When is an ultrasound performed during pregnancy
Fetal ultrasound - Mayo Clinic
Overview
2D fetal ultrasound
2D fetal ultrasound
A 2D fetal ultrasound can help your health care provider evaluate your baby's growth and development.
A fetal ultrasound (sonogram) is an imaging technique that uses sound waves to produce images of a fetus in the uterus. Fetal ultrasound images can help your health care provider evaluate your baby's growth and development and monitor your pregnancy. In some cases, fetal ultrasound is used to evaluate possible problems or help confirm a diagnosis.
The first fetal ultrasound is usually done during the first trimester to confirm the pregnancy and estimate how long you've been pregnant. If your pregnancy remains uncomplicated, the next ultrasound is typically offered during the second trimester, when anatomic details are visible. If a problem is suspected, a follow-up ultrasound or additional imaging tests, such as an MRI, might be recommended.
There are two main types of fetal ultrasound exams:
- Transvaginal ultrasound. With this type of fetal ultrasound, a wandlike device called a transducer is placed in your vagina to send out sound waves and gather the reflections. Transvaginal ultrasounds are used most often during early pregnancy. This type of ultrasound also might be done if a transabdominal ultrasound didn't provide enough information.
- Transabdominal ultrasound. A transabdominal fetal ultrasound is done by moving a transducer over your abdomen.
Various other types of transabdominal ultrasounds are available, including:
- Specialized sonographic evaluation. This type of exam might be needed in specific circumstances, such as when a fetal abnormality is known or suspected. In this situation, a more detailed evaluation can provide additional information about the abnormality.
- 3D ultrasound. This exam provides a two-dimensional display of three-dimensional data.
 This type of ultrasound is sometimes used to help health care providers detect facial abnormalities or neural tube defects.
This type of ultrasound is sometimes used to help health care providers detect facial abnormalities or neural tube defects. - Doppler ultrasound. A Doppler ultrasound measures slight changes in the ultrasound waves as they bounce off moving objects, such as blood cells. It can provide details about a baby's blood flow.
- Fetal echocardiography. This exam provides a detailed picture of a baby's heart. It might be used to confirm or rule out a congenital heart defect.
Products & Services
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Book: Obstetricks
Why it's done
First trimester ultrasound examination is done to evaluate the presence, size and location of the pregnancy, determine the number of fetuses, and estimate how long you've been pregnant (gestational age). Ultrasound can also be used for first trimester genetic screening, as well as screening for abnormalities of your uterus or cervix.
In the second or third trimester a standard ultrasound is done to evaluate several features of the pregnancy, including fetal anatomy. This exam is typically done between weeks 18 and 20 of pregnancy. However, the timing of this ultrasound might be altered for reasons such as obesity, which could limit visualization of the fetus.
During the second and third trimesters, limited ultrasound evaluation might be needed when a specific question requires investigation. Examples include the evaluation of fetal growth and the estimation of amniotic fluid volume. A specialized or detailed exam is done when an anomaly is suspected based on your history or other prenatal exam results.
Your health care provider might use fetal ultrasound to:
- Confirm the pregnancy and its location. Some fetuses develop outside of the uterus, in the fallopian tube. A fetal ultrasound can help your health care provider detect a pregnancy outside of the uterus (ectopic pregnancy).

- Determine your baby's gestational age. Knowing the baby's age can help your health care provider determine your due date and track various milestones throughout your pregnancy.
- Confirm the number of babies. If your health care provider suspects a multiple pregnancy, an ultrasound might be done to confirm the number of babies.
- Evaluate your baby's growth. Your health care provider can use ultrasound to determine whether your baby is growing at a normal rate. Ultrasound can be used to monitor your baby's movement, breathing and heart rate.
- Study the placenta and amniotic fluid levels. The placenta provides your baby with vital nutrients and oxygen-rich blood. Too much or too little amniotic fluid — the fluid that surrounds the baby in the uterus during pregnancy — or complications with the placenta need special attention. An ultrasound can help evaluate the placenta and amniotic fluid around the baby.

- Identify birth defects. An ultrasound can help your health care provider screen for some birth defects.
- Investigate complications. If you're bleeding or having other complications, an ultrasound might help your health care provider determine the cause.
- Perform other prenatal tests. Your health care provider might use ultrasound to guide needle placement during certain prenatal tests, such as amniocentesis or chorionic villus sampling.
