10 weeks premature babies
Premature baby | Pregnancy Birth and Baby
Premature baby | Pregnancy Birth and Baby beginning of content10-minute read
Listen
What is a premature baby?
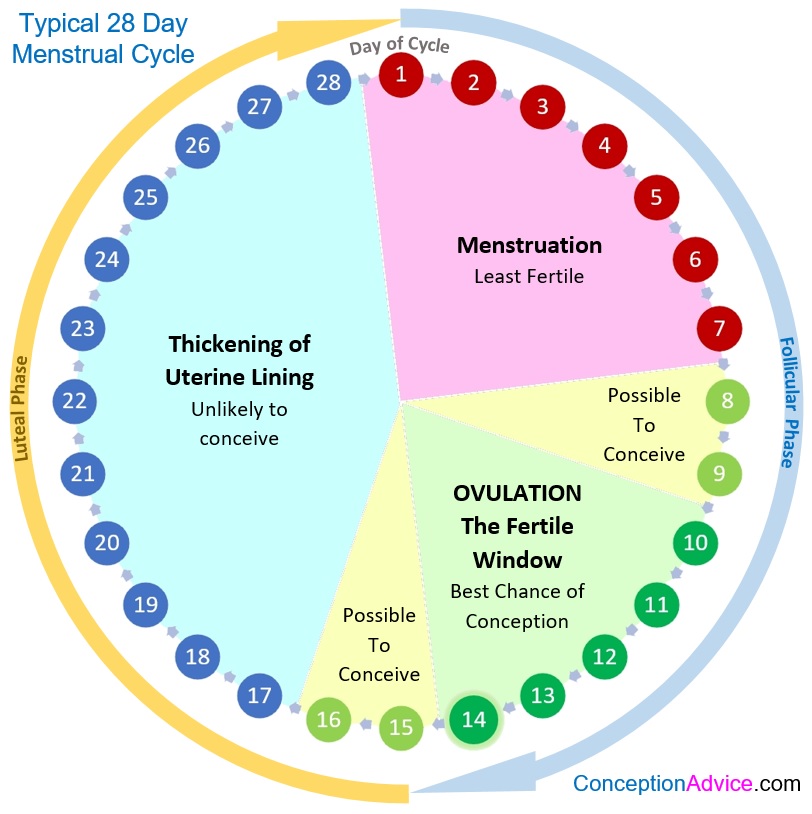
Most pregnancies last 40 weeks. A baby born before the 37th week is known as a premature or pre-term baby. Medical advances have meant that more than 9 out of 10 premature babies survive, and most go on to develop normally.
In Australia, almost 1 in every 10 babies is born prematurely. Most Australian premature babies are born between 32 and 36 weeks and don't have any serious long-term problems.
Very premature babies are at a higher risk of developmental problems. It is possible for babies born at 23 to 24 weeks to survive, but it is risky.
Most babies born before 32 weeks, and those weighing 2. 5 kg or less, may need help breathing and may be cared for in a neonatal intensive care unit (NICU) until they have developed enough to survive on their own. Babies born between 32 and 37 weeks may need care in a special care nursery (SCN)
Why are babies born prematurely?
The cause of premature birth is unknown in about half of all cases. However, some of the reasons babies are born prematurely include:
- problems with the cervix, when it is too weak to hold the weight of the baby and uterus so it starts to open prematurely (called cervical incompetence)
- multiple pregnancy (twins or more)
- the mother gets an infection
- the mother has a medical condition that means the baby must be delivered early, such as pre-eclampsia
- problems with the placenta such as placental insufficiency, placenta praevia, placenta accreta or placental abruption
- preterm premature rupture of membranes, when the amniotic sac spontaneously ruptures
- the mother has a health condition like diabetes
- a history of premature birth
If you are less than 37 weeks pregnant and you experience any of the signs of premature labour, such as contractions, your waters breaking, bleeding, a 'show' of mucus from your vagina or a sudden decrease in your baby's movements, contact your doctor or nearest delivery suite immediately. It may be possible to slow down or stop the labour. But each day the baby stays inside your womb, the greater their chance of survival.
It may be possible to slow down or stop the labour. But each day the baby stays inside your womb, the greater their chance of survival.
In most cases labour starts by itself, and the signs will usually be the same as labour that starts at full term.
The signs of premature labour include:
- pressure in the pelvis, as if the baby is pushing down
- cramping in the lower part of the belly
- diarrhoea, nausea or vomiting
- constant lower back pain
- a change in your vaginal discharge, or more discharge than normal
- mucous, blood or fluid leaking from your vagina
- waters breaking
- regular contractions, or contractions that come more than 4 times an hour
- baby’s movements slowing down or stopping
Find out more about the signs of labour and what happens.
What should I do if I experience the signs of premature labour?
If you have any of the signs listed above, contact your midwife or doctor straight away. If you are going to have your baby early, it’s important to get help as soon as possible.
If you are going to have your baby early, it’s important to get help as soon as possible.
You should also contact your midwife or doctor if you experience swelling in your face, hands or feet, or double vision, blurred vision or other eye disturbances. These are signs of pre-eclampsia, which is a common cause of pre-term deliveries.
If you go into labour prematurely, you will need to be treated in a hospital that has facilities for the newborn, such as a neonatal intensive care unit (NICU) or special care nursery (SCN).
You can find your nearest suitable hospital on the Miracle Babies Foundation website.
How is a premature labour managed?
At the hospital, you will probably have a pelvic examination or an ultrasound. The medical team will check whether your cervix has started to open for labour and monitor the baby.
It is best for very premature babies to be born at a hospital that has an NICU. If the hospital where the baby is born does not have an NICU, you and your baby may be transferred to another hospital.
When you are in labour, you may be given medicines to stop the contractions for a while. This allows you to be transferred to another hospital if necessary. You may also receive injections of corticosteroids 12 to 24 hours before the birth. Steroids will reduce the risk of the baby suffering from the complications of being born very early (particularly breathing difficulties and bleeding).
Premature babies can be born very quickly. They will usually be born through the vagina. However, in some cases the doctor may decide it is safest to deliver the baby via caesarean. Your doctor will discuss this decision with you.
A medical team from the neonatal (newborn) unit will be there for the birth. As soon as your baby is born, they will care for the baby in your room, possibly using a neonatal (baby) resuscitation bed. The team will keep your baby warm and help them to breathe with an oxygen mask or breathing tube, and possibly medicine. Some babies need help to keep their heart beating with cardio-pulmonary resuscitation (CPR) or an injection of adrenalin.
Once your baby is stable, they may be transferred to the NICU or SCN.
