37 months pregnant
Pushing during childbirth | BabyCenter
There are two ways to push during labor. Coached (or directed) pushing means that your labor nurse gives you directions about when and how to push. Spontaneous (or physiological or mother-led) pushing means that you follow your body's natural urge to push.
Is there more than one way to push during labor?
Yes. There are two very different ways to push or bear down to help move your baby move through the birth canal during the second stage of labor. (The pushing stage goes until the baby is born, and it can last from a few minutes to several hours.)
- Coached pushing. This widely practiced method is also called directed pushing. With this type, a labor support person (often a nurse) directs you to begin pushing, often as soon as you're fully dilated to 10 centimeters, even if you don't feel an urge to bear down. You may also be instructed how to push. Coached pushing has long been routine in most U.S.
hospitals.
- Spontaneous pushing. This method is also known as physiological or mother-led pushing. With this method, you follow your body's natural urges, pushing when you feel ready, and in whatever way feels right to you. Midwives often favor spontaneous pushing.
There is ongoing research on the advantages and disadvantages of each method. The American College of Obstetricians and Gynecologists (ACOG) now recommends that women be encouraged to use whichever pushing technique is preferred and most effective for them.
What is delayed pushing?
Delayed pushing simply means resting for an hour or more at the beginning of the second stage of labor - after you are fully dilated but before you feel the urge to push. (The urge to push feels somewhat like the urge to have a bowel movement.) Pushing can be delayed with either coached or spontaneous pushing methods.
Women sometimes don't feel a strong urge to push as soon as they are dilated, and resting gives time for the sensation to develop. This is especially true for women who have had an epidural (see below).
This is especially true for women who have had an epidural (see below).
If, however, you feel a natural urge to push, there is no reason to delay pushing unless you are exhausted. In fact, pushing as soon as you feel the urge may feel like a relief.
How is coached pushing done?
Coached pushing can begin as soon as your cervix has dilated completely to 10 centimeters, which marks the beginning of the second stage of labor, or it may be delayed, as described above, to allow your sensation to build up.
In most cases, a labor and delivery nurse leads the coaching. Typically, you're told to take a deep breath at the beginning of every contraction, hold it, then tighten your abdominal muscles and push down with as much force as possible while the nurse counts to 10. This is also known as the Valsalva method. (Some moms say it feels like straining to have a bowel movement.)
Then you take a quick breath and push for another count of 10, aiming to get in three pushes during each contraction.
To avoid tearing, you may be told to stop pushing when your baby is crowning - that's when the widest part of the baby's head is passing through your vagina.
How does spontaneous pushing differ from coached pushing?
With spontaneous pushing, you simply follow your urge to push when and how your body tells you to (rather than when and how a nurse tells you to).
Women doing spontaneous pushing tend not to take a deep breath beforehand, and they often exhale while pushing instead of holding their breath. The role of the labor support person is to remind you to listen to your body and encourage you to bear down whenever and however it feels right to you.
You may feel an uncontrollable urge to push as soon as you're fully dilated, but many women don't - particularly those who have an epidural. If you don't have an urge to bear down at this point, you can rest while the baby continues to descend from the force of your contractions alone. (This is sometimes referred to as “laboring down. ”)
”)
Once you start feeling the urge, you may push for just a few seconds during the peak of the contractions at first, and not during every contraction, or you may push with tremendous force - again, doing what your body tells you to do. Women who aren't being coached generally let a contraction build before bearing down. Also, spontaneous pushes tend to be in shorter but more frequent bursts during contractions. Your body will help to guide your efforts.
As the baby descends and puts increasing pressure on your pelvic floor (the muscles and other tissue that support the uterus, vagina, bladder, and rectum), you may begin to push harder and more often during contractions. You may also grunt, groan, or make other noises when pushing.
How does having an epidural affect pushing?
If you have an epidural, the sensation to push may be delayed. (It’s also possible to have an epidural so strong that you never feel this urge.) In some cases, a provider may let the epidural start to wear off when it's almost time to push, to aid the sensation.