- Determine fetal position before delivery. Most babies are positioned headfirst by the end of the third trimester. That doesn't always happen, though. Ultrasound imaging can confirm the baby's presentation so that your health care provider can discuss options for delivery.
Fetal ultrasound should be done only for valid medical reasons. Fetal ultrasound isn't recommended only to determine a baby's sex. Similarly, fetal ultrasound isn't recommended solely for the purpose of producing keepsake videos or pictures.
If your health care provider doesn't suggest a fetal ultrasound but you'd like the reassurance an ultrasound can provide, share your wishes with your care provider so that you can work together to determine what's best for you and your baby.
More Information
- Prenatal testing: Quick guide to common tests
- Hypoplastic left heart syndrome
- Preeclampsia
Request an Appointment at Mayo Clinic
Risks
Diagnostic ultrasound has been used during pregnancy for many years and is generally considered safe when used appropriately. The lowest amount of ultrasound energy that provides an accurate assessment should be used.
Fetal ultrasound also has limitations. Fetal ultrasound might not detect all birth defects — or might incorrectly suggest a birth defect is present when it's not.
How you prepare
You might be asked to drink a certain amount of fluid or avoid urinating before a fetal ultrasound, depending on the type of ultrasound. When scheduling your ultrasound, ask your health care provider for instructions.
When scheduling your ultrasound, ask your health care provider for instructions.
Also be aware that fetal ultrasound can be done through the vagina (transvaginal) or over the abdomen (transabdominal), depending on why it's being done or the stage of your pregnancy. If you're having a transabdominal ultrasound, consider wearing loosefitting clothing so that you can easily expose your abdomen.
What you can expect
During the procedure
During a transabdominal fetal ultrasound, you'll recline on an exam table and expose your abdomen. Your health care provider or technician will apply a special gel to your abdomen. This will improve the conduction of sound waves and eliminate air between your skin and the transducer.
Your health care provider or technician will move or scan the transducer back and forth over your abdomen. The sound waves reflected off your bones and other tissues will be converted into images on a monitor.
Your health care provider or technician will measure your baby's anatomy. He or she might print or store certain images to document important structures. You'll likely be given copies of some of the images.
He or she might print or store certain images to document important structures. You'll likely be given copies of some of the images.
Depending on your baby's position and stage of development, you might be able to make out a face, hands and fingers, or arms and legs. Don't worry if you can't "see" your baby. Ultrasound images can be hard for an untrained observer to decipher. Ask your health care provider or technician to explain what's on the screen.
The procedure for other types of fetal ultrasound exams is similar. If you're having a transvaginal ultrasound, however, you'll be asked to change into a hospital gown or undress from the waist down. You'll recline on an exam table and place your feet in stirrups. The transducer will be covered in a plastic sheath, like a condom, and be lubricated with gel. Your health care provider or technician will place the transducer in your vagina.
After the procedure
You can wipe off any residual gel or lubricant. If you had a full bladder during the ultrasound, you can urinate after the exam.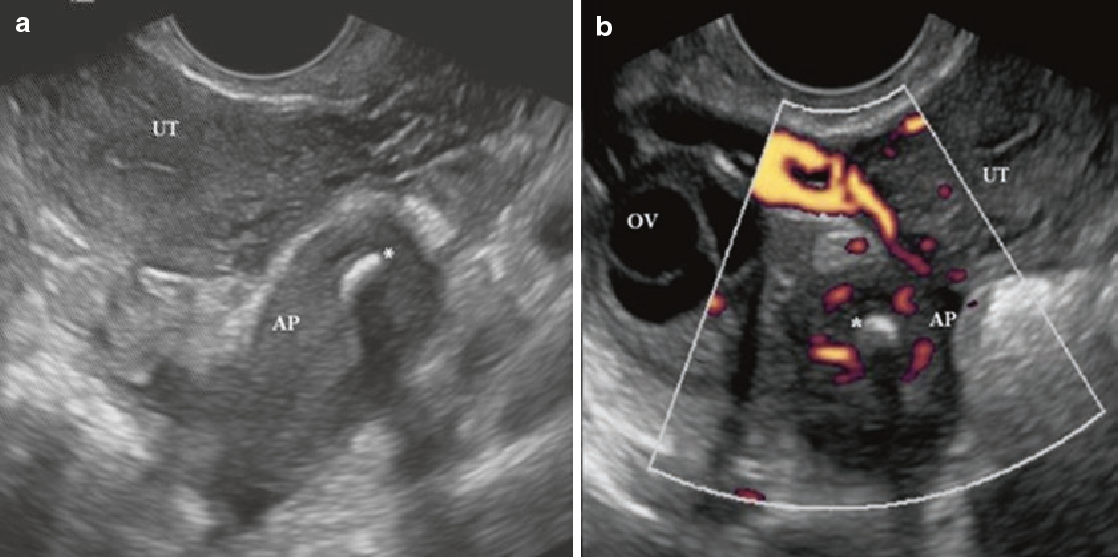
Results
3D fetal ultrasound
3D fetal ultrasound
A 3D fetal ultrasound can detect facial abnormalities or neural tube defects.
