter as much. Even though to me, she does. But to other people, they might just see it as 'oh well, it's a miscarriage, like how are you so devastated, you know, why aren't you over it yet, why is it - why is it that you can't move on?' But like to me, like - like my daughter died, I can never move on from that. Like I'm always going to be heartbroken. There's no good that comes out of a baby dying. Like it's not like when someone's old or ill, and they've had a fully life. Like when a baby dies, it's just - it's always sad forever, forever. I'll never ever feel okay about it. And I mean, I'm a lot better. And I can talk about it. And you know, I can function okay now. But I'll never be - you know - happy about what's happened. I'm always going to feel devastated over it.
Because you're not categorised as a stillbirth mother, I find that hard. I feel sometimes almost like I'm a fraud. Like my baby didn't matter as much. Even though to me, she does. But to other people, they might just see it as 'oh well, it's a miscarriage, like how are you so devastated, you know, why aren't you over it yet, why is it - why is it that you can't move on?' But like to me, like - like my daughter died, I can never move on from that. Like I'm always going to be heartbroken. There's no good that comes out of a baby dying. Like it's not like when someone's old or ill, and they've had a fully life. Like when a baby dies, it's just - it's always sad forever, forever. I'll never ever feel okay about it. And I mean, I'm a lot better. And I can talk about it. And you know, I can function okay now. But I'll never be - you know - happy about what's happened. I'm always going to feel devastated over it.When I'm 90, I'll feel like that.
And the difference of if she'd been born after twenty four weeks? So the maternity leave, and -
Yes.
- birth and death certificates?
Yes. So important.
Yeah. Which - Are there some of those that are really?
Well, it just makes you feel like you're less significant than a mother whose baby had been born dead a couple of days later, and that's just not the case. You know, my baby existed, and she was here. And I laboured and delivered her. And I held her. And I had a funeral for her. You know, she was a real person. Like I felt her move. And, I - I feel like any woman that goes through that deserves the same recognition as a woman who has a baby a little later on. I don't think that you should be categorised. It's almost like you're being punished, on top of all your heartbreak. It feels like a punishment. You know, like you're pushed down into a subcategory of loss, and your grief should be as deep as somebody else's. And that's not how it is.
You know? 'Mother Carly' on her little band. That's like the only real medical documented proof that I have that she was here. And so that band's so precious now, because I don't have anything else. Except her - I've got like a little document, like I got with her ashes. But those are the only official things that I have of her.
And so that band's so precious now, because I don't have anything else. Except her - I've got like a little document, like I got with her ashes. But those are the only official things that I have of her.
As well as the emotional impact of being born showing no signs of life before this 24 week limit, there were also practical implications. Being this wrong side of the limit had a major impact on parents access to maternity and paternity pay and parental leave as well as other financial aid. Sarah found it “was really rubbing salt in the wound” when she had to go back and pay for dental treatment that she was no longer exempt from because she lost her baby before 24 weeks of pregnancy.
Elaine regretted not hanging on an extra day before giving birth to her baby as her baby may then have been registered as a stillbirth.
Elaine regretted not hanging on an extra day before giving birth to her baby as her baby may then have been registered as a stillbirth.

View full profile
SHOW TEXT VERSION
EMBED CODE
PRINT TRANSCRIPT
Once I delivered her - it was twenty three weeks and six days. And I regret to this day that I hadn't hung on to that Tuesday, and I could have a birth certificate and death certificate. And I really wish - There was no - They said I could have carried her for a few weeks. And they said infection can then set in.But because I was so - in such a like, such a state - I wish somebody had explained to me, "Look, if you just - you know. If you choose to wait another day, you can have a birth certificate and a death certificate." And it wasn't until, I don't know how long after, that I realised - I tell people I was twenty four weeks. Because she wasn't a miscarriage, she was stillborn. She was a baby. She was formed. She was little, she was tiny, but she was perfect.