With an epidural, a combination of delayed pushing for an hour or so (until you have a stronger sensation,) and pushing with coaching may be best.
What other factors might affect pushing?
In cases where your labor needs to be induced because your baby is measuring smaller than expected, or your amniotic fluid is low - conditions that might be found in a routine sonogram around your due date - or you are a week or so past your due date, pushing gently and following your body's urges may be easier for the baby than coached, breath-holding pushing. Sometimes, in these cases, if the baby shows signs of stress during the second stage, you may be advised to push every other contraction.
However, it's also possible in these circumstances that your provider may want to get the baby out as quickly as possible. Then you'd likely be coached to push.
Is coached pushing or spontaneous pushing better?
A 2017 review of eight studies comparing coached and spontaneous pushing found no significant differences in outcomes between the two methods. Researchers recommended letting the mother choose to push as she wishes. Other researchers, however, have found some negative associations with coached pushing and with delayed pushing. (see below).
Researchers recommended letting the mother choose to push as she wishes. Other researchers, however, have found some negative associations with coached pushing and with delayed pushing. (see below).
Discuss pushing techniques with your doctor or midwife during your pregnancy. Your decision about how to push may be based on a number of factors, including how you feel about the coaching process, whether or not you will be having an unmedicated birth, whether your labor is being induced for reasons pertaining to the baby and how previous labors and deliveries progressed (if this is not your first baby), for example.
Are there disadvantages of coached pushing?
Some studies have found that coached pushing as it's typically practiced is associated with one or more of the following:
- Higher risk of moderate and severe perineal injury
- Higher rate of episiotomy
- Higher risk of the need for neonatal resuscitation and intensive care nursery admission due to increased stress on the baby during the pushing stage.
 (This is often the result of acidemia, a buildup of lactic acid in the blood due to reduced oxygen flow from the placenta. It may be caused by prolonged breath-holding during pushing.)
(This is often the result of acidemia, a buildup of lactic acid in the blood due to reduced oxygen flow from the placenta. It may be caused by prolonged breath-holding during pushing.)
Many midwives point out that coached pushing dismisses a woman's instinctual knowledge of when and how to push and limits her ability to give birth in a gentle manner.
Are there disadvantages of spontaneous pushing?
Spontaneous pushing may take longer than coached pushing. Women who use the spontaneous pushing method push about nine minutes less than those who are coached to push immediately, but overall their second stage of labor is longer by about half an hour, if they delay pushing until they have the urge.
In addition, women who don't feel the urge to push may eventually need some guidance to help them push effectively. And if you're so fearful or tense during labor that you have trouble listening to your body's cues, or if you're too afraid to push because you don't like the sensation, coaching may be more appropriate than spontaneous pushing.
The risks of spontaneous pushing are those associated with delayed pushing (see below).
What are the disadvantages of delayed pushing?
In some studies, women who delayed pushing (rather than pushing as soon as they reached 10 cm dilation) had higher rates of :
- Intrauterine infections
- Postpartum bleeding
- Babies with acidemia (excess lactic acid in the blood from reduced oxygen transmission from the placenta. In this case, acidemia may be caused by a longer labor.)
- Babies with higher rates of sepsis (again, likely due to longer labor)
One study concluded that delayed pushing for an hour or more was associated with a modest increase in cesarean delivery and assisted delivery.
Want to learn more about the process of labor and delivery? Our Childbirth Class Videos will teach you the signs and stages of labor, pain management techniques, medical procedures, and more.
Learn more:
- Birth plan: Your expectations and preferences
- What to pack in your hospital bag
- Preparing for your baby's arrival
- What happens to your baby after delivery
advertisement | page continues below
37 Weeks Pregnant: Symptoms and Baby Development
37 Weeks Pregnant: Your Baby’s Development
Your pregnancy is quickly coming to an end, but your little one still has a bit more growing to do. This week, she’s probably gaining about a half an ounce each day, adding fat and plumping up before birth.
