Tips to deal with morning sickness
Vomiting and morning sickness - NHS
Nausea and vomiting in pregnancy, often known as morning sickness, is very common in early pregnancy.
It can affect you at any time of the day or night or you may feel sick all day long.
Morning sickness is unpleasant, and can significantly affect your day-to-day life. But it usually clears up by weeks 16 to 20 of your pregnancy and does not put your baby at any increased risk.
There is a chance of developing a severe form of pregnancy sickness called hyperemesis gravidarum. This can be serious, and there's a chance you may not get enough fluids in your body (dehydration) or not get enough nutrients from your diet (malnourishment). You may need specialist treatment, sometimes in hospital.
Sometimes urinary tract infections (UTIs) can also cause nausea and vomiting. A UTI usually affects the bladder, but can spread to the kidneys.
Non-urgent advice: Call your midwife, GP or 111 if:
you're vomiting and:
- have very dark-coloured urine or have not had a pee in more than 8 hours
- are unable to keep food or fluids down for 24 hours
- feel severely weak, dizzy or faint when standing up
- have tummy (abdominal) pain
- have a high temperature
- vomit blood
- have lost weight
Treatments for morning sickness
Unfortunately, there's no hard and fast treatment that will work for everyone’s morning sickness. Every pregnancy will be different.
But there are some changes you can make to your diet and daily life to try to ease the symptoms.
If these do not work for you or you're having more severe symptoms, your doctor or midwife might recommend medicine.
Things you can try yourself
If your morning sickness is not too bad, your GP or midwife will initially recommend you try some lifestyle changes:
- get plenty of rest (tiredness can make nausea worse)
- avoid foods or smells that make you feel sick
- eat something like dry toast or a plain biscuit before you get out of bed
- eat small, frequent meals of plain foods that are high in carbohydrate and low in fat (such as bread, rice, crackers and pasta)
- eat cold foods rather than hot ones if the smell of hot meals makes you feel sick
- drink plenty of fluids, such as water (sipping them little and often may help prevent vomiting)
- eat foods or drinks containing ginger – there's some evidence ginger may help reduce nausea and vomiting (check with your pharmacist before taking ginger supplements during pregnancy)
- try acupressure – there's some evidence that putting pressure on your wrist, using a special band or bracelet on your forearm, may help relieve the symptoms
Find out more about vitamins and supplements in pregnancy
Anti-sickness medicine
If your nausea and vomiting is severe and does not improve after trying the above lifestyle changes, your GP may recommend a short-term course of an anti-sickness medicine, called an antiemetic, that's safe to use in pregnancy.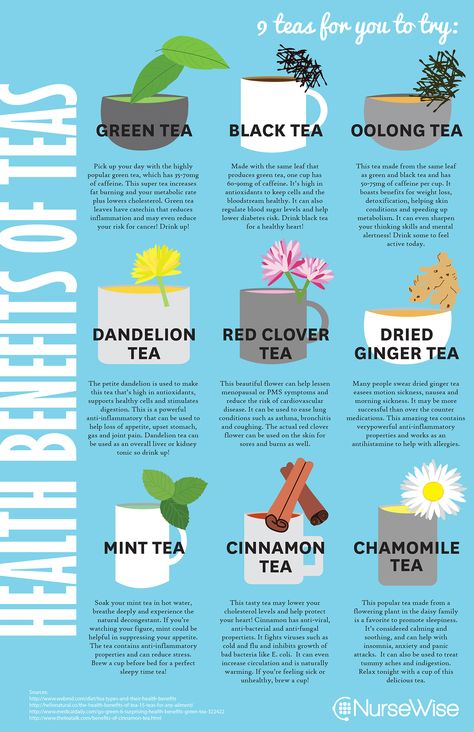
Often this will be a type of antihistamine, which are usually used to treat allergies but also work as medicines to stop sickness (antiemetic).
Antiemetics will usually be given as tablets for you to swallow.
But if you cannot keep these down, your doctor may suggest an injection or a type of medicine that's inserted into your bottom (suppository).
See your GP if you'd like to talk about getting anti-sickness medication.
Risk factors for morning sickness
It's thought hormonal changes in the first 12 weeks of pregnancy are probably one of the causes of morning sickness.
But you may be more at risk of it if:
- you're having twins or more
- you had severe sickness and vomiting in a previous pregnancy
- you tend to get motion sickness (for example, car sick)
- you have a history of migraine headaches
- morning sickness runs in the family
- you used to feel sick when taking contraceptives containing oestrogen
- it's your first pregnancy
- you're obese (your BMI is 30 or more)
- you're experiencing stress
Visit the pregnancy sickness support site for tips for you and your partner on dealing with morning sickness.
Find maternity services near you
Sign up for pregnancy emails
Sign up for Start4Life's weekly emails for expert advice, videos and tips on pregnancy, birth and beyond.
Video: how can I cope with morning sickness?
In this video, a midwife gives advice on how to deal with morning sickness during your pregnancy.
Media last reviewed: 25 January 2023
Media review due: 25 January 2026
Page last reviewed: 13 April 2021
Next review due: 13 April 2024
12 Tips To Help Calm Morning Sickness – Cleveland Clinic
If you’ve had morning sickness during pregnancy, you probably know that the name is cruelly misleading. Feelings of nausea or vomiting can strike anytime — day or night. There’s good news, though.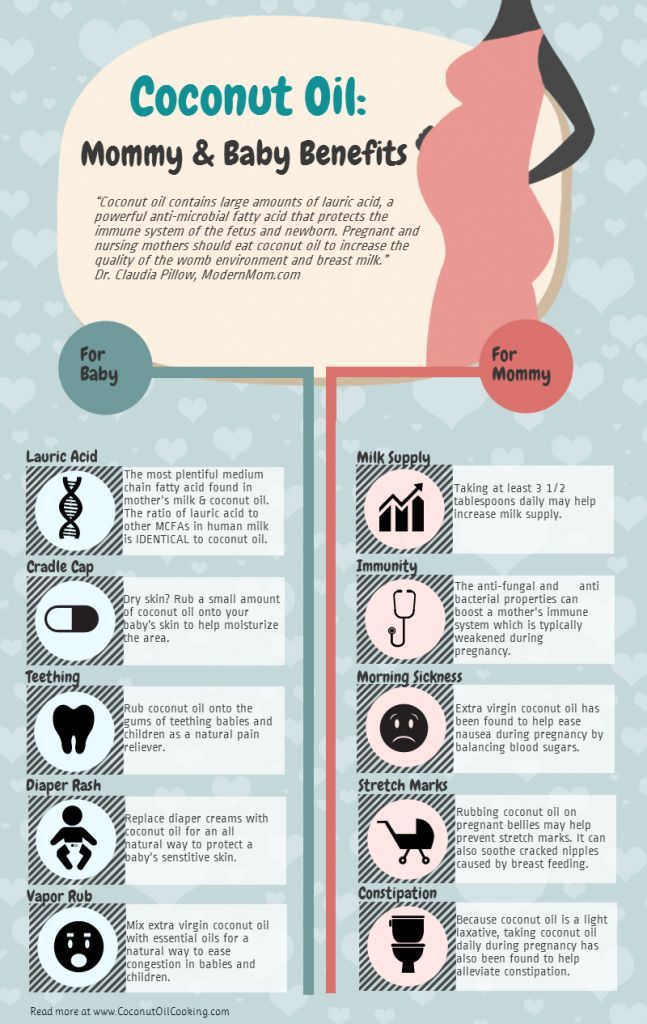 There are several things you can do to help tame your turbulent tummy.
There are several things you can do to help tame your turbulent tummy.
Morning sickness is common. In fact, one study shows that up to 80% of pregnant people experience at least some symptoms of morning sickness — but that doesn’t mean you have to simply accept it.
Certified nurse-midwife Jessica Costa, MSN, APRN, CNM, explains what causes morning sickness and how you can ease it.
What causes morning sickness?
It’s not clear exactly which hormones trigger symptoms — which can range from mild nausea to frequent vomiting — but doctors suspect that surging human chorionic gonadotropin (hCG) and progesterone levels are the culprits.
Two pieces of good news: Though unpleasant for you, these symptoms won’t harm your baby. And pregnancy nausea is often short-lived, with symptoms typically ending early in the second trimester or sooner.
“Usually, we see an increase in morning sickness symptoms between eight and 10 weeks gestation, with many people reporting relief by week 16,” Costa says.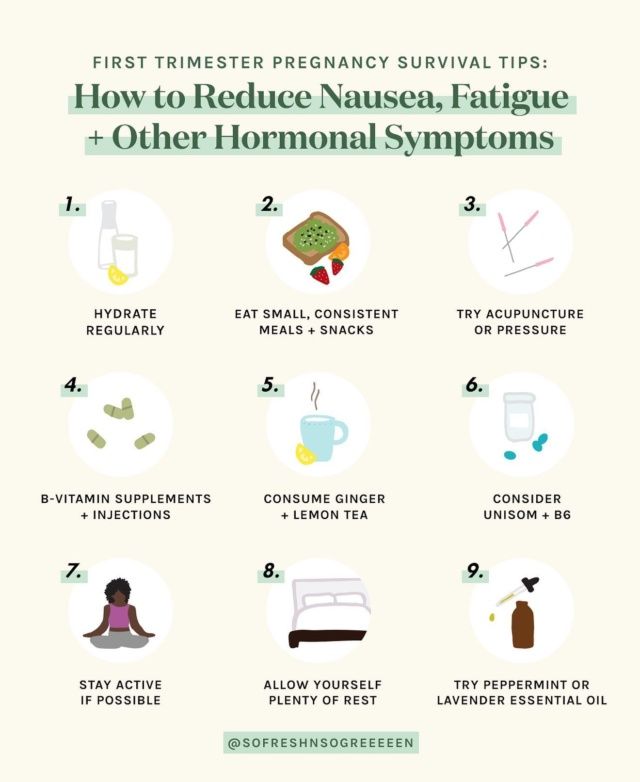
But not everyone who’s pregnant has morning sickness, and those who do have it don’t always have the same severity of symptoms. You may even find that your experience varies from one pregnancy to the next.
Remedies for morning sickness
If morning sickness has your stomach in knots, try one (or all!) of these tips to help ease your discomfort and start feeling like yourself again.
1. Eat often
“It may seem counterintuitive, but an empty stomach can actually make nausea worse,” Costa says. Every few hours, eat small meals or snacks that are easy to get down, like a handful of nuts or a few crackers.
Speaking of crackers — bland, starchy foods can help soak up gastric acid and settle the stomach, so keep some on hand.
2. Avoid food triggers
Pay attention to which foods seem to set off your nausea. Spicy, greasy, fatty and otherwise heavy foods are common culprits, while bland foods (like those found in the BRAT diet) are easier to stomach, literally.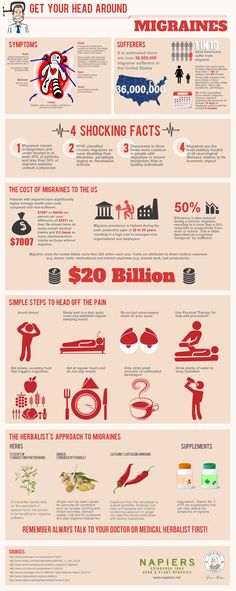
Advertising Policy
3. Prioritize protein
Studies show that protein-rich offer longer-lasting relief from nausea than foods that are high in carbohydrates or fats, so keep a supply of high-protein snacks at the ready to stave off the nausea. Costa’s favorite picks are yogurt, cottage cheese, milk, nuts and seeds.
4. Go sour for sweet relief
Fight a sour stomach with sour candies. “Sour flavors seem to help curb nausea,” Costa says. Try sucking on a piece of lemon-flavored hard candy.
You can also go straight to the source and suck on a slice of citrus fruit (think lemon, lime or orange). They’re all high in citric acid, which can help with digestion and may ease that nausea.
5. Drink for two
This one can be a bit of a “Catch-22”: Being dehydrated can contribute to nausea, but so can being uncomfortably full after drinking a lot of water. In short, you want to do your best to stay hydrated, but you don’t want to drink so much water that you make things worse.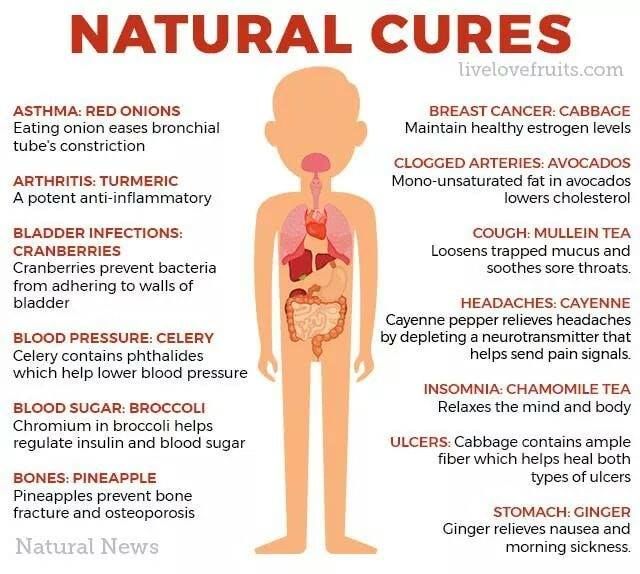
And you don’t have to always go the plain water route, either. Give yours a squeeze of lemon or another fruit infusion, or try sipping ginger ale, clear soda or a fruity tea.
6. Stay vertical
You may feel inclined to lie down when you’re not feeling well, but the opposite is actually best for pregnancy nausea.
Avoid lying down after eating, which can cause the gastric juices in your stomach to rise. “This hinders digestion and contributes to that queasy feeling,” Costa explains.
7. Wait awhile to brush
Brushing your teeth right after eating can trigger your gag reflex, which is the last thing you want when you’re prone to nausea. “For best results, try to hold off on brushing for 30 minutes or so after you eat,” Costa suggests.
8. Avoid strong odors
“Odors that might seem innocuous when you’re not pregnant may suddenly turn your stomach,” Costa says.
Advertising Policy
Studies show that everything from food to perfume to body odor can lead to nausea when you’re pregnant, thanks to the surging hormones. Try to steer clear of strong or offensive smells in the meantime.
Try to steer clear of strong or offensive smells in the meantime.
9. Embrace pleasant aromas
Lightly scented essential oil scents can help ease nausea symptoms quickly. “For the fastest results, dab a few drops on a cotton ball and sniff,” Costa advises. Try:
- Chamomile.
- Ginger.
- Lemon.
- Orange.
- Peppermint.
Of course, every pregnant body is different, so if any of these scents seem to make your nausea worse, skip them and move on to the next.
10. Try a motion-sickness band
“These wristbands curb morning sickness, motion sickness and seasickness by putting pressure on the P6 pressure point on your wrists,” Costa explains. In acupressure terms, this spot is also known as the nei guan point.
If you don’t have a motion-sickness band handy, you can put light pressure on the nei guan spot on your own. Place three fingers on your wrist, just below your hand; the nei guan point is just below them, directly beneath your index finger.
11. Take your pills at night
Prenatal vitamins are an important part of a healthy pregnancy, but some people find that taking them in the morning contributes to an upset stomach. If you suspect this is the case for you, switch to taking them in the evening with a small, healthy snack.
12. Take care of yourself
Healthy lifestyle choices can go a long way toward keeping you and baby healthy — and help ward off nausea in the process. Aim to get a good night’s sleep, regular exercise and plenty of fresh air, all of which can help keep queasiness at bay.
When to see your doctor for morning sickness
Sure, pregnancy comes with its share of discomfort — but don’t ignore unusual symptoms. Talk to your doctor if you’re experiencing any of these troubling symptoms:
- Abdominal pain.
- Difficulty urinating.
- Fever.
- Inability to keep food/drinks down for 24 hours.
- Vomiting blood.
- Weight loss.
“It’s important to keep in mind that the hormones responsible for making you feel sick also play an important role in helping your baby develop and grow,” Costa says. “But if you’ve tried everything and your symptoms are still severely impacting your daily life, talk with your healthcare provider.”
“But if you’ve tried everything and your symptoms are still severely impacting your daily life, talk with your healthcare provider.”
We fight against toxicosis - articles from the specialists of the clinic "Mother and Child"
Alexandrova Anna Evgenievna
Embryologist
Clinic "Mother and Child" South-West
rest more
Very often in the first trimester, the expectant mother feels weak, drowsy, she wants to lie down to rest, and sometimes she simply does not even have the strength to move. This, of course, is not toxicosis, but if such sensations arise, then they must be indulged so as not to inadvertently provoke another attack of nausea. Get plenty of rest and do not make any sudden movements, because even if you just fail to get up from a chair, you can provoke an attack of nausea.
Sleep with the windows open: the air in the bedroom should be fresh and cool. Go to bed on time, do not sit at midnight in front of the TV or at the computer, eliminate all irritating factors: an uncomfortable mattress, blanket, pillow, hard bedding - lack of sleep can respond with morning sickness.
eat right
Eat small meals, 5-6 times a day, or even more often. When you wake up, don't get out of bed right away. One of the most effective methods against toxicosis is breakfast in bed. In the evening, put crackers, yogurt, or any product that you can tolerate well next to your bed. Eat it before you get up, and then lie down for a while. Most likely, morning sickness will either not appear at all, or will be very weak.
Usually, in case of toxicosis, it is not recommended to eat fatty, smoked, salty, pickled, drink soda (the usual set of food hazards). But it is likely that some not very healthy product will now be well tolerated, and something from healthy food, on the contrary, will cause nausea. "Pregnant whims" - a cake with herring or pineapples at night - these are the requests of the body that it needs one or another component in food. For example, the desire to chew chalk is a sign of calcium deficiency. So eat what you like and what you want, within reason, of course. And if you don’t feel like something, even if this product is extremely useful and necessary, don’t eat it. If you feel sick from some dish, it means that the body signals you: I don’t need this now!
And if you don’t feel like something, even if this product is extremely useful and necessary, don’t eat it. If you feel sick from some dish, it means that the body signals you: I don’t need this now!
drink more often
Toxicosis may not be limited to nausea, some may also vomit. This means fluid is lost. Therefore, between meals, drink more often: a sip or two of mineral water or tea with lemon will help to cope with nausea and replenish lost fluids. But drink in small sips. Also, you should not drink food and you should give up soups for a while - a large amount of food drunk and eaten, on the contrary, only provokes nausea and vomiting.
breathe fresh air
Outdoor walks are good for everyone, but especially for toxicosis. Firstly, when walking, the blood of the expectant mother and baby is saturated with oxygen, which is very important for health, and secondly, walking calms the nervous system. Together, this helps to reduce the unpleasant symptoms of toxicosis. You need to walk at least two hours a day - but not just along the street, but in the place where the air is really fresh: in the forest, park, square, and best of all outside the city. Before you go out, think over the route: go away from gas-polluted highways, street cafes, food stalls and other "fragrant" places.
You need to walk at least two hours a day - but not just along the street, but in the place where the air is really fresh: in the forest, park, square, and best of all outside the city. Before you go out, think over the route: go away from gas-polluted highways, street cafes, food stalls and other "fragrant" places.
eliminate fragrances
Taste and smell preferences change during the first trimester. Now even your favorite perfumes can cause nausea, headaches and allergic reactions. Therefore, put away all fragrant cosmetics that irritate you: perfumes, deodorants, creams, and so on. You will have to stop using your favorite perfume for both your husband and loved ones. Explain to others that this is not a whim, but a temporary measure, very soon everything will return to normal.
And do not worry that now you will be left without your usual beauty products. Both the cosmetic store and the pharmacy are full of different creams, tonics, shampoos without fragrance or with a minimal smell.
work with yourself
Psychologists believe that the cause of toxicosis is not only in hormonal changes, but also in the psychological state of a woman. The more a woman experiences, the more anxieties and fears she has, the more pronounced toxicosis can be. Ideally, it is better to limit yourself during pregnancy from any stress. Of course, it’s not always possible to eliminate nervous work or crowding in public transport, but watch less TV, don’t read negative news and various pregnant “horror stories” on the Internet, and don’t react to minor or even major everyday troubles everyone can do. Therefore, if you are worried about toxicosis, create your own comfortable world during pregnancy. If you can’t cope on your own, contact a specialist (psychologist). Toxicosis is really well treated with psychotherapy. The main thing is that the expectant mother should want to get rid of her own anxiety.
No matter how unpleasant toxicosis is, it does not last forever. It is necessary to suffer until the beginning or (less often) the middle of the II trimester. And very soon all the unpleasant symptoms of toxicosis will remain in the past!
It is necessary to suffer until the beginning or (less often) the middle of the II trimester. And very soon all the unpleasant symptoms of toxicosis will remain in the past!
Make an appointment
to the doctor - Alexandrova Anna Evgenievna
Clinic "Mother and Child" South-West
ICSIECO
By clicking on the send button, I consent to the processing of personal data
Attention! Prices for services in different clinics may vary. To clarify the current cost, select clinic
The administration of the clinic takes all measures to update the prices for programs in a timely manner, however, in order to avoid possible misunderstandings, we recommend that you clarify the cost of services by phone / with the managers of the clinic
Clinical Hospital MD GROUPClinical Hospital Lapino-1 "Mother and Child"Clinic KG "Lapino" in Odintsovo (branch)Clinic "Mother and Child" Khodynskoye PoleClinic "Mother and Child" KuntsevoClinic "Mother and Child" Savelovskaya Clinic "Mother and Child" » South-WestClinic "Mother and Child" NovogireevoClinic "Mother and Child" Lefortovo
All directionsSpecialist consultations (adults)Specialist consultations (children)Laboratory of molecular geneticsGeneral clinical studiesTreatment roomTelemedicine for adultsTherapeutic studiesUltrasound examinations for adults
01.
Specialist consultations (adults)
02.
Specialist consultations (children)
03.
Laboratory of molecular genetics
04.
General clinical studies
05.
Procedure cabinet
06.
Telemedics for adults
07.
Therapeutic studies
08. 9000 Nothing found
The administration of the clinic takes all measures to timely update the price list posted on the website, however, in order to avoid possible misunderstandings, we advise you to clarify the cost of services and the timing of the tests by calling
How to deal with toxicosis - doctor's advice
The head of the Department of Pregnancy Pathology of the Perinatal Center of St. Petersburg State Pediatric Medical University, obstetrician-gynecologist Olga Sergienko told about how to competently deal with toxicosis
Toxicosis occurs at different stages of pregnancy, and this condition is associated with exposure to substances that are formed in the mother's body during the development of the fetus. The most common symptoms of early toxicosis are weakness, drowsiness, and nausea.
The most common symptoms of early toxicosis are weakness, drowsiness, and nausea.
Toxicosis during pregnancy - a norm or a pathology?
Toxicosis is a manifestation of a pathological reaction of a woman's body to a developing pregnancy. The severity of this reaction can vary from minor complaints to changes that require medical attention.
Is toxicosis dangerous for mother or baby?
Toxicosis can be dangerous if it becomes severe. For example, excessive vomiting causes:
- severe dehydration,
- changes in the electrolyte balance of the blood,
- violation of the function of various organs and systems, which makes it necessary to raise the question of artificial termination of pregnancy.
Nausea and vomiting are the most common manifestations of toxicosis in pregnant women. For any complaints, you should consult a doctor for examination, assessment of the severity of the condition, identification of concomitant pathology, which is aggravated during toxicosis and the timely start of adequate treatment.
How to make life easier for a future mother during pregnancy with toxicosis?
Recommended:
- eat often and in small portions,
- eat easily digestible food,
- avoid fatty, fried, spicy foods.
Depending on the accompanying pathology, drug therapy may be prescribed by a doctor. And, of course, preventive measures at the stage of pregnancy planning are of great importance, such as:
- treatment of chronic diseases, especially of the gastrointestinal tract,
- , if necessary, correction of the emotional state of the expectant mother,
- elimination of mental stress, adverse environmental factors,
- depression in pregnant women.
What happens in the body of a pregnant woman with preeclampsia?
According to the international classification, this condition is called preeclampsia (preeclampsia), in other words, it is toxicosis that occurs later in pregnancy.
There are several theories for the development of preeclampsia. The main reason is the disruption of the placenta and the blood supply to the uterus, which triggers a mechanism for increasing pressure due to vasospasm and further disruption of the function of various organs and body systems.
Who has the highest risk of preeclampsia?
Various factors contribute to the development of pre-eclampsia, such as:
- first upcoming birth,
- extragenital pathology (pre-existing arterial hypertension, kidney pathology),
- vascular diseases (chronic venous insufficiency),
- endocrine pathology (diabetes mellitus, dyslipidemia, obesity),
- autoimmune diseases (antiphospholipid syndrome, systemic lupus erythematosus),
- Age of pregnancy (under 18 and over 30),
- multiple pregnancy,
- genetic predisposition,
- occupational hazards,
- unfavorable working and living conditions.