Typically, a fetal ultrasound offers reassurance that a baby is growing and developing normally. If your health care provider wants more details about your baby's health, he or she might recommend additional tests.
By Mayo Clinic Staff
Related
Products & Services
What Every Mom-To-Be Needs to Know
Moms-to-be typically look forward to ultrasounds during pregnancy more than any other prenatal appointment. It’s easy to see why! It’s fun to get a sneak peek of your bundle of joy while your OBGYN looks for specific growth and development markers. Many women look forward to learning their baby’s sex as soon as possible and wait impatiently for their 20-week ultrasound. Others want to be surprised. Whether or not you intend to learn about your baby’s sex ASAP, it’s important to keep all your ultrasound appointments.
An ultrasound, also known as a sonogram, is typically performed by an ultrasound technician or sometimes by an OBGYN. It uses sound waves to create an image of the organs inside your body. (These sound waves are not harmful to you or your baby.) Ultrasounds during pregnancy help doctors diagnose many diseases and conditions, even those not related to pregnancy.
This article will cover why and how ultrasounds are used during your pregnancy, how many ultrasounds to expect while you’re pregnant, and what your OBGYN may be looking for at each ultrasound.
Most pregnant women typically only get two ultrasounds, one at the beginning of pregnancy and one about halfway through. Other women may have three or more ultrasounds done depending on a number of factors.
Your First Ultrasound
Your first ultrasound is called the “dating” or “viability” ultrasound. It’s typically done between 7 and 8 weeks to verify your due date, to look for a fetal heartbeat, and to measure the length of the baby from “crown to rump. ” At this ultrasound, you’ll also learn whether you’re having one baby, pregnant with twins, or more! You may even get to see or hear your baby’s heartbeat during this appointment.
” At this ultrasound, you’ll also learn whether you’re having one baby, pregnant with twins, or more! You may even get to see or hear your baby’s heartbeat during this appointment.
If you have irregular periods, or didn’t have a period after coming off birth control, this ultrasound will be especially helpful in determining a more accurate due date. Your due date is important because it helps your doctor know whether your baby’s development is on track each month.
We’ll perform this ultrasound at our Madison Women’s Health clinic.
What to Expect at Your First Ultrasound
When you’re just 7 or 8 weeks pregnant, your fetus is only about two centimeters long. In order to get a close enough view of your uterus and fetus, the dating ultrasound is done transvaginally. This means the ultrasound is done internally, literally “through the vagina.” A transvaginal ultrasound can be a little uncomfortable, but it is not painful. Most would say it feels less invasive than a gynecological exam that uses a speculum.
To perform this ultrasound, your OBGYN or ultrasound tech will gently insert a narrow ultrasound wand just inside your vagina. The transvaginal ultrasound wand is also called a transducer. It’s about three centimeters around, a little larger than a tampon. It will be covered by a condom and lubricant. The wand will not reach your cervix and is safe for your baby.
You may be asked to arrive at your first ultrasound with a full bladder. Having a fuller bladder helps to put your uterus in a better position for the ultrasound.
What Your Doctor is Looking for at Your First Ultrasound
- Viability of pregnancy
- Fetal heartbeat
- Fetal size
- Single or multiple pregnancy
Genetic Screening Ultrasound
If you choose to have prenatal genetic testing done, you’ll have your next ultrasound at 12 to 13 weeks gestation. This ultrasound is also called nuchal translucency screening. It’s offered to everyone and is covered by most insurance plans. This genetic screening ultrasound is optional.
It’s offered to everyone and is covered by most insurance plans. This genetic screening ultrasound is optional.
During this ultrasound, your doctor will look for indicators of chromosomal disorders. Chromosomal disorders mean that the baby received an extra chromosome at conception and could have moderate to extreme physical or mental challenges. These disorders include:
- Trisomy 21, known as Down Syndrome
- Trisomy 13
- Trisomy 18
Read more about carrier screening and prenatal genetic testing.
