20 weeks miscarriage pictures
Miscarriage - what you might actually see and feel
Miscarriage - what you might actually see and feel | Pregnancy Birth and Baby beginning of content7-minute read
Listen
WARNING — This article contains some graphic descriptions of what you might see during a miscarriage.
A miscarriage requires prompt medical care. If you think you are having a miscarriage, call your doctor or midwife for advice and support. Go to the Emergency Department if:
- you are bleeding very heavily (soaking more than 2 pads per hour or passing clots larger than golf balls)
- you have severe pain in your tummy or shoulder
- you have a fever (a temperature above 38 degrees C)
- you are dizzy, fainting or feel like fainting
- you notice fluid coming from your vagina that smells bad
- you have diarrhoea or pain when you have a bowel motion (do a poo)
Miscarriage is a very unfortunate and sad outcome of pregnancy that takes a significant emotional and physical toll on a woman. It also happens more frequently than many people think. It's important to recognise that there's no right or wrong way to feel about a miscarriage.
Despite close to one in 5 pregnancies ending in miscarriage, what actually happens and what a woman needs to know and do when faced with a possible miscarriage are subjects that rarely get discussed.
This article aims to give you an idea of what happens and what a woman needs to know and do at different stages in her pregnancy.
Please call Pregnancy, Birth and Baby on 1800 882 436 if you have any concerns or wish to discuss the topic further.
What might I feel during a miscarriage?
Many women have a miscarriage early in their pregnancy without even realising it. They may just think they are having a heavy period. If this happens to you, you might have cramping, heavier bleeding than normal, pain in the tummy, pelvis or back, and feel weak. If you have started spotting, remember that this is normal in many pregnancies — but talk to your doctor or midwife to be safe and for your own peace of mind.
Later in your pregnancy, you might notice signs like cramping pain, bleeding or passing fluid and blood clots from your vagina. Depending on how many weeks pregnant you are, you may pass tissue that looks more like a fetus, or a fully-formed baby.
In some types of miscarriage, you might not have any symptoms at all — the miscarriage might not be discovered until your next ultrasound. Or you might just notice your morning sickness and breast tenderness have gone.
It is normal to feel very emotional and upset when you realise you’re having a miscarriage. It can take a while to process what is happening. Make sure you have someone with you, for support, and try to be kind to yourself.
What happens during a miscarriage?
Unfortunately, nothing can be done to stop a miscarriage once it has started. Any treatment is to prevent heavy bleeding or an infection.
Your doctor might advise you that no treatment is necessary. This is called 'expectant management', and you just wait to see what will happen.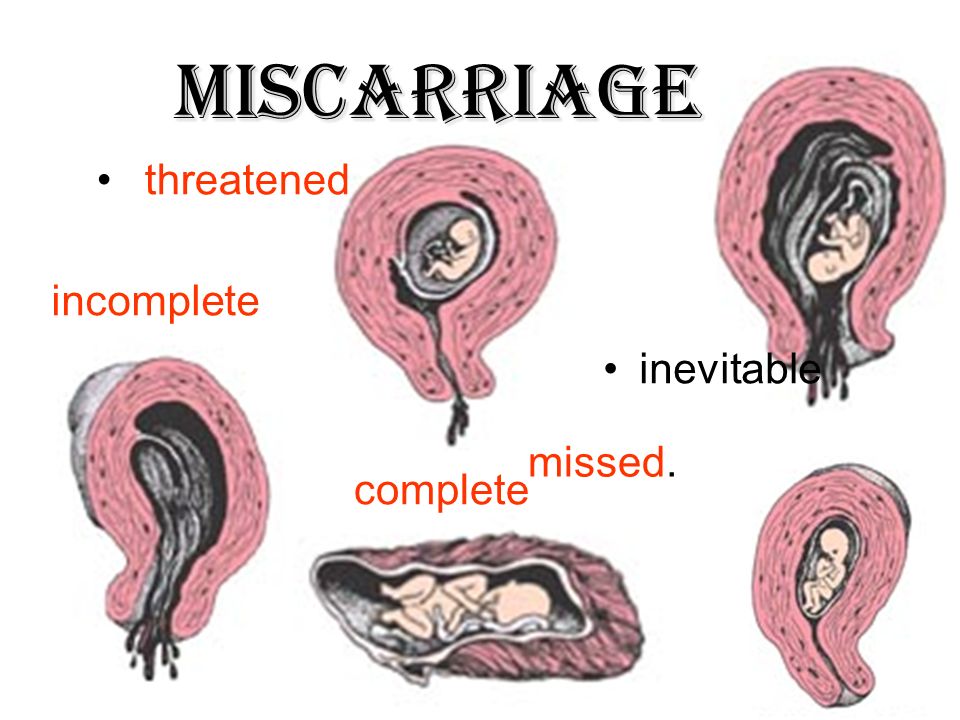 Eventually, the pregnancy tissue (the fetus or baby, pregnancy sac and placenta) will pass naturally. This can take a few days or as long as 3 to 4 weeks.
Eventually, the pregnancy tissue (the fetus or baby, pregnancy sac and placenta) will pass naturally. This can take a few days or as long as 3 to 4 weeks.
It can be very hard emotionally to wait for the miscarriage because you don’t know when it will happen. When it starts, you will notice spotting and cramping and then, fairly quickly, you will start bleeding heavily. The cramps will get worse until they feel like contractions, and you will pass the pregnancy tissue.
Some women opt to have medicine to speed up the process. In this case, the pregnancy tissue is likely to pass within a few hours.
If not all the tissue passes naturally or you have signs of infection, you may need to have a small operation called a ‘dilatation and curettage’ (D&C). You may need to wait some time for your hospital appointment. The operation only takes 5 to 10 minutes under general anaesthetic, and you will be able to go home the same day.
While you are waiting for a miscarriage to finish, it’s best to rest at home — but you can go to work if you feel up to it. Do what feels right for you. You can use paracetamol for any pain. If you are bleeding, use sanitary pads rather than tampons.
Do what feels right for you. You can use paracetamol for any pain. If you are bleeding, use sanitary pads rather than tampons.
What might I see during a miscarriage?
In the first month of pregnancy, the developing embryo is the size of a grain of rice so it is very hard to see. You may pass a blood clot or several clots from your vagina, and there may be some white or grey tissue in the clots. The bleeding will settle down in a few days, although it can take up to 2 weeks.
At 6 weeks
Most women can’t see anything recognisable when they have a miscarriage at this time. During the bleeding, you may see clots with a small sac filled with fluid. The embryo, which is about the size of the fingernail on your little finger, and a placenta might be seen inside the sac. You might also notice something that looks like an umbilical cord.