Miscarriage
Gynecology
Miscarriage (spontaneous abortion, miscarriage) is the spontaneous termination of pregnancy in the period from conception to the 28th week. Miscarriage up to 28 weeks is referred to as spontaneous miscarriages (abortions), termination of pregnancy in terms of more than 28 weeks - to premature birth. Spontaneous miscarriages are divided into early (up to 16 weeks) and late (from 16 to 28 weeks). There is also habitual miscarriage (termination of pregnancy two or more times in a row).
Miscarriage up to 28 weeks is referred to as spontaneous miscarriages (abortions), termination of pregnancy in terms of more than 28 weeks - to premature birth. Spontaneous miscarriages are divided into early (up to 16 weeks) and late (from 16 to 28 weeks). There is also habitual miscarriage (termination of pregnancy two or more times in a row).
Unfortunately, today, premature termination of pregnancy is not such a rare occurrence. According to statistics, in the last 40 years, almost every fifth pregnancy ended in miscarriage. Scientific studies say that in fact, more than half of spontaneous miscarriages! But this happens during the first three or four days of pregnancy, and therefore women do not even realize that they were pregnant for some time: after all, the next menstruation came either on time or with a slight delay. Naturally, such cases could not be taken into account by medical statistics. An analysis of reported cases of spontaneous abortions shows that 80% of them occur in the first 12 weeks of pregnancy.
The causes of spontaneous miscarriage are numerous. More than half of them are associated with genetic causes - violations of the quantity and quality of chromosomes in the cells of the embryo, as a result of which it becomes unviable, dies and is removed from the uterus. In this case, spontaneous miscarriage is the result of natural selection working against unviable fetuses.
In addition, miscarriage can be caused by various infections, chronic diseases, disorders in the immune system. Gynecological problems also play an important role - inflammatory diseases of the genital organs, uterine fibroids, ovarian cysts, postoperative scar on the uterus, uterine malformations, cervical insufficiency and various hormonal disorders , of which ovarian hypofunction and hyperandrogenism, genital and general infantilism are the most common.
Miscarriage is practically not affected by light falls and lifting of moderate weights by the mother. The fetus is sufficiently protected, and if the mother's body is healthy and the fetus's genetic program is normal, then the injury must be truly terrible to harm the fetus.
The fetus is sufficiently protected, and if the mother's body is healthy and the fetus's genetic program is normal, then the injury must be truly terrible to harm the fetus.
The causes of recurrent miscarriage (i.e., multiple spontaneous abortions) are practically the same, but a violation of the immune system plays a more definite role when the development of maternal sensitization to fetal tissue antigens or erythrocyte and leukocyte sensitization reactions takes place.
The clinical picture of premature termination of pregnancy depends on the stage of miscarriage and the duration of pregnancy. Usually, with the threat of interruption, pregnant women complain of pain in the lower abdomen and lower back, periodic tension (tonus) of the uterus. There are five stages in the course of early abortion: threatening, incipient abortion, ongoing abortion, incomplete and complete abortion. Early abortions are characterized by the birth of the entire fetal egg. The correct regimen and treatment in the first two stages can save the pregnancy. In subsequent stages, the removal of the entire fetal egg or its delayed parts is required. Symptoms of a threatened and incipient abortion are distinguished by the state of the cervix: it is unchanged in a threatened abortion and somewhat shortened with a closed or ajar canal in an incipient abortion. In addition, the intensity of the pain syndrome, the degree of uterine tension and / or the presence of blood discharge are taken into account.
In subsequent stages, the removal of the entire fetal egg or its delayed parts is required. Symptoms of a threatened and incipient abortion are distinguished by the state of the cervix: it is unchanged in a threatened abortion and somewhat shortened with a closed or ajar canal in an incipient abortion. In addition, the intensity of the pain syndrome, the degree of uterine tension and / or the presence of blood discharge are taken into account.
Late miscarriage proceeds according to the type of childbirth: there is an opening of the cervix, then the outflow of amniotic fluid, the birth of the fetus and, finally, the birth of the placenta. Clinically, it is manifested by cramping or aching pain in the lower abdomen, periodic uterine tension and, less commonly, bloody discharge.