Will I be able to hold my baby?
How soon you are able to hold your baby will depend on their medical condition. You may be able to hold them on the day they are born, but you might need to wait a few days or weeks until they are stable enough.
Holding you baby, known as kangaroo care, is important part of your baby’s health and wellbeing, and the maternity staff will support you as soon as you are able.
Will I be able to feed my baby?
After your baby is born, you’ll be asked to start expressing breastmilk. Maternity staff, lactation consultants and Australian Breastfeeding Association counsellors will help you. Breastmilk is full of antibodies and nutrients that will be very important for your baby’s health and growth.
What will my premature baby look like?
Babies born at 36 to 37 weeks usually look like small full-term babies. Very premature babies will be small (perhaps fitting in your hand) and look very fragile.
- Skin: it might not be fully developed, and may appear shiny, translucent, dry or flaky. The baby may not have any fat under the skin to keep them warm.
- Eyes: the eyelids of very premature babies may be fused shut at first. By 30 weeks they should be able to respond to different sights.
- Immature development: your baby might not be able to regulate its body temperature, breathing or heart rate. They may twitch, become stiff or limp or be unable to stay alert.
- Hair: your baby may have little hair on its head, but lots of soft body hair (called 'lanugo').
- Genitals: the baby's genitals may be small and underdeveloped.
Will my premature baby's development be delayed?
Some common issues for premature babies include:
- breathing problems
- heart problems
- problems in their digestive tract
- jaundice
- anaemia
- infections
Most premature babies will develop normally, but they are at higher risk of developmental problems so will need regular health and development checks at the hospital or with a paediatrician. If you are worried about your child's development, talk to your doctor.
If you are worried about your child's development, talk to your doctor.
Problems that may occur later in children who were born prematurely include:
- language delays
- growth and movement problems
- problems with teeth
- problems with vision or hearing
- thinking and learning difficulties
- social and emotional problems
How do I calculate my baby's correct age?
When you're judging whether your premature baby is developing normally, it is important to understand their 'corrected age'.
The corrected age is your baby's chronological age minus the number of weeks or months they were born early. For example, a 6-month-old baby who was born 2 months early would have a corrected age of 4 months. That means they may only be doing the things that other 4-month-olds do. Most paediatricians recommend correcting age when assessing growth and development until your child is 2 years old.
When will my baby be able to come home?
The hospital will not send your baby home until they are confident both the baby and you are ready. Staff will make sure you understand how to care for your baby at home. They will also show you how to use any equipment you may need.
Staff will make sure you understand how to care for your baby at home. They will also show you how to use any equipment you may need.
You will need appointments to see a neonatologist (newborn baby doctor) or paediatrician. Your local child health nurse will also see you regularly.
It is normal to feel a little worried when you are looking after your baby yourself after so long in hospital. Take it slowly in a calm and quiet environment until you both get used to being at home.
Who can I talk to for advice and support?
If you need support, contact the Miracle Babies Foundation's 24-hour support line on 1300 622 243.
The Australian Breastfeeding Association can provide advice and support on feeding your baby on 1800 686 268.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Australian Institute of Health and Welfare (AIHW) (Mothers and babies), Raising Children Network (Premature labour, birth and babies), Raising Children Network (Your premature baby's appearance), Raising Children Network (Premature baby development concerns), Raising Children Network (Going home with your premature baby), Women’s and Children’s Health Network (Premature babies), NSW Pregnancy and Newborn Services Network (Birth before 32 weeks), Miracle Babies (What is prematurity?), Miracle Babies (Treatment of preterm labour), Queensland Government (Queensland Clinical Guidelines; Preterm labour and birth)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: March 2020
Back To Top
Related pages
- Neonatal intensive care unit (NICU)
- Special care nursery (SCN)
- What is kangaroo care?
Need more information?
Premature birth & premature babies | Raising Children Network
This essential guide for parents of premature babies covers gestational age, premature birth risk factors, premature labour and premature development.
Read more on raisingchildren.net.au website
Premature babies and birth | Raising Children Network
Premature babies are born before 37 weeks of pregnancy. Our essential guide covers premature birth, babies, development, NICU and more.
Read more on raisingchildren. net.au website
net.au website
Dads: premature birth and premature babies | Raising Children Network
After a premature birth, it can be hard for dads. Our dads guide to premature babies and birth covers feelings, bonding, and getting involved with your baby.
Read more on raisingchildren.net.au website
Premature birth: questions & checklist | Raising Children Network
Our checklist has answers to questions about premature birth and labour, covering where and how premature babies are born, and things to ask medical staff.
Read more on raisingchildren.net.au website
Bonding with premature babies in the NICU | Raising Children Network
For parents with premature babies in the NICU, bonding might seem hard. This guide explains how to use touch, song, play and daily care to bond with baby.
This guide explains how to use touch, song, play and daily care to bond with baby.
Read more on raisingchildren.net.au website
Premature birth: coping with your feelings | Raising Children Network
After a premature birth and while caring for a premature baby, it’s normal to have powerful and mixed feelings. Here’s how to cope with your feelings.
Read more on raisingchildren.net.au website
Breastfeeding your premature baby | Australian Breastfeeding Association
This article is based on our booklet 'Breastfeeding Your Premature Baby'. The booklet contains valuable information from research on breastfeeding premature infants, as well as experiences of other parents of premature babies to inform, reassure and encourage you. If your baby has been, or is about to be born prematurely, we recommend that you purchase the booklet, which will provide much more information to help you deal with the challenges of breastfeeding and parenting your baby.
Read more on Australian Breastfeeding Association website
NICU: sleep & noise for premature babies | Raising Children Network
Noise in the neonatal intensive care unit (NICU) can affect how premature babies sleep. Here’s how you and staff can help your premature baby sleep better.
