White blister on baby tongue
Oral conditions - young children
It is a good idea to look inside your child’s mouth regularly. Look at the gums, the teeth and tongue. Also look at the cheeks, the roof of the mouth and lips as well. Oral thrush, mouth ulcers and cold sores are common problems. The early signs of tooth decay is another thing to look out for when checking your child’s mouth (see Tooth decay – young children). Speak to your doctor, dentist or oral health professional if you are concerned about anything in your child’s mouth.
Oral thrush in young children
Oral thrush is a fungal infection that affects the soft tissue inside the mouth. It is quite common in young children. Oral thrush looks like milky white patches in the mouth. On the tongue it appears as a white coating which does not disappear after feeding. Your child may also have an infection in the nappy area at the same time. Very rarely a fever and abdominal irritation may show with an oral thrush infection; however, this may also indicate a more general infection.
Thrush is treated with antifungal medications applied directly to the affected areas. See your pharmacist, doctor or oral health professional.
Mouth ulcers in young children
Mouth ulcers are a type of sore inside the mouth. They can have several causes and are not contagious.
Traumatic ulcers are a common type of mouth ulcer that results from injury to the mouth; for example, after biting the cheek.
Aphthous ulcers are a painful type of ulcer that tends to come back again and again as one or many sores a few millimetres in size.
Mouth ulcers usually heal on their own in a week or two. If any ulcer does not heal after two weeks, it is important to see a doctor or oral health professional. While oral cancer is extremely rare in children, ulcers that don’t heal can be a sign of oral cancer.
There is treatment for mouth ulcers but you can help to reduce pain by:
- avoiding acidic foods and drinks, such as oranges and other citrus fruits.
 Salty, spicy or hot food, can also sting the ulcer and make it worse.
Salty, spicy or hot food, can also sting the ulcer and make it worse. - making sure children regularly drink water
- using a protective gel on the affected area, especially before eating.
Take care with any anaesthetic gel or medication, as they can have ingredients which might not be suitable for young children. Ask your pharmacist, doctor or oral health professional.
Oral herpes (cold sores) in young children
Cold sores are blisters around the mouth and nose, caused by the Herpes Simplex Virus (HSV). Cold sores are very infectious and spread easily from one person to another. The most infectious time is in the first few days when the cold sore blister is forming. The virus may be spread by touching the sore directly or via saliva. Sometimes, people can pass the virus to others when they have no symptoms.
The first HSV infection
If your child has been infected with herpes simplex, they may show no symptoms. However one in four children develop mouth ulcers If they do have symptoms, they may include:
- fever
- irritability and tiredness
- painful mouth ulcers and lip blisters
- sores (blisters and ulcers) in and around the mouth
- a sore throat
- swollen neck glands
- poor appetite or reluctance to drink.

Symptoms of cold sores in children
The ulcers/blisters usually take 10 to 14 days to go away. The blisters never leave scars.
Symptoms in children may include:
- tingling, burning or itchiness of the skin (these are early signs of a cold sore)
- small clusters of blisters that quickly break out inside the mouth, or on the gums or lips
- yellowish ulcers surrounded by a red circle, which develop after the blisters burst
- red, swollen gums that bleed when touched
- fever, feeling unwell, tiredness and irritability.
See your doctor, or oral health professional if sores do not heal within two weeks or the child has fever.
Treatment for cold sores in children
There is no cure for the HSV infection, but you can help to reduce pain by giving your child:
- lots of fluids, preferably water – dehydration is a risk in small children if it is painful to swallow
- bland foods such as plain natural yoghurt
- little or no salty, spicy or acidic foods.

Ask your pharmacist or doctor about pain relief medication and antiviral creams which may make it more comfortable for your child to drink and eat.
Preventing the spread of cold sores
HSV is transmitted easily. Steps that can help to reduce its spread include:
- Avoid touching your child’s cold sores and try to keep them from touching them too. Wash your and their hands thoroughly, and as soon as possible, if a sore is touched.
- Keep your child’s utensils such as cups and forks, and items such as towels and face washers separate from everyone else’s, and wash them thoroughly after use.
- Take extra care not to let your child touch anyone around the eyes, including themselves. A herpes infection in the eyes can be quite serious.
- You may need to keep them home from childcare or school until their cold sore blister stops weeping to prevent spreading the virus.