What Your Doctor is Looking for at the Genetic Screening Ultrasound
This ultrasound will be an anatomical scan. Your doctor will look to see if all four limbs are present. They will also look for basic structures in the brain, the stomach, the bladder, the nasal bone, and last but not least, something called nuchal translucency. Nuchal translucency is a fluid sack at the back of the baby’s neck that is filled with lymphatic fluid. There are correlations between the size of that sack of fluid and the likelihood that the fetus could be affected by a major chromosomal disorder.
There are correlations between the size of that sack of fluid and the likelihood that the fetus could be affected by a major chromosomal disorder.
After the ultrasound has been performed, your OBGYN will interpret the results and share the information with you. You may also meet with a genetic counselor who could recommend having additional tests done to verify the ultrasound results.
Keep in mind that ultrasound screenings for other genetic disorders or anatomic abnormalities become more accurate further into the pregnancy.
We’ll perform this ultrasound at the Madison Women’s Health clinic.
Should you Get a Genetic Screening Ultrasound?
There’s no right or wrong answer to this question. Ultimately, the decision is up to you. Here are some good questions to ask yourself as you decide whether to have the genetic screening:
- Is there a family history of these genetic birth disorders?
- Would I terminate my pregnancy if there was a risk of Downs Syndrome, Trisomy 13, Trisomy 18, or other genetic disorder?
- Would knowing about my pregnancy’s risk of genetic defect make it easier to emotionally or physically prepare for a baby with a birth defect?
- Would it be easier for me to cope with and enjoy pregnancy if I focus on the more likely positive outcome rather than the chance of birth defects?
Whether you choose to have genetic screening done at this time is entirely your decision. Some women prefer to have as much information as possible as early as possible, while other women do not. If you’re still uncertain, you can discuss the pros and cons with your OBGYN.
Some women prefer to have as much information as possible as early as possible, while other women do not. If you’re still uncertain, you can discuss the pros and cons with your OBGYN.
Basic Anatomy Scan Ultrasound
This is the ultrasound that people look forward to the most! The full anatomy ultrasound is typically performed at about 20 weeks, or 5 months. As the name implies, this ultrasound will look at all the baby’s organ systems to make sure they’re present, are a normal size and shape, and are in the right location.
What to Expect at a Full Anatomy Scan Ultrasound
The full anatomy scan is a transabdominal ultrasound. It uses a transducer that looks a lot like a store checkout scanner. The ultrasound technician will put warm ultrasound gel on your stomach and then slide the transducer in the gel around your stomach. The gel helps the sound waves travel through your skin.
Tip: Come to your appointment with a relatively full bladder. This will make it easier for your ultrasound technician to get better images of your baby.
Because there are so many things to look for, this ultrasound will take at least 45 minutes—if your little one cooperates! If you’ve got an extra squirmy baby who is “camera shy,” it could take a few hours to get all the images that we need. Don’t worry, we have a lot of tricks to encourage your baby to change positions—everything from asking you to lay on one side and then the other, emptying your bladder or filling it, maybe even walking around. We’ll do whatever it takes to get the images we need to track your baby’s growth and development.
What Your OBGYN is Looking for at a Full Anatomy Scan
During the full anatomy, 20-week ultrasound, you can find out if your baby is male or female. If you want the sex to be a surprise, be sure to tell your technician know ahead of time so they don’t accidentally let it slip. When the scan is complete, Meriter will even send you a link to view some fun photos of your baby!
Your ultrasound technician will capture a large number images and measurements:
- limbs: arms, legs, feet, hands
- torso: chest, heart, kidneys, stomach, bladder, diaphragm, genitals
- head and face
- spine
- umbilical cord
- amount of amniotic fluid
- location, size, and shape of your placenta
- length of your cervix
After your ultrasound technician has captured all these images and measurements, your OBGYN will review the pictures and look for abnormalities such as congenital heart defects or cleft lip or palate. They’ll discuss their findings with you and help you understand what you’re looking at in the different images.
They’ll discuss their findings with you and help you understand what you’re looking at in the different images.
If everything looks normal and there are no other issues during your pregnancy, the next time you’ll see your baby is when he or she is in your arms! In the meantime, you can enjoy those 2D or 3D photos of your baby!
This ultrasound will be performed at UnityPoint Health – Meriter Hospital Center for Perinatal Care.