Keep in mind that although you’re super close to your due date, your pregnancy is still considered to be in the “early term” stage at this point. Your pregnancy won’t be considered “full term” until the start of 39 weeks.
In other developments, your baby has now shed most of the lanugo, the fine body hair that covered her little body while in your uterus. She’s now able to make grasping motions with her fingers. Plus, she may also respond to bright lights in the outside world by moving or turning toward the light.
If she hasn’t already, she may also be moving into a head-down position in preparation for labor.
This week, she’s probably gaining about a half an ounce each day, adding fat and plumping up before birth.
Keep in mind that although you’re super close to your due date, your pregnancy is still considered to be in the “early term” stage at this point. Your pregnancy won’t be considered “full term” until the start of 39 weeks.
In other developments, your baby has now shed most of the lanugo, the fine body hair that covered her little body while in your uterus. She’s now able to make grasping motions with her fingers. Plus, she may also respond to bright lights in the outside world by moving or turning toward the light.
If she hasn’t already, she may also be moving into a head-down position in preparation for labor.
RELATED PREGNANCY TOOL
Baby Name Generator
By gender:
Unisex
By theme:
Nature
Mythology
The Size of the Fetus at 37 Weeks Pregnant
At 37 weeks, the average fetus is about the size of a Swiss chard. Wondering how your baby may be positioned at 37 weeks? Although we can’t say for sure exactly how your little one is curled up inside your belly this week, check out this illustration for a general idea of what you might see if you could take a sneak peek inside:
Wondering how your baby may be positioned at 37 weeks? Although we can’t say for sure exactly how your little one is curled up inside your belly this week, check out this illustration for a general idea of what you might see if you could take a sneak peek inside:
Mom's Body at 37 Weeks Pregnant
Are you wondering how many months along you are at 37 weeks pregnant? Because pregnancy doesn't divide neatly into months, it’s possible you’re either 9 or 10 months pregnant at this point.
At 37 weeks pregnant, your cervix may be beginning to dilate. When this starts to happen, you may lose the seal that protected your uterus from infection throughout your pregnancy. This seal is known as the mucus plug.
If, at 37 weeks pregnant, you notice some extra vaginal discharge that is clear, pinkish, or slightly bloody, this may be the mucus plug. Seeing this mucus discharge is an indication that labor is starting or is not far off. Keep in mind, you can lose the mucus plug hours, days, or even weeks before labor begins. Some moms-to-be don’t notice it at all.
At 37 weeks, if you do notice the mucus plug on your panties or on the toilet paper after you wipe, or if you are unsure if this means your labor has started, you may want to call your healthcare provider for advice on what to do next.
Twins and triplets are more likely to be born earlier than a single baby, so keep an eye out for signs of labor if you’re 37 weeks pregnant with twins or more.
Keep in mind, you can lose the mucus plug hours, days, or even weeks before labor begins. Some moms-to-be don’t notice it at all.
At 37 weeks, if you do notice the mucus plug on your panties or on the toilet paper after you wipe, or if you are unsure if this means your labor has started, you may want to call your healthcare provider for advice on what to do next.
Twins and triplets are more likely to be born earlier than a single baby, so keep an eye out for signs of labor if you’re 37 weeks pregnant with twins or more.
37 Weeks Pregnant: Your Symptoms
At 37 weeks pregnant, here are some of the symptoms you may be experiencing:
Pelvic pain or pressure. Is your baby sitting lower in your pelvis these days? This dropping — also called lightening or engagement — can occur a few weeks before your baby is born, and you might notice it if you feel a little extra pressure on your lower abdomen.
 This pelvic pain can even make it hard to walk. If pelvic pressure is causing you discomfort, a warm bath may provide some relief. Contact your healthcare provider for more advice on what to do to relieve pelvic or lower back pain.
