White cream from vag
What Is It? And Why Does It Happen?
Ever noticed that your body produces white discharge when you’re enjoying some solo pleasure or having sex with a partner? Then you’re not alone — one of the most common Google searches is “white discharge during sex.” So what is it? And why does it happen?
Getting “wet” during sex is a term you’ve likely heard in sex education, pornography, or while chatting with your friends. However, the white discharge that your body releases during sex is the same mucus-like substance that you might find in your underwear as you go about your day-to-day life. It might be thicker and more translucent, thinner and wetter, or something in between.
Whatever your white discharge looks like, it’s a totally normal part of having sex. In fact, it’s your body’s natural response to being aroused or “turned on” to help with lubrication.
Just remember that, when it comes to intimate health, there’s no such thing as one-size-fits-all. So your white discharge will probably look different from a friend or partner’s. Consistency and color can also be affected by lots of different things, which we’ll go into below.
Understanding what healthy discharge looks like can help you spot when you may be experiencing an infection and when you may need to speak to your health professional. Here’s what you need to know.
White Discharge During Sex: What Does Normal Vaginal Discharge Look Like?
As mentioned above, healthy vaginal discharge can be slightly different in look, texture, and color from person to person. Before we get into what it looks like, let’s go over what it does.
Well, the vagina (or the internal part of your genitals) is actually self-cleaning, thanks to discharge. Fluid is released from glands within your cervix and vagina to flush out any bacteria and old cells that might lead to infections. Think of discharge as the body’s own shower gel, which means you don’t need to clean it with anything other than water.
It’s normal to start producing discharge in the months before your first period. And the production of discharge slows as you transition into menopause.
And the production of discharge slows as you transition into menopause.
There’s no such thing as “normal” discharge because everyone is different. However, the National Health Service (NHS) in the U.K. says that healthy vaginal discharge is white or clear and doesn’t have a strong or unpleasant smell.
Similarly, if your discharge is thick or sticky, it’s nothing to worry about. Discharge can also be more slippery and stretchy, kind of like egg whites — this signals that ovulation is about to happen, which is when an ovary releases an egg.
Don’t panic if your discharge leaves a slight yellow or white stain in your underwear or sheets — this is perfectly normal, and lots of us experience this (even if we aren’t talking about it).
White Discharge During Sex: Why Does It Happen?
You may be wondering how the vaginal discharge you produce as you go about your everyday life is linked to the natural lubrication your body produces when you’re turned on.
Simply put, the primary purpose of any discharge is to moisturize the vagina. But, even around ovulation — when you probably notice more discharge in your underwear than usual — there might not be enough lubrication for comfortable sex.This calls for even more moisture.
That’s why when you’re sexually aroused a few different things happen to create more lubrication. Arousal increases blood flow to your vulva, causing the blood vessels to swell and allowing fluid to pass through its walls. The Bartholin’s glands (in the vulva just outside the vaginal opening) and Skene’s glands (around the urethra) both produce extra fluid to help reduce the friction and irritation from pentrative sex. Often this fluid is white.
There’s no amount of discharge you “should” be producing when you’re turned on. Nor is there such a thing as being too wet. But if you’re not producing enough natural lubrication during sex to feel comfortable, your hormone levels, any medication you’re taking (such as hormonal birth control), or the kinds of sexual activities you engage in could all be having an impact.
Speaking of hormone levels, where you are in your menstrual cycle can also play a part. Estrogen levels are lower at the beginning of your menstrual cycle, so you might notice less white discharge during sex.
White Discharge During Sex: How Is Your Vaginal Discharge Linked To Your Menstrual Cycle?
Your period, the discharge you experience throughout the month, and the white discharge you produce during sex might feel like separate occurrences, but they’re actually inherently linked.
Puberty causes hormonal changes to happen in your body, including the production of discharge in the run-up to your first period.