Read more on raisingchildren.net.au website
Sleeping - Miracle Babies
A premature baby’s success at sleeping is vitally important to their health and growth
Read more on Miracle Babies Foundation website
What is Prematurity? - Miracle Babies
Prematurity is the term used to describe when a baby is born early
Read more on Miracle Babies Foundation website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.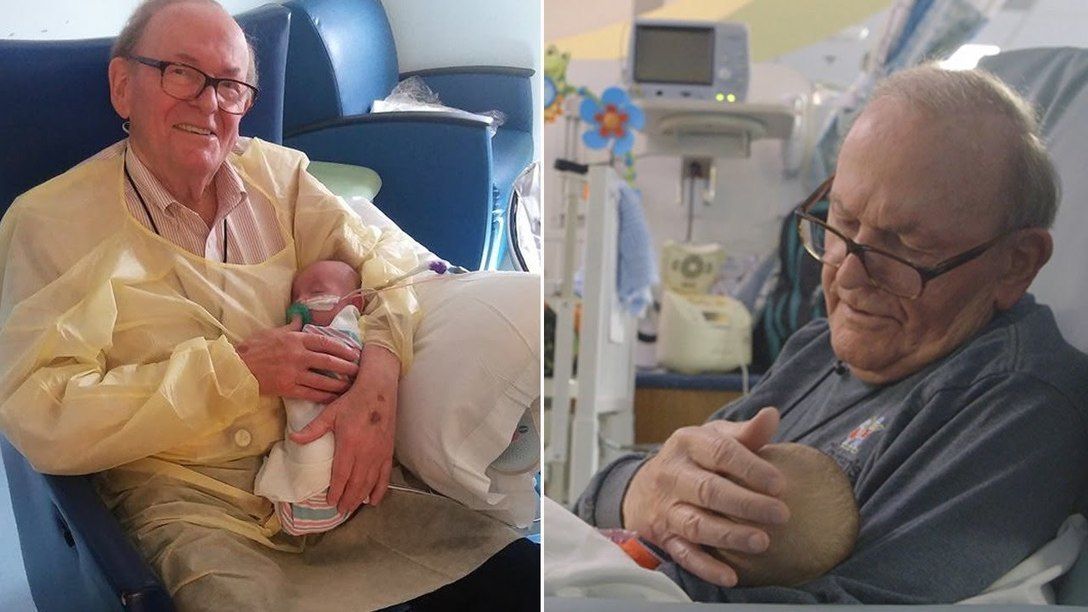
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
the long-term impacts of being born extremely early
Scientists are watching out for the health of adults born extremely premature, such as these people who took part in a photography project.Credit: Red Méthot
They told Marcelle Girard her baby was dead.
Back in 1992, Girard, a dentist in Gatineau, Canada, was 26 weeks pregnant and on her honeymoon in the Dominican Republic.
When she started bleeding, physicians at the local clinic assumed the baby had died. But Girard and her husband felt a kick. Only then did the doctors check for a fetal heartbeat and realize the baby was alive.
The couple was medically evacuated by air to Montreal, Canada, then taken to the Sainte-Justine University Hospital Center. Five hours later, Camille Girard-Bock was born, weighing just 920 grams (2 pounds).
Five hours later, Camille Girard-Bock was born, weighing just 920 grams (2 pounds).
Babies born so early are fragile and underdeveloped. Their lungs are particularly delicate: the organs lack the slippery substance, called surfactant, that prevents the airways from collapsing upon exhalation. Fortunately for Girard and her family, Sainte-Justine had recently started giving surfactant, a new treatment at the time, to premature babies.
After three months of intensive care, Girard took her baby home.
Today, Camille Girard-Bock is 27 years old and studying for a PhD in biomedical sciences at the University of Montreal. Working with researchers at Sainte-Justine, she’s addressing the long-term consequences of being born extremely premature — defined, variously, as less than 25–28 weeks in gestational age.
Families often assume they will have grasped the major issues arising from a premature birth once the child reaches school age, by which time any neurodevelopmental problems will have appeared, Girard-Bock says. But that’s not necessarily the case. Her PhD advisers have found that young adults of this population exhibit risk factors for cardiovascular disease — and it may be that more chronic health conditions will show up with time.
But that’s not necessarily the case. Her PhD advisers have found that young adults of this population exhibit risk factors for cardiovascular disease — and it may be that more chronic health conditions will show up with time.
Camille Girard-Bock, born at 26 weeks of gestation, is now studying the effects of prematurity for a PhD.Credit: Red Méthot
Girard-Bock doesn’t let these risks preoccupy her. “As a survivor of preterm birth, you beat so many odds,” she says. “I guess I have some kind of sense that I’m going to beat those odds also.”
She and other against-the-odds babies are part of a population which is larger now than at any time in history: young adults who are survivors of extreme prematurity. For the first time, researchers can start to understand the long-term consequences of being born so early. Results are pouring out of cohort studies that have been tracking kids since birth, providing data on possible long-term outcomes; other studies are trialling ways to minimize the consequences for health.
These data can help parents make difficult decisions about whether to keep fighting for a baby’s survival. Although many extremely premature infants grow up to lead healthy lives, disability is still a major concern, particularly cognitive deficits and cerebral palsy.
Researchers are working on novel interventions to boost survival and reduce disability in extremely premature newborns. Several compounds aimed at improving lung, brain and eye function are in clinical trials, and researchers are exploring parent-support programmes, too.
Researchers are also investigating ways to help adults who were born extremely prematurely to cope with some of the long-term health impacts they might face: trialling exercise regimes to minimize the newly identified risk of cardiovascular disease, for example.
“We are really at the stage of seeing this cohort becoming older,” says neonatologist Jeanie Cheong at the Royal Women’s Hospital in Melbourne, Australia. Cheong is the director of the Victorian Infant Collaborative Study (VICS), which has been following survivors for four decades. “This is an exciting time for us to really make a difference to their health.”
“This is an exciting time for us to really make a difference to their health.”
The late twentieth century brought huge changes to neonatal medicine. Lex Doyle, a paediatrician and previous director of VICS, recalls that when he started caring for preterm infants in 1975, very few survived if they were born at under 1,000 grams — a birthweight that corresponds to about 28 weeks’ gestation. The introduction of ventilators, in the 1970s in Australia, helped, but also caused lung injuries, says Doyle, now associate director of research at the Royal Women’s Hospital. In the following decades, doctors began to give corticosteroids to mothers due to deliver early, to help mature the baby’s lungs just before birth. But the biggest difference to survival came in the early 1990s, with surfactant treatment.
“I remember when it arrived,” says Anne Monique Nuyt, a neonatologist at Sainte-Justine and one of Girard-Bock’s advisers. “It was a miracle.” Risk of death for premature infants dropped to 60–73% of what it was before1,2.
Marcelle Girard looks in at baby Camille, born weighing just 920 grams (2 pounds).Credit: Camille Girard-Bock
Today, many hospitals regularly treat, and often save, babies born as early as 22–24 weeks. Survival rates vary depending on location and the kinds of interventions a hospital is able to provide. In the United Kingdom, for example, among babies who are alive at birth and receiving care, 35% born at 22 weeks survive, 38% at 23 weeks, and 60% at 24 weeks3.