This pelvic pain can even make it hard to walk. If pelvic pressure is causing you discomfort, a warm bath may provide some relief. Contact your healthcare provider for more advice on what to do to relieve pelvic or lower back pain.
Shortness of breath. If your baby hasn’t dropped yet, she might be pressing up against your lungs, making breathing a little more difficult. Try to rest more, move slowly, and sit or stand up straight to help give your lungs more room to expand with each breath. Once your baby “drops” lower into your pelvis, this may take some pressure off your lungs and diaphragm, making it easier for you to breathe.
Nausea. Some moms-to-be experience nausea around 37 weeks pregnant, and it could be a sign that labor is about to start. Try to eat four or five smaller meals instead of three larger meals. Bland foods like rice, toast, or bananas can also help get you through these bouts of nausea.
Snoring.
 This one might not trouble you as much as your partner. Most moms-to-be go through some breathing changes during pregnancy thanks to hormonal changes, and toward the end, some snoring is not uncommon as the mucus membranes in your nasal passages tend to dry out. Make sure you’re staying hydrated, and use a humidifier in your bedroom if your partner starts to complain about your snoring.
This one might not trouble you as much as your partner. Most moms-to-be go through some breathing changes during pregnancy thanks to hormonal changes, and toward the end, some snoring is not uncommon as the mucus membranes in your nasal passages tend to dry out. Make sure you’re staying hydrated, and use a humidifier in your bedroom if your partner starts to complain about your snoring.
Unstable on your feet. By now, your pregnancy weight gain means your center of gravity has shifted, making it easier for you to lose your balance. This extra weight from your baby, the placenta, amniotic fluid, and more can make it challenging to move around. Once your baby drops lower into your pelvis, the distribution of your weight may even change again, so be extra careful whenever you’re on your feet! To keep yourself steady, stand with your feet pointed in the same direction with your weight balanced evenly on both feet. Try not to tilt your pelvis forward or backward, and avoid lifting or carrying heavy or bulky items.

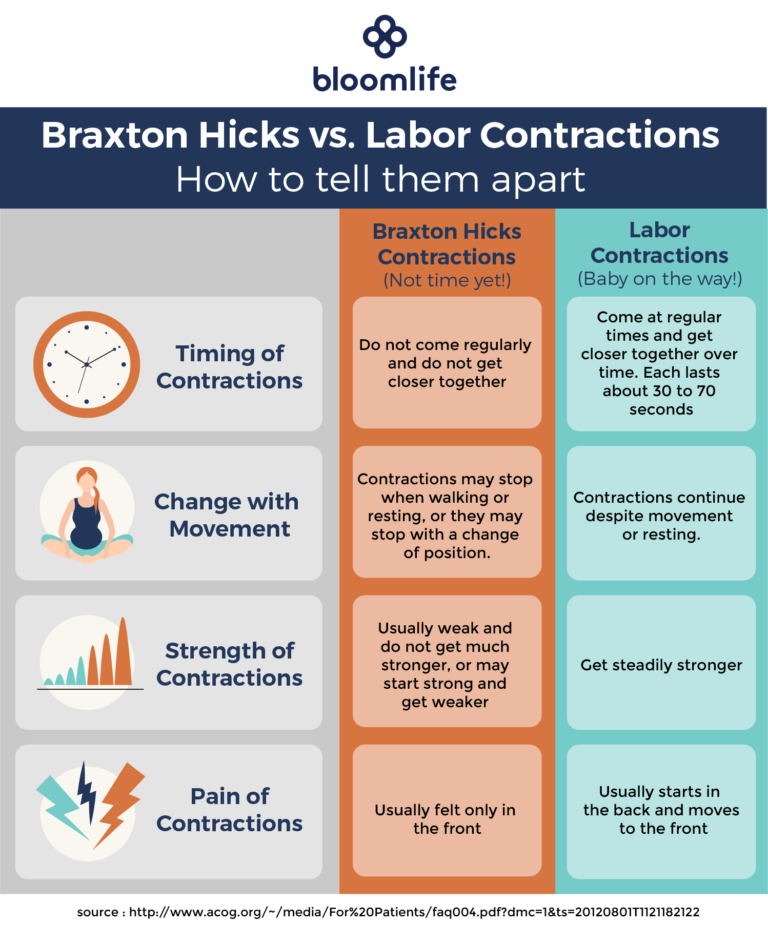
Contractions. At 37 weeks pregnant, you could start to feel contractions that you might recognize as being similar to menstrual cramping. Contractions that are irregular and go away when you move or change positions are likely Braxton Hicks “practice” contractions. But, if you feel contractions that occur regularly, get progressively stronger, and don’t subside if you move or change positions, you’ll want to call your healthcare provider for advice. Timing your contractions and having this info to give your provider on the phone, will give your provider important information. Learn how to time contractions here.