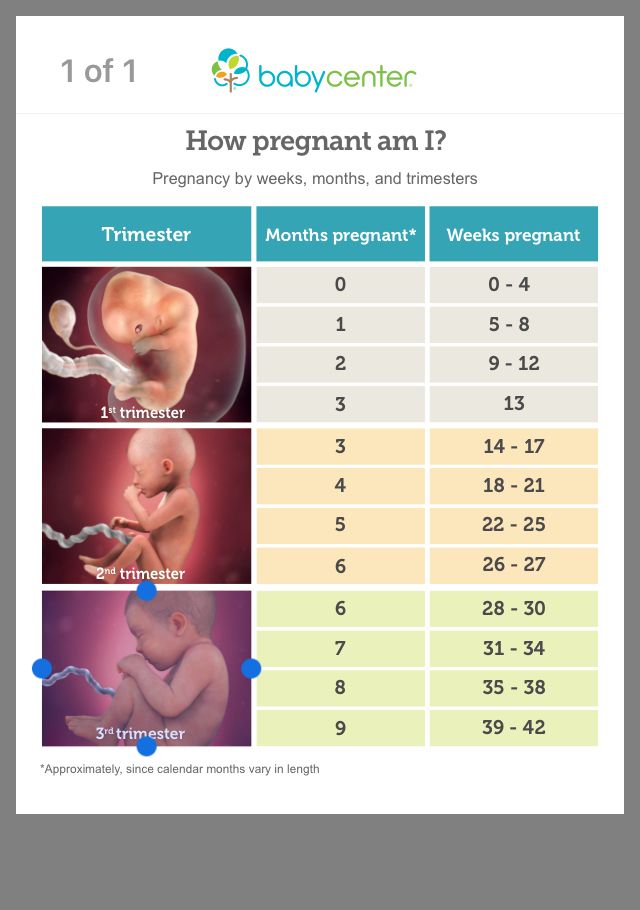
During your period, your body sheds the lining of your uterus, which comes out as blood, but there’s also a little bit of discharge mixed in there. About a week after your period, a few days before ovulation, discharge is stretchy, clear, and similar in consistency to egg whites. High levels of estrogen are at play here, as your ovaries prepare to release an egg.
In the middle of your cycle, during ovulation, your discharge may feel slippery or thinner. Then during the second part of the menstrual cycle, after ovulation, you may notice creamy, white discharge. Healthy vaginal discharge during this time is typically white, creamy, milky, or cloudy and is sometimes thick.
As long as your discharge doesn’t have a strong, unpleasant smell and isn’t accompanied by symptoms like itching, burning, painful urination, or pain during sex, it’s likely to be normal.
White Discharge During Sex: Causes Of Heavier Vaginal Discharge
It can be tricky to spot slight changes in your vaginal discharge. However, if you do notice that the colour and consistency of your discharge changes, don’t panic.
Factors such as where you are in your cycle and whether you’re turned on are usually at play and often nothing to worry about.
For example, if changes to your discharge happen just before or during, sex, then it may just be your body’s natural response to being turned on. As more blood flows to your genitals, discharge is pushed to the surface to help aid lubrication. You may notice you feel wet after sex.
As more blood flows to your genitals, discharge is pushed to the surface to help aid lubrication. You may notice you feel wet after sex.
Similarly, your body releases more estrogen in the days leading up to ovulation, which also causes vaginal discharge to change during ovulation as your body releases more estrogen. It can be handy to track your menstrual cycle with apps like Flo to help you understand what’s going on.
Your estrogen levels are also high during early pregnancy, which means that you may produce more discharge than normal. This is one way that your body protects the fertilized egg from infections. Healthy discharge during pregnancy should look the same as your discharge when you’re not pregnant.
White Discharge During Sex: Is My Discharge Healthy?
There are a number of signs or changes that you can look out for in your vaginal discharge or overall well-being that may indicate that you have an infection:
- A change in color
- A change in smell
- Other symptoms such as pain, burning, or itching around or in the vagina
A change in color
While the consistency of white discharge you produce during sex may change throughout your menstrual cycle, when you’re pregnant, or when you’re sexually aroused, the color should always be clear or milky white.
If your discharge appears to have a red tinge or be bloody or brown during your period, that’s totally fine. However, if you notice a lot of spotting or bleeding between your periods, it could be a sign of other conditions.
Uterine fibroids, which are growths within your uterus, can cause bleeding between periods. Similarly, cervical polyps (growths on your cervix) can trigger spotting. Both of these conditions are treatable and your doctor can advise you on the best treatment to manage your symptoms.
Sexually Transmitted Infections (STIs)
If your discharge appears yellow or green in color and starts to smell, it’s a sign something’s off. Some STIs, such as chlamydia and gonorrhea, can cause discharge to look yellow or green.
Other symptoms can include painful urination, pelvic pain, and pain during sex. It’s worth noting that some people don’t experience any symptoms when they have chlamydia or gonorrhea, so it’s important to practice safe sex by using condoms or similar barrier methods of contraception. If you suspect that you’ve been exposed to an STI, schedule an appointment to get tested.
If you suspect that you’ve been exposed to an STI, schedule an appointment to get tested.
Trichomoniasis, or trich, is another STI that may cause your vaginal discharge to appear yellow or green. The NHS outlines that the infection is caused by a tiny parasite called Trichomonas Vaginalis (TV), and symptoms often present within a month. However, up to half of all people don’t present any symptoms at all. If you think you have trich, definitely get tested.
Bacterial Vaginosis (BV)
If you notice that your discharge is grey or has developed a strong “fishy” smell, bacterial vaginosis could be the culprit. BV is an inflammatory infection that is caused by an overgrowth of the bacteria that lives in your vagina. This can be caused by douching or intensively washing your vagina.
For most people, BV is easily treatable with a course of antibiotics, creams, or gels. See your doctor or health care professional for a checkup if something seems off.