For babies who survive, the earlier they are born, the higher the risk of complications or ongoing disability (see ‘The effects of being early’). There is a long list of potential problems — including asthma, anxiety, autism spectrum disorder, cerebral palsy, epilepsy and cognitive impairment — and about one-third of children born extremely prematurely have one condition on the list, says Mike O’Shea, a neonatologist at the University of North Carolina School of Medicine in Chapel Hill, who co-runs a study tracking children born between 2002 and 2004. In this cohort, another one-third have multiple disabilities, he says, and the rest have none.
In this cohort, another one-third have multiple disabilities, he says, and the rest have none.
“Preterm birth should be thought of as a chronic condition that requires long-term follow-up,” says Casey Crump, a family physician and epidemiologist at the Icahn School of Medicine at Mount Sinai in New York, who notes that when these babies become older children or adults, they don’t usually get special medical attention. “Doctors are not used to seeing them, but they increasingly will.”
Outlooks for earliesWhat should doctors expect? For a report in the Journal of the American Medical Association last year4, Crump and his colleagues scraped data from the Swedish birth registry. They looked at more than 2.5 million people born from 1973 to 1997, and checked their records for health issues up until the end of 2015.
Source: Ref. 4
Of the 5,391 people born extremely preterm, 78% had at least one condition that manifested in adolescence or early adulthood, such as a psychiatric disorder, compared with 37% of those born full-term. When the researchers looked at predictors of early mortality, such as heart disease, 68% of people born extremely prematurely had at least one such predictor, compared with 18% for full-term births — although these data include people born before surfactant and corticosteroid use were widespread, so it’s unclear if these data reflect outcomes for babies born today. Researchers have found similar trends in a UK cohort study of extremely premature births. In results published earlier this year5, the EPICure study team, led by neonatologist Neil Marlow at University College London, found that 60% of 19-year-olds who were extremely premature were impaired in at least one neuropsychological area, often cognition.
When the researchers looked at predictors of early mortality, such as heart disease, 68% of people born extremely prematurely had at least one such predictor, compared with 18% for full-term births — although these data include people born before surfactant and corticosteroid use were widespread, so it’s unclear if these data reflect outcomes for babies born today. Researchers have found similar trends in a UK cohort study of extremely premature births. In results published earlier this year5, the EPICure study team, led by neonatologist Neil Marlow at University College London, found that 60% of 19-year-olds who were extremely premature were impaired in at least one neuropsychological area, often cognition.
Such disabilities can impact education as well as quality of life. Craig Garfield, a paediatrician at the Northwestern University Feinberg School of Medicine and the Lurie Children’s Hospital of Chicago, Illinois, addressed a basic question about the first formal year of schooling in the United States: “Is your kid ready for kindergarten, or not?”
To answer it, Garfield and his colleagues analysed standardized test scores and teacher assessments on children born in Florida between 1992 and 2002. Of those born at 23 or 24 weeks, 65% were considered ready to start kindergarten at the standard age, 5–6 years old, with the age adjusted to take into account their earlier birth. In comparison, 85.3% of children born full term were kindergarten-ready6.
Of those born at 23 or 24 weeks, 65% were considered ready to start kindergarten at the standard age, 5–6 years old, with the age adjusted to take into account their earlier birth. In comparison, 85.3% of children born full term were kindergarten-ready6.
Despite their tricky start, by the time they reach adolescence, many people born prematurely have a positive outlook. In a 2006 paper7, researchers studying individuals born weighing 1,000 grams or less compared these young adults’ perceptions of their own quality of life with those of peers of normal birthweight — and, to their surprise, found that the scores were comparable. Conversely, a 2018 study8 found that children born at less than 28 weeks did report having a significantly lower quality of life. The children, who did not have major disabilities, scored themselves 6 points lower, out of 100, than a reference population.
As Marlow spent time with his participants and their families, his worries about severe neurological issues diminished. Even when such issues are present, they don’t greatly limit most children and young adults. “They want to know that they are going to live a long life, a happy life,” he says. Most are on track to do so. “The truth is, if you survive at 22 weeks, the majority of survivors do not have a severe, life-limiting disability.”
Even when such issues are present, they don’t greatly limit most children and young adults. “They want to know that they are going to live a long life, a happy life,” he says. Most are on track to do so. “The truth is, if you survive at 22 weeks, the majority of survivors do not have a severe, life-limiting disability.”
A nurse uses electroencephalography (EEG) to carry out a check of brain development on a baby born at 25 weeks.Credit: BSIP/Universal Images Group via Getty
BreathlessBut scientists have only just begun to follow people born extremely prematurely into adulthood and then middle age and beyond, where health issues may yet lurk. “I’d like scientists to focus on improving the long-term outcomes as much as the short-term outcomes,” says Tala Alsadik, a 16-year-old high-school student in Jeddah, Saudi Arabia.
When Alsadik’s mother was 25 weeks pregnant and her waters broke, doctors went so far as to hand funeral paperwork to the family before consenting to perform a caesarean section. As a newborn, Alsadik spent three months in the neonatal-intensive-care unit (NICU) with kidney failure, sepsis and respiratory distress.
As a newborn, Alsadik spent three months in the neonatal-intensive-care unit (NICU) with kidney failure, sepsis and respiratory distress.
The complications didn’t end when she went home. The consequences of her prematurity are on display every time she speaks, her voice high and breathy because the ventilator she was put on damaged her vocal cords. When she was 15, her navel unexpectedly began leaking yellow discharge, and she required surgery. It turned out to be caused by materials leftover from when she received nutrients through a navel tube.
The brain, interrupted
That certainly wasn’t something her physicians knew to check for. In fact, doctors don’t often ask if an adolescent or adult patient was born prematurely — but doing so can be revealing.
Charlotte Bolton is a respiratory physician at the University of Nottingham, UK, where she specializes in patients with chronic obstructive pulmonary disease (COPD). People coming into her practice tend to be in their 40s or older, often current or former smokers. But in around 2008, she began to notice a new type of patient being referred to her owing to breathlessness and COPD-like symptoms: 20-something non-smokers.
But in around 2008, she began to notice a new type of patient being referred to her owing to breathlessness and COPD-like symptoms: 20-something non-smokers.
Quizzing them, Bolton discovered that many had been born before 32 weeks. For more insight, she got in touch with Marlow, who had also become concerned about lung function as the EPICure participants aged. Alterations in lung function are a key predictor of cardiovascular disease, the leading cause of death around the world. Clinicians already knew that after extremely premature birth, the lungs often don’t grow to full size. Ventilators, high oxygen levels, inflammation and infection can further damage the immature lungs, leading to low lung function and long-term breathing problems, as Bolton, Marlow and their colleagues showed in a study of 11-year-olds9.