If there is a threat of termination of pregnancy, complex treatment is prescribed: medications, especially hormonal ones, are prescribed only according to strict indications and in minimal doses, since the consequences of hormonal treatment on both the fetus and the unborn child can appear even after many years.
In order to determine the cause of miscarriage, the doctors of our Clinic in each case are assigned an individual comprehensive examination: genetic, gynecological, ultrasound, laboratory, etc. If intrauterine pathology and / or endometrial pathology are suspected, separate diagnostic curettage is performed under hysteroscopy control, and if endometriosis is suspected, tubal pathology and adhesive process in the pelvis, with uterine myoma and scleropolycystic ovaries, operative laparoscopy may also be necessary. Such a large volume of examination should be clear to the patient: after all, miscarriage, as a rule, is the result of not one, but several causes that have their effect simultaneously or sequentially. In addition, many women who have experienced a spontaneous miscarriage may need the help of a psychotherapist who can provide professional advice to help eliminate the negative psychological consequences of this phenomenon. After the examination, a set of appropriate therapeutic measures is planned, depending on the identified factors of miscarriage. The patient's partner is also examined, which includes the identification of hereditary diseases, clarification of the presence of previously or currently existing diseases of various organs and systems, semen analysis and examination for infections.
The patient's partner is also examined, which includes the identification of hereditary diseases, clarification of the presence of previously or currently existing diseases of various organs and systems, semen analysis and examination for infections.
Prevention of miscarriage is carried out both before and during pregnancy. Our obstetricians-gynecologists conduct a special examination for all women who have undergone spontaneous abortion and preterm birth, including a targeted history taking, elucidation of the features of menstrual function (by functional diagnostic tests), hysterosalpingography and ultrasound scanning. According to strict indications, a strictly defined bacteriological, virological, immunological and genetic study is prescribed. If deviations from the norm are detected, they are corrected. During pregnancy, we single out a risk group for miscarriage, outline the terms and methods of treatment and preventive measures, recommend the sanitation of foci of chronic infection, which creates optimal conditions for the development of pregnancy. If the next medical examination confirms the presence of a threat of miscarriage, then urgent measures are prescribed to preserve the pregnancy, and most often the treatment we have performed is effective.
If the next medical examination confirms the presence of a threat of miscarriage, then urgent measures are prescribed to preserve the pregnancy, and most often the treatment we have performed is effective.
What is a miscarriage and why it can happen
###1### What is a miscarriage
First of all, you should define the terms. Miscarriage in gynecological practice is called spontaneous termination of pregnancy in the first 20–22 weeks. Why 20-22 weeks? There is such a consensus: doctors save a fetus born with a mass of 500 grams or more. The chances of saving someone who was born weighing less than 500 grams are zero. At 20–22 weeks, the fetus just usually reaches such a mass.
The frequency of miscarriages is quite high: they end in 15-20% of pregnancies.
That is, for a practicing doctor, this is a fairly common situation, although in the life of each person, of course, this can happen only once or not at all.
Medical statistics, which translate medicine into numbers and make it a more accurate science, show that of these 15-20% of pregnancies that end in miscarriages, 80% or more occur in the first 12 weeks. That is, the longer the gestational age, the less likely it is that a spontaneous miscarriage will occur. Thus, if I, as a doctor, meet a woman who is diagnosed with a threatened miscarriage, give her an ultrasound and see a fetus with a heartbeat, I can immediately tell her that the probability of a miscarriage is no longer 15%, but 5%. If I see a situation where the gestation period is already more than 12 weeks, then the probability is already 2-3%.
That is, the longer the gestational age, the less likely it is that a spontaneous miscarriage will occur. Thus, if I, as a doctor, meet a woman who is diagnosed with a threatened miscarriage, give her an ultrasound and see a fetus with a heartbeat, I can immediately tell her that the probability of a miscarriage is no longer 15%, but 5%. If I see a situation where the gestation period is already more than 12 weeks, then the probability is already 2-3%.
How does a miscarriage happen? Regardless of the reason, the scenario is the same.