Yeast Infection
Yeast infections (candidiasis or thrush) is another really common condition that can cause a change in your vaginal discharge. You may notice that it’s thicker, whiter, and has a cottage cheese-type texture. This is indicative of a yeast infection which is often accompanied by burning or itching.
You may notice that it’s thicker, whiter, and has a cottage cheese-type texture. This is indicative of a yeast infection which is often accompanied by burning or itching.
See your doctor who can prescribe antifungal medication, either in the form of a pessary or a tablet you take orally. You may also be given cream to soothe the irritation you’re experiencing.
Pelvic Inflammatory Disease (PID)
Pelvic inflammatory disease is an infection that occurs if bacteria spreads up the vagina to the cervix. It can affect your uterus, uterine tubes, and ovaries. You may notice that your discharge becomes yellowish in colour. Other symptoms include heavy or painful periods, pain in your lower abdomen, and discomfort during sex.
If caught early, PID is easily treated — antibiotics and over-the-counter pain medication is usually all it takes.
White Discharge During Sex: When To Speak To Your Doctor
White discharge during sex is healthy and normal. It’s your body’s natural response to pleasure that helps with lubrication. So, the more turned on you become, the more your body might produce.
It’s your body’s natural response to pleasure that helps with lubrication. So, the more turned on you become, the more your body might produce.
However, if you notice that the white discharge you produce during sex changes color or smell — or you start to experience symptoms like fatigue, pelvic pain, bleeding between your periods, burning, or itching — schedule an appointment for a checkup.
Tracking discharge changes and symptoms in a period tracking app like Flo can help your doctor get up to speed quickly and narrow down what’s going on. They might also do a pelvic exam and ask you questions about your sexual and general health history.
If a diagnosis isn’t immediately clear, they might conduct a Pap smear (swab your cervix to take a sample of cells for testing) or take a sample of your discharge to examine under a microscope. It’s crucial to remember that you’re totally in control during any consultation; whoever’s treating you should outline what they’re going to do during the procedures before they begin them.
White Discharge During Sex Causes and Whether Treatment Is Needed
White Discharge During Sex Causes and Whether Treatment Is NeededMedically reviewed by Janet Brito, Ph.D., LCSW, CST — By Kirsten Nunez on July 8, 2019
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
White discharge is a white fluid that comes out from the vagina or penis, including during and after sexual activity.
Some types of discharge are meant to help sexual intercourse.
For example, cervical mucus cleans and lubricates the vagina. Penile fluid, which flows through the same tube as urine, neutralizes leftover acidity so sperm can safely pass.
These fluids are normal. They’re usually clear to milky white.
In other cases, white discharge is caused by an infection. Let’s look at the possible reasons for white discharge during or after sexual activity.
Vaginal discharge during penile-vaginal penetration is usually expected.
Sexual arousal
Sexual excitement is a common cause of white discharge. Normally, vaginal discharge is clear or milky white. This fluid cleans, protects, and lubricates the vagina.
When you’re sexually aroused, the discharge is more noticeable because it thickens and increases. As long as penetration isn’t painful, this type of discharge is typical.
Menstrual cycle changes
It’s normal for your vaginal discharge to change throughout your menstrual cycle.
In the beginning and end of your period, it’s typical to have thick white discharge. During ovulation, vaginal discharge is clear and stretchy, like egg white.
If you have sex during these times, you may notice this type of white discharge. This is expected.
Generally, white vaginal discharge after sexual intercourse indicates an infection.
Bacterial vaginosis
Bacterial vaginosis (BV) is an overgrowth of normal vaginal bacteria. It happens when the pH of your vagina is disrupted during sexual intercourse, douching, or frequent cleaning.
While BV often affects people who are sexually active, it’s possible to get BV without having sexual activity.
BV discharge may be off-white or gray. Other possible symptoms include:
- fishy odor that gets stronger after intercourse
- more discharge than usual
- itchiness
- burning during urination
Sometimes BV doesn’t cause any symptoms.
BV is treated with antibiotics. It could also go away without treatment, but it’s best to see a doctor if you have it. Untreated BV can increase your risk of sexually transmitted infections (STIs) and complications during pregnancy.
Yeast infection
A yeast infection occurs when Candida, a normal vaginal fungus, grows too much. It’s also known as vaginal candidiasis.
Yeast infections can spread through vaginal sex. But like BV, you can develop a yeast infection without having sexual intercourse.
Typically, yeast infection discharge is thick, white, and looks like cottage cheese. It usually doesn’t have a bad odor.
It usually doesn’t have a bad odor.
Additional symptoms include:
- burning
- redness of the vagina and vulva
- painful urination
- painful sexual penetration
Treatment includes over-the-counter or prescription antifungal medicine.
Sexually transmitted infection
A sexually transmitted infection (STI) can cause white vaginal discharge after sexual activity. STIs are spread through unprotected vaginal, anal, or oral sex.
