Woman with headache
Headaches and Women: What Do Hormones Have to Do With It?
A bad headache can ruin your workday, strain your relationship with family members and affect your ability to exercise. In the U.S., headaches cause 112 million sick days each year. While one-third of the population gets headaches, women suffer more than men do.
Changes in hormones could be among the reasons women have more headaches than men do.
These hormone-related headache triggers include:
- menstruation
- taking oral contraceptives
- pregnancy
- lactation
- menopause
Why hormones?
Estrogen is responsible for the development and regulation of the female reproductive system. A headache can be triggered any time there is a fluctuation in estrogen levels, including when there is a dip in estrogen levels around the time of your menstrual cycle. Women may also experience more headaches around the start of menopause and when they undergo hysterectomy.
Pre-pubescent girls and boys get headaches at the same rate. However, they occur more often for girls once they reach puberty and their menstrual cycle begins, and headaches only level off again after menopause.
To see if your menstrual cycle is affecting your headaches, try keeping a calendar to track when your symptoms begin. If you see a pattern, your doctor might be able to offer some preventions and treatment such as:
- starting medications before your monthly menstrual cycle begins to help lessen the headache pain
- taking oral contraception or using hormone replacement therapy, which may benefit some patients but not all
- in some cases, shutting down the menstrual cycle with the help of medication if the pain is extreme
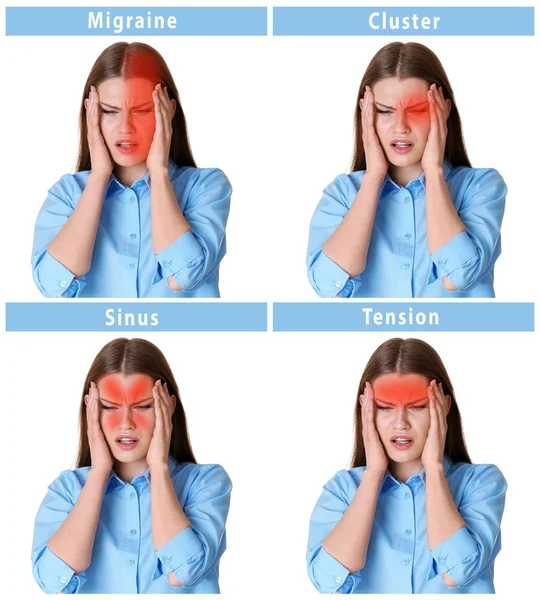
Do I have a migraine or a tension headache?
The most common types of headaches for women are tension headaches and migraines. Tension headaches are commonly described as feeling like a band around the head, but if you’ve ever felt a throbbing and pounding in your head, you may have experienced a migraine headache.
- typically last four to 72 hours (this includes pre-headache and post-headache symptoms)
- spots or zigzag lines in vision (only among 15–25 percent of headache sufferers)
- pain on one side of the head (15 percent of patients can have pain on both sides)
- pain worsened by physical activity
- sensitivity to light, sound or smell
- nausea and/or vomiting (patients with tension type headaches typically do not have nausea)
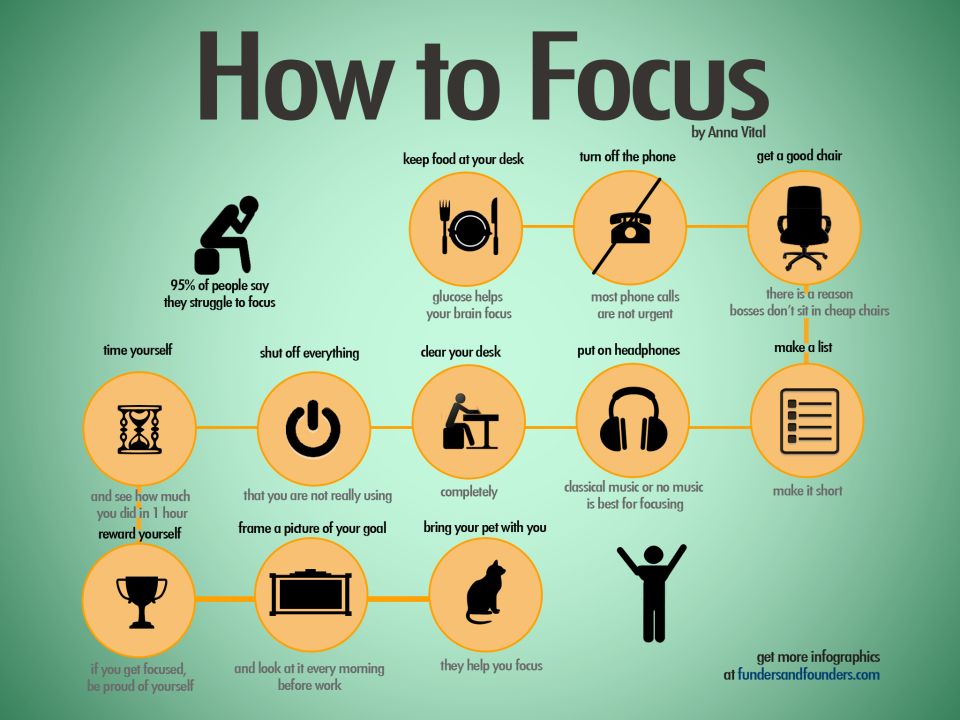