At 8 weeks
The tissue you pass may look dark red and shiny — some women describe it as looking like liver. You might find a sac with an embryo inside, about the size of a small bean.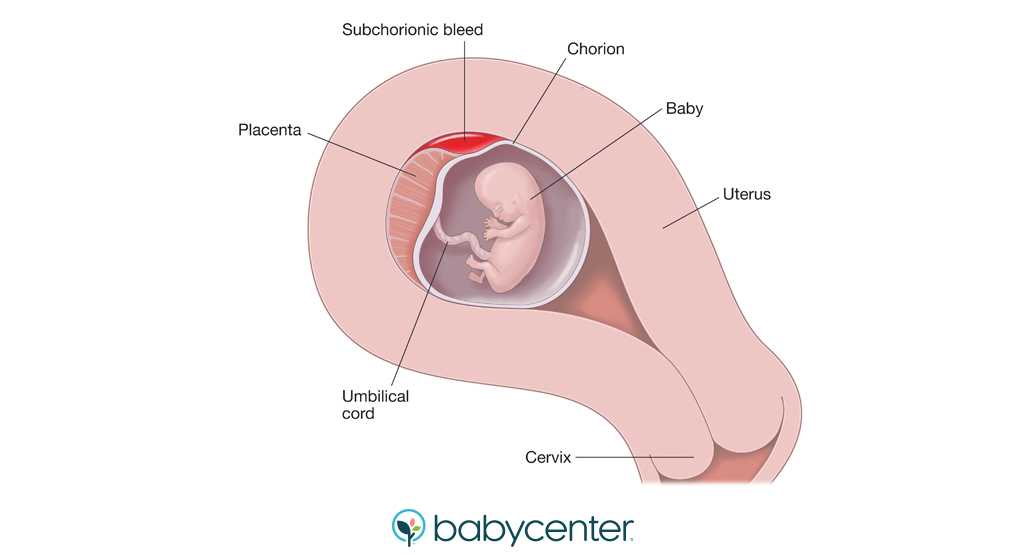 If you look closely, you might be able to see where the eyes, arms and legs were forming.
If you look closely, you might be able to see where the eyes, arms and legs were forming.
At 10 weeks
The clots that are passed are dark red and look like jelly. They might have what looks like a membrane inside, which is part of the placenta. The sac will be inside one of the clots. At this time, the developing baby is usually fully formed but still tiny and difficult to see.
At 12 to 16 weeks
If you miscarry now, you might notice water coming out of your vagina first, followed by some bleeding and clots. The fetus will be tiny and fully formed. If you see the baby it might be outside the sac by now. It might also be attached to the umbilical cord and the placenta.
From 16 to 20 weeks
This is often called a 'late miscarriage'. You might pass large shiny red clots that look like liver as well as other pieces of tissue that look and feel like membrane. It might be painful and feel just like labour, and you might need pain relief in hospital. Your baby will be fully formed and can fit on the palm of your hand.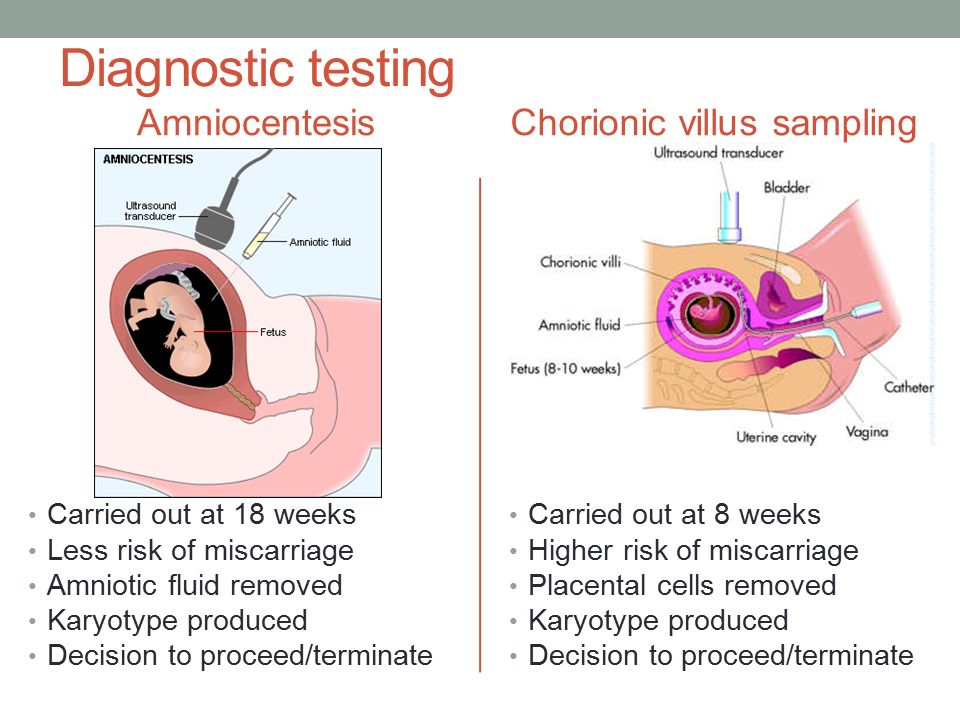
After the miscarriage
You will have some cramping pain and bleeding after the miscarriage, similar to a period. It will gradually get lighter and will usually stop within 2 weeks.
The signs of your pregnancy, such as nausea and tender breasts, will fade in the days after the miscarriage. If you had a late miscarriage, your breasts might produce some milk. You will probably have your next period in 4 to 6 weeks.
Remember, it’ll be normal to feel very emotional and upset at this time.
More information
Read more about miscarriage:
- What is a miscarriage?
- What happens after a miscarriage
- Emotional support after miscarriage
- Fathers and miscarriage
- Experiencing a pregnancy loss
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
KidsHealth (Understanding miscarriage), The Royal Women's Hospital (Treating miscarriage), Pink Elephants Support Network (Sorry for your loss), Women’s and Children’s Health Network (Miscarriage), Patient.com (Miscarriage and bleeding in early pregnancy), Pink Elephants Support Network (Treatments and procedures), New Kids Center (Blood Clots of Miscarriage: What It Looks Like?), Babycenter Australia (Understanding late miscarriage)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: March 2022
Back To Top
Related pages
- Fathers and miscarriage
- Emotional support after miscarriage
- What happens after miscarriage
- Miscarriage
- Experiencing a pregnancy loss
Need more information?
Miscarriage
Miscarriage Despite being common and widespread, miscarriage can be a heartbreaking experience – with up to one in five pregnancies ending before week 20
Read more on Gidget Foundation Australia website
Miscarriage
A miscarriage is the loss of a baby, usually during the first three months or first trimester of pregnancy.
Read more on Pregnancy, Birth & Baby website
Fathers and miscarriage
A miscarriage can be a time of great sadness for the father as well as the mother.