Possible causes and symptoms include:
- Chlamydia, which may cause yellow-white discharge, vaginal bleeding between periods, and painful urination. Sometimes chlamydia has no symptoms.
- Trichomoniasis, which causes a fishy discharge that may be white, clear, green, or yellow. You might also have itching, redness, burning, and discomfort while urinating.
- Gonorrhea, which can be without symptoms. If you have symptoms, you may have white discharge, more discharge than usual, vaginal bleeding between periods, and painful urination.

These STIs are treated with antibiotics. If you have an STI, your recent sexual partners should be treated too.
The following causes could explain white discharge from your penis.
Sexual arousal
Sexual arousal can cause clear to milky white penile discharge. This fluid, known as pre-come, is typical.
During ejaculation, the discharge is also white. It’s made of semen and sperm.
White discharge caused by sexual excitement is the only type of penile discharge that’s normal.
Urinary tract infection
Urinary tract infections (UTIs) can affect different parts of the urinary tract. This includes the penile urethra, which connects the bladder to the penis.
A UTI in the urethra usually happens when bacteria from the anus enters the urethra.
This can lead to urethritis, or inflammation of the urethra. Urethritis symptoms include penile discharge and burning during urination.
Other symptoms of a UTI include:
- frequently passing small amounts of urine
- a constant need to urinate
- cloudy urine
- red or pink (bloody) urine
- strong urine smell
UTIs are treated with prescription antibiotics, although your doctor may prescribe other medications.
Yeast infection
Like vaginal yeast infections, penile yeast infections are due to Candida overgrowth. It often happens after having penile-vaginal intercourse with someone who has a vaginal yeast infection.
In addition to white discharge, penile yeast infections may cause:
- inflammation of the penis head (balanitis)
- white patches
- itching
- burning
- red rash
You’re more likely to have balanitis if you are uncircumcised or overweight, or have an impaired immune system.
Treatment includes antifungal creams or ointments.
Sexually transmitted infection
An STI can lead to white penile discharge with pain and irritation. STIs are spread through unprotected penile, anal, or oral sex.
The following STIs may cause white discharge:
- Chlamydia. Symptoms of this STI include penile discharge and urethritis.
- Trichomoniasis. In addition to discharge, trichomoniasis may cause itching and irritation.
 You may feel burning after ejaculating or urinating.
You may feel burning after ejaculating or urinating. - Gonorrhea. Discharge may be white, green, or yellow. Additional gonorrhea symptoms include foreskin inflammation and painful urination.
Antibiotics are the first line of treatment for STIs.
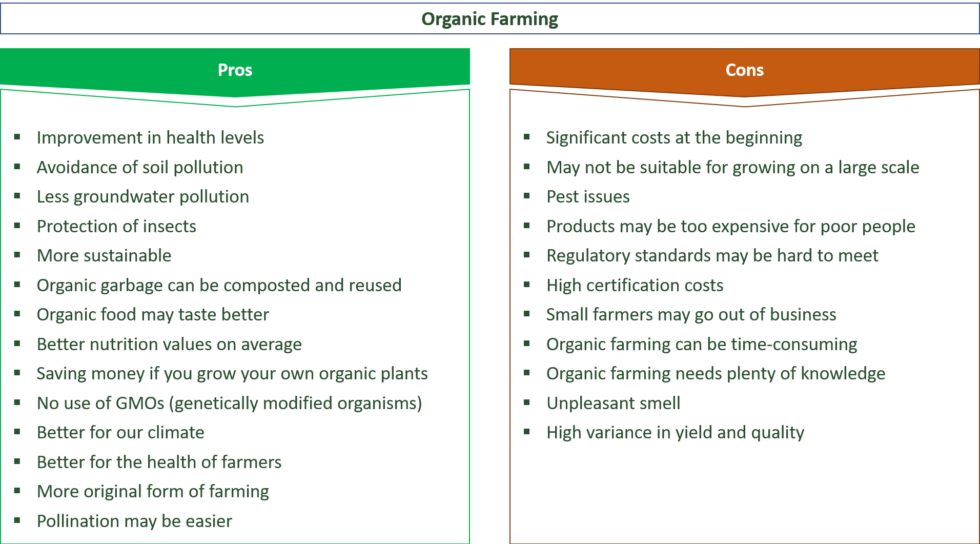
This chart compares white discharge and accompanying symptoms with their likeliest cause.
| Bacterial vaginosis | Yeast infection | Chlamydia | Trichomoniasis | Gonorrhea | UTI/Urethritis | |
| Odor | fishy, especially after sex | none | strong smell possible | fishy (vaginal) | possible | none |
| Itching | usual | usual | possible | usual | possible | none |
| Rash/Redness | none | usual | possible | usual | foreskin inflammation | none |
| Bleeding | none | none | vaginal bleeding between periods or after sexual penetration | none | vaginal bleeding between periods | bloody urine |
| Burning | during urination | usual | during urination or sexual penetration | during sexual penetration, urination, or ejaculation | during sexual penetration or urination | during urination |
| Pain | none | during sexual penetration or urination | during sexual penetration; testicular pain or lower abdominal pain | possible | lower back, abdominal (vaginal), or testicular pain | during urination |
Everyone has a different amount of discharge during and after sexual activity.
