Abortion and miscarriage difference
Miscarriage: MedlinePlus Medical Encyclopedia
A miscarriage is the spontaneous loss of a fetus before the 20th week of pregnancy. Pregnancy losses after the 20th week are called stillbirths. Miscarriage is a naturally occurring event, unlike medical or surgical abortions.
A miscarriage may also be called a "spontaneous abortion." Other terms for the early loss of pregnancy include:
- Complete abortion: All of the products (tissue) of conception leave the body.
- Incomplete abortion: Only some of the products of conception leave the body.
- Inevitable abortion: Symptoms cannot be stopped and a miscarriage will happen.
- Infected (septic) abortion: The lining of the womb (uterus) and any remaining products of conception become infected.
- Missed abortion: The pregnancy is lost and the products of conception do not leave the body.
Your health care provider may also use the term "threatened miscarriage." The symptoms of this condition are abdominal cramps with or without vaginal bleeding. They are a sign that a miscarriage may occur.
Most miscarriages are caused by chromosome problems that make it impossible for the baby to develop. In rare cases, these problems are related to the mother's or father's genes.
Other possible causes of miscarriage may include:
- Drug and alcohol abuse
- Clotting disorders
- Exposure to environmental toxins
- Hormone problems
- Infection
- Overweight
- Physical problems with the mother's reproductive organs
- Problem with the body's immune response
- Serious body-wide (systemic) diseases in the mother (such as uncontrolled diabetes)
- Smoking
Around half of all fertilized eggs die and are lost (aborted) spontaneously, usually before the woman knows she is pregnant. Among women who know they are pregnant, about 10% to 25% will have a miscarriage. Most miscarriages occur during the first 7 weeks of pregnancy. The rate of miscarriage drops after the baby's heartbeat is detected.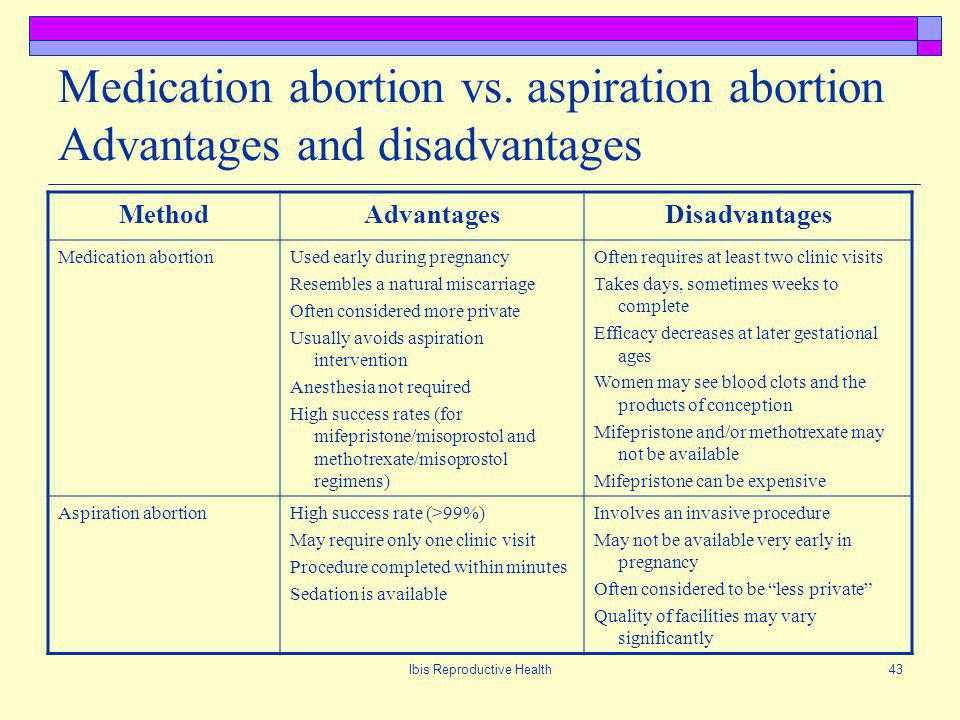
The risk for miscarriage is higher:
- In women who are older -- The risk increases after 30 years of age and becomes even greater between 35 and 40 years, and is highest after age 40.
- In women who have already had several miscarriages.
Possible symptoms of miscarriage may include:
- Low back pain or abdominal pain that is dull, sharp, or cramping
- Tissue or clot-like material that passes from the vagina
- Vaginal bleeding, with or without abdominal cramps
Some women may not have any symptoms at the beginning.
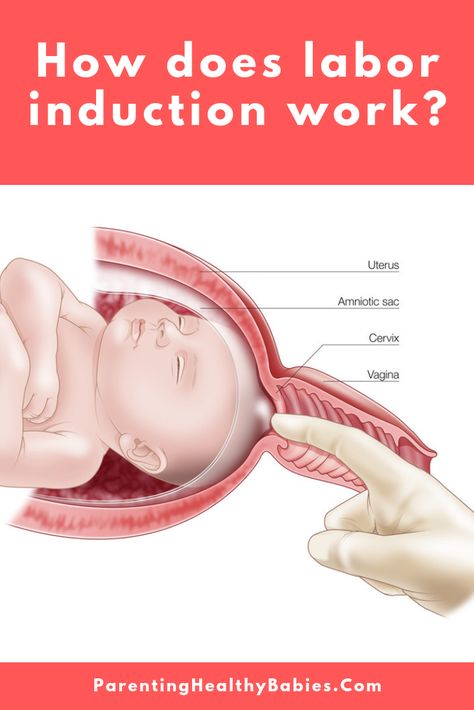
During a pelvic exam, your provider may see that your cervix has opened (dilated) or thinned out (effacement).