Read more on Pregnancy, Birth & Baby website
Emotional support after miscarriage
It is important to know that there is no right or wrong way to feel after experiencing a miscarriage.
Read more on Pregnancy, Birth & Baby website
What happens after miscarriage
There are a number of things you may need to consider after a miscarriage.
Read more on Pregnancy, Birth & Baby website
Miscarriage | SANDS - MISCARRIAGE STILLBIRTH NEWBORN DEATH SUPPORT
Helping you understand the complex range of emotions you may experience during fertility treatment or after miscarriage or early pregnancy loss
Read more on Sands Australia website
Miscarriage: a guide for men | Raising Children Network
This Dads Guide to Pregnancy covers miscarriage, the grief men might experience after miscarriage, and how to support partners after pregnancy loss.
Read more on raisingchildren.net.au website
The Pink Elephants Support Network - Medical Options for Recurrent Miscarriage
In some cases, a medical reason for miscarriage or recurrent miscarriage can be found through testing
Read more on Pink Elephants Support Network website
New research on vitamin B3 and miscarriages
Pregnant women are being warned not to start taking vitamin B3 supplements, despite a recent study that suggests it might reduce the risk of miscarriages and birth defects.
Read more on Pregnancy, Birth & Baby website
Pregnancy: miscarriage & stillbirth | Raising Children Network
Have you experienced a miscarriage or stillbirth? Find articles and videos about coping with the grief of losing a pregnancy or having a stillbirth.
Read more on raisingchildren.net.au website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.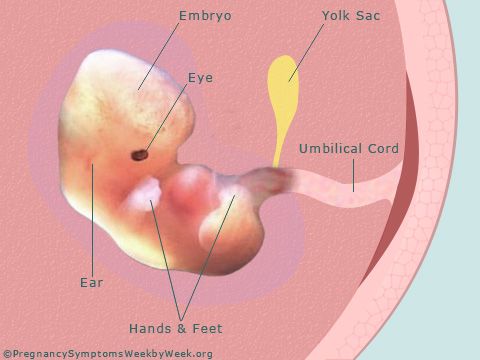
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Blood Clots of Miscarriage: What It Looks Like?
Miscarriage of a baby can be a very traumatic thing. Seeing a miscarriage can be even more traumatic. Miscarriage is defined as losing your baby prior to being 20 weeks or at the 20th week of pregnancy. About 50% of pregnancies result in a miscarriage, but many women do not even know they are pregnant yet and haven’t tested for pregnancy. After a positive pregnancy test, about 15% of those result in miscarriage. Miscarriage blood clot pictures can help you prepare if you have been told that you will probably lose your baby. This article will also help prepare you for what to expect with a miscarriage.
After a positive pregnancy test, about 15% of those result in miscarriage. Miscarriage blood clot pictures can help you prepare if you have been told that you will probably lose your baby. This article will also help prepare you for what to expect with a miscarriage.
Before we take a look at some pictures, it is important to discuss bleeding during pregnancy.
If you have bleeding in early pregnancy, you are likely very nervous. Bleeding can be a very normal thing in the first 12 weeks and usually nothing to worry about. Most often, the pregnancy continues just fine and a healthy live baby is born. However, certain types of bleeding can be a sign of something more serious, especially if it’s heavy or accompanied by cramping.
It can be red like your period or a light brown in color. Spotting is usually normal and often a sign that the pregnancy has implanted in the uterus. This usually happens around the time of your expected period and then stops after a few days.
While a pregnancy can end at any time, these are the points when certain things are most noticeable such asonly seeing clots, seeing the pregnancy sac with an embryo, to seeing a fully formed baby. Please keep in mind these photos may be quite graphic, but are intended to help you prepare yourself.
Please keep in mind these photos may be quite graphic, but are intended to help you prepare yourself.
4-5 Weeks
If you are 4 weeks pregnant, bleeding with clots, you may notice some white or grey tissue in the clots. At this point in pregnancy, you may not see a baby at all if you miscarry. The baby is less than ½ cm long or about the size of a grain of rice.
6 Weeks
You may have bleeding, clots and possibly be able to find a small sac filled with fluid, a very small embryo about the size of your pinky nail and a placenta attached. Some women have even found the umbilical cord at this time, but at six weeks it could still be difficult to find the baby.
Around the eighth week of pregnancy, a lot of women describe the tissue as looking like “liver.” The clots and placenta are dark red and very shiny. You may be able to find the sac and enclosed fetus. Your baby will almost look like a “kidney bean.” There is evidence of eyes that are sealed up and buds forming for arms and legs.
10 Weeks
If you miscarry at ten weeks the clots are darker red in color and are almost like jelly. In the clots, you may notice tissue that looks like membrane and this can be parts of the placenta breaking up. If you pull apart the clots, you will most likely find the gestational sac and you will see a formed baby inside the fluid. The baby now looks more like a baby with fully formed fingers, arms, legs and toes.
12 Weeks
The baby will most likely come out in the sac, but often the water breaks on its own at this point. You may notice after passing clots, you will then pass the baby with the umbilical cord still inside of you. Then the placenta is expelled. At this point in pregnancy, you may even be able to tell if your baby was a girl or a boy.
16 Weeks to 20 Weeks
In the sixteen to twenty week timeframe you may pass very large clots that look like “liver.” They may also be around the baby. You will also pass pieces of tissue that feel like membrane. At this time, you may notice water coming out of your vagina. Around twenty weeks, you most likely will give birth to a fully formed baby about the size of your hand.
At this time, you may notice water coming out of your vagina. Around twenty weeks, you most likely will give birth to a fully formed baby about the size of your hand.
If you notice miscarriage blood clot pictures, place a pad in your underwear. If you soak more than two pads an hour or have severe cramping, contact your doctor immediately or go to your nearest emergency room.
The doctor will take a look at your cervix to see if it is open. They will check your hCG levels to see where you are at in your pregnancy and then repeat the tests to see if the levels go up or down. If they go up your pregnancy is most likely progressing and if the levels drop you are most likely having a miscarriage. You will probably have an ultrasound to check for a heartbeat and make sure the pregnancy is not in your tubes.
If you are at risk for a miscarriage, you will most likely be sent home and told to rest. If the bleeding stops and you have pregnancy symptoms then the pregnancy is more likely to progress. If your pregnancy symptoms go away suddenly and you begin severe cramping and passing clots then the doctor will give you the option of passing the pregnancy at home. Your doctor may have you bring the clots and tissue in for examination.
If your pregnancy symptoms go away suddenly and you begin severe cramping and passing clots then the doctor will give you the option of passing the pregnancy at home. Your doctor may have you bring the clots and tissue in for examination.