You may need to consider lifestyle changes to help manage your migraine headache symptoms. Avoid known triggers such as alcohol and stress, and be sure to hydrate, hydrate, hydrate! (You should drink 1.5 to 2 liters of water each day.) If your caffeine consumption is affecting your sleep patterns, limit excessive coffee and energy drinks. Lastly, sleep – both quality and quantity are extremely important for a healthy, migraine-free life. The key is to stay consistent with your sleep, wake-up and meal times.
The key is to stay consistent with your sleep, wake-up and meal times.
Physical therapy, especially around the neck and shoulders, can be extremely useful in easing muscle stiffness that could cause a tension headache. Behavioral therapy and relaxation training can also help with stress reduction to treat headaches.
If lifestyle modification measures fail, see your doctor.
Migraine as well as tension headaches can be managed, allowing you to enjoy your everyday activities. Understanding how hormones affect you and how they can cause migraines or headaches is the first step to finding treatment options that work for you.
Headaches and Hormones: What to Know
Headaches can be caused by many factors, and headache disorders are the leading cause of disability among women under 50 years of age. When you learn the most common causes of headaches, you may be better able to alleviate your pain.
Understanding the Relationship
For people with higher estrogen levels, you can likely blame the hormone for your headache woes. Fluctuating estrogen levels can contribute to the development of chronic headaches or migraines. Northwestern Medicine Neurologist Charulatha P. Nagar, MD , explains, “In childhood, migraines are more prevalent in males. But once the influence of estrogen begins, that’s when the prevalence starts to rise in females.” She continues that this provides the basic understanding of why headaches can be more common, longer-lasting and frequent in women.
Fluctuating estrogen levels can contribute to the development of chronic headaches or migraines. Northwestern Medicine Neurologist Charulatha P. Nagar, MD , explains, “In childhood, migraines are more prevalent in males. But once the influence of estrogen begins, that’s when the prevalence starts to rise in females.” She continues that this provides the basic understanding of why headaches can be more common, longer-lasting and frequent in women.
Headaches are one of the most modifiable disorders.
— Charulatha P. Nagar, MD
Estrogen regulates the female reproductive system, and it also happens to control chemicals in the brain that impact the sensation of pain. A decrease in estrogen levels can cause a headache, typically in the form of a migraine, which lasts anywhere from four to 72 hours.