Abdominal or vaginal ultrasound may be done to check the baby's development and heartbeat, and the amount of your bleeding.
The following blood tests may be performed:
- Blood type (if you have an Rh-negative blood type, you would require a treatment with Rh-immune globulin).
- Complete blood count (CBC) to determine how much blood has been lost.

- HCG (qualitative) to confirm pregnancy.
- HCG (quantitative) done every several days or weeks.
- White blood count (WBC) and differential to rule out infection.
When a miscarriage occurs, the tissue passed from the vagina should be examined. This is done to determine if it was a normal placenta or a rare condition known as a hydatidiform mole. It is also important to find out whether any pregnancy tissue remains in the uterus. In rare cases an ectopic pregnancy can look like a miscarriage. If you have passed tissue, ask your provider if the tissue should be sent for genetic testing. This can be helpful to determine if a treatable cause of miscarriage is present.
If the pregnancy tissue does not naturally leave the body, you may be closely watched for up to 2 weeks. Surgery (suction curettage, D and C) or medicine may be needed to remove the remaining contents from your womb.
After treatment, women usually resume their normal menstrual cycle within 4 to 6 weeks.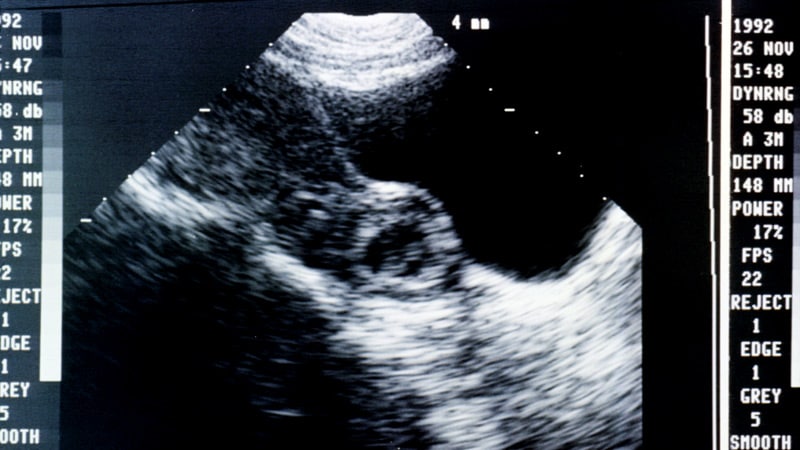 Any further vaginal bleeding should be carefully monitored. It is often possible to become pregnant immediately. It is suggested that you wait one normal menstrual cycle before trying to become pregnant again.
Any further vaginal bleeding should be carefully monitored. It is often possible to become pregnant immediately. It is suggested that you wait one normal menstrual cycle before trying to become pregnant again.
In rare cases, complications of miscarriage are seen.
An infected abortion may occur if any tissue from the placenta or fetus remains in the uterus after the miscarriage. Symptoms of an infection include fever, vaginal bleeding that does not stop, cramping, and a foul-smelling vaginal discharge. Infections can be serious and need immediate medical attention.
Women who lose a baby after 20 weeks of pregnancy receive different medical care. This is called premature delivery or fetal demise. This needs immediate medical attention.
After a miscarriage, women and their partners may feel sad. This is normal. If your feelings of sadness do not go away or get worse, seek advice from family and friends as well as your provider. However, for most couples, a history of a miscarriage doesn't reduce the chances of having a healthy baby in the future.
Contact your provider if you:
- Have vaginal bleeding with or without cramping during pregnancy.
- Are pregnant and notice tissue or clot-like material that passes through your vagina. Collect the material and bring it to your provider for examination.
Early, complete prenatal care is the best prevention for complications of pregnancy, such as miscarriage.
Miscarriages that are caused by systemic diseases can be prevented by detecting and treating the disease before pregnancy occurs.
Miscarriages are also less likely if you avoid things that are harmful to your pregnancy. These include x-rays, recreational drugs, alcohol, high caffeine intake, and infectious diseases.
When a mother's body has difficulty keeping a pregnancy, signs such as slight vaginal bleeding may occur. This means there is a risk for miscarriage. But it does not mean one will definitely occur. A pregnant woman who develops any signs or symptoms of threatened miscarriage should contact her prenatal provider instantly.
Taking a prenatal vitamin or folic acid supplement before you become pregnant can greatly lower the chances of miscarriage and certain birth defects.
Abortion - spontaneous; Spontaneous abortion; Abortion - missed; Abortion - incomplete; Abortion - complete; Abortion - inevitable; Abortion - infected; Missed abortion; Incomplete abortion; Complete abortion; Inevitable abortion; Infected abortion
- Normal uterine anatomy (cut section)
Jauniaux ERM, Simpson JL. Pregnancy loss. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 33.