“At eight weeks my pregnancy symptoms just disappeared overnight. Then I started to bleed so I called the doctor. They told me to rest, but I started getting really bad cramps and passed some pretty big clots. The bleeding then stopped suddenly. I knew I had miscarried and my periods returned about 6 weeks later. I was able to get pregnant again and had a successful pregnancy the next time around.” --- Kaitlyn
“At around seven weeks I started bleeding and then passed about a two centimeter rubber-like piece of white tissue. I reminded me of a small piece of uncooked chicken. After this passed, a stringy clot about two inches long came out and then nothing else.” ---Julie
After this passed, a stringy clot about two inches long came out and then nothing else.” ---Julie
Spontaneous miscarriage and miscarriage
Over the past 10 years, the number of spontaneous miscarriages has been growing rapidly. The International Histological Classification Organization (FIGO) has declared the situation with an increase in the frequency of miscarriages an epidemic.
Spontaneous miscarriage is the termination of pregnancy before the fetus reaches a viable term (up to 22 weeks of pregnancy and fetal weight 500 g.).
Most miscarriages (about 80%) occur before 12 weeks of gestation. Moreover, in the early stages up to 8 weeks of pregnancy, the cause of miscarriage is chromosomal abnormalities in 50% of cases. It turns out that nature eliminates the defective product of conception.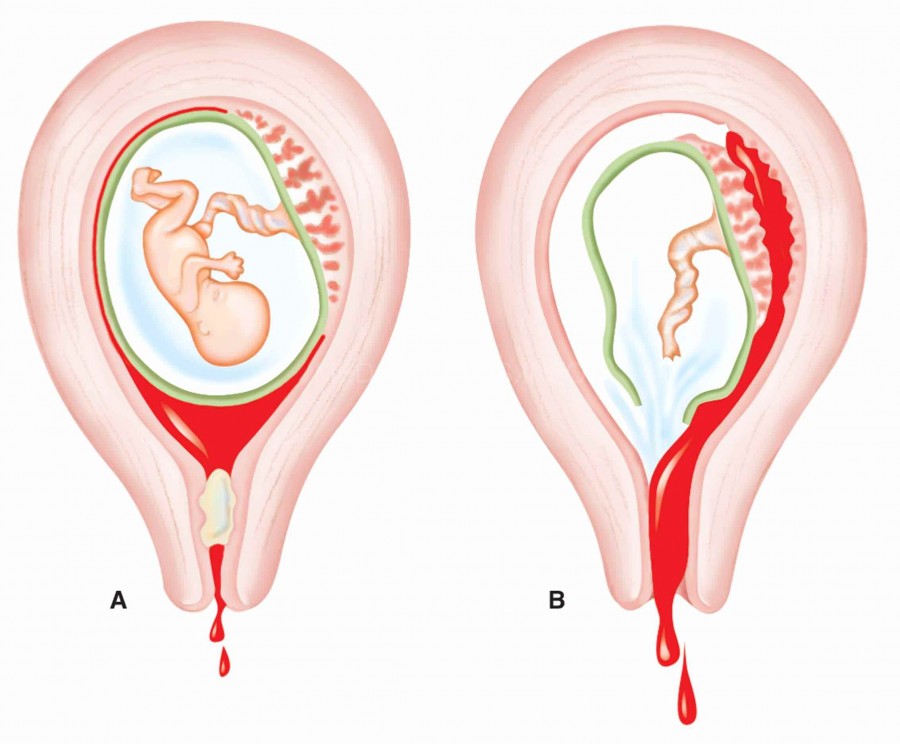 And these causes are difficult to prevent, especially in the presence of hereditary diseases. Fortunately, accidental breakdowns are much more common than genetically determined ones. Therefore, subsequent pregnancies usually end happily. But the remaining 50% of miscarriages have completely real and removable causes. They can be easily identified at the stage of preparation for pregnancy by a gynecologist.
And these causes are difficult to prevent, especially in the presence of hereditary diseases. Fortunately, accidental breakdowns are much more common than genetically determined ones. Therefore, subsequent pregnancies usually end happily. But the remaining 50% of miscarriages have completely real and removable causes. They can be easily identified at the stage of preparation for pregnancy by a gynecologist.
What are the reasons?
- chronic diseases: inflammatory diseases of the uterus and appendages, polycystic ovary syndrome, uterine fibroids, endometriosis, malformations of the genital organs.
- infections: toxoplasmosis, listeriosis, genital tuberculosis, sexual infections - chlamydia, mycoplasma, ureaplasma, syphilis.
- antiphospholipid syndrome.
- endocrine diseases: diabetes, thyroid disease.
- metabolic disorders in the body: obesity, folic acid deficiency, iron deficiency, vitamin D deficiency.
- male factor.
Of course, these causes are identified and eliminated before the planned conception.
There are harmful factors that can affect the development of the fetus in the early stages of pregnancy and lead to miscarriage:
- alcohol consumption.
- caffeine use (4-5 cups of coffee per day).
- smoking (more than 10 cigarettes a day).
- drug use.
- taking medications with a teratogenic effect (for example: aspirin, nise and others from this group of drugs; antifungals; antidepressants; some antibiotics and a number of other drugs).
- toxins and occupational hazards: ionizing radiation, pesticides, inhalation of anesthetic gases.
What are the signs of possible pregnancy loss?
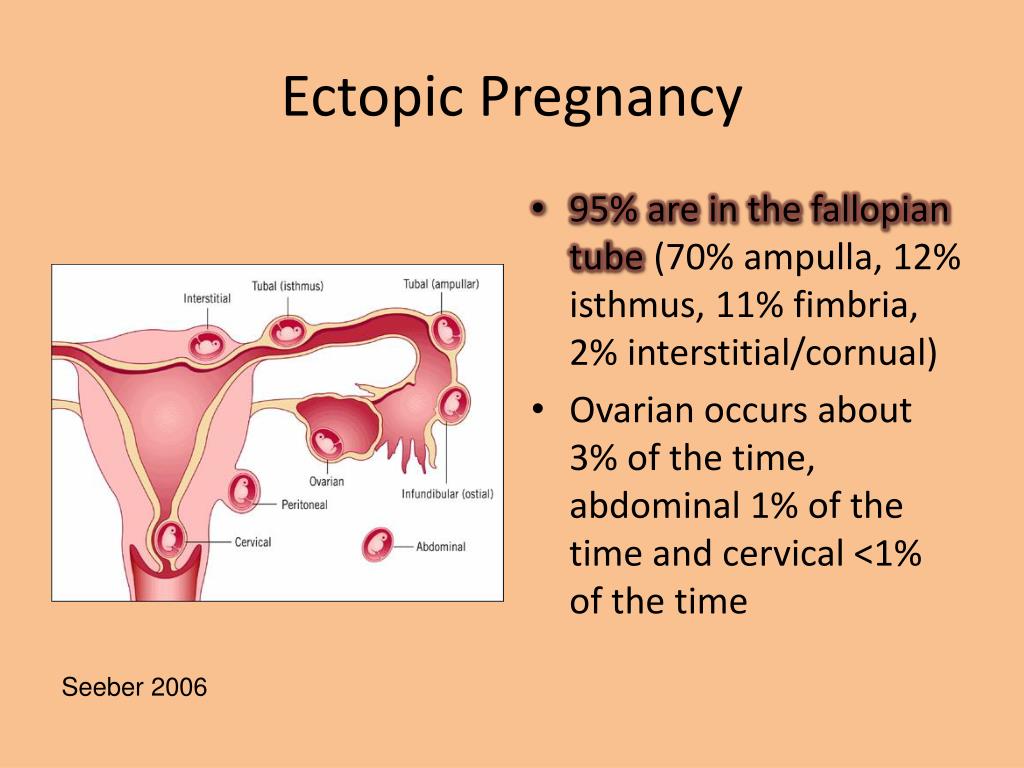
These are complaints of pain in the lower abdomen and lower back, bloody discharge from the genital tract. It is necessary to consult a doctor to rule out an ectopic pregnancy and conduct an additional examination (hCG test, blood test for progesterone, ultrasound).