Hormone levels fluctuate for a number of reasons. However, the most dramatic hormone fluctuations occur:
- Before menstruation: To prepare your uterus for menstruation, estrogen levels drop shortly before you get your period.
 That drop may contribute to migraine headaches.
That drop may contribute to migraine headaches. - During pregnancy: Your estrogen level rises quickly, particularly in the first trimester, to help the uterus and placenta better transfer nutrients and support the development of your baby.
- After giving birth: After delivering your baby, your level of estrogen drops because it is no longer needed to support a pregnancy.
- During perimenopause and menopause: As your body prepares to shut down the ovaries, it undergoes fluctuations in hormone levels.
- If you are taking oral contraceptives: Certain medications can alter your hormone levels.
Hormone fluctuations may also occur, for example, during gender-affirming care, such as hormone-replace therapy.
Learning Other Triggers
Hormones play a significant role in headaches, but they are not the only cause. Migraines, cluster headaches and tension headaches can occur from heightened stress or emotional distress. Other causes include:
Migraines, cluster headaches and tension headaches can occur from heightened stress or emotional distress. Other causes include:
- Anxiety. When you are anxious as a result of stress, you are more likely to eat unhealthy foods, have a disrupted sleep schedule and engage in other behaviors that can perpetuate headaches.
- Glare. The brightness from your computer screen, sunlight or overhead lights can make your head hurt.
- Noise. Sound — whether loud and repetitive or continuous, low-level noise — can cause headache pain.
- Eating and sleeping patterns. Being hungry can cause headaches, as can lack of sleep.
- Medication. Certain prescriptions can trigger headaches.
- Concussion. Headache is a common symptom of a concussion.
- Physical activity. Overexertion can cause swelling of blood vessels in your head, neck and scalp, giving you a headache.

- Lack of physical activity. A sedentary lifestyle can cause headaches.
- Posture. Sitting up straight keeps blood flowing and can help you avoid headaches.
- Food sensitivities. Certain types of foods and drinks release neurotransmitters that can lead to headaches. Common triggers include aspartame, caffeine, chocolate, alcohol and aged cheeses like Parmesan.
- Dehydration. A lack of fluids can cause several types of headaches, so it’s important to stay hydrated and drink plenty of water.
“Headaches are one of the most modifiable disorders,” says Dr. Nagar. “There is hope for seeking relief, and they’re very simple things.” For example, lifestyle changes may help prevent headaches. Maintain a healthy lifestyle that includes nutritious foods, adequate hydration, frequent exercise and proper sleep. Ask your physician about daily vitamins or supplements, such as vitamin B or magnesium.
If you find yourself experiencing a headache, seek a quiet, dark place to rest. Use a damp cloth on your forehead to provide additional relief. Gently rub the area with your forefingers. If headaches persist, keep a journal to better identify possible triggers to discuss with your physician.
“All of this makes a difference,” says Dr. Nagar.
Exploring Treatment Options
If you suffer from headaches, treatment options will depend on the severity of the headache and your overall health.
Fortunately, there are a number of options available if lifestyle changes do not provide adequate relief. “There are more tools in our toolbox as physicians,” says Dr. Nagar. Treatments can include nonsteroidal anti-inflammatory drugs (NSAIDs), triptans, and the most recent addition, calcitonin gene-related peptide (CGRP) inhibitors. These block the effect of CGRP, a small protein found in the sensory nerves that supply to the head and neck, and CGRP inhibitors can prevent headaches.
“The preventive medications are really for people whose headaches are disruptive to their quality of life,” she explains. “It’s really changing the whole paradigm of how they are treated.”
Some headaches, such as those resulting from a concussion, may require specialized care during recovery. Your care team can help you determine what treatment is right for you.
Download Headaches and Hormones: What to Know
Headache in women: causes of frequent headaches in women
Co-author, editor and medical expert - Volosov Dmitry Dmitrievich.