First the fetus dies; then detachment from the walls of the uterus begins (then the woman has spotting, which is classified as a “threatening miscarriage”), and then the exfoliated is thrown out of the uterine cavity. The problem is that the same symptoms can be observed in both an ectopic pregnancy and a normal, healthy intrauterine pregnancy. If the ultrasound shows a live intrauterine pregnancy, in most cases the cause of bleeding during pregnancy remains unknown. It is the appearance of bloody discharge against the background of a live intrauterine pregnancy that is designated by doctors as a “threatening miscarriage”. In the vast majority of cases, despite the formidable diagnosis, such a pregnancy is completely safely completed. Of course, any woman passionately wants to know what this bloody discharge is because of, because she thinks: now I will find out what it is because of, I will remove this factor from my life, and everything will be fine, they will stop with me. We have to disappoint a woman: in most cases, we do not know the reason.
It is the appearance of bloody discharge against the background of a live intrauterine pregnancy that is designated by doctors as a “threatening miscarriage”. In the vast majority of cases, despite the formidable diagnosis, such a pregnancy is completely safely completed. Of course, any woman passionately wants to know what this bloody discharge is because of, because she thinks: now I will find out what it is because of, I will remove this factor from my life, and everything will be fine, they will stop with me. We have to disappoint a woman: in most cases, we do not know the reason.
Accidental and habitual miscarriage
All miscarriages are divided into two large types - sporadic (accidental) and habitual. In essence, they are determined by the same range of causes, only the proportion of each of the causes in two cases will be very different. In turn, all causes can be divided into two large groups: internal causes caused by fetal problems, and external causes caused by problems in the mother's body. Accordingly, sporadic miscarriages are most often determined by causes associated with the fetus, and habitual miscarriages are determined by the mother's body.
Accordingly, sporadic miscarriages are most often determined by causes associated with the fetus, and habitual miscarriages are determined by the mother's body.
Medical statistics show that more than half of sporadic miscarriages in the first 12 weeks are due to genetic disorders in the fetus.
Moreover, the shorter the gestational age, the higher the likelihood that the cause was a genetic disorder in the fetus. These are generalized data from numerous studies, mostly Western ones. Let's look at this most common reason first. The fact is that no matter how kings of nature we think we are, the same laws of nature apply to us as to an ant, an insect, a blade of grass.
Nobody canceled these biological laws: the best and the strongest survive in the good sense of the word, in the biological sense.
A biological individual cannot always produce 100% quality cells (in this case we are talking about germ cells). So, 1 ml of a man's sperm contains on average 20 million spermatozoa, and normally about 10% of them, that is, 2 million, are pathological forms. And such a spermogram will be considered normal. In a woman, too, poor-quality eggs can mature, and the older we get, the more likely it is that a poor-quality egg will mature. It's not because we're deliberately doing something wrong - lifting something heavy, drinking an extra cup of coffee, overworking at home/work. Unlike spermatozoa, which are constantly renewed, all the eggs of a future woman are laid at the moment when her mother is at the 20th week of pregnancy.
And such a spermogram will be considered normal. In a woman, too, poor-quality eggs can mature, and the older we get, the more likely it is that a poor-quality egg will mature. It's not because we're deliberately doing something wrong - lifting something heavy, drinking an extra cup of coffee, overworking at home/work. Unlike spermatozoa, which are constantly renewed, all the eggs of a future woman are laid at the moment when her mother is at the 20th week of pregnancy.
And new eggs are never laid again, they are only used up, only lost throughout the life of a girl/woman.
That is, if you are 35 years old, then the egg that came out of your ovary this month has been lying in the ovary waiting for its turn to ovulate for more than 35 years. Therefore, of course, in a 20-year-old woman and in a 40-year-old woman, not only the quantity, but also the quality of the eggs will be different. Because everything unfavorable that is around us in terms of nutrition, environment, air and water affects the first only 20 years, and the second - already 40.