In early pregnancy, with dubious ultrasound data or suspected non-developing (missing) pregnancy, expectant management is chosen with a repeat examination by a gynecologist, ultrasound, tests after 7-10 days. If a the diagnosis was made and the fact of uterine pregnancy was confirmed, with a threatened miscarriage, preservation therapy is carried out in an outpatient day hospital. A miscarriage that has begun requires hospitalization in the gynecological department. In the case of a non-developing pregnancy, an abortion is performed.
In accordance with the clinical treatment protocol approved by the Ministry of Health of the Russian Federation dated 07.06.2016. Preference is given to drug therapy aimed at terminating pregnancy with prostaglandin analogues (misoprostol) with or without prior use of an antiprogestin (mifepristone). In case of need for surgical treatment (with incomplete miscarriage with infected miscarriage), it is recommended to use aspiration curettage (with an electric vacuum source or a manual vacuum aspirator). What has a significant advantage over curettage of the uterine cavity because it is less traumatic and can be performed on an outpatient basis.
What has a significant advantage over curettage of the uterine cavity because it is less traumatic and can be performed on an outpatient basis.
All women who have had a miscarriage need treatment to prevent complications and prevent recurrent miscarriages. Why is rehabilitation therapy necessary?
According to the decision of the XVIII World Congress of Obstetricians and Gynecologists , the diagnosis of chronic endometritis should be made to absolutely all women who have had an undeveloped pregnancy. Two out of three miscarriages according to Professor V.E. Radzinsky are caused by this disease. When examining the material from the uterine cavity, infectious pathogens were isolated: ureaplasmas, mycoplasmas, streptococci, staphylococci, Escherichia coli, viruses (herpes, HPV). Therefore, it is very important to carry out treatment immediately after the termination of pregnancy.
If time is lost, it is necessary to carry out additional diagnostics: a pipel biopsy of the endometrium with a histological examination and a study for infections, including tuberculosis. Then, taking into account the results obtained, symptomatic anti-inflammatory therapy is carried out (immunomodulators, antibacterial drugs, physiotherapy, gynecological massage, mud therapy). In parallel, an examination is prescribed to identify other causes of miscarriage (male factor, chronic maternal diseases, genital infections, antiphospholipid syndrome).
Then, taking into account the results obtained, symptomatic anti-inflammatory therapy is carried out (immunomodulators, antibacterial drugs, physiotherapy, gynecological massage, mud therapy). In parallel, an examination is prescribed to identify other causes of miscarriage (male factor, chronic maternal diseases, genital infections, antiphospholipid syndrome).
In the medical center "Mifra-Med" at the level of modern requirements of medicine, all the possibilities for a complete adequate examination have been created: all types of tests, ultrasound, hysteroscopy, aspiration biopsy, consultations of narrow specialists (endocrinologist, therapist, neurologist, urologist). Our gynecologists of the highest category Melko O.N., Novitskaya E.L., Tikhonova T.N. and urologist of the highest category Kanaev S.A. have sufficient experience in the rehabilitation and preparation of couples for the next pregnancy with a successful outcome. Treatment is carried out in a day hospital with the use of drugs, physiotherapy, gynecological massage, prostate massage.
WE WILL HELP YOU!
st. Yakovleva, 16 st. Kirova 47 B
tel. 244-744 tel. 46-43-57
What is a miscarriage and why it can happen
###1### What is a miscarriage
First of all, you should define the terms. Miscarriage in gynecological practice is called spontaneous termination of pregnancy in the first 20–22 weeks. Why 20-22 weeks? There is such a consensus: doctors save a fetus born with a mass of 500 grams or more. The chances of saving someone who was born weighing less than 500 grams are zero. At 20–22 weeks, the fetus just usually reaches such a mass.
The frequency of miscarriages is quite high: they end in 15-20% of pregnancies.
That is, for a practicing doctor, this is a fairly common situation, although in the life of each person, of course, this can happen only once or not at all.
Medical statistics, which translate medicine into numbers and make it a more accurate science, show that of these 15-20% of pregnancies that end in miscarriages, 80% or more occur in the first 12 weeks. That is, the longer the gestational age, the less likely it is that a spontaneous miscarriage will occur. Thus, if I, as a doctor, meet a woman who is diagnosed with a threatened miscarriage, give her an ultrasound and see a fetus with a heartbeat, I can immediately tell her that the probability of a miscarriage is no longer 15%, but 5%. If I see a situation where the gestation period is already more than 12 weeks, then the probability is already 2-3%.
That is, the longer the gestational age, the less likely it is that a spontaneous miscarriage will occur. Thus, if I, as a doctor, meet a woman who is diagnosed with a threatened miscarriage, give her an ultrasound and see a fetus with a heartbeat, I can immediately tell her that the probability of a miscarriage is no longer 15%, but 5%. If I see a situation where the gestation period is already more than 12 weeks, then the probability is already 2-3%.
How does a miscarriage happen? Regardless of the reason, the scenario is the same.
First the fetus dies; then detachment from the walls of the uterus begins (then the woman has spotting, which is classified as a “threatening miscarriage”), and then the exfoliated is thrown out of the uterine cavity. The problem is that the same symptoms can be observed in both an ectopic pregnancy and a normal, healthy intrauterine pregnancy. If the ultrasound shows a live intrauterine pregnancy, in most cases the cause of bleeding during pregnancy remains unknown. It is the appearance of bloody discharge against the background of a live intrauterine pregnancy that is designated by doctors as a “threatening miscarriage”. In the vast majority of cases, despite the formidable diagnosis, such a pregnancy is completely safely completed. Of course, any woman passionately wants to know what this bloody discharge is because of, because she thinks: now I will find out what it is because of, I will remove this factor from my life, and everything will be fine, they will stop with me. We have to disappoint a woman: in most cases, we do not know the reason.