Views: 80 507
Last update date: 02/21/2023 G. pregnant woman
Headache while taking oral contraceptives
How to deal with menstrual headaches
Motrin® for headaches
Experts believe that migraines are more common in women than in men
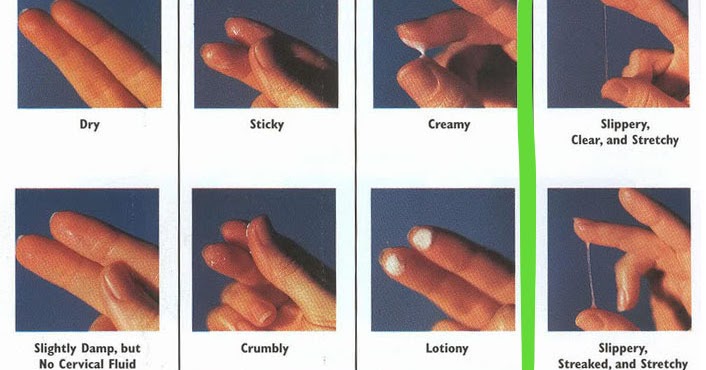
9 1 . At the same time, her attacks are longer and are much more severe. The reasons for this difference are not completely clear, however, scientists have suggested that in most cases the change in the concentration of sex hormones (in particular estrogen) is to blame. That is why frequent headaches in women often appear in reproductive age, especially during ovulation and menstruation 2 .
The reasons for this difference are not completely clear, however, scientists have suggested that in most cases the change in the concentration of sex hormones (in particular estrogen) is to blame. That is why frequent headaches in women often appear in reproductive age, especially during ovulation and menstruation 2 . Back to Contents
Headache during menstruation
Quite a number of women suffer from headaches during menstruation. This condition is called menstrual cephalgia 2 . The sensations experienced by a woman during this period are of varying intensity: from a completely tolerable and intermittent feeling of pressure inside the head to pronounced migraines that can temporarily deprive them of working capacity. Headache is often accompanied by nausea, changes in the perception of smells and tastes, increased sensitivity to sounds, mood instability and sleep disturbances 3.5 .
Menstrual pains may bother you 2 days before and 3 days after your period 4 . Usually they do not pose a health risk, however, with recurring cephalgic episodes, you should consult a doctor. The reason for this condition is a sharp change in the hormonal background during the menstrual cycle, which is especially typical for women suffering from disorders of the hypothalamic-pituitary system, which regulates the production of hormones 3 . The main causes of headaches during menstruation include the following:
Usually they do not pose a health risk, however, with recurring cephalgic episodes, you should consult a doctor. The reason for this condition is a sharp change in the hormonal background during the menstrual cycle, which is especially typical for women suffering from disorders of the hypothalamic-pituitary system, which regulates the production of hormones 3 . The main causes of headaches during menstruation include the following:
- a sharp drop in the level of the hormone progesterone 3 ;
- change in water-salt balance 6 ;
- menses-related change in prostaglandin levels 3 ;
- chronic iron deficiency anemia, which is often observed in women with heavy and prolonged menstrual bleeding 7 .
Menstrual headaches are predisposed to eating disorders with an excess of carbohydrates and saturated fats in the diet, excessively frequent consumption of strong coffee 6 . Cervical osteochondrosis, blood clotting disorders, and previous head and neck injuries also increase the likelihood of menstrual cephalgia.
Cervical osteochondrosis, blood clotting disorders, and previous head and neck injuries also increase the likelihood of menstrual cephalgia.
Back to Contents
Headache in Pregnancy
The causes of headaches in women during pregnancy and lactation can be different. In some cases, they are associated with a change in the hormonal background, in others - with an exacerbation of osteochondrosis of the cervical spine 8.9 . Only a specialist can understand the true causes of a pathological condition. The complexity of this situation lies in the fact that during such a period the choice of medicines for headache is very limited 8 . Therefore, only a doctor can prescribe the drug.