Tooth abscesses in young children
A tooth abscess is a pocket of pus caused by an infection and is normally associated with tooth decay. An abscess can also be caused by the gums directly on a healthy tooth, for example when food keeps getting stuck and not being able to get cleaned out, or a sharp piece of food or tooth fragment gets lodged into the gums, or even an infection/abscess over a newly erupting tooth. It appears as a pimple on the gum, swelling of the gum or as swelling of the face on the side of the affected tooth.
An abscess can also be caused by the gums directly on a healthy tooth, for example when food keeps getting stuck and not being able to get cleaned out, or a sharp piece of food or tooth fragment gets lodged into the gums, or even an infection/abscess over a newly erupting tooth. It appears as a pimple on the gum, swelling of the gum or as swelling of the face on the side of the affected tooth.
A child may complain of:
- Throbbing toothache that can go to the jaw
- Sensitivity to hot and cold temperatures
- Sensitivity to the pressure of chewing or biting
- Fever
- Your child’s face or cheek is swollen and you feel swollen glands on the child’s jaw or neck.
See a doctor or oral health professional immediately if you think your child may have a tooth abscess.
Brushing teeth twice a day with low fluoride toothpaste (18 months- 6 years) or adult toothpaste (6 years and above) is an important preventative measure for tooth decay.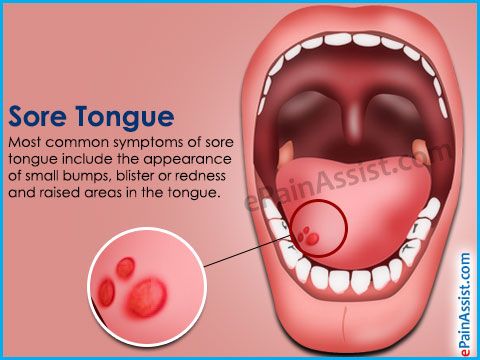
Cellulitis
Cellulitis is caused by bacteria that enters the body through broken skin. It can appear as redness of the skin, swelling and fever, and can spread very quickly to the rest of the body. If this infection is seen on the face, it can be related to a tooth or gums, where the infection has spread deep.
The treatment for cellulitis is a course of antibiotics, so it is important for your child to see a doctor or oral health professional as soon as any swelling of the face appears. In severe cases you may need to go to the hospital emergency department.
Mucoceles in young children
A mucocele is a harmless, mucus-containing cyst of a small saliva gland. It looks like a soft, bluish-grey swelling, usually on the lower lip. It can be caused by trauma to the lip, often from lip biting.
Mucoceles will often burst and heal by themselves. If they don’t heal, or if they become a problem, see your doctor or oral health professional.
Eruption cysts in young children
An eruption cyst is a smooth, bluish, dome-shaped blister that appears on the gum where a tooth is coming through. Usually treatment is not required because the cyst bursts when the tooth breaks through.
Usually treatment is not required because the cyst bursts when the tooth breaks through.
Seek advice from a doctor or oral health professional if you think the area may be infected or if the cyst doesn’t go away when the tooth erupts, or within two weeks.
Hand, foot and mouth disease in young children
Hand, foot and mouth disease is a common viral infection occurring in infants and children younger than 5 years old. Most children have mild symptoms for 7 to 10 days. It is characterised by painful ulcers in the front of the mouth and small blisters on the hands and feet. Your child may also have a sore throat or mouth and a minor fever.
This disease will heal by itself. Give fluids (mostly water) and soft foods to reduce discomfort. Keep your child at home until the sores have dried to prevent spreading the disease.
See your GP if:
- Your child is not drinking enough to stay hydrated
- Your child’s fever lasts longer than 3 days
- Your child has a weakened immune system (body’s ability to fight germs and sickness)
- Symptoms are severe.
- Symptoms do not improve after 10 days
- Your child is very young, especially younger than 6 months
Measles in young children
Measles is a viral infection that first appears as lots of small white spots that look like grains of salt surrounded by inflammation (swelling and redness) on the inside the mouth on the cheeks. The white spots appear two to three days before the measles rash shows on the face and body. Prevention is through the combined vaccination against measles, mumps and varicella given at 12 months of age.
Measles can be a serious condition in young children and is contagious. See your doctor immediately if you think your child might have measles.
A number of other viral and bacterial infections can show signs in the mouth. It’s always a good idea to check with an oral health professional, GP or paediatrician if you have any concerns.