If you’re not sure what to expect, consider your normal discharge when you don’t have oral, vaginal, or anal sex.
You can expect to have more than this amount during sexual intercourse.
People with a vagina usually have about one teaspoon of clear to milky white discharge every day. On the other hand, people with a penis don’t have discharge unless they’re sexually aroused or ejaculating. A standard ejaculation is about one teaspoon.
Even then, normal discharge during sexual activity depends on several factors, including:
- your menstrual cycle
- sexual arousal
- hormonal changes
- birth control
- your overall health
- vaginal or penile infections
If you have an infection, sexual activity might increase symptoms like discharge and pain. It’s best to get treatment and avoid oral, anal, and vaginal sex until your infection gets better.
Visit a doctor if your discharge looks or smells different than usual.
White discharge with a yellow, green, or gray tinge is a cause for concern.
You should also seek medical help if you have:
- pain during sexual activities
- painful urination
- abdominal pain
- pelvic pain
- itching
- burning
- rash
- sores
Your discharge is probably typical if you don’t have any of these symptoms.
Some white discharge during sexual activities is expected. Typically, it’s brought on by sexual arousal and isn’t accompanied by pain.
New white discharge after sexual intercourse may be a sign of an infection. Common causes include bacterial vaginosis, yeast infections, and STIs.
It’s a good idea to pay attention to what your discharge normally looks like. If you notice an unusual odor or color, or if you have pain, visit a doctor.
Last medically reviewed on July 8, 2019
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Centers for Disease Control and Prevention. (2016). Gonorrhea - CDC fact sheet.
cdc.gov/std/gonorrhea/stdfact-gonorrhea-detailed.htm - Centers for Disease Control and Prevention. (2017). Trichomoniasis - CDC fact sheet.
cdc.gov/std/trichomonas/stdfact-trichomoniasis.htm - Chlamydia, gonorrhea, and syphilis. (2019).
acog.org/Patients/FAQs/Chlamydia-Gonorrhea-and-Syphilis?IsMobileSet=false - Chlamydia symptoms. (n.d.).
plannedparenthood.org/learn/stds-hiv-safer-sex/chlamydia/chlamydia-symptoms - How to decode your vaginal discharge - and when to worry. (2016).
health.clevelandclinic.org/vaginal-discharge-mean/ - Kairys N, et al. (2019). Bacterial vaginosis. StatPearls.
ncbi.nlm.nih.gov/books/NBK459216/ - Mayo Clinic Staff. (2018).
 Vaginal odor.
Vaginal odor.
mayoclinic.org/symptoms/vaginal-odor/basics/causes/sym-20050664 - Mayo Clinic Staff. (2019). Penis health: Identify and prevent problems.
mayoclinic.org/healthy-lifestyle/mens-health/in-depth/penis-health/art-20046175 - Mayo Clinic Staff. (2019). Urinary tract infections (UTI).
mayoclinic.org/diseases-conditions/urinary-tract-infection/symptoms-causes/syc-20353447 - Nutritional value in a serving of semen. (n.d.).
goaskalice.columbia.edu/answered-questions/nutritional-value-serving-semen - Penis discharge. (2017).
conditions.health.qld.gov.au/HealthCondition/condition/16/166/111/penis-discharge - Steckelberg JM. (2018). Yeast infection in men: How can I tell if I have one?
mayoclinic.org/male-yeast-infection/expert-answers/faq-20058464 - Vaginal discharge. (n.d.).
playsafe.health.nsw.gov.au/2015/01/15/vaginal-discharge/ - Vaginal infections.
 (2014).
(2014).
girlshealth.gov/body/reproductive/infections.html - Vaginal yeast infections. (2019).
womenshealth.gov/a-z-topics/vaginal-yeast-infections - What is pre-ejaculate or precum? (n.d.).
issm.info/sexual-health-qa/what-is-pre-ejaculate-or-precum
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Share this article
Medically reviewed by Janet Brito, Ph.D., LCSW, CST — By Kirsten Nunez on July 8, 2019
Read this next
Thick White Discharge: What It Means
Medically reviewed by Carolyn Kay, M.D.
Discharge is a healthy part of vaginal health, but it can occasionally mean you're experiencing a health condition. Learn what to look for, and when…
READ MORE
The Ultimate Vaginal Discharge Color Guide
Medically reviewed by Fernando Mariz, MD
Vaginal discharge can say a lot about your health.