Top of page
Headache while taking oral contraceptives
The cause of frequent headaches in women of childbearing age may be the regular use of birth control pills, or rather, the synthetic hormone they contain. Unpleasant sensations can disturb a woman while the body is getting used to the drug. This is about three months, however, if the side effects are severe and significantly reduce the quality of life, you should consult a doctor to select another remedy 10 .
This is about three months, however, if the side effects are severe and significantly reduce the quality of life, you should consult a doctor to select another remedy 10 .
Back to Contents
What to do if you have a menstrual headache
Seek medical attention if your symptoms are severe . Frequent and severe headache during menstruation should be a reason to see a doctor, regardless of the age of the woman. Consultation with a specialist is also required when the nature and duration of pain changes, new symptoms join, discomfort persists during the next cycle, and menstrual irregularity.
Maintain a healthy lifestyle . Women prone to headaches are recommended evening walks, adherence to the daily regimen, sufficient night sleep and physical activity. Don't forget to drink enough fluids. It is advisable to limit the diet of foods that are difficult to digest and contribute to fluid retention, reduce the number of dishes with "fast" (easily accessible) carbohydrates. It is recommended to minimize or eliminate the use of alcohol, try to give up bad habits 11 . On the recommendation of a doctor, you can go for a medical massage of the back, neck, head.
It is recommended to minimize or eliminate the use of alcohol, try to give up bad habits 11 . On the recommendation of a doctor, you can go for a medical massage of the back, neck, head.
Take medicine recommended by your doctor . Antispasmodics, non-steroidal anti-inflammatory drugs are often used to relieve headaches 12 . With concomitant hypertension, antihypertensive drugs are indicated, and with anemia, a therapeutic diet and iron-containing drugs are usually prescribed. For migraine, the doctor prescribes the correct therapy: anti-migraine drugs, triptans 12 . Medications should be taken only with the permission of a doctor.
Back to Contents
Motrin® for headaches
Motrin® is a complex drug that helps relieve headaches. This drug has a high cardiosafety profile and is approved for dispensing in pharmacies without a prescription 13 . One dose of Motrin® is sufficient up to 12 hours 14 . For best results and proper dosage, read the instructions and consult your doctor before using it.
For best results and proper dosage, read the instructions and consult your doctor before using it.
Back to Contents
The information in this article is for reference only and does not replace professional medical advice. For diagnosis and treatment, contact a qualified specialist.
References
- Voznesenskaya TG Primary chronic daily headache in women //Problems of women's health. - 2008. - T. 3. - No. 3. - S. 38-42.
- Azimova Yu. E. Menstrual migraine: a modern view on the problem // BC. - 2017. - T. 25. - No. 21. - S. 1586-1590.
- Pustotina OA Estrogen-associated migraine and hormonal contraception //Obstetrics and gynecology: News. Opinions. Learning. – 2017. – no. 3 (17).
- Karpova M. I. et al. Migraine in women: clinical and therapeutic aspects // Journal of Neurology and Psychiatry. SS Korsakov. - 2019. - T. 119. - No. 3. - S. 98-107.
- Sadokha K. A., Misnikova V. A., Yakush S. L. Modern ideas about migraine // Medicine: a scientific and practical therapeutic journal.
 – 2016. – no. 3. - S. 78-84.
– 2016. – no. 3. - S. 78-84. - Sergeev AV Effective approaches to non-drug therapy of migraine: the role of triggers and behavioral therapy //Medical Alphabet. - 2018. - T. 3. - No. 27. - S. 21-26.
- Chernukha GE, Ilyina LM Inflammation is the biological basis of heavy menstrual bleeding, dysmenorrhea and CNS disorders. Complex solution of the problem //Medical Council. – 2015. – no. XX.
- Ekusheva E. V., Damulin I. V. Migraine attacks during pregnancy: patient management tactics and therapy priorities // Russian Medical Journal. – 2014. – no. 3.