It is the appearance of bloody discharge against the background of a live intrauterine pregnancy that is designated by doctors as a “threatening miscarriage”. In the vast majority of cases, despite the formidable diagnosis, such a pregnancy is completely safely completed. Of course, any woman passionately wants to know what this bloody discharge is because of, because she thinks: now I will find out what it is because of, I will remove this factor from my life, and everything will be fine, they will stop with me. We have to disappoint a woman: in most cases, we do not know the reason.
Accidental and habitual miscarriage
All miscarriages are divided into two large types - sporadic (accidental) and habitual. In essence, they are determined by the same range of causes, only the proportion of each of the causes in two cases will be very different. In turn, all causes can be divided into two large groups: internal causes caused by fetal problems, and external causes caused by problems in the mother's body. Accordingly, sporadic miscarriages are most often determined by causes associated with the fetus, and habitual miscarriages are determined by the mother's body.
Accordingly, sporadic miscarriages are most often determined by causes associated with the fetus, and habitual miscarriages are determined by the mother's body.
Medical statistics show that more than half of sporadic miscarriages in the first 12 weeks are due to genetic disorders in the fetus.
Moreover, the shorter the gestational age, the higher the likelihood that the cause was a genetic disorder in the fetus. These are generalized data from numerous studies, mostly Western ones. Let's look at this most common reason first. The fact is that no matter how kings of nature we think we are, the same laws of nature apply to us as to an ant, an insect, a blade of grass.
Nobody canceled these biological laws: the best and the strongest survive in the good sense of the word, in the biological sense.
A biological individual cannot always produce 100% quality cells (in this case we are talking about germ cells). So, 1 ml of a man's sperm contains on average 20 million spermatozoa, and normally about 10% of them, that is, 2 million, are pathological forms.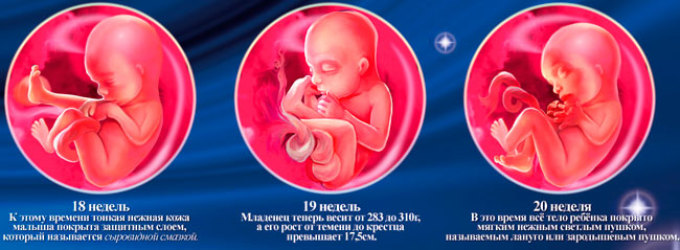 And such a spermogram will be considered normal. In a woman, too, poor-quality eggs can mature, and the older we get, the more likely it is that a poor-quality egg will mature. It's not because we're deliberately doing something wrong - lifting something heavy, drinking an extra cup of coffee, overworking at home/work. Unlike spermatozoa, which are constantly renewed, all the eggs of a future woman are laid at the moment when her mother is at the 20th week of pregnancy.
And such a spermogram will be considered normal. In a woman, too, poor-quality eggs can mature, and the older we get, the more likely it is that a poor-quality egg will mature. It's not because we're deliberately doing something wrong - lifting something heavy, drinking an extra cup of coffee, overworking at home/work. Unlike spermatozoa, which are constantly renewed, all the eggs of a future woman are laid at the moment when her mother is at the 20th week of pregnancy.
And new eggs are never laid again, they are only used up, only lost throughout the life of a girl/woman.
That is, if you are 35 years old, then the egg that came out of your ovary this month has been lying in the ovary waiting for its turn to ovulate for more than 35 years. Therefore, of course, in a 20-year-old woman and in a 40-year-old woman, not only the quantity, but also the quality of the eggs will be different. Because everything unfavorable that is around us in terms of nutrition, environment, air and water affects the first only 20 years, and the second - already 40.
The dependence of the frequency of spontaneous miscarriage due to genetic disorders in the fetus on the age of the eggs (and, consequently, on the age of the woman) was shown thanks to the introduction of in vitro fertilization technology - IVF. A very good study was conducted on a group of patients over 40 who underwent IVF. Half of them were implanted with their own fertilized eggs, and the other half - donor eggs taken from women under 25 years old. In the group that carried embryos from donor eggs, the miscarriage rate corresponded to that of women under 25 years of age and was three to four times lower than in the group that was implanted with embryos obtained from their 40-year-old eggs. Thus, the probability of miscarriages and genetic disorders of the fetus is determined by the biological age of the woman. It's the kind of thing we can't reverse in any way, and it should be taken into account when a pregnancy is postponed to a later date.
Thus, if a defective egg meets a normal sperm or vice versa, then the resulting pregnancy with a poor-quality embryo is rejected at a certain stage and a miscarriage occurs.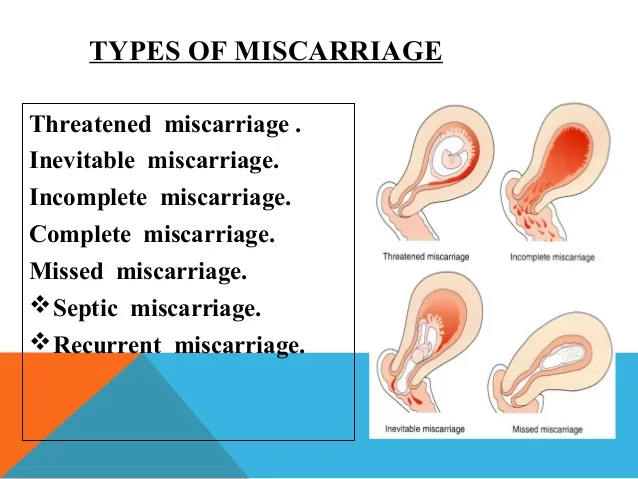
And here comes the most interesting thing, because we still don't know which mechanism in the body recognizes that the pregnancy is of poor quality. But this mechanism exists, and it works very well, otherwise all abnormal pregnancies would lead to the birth of not quite healthy or completely unhealthy people, and humanity would have already degenerated. We do not know this mechanism, but we can say: if a woman has a spontaneous miscarriage, then these mechanisms work for her and from a biological point of view she is healthy. It is much worse if we see a different situation (although it is quite rare): far beyond the 20-week period, we do an ultrasound and find severe defects in the fetus. Because of these defects, after birth, he may either be disabled or not be able to survive at all, but now he lives inside the uterus, which suggests that the mechanisms that recognize healthy and unhealthy pregnancy did not work in this woman.
Therefore, with all the emotional and psychological disadvantages that a spontaneous miscarriage brings for a woman, there is a big plus in this event, which is not obvious to the patient.