 Most of the time it’s typical, even if it's a different color. Here's our color swatch guide to…
Most of the time it’s typical, even if it's a different color. Here's our color swatch guide to…READ MORE
Is Male Discharge Normal?
Medically reviewed by Daniel Murrell, M.D.
While male discharge can be normal, there are reasons why discharge may be a symptom of infection or allergy. If you have penile discharge, your…
READ MORE
Sexually Transmitted Disease (STD) Information for Men
Medically reviewed by Joseph Vinetz, MD
STDs and STIs affect many people, but many people with a penis don't know they've acquired a condition that's affecting their health. Learn the risks.
READ MORE
Ask the Expert: Can Bacterial Vaginosis Clear Up on Its Own?
Bacterial vaginosis happens when there’s an imbalance of bacteria normally in the vagina.
 A doctor answers questions about treating it.
A doctor answers questions about treating it. READ MORE
Everything You Need to Know About Vaginal Infections
Vaginitis describes a number of conditions that can cause infection or inflammation of your vagina. We break down symptoms, treatment, and more.
READ MORE
The Best Yeast Infection Pills, Creams, and Treatment Options
Medically reviewed by Jennie Olopaade, PharmD, RPH
Yeast infections are common. Here are 7 of the best over-the-counter yeast infection pills, creams, gels, and treatments.
READ MORE
How Sanitary Are Bidets, Anyway?
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
Some research has shown that regular bidet use could increase your exposure to certain pathogens. Learn more.
READ MORE
Arpimed
What Clotrimazole is and what it is used for
Clotrimazole is used to treat vaginal yeast infections. Clotrimazole is effective against many vaginal fungal infections caused by yeast. Even if the symptoms of the infection disappear within a few hours or days, Clotrimazole should be used for at least 3 days. This will reduce the chance of a recurrence of the infection.
Clotrimazole is effective against many vaginal fungal infections caused by yeast. Even if the symptoms of the infection disappear within a few hours or days, Clotrimazole should be used for at least 3 days. This will reduce the chance of a recurrence of the infection.
Yeast infections
Yeast infections develop when there is an overgrowth of yeast in the vagina. The normal microflora of the vagina contains both various yeast fungi and bacteria. Under the influence of certain factors, the number of yeast fungi increases, causing irritation of the sensitive tissues of the vagina and the vaginal opening. Conditions that increase the likelihood of these infections are diseases and the use of antibiotics (antibiotics do not work against yeast). Changes in hormone levels in the body can also increase the risk of fungal infections. Changes that may occur during pregnancy, when taking birth control pills, or before the menstrual cycle can also increase the risk of developing vaginal fungal infections. Certain medical conditions, such as diabetes, can also increase your susceptibility to developing infections. Even factors such as hot, humid weather, constant use of panty liners, or tight, airtight clothing can increase your chance of developing yeast infections. These infections are not usually sexually transmitted, although a small percentage of male partners have these infections at the same time as women.
Certain medical conditions, such as diabetes, can also increase your susceptibility to developing infections. Even factors such as hot, humid weather, constant use of panty liners, or tight, airtight clothing can increase your chance of developing yeast infections. These infections are not usually sexually transmitted, although a small percentage of male partners have these infections at the same time as women.
What you need to know if you develop a yeast infection
When you develop a yeast infection, your body reacts with increased vaginal discharge. These secretions are mostly thick and sticky, but odorless. Outwardly, they resemble cheese or curd secretions, due to the similarity in appearance with cottage cheese. These secretions irritate the tissues of the vaginal area, causing intense itching, redness, and swelling. Sometimes red spots or sores may occur, especially due to severe itching if the area has been scratched during scratching. Possible symptoms are also soreness in the vaginal area, discomfort when urinating, pain during sexual intercourse.
Possible symptoms are also soreness in the vaginal area, discomfort when urinating, pain during sexual intercourse.
How Clotrimazole works
Clotrimazole is an antifungal drug that has a fungicidal effect against fungal yeast infections.
What do you need to know before the use of Clotrimazole
not use Clotrimazole Cream:
- If you are allergic to Clotrimazole or any other component of the drug,
- girls under 12 years of age, unless the medicine is prescribed by the attending physician.
Warnings and precautions
Talk to your doctor or pharmacist before using Clotrimazole if:
- are promiscuous or change partners frequently.
- You have diabetes.
- You have a fungal infection for the first time.
- You have frequent vaginal infections or if a fungal infection recurs in less than 2 months.

- You are pregnant, think you might be pregnant, or are breastfeeding.
Clotrimazole vaginal cream is for vaginal use only.
Do not use clotrimazole if you have abdominal pain, fever, or a foul-smelling vaginal discharge. If you experience these symptoms, it may be a sign of a more serious condition and therefore you should consult your doctor immediately.
Do not use tampons, intravaginal washes, or other vaginal products while using this drug.