Keyhan S, Muasher L, Muasher SJ. Spontaneous abortion and recurrent pregnancy loss; etiology, diagnosis, treatment. In: Lobo RA, Gershenson DM, Lentz GM, Valea FA, eds. Comprehensive Gynecology. 7th ed. Philadelphia, PA: Elsevier; 2017:chap 16.
Reddy UM, Silver RM. Stillbirth. In: Resnik R, Lockwood CJ, Moore TR, Greene MF, Copel JA, Silver RM, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 45.
Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 45.
Salhi BA, Nagrani S. Acute complications of pregnancy. In: Walls RM, Hockberger RS, Gausche-Hill M, eds. Rosen's Emergency Medicine: Concepts and Clinical Practice. 9th ed. Philadelphia, PA: Elsevier; 2018:chap 178.
Updated by: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
What’s the difference between miscarriage and abortion? For some women, it’s hard to tell | Abortion
Zoé Champion was 19 when she had an abortion. She was 26 when she realized it was an abortion.
Champion, who was sitting her high school exams in France at the time, had developed a pregnancy outside the uterus, threatening to rupture her fallopian tubes – a condition medically known as an ectopic pregnancy. The doctors intervened immediately, ending the pregnancy and saving her life.
The doctors intervened immediately, ending the pregnancy and saving her life.
But similarly to cookbook author and model Chrissy Teigen, who this week spoke out about miscategorizing her own abortion as a miscarriage, Champion didn’t realize she’d had an abortion until long after.
“It wasn’t an abortion for me [at the time]. I think because my health was at stake, there was no decision to be made,” says Champion, now 31 and living in New York.
Teigen told an audience at a social impact summit that she was pregnant with her third child with her husband, the singer John Legend, when she learned her pregnancy would not be viable – and that she would not survive without medical intervention.
“[It was] an abortion to save my life for a baby that had absolutely no chance. And to be honest, I never, ever put that together until, actually, a few months ago,” Teigen said.
She had very publicly discussed her pregnancy loss as a miscarriage at the time. It was only after the right to an abortion, long established by the supreme court in Roe v Wade, was overturned this summer that she realized she’d had the procedure: when she told Legend that she empathized with people who have an abortion, he pointed out she was one.
It was only after the right to an abortion, long established by the supreme court in Roe v Wade, was overturned this summer that she realized she’d had the procedure: when she told Legend that she empathized with people who have an abortion, he pointed out she was one.
Although it is common for many people to think of miscarriage and abortion as entirely separate matters, doctors say that medically the distinction isn’t so clear. Many doctors consider an abortion as any termination of pregnancy, whether through spontaneous miscarriage or a voluntary action like taking pills to induce one. The line between voluntary and involuntary also shifts and blurs: a patient might start spontaneously bleeding during a wanted pregnancy, then require an intervention; a different patient might want to end their pregnancy only to be told to wait because early signs suggest it will be unsuccessful anyway (around a quarter of pregnancies end spontaneously).
The gray area between miscarriage and abortion is newly worrying now that more than a dozen states criminalize abortion.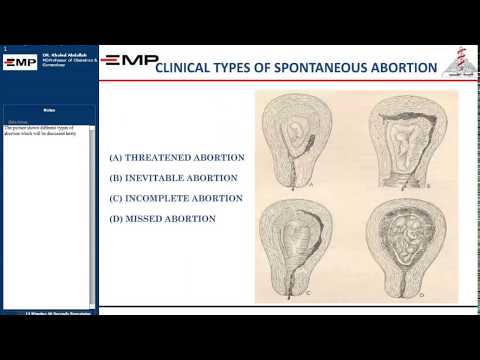 Patients could find themselves facing legal repercussions or traveling hundreds of miles to seek miscarriage care, for fear of it being mislabeled as an abortion. Dr Joan Fleischman, a New York-based doctor, sees a lot of overlap between abortion and miscarriage – in both cases “it’s not the right time” for a pregnancy to continue, be it for chromosomal or environmental reasons. She recently performed an abortion for a patient carrying triplets. The pregnancies, each implanted through in vitro fertilization, had stopped developing at different stages: one at six weeks, one at seven and one at eight.
Patients could find themselves facing legal repercussions or traveling hundreds of miles to seek miscarriage care, for fear of it being mislabeled as an abortion. Dr Joan Fleischman, a New York-based doctor, sees a lot of overlap between abortion and miscarriage – in both cases “it’s not the right time” for a pregnancy to continue, be it for chromosomal or environmental reasons. She recently performed an abortion for a patient carrying triplets. The pregnancies, each implanted through in vitro fertilization, had stopped developing at different stages: one at six weeks, one at seven and one at eight.
“None of them were going to be successful, so I removed that tissue for her,” she says.
During in vitro fertilization, Fleischman notes, people commonly fertilize more eggs than needed, to increase the chances of a successful pregnancy. Those excess eggs are commonly frozen, disposed of or donated for scientific research (which means destroying them), but none of that is thought of as abortion. What’s more, Fleischman’s patient wanted her pregnancy to be successful – she had invested tens of thousands of dollars in it – but still, the pregnancy ended in someone making a decision that the cells had to be removed: an abortion.