The dependence of the frequency of spontaneous miscarriage due to genetic disorders in the fetus on the age of the eggs (and, consequently, on the age of the woman) was shown thanks to the introduction of in vitro fertilization technology - IVF. A very good study was conducted on a group of patients over 40 who underwent IVF. Half of them were implanted with their own fertilized eggs, and the other half - donor eggs taken from women under 25 years old. In the group that carried embryos from donor eggs, the miscarriage rate corresponded to that of women under 25 years of age and was three to four times lower than in the group that was implanted with embryos obtained from their 40-year-old eggs. Thus, the probability of miscarriages and genetic disorders of the fetus is determined by the biological age of the woman. It's the kind of thing we can't reverse in any way, and it should be taken into account when a pregnancy is postponed to a later date.
Thus, if a defective egg meets a normal sperm or vice versa, then the resulting pregnancy with a poor-quality embryo is rejected at a certain stage and a miscarriage occurs.
And here comes the most interesting thing, because we still don't know which mechanism in the body recognizes that the pregnancy is of poor quality. But this mechanism exists, and it works very well, otherwise all abnormal pregnancies would lead to the birth of not quite healthy or completely unhealthy people, and humanity would have already degenerated. We do not know this mechanism, but we can say: if a woman has a spontaneous miscarriage, then these mechanisms work for her and from a biological point of view she is healthy. It is much worse if we see a different situation (although it is quite rare): far beyond the 20-week period, we do an ultrasound and find severe defects in the fetus. Because of these defects, after birth, he may either be disabled or not be able to survive at all, but now he lives inside the uterus, which suggests that the mechanisms that recognize healthy and unhealthy pregnancy did not work in this woman.
Therefore, with all the emotional and psychological disadvantages that a spontaneous miscarriage brings for a woman, there is a big plus in this event, which is not obvious to the patient.
This is a universal biological mechanism that allows you to keep us and our offspring healthy and prevents the birth of a handicapped child.
If the majority of spontaneous miscarriages are caused by genetic disorders, the question arises which pregnancies should then be saved. Unfortunately, any gynecologist has encountered cases in his practice when attempts to “pull out” a pregnancy with incredible efforts lead to a deplorable result. That is, the pregnancy threatened to terminate, the woman was given numerous medications, and she persisted, but after the 20th week it turned out that the fetus had serious developmental disorders. It should be said separately about medicines. Serious Western studies (there is such a term as "double-blind placebo-controlled study", it guarantees the quality and statistical significance of the results as much as possible) show that there is not a single medication, except for progesterone, a female hormone that can affect pregnancy.
If a pregnancy is doomed to death, it will die; if it must survive, it will survive, unless, of course, we are talking about a healthy woman who has biological mechanisms that are currently unknown to us for culling poor-quality pregnancies.
We, in Russia, have a different practice, caused not by scientific objective data, but rather by cultural differences - the fact that our medicine has been isolated from the world community for a long time.
The second most common cause of miscarriage is infection. This is the same failure. Severe flu is an obvious reason for sporadic miscarriage. Pregnancy does not destroy the disease, but its consequence - the general poor condition of the woman's body, the environment that ensures the life of the fetus. Unlike genetic reasons, when the embryo was laid "bad", in the case of infection, the embryo was laid healthy and of high quality. But suddenly the woman fell ill with a severe flu - a temperature of 40, vomiting, dehydration. It is difficult for a tiny creature to survive in such adverse conditions, and it dies. The death of the embryo is due to environmental disturbances - high temperature, dehydration, intoxication.
If a second miscarriage occurs, it is difficult to attribute it to the flu: it is hard to believe that a woman gets the same severe flu every year at the same time. Here it is - the difference between sporadic and habitual miscarriage.
Here it is - the difference between sporadic and habitual miscarriage.
The first happens really by chance - it's a classic "failure". The second is a pattern: when we see a woman with a habitual miscarriage, she, as a rule, has an interruption at about the same time. Then we assume that there is a reason that does not exist very clearly in the body: it does not prevent a woman from living outside the state of pregnancy, but it makes itself felt when a normal pregnancy occurs. This reason, which does not exist very noticeably in a woman's body, prevents her from carrying a pregnancy to term. It leads to the fact that normal conditions for the survival of a healthy fetus are not created, and it dies, and this happens from time to time. This is the fundamental difference between a habitual miscarriage and a sporadic one. In this case, we will conduct a series of studies (quite expensive) to find out what the reason is.