37 Weeks Pregnant: Things to Consider
There are a variety of different birthing positions and comfort measures that can help during labor and delivery. Some require equipment such as a birthing bed, chair, pool, or ball. It’s a good idea to ask ahead of time what’s available at your hospital or birth center.
 Also, try to keep an open mind; once you’re in labor, you may find that what you actually find comfortable is different from what you expected to find comfortable.
Also, try to keep an open mind; once you’re in labor, you may find that what you actually find comfortable is different from what you expected to find comfortable.
37 Weeks Pregnant: Ask Your Doctor
What happens if your baby doesn’t turn head-down?
Under what circumstances might you need a cesarean section?
Is your birth partner allowed to be with you when you give birth? What if you’re having a cesarean section?
How many people can you have with you during labor?
What happens right after you give birth?
How long are you likely to stay in hospital after you give birth, and what happens during that time?
37 Weeks Pregnant: Your Checklist
If you haven’t already done so, pack your hospital bag. The big day could be just around the corner!
Stock your freezer with meals you can simply heat up.
 After your baby is born, you may not have time to cook.
After your baby is born, you may not have time to cook.
Finalize your baby’s nursery, and get any baby essentials you haven’t bought yet. Keep in mind that most babies don’t arrive exactly on their due date and that yours could come early.
Consider getting a waterproof sheet to protect your mattress in case your water happens to break while you’re asleep.
If you see breastfeeding or pumping in your future, make sure you have several quality nursing bras.
Consider setting up a comfortable “feeding station” in your baby’s nursery or elsewhere in your home. For example, you might like to buy a comfy nursery glider, place a lamp or night light next to it, and have a nursing pillow and a quilt on hand to help you feel comfortable. Some parents also have a nursing basket nearby with supplies like tissues, burp cloths, nipple cream (if you’re planning to breastfeed), and snacks for you.
Start stocking up on diapers and collecting rewards points from our Pampers Club app.

If you have a little downtime this week, spend a little of it browsing the net for the best baby gear as voted by Pampers Parents. You might already have your eye on lots of what you’ll need, but you may like to check out some feeding essentials (and nice-to-haves) like the best baby bottles and the best bottle warmers.
Sign up for even more weekly pregnancy tips:
37-40 weeks of pregnancy
37th week of pregnancy for a baby
At 37 weeks of gestation, the baby is approximately 48 cm tall and weighs 2,600 g. facial features, pronounced cartilage tissue. The accumulation of subcutaneous fat at this stage of pregnancy makes the outline of the body softer and more rounded. The skin of the child is gradually smoothed out, it is no longer as pink as in the previous weeks of intrauterine development, the integument gradually brightens. The body of the baby is still abundantly covered with grease, but the amount of fluff is noticeably reduced, fluff hair remains only on the shoulders and back, in some babies they disappear almost completely.
Fat accumulation continues this week. It reaches a maximum of 15% of the total body weight of the child. It is difficult to overestimate the importance of adipose tissue for newborns, it is it that protects the child from overheating or hypothermia, since the baby's thermoregulation system after childbirth is still not sufficiently formed and continues to develop in the first months of a small person's life.