What’s more, Fleischman’s patient wanted her pregnancy to be successful – she had invested tens of thousands of dollars in it – but still, the pregnancy ended in someone making a decision that the cells had to be removed: an abortion.
Calling something a miscarriage rather than an abortion can be helpful for patients who want to avoid stigma, Fleischman says. “Often, they don’t want their doctor to know, they don’t want their husband to know,” she says.
“If somebody wants their privacy, [the term] ‘miscarriage’ offers a way to talk about a loss. You know, without dealing with the stigma that people just dish on you, no matter who you are, no matter what your situation,” she says.
The danger is not just stigma: after people who miscarry, they often need an abortion procedure to protect their health, and many people miscarry after admitting a pregnancy was unwanted, leaving them open to skepticism – and possible investigation.
In some states, like Texas, abortion-inducing pills have been forbidden, although the same pills are commonly prescribed for miscarriage.
One of Fleischman’s patients traveled from Florida to New York for miscarriage care because of Florida’s 15-week abortion ban. Although the state law makes an exception in some cases “to remove a dead fetus”, some providers are wary of providing care that might be interpreted as violating the ban – and some patients feel uncomfortable about the scrutiny they endure regarding their pregnancy.
Following Teigen’s comments, many anti-abortion advocates argued that abortion and miscarriage cannot be equated. The anti-abortion media platform LifeNews tweeted: “There is a distinct difference between losing a child to ectopic pregnancy or miscarriage and brutality and intentionally ending a life through abortion.”
“In a miscarriage a mother who wants a child loses it through medical complications outside her control. In an abortion a mother willfully enlists an abortionist to scald, dismember and kill her unborn child.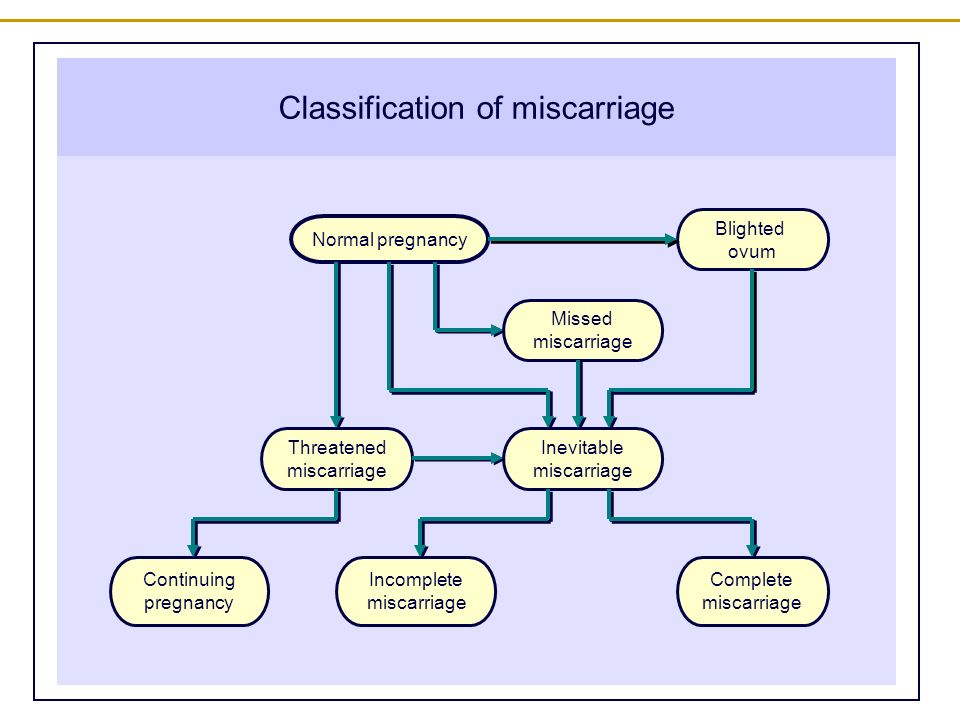 See the difference?” the right-wing commentator Dinesh D’Souza said.
See the difference?” the right-wing commentator Dinesh D’Souza said.
These sentiments reflect the changing language around abortion, says Dr Leah Torres, an obstetrician-gynecologist in Alabama. Reproductive healthcare has been subject to public redefinition for centuries, she notes, pointing to laws used to criminalize birth control in the 19th century or, more recently, to posit the existence of ‘fetal heartbeats’ or redefine ‘personhood’.
“When someone calls me and says ‘I’m aborting,’ the image I have is of someone voluntarily inducing their own abortion,” says Torres. “But it’s perfectly scientific to say they started aborting in the bathroom, right? Meaning their pregnancy was unsuccessful and it was ending – exiting their body.”
Torres, whose license was temporarily suspended after she went to Alabama to practice following that state’s abortion ban (her license has since been restored, though she remains $115,000 in debt due to the case), argues these terms matter.
“In the desire to politicize pregnancy termination, [anti-abortion advocates] have removed abortion from being a healthcare issue. They have used the word ‘abortion’ to mean one thing: you got pregnant, now you want to kill your baby. So there’s no room for the actual medical nuance,” she says.
Fleischman says so many of her patients are shocked when they see the mucus-like tissue that is extracted during early pregnancy in an abortion, because it doesn’t look like the images they’ve seen of little fetuses curled up and forming a head, eyes and an abdomen – images commonly and incorrectly used to convey what pregnancy looks like prior to nine weeks.