Treatments for premature babies have improved in recent decades, but survival rates vary by age and country.Credit: Mohammed Hamoud/Getty
VICS research backs up the cardiovascular concerns: researchers have observed diminished airflow in 8-year-olds, worsening as they aged10, as well as high blood pressure in young adults11. “We really haven’t found the reason yet,” says Cheong. “That opens up a whole new research area.”
“We really haven’t found the reason yet,” says Cheong. “That opens up a whole new research area.”
At Sainte-Justine, researchers have also noticed that young adults who were born at 28 weeks or less are at nearly three times the usual risk of having high blood pressure12. The researchers figured they would try medications to control it. But their patient advisory board members had other ideas — they wanted to try lifestyle interventions first.
The scientists were pessimistic as they began a pilot study of a 14-week exercise programme. They thought that the cardiovascular risk factors would be unchangeable. Preliminary results indicate that they were wrong; the young adults are improving with exercise.
Girard-Bock says the data motivate her to eat healthily and stay active. “I’ve been given the chance to stay alive,” she says. “I need to be careful.”
From the startFor babies born prematurely, the first weeks and months of life are still the most treacherous. Dozens of clinical trials are in progress for prematurity and associated complications, some testing different nutritional formulas or improving parental support, and others targeting specific issues that lead to disability later on: underdeveloped lungs, brain bleeds and altered eye development.
Dozens of clinical trials are in progress for prematurity and associated complications, some testing different nutritional formulas or improving parental support, and others targeting specific issues that lead to disability later on: underdeveloped lungs, brain bleeds and altered eye development.
For instance, researchers hoping to protect babies’ lungs gave a growth factor called IGF-1 — which the fetus usually gets from its mother during the first two trimesters of pregnancy — to premature babies in a phase II clinical trial reported13 in 2016. Rates of a chronic lung condition that often affects premature babies halved, and babies were somewhat less likely to have a severe brain haemorrhage in their earliest months.
Could baby’s first bacteria take root before birth?
Another concern is visual impairment. Retina development halts prematurely when babies born early begin breathing oxygen. Later it restarts, but preterm babies might then make too much of a growth factor called VEGF, causing over-proliferation of blood vessels in the eye, a disorder known as retinopathy. In a phase III trial announced in 2018, researchers successfully treated 80% of these retinopathy cases with a VEGF-blocking drug called ranibizumab14, and in 2019 the drug was approved in the European Union for use in premature babies.
In a phase III trial announced in 2018, researchers successfully treated 80% of these retinopathy cases with a VEGF-blocking drug called ranibizumab14, and in 2019 the drug was approved in the European Union for use in premature babies.
Some common drugs might also be of use: paracetamol (acetaminophen), for example, lowers levels of biomolecules called prostaglandins, and this seems to encourage a key fetal vein in the lungs to close, preventing fluid from entering the lungs15.
But among the most promising treatment programmes, some neonatologists say, are social interventions to help families after they leave the hospital. For parents, it can be nerve-racking to go it alone after depending on a team of specialists for months, and lack of parental confidence has been linked to parental depression and difficulties with behaviour and social development in their growing children.
At Women & Infants Hospital of Rhode Island in Providence, Betty Vohr is director of the Neonatal Follow-Up Program. There, families are placed in private rooms, instead of sharing a large bay as happens in many NICUs. Once they are ready to leave, a programme called Transition Home Plus helps them to prepare and provides assistance such as regular check-ins by phone and in person in the first few days at home, and a 24/7 helpline. For mothers with postnatal depression, the hospital offers care from psychologists and specialist nurses.
There, families are placed in private rooms, instead of sharing a large bay as happens in many NICUs. Once they are ready to leave, a programme called Transition Home Plus helps them to prepare and provides assistance such as regular check-ins by phone and in person in the first few days at home, and a 24/7 helpline. For mothers with postnatal depression, the hospital offers care from psychologists and specialist nurses.
The results have been significant, says Vohr. The single-family rooms resulted in higher milk production by mothers: 30% more at four weeks than for families in more open spaces. At 2 years old, children from the single-family rooms scored higher on cognitive and language tests16. After Transition Home Plus began, babies discharged from the NICU had lower health-care costs and fewer hospital visits — issues that are of great concern for premature infants17. Other NICUs are developing similar programmes, Vohr says.
With these types of novel intervention, and the long-term data that continue to pour out of studies, doctors can make better predictions than ever before about how extremely premature infants will fare. Although these individuals face complications, many will thrive.
Although these individuals face complications, many will thrive.
Alsadik, for one, intends to be a success story. Despite her difficult start in life, she does well academically, and plans to become a neonatologist. “I, also, want to improve the long-term outcomes of premature birth for other people.”
Your baby was born prematurely | Regional Perinatal Center
Premature babies
If your baby is born too early, the joy of having a baby can be overshadowed by health concerns and thoughts about the possible consequences.
Instead of returning home with the baby, holding him and caressing him, you will have to stay in the department, learn to cope with the fear of touching the baby, realize the need for treatment and various manipulations, get used to the complex equipment that surrounds him.
In this situation, not only your baby needs help, you need it too! The best assistants are your loved ones, their love and care, as well as professional advice and recommendations from doctors and psychologists. This section of articles will help you improve your knowledge of preterm infant care, development and nutrition.
This section of articles will help you improve your knowledge of preterm infant care, development and nutrition.
Your help for the baby
Previously, parents were often not allowed into the neonatal unit and, especially, into the intensive care unit because of the fear of infection of the baby, but now the contact of the parent with the child is recognized as desirable and is prohibited only in exceptional cases (for example, if parents have acute infections)
Close communication between you and your baby is very important from the first days of his life. Even very immature premature babies recognize the voices and feel the touch of their parents.
The newborn needs this contact. Studies have shown that it greatly contributes to the faster adaptation of an immature child to new conditions and the stabilization of his condition. The baby's resistance to therapy increases, he absorbs large amounts of food and quickly begins to suck on his own. Contact with the child is important for parents. Taking part in the care of the baby, they feel their involvement in what is happening and quickly get used to a new role, especially when they see how he reacts to their presence.
Contact with the child is important for parents. Taking part in the care of the baby, they feel their involvement in what is happening and quickly get used to a new role, especially when they see how he reacts to their presence.
By constantly and attentively observing the baby, parents can notice the smallest changes in his condition before others. In addition, communication in the hospital is a good practice that will undoubtedly come in handy after discharge. For parents, early physical contact with the baby is very valuable, because it allows them to feel him, despite the incubator and other obstacles, and show him their love.