“Extra” Ultrasounds
Sometimes, women need additional ultrasounds during pregnancy. Your OBGYN may ask you to come in for additional ultrasounds to check your:
- Cervical length: if your cervix is shorter than expected, you may need to have your cervix checked regularly to be sure it stays closed so that you can maintain your pregnancy. If the cervix continues to shorten or thin, you may need a cerclage to help strengthen it until it’s time to deliver your baby. Cervical length ultrasounds occur at 16, 18, 20 and 22 weeks and are done transvaginally.

- Placental location and size: if your placenta is too small, if it is in an abnormal location or if it is an abnormal shape, then we will need to monitor it and the growth of your baby with regular ultrasounds. Your placenta is responsible for passing blood and nutrients to your baby, so it’s important thrat it is growing correctly.
You may need growth ultrasounds if you have:
- hypertension
- diabetes
- high BMI (body mass index) going into pregnancy
- preeclampsia
- indicators that your placenta or uterus is not growing appropriately
Sometimes, growth ultrasounds are needed to check that your baby’s growth is continuing along the growth curve. They’re done at 28, 32, and 36 weeks. One way doctors estimate whether your baby is growing as expected is by measuring your fundal height. Fundal height is the number of centimeters from your pubic bone to the top of your uterus. This measurement typically increases about 1 cm each week. If your uterus has not grown appropriately in the last month, your OBGYN will surmise that your baby is also not growing and will want to perform monthly growth ultrasounds.
This measurement typically increases about 1 cm each week. If your uterus has not grown appropriately in the last month, your OBGYN will surmise that your baby is also not growing and will want to perform monthly growth ultrasounds.
What to Expect at a Growth Ultrasound
These ultrasounds take less time than the full basic anatomy ultrasound because there are fewer measurements required. The ultrasound technician will measure the baby’s head circumference, bi-parietal diameter, abdominal circumference, and femur length.
What Your OBGYN is Looking for at Growth Ultrasounds
Your OBGYN is looking to see if your baby is staying on its growth curve. We will also use the measurements to estimate your baby’s weight. A large or extra large baby isn’t typically concerning. An extra-small baby or a baby who does not grow according to their growth curve could mean that the baby is not getting enough nourishment through the placenta and may need to be delivered early.
2D, 3D, and 4D Ultrasounds
2D ultrasounds are the black and white images that you’re probably used to seeing. To an untrained eye, they can look pretty fuzzy or obscure. However, they give the best definition of the structures of your growing peanut and are considered the “gold standard” of diagnostic imaging.
To an untrained eye, they can look pretty fuzzy or obscure. However, they give the best definition of the structures of your growing peanut and are considered the “gold standard” of diagnostic imaging.
3D images are especially popular among parents-to-be who want to enjoy those cute baby pictures even before the baby is born! These pictures show facial features and look much more baby-like than the kind of obscure 2D images. 3D ultrasounds have usefulness beyond the cuteness factor, however! In the case of abnormalities of the spine or palate, 3D ultrasounds can help your OBGYN get a better idea of the severity.
4D images are like a 3D image, but show the baby moving around. They’re like getting to see a live action video of your little one. These are less commonly done because they don’t actually help with diagnoses. Depending on which perinatal center you go to, you might receive a link to view your ultrasound images or videos online.
While there are some stand-alone ultrasound centers offering to tell you your baby’s sex early on or to give you keepsake 3D or 4D images, these aren’t necessary and are rarely covered by insurance. You’ll find out everything you need to know during your appointments at the perinatal center — and those appointments will be covered by your insurance.
You’ll find out everything you need to know during your appointments at the perinatal center — and those appointments will be covered by your insurance.
The best place to have an ultrasound performed is always at a clinic, where you will have access to a physician who has been trained in interpreting the images. At Madison Women’s Health, we’re happy to print off pictures for you to put in your baby’s scrapbook — or anywhere else you’d like to display those “coming soon” photos.
Final Thoughts
Ultrasounds during pregnancy are a fascinating way to get a glimpse of your developing baby. Don’t be afraid to ask your OBGYN for more details about genetic screening as you determine whether that is something you want done. And make sure you’ve set aside a good amount of time for your ultrasounds — especially the all-important full anatomy scan!
—
Dr. Beth Wiedel has been providing healthcare to women in Madison since 2002 and is a founding partner of Madison Women’s Health. She shares the vision of all the partners of being a strong healthcare advocate for her patients, emphasizing compassion and communication throughout her practice.