Chalky teeth in young children
About one in six children have ‘chalky teeth’ (also known as hypomineralised enamel). This can look like creamy-brown or very white spots (like the colour of chalk), particularly on the molars (back teeth).
This can look like creamy-brown or very white spots (like the colour of chalk), particularly on the molars (back teeth).
Teeth can become ‘chalky’ if the enamel (tooth surface) doesn’t harden properly when the tooth is forming. Because these teeth are weaker, they have a much higher risk of tooth decay. Taking your child for a dental check-up before two years of age will help with early identification and care of this problem.
Chalky teeth can sometimes be confused with tooth decay. If you notice anything unusual about your child’s teeth, always see your dentist or oral health professional as soon as possible.
Where to get help
- Your GP (doctor)
- Your oral health professional (dentist)
- Dental Health Services Victoria provide public dental services through the Royal Dental Hospital Melbourne and community dental clinics, for eligible people. For more information about public dental services Tel. (03) 9341 1000, or 1800 833 039 outside Melbourne metro
- Australian Dental Association ‘Find a Dentist’ search function or Tel.
 (03) 8825 4600
(03) 8825 4600 - Your maternal and child health nurse
Oral conditions - young children
It is a good idea to look inside your child’s mouth regularly. Look at the gums, the teeth and tongue. Also look at the cheeks, the roof of the mouth and lips as well. Oral thrush, mouth ulcers and cold sores are common problems. The early signs of tooth decay is another thing to look out for when checking your child’s mouth (see Tooth decay – young children). Speak to your doctor, dentist or oral health professional if you are concerned about anything in your child’s mouth.
Oral thrush in young children
Oral thrush is a fungal infection that affects the soft tissue inside the mouth. It is quite common in young children. Oral thrush looks like milky white patches in the mouth. On the tongue it appears as a white coating which does not disappear after feeding. Your child may also have an infection in the nappy area at the same time. Very rarely a fever and abdominal irritation may show with an oral thrush infection; however, this may also indicate a more general infection.
Thrush is treated with antifungal medications applied directly to the affected areas. See your pharmacist, doctor or oral health professional.
Mouth ulcers in young children
Mouth ulcers are a type of sore inside the mouth. They can have several causes and are not contagious.
Traumatic ulcers are a common type of mouth ulcer that results from injury to the mouth; for example, after biting the cheek.
Aphthous ulcers are a painful type of ulcer that tends to come back again and again as one or many sores a few millimetres in size.
Mouth ulcers usually heal on their own in a week or two. If any ulcer does not heal after two weeks, it is important to see a doctor or oral health professional. While oral cancer is extremely rare in children, ulcers that don’t heal can be a sign of oral cancer.
There is treatment for mouth ulcers but you can help to reduce pain by:
- avoiding acidic foods and drinks, such as oranges and other citrus fruits.
 Salty, spicy or hot food, can also sting the ulcer and make it worse.
Salty, spicy or hot food, can also sting the ulcer and make it worse. - making sure children regularly drink water
- using a protective gel on the affected area, especially before eating.
Take care with any anaesthetic gel or medication, as they can have ingredients which might not be suitable for young children. Ask your pharmacist, doctor or oral health professional.
Oral herpes (cold sores) in young children
Cold sores are blisters around the mouth and nose, caused by the Herpes Simplex Virus (HSV). Cold sores are very infectious and spread easily from one person to another. The most infectious time is in the first few days when the cold sore blister is forming. The virus may be spread by touching the sore directly or via saliva. Sometimes, people can pass the virus to others when they have no symptoms.
The first HSV infection
If your child has been infected with herpes simplex, they may show no symptoms. However one in four children develop mouth ulcers If they do have symptoms, they may include:
- fever
- irritability and tiredness
- painful mouth ulcers and lip blisters
- sores (blisters and ulcers) in and around the mouth
- a sore throat
- swollen neck glands
- poor appetite or reluctance to drink.

Symptoms of cold sores in children
The ulcers/blisters usually take 10 to 14 days to go away. The blisters never leave scars.
Symptoms in children may include:
- tingling, burning or itchiness of the skin (these are early signs of a cold sore)
- small clusters of blisters that quickly break out inside the mouth, or on the gums or lips
- yellowish ulcers surrounded by a red circle, which develop after the blisters burst
- red, swollen gums that bleed when touched
- fever, feeling unwell, tiredness and irritability.