Treatment in the neonatal intensive care unit requires parents to have full confidence in all medical staff.
Nursing premature babies in the hospital
Many premature babies cannot breathe, suckle and regulate their body temperature sufficiently after birth. Only in the last weeks of pregnancy is the maturation of the lungs, gastrointestinal tract, kidneys, brain, which regulates and coordinates the work of all organs and systems./imgs/2021/06/09/07/4709205/21fab6918e417efd3138c9d58cd454af76bf0023.jpg)
Fluid loss due to the immaturity of the skin of premature babies and the insufficiency of thermoregulation processes require constant attention. Modern approaches focused on nursing premature babies help to cope with these problems.
Heat regulation incubator
Premature babies are very susceptible to temperature fluctuations. At the same time, clothing can interfere with the monitoring of the baby's condition and its treatment. That is why an incubator is used to provide the conditions necessary for premature babies. It maintains a certain temperature and humidity, which change as the child grows. When the body weight of a premature infant reaches 1500-1700 g, he can be transferred to a heated bed, and after reaching a weight of 2000, most premature babies can do without this support. There are no strict rules here: when nursing children with low body weight, doctors are guided by the severity of the condition of each premature baby and its degree of maturity.
In incubators, very young premature babies are placed in special "nests" - soft hemispheres in which the baby feels comfortable and assumes a position close to intrauterine. It must be protected from bright lights and loud noises. For this purpose, special screens and coatings are used.
Critical treatments during the first days of life of premature babies with low and very low birth weight:
Use of an incubator or heated bed.
Oxygen supply for respiratory support.
If necessary, artificial ventilation of the lungs or breathing using the CPAP system.
Intravenous administration of various drugs and fluids.
Carrying out parenteral nutrition with solutions of amino acids, glucose and fat emulsions.
Don't worry: not all premature babies need such extensive treatment!
Mechanical ventilation and CPAP for respiratory support
When it comes to nursing, oxygen supply is of the utmost importance for premature babies. In a child born before the 34-35th week of pregnancy, the ability of the lungs to work independently is not yet sufficiently developed. The use of a constant flow of air with oxygen, which maintains a positive airway pressure (CPAP), leads to an increase in blood oxygen saturation.
In a child born before the 34-35th week of pregnancy, the ability of the lungs to work independently is not yet sufficiently developed. The use of a constant flow of air with oxygen, which maintains a positive airway pressure (CPAP), leads to an increase in blood oxygen saturation.
This new method made it possible for the majority of even very immature children to do without mechanical ventilation. The need for intubation of children has disappeared: during treatment with CPAP, oxygen is supplied through short tubes - cannulas that are inserted into the nasal passages. CPAP or mechanical ventilation is continued until the lungs can function at full capacity on their own.
In order for the lungs to expand and remain in such a state in the future, a surfactant is needed - a substance that lines the alveoli from the inside and reduces surface tension. Surfactant is produced in sufficient quantities starting from the 34-35th week of pregnancy. Basically, it is by this time that the formation of the lungs is completed. If the baby was born earlier, modern technologies allow the introduction of surfactant into the lungs of premature babies immediately after their birth.
If the baby was born earlier, modern technologies allow the introduction of surfactant into the lungs of premature babies immediately after their birth.
Parenteral nutrition - administering nutrient solutions by vein
Premature babies, especially those born weighing less than 1500 g, are not able to get and absorb enough nutrients, even when fed through a tube. For the rapid growth of the baby, a large amount of nutrition is needed, and the size of the stomach is still very small, and the activity of digestive enzymes is also reduced. Therefore, such children are given parenteral nutrition.
Special nutrients are injected into a vein using infusion pumps that deliver solutions slowly at a predetermined rate. In this case, amino acids necessary for building proteins, fat emulsions and glucose, which are sources of energy, are used. These substances are also used for the synthesis of a number of hormones, enzymes and other biologically active substances. Additionally, minerals and vitamins are introduced.
Additionally, minerals and vitamins are introduced.
Gradually, the volume of enteral nutrition increases, and parenteral nutrition decreases until it is completely canceled.
Premature infants with gastrointestinal disease require parenteral nutrition for a longer period of time.
By the time your grown baby is discharged from the hospital, everything should be well prepared at home. And this applies not only to the environment, clothes and means of caring for the child.
All family members must be ready to receive the baby. Of course, the main care will fall on the shoulders of the parents. Although you have already gained some experience in the hospital, it is important to feel the support of others, especially in the early days.
Older children can also help. The discharge of your baby is a great joy that you want to share with all your relatives.
While you are getting used to your new role, it is important that nothing distracts you from communicating with your child. Now all the care and responsibility for the baby lies entirely with you. Everything you need to take care of him should be at hand.
Now all the care and responsibility for the baby lies entirely with you. Everything you need to take care of him should be at hand.
Preparing for discharge from the hospital
Before discharge, you must make sure that:
- Prepared the crib, bath for bathing and a place for changing clothes, preferably a changing table. A crib should be placed in the parents' bedroom, the child should not be left alone even at night. A stroller is also required. you have baby milk that was recommended by the doctor before discharge (if the child is on mixed or artificial feeding). As a rule, this is a specialized medical product. You need a certain number of small bottles and teats of the appropriate size, as well as a sterilizer. All premature babies will need pacifiers.
- You have fully mastered breastfeeding or bottle feeding.
- If your baby is not suckling all the required amount of milk from the breast and is supplementing from a bottle, you have purchased a breast pump that you have learned to use; you may also need it if you have a lot of breast milk.

- You have asked your doctor how often your child's weight should be monitored.
- If your baby still needs medication, you have the required amount at home. And you know exactly how and when to give them to your child.
- You know which warning signs to look out for.
- After the baby is discharged, a pediatrician and a neonatologist will look after the baby, to whom you will give the discharge summary from the hospital.
- You know how the hospital from which your child is being discharged will provide follow-up care after discharge.
- You know which specialists and how often should examine your baby (oculist, neuropathologist, etc.).
- All the emergency phone numbers you need are at your fingertips.
When can a child go home
This question is very difficult to answer because all children are different. The stay in the hospital can last from 6 days to 6 months, depending on the degree of prematurity of the child, the severity of his condition, as well as the presence of certain complications.
Of course, all parents look forward to the moment when the baby can be brought home. Long-term nursing of a premature baby is often a difficult test for you. But we must not forget that safety comes first, and the baby can be discharged home only when the doctors are confident in the stability of his condition. It is certainly in your interest as well.