This is a universal biological mechanism that allows you to keep us and our offspring healthy and prevents the birth of a handicapped child.
If the majority of spontaneous miscarriages are caused by genetic disorders, the question arises which pregnancies should then be saved. Unfortunately, any gynecologist has encountered cases in his practice when attempts to “pull out” a pregnancy with incredible efforts lead to a deplorable result. That is, the pregnancy threatened to terminate, the woman was given numerous medications, and she persisted, but after the 20th week it turned out that the fetus had serious developmental disorders. It should be said separately about medicines. Serious Western studies (there is such a term as "double-blind placebo-controlled study", it guarantees the quality and statistical significance of the results as much as possible) show that there is not a single medication, except for progesterone, a female hormone that can affect pregnancy.
If a pregnancy is doomed to death, it will die; if it should survive, it will survive, unless, of course, we are talking about a healthy woman who has biological mechanisms currently unknown to us for culling poor-quality pregnancies.
We, in Russia, have a different practice, caused not by scientific objective data, but rather by cultural differences - the fact that our medicine has been isolated from the world community for a long time.
The second most common cause of miscarriage is infection. This is the same failure. Severe flu is an obvious reason for sporadic miscarriage. Pregnancy does not destroy the disease, but its consequence - the general poor condition of the woman's body, the environment that ensures the life of the fetus. Unlike genetic reasons, when the embryo was laid "bad", in the case of infection, the embryo was laid healthy and of high quality. But suddenly the woman fell ill with a severe flu - a temperature of 40, vomiting, dehydration. It is difficult for a tiny creature to survive in such adverse conditions, and it dies. The death of the embryo is due to environmental disturbances - high temperature, dehydration, intoxication.
If a second miscarriage occurs, it is difficult to attribute it to the flu: it is hard to believe that a woman gets the same severe flu from year to year at the same time. Here it is - the difference between sporadic and habitual miscarriage.
Here it is - the difference between sporadic and habitual miscarriage.
The first happens really by chance - it's a classic "failure". The second is a pattern: when we see a woman with a habitual miscarriage, she, as a rule, has an interruption at about the same time. Then we assume that there is a reason that does not exist very clearly in the body: it does not prevent a woman from living outside the state of pregnancy, but it makes itself felt when a normal pregnancy occurs. This reason, which does not exist very noticeably in a woman's body, prevents her from carrying a pregnancy to term. It leads to the fact that normal conditions for the survival of a healthy fetus are not created, and it dies, and this happens from time to time. This is the fundamental difference between a habitual miscarriage and a sporadic one. In this case, we will conduct a series of studies (quite expensive) to find out what the reason is.
Today, there is a consensus in the world scientific community that recurrent miscarriage is considered a case when a woman has two miscarriages in a row. If a woman had one miscarriage and she comes to me and asks what is the probability that this will happen again, these are the same 15-20%. If this situation occurred twice in a row, then the probability that this will happen again is already about 30–35%, and if three times in a row, it is almost 40%.
If a woman had one miscarriage and she comes to me and asks what is the probability that this will happen again, these are the same 15-20%. If this situation occurred twice in a row, then the probability that this will happen again is already about 30–35%, and if three times in a row, it is almost 40%.
In about 2% of couples, wives suffer from recurrent miscarriage.
If in the case of sporadic miscarriages, the fetus and its disorders are most often “to blame”, then in case of habitual miscarriages, its environment, the woman’s body, is usually “to blame”. As with sporadic miscarriages, genetics can be the cause. But if in sporadic miscarriage genetics is the cause of 70–80% (up to 6 weeks in general 90%) of all interruptions, then in the case of habitual miscarriage, genetic disorders are found only in 2–3% of patients. The same is true for infections: in a recurrent miscarriage, the likelihood that repeated abortions are due to infection is no more than 1%.
Hormonal imbalances in a woman's body, on the other hand, are more likely to cause habitual miscarriage than accidental miscarriage.
Disturbances in the structure of the uterus - a septum inside the uterus, a bicornuate uterus, the presence of synechia (the so-called adhesions inside the uterus) - these are all things that can also lead to repeated miscarriages.
Approximately 40% of women diagnosed with "recurrent miscarriage" are found to have various immune disorders that cause the fetus to be rejected by the mother's body. Immune disorders are divided into autoimmune and alloimmune. Autoimmune disorders are situations where a woman's immune system works against its own genes, proteins. One of the most common diseases of this kind among women with recurrent miscarriage is antiphospholipid syndrome. Phospholipids are the "glue" that holds cells together. A woman with antiphospholipid syndrome produces factors (antibodies) against her own phospholipids, which are abundant in the placenta. As a result of the syndrome, blood clots form in the small vessels of the placenta, which disrupt blood circulation, and therefore disrupt the function of the placenta to deliver nutrients to the fetus. Pregnancy under such conditions cannot “stretch” for a long time - sooner or later, the death of a healthy embryo / fetus occurs. Women suffering from antiphospholipid syndrome carry a pregnancy in no more than 10% of cases. Its treatment allows you to reverse the statistics - gestation occurs as early as 90% of cases. A woman is given drugs that thin the blood and prevent the formation of blood clots - the placenta performs its function, and the pregnancy is carried.
Pregnancy under such conditions cannot “stretch” for a long time - sooner or later, the death of a healthy embryo / fetus occurs. Women suffering from antiphospholipid syndrome carry a pregnancy in no more than 10% of cases. Its treatment allows you to reverse the statistics - gestation occurs as early as 90% of cases. A woman is given drugs that thin the blood and prevent the formation of blood clots - the placenta performs its function, and the pregnancy is carried.