She shares the vision of all the partners of being a strong healthcare advocate for her patients, emphasizing compassion and communication throughout her practice.
When to do the first ultrasound during pregnancy - "happy days" for screening of the 1st trimester
The world of a modern woman is always full of important events, meetings and an endless series of pre-planned things. When pregnancy occurs, many planned events can be moved from “expected” to “impossible” or simply postponed indefinitely. It is quite difficult to worry in advance and reschedule an important event at the most appropriate time, because planning events against the backdrop of pregnancy is a very difficult science.
Therefore, when pregnancy occurs, it is advisable to draw up at least an approximate “life plan for 9 months”. For example, it is known that maternity leave is most often preceded by unspent regular leave, and registration for pregnancy is preceded by the fact that a pregnancy has occurred and is developing normally.
Many events will now depend on how the new life develops. So, when a multiple pregnancy is diagnosed, not only the estimated due date will change, but maternity leave will come 14 days earlier, and the beginning of unspent leave will move with it. Therefore, one of the first steps in the event of a desired pregnancy is the passage of an ultrasound examination (ultrasound). Scientific and technological progress is rapidly changing the whole world, including the state of the prenatal ultrasound diagnostic service. Opportunities are changing, and with them the timing of the passage of research, which I would like to dwell on in more detail.
When to do an ultrasound scan during pregnancy
In 2012, the regulation “Decree of the Health Committee of the Government of St. Petersburg No. 39-r”1 came into force in St. Petersburg. Based on the above document, for a full-fledged ultrasound screening, it is desirable to undergo a study in “. .. the first trimester: 11 + 0-13 + 6 weeks; 18+0-20+6 weeks; and 32+0-34+6 weeks of pregnancy.” However, these terms apply only to uncomplicated singleton pregnancies. At the same time, early registration is limited to up to 12 weeks of pregnancy with the ensuing consequences (payment of a lump-sum allowance to women registered in medical institutions in the early stages of pregnancy, clause 2-c of Decree of the Government of the Russian Federation of October 15, 2001 N 727 (as amended on 04.09.2012).
.. the first trimester: 11 + 0-13 + 6 weeks; 18+0-20+6 weeks; and 32+0-34+6 weeks of pregnancy.” However, these terms apply only to uncomplicated singleton pregnancies. At the same time, early registration is limited to up to 12 weeks of pregnancy with the ensuing consequences (payment of a lump-sum allowance to women registered in medical institutions in the early stages of pregnancy, clause 2-c of Decree of the Government of the Russian Federation of October 15, 2001 N 727 (as amended on 04.09.2012).
Therefore, at 11 weeks, a pregnant woman can be registered when establishing the fact of a developing pregnancy , for which ultrasound "... in the first trimester" is recommended. Most doctors recommend doing it at terms 7-8 weeks of pregnancy , because it is at this time that the heartbeat of a developing embryo is always determined as a sign of the physiological development of pregnancy.
The next obligatory steps in the ultrasound are screening. The entire pregnancy is divided into three periods (trimesters) and ultrasound plays an important role in each.
The entire pregnancy is divided into three periods (trimesters) and ultrasound plays an important role in each.
What is the diagnostic window for ultrasound during pregnancy
The first screening study is carried out from 11 weeks 0 days of pregnancy to 13 weeks 6 days of pregnancy. These limits are adopted for the timely detection of pathological conditions that determine the prognosis for the health of the fetus. Theoretically, any pregnant woman can apply for an ultrasound both at the beginning of the eleventh and at the end of the thirteenth week - the entire period is screening. However, among doctors who have dedicated their lives to prenatal ultrasound diagnostics, there is an opinion about the most preferable period in each screening period - the so-called " diagnostic window" or "happy days" .
Terms of fetal ultrasound examination
| Legally regulated period (order KZ SPb No.  39-r dated 02/01/12) 39-r dated 02/01/12) | Optimal timing/happy days |
| - | 7-8 |
| 11 weeks 0 days – 13 weeks 6 days | 12 weeks 2 days - 12 weeks 4 days |
| 18 weeks 0 days – 20 weeks 6 days | 20 weeks 0 days - 20 weeks 6 days |
| 32 weeks 0 days – 34 weeks 6 days | 32 weeks 0 days - 33 weeks 3 days |
Diagnostic window in the 1st trimester of pregnancy
For the first screening study, these days include the interval from 12 weeks to 12 weeks. 2 days to 12 weeks 4 days . It is in this interval that the fetus has already grown enough to evaluate the smallest organs (eye lenses, heart), and the probability of ascertaining the most important morphological changes is significantly higher than at 11 weeks 0 days. On the other hand, each day lived by the baby increases not only the height and weight of the body, but the quality of the picture on the ultrasound machine.