The rate of increase in body weight and length
Weight gain is the main indicator of the growth of the baby and the adequacy of the treatment. The weight of the child, especially in the first days and weeks of life, is influenced by a number of factors: the presence of milk in the stomach (immediately after feeding), the time of bowel movement, the degree of filling of the bladder, the presence of edema. Therefore, if an edematous child does not gain weight for several days, and perhaps even loses it, do not worry. It should be remembered that children grow unevenly and periods of high weight gain alternate with lower ones. It is better to focus not on weight gain per day, but on the dynamics of this indicator over several days or a week.
It is better to focus not on weight gain per day, but on the dynamics of this indicator over several days or a week.
It is currently accepted that in the interval corresponding to 28-34 weeks of pregnancy, the normal weight gain of the child is 16-20 g/kg per day. Then it is reduced to 15 g/kg.
It is also important to take into account the rate of increase in body length. With malnutrition, at first the child gains less weight (or even loses it), and with a more pronounced deficiency of nutrients, his growth is also disturbed.
The weight must not only increase at a certain rate, but must also correspond to the length of the baby. An important parameter characterizing the development of the baby is an increase in the circumference of the head. The brain most actively increases in size during the first 12–18 months of life. But an excessively rapid increase in head circumference, as well as a slowdown in its increase, indicate neurological disorders.
A premature baby can be discharged from the hospital if:
- he is able to independently maintain the required body temperature;
- does not need breathing support and constant monitoring of the work of the respiratory and cardiovascular systems;
- can suck out the required amount of nutrition on its own;
- does not need round-the-clock monitoring and frequent determination of biochemical or other indicators;
- supportive care can be provided at home;
- he will be under the supervision of a local pediatrician and neonatologist at the place of residence.

The decision to discharge home is made for each patient individually. In addition to the state of health of the baby, the degree of preparedness of parents, their ability to provide high-level care for a premature baby is also taken into account.
Feeding a premature baby after discharge
Breastfeeding is the ideal way to feed premature babies.
However, if the baby was born much prematurely and his birth weight did not exceed 1800-2000 g, his high nutritional requirements cannot be met by breastfeeding. The growth rate will be insufficient. Moreover, over time, the content of many nutrients, including protein, in milk decreases. And it is the main material for building organs, and primarily brain tissue. Therefore, proteins must be supplied to the body of a premature infant in the optimal amount.
In addition, premature babies have a significantly increased need for calcium and phosphorus, which are essential for bone formation.
In order for the baby's nutrition to be complete even after being discharged from the hospital, special additives - "enrichers" are introduced into breast milk in a certain amount, already less than in the hospital. They make up for the lack of protein in it, as well as some vitamins and minerals. As a result, the child receives them in the optimal amount. The duration of their use will be determined by your doctor. If there is not enough milk or it does not exist at all, children born prematurely should be transferred to artificial feeding. Complementary feeding of premature babies is carried out with special children's dairy products designed for children with low birth weight. This baby milk is ideally suited to both the ability of immature children to digest and assimilate nutrients, and their needs.
Premature infant milk contains more protein, fat and carbohydrates than term infant milk, resulting in a higher calorie content. In specialized baby milk, the concentration of many minerals is higher, especially iron, zinc, calcium, phosphorus, as well as vitamins, including vitamin D. Long-chain polyunsaturated fatty acids of the Omega-3 and Omega-6 classes are introduced into such products, which are necessary for proper development of the brain and organ of vision, as well as nucleotides that contribute to the optimal development of immunity. However, when the child reaches a certain weight (2000-2500 g), you should gradually switch to feeding with standard baby milk, but not completely. Specialized baby milk can be present in the diet of a premature baby for several months. This time, as well as the volume of the product, will be determined by the doctor. He will answer all your questions about how to feed your baby.
Long-chain polyunsaturated fatty acids of the Omega-3 and Omega-6 classes are introduced into such products, which are necessary for proper development of the brain and organ of vision, as well as nucleotides that contribute to the optimal development of immunity. However, when the child reaches a certain weight (2000-2500 g), you should gradually switch to feeding with standard baby milk, but not completely. Specialized baby milk can be present in the diet of a premature baby for several months. This time, as well as the volume of the product, will be determined by the doctor. He will answer all your questions about how to feed your baby.
At present, specialized children's dairy products have been developed and are being used to feed premature babies after discharge from the hospital. In its composition, it occupies an intermediate position between a specialized product for premature babies and regular baby milk. Your baby will be transferred to such baby milk while still in the hospital. You will continue to give it to your child at home, and the doctor, watching him, will tell you when it will be possible to switch to regular standard baby milk. If the baby was born with a very low body weight or is not gaining weight well, special baby milk can be used for a long time - up to 4 months, 6 or even 9months. The beneficial effect of such children's dairy products on the growth and development of the child has been proven in scientific studies.
You will continue to give it to your child at home, and the doctor, watching him, will tell you when it will be possible to switch to regular standard baby milk. If the baby was born with a very low body weight or is not gaining weight well, special baby milk can be used for a long time - up to 4 months, 6 or even 9months. The beneficial effect of such children's dairy products on the growth and development of the child has been proven in scientific studies.
Feeding needs for premature babies
Higher caloric intake because they need to gain weight faster than term babies.
More protein as premature babies grow faster.
More calcium and phosphorus for bone building.
More trace elements and vitamins for growth and development.
A premature baby grows faster than a term baby. Nutrition for such children is calculated taking into account body weight at birth, the age of the baby and its growth rate. As a rule, the calorie content of the daily diet is about 120-130 calories per 1 kg of body weight.
It is very important that your baby continues to gain weight quickly and grow in length after discharge. To do this, feeding premature babies must be carried out using a specialized fortified diet prescribed by a doctor.
Features of adaptation and development of premature babies. Doctor Plus Medical Center
The first year of a child's life is characterized by the most intensive growth and rapid development. But during this period, the body is extremely vulnerable, the defenses are weak and imperfect. This is especially true for children who were born prematurely and are considered premature.
Premature are children born at gestational age from 28 to 37 completed weeks, weighing from 1000 - 2500 grams, height 35 - 45 cm.
The reasons for their premature birth are varied: too young age and, accordingly, the mother's body; hemolytic disease of the fetus, which develops as a result of Rhesus conflict; pathological (not normal) course of pregnancy; previous abortions, illness, physical and mental trauma; harmful working conditions, the use of nicotine and alcohol.
What a premature baby looks like. Anatomical and physiological signs.
There are 4 degrees of prematurity, depending on the weight of the child:
Grade 1: 2500 -2001 grams Grade 3: 1500 - 1001 grams
Grade 2: 2000 – 1500 grams Grade 4: 1000 grams or less.