At this time, not only the volume of subcutaneous fat increases, but muscles and skeleton also develop intensively. The child constantly moves arms and legs. These unique workouts help increase muscle mass. Also, the baby makes rhythmic respiratory movements that strengthen the intercostal muscles and the diaphragm, and prepare the respiratory organs for childbirth.
Pregnant woman at 37 weeks
As the due date approaches, pregnant women begin to notice the appearance of their precursors, that is, certain signs, changes that occur under the influence of hormones. The body of a woman is preparing to give birth to a child, progesterone gives way to the dominant role of the birth hormone estrogen, the state of health of a pregnant woman changes.
The body of a woman is preparing to give birth to a child, progesterone gives way to the dominant role of the birth hormone estrogen, the state of health of a pregnant woman changes.
From the 37th week, expectant mothers can observe the following changes:
- slight weight loss;
- abdominal shrinkage;
- the appearance of training or "false" contractions and the increase in their intensity;
- discharge of mucus from the cervix.
The nature of the stool changes, it becomes looser, aching pains in the lower back of varying intensity may appear, the fundus of the uterus descends. A woman notes some signs on her own, others are observed by a gynecologist during a routine examination.
Harbingers do not appear in all women. Some expectant mothers notice only some of the above symptoms, while others observe signs of an impending birth not two or three weeks before their date, but just a few hours. Both the appearance of precursors at the 37th week and their absence are a variant of the norm and depend on the individual characteristics of the woman's body.
This week the woman's body is intensified preparation for the birth of a child. If the fetus is located correctly, head down, it gradually descends, goes to the lower part of the uterus, presses to the body and bends the limbs, intuitively taking the most comfortable position for passing the birth canal. The consequence of the movement of the fetus is the omission of the bottom of the uterus. The abdomen drops, the pressure on the diaphragm significantly decreases, the pregnant woman can breathe easily, the shortness of breath that haunted her in previous weeks disappears. The pressure on the stomach also decreases, heartburn disappears, a feeling of heaviness after eating and other unpleasant sensations. Moving the baby can put pressure on the bowels and bladder. A pregnant woman at this time often experiences the urge to urinate, may suffer from frequent loose stools. The reason for frequent bowel movements is not only the mechanical effect of the uterus on it, but also an increase in the content of estrogens in the body, hormones that contribute to the excretion of fluid. At the 37th week, the expectant mother can empty her intestines up to 3-4 times a day and at the same time observe a significant liquefaction of feces.
At the 37th week, the expectant mother can empty her intestines up to 3-4 times a day and at the same time observe a significant liquefaction of feces.
38th week of pregnancy: the development of the future baby
At the 38th week, the fetus is fully formed, so childbirth at this time is no longer dangerous for both the mother and the baby. The weight of the fetus is about 3 kg, but this indicator can vary significantly for different babies, the weight depends on the individual characteristics of the mother and child, the structural features of the body and other factors. The body length of a newborn is approximately 50 cm.
All organs and systems at 38 weeks of age are characterized by physiological and morphological maturity, they are fully ready for work. At this time, the child prepares for childbirth, makes respiratory movements and prepares the intercostal muscles for breathing. The tissues of the lungs are bathed in amniotic fluid, which helps maintain the right level of surfactant that coats the baby's lungs from the inside. All elements of the respiratory system are ready for use. With the first breath after birth, the alveoli begin to transfer oxygen from the air to the blood, gas exchange occurs, the respiratory and circulatory systems begin to work intensively.
All elements of the respiratory system are ready for use. With the first breath after birth, the alveoli begin to transfer oxygen from the air to the blood, gas exchange occurs, the respiratory and circulatory systems begin to work intensively.