See your doctor, or oral health professional if sores do not heal within two weeks or the child has fever.
Treatment for cold sores in children
There is no cure for the HSV infection, but you can help to reduce pain by giving your child:
- lots of fluids, preferably water – dehydration is a risk in small children if it is painful to swallow
- bland foods such as plain natural yoghurt
- little or no salty, spicy or acidic foods.

Ask your pharmacist or doctor about pain relief medication and antiviral creams which may make it more comfortable for your child to drink and eat.
Preventing the spread of cold sores
HSV is transmitted easily. Steps that can help to reduce its spread include:
- Avoid touching your child’s cold sores and try to keep them from touching them too. Wash your and their hands thoroughly, and as soon as possible, if a sore is touched.
- Keep your child’s utensils such as cups and forks, and items such as towels and face washers separate from everyone else’s, and wash them thoroughly after use.
- Take extra care not to let your child touch anyone around the eyes, including themselves. A herpes infection in the eyes can be quite serious.
- You may need to keep them home from childcare or school until their cold sore blister stops weeping to prevent spreading the virus.
Tooth abscesses in young children
A tooth abscess is a pocket of pus caused by an infection and is normally associated with tooth decay. An abscess can also be caused by the gums directly on a healthy tooth, for example when food keeps getting stuck and not being able to get cleaned out, or a sharp piece of food or tooth fragment gets lodged into the gums, or even an infection/abscess over a newly erupting tooth. It appears as a pimple on the gum, swelling of the gum or as swelling of the face on the side of the affected tooth.
An abscess can also be caused by the gums directly on a healthy tooth, for example when food keeps getting stuck and not being able to get cleaned out, or a sharp piece of food or tooth fragment gets lodged into the gums, or even an infection/abscess over a newly erupting tooth. It appears as a pimple on the gum, swelling of the gum or as swelling of the face on the side of the affected tooth.
A child may complain of:
- Throbbing toothache that can go to the jaw
- Sensitivity to hot and cold temperatures
- Sensitivity to the pressure of chewing or biting
- Fever
- Your child’s face or cheek is swollen and you feel swollen glands on the child’s jaw or neck.
See a doctor or oral health professional immediately if you think your child may have a tooth abscess.
Brushing teeth twice a day with low fluoride toothpaste (18 months- 6 years) or adult toothpaste (6 years and above) is an important preventative measure for tooth decay.
Cellulitis
Cellulitis is caused by bacteria that enters the body through broken skin. It can appear as redness of the skin, swelling and fever, and can spread very quickly to the rest of the body. If this infection is seen on the face, it can be related to a tooth or gums, where the infection has spread deep.
The treatment for cellulitis is a course of antibiotics, so it is important for your child to see a doctor or oral health professional as soon as any swelling of the face appears. In severe cases you may need to go to the hospital emergency department.
Mucoceles in young children
A mucocele is a harmless, mucus-containing cyst of a small saliva gland. It looks like a soft, bluish-grey swelling, usually on the lower lip. It can be caused by trauma to the lip, often from lip biting.
Mucoceles will often burst and heal by themselves. If they don’t heal, or if they become a problem, see your doctor or oral health professional.
Eruption cysts in young children
An eruption cyst is a smooth, bluish, dome-shaped blister that appears on the gum where a tooth is coming through. Usually treatment is not required because the cyst bursts when the tooth breaks through.
Usually treatment is not required because the cyst bursts when the tooth breaks through.
Seek advice from a doctor or oral health professional if you think the area may be infected or if the cyst doesn’t go away when the tooth erupts, or within two weeks.
Hand, foot and mouth disease in young children
Hand, foot and mouth disease is a common viral infection occurring in infants and children younger than 5 years old. Most children have mild symptoms for 7 to 10 days. It is characterised by painful ulcers in the front of the mouth and small blisters on the hands and feet. Your child may also have a sore throat or mouth and a minor fever.
This disease will heal by itself. Give fluids (mostly water) and soft foods to reduce discomfort. Keep your child at home until the sores have dried to prevent spreading the disease.
See your GP if:
- Your child is not drinking enough to stay hydrated
- Your child’s fever lasts longer than 3 days
- Your child has a weakened immune system (body’s ability to fight germs and sickness)
- Symptoms are severe.