“It’s just like this huge ‘aha!’ moment for women, like, ‘Oh my God, I’ve been duped. I’ve been on this emotional, judgmental, roller coaster, like this is murder, and this thing just looks like mucus?’” she says.
“This is a very intentional,” says Torres. “Because it’s essentially about taking abortion out of [the] healthcare bracket, and viewing it as an issue of intention, an issue of morality, not an issue of healthcare. ”
”
People would find it ridiculous to say that Chrissy Teigen murdered her child, Torres notes, after a pregnancy she would have continued had it not become life-threatening. But Torres says that this differentiation – between the type of abortion Teigen had, or someone has after spontaneously bleeding on their bathroom floor, and an abortion someone has after walking into a clinic – is essential for anti-abortion activists to justify their rhetoric.
“The right needs to see what happened to her to seem different, because the right has equated abortion with murder,” she says.
Champion, who had her abortion at 19, wants that distinction to be done away with, and not just for herself.
“I want to contribute to depoliticizing this word ‘abortion’. To give it more meaning, so people see it as healthcare access,” she says. “The sooner we can all talk about it as healthcare, the better.”
Spontaneous miscarriage and miscarriage
Over the past 10 years, the number of spontaneous miscarriages has been growing rapidly. The International Histological Classification Organization (FIGO) has declared the situation with an increase in the frequency of miscarriages an epidemic.
The International Histological Classification Organization (FIGO) has declared the situation with an increase in the frequency of miscarriages an epidemic.
Spontaneous miscarriage is the termination of pregnancy before the fetus reaches a viable term (up to 22 weeks of pregnancy and fetal weight 500 g.).
Most miscarriages (about 80%) occur before 12 weeks of gestation. Moreover, in the early stages up to 8 weeks of pregnancy, the cause of miscarriage is chromosomal abnormalities in 50% of cases. It turns out that nature eliminates the defective product of conception. And these causes are difficult to prevent, especially in the presence of hereditary diseases. Fortunately, accidental breakdowns are much more common than genetically determined ones. Therefore, subsequent pregnancies usually end happily. But the remaining 50% of miscarriages have completely real and removable causes. They can be easily identified at the stage of preparation for pregnancy by a gynecologist.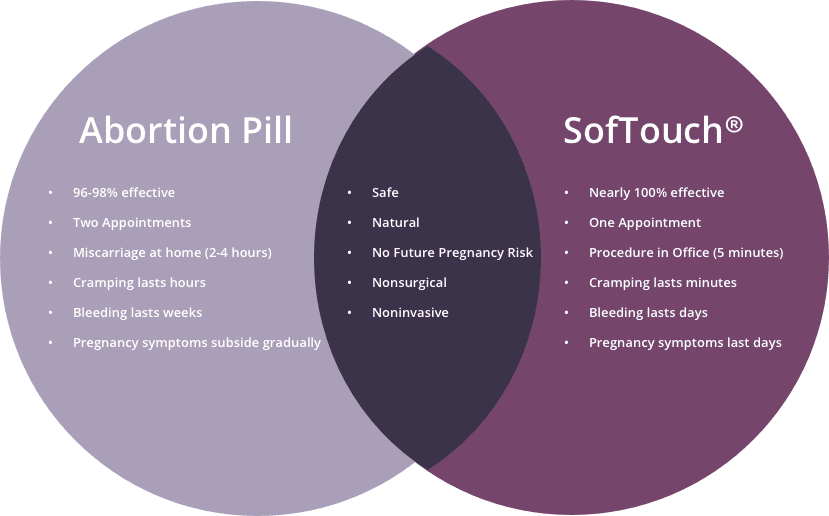
What are the reasons?
- chronic diseases: inflammatory diseases of the uterus and appendages, polycystic ovary syndrome, uterine fibroids, endometriosis, malformations of the genital organs.
- infections: toxoplasmosis, listeriosis, genital tuberculosis, sexual infections - chlamydia, mycoplasma, ureaplasma, syphilis.
- antiphospholipid syndrome.
- endocrine diseases: diabetes, thyroid disease.
- metabolic disorders in the body: obesity, folic acid deficiency, iron deficiency, vitamin D deficiency.
- male factor.
Of course, these causes are identified and eliminated before the planned conception.
There are harmful factors that can affect the development of the fetus in the early stages of pregnancy and lead to miscarriage:
- alcohol consumption.
- caffeine use (4-5 cups of coffee per day).
- smoking (more than 10 cigarettes a day).
- drug use.