Pregnant woman
The body of a pregnant woman continues to actively prepare for the birth of a baby, the estrogen content rapidly increases, and the progesterone level decreases significantly. A change in the hormonal background contributes to the softening of the tissues of the birth canal and cervix. Throughout pregnancy, the lumen of the cervical canal is closed by a plug of thick mucus, which protects the baby from infection, and the uterine cavity protects against the penetration of microorganisms dangerous to health. In the last weeks of pregnancy, the consistency of the mucus changes, it becomes more liquid and begins to gradually flow out. In some women, mucus leaves gradually, while in other women in labor at the same time. The discharge resembles colorless egg white in its consistency and appearance. Sometimes the mucus is colored pinkish, brown or yellow. The discharge of the cork is painless, a woman may experience a slight feeling of discomfort in the lower abdomen. More abundant vaginal discharge than during the entire pregnancy can signal the passage of the cork.
The discharge resembles colorless egg white in its consistency and appearance. Sometimes the mucus is colored pinkish, brown or yellow. The discharge of the cork is painless, a woman may experience a slight feeling of discomfort in the lower abdomen. More abundant vaginal discharge than during the entire pregnancy can signal the passage of the cork.
A woman should carefully monitor the color and volume of discharge, since too much colorless discharge may indicate not only the cork has come off, but also be one of the symptoms of amniotic fluid leakage. Indicator pads and amnio tests or test strips will help determine the cause of the discharge. Pads are sold in many pharmacies and can be easily used at home. If amniotic fluid leakage is confirmed, you should immediately consult a doctor.
After the mucus plug has passed, you should stop visiting the pool and swimming in open water, as the risk of infection of the child increases significantly. It is also necessary to exclude sexual contact.
39th week of pregnancy: what happens to the fetus?
At 39 weeks, the baby weighs 3100-3500 g and is 50-52 cm tall. Height and weight are very relative and can vary significantly. The baby is rapidly preparing for the most important test of his life - birth, which requires endurance and considerable effort. During this period of pregnancy, the size and weight of the child's adrenal glands, that is, the glands of the endocrine system, which are responsible for the reaction of the human body to stress factors, increase. It is the hormones adrenaline and norepinephrine produced by the adrenal glands that help the child quickly adapt to new temperature conditions, tactile, sound and light impulses.
All the senses of the baby are developed at 39 weeks. Within a few moments after birth, the baby can focus his eyes, he reacts to bright light and moving objects, many scientists claim that newborns distinguish colors, see the faces of parents and doctors. The hearing of the baby in the last weeks of fetal life is also fully developed; after birth, he reacts to loud sounds and noise. A newborn baby is able to determine the main shades of taste, recognize sour, bitter, sweet and salty.
A newborn baby is able to determine the main shades of taste, recognize sour, bitter, sweet and salty.
In the womb, the baby is in an aquatic environment that minimizes contact. Immediately after birth, the baby experiences many tactile sensations, unlike intrauterine life, he feels the touch of his mother's hands and diapers, towels, dressings and other materials. Babies especially like the touch of skin to skin, so in a modern maternity hospital, newborns must be laid out on their mother's stomach even before cutting the umbilical cord. The child adapts to the new environment more easily, feels protected. Laying out a child has not only a psychological aspect, since it contributes to the colonization of microorganisms from the mother's skin to the skin and mucous membranes of the baby, and increases its immunity.
Pregnant woman
In the last weeks of pregnancy, the expectant mother strives to prepare her apartment or house as much as possible for the arrival of a new family member. Scientists call this sign of impending birth the nesting syndrome. Many women observe signs of the syndrome from the thirtieth week of pregnancy, however, nesting reaches its maximum point at the 39-40th week. Pregnant women tend to do general cleaning and repairs, re-paste the wallpaper and purchase a lot of new things that, in their opinion, are simply necessary in the house. After giving birth, many purchases are puzzling. The reason for this behavior is an increase in the level of adrenaline and norepinephrine in the body. These hormones are produced by the adrenal glands, they are necessary not only for the woman, but also for the baby to prepare for the upcoming birth.