Yeast infections do not cause fever, chills, nausea, vomiting, diarrhea, back pain, shoulder pain, or vaginal bleeding. If these symptoms are observed or an unpleasant odor from the vaginal discharge, there may be a more serious pathology and an immediate consultation of the attending physician is necessary.
If there is no improvement within 3 days, or if symptoms do not go away within 7 days, you may not have a vaginal yeast infection. Stop the course of treatment and consult a doctor.
If symptoms worsen, seek medical attention.
Avoid contact with eyes. If this happens, rinse your eyes thoroughly with water.
If you accidentally swallow clotrimazole, contact the nearest hospital emergency room immediately.
If you have any questions about the use of Clotrimazole or vaginal infections, ask your pharmacist or doctor.
Other medicines and Clotrimazole
Medicines that may interact with Clotrimazole:
- tacrolimus/sirolimus (immunosuppressants).
Clotrimazole cream may reduce the effectiveness of some contraceptives such as condoms, diaphragms, or vaginal spermicides.
This effect is temporary and is observed only during treatment.
How to take Clotrimazole
Recommended dose:
Cream Clotrimazole is injected as far as possible into the vagina once a day (preferably at bedtime) for 3 days without interruption. A sufficient course of cream treatment is 3 intravaginal applications, according to the procedure described below. In addition, you may need to apply a cream to relieve external itching and burning, sometimes associated with a vaginal yeast infection. Clotrimazole is for vaginal use only and should never be taken by mouth. You should not conduct a treatment course during the menstrual cycle. Treatment must be completed before the onset of menstruation. Although it is possible that there may be sexual intercourse during treatment with Clotrimazole, it is preferable that couples wait until the end of the treatment course in order to prevent infection of your partner.
A sufficient course of cream treatment is 3 intravaginal applications, according to the procedure described below. In addition, you may need to apply a cream to relieve external itching and burning, sometimes associated with a vaginal yeast infection. Clotrimazole is for vaginal use only and should never be taken by mouth. You should not conduct a treatment course during the menstrual cycle. Treatment must be completed before the onset of menstruation. Although it is possible that there may be sexual intercourse during treatment with Clotrimazole, it is preferable that couples wait until the end of the treatment course in order to prevent infection of your partner.
Applicator filling:
Remove the cap from the Clotrimazole tube, press and pierce the aluminum foil with the cap of the tube. To fill the applicator, screw the open end of the applicator barrel onto the threaded neck of the tube. Gently start squeezing the cream out of the tube. After that, by moving the piston upwards, the required amount of cream is drawn into the applicator cylinder. As the applicator fills, the piston is brought out. When the plunger reaches the stop and stops, the proper amount of Clotrimazole has already been filled into the applicator and the applicator can be unscrewed from the tip of the tube. Close the cap and leave the tube for the next use.
After that, by moving the piston upwards, the required amount of cream is drawn into the applicator cylinder. As the applicator fills, the piston is brought out. When the plunger reaches the stop and stops, the proper amount of Clotrimazole has already been filled into the applicator and the applicator can be unscrewed from the tip of the tube. Close the cap and leave the tube for the next use.
Cream administration:
Clotrimazole cream is inserted into the vagina in the same way as a tampon, standing, crouching or lying on your back, in a position convenient for you. Insert the filled applicator into the vagina. The depth of insertion depends on how comfortable you feel with the insertion. Hold the applicator barrel steady, insert the cream into the vagina by gently pressing on the applicator plunger until it stops. Insert the cream as deep as possible into the vagina, which will ensure the maximum effect of the drug. Remove the applicator.
Use a new applicator for each procedure.
External use of the cream:
A small amount of cream cutimazole can be applied to the external opening of the vagina to help additional relief of external symptoms. Squeeze a small amount of cream onto your finger and gently spread over the irritated area of the vagina. The cream should be used once or twice a day and only during the period when external symptoms are present, no more than 7 days.
If you have taken more clotrimazole than recommended
If you have taken more clotrimazole than recommended, contact your doctor immediately, contact the nearest hospital emergency room even if you do not have symptoms.
Possible side effects
If you develop a rash or new irritation while using the drug, stop using the drug and contact your doctor.
This is not a complete list of side effects. If you develop unexpected side effects while using Clotrimazole, contact your doctor or pharmacist.
If you develop unexpected side effects while using Clotrimazole, contact your doctor or pharmacist.
Reporting side effects:
Tell your doctor, pharmacist or nurse if you notice any side effects. This includes any possible side effects not listed in this package insert. You can also report side effects to Arpimed LLC by going to the website www.arpimed.com and filling out the appropriate form “Report a side effect or ineffectiveness of a drug” and to the Scientific Center for Expertise of Drugs and Medical Technologies named after. Academician E.Gabrielyan, by going to the website www.pharm.am in the section “Report a side effect of a drug” and fill out the form “Map of reporting a side effect of a drug”. Scientific center hotline: +37410237665; +37498773368
How to store Clotrimazole
Store at room temperature, dry and out of reach of children.