Today, there is a consensus in the world scientific community that recurrent miscarriage is considered a case when a woman has two miscarriages in a row. If a woman had one miscarriage and she comes to me and asks what is the probability that this will happen again, these are the same 15-20%. If this situation occurred twice in a row, then the probability that this will happen again is already about 30–35%, and if three times in a row, it is almost 40%.
If a woman had one miscarriage and she comes to me and asks what is the probability that this will happen again, these are the same 15-20%. If this situation occurred twice in a row, then the probability that this will happen again is already about 30–35%, and if three times in a row, it is almost 40%.
Approximately 2% of married couples have wives with recurrent miscarriages.
If in the case of sporadic miscarriages, the fetus and its disorders are most often “to blame”, then in case of habitual miscarriages, its environment, the woman’s body, is usually “to blame”. As with sporadic miscarriages, genetics can be the cause. But if in sporadic miscarriage genetics is the cause of 70–80% (up to 6 weeks in general 90%) of all interruptions, then in the case of habitual miscarriage, genetic disorders are found only in 2–3% of patients. The same is true for infections: in a recurrent miscarriage, the likelihood that repeated abortions are due to infection is no more than 1%.
Hormonal imbalances in women, on the other hand, are more likely to cause habitual miscarriage than accidental miscarriage.
Disturbances in the structure of the uterus - a septum inside the uterus, a bicornuate uterus, the presence of synechia (the so-called adhesions inside the uterus) - these are all things that can also lead to repeated miscarriages.
Approximately 40% of women diagnosed with "recurrent miscarriage" are found to have various immune disorders that cause the fetus to be rejected by the mother's body. Immune disorders are divided into autoimmune and alloimmune. Autoimmune disorders are situations where a woman's immune system works against its own genes, proteins. One of the most common diseases of this kind among women with recurrent miscarriage is antiphospholipid syndrome. Phospholipids are the "glue" that holds cells together. A woman with antiphospholipid syndrome produces factors (antibodies) against her own phospholipids, which are abundant in the placenta. As a result of the syndrome, blood clots form in the small vessels of the placenta, which disrupt blood circulation, and therefore disrupt the function of the placenta to deliver nutrients to the fetus. Pregnancy under such conditions cannot “stretch” for a long time - sooner or later, the death of a healthy embryo / fetus occurs. Women suffering from antiphospholipid syndrome carry a pregnancy in no more than 10% of cases. Its treatment allows you to reverse the statistics - gestation occurs as early as 90% of cases. A woman is given drugs that thin the blood and prevent the formation of blood clots - the placenta performs its function, and the pregnancy is carried.
As a result of the syndrome, blood clots form in the small vessels of the placenta, which disrupt blood circulation, and therefore disrupt the function of the placenta to deliver nutrients to the fetus. Pregnancy under such conditions cannot “stretch” for a long time - sooner or later, the death of a healthy embryo / fetus occurs. Women suffering from antiphospholipid syndrome carry a pregnancy in no more than 10% of cases. Its treatment allows you to reverse the statistics - gestation occurs as early as 90% of cases. A woman is given drugs that thin the blood and prevent the formation of blood clots - the placenta performs its function, and the pregnancy is carried.
Alloimmune causes are aggressive factors directed against foreign proteins, that is, the paternal part of the fetal genome. In general, our immune system is required to produce antibodies and get rid of any foreign and pathologically altered cells. Why a pregnancy consisting of 50% of "foreign" genes is not rejected (not to mention 100% of genetic foreignness when a surrogate mother carries a "foreign" embryo in the IVF program) is not yet entirely clear. By the way, scientists believe that when it is found out what is the mechanism that prevents the rejection of pregnancy cells with "foreign genes", this can help in the development of a cure for cancer. After all, cancer consists of pathologically altered cells, which, for some reason, are also not rejected, not destroyed by the immune system. One way or another, during pregnancy, a woman in relation to foreign genes / proteins of the placenta and fetus develops a condition called immunological tolerance - “we do not notice and do not attack strangers”. In the case of a habitual miscarriage, this tolerance does not exist: the mother's immune system recognizes foreign genes and proteins of pregnancy, attacks them, and thereby leads to repeated miscarriages.