Alloimmune causes are aggressive factors directed against foreign proteins, that is, the paternal part of the fetal genome. In general, our immune system is required to produce antibodies and get rid of any foreign and pathologically altered cells. Why a pregnancy consisting of 50% of "foreign" genes is not rejected (not to mention 100% of genetic foreignness when a surrogate mother carries a "foreign" embryo in the IVF program) is not yet entirely clear. By the way, scientists believe that when it is found out what is the mechanism that prevents the rejection of pregnancy cells with "foreign genes", this can help in the development of a cure for cancer.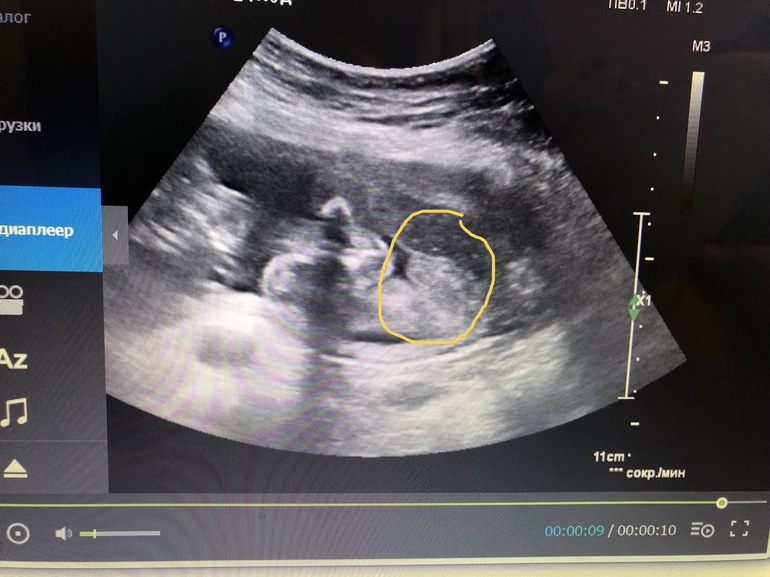 After all, cancer consists of pathologically altered cells, which, for some reason, are also not rejected, not destroyed by the immune system. One way or another, during pregnancy, a woman in relation to foreign genes / proteins of the placenta and fetus develops a condition called immunological tolerance - “we do not notice and do not attack strangers”. In the case of a habitual miscarriage, this tolerance does not exist: the mother's immune system recognizes foreign genes and proteins of pregnancy, attacks them, and thereby leads to repeated miscarriages.
After all, cancer consists of pathologically altered cells, which, for some reason, are also not rejected, not destroyed by the immune system. One way or another, during pregnancy, a woman in relation to foreign genes / proteins of the placenta and fetus develops a condition called immunological tolerance - “we do not notice and do not attack strangers”. In the case of a habitual miscarriage, this tolerance does not exist: the mother's immune system recognizes foreign genes and proteins of pregnancy, attacks them, and thereby leads to repeated miscarriages.
Quite often, in about 40% of all cases, after conducting the necessary examination of both spouses, we, unfortunately, do not find any reasons explaining why this couple has repeated miscarriages.
There is such a term as "unexplained recurrent miscarriage", as well as "unexplained infertility". Maybe in five years, medicine will find something new in this area, new explanations, but so far this has not happened. This is a psychologically difficult moment for both the doctor and the patients.
Two worlds, two approaches
When a woman is threatened with a miscarriage, the actions of a doctor in Russia and abroad will be fundamentally different, and this is due not so much to different scientific data as to cultural differences that have arisen during the isolation of our medical school. Abroad, such women are simply sent home: they are "prescribed" bed rest, a general clinical examination, and sexual rest. Time will tell how this situation will end: either the pregnancy will continue, or a miscarriage will occur if it was of poor quality, and it’s good that it was “rejected” by the body.
In Russia, the psychological attitude of the population towards medicine is slightly different and medicine is slightly different.
In our country, a threatened miscarriage is an indispensable indication for hospitalization: there, the patient is prescribed "no-shpu", drugs that relax the uterus, hemostatic drugs. This is not a matter of biological or medical differences - it is a matter of psychology for most of our population: if a doctor did not give a pill, then he did not seek to help.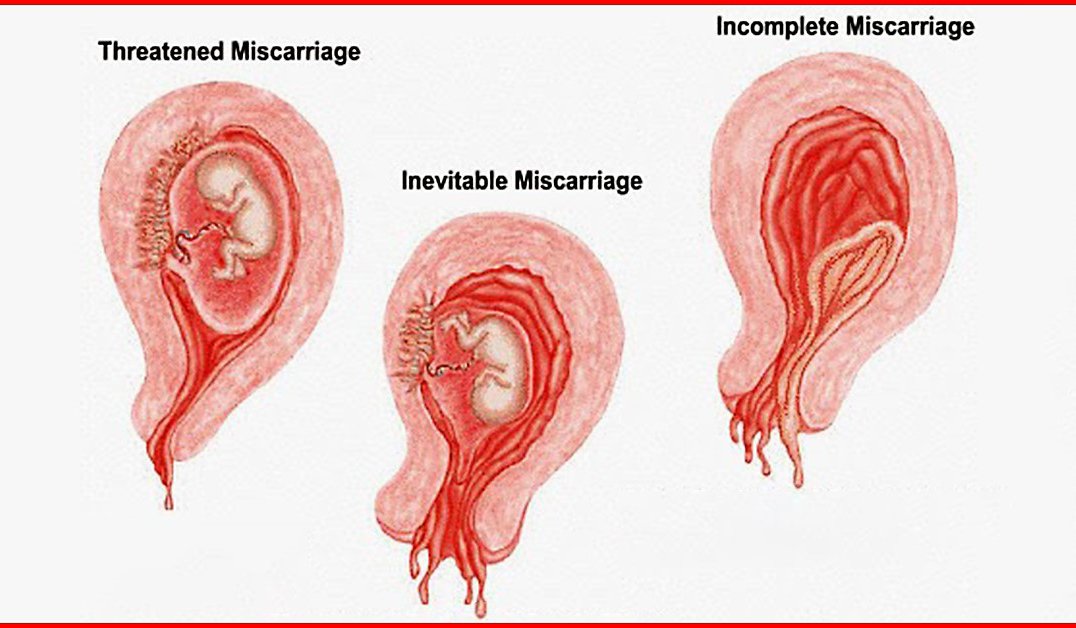 And it is quite difficult to convey to people that the laws of nature apply here - you cannot influence them. According to our Russian protocol, I have no right not to offer hospitalization in case of a threatened miscarriage. However, scientific medical facts clearly show that hospitalization does not fundamentally change anything in the prognosis: the likelihood of spontaneous miscarriage does not decrease from this. Western studies show that there are no medications that can cure sporadic miscarriage. If the pregnancy persists, then it is nature that preserves the pregnancy, not the cure. There are such medicines for a habitual miscarriage: if it was possible to identify the cause of repeated abortions, it can be influenced. This treatment is prescribed either before the onset of pregnancy, or in the early stages of pregnancy, before any symptoms of threatened miscarriage appear.
And it is quite difficult to convey to people that the laws of nature apply here - you cannot influence them. According to our Russian protocol, I have no right not to offer hospitalization in case of a threatened miscarriage. However, scientific medical facts clearly show that hospitalization does not fundamentally change anything in the prognosis: the likelihood of spontaneous miscarriage does not decrease from this. Western studies show that there are no medications that can cure sporadic miscarriage. If the pregnancy persists, then it is nature that preserves the pregnancy, not the cure. There are such medicines for a habitual miscarriage: if it was possible to identify the cause of repeated abortions, it can be influenced. This treatment is prescribed either before the onset of pregnancy, or in the early stages of pregnancy, before any symptoms of threatened miscarriage appear.
After the first miscarriage, we examine the woman, but this is the usual list of studies that are needed before any pregnancy.