Shelf life - 3 years.
The contents of the packaging and additional information
that contains Clotrimazole
Each gram of Clotrimazole 2% vaginal cream contains:
Active substance: Clotrimazole - 20 mg;
other components: ceteareth-12, ceteareth-20, liquid paraffin, cetostearyl alcohol, methylparaben, propylparaben, propylene glycol, dimethicone, purified water.
What Clotrimazole looks like and contents of the pack
Uniform, even white cream, odorless.
Description of packaging
50 g vaginal cream in an aluminum tube with 3 vaginal applicators and leaflet in a cardboard box. The capacity of one applicator is 6 g Clotrimazole 2% vaginal cream.
Dispensing conditions
Available by prescription.
Pharmacy on Moskovskaya
PHARMATEX
Registration number:
Trade name: PHARMATEX
INN: Benzalkonium chloride
Dosage form: vaginal cream 1.2%
Composition per 100 g of cream
Active ingredient:
Benzalkonium chloride 50% ... ... aqueous solution2, ... ... .4 g,
which corresponds to benzalkonium chloride…………..….1.2 g
Excipients:
citric acid ……………………………….0.002 g
disodium hydrophosphate dodecahydrate ………up to pH 4.5-5.5
macrogol and ethylene glycol
palmitostearate (Tephose® 63) …………… ……24. 0 g
0 g
lavender oil…………………………………….0.05 g
purified water…………………………………. up to 100 g
Description
White homogeneous cream with lavender scent.
Pharmacotherapeutic group
Contraceptive for topical use.
ATC code: G02BB
Pharmacological properties
Pharmacodynamics
Spermicidal action is due to the ability of the active substance to destroy the membranes of spermatozoa (first the flagella, then the heads), which leads to the impossibility of fertilizing the egg with a damaged spermatozoon.
The effect develops immediately after insertion into the vagina.
In vitro active against Neisseria gonorrhoeae., Chlamydia spp., Trichomonas vaginalis., Herpes simplex type 2, Staphylococcus aureus. Has no effect on Mycoplasma spp. and has little effect on Gardnerella vaginalis, Candida albicans, Haemophilus ducreyi and Treponema pallidum.
Does not affect the normal microflora of the vagina (including the Doderlein stick) and the hormonal cycle.
Pharmacokinetics
Benzalkonium chloride is not absorbed by the vaginal mucosa, is removed by simple washing with water and with normal physiological secretions.
Indications for use
Local contraception for women of reproductive age (including if there are contraindications to the use of oral contraceptives or intrauterine contraception, in the postpartum period, lactation, after termination of pregnancy, during menopause, irregular sexual intercourse, missed or late appointments constantly used oral contraceptives).
As an additional local contraception when using a vaginal diaphragm or intrauterine device.
Contraindications
Hypersensitivity to the components of the drug, vaginitis, ulceration and irritation of the mucous membrane of the vagina and cervix.
Pregnancy and lactation
The drug is a contraceptive, not used during pregnancy.
When pregnancy occurs while using benzalkonium chloride contraception, no effects on the course of pregnancy were found. Not excreted in breast milk, can be used during lactation.
Not excreted in breast milk, can be used during lactation.
Dosage and Administration
For vaginal use.
Attach the dispenser to the tube instead of the cap. Gently squeeze out the contents of the tube until the dispenser is full (up to the stop of the piston) so that no air bubbles form. Disconnect the dispenser from the tube. Close the tube with a lid.
Lying on your back, insert the cream deep into the vagina using the dispenser, slowly pressing the plunger. The duration of action is 10 hours. Be sure to introduce a new dose of cream before each repeated sexual intercourse.
One dose (5 g of cream) is designed for one sexual intercourse.
Side effects
Allergic reactions, contact dermatitis, itching and burning in the vagina and/or partner's penis, painful urination.
If they occur, stop using Pharmatex.
If any of the side effects listed in the instructions worsen, or you notice any other side effects not listed in the instructions, tell your doctor.
Overdose
No cases of overdose have been reported.
Interaction with other medicinal products
Concomitant use with medicinal products administered vaginally is not recommended. Any drug introduced into the vagina can inactivate the local spermicidal action of Pharmatex.
Pharmatex is destroyed by soap. Do not irrigate the vagina before and after sexual intercourse, because soap, even its traces, destroys the active substance.
Special instructions
The effectiveness of contraception depends on the correct use of the drug.
• Do not use soap for the toilet of the genitals 2 hours before and after sexual intercourse, because. Soap destroys the active ingredient of Pharmatex.
• After sexual intercourse, the vulva can only be washed with clean water. Vaginal irrigation is applied 2 hours after intercourse.
• With Pharmatex inserted into the vagina, due to the risk of reducing the subsequent contraceptive effect, you can not take baths and swim in the sea, pool and reservoirs.