- Symptoms do not improve after 10 days
- Your child is very young, especially younger than 6 months
Measles in young children
Measles is a viral infection that first appears as lots of small white spots that look like grains of salt surrounded by inflammation (swelling and redness) on the inside the mouth on the cheeks. The white spots appear two to three days before the measles rash shows on the face and body. Prevention is through the combined vaccination against measles, mumps and varicella given at 12 months of age.
Measles can be a serious condition in young children and is contagious. See your doctor immediately if you think your child might have measles.
A number of other viral and bacterial infections can show signs in the mouth. It’s always a good idea to check with an oral health professional, GP or paediatrician if you have any concerns.
Chalky teeth in young children
About one in six children have ‘chalky teeth’ (also known as hypomineralised enamel). This can look like creamy-brown or very white spots (like the colour of chalk), particularly on the molars (back teeth).
This can look like creamy-brown or very white spots (like the colour of chalk), particularly on the molars (back teeth).
Teeth can become ‘chalky’ if the enamel (tooth surface) doesn’t harden properly when the tooth is forming. Because these teeth are weaker, they have a much higher risk of tooth decay. Taking your child for a dental check-up before two years of age will help with early identification and care of this problem.
Chalky teeth can sometimes be confused with tooth decay. If you notice anything unusual about your child’s teeth, always see your dentist or oral health professional as soon as possible.
Where to get help
- Your GP (doctor)
- Your oral health professional (dentist)
- Dental Health Services Victoria provide public dental services through the Royal Dental Hospital Melbourne and community dental clinics, for eligible people. For more information about public dental services Tel. (03) 9341 1000, or 1800 833 039 outside Melbourne metro
- Australian Dental Association ‘Find a Dentist’ search function or Tel.
 (03) 8825 4600
(03) 8825 4600 - Your maternal and child health nurse
Stomatitis in a child - what is it? . Official site of KGAUZ "Norilsk GSP"
Stomatitis is an inflammation of the oral mucosa. The name comes from the Latin word “stoma” (mouth). Stomatitis occurs in both children and adults, but most often it appears in infants and preschoolers. This is because the mucosa at this age is thinner and more tender. It’s more common for everyone to say “stomatitis”, but it would be more correct to say “stomatitis”, since this is a generalizing concept for a whole group of diseases.
Causes of stomatitis in children
The causes of stomatitis in children are different. These are dirty hands, and fragile children's immunity, and the features of thermoregulation, on which the respiratory system directly depends. You need to understand that the children's mucosa, unlike the adult one, is a very thin and vulnerable substance, so the attachment of any infection occurs very quickly. At an early age, salivation is not yet fully formed in a child, and saliva enzymes play a very important role in protecting the body. As a result, the mucous membrane often dries up, cracks appear, an infection occurs, and stomatitis follows it. It is impossible not to take into account the long-term use of medications, such as antibiotics, as well as neuropsychiatric disorders, unfavorable living conditions, poor child care and inadequate oral hygiene by the parents themselves.
At an early age, salivation is not yet fully formed in a child, and saliva enzymes play a very important role in protecting the body. As a result, the mucous membrane often dries up, cracks appear, an infection occurs, and stomatitis follows it. It is impossible not to take into account the long-term use of medications, such as antibiotics, as well as neuropsychiatric disorders, unfavorable living conditions, poor child care and inadequate oral hygiene by the parents themselves.
It is often the parents who help the doctor to find out the cause of the disease. Only they can try to analyze what caused the appearance of a bubble, sore or plaque. For example, the child ate something wrong, bought a new toothpaste or toothbrush, or maybe the baby suffered a temperature drop.
Depending on the causes of occurrence, stomatitis can be divided into several types, each of which has a number of features.
Viral, herpes, or herpetic stomatitis in children is one of the most common types of childhood stomatitis. Usually a child becomes infected with it by airborne droplets. The virus is also transmitted through dishes, toys, household items. Most often, herpetic stomatitis in a child appears at the age of one to 4 years. The disease begins as a cold and is accompanied by a rash on the lips, lethargy, and fever. Sometimes there is a runny nose and cough. Around the second day, aphthae appear on the lips, tongue, and inside of the cheeks - small round or oval sores of light yellow color with a bright red border. They exude an unpleasant odor, are easily torn off and then bleed. These ulcers are the main symptom of this type of stomatitis. Therefore, such stomatitis in children is also called aphthous, or ulcerative. This is a particularly unpleasant type of disease, as it can be severe and accompanied by severe intoxication. Viral stomatitis in children also often occurs against the background of other viral diseases, such as influenza, chickenpox or measles.