Since body weight may or may not correspond to the gestational age at the time of birth, premature babies are divided into 2 groups also according to these signs
• children whose physical development corresponds to the gestational age at the time of birth;
In premature babies, the subcutaneous fat layer is not sufficiently developed, i.e. they suffer more from overheating and hypothermia. The skin is thin, dry, wrinkled, abundantly covered with fluff. Insufficient maturity of blood vessels is manifested by the Harlequin symptom. If you put the baby on its side, the skin acquires a contrasting pink color.
The bones of the skull are malleable, not only a large, but also a small fontanel is open.
The auricles are soft - the cartilage in them has not yet formed, they are pressed to the head, and not separated from it, as in full-term ones.
The nails do not reach the edge of the phalanges of the fingers, the umbilical cord is located below the middle of the body, and not in the center.
The underdevelopment of the genital organs is indicative: in girls, the labia minora are not covered by the large ones. In boys, the testicles are not descended into the scrotum.
The child sucks badly, swallows with difficulty. The cry is weak, breathing is not rhythmic. Physiological jaundice often lasts up to 3-4 weeks.
The umbilical cord falls off much later, and the umbilical wound heals more slowly.
It has its own characteristics and physiological weight loss. It is restored only by 2-3 weeks of life, and the timing of weight recovery is directly dependent on the maturity of the child, i.e. not only the date of his birth, but also the degree of adaptation of the baby to environmental conditions.
In premature babies, the nerve centers that regulate the rhythm of breathing are not fully formed. The formation of lung tissue has not been completed, in particular, a substance that prevents the “falling off” of the lungs - Surfactant. Therefore, their respiratory rate is not constant. With anxiety, it reaches 60-80 in 1 minute, at rest and during sleep it becomes less frequent, respiratory arrests may even be observed. The expansion of the lungs due to an insufficient amount of Surfactant is slowed down, and respiratory failure may occur.
The heart rate also depends on the condition of the child and environmental conditions. With an increase in the ambient temperature and the child's anxiety, the heart rate increases to 200 beats per minute.
In premature newborns, asphyxia and cerebral hemorrhage occur more often. They are more likely to suffer from acute respiratory diseases, intestinal infections, which is due to weak immunity and insufficient development of many adaptive reactions.
These babies are more likely than full-term babies to develop anemia (anemia).
Especially during the period when intensive growth and weight gain begins (2-3 months). With proper nutrition of the child and the mother, if she breastfeeds, these phenomena quickly pass. In the case when anemia is of a protracted nature, it is necessary to prescribe iron preparations.
The further development of the child is determined not only by the degree of prematurity, but also in many respects, by the state of his health for a given period of time.
If the child is practically healthy, from the 2nd month of life, he gains weight and height in the same way as full-term ones. By the end of the 1st year, the weight increases by 5-10 times compared to the weight at birth.
The average height is 70-77 cm.
The nervous system of premature babies is also more immature. The development of various skills, their intellectual development lags behind by 1-2 months.
These children sit down later, start walking later, they may have anomalies in the structure of the foot, curvature of the legs, and spine. If children are born very premature and often get sick, their development slows down by about a year. In the future, it levels off, approximately to preschool age.
If you have suffered intrauterine malnutrition, i.e. the nutrition of the fetus was disturbed for some reason - diseases of the mother, anomalies in the development of the child itself, anomalies in the development of the umbilical cord and placenta, then its central nervous system can recover for a long time (therefore, the observation of a neurologist is very important).
There may be lability of the nervous system (mood changes easily, often gives in to emotions, conflicts with other people are not uncommon), night terrors, enuresis (urinary incontinence), lack of appetite, a tendency to nausea.
However, in general, premature babies grow up as quite normal people.
Caring for a premature baby after discharge from the maternity hospital.
For a child born prematurely, dispensary observation is established at the place of residence up to 7 years.
Periodic consultations of specialists are obligatory, first of all - a neurologist, as well as a surgeon, an otolaryngologist, an ophthalmologist
From the age of 2-4 weeks, rickets is prevented (ultraviolet
irradiation - quartzization, the addition of vitamin D to food, massage, hardening).
The most adequate type of nutrition for a premature baby is breastfeeding. But given that the baby can suck out an insufficient amount of breast milk, you can supplement it with expressed milk or adapted mixtures.
From 4 months - vegetable purees, 5 months. - porridge, 6 months. - give meat soufflé.
Correction of protein and fat deficiency is carried out by adding the required amount of kefir and cottage cheese, starting with 5 ml, gradually increasing the dosage.
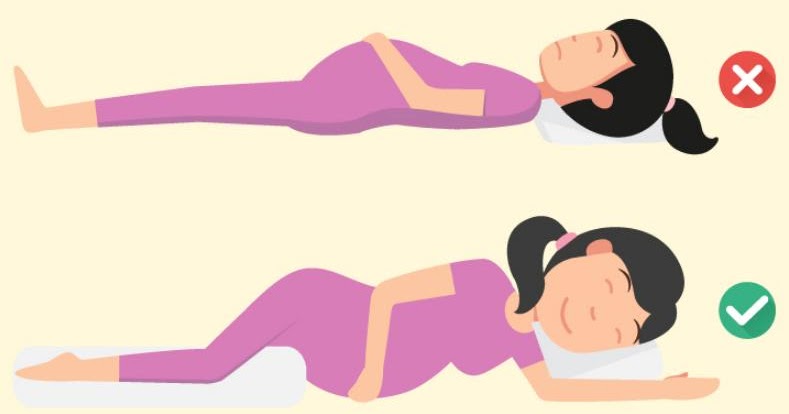
The room in which a premature baby lives should be bright, dry and thoroughly ventilated. The optimum room temperature is 20-22 *. S. Walks are very important. Sufficient exposure to fresh air prevents the development of pathological conditions.
In winter, walks start from the age of 2 months at an air temperature not lower than -8, -10*C. The duration of the walk is from 15 minutes to 2 hours. In summer, a child can spend all the intervals between feedings during the day in the fresh air. On windy, rainy and very hot days (more than 30*C), it is better for children to sleep indoors with windows open or on the veranda.
Daily warm baths are helpful. When bathing premature babies, the water temperature should be at least 37*C.
Vaccination of premature babies is carried out strictly according to an individual schedule, it depends on the state of health, physical and neuropsychic development of the child.
When organizing care for a child born prematurely, one should take into account the functional characteristics of the body.

:strip_icc():format(jpeg)/kly-media-production/medias/677579/original/Ilustrasi-hamil-1-140514-andri.jpg)