On the other hand, each day lived by the baby increases not only the height and weight of the body, but the quality of the picture on the ultrasound machine.
According to various authors, the frequency of congenital pathology reaches 5%, and for patients in this group it is especially important to identify the problem at an early stage. In such special cases, it may be necessary to expand the range of diagnostic procedures, including prenatal karyotyping (obtaining samples of fetal tissue or amniotic structures in order to determine its karyotype). It takes time to carry out these procedures, from preparing the necessary tests for a pregnant woman, ending with directly invasive diagnostics and obtaining results about the health of the fetus.
In some cases, the established disease of the fetus raises the question of the impossibility of prolonging the pregnancy. According to the current legislation of the Russian Federation, the procedure of medical termination of pregnancy by the decision of the woman can be performed ". .. no later than the end of the twelfth week of pregnancy", but "... not earlier than 48 hours from the moment the woman applied to the medical organization for artificial termination of pregnancy" (clause 3.1, clause 3-b of article 56. Federal Law No. 323 of November 21, 2012)2. In other words, if a patient goes for an ultrasound scan at 12 weeks 5 days, if a serious pathology is detected, she is no longer sent for an artificial medical abortion, but for an abortion, which is a more complex and traumatic procedure. Therefore, when asked about the best rock for the first screening, almost any practitioner will answer: "up to 12 weeks 4 days" .
.. no later than the end of the twelfth week of pregnancy", but "... not earlier than 48 hours from the moment the woman applied to the medical organization for artificial termination of pregnancy" (clause 3.1, clause 3-b of article 56. Federal Law No. 323 of November 21, 2012)2. In other words, if a patient goes for an ultrasound scan at 12 weeks 5 days, if a serious pathology is detected, she is no longer sent for an artificial medical abortion, but for an abortion, which is a more complex and traumatic procedure. Therefore, when asked about the best rock for the first screening, almost any practitioner will answer: "up to 12 weeks 4 days" .
Diagnostic window in the 2nd trimester of pregnancy
The second screening period occurs at 18 weeks. 0 days and ends at 20 weeks 6 days pregnant . "Lucky days" is considered the entire twentieth week: 20 weeks. 0 days - 20 weeks 6 days . Not all the subtleties of the architectonics of the main organs can be considered so successfully, especially in pregnant women with increased body weight at 18 weeks of pregnancy. If so-called "markers of chromosomal problems" are detected, it may be necessary to perform prenatal karyotyping (obtaining fetal blood or amniotic fluid), which may take some time.
Not all the subtleties of the architectonics of the main organs can be considered so successfully, especially in pregnant women with increased body weight at 18 weeks of pregnancy. If so-called "markers of chromosomal problems" are detected, it may be necessary to perform prenatal karyotyping (obtaining fetal blood or amniotic fluid), which may take some time.
The collection of the material itself takes several minutes, but the preparation of the pregnant woman (examination, obtaining the results of blood and urine tests, etc.), transporting the material to the laboratory, examination and obtaining the results can take several days. If serious deviations in the state of health of the fetus are detected, in order to resolve the issue of further management tactics, the pregnant woman is sent to undergo a prenatal consultation consisting of an ultrasound doctor, a specialist in the field to which the identified disease belongs (for example, a surgeon, neurosurgeon, cardiologist, etc. ) .
) .
Prior to the new regulation, the second screening period ranged from 18-22 weeks, even earlier than 18-24 weeks of pregnancy. According to WHO recommendations, the fetus becomes viable from the 22nd week of pregnancy, therefore, before this period it is very important to obtain all possible information about its condition and form a prognosis for health and later life. That is why now there is a restriction regulated by law, so that if serious problems with the health of the fetus are detected, all additional diagnostic procedures should be carried out in a timely manner and, if necessary, terminate the pregnancy without violating the Legislation of the Russian Federation2.