Usually a child becomes infected with it by airborne droplets. The virus is also transmitted through dishes, toys, household items. Most often, herpetic stomatitis in a child appears at the age of one to 4 years. The disease begins as a cold and is accompanied by a rash on the lips, lethargy, and fever. Sometimes there is a runny nose and cough. Around the second day, aphthae appear on the lips, tongue, and inside of the cheeks - small round or oval sores of light yellow color with a bright red border. They exude an unpleasant odor, are easily torn off and then bleed. These ulcers are the main symptom of this type of stomatitis. Therefore, such stomatitis in children is also called aphthous, or ulcerative. This is a particularly unpleasant type of disease, as it can be severe and accompanied by severe intoxication. Viral stomatitis in children also often occurs against the background of other viral diseases, such as influenza, chickenpox or measles.
Infectious stomatitis occurs in children of both school and preschool age. Most often they occur with tonsillitis, sinusitis, pneumonia. The main symptom is a thick yellow crust on the lips. At the same time, the lips stick together, the mouth opens with difficulty. The temperature usually rises. Bacterial stomatitis in a child most often occurs due to weakened immunity in the autumn-winter period.
Most often they occur with tonsillitis, sinusitis, pneumonia. The main symptom is a thick yellow crust on the lips. At the same time, the lips stick together, the mouth opens with difficulty. The temperature usually rises. Bacterial stomatitis in a child most often occurs due to weakened immunity in the autumn-winter period.
Traumatic stomatitis in a child is caused by mechanical trauma to the oral cavity. For example, burns from hot food, a too hard nipple, the habit of chewing on a pencil. Also, traumatic stomatitis often occurs in children with malocclusion due to frequent biting of the cheeks and tongue.
Candidal stomatitis occurs in children under one year old. The cause is Candida fungus. The milk left in the baby's mouth after breastfeeding is an excellent breeding ground for them. Therefore, parents call candidal stomatitis in children thrush. The main symptom is the appearance of white plaque in the baby's mouth. It is worth noting that this plaque should not be confused with the usual plaque after feeding. A cause for alarm is if the plaque does not go away, and the child refuses to eat.
A cause for alarm is if the plaque does not go away, and the child refuses to eat.
Drug-induced or allergic stomatitis in children is caused by some type of allergy or drug reaction. In case of suspicion of this type of disease, the allergen should be identified and removed, otherwise there is a risk of getting unpleasant consequences, up to anaphylactic shock.
Symptoms of stomatitis in children
For all types of stomatitis, a common and defining symptom is inflammation of the oral mucosa and the appearance on any of its parts, such as the tongue, the inside of the lips, cheeks, throat of various formations in the form of sores, vesicles, characteristic plaque, vesicles (blistering rashes) and in cases of traumatic stomatitis - burns, bites, injuries. It is important to understand that stomatitis is not one acute or chronic disease with certain classic symptoms, each type has its own special cause, and they manifest themselves in the oral cavity in different ways, therefore, they need to be treated differently.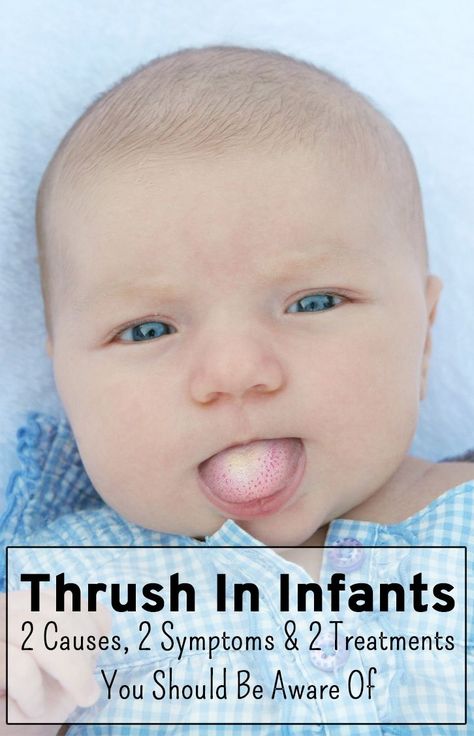
Treatment of stomatitis in children
There is no single algorithm for the treatment of stomatitis in children. Each case is individual in its own way. It often happens when a mother comes in the hope that the doctor will prescribe an ointment, and she will immediately cure her child with it. This does not happen! It is necessary to understand what preceded the inflammation, taking into account the age of the child, the stage and severity of the disease. Treatment is carried out both locally and symptomatically, i.e. symptoms are relieved. Doctors dentist-therapist and pediatrician give their recommendations, it is possible to involve highly specialized specialists, such as ENT, mycologist, dermatologist. Of course, there are some textbook principles that guide specialists in order to relieve or relieve pain or prevent complications. We are talking about compliance with the rules of oral hygiene, diet and sleep, treatment of the mucous membrane with special gels, solutions and applications. For example, with allergic stomatitis in children, antihistamines are recommended, with herpetic forms - antiviral, if there is a temperature - it is antipyretic. It is important that when you find a problem, contact a specialist without delay.