- taking medications with a teratogenic effect (for example: aspirin, nise and others from this group of drugs; antifungals; antidepressants; some antibiotics and a number of other drugs).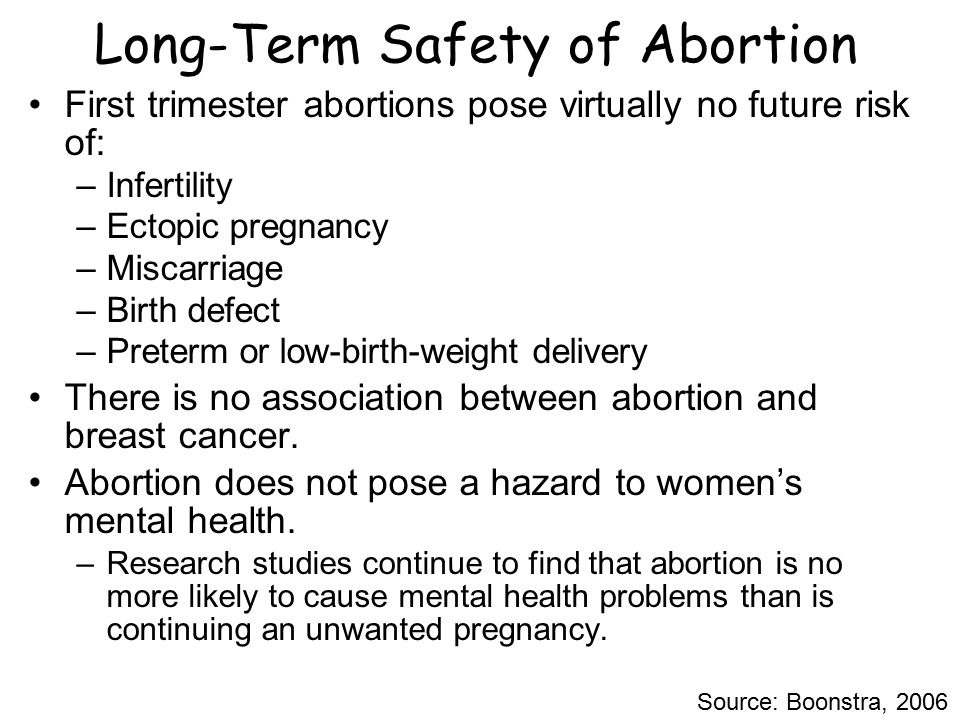
- toxins and occupational hazards: ionizing radiation, pesticides, inhalation of anesthetic gases.
What are the signs of possible pregnancy loss?
These are complaints of pain in the lower abdomen and lower back, bloody discharge from the genital tract. It is necessary to consult a doctor to rule out an ectopic pregnancy and conduct an additional examination (hCG test, blood test for progesterone, ultrasound).
In early pregnancy, with dubious ultrasound data or suspected non-developing (missing) pregnancy, expectant management is chosen with a repeat examination by a gynecologist, ultrasound, tests after 7-10 days. If a the diagnosis was made and the fact of uterine pregnancy was confirmed, with a threatened miscarriage, preservation therapy is carried out in an outpatient day hospital. A miscarriage that has begun requires hospitalization in the gynecological department. In the case of a non-developing pregnancy, an abortion is performed.
In accordance with the clinical treatment protocol approved by the Ministry of Health of the Russian Federation dated 07.06.2016. Preference is given to drug therapy aimed at terminating pregnancy with prostaglandin analogues (misoprostol) with or without prior use of an antiprogestin (mifepristone). In case of need for surgical treatment (with incomplete miscarriage with infected miscarriage), it is recommended to use aspiration curettage (with an electric vacuum source or a manual vacuum aspirator). What has a significant advantage over curettage of the uterine cavity because it is less traumatic and can be performed on an outpatient basis.
All women who have had a miscarriage need treatment to prevent complications and prevent recurrent miscarriages. Why is rehabilitation therapy necessary?
According to the decision of the XVIII World Congress of Obstetricians and Gynecologists , the diagnosis of chronic endometritis should be made to absolutely all women who have had an undeveloped pregnancy.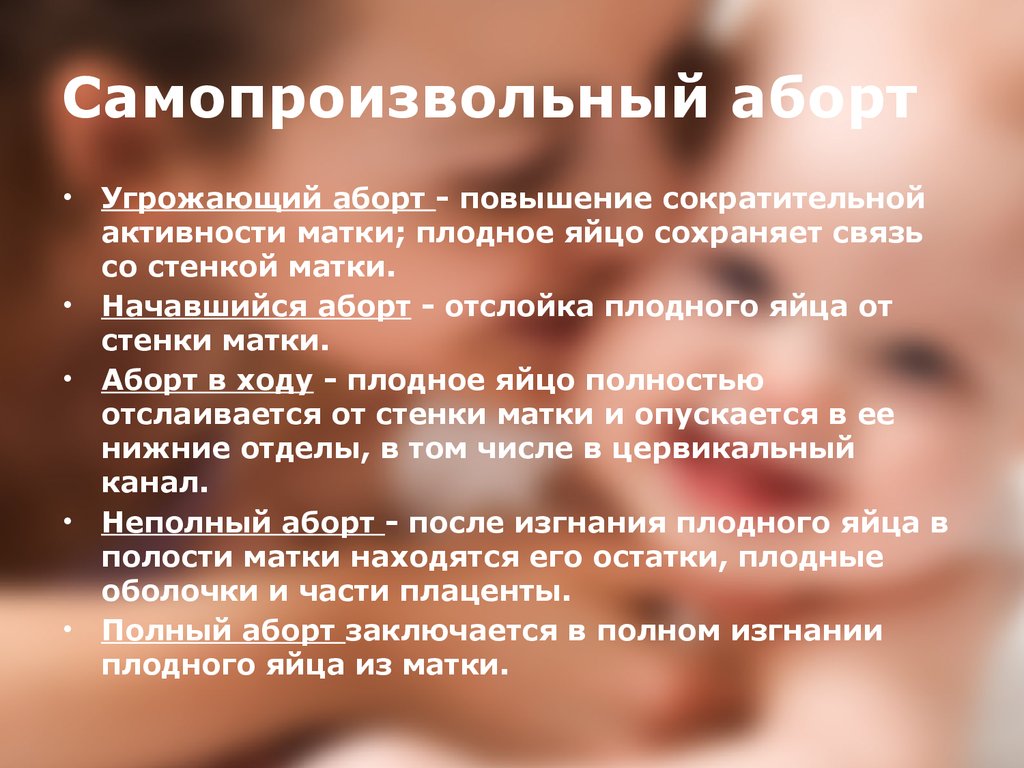 Two out of three miscarriages according to Professor V.E. Radzinsky are caused by this disease. When examining the material from the uterine cavity, infectious pathogens were isolated: ureaplasmas, mycoplasmas, streptococci, staphylococci, Escherichia coli, viruses (herpes, HPV). Therefore, it is very important to carry out treatment immediately after the termination of pregnancy.