Diagnostic window in the 3rd trimester of pregnancy
The third screening period (32 weeks 0 days - 34 weeks 6 days of pregnancy) has two main objectives: the exclusion of congenital malformations with late manifestation and assessment of the fetal condition. Issuance of a referral for the passage of the third ultrasound along with maternity leave of 30 weeks. 0 days of pregnancy potentiates untimely early appeal of pregnant women for the third screening ultrasound before the period of 32 weeks 0 days, which in turn may require a second planned ultrasound in the "scheduled time". A later turnout (after 34 weeks) reduces the quality of the ultrasound picture obtained by changing the relationship between the amount of amniotic fluid and the volume of the fetal body towards the latter. Therefore " happy days" the third trimester can be considered the period 32 weeks 0 days - 33 weeks 3 days of pregnancy .
Issuance of a referral for the passage of the third ultrasound along with maternity leave of 30 weeks. 0 days of pregnancy potentiates untimely early appeal of pregnant women for the third screening ultrasound before the period of 32 weeks 0 days, which in turn may require a second planned ultrasound in the "scheduled time". A later turnout (after 34 weeks) reduces the quality of the ultrasound picture obtained by changing the relationship between the amount of amniotic fluid and the volume of the fetal body towards the latter. Therefore " happy days" the third trimester can be considered the period 32 weeks 0 days - 33 weeks 3 days of pregnancy .
Unscheduled ultrasound at any stage is required, as a rule, only in case of complicated pregnancy, therefore, it is prescribed only according to indications and is performed regardless of the gestational age.
Notes: 1 - Order of the Health Committee of the Government of St. Petersburg dated February 1, 2012 N 39-r "On measures to reduce hereditary and congenital diseases in children in St. Petersburg".
Petersburg dated February 1, 2012 N 39-r "On measures to reduce hereditary and congenital diseases in children in St. Petersburg".
2- Article 56 "Artificial termination of pregnancy". Federal Law of the Russian Federation of November 21, 2011 N 323-FZ "On the basics of protecting the health of citizens in the Russian Federation", entered into force: November 22, 2011, published on November 23, 2011 in "RG" - Federal issue No. 5639
Ultrasound of the fetus 1,2,3 trimesters of pregnancy
Ultrasound during pregnancy
Ultrasound examination (ultrasound) during pregnancy is today the safest and most detailed monitoring of fetal development and assessment of the state of the placenta. Ultrasound diagnostics is required for all women during pregnancy, since any married couple has the possibility of various diseases in a child.
How many times to do fetal ultrasound for pregnant women
In 2021, two necessary ultrasound monitorings are being carried out in Russia:
- 1st fetal ultrasound at 11-14 weeks,
- 2nd ultrasound at 19-21 weeks
The specified amount of research can be increased if there is a threat of fetal pathology or abortion.
There is no harm from ultrasound diagnostics!
You can do an ultrasound examination at any stage of pregnancy in Medgard using modern equipment. Leading doctors of ultrasonic diagnostics of Orenburg accept.
First fetal ultrasound at 11-14 weeks gestation
The first screening at 11-14 weeks. optimally carried out at 12-13 weeks of pregnancy. The child is not yet formed, however, on ultrasound, you can see some obvious violations in the development of the embryo. At the 1st ultrasound, a number of indicative markers are examined, among which the indicators of the development of the collar structures of the fetus are considered the most important. These data are refined in order to detect the risk of chromosomal abnormalities in the fetus (for example, Down syndrome, etc.). The collar zone is considered only in the first trimester of pregnancy, i.e. after 14 weeks, these markers are no longer detected. Proceeding from this, it is extremely important to go to the 1st detailed ultrasound screening in time to be sure that the child has no pathologies.
These data are refined in order to detect the risk of chromosomal abnormalities in the fetus (for example, Down syndrome, etc.). The collar zone is considered only in the first trimester of pregnancy, i.e. after 14 weeks, these markers are no longer detected. Proceeding from this, it is extremely important to go to the 1st detailed ultrasound screening in time to be sure that the child has no pathologies.
Second ultrasound at 19-21 weeks of pregnancy
The second ultrasound is performed at 19-21 weeks of pregnancy.
This screening is the main one, because the baby is already almost formed and in this period the main mass of defects and diseases in the fetus is manifested. In addition to a detailed diagnosis of the structure of the fetus, the doctor determines all the important dimensions, assesses the condition of the placenta, the volume of amniotic fluid, blood flow in the uterine arteries and vessels in the child (this technology is called Doppler).
Third fetal ultrasound at 30-33 weeks gestation
Until 2021, there was also a third screening at 30-33 weeks.