For example, with allergic stomatitis in children, antihistamines are recommended, with herpetic forms - antiviral, if there is a temperature - it is antipyretic. It is important that when you find a problem, contact a specialist without delay.
Caring for a child with stomatitis
Parental involvement in treatment and proper care of the child are not only important, they are decisive. With stomatitis, it is necessary to strictly follow the treatment plan, which is often very laborious, so the result depends on parental care and control. The oral cavity is a kind of epicenter of pain, so it is not surprising that the child will be capricious a lot. Therefore, it is important for parents to stock up on patience and perseverance.
Most moms and dads are concerned about how to feed a child with stomatitis. Firstly, it is necessary to consume only soft, warm (not hotter than 30 degrees) and mushy food, for example, in the form of mashed potatoes. The main thing is that the food is high-calorie and positive, because the child's immunity is already weakened. After eating, it is imperative to rinse your mouth so as not to provoke the development of stomatitis and not to attach any additional infection. A diet for stomatitis in a child should be with the exclusion from the diet of spicy, sour, sweet foods and citrus fruits.
After eating, it is imperative to rinse your mouth so as not to provoke the development of stomatitis and not to attach any additional infection. A diet for stomatitis in a child should be with the exclusion from the diet of spicy, sour, sweet foods and citrus fruits.
Children with stomatitis need to be anesthetized. It is carried out with the help of various medications in order to avoid refusal of food and deterioration of sleep. In addition, with stomatitis in children, proper treatment of the oral cavity is very important. How to handle and rinse the child's mouth should be recommended by the doctor.
Prevention of stomatitis in children
If a person had stomatitis at least once in his life, there will always be a risk of its recurrence, therefore, prevention comes to the fore - in general, strengthening immunity in order to prevent the disease from returning. Both parents and children should follow simple rules of oral hygiene. Obligatory observation at the dentist 2 - 3 times a year, even eating the child does not bother anything. It is advisable, when choosing personal hygiene products, to be guided by the recommendations of your attending dentist. With the onset of recovery, after the end of the disease, it is necessary to replace personal hygiene items, such as a toothbrush, bottles, nipples, etc.
It is advisable, when choosing personal hygiene products, to be guided by the recommendations of your attending dentist. With the onset of recovery, after the end of the disease, it is necessary to replace personal hygiene items, such as a toothbrush, bottles, nipples, etc.
Remember, the main thing is to eliminate the cause of stomatitis. Therefore, the child simply needs to be shown to the doctor. Only he can say how to treat children's stomatitis. Self-medication can only aggravate the course of the disease and prolong the suffering of your baby.
Pimples on the child's tongue: causes and treatment of pimples
Contents:
- What is it
- Causes
- Treatment
Pimples on the tongue - what is it?
The mucosa in the oral cavity and on the tongue does not have sebaceous glands, so typical pimples cannot form on it. Such formations have two formation mechanisms:
- Under the influence of damaging factors, viruses or bacteria, the mucosal stratification occurs, under the upper layer of which liquid accumulates - small bubbles are formed.
 If such a formation is not infected, then its contents will be transparent, but if an infection has entered its cavity, then suppuration is possible - the bubble turns white. If blood enters the liquid, then such a formation acquires a red or dark hue. Bubbles can open and painful sores form in their place.