By the way, scientists believe that when it is found out what is the mechanism that prevents the rejection of pregnancy cells with "foreign genes", this can help in the development of a cure for cancer. After all, cancer consists of pathologically altered cells, which, for some reason, are also not rejected, not destroyed by the immune system. One way or another, during pregnancy, a woman in relation to foreign genes / proteins of the placenta and fetus develops a condition called immunological tolerance - “we do not notice and do not attack strangers”. In the case of a habitual miscarriage, this tolerance does not exist: the mother's immune system recognizes foreign genes and proteins of pregnancy, attacks them, and thereby leads to repeated miscarriages.
Quite often, in about 40% of all cases, after conducting the necessary examination of both spouses, we, unfortunately, do not find any reasons explaining why this couple has repeated miscarriages.
There is such a term as "unexplained recurrent miscarriage", as well as "unexplained infertility". Maybe in five years, medicine will find something new in this area, new explanations, but so far this has not happened. This is a psychologically difficult moment for both the doctor and the patients.
Maybe in five years, medicine will find something new in this area, new explanations, but so far this has not happened. This is a psychologically difficult moment for both the doctor and the patients.
Two worlds, two approaches
When a woman is at risk of miscarriage, the actions of a doctor in Russia and abroad will be fundamentally different, and this is due not so much to different scientific data as to cultural differences that have arisen during the isolation of our medical school. Abroad, such women are simply sent home: they are "prescribed" bed rest, a general clinical examination, and sexual rest. Time will tell how this situation will end: either the pregnancy will continue, or a miscarriage will occur if it was of poor quality, and it’s good that it was “rejected” by the body.
In Russia, the psychological attitude of the population towards medicine is slightly different and medicine is slightly different.
In our country, a threatened miscarriage is an indispensable indication for hospitalization: there the patient is prescribed "no-shpu", drugs that relax the uterus, hemostatic drugs. This is not a matter of biological or medical differences - it is a matter of psychology for most of our population: if a doctor did not give a pill, then he did not seek to help. And it is quite difficult to convey to people that the laws of nature apply here - you cannot influence them. According to our Russian protocol, I have no right not to offer hospitalization in case of a threatened miscarriage. However, scientific medical facts clearly show that hospitalization does not fundamentally change anything in the prognosis: the likelihood of spontaneous miscarriage does not decrease from this. Western studies show that there are no medications that can cure sporadic miscarriage. If the pregnancy persists, then it is nature that preserves the pregnancy, not the cure. There are such medicines for a habitual miscarriage: if it was possible to identify the cause of repeated abortions, it can be influenced. This treatment is prescribed either before the onset of pregnancy, or in the early stages of pregnancy, before any symptoms of threatened miscarriage appear.
This is not a matter of biological or medical differences - it is a matter of psychology for most of our population: if a doctor did not give a pill, then he did not seek to help. And it is quite difficult to convey to people that the laws of nature apply here - you cannot influence them. According to our Russian protocol, I have no right not to offer hospitalization in case of a threatened miscarriage. However, scientific medical facts clearly show that hospitalization does not fundamentally change anything in the prognosis: the likelihood of spontaneous miscarriage does not decrease from this. Western studies show that there are no medications that can cure sporadic miscarriage. If the pregnancy persists, then it is nature that preserves the pregnancy, not the cure. There are such medicines for a habitual miscarriage: if it was possible to identify the cause of repeated abortions, it can be influenced. This treatment is prescribed either before the onset of pregnancy, or in the early stages of pregnancy, before any symptoms of threatened miscarriage appear.