Two out of three miscarriages according to Professor V.E. Radzinsky are caused by this disease. When examining the material from the uterine cavity, infectious pathogens were isolated: ureaplasmas, mycoplasmas, streptococci, staphylococci, Escherichia coli, viruses (herpes, HPV). Therefore, it is very important to carry out treatment immediately after the termination of pregnancy.
If time is lost, it is necessary to carry out additional diagnostics: a pipel biopsy of the endometrium with a histological examination and a study for infections, including tuberculosis. Then, taking into account the results obtained, symptomatic anti-inflammatory therapy is carried out (immunomodulators, antibacterial drugs, physiotherapy, gynecological massage, mud therapy). In parallel, an examination is prescribed to identify other causes of miscarriage (male factor, chronic maternal diseases, genital infections, antiphospholipid syndrome).
In the medical center "Mifra-Med" at the level of modern requirements of medicine, all the possibilities for a complete adequate examination have been created: all types of tests, ultrasound, hysteroscopy, aspiration biopsy, consultations of narrow specialists (endocrinologist, therapist, neurologist, urologist). Our gynecologists of the highest category Melko O.N., Novitskaya E.L., Tikhonova T.N. and urologist of the highest category Kanaev S.A. have sufficient experience in the rehabilitation and preparation of couples for the next pregnancy with a successful outcome. Treatment is carried out in a day hospital with the use of drugs, physiotherapy, gynecological massage, prostate massage.
Our gynecologists of the highest category Melko O.N., Novitskaya E.L., Tikhonova T.N. and urologist of the highest category Kanaev S.A. have sufficient experience in the rehabilitation and preparation of couples for the next pregnancy with a successful outcome. Treatment is carried out in a day hospital with the use of drugs, physiotherapy, gynecological massage, prostate massage.
WE WILL HELP YOU!
st. Yakovleva, 16 st. Kirova 47 B
tel. 244-744 tel. 46-43-57
Miscarriage
Gynecology
Miscarriage (spontaneous abortion, miscarriage) is the spontaneous termination of pregnancy in the period from conception to the 28th week. Miscarriage up to 28 weeks is referred to as spontaneous miscarriages (abortions), termination of pregnancy in terms of more than 28 weeks - to premature birth. Spontaneous miscarriages are divided into early (up to 16 weeks) and late (from 16 to 28 weeks). There is also habitual miscarriage (termination of pregnancy two or more times in a row).
Unfortunately, today, premature termination of pregnancy is not such a rare occurrence. According to statistics, in the last 40 years, almost every fifth pregnancy ended in miscarriage. Scientific studies say that in fact, more than half of spontaneous miscarriages! But this happens during the first three or four days of pregnancy, and therefore women do not even realize that they were pregnant for some time: after all, the next menstruation came either on time or with a slight delay. Naturally, such cases could not be taken into account by medical statistics. An analysis of reported cases of spontaneous abortions shows that 80% of them occur in the first 12 weeks of pregnancy.
The causes of spontaneous miscarriage are numerous. More than half of them are associated with genetic causes - violations of the quantity and quality of chromosomes in the cells of the embryo, as a result of which it becomes unviable, dies and is removed from the uterus. In this case, spontaneous miscarriage is the result of natural selection working against unviable fetuses.
In addition, miscarriage can be caused by various infections, chronic diseases, disorders in the immune system. Gynecological problems also play an important role - inflammatory diseases of the genital organs, uterine fibroids, ovarian cysts , postoperative scar on the uterus, uterine malformations, cervical insufficiency and various hormonal disorders , of which ovarian hypofunction and hyperandrogenism, genital and general infantilism are the most common.
Miscarriage is practically not affected by light falls and lifting of moderate weights by the mother. The fetus is sufficiently protected, and if the mother's body is healthy and the fetus's genetic program is normal, then the injury must be truly terrible to harm the fetus.