- Yurkovskaya A. I., Chekhonatsky V. A., Chekhonatsky I. A. Osteochondrosis in pregnant women // Bulletin of medical Internet conferences. - Limited Liability Company "Science and Innovations", 2017. - V. 7. - No. 6.
- Baranov II Combined oral contraceptives: principles of individual selection, prevention of unwanted pregnancy and possible side effects, therapeutic and prophylactic effect //RMZH.
Mother and child. - 2013. - T. 21. - No. 14. - S. 745-750.
- Tabeeva G.R., Golubeva V.V. Prevention and treatment of migraine //Medical Council. – 2012. – no. 4.
- Sturov N. V., Kuznetsov V. I., Mansur T. I. Treatment of acute attacks and preventive therapy of migraine // Zemsky doctor. – 2010. – no. 4.
- Instructions for use of the drug Motrin ® tablets // Registration number P N002874/01 // URL: http : //grls . rosminzdrav . en/Grls_View_v2.aspx?routingGuid=27b4d367-41fd-49a1-a764-3129fec43869&t= (accessed 03/16/2017)
- See leaflet, section Dosing and Administration
Woman and headache: is it all about hormones?
A severe headache can ruin your work day, relationships with family members, and prevent you from playing sports or hobbies. Almost one third of the world's population periodically suffers from headaches, but it must be said that women suffer from them more often than men.
Nauman Tariq, professor, neurologist, director of the Johns Hopkins Headache Center, explains that hormonal changes may be the cause.
Causes of pain related to hormones:
What about hormones?
Estrogen is responsible for the production and regulation of the female reproductive system. Headache can be caused by changes in estrogen levels, including when it drops during menstruation. Women may also experience headaches at the onset of menopause and when they undergo a hysterectomy (removal of the uterus).
Tariq explains that girls and boys get headaches as they grow up. However, they are more common in girls who have reached puberty when their menstrual cycle began. And after menopause, headaches level out again among women and men.
To find out if there is a relationship between headaches and the menstrual cycle, Tariq suggests having a calendar to mark when the symptoms start. If you see a pattern, then your doctor may suggest preventive treatment, such as:
-
take headache medication before menstruation starts
-
when taking oral contraceptives, use hormone replacement therapy (however, this is not suitable for all patients)
-
in some cases, the menstrual cycle is stopped with medication if the pain is extremely severe
How to recognize a migraine?
Tension headaches, most common in women, are usually described as feeling as if a tight bandage had been pulled around the head. But if you have ever felt a throbbing and pounding in your head, then you may be experiencing a migraine.
Migraine symptoms
-
pain typically lasts 4 to 72 hours (this includes headache and post-headache symptoms)
accompanied by spots, zigzags before the eyes (only among 15-25% of patients suffering from headache)
-
pain in only one part of the head (but may be on both sides in 15% of patients)
-
pain aggravated by physical activity
-
sensitivity to light, sounds or smells
-
nausea and/or vomiting (patients with tension-type headaches usually do not have nausea)
What can help?
You may need to make lifestyle changes to manage your migraine symptoms. Avoid factors like alcohol and stress, and be sure to drink and drink more water! You need to drink 1.5 to 2 liters of water every day. If caffeine intake affects the quality of your sleep, then limit your excessive intake of coffee and energy drinks. And finally, sleep, its quality and quantity, is important for a healthy, migraine-free life. The key to health lies in the pattern of sleep, waking up and eating.
Massage, especially around the neck and shoulders, can be extremely helpful in relieving muscle tension that can cause a compressive headache. Any type of relaxation exercise can help prevent headaches.
If the lifestyle has changed, but the pain has not stopped, you should consult a doctor.
Dr. Tariq emphasizes that migraines as well as tension headaches can be managed, allowing you to enjoy your daily activities. Understanding how hormones affect you and how they can cause migraines or headaches is the first step to finding treatment options that will work for you.