Scientists call this sign of impending birth the nesting syndrome. Many women observe signs of the syndrome from the thirtieth week of pregnancy, however, nesting reaches its maximum point at the 39-40th week. Pregnant women tend to do general cleaning and repairs, re-paste the wallpaper and purchase a lot of new things that, in their opinion, are simply necessary in the house. After giving birth, many purchases are puzzling. The reason for this behavior is an increase in the level of adrenaline and norepinephrine in the body. These hormones are produced by the adrenal glands, they are necessary not only for the woman, but also for the baby to prepare for the upcoming birth.
40th week of pregnancy: how does the baby develop?
40 weeks - term pregnancy. The weight of a child who was born at such a period ranges from 2,600 g to 4,400 g, and his body length is 48-53 cm. These indicators are very arbitrary, since miniature babies weighing 2,600 g and real heroes are born at 40 weeks, whose body weight approaches 5,000 g. The length of the newborns can also vary from 45 to 55 cm.
The length of the newborns can also vary from 45 to 55 cm.
Most women give birth exactly at 40 weeks. At this time, the baby is completely ready for birth, it meets all the parameters of a full-term baby. Before childbirth, the child closely presses the arms and legs to the body, bends the head as much as possible and presses against the exit from the uterus. This position allows you to make it possible to pass the birth canal with the narrowest part of the skull. In the course of labor, with each contraction, the child gradually moves down, he does not move in a straight line, but makes helical-translational movements, as if screwing into the mother's birth canal. During the progress of the newborn, the complete descent of his head, the cervix fully opens. This is followed by attempts, that is, contractions of the uterus, which advance the child through the birth canal. Gradually, the head of the baby is shown, and after it - his torso. Childbirth is a complex mechanism that is aimed not only at the safe passage of the birth canal by the child, protecting him from accidental injuries due to increased pressure, but also at preventing ruptures of the woman's soft tissues.
Pregnant woman
The long wait for meeting her unborn child is coming to an end, and the 40th week of pregnancy is the last for most women. Every day, the anxiety of the expectant mother increases, a long wait affects the mood and well-being. Women strive to have a baby as soon as possible so that pregnancy and painful contractions are a thing of the past. Every pregnant woman dreams of meeting a baby, wants to hug him to her chest and stroke the delicate head.
Many women, especially primiparas, are afraid that labor will begin unnoticed, but such cases are extremely rare. A woman feels the onset of childbirth, feels regular contractions, which are repeated at regular intervals and gradually increase, the time interval between them is reduced.
Labor may be preceded by prenatal rupture of amniotic fluid, which occurs in a certain percentage of women in labor. After the waters break, contractions may be quite weak or completely absent. Regardless of the intensity of contractions, the outpouring of water is one of the signs of the onset of labor and requires immediate contact with specialists, hospitalization of a woman in a maternity hospital or hospital, since when the water breaks, the integrity of the bladder is violated and the risk of penetration of microorganisms dangerous to the health of the child increases into the uterine cavity. It is important that after the water breaks, the baby is born in a maximum of 10-12 hours.
It is important that after the water breaks, the baby is born in a maximum of 10-12 hours.
A pregnant woman should properly tune in to childbirth, concentrate on the desired result and believe in her own strength, fulfill the task assigned to her by nature. The right psychological attitude and theoretical knowledge will help a woman become a mother, successfully go through all the stages of childbirth and press the long-awaited child to her heart.
37th week of pregnancy - fetal development, mother's feelings. What happens to mom at 37 weeks pregnant?
Congratulations, your pregnancy is considered full-term! Childbirth can begin at any time. If you are expecting a planned caesarean section, then most likely it will be scheduled for 38-39week. The placenta has reached the third degree of maturity and begins to age.
The cartilage and bones of the baby are strengthened, the respiratory and digestive systems are ready to function outside the mother's womb, the sufractant continues to accumulate in the lungs.