The causes of recurrent miscarriage (i.e., multiple spontaneous abortions) are practically the same, but a violation of the immune system plays a more definite role when the mother develops sensitization to fetal tissue antigens or erythrocyte and leukocyte sensitization reactions.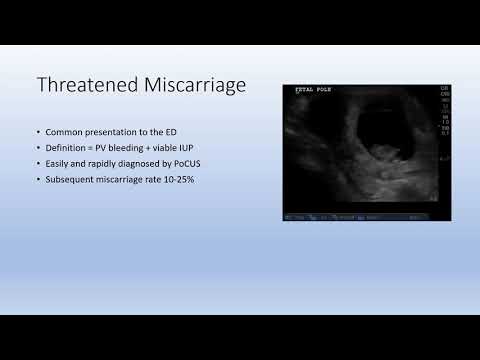
The clinical picture of premature termination of pregnancy depends on the stage of miscarriage and the duration of pregnancy. Usually, with the threat of interruption, pregnant women complain of pain in the lower abdomen and lower back, periodic tension (tonus) of the uterus. There are five stages in the course of early abortion: threatening, incipient abortion, ongoing abortion, incomplete and complete abortion. Early abortions are characterized by the birth of the entire fetal egg. The correct regimen and treatment in the first two stages can save the pregnancy. In subsequent stages, the removal of the entire fetal egg or its delayed parts is required. Symptoms of a threatened and incipient abortion are distinguished by the state of the cervix: it is unchanged in a threatened abortion and somewhat shortened with a closed or ajar canal in an incipient abortion. In addition, the intensity of the pain syndrome, the degree of uterine tension and / or the presence of blood discharge are taken into account.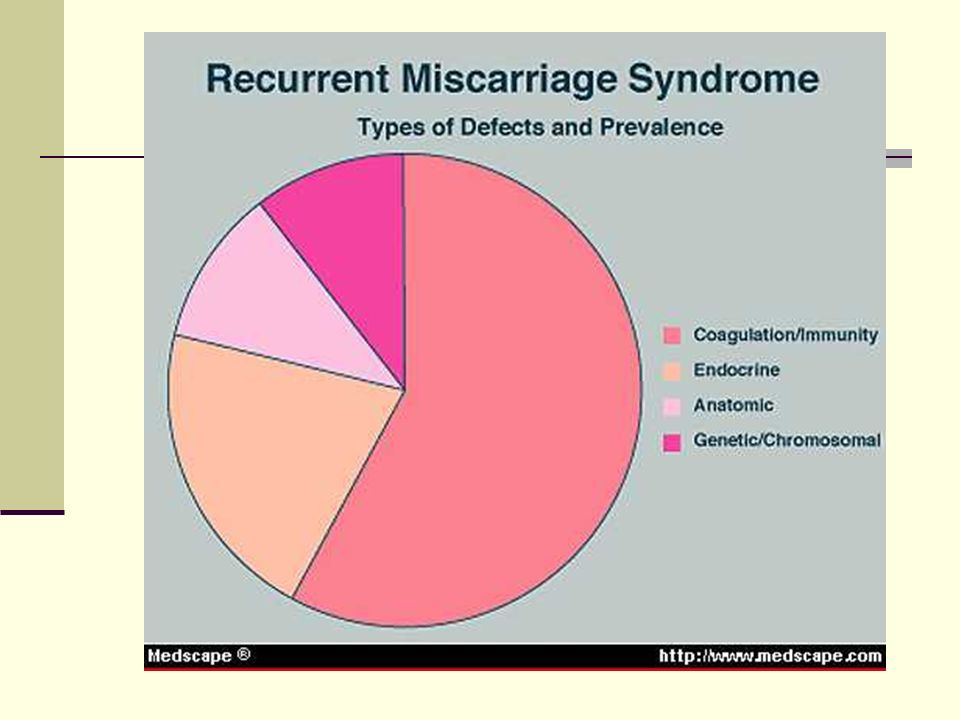
Late miscarriage proceeds according to the type of childbirth: there is an opening of the cervix, then the outflow of amniotic fluid, the birth of the fetus and, finally, the birth of the placenta. Clinically, it is manifested by cramping or aching pain in the lower abdomen, periodic uterine tension and, less commonly, bloody discharge.
When there is a threat of miscarriage, complex treatment is prescribed: medications, especially hormonal ones, are prescribed only according to strict indications and in minimal doses, since the consequences of hormonal treatment on both the fetus and the unborn child can appear even after many years.
In order to determine the cause of miscarriage, the doctors of our Clinic in each case are assigned an individual comprehensive examination: genetic, gynecological, ultrasound, laboratory, etc. If intrauterine pathology and/or endometrial pathology are suspected, separate diagnostic curettage is performed under hysteroscopy control, and if endometriosis is suspected, tubal pathology and adhesive process in the pelvis, with uterine myoma and scleropolycystic ovaries, operative laparoscopy may also be necessary. Such a large volume of examination should be clear to the patient: after all, miscarriage, as a rule, is the result of not one, but several causes that have their effect simultaneously or sequentially. In addition, many women who have experienced a spontaneous miscarriage may need the help of a psychotherapist who can provide professional advice to help eliminate the negative psychological consequences of this phenomenon. After the examination, a set of appropriate therapeutic measures is planned, depending on the identified factors of miscarriage. The patient's partner is also examined, which includes the identification of hereditary diseases, clarification of the presence of previously or currently existing diseases of various organs and systems, semen analysis and examination for