If such a formation is not infected, then its contents will be transparent, but if an infection has entered its cavity, then suppuration is possible - the bubble turns white. If blood enters the liquid, then such a formation acquires a red or dark hue. Bubbles can open and painful sores form in their place. - Sometimes, in response to inflammation, cells on the surface of the tongue begin to actively divide and exfoliate. Whitish or red formations are formed that resemble ordinary pimples, but at the same time they are only enlarged papillae.
Causes of pimples
There are many reasons for the appearance of such formations on the child's tongue. Let's try to understand each of them in more detail.
Injuries of the tongue
Babies after three months of age begin to actively explore the world around them, including trying to taste everything. But not always those objects that fall into the child's mouth are sterile. Older children often have a habit of chewing on sharp objects, which can also scratch or injure the tongue. Even a slight injury to the mucous membranes, combined with the ingress of microbes, can provoke an inflammatory reaction and the appearance of painful pimples, which are often localized on the tip of the tongue.
Even a slight injury to the mucous membranes, combined with the ingress of microbes, can provoke an inflammatory reaction and the appearance of painful pimples, which are often localized on the tip of the tongue.
Candidiasis or thrush
In children under one year old, the immune system is not fully formed, so any disease leads to a decrease in the protective properties of the body. The consequence of this is candidiasis in the oral cavity - active growth on the mucous membranes of fungi of the genus Candida, which can also be provoked by taking antibiotics. One of the typical manifestations of thrush is the appearance of pimples and curdled white plaque on the entire tongue surface with their spread to the entire oral cavity. If you remove such a plaque, you can find redness, swelling and even the appearance of small ulcers under it.
Stomatitis
With stomatitis on the root of the tongue at its base, on its lateral surfaces or at the tip, a large number of small white pimples appear, which are very painful and cause discomfort during eating or talking. Such pimples can merge to form extensive ulcers. In severe cases, the general poor health of the child and high body temperature are characteristic.
Such pimples can merge to form extensive ulcers. In severe cases, the general poor health of the child and high body temperature are characteristic.
Allergies
Children under two years of age are more likely than adults to experience allergic reactions. One of the manifestations of allergies is the appearance of small whitish or red pimples on the tongue. They can be located both at the tip and in the region of the root of the tongue and move to other parts of the oral mucosa: lips, gums, palate. Most often, such formations disturb the child, itch and cause pain when eating and swallowing. But at the same time, an increase in body temperature is not characteristic.
An increase in allergy symptoms and the appearance of new pimples is caused by the ingestion of a product to which there is an increased sensitivity. Often the cause of these allergic reactions is toothpaste or other oral care products, even if they are recommended for use in children.

Angina
A bacterial infection that affects the tonsils in children can also spread to the lymphoid tissue, which is located at the root of the tongue closer to the throat. This is accompanied by the appearance of white acne with a purulent coating in the area of the tongue. When the pus is removed, areas with redness and slight swelling are exposed. The formations are painful, interfere with normal swallowing and significantly worsen the child's well-being: he becomes capricious, refuses to eat, his body temperature rises. Often, in the presence of such pimples near the throat, enlarged lymph nodes can be felt.
Herpes infection
Infection with the herpes virus most often occurs in childhood and with a decrease in the body's immune defense, the infection can worsen. At the same time, watery small pimples appear on the tongue on a red background, which can also be on the lips and throat of the child. They are very painful and after opening them, shallow sores appear that prevent the child from eating and talking normally.
Dysbacteriosis and unbalanced nutrition
Errors in the nutrition of a child, especially of a younger age, as well as violations of the normal composition of the intestinal microflora can lead to glossitis - inflammation of the mucous membrane of the tongue. This leads to the fact that the epithelium of the papillae begins to actively divide, they take the form of inflamed red or whitish pimples. They rarely bother the child, the sensitivity to hot, cold or sour food can only change.
Treatment
In the treatment of pimples on the tongue, regardless of the reasons that caused their appearance, there are common points:
- Compulsory meticulous oral hygiene. After each meal, it is desirable to treat pimples with an antiseptic solution.
- Exclusion from the child's diet of any irritating factors: spicy, hot or sour food. It is desirable that the food be soft and not cause additional injury to the mucosa.
- In no case should you squeeze or open pimples, this can lead to the development of complications in the child and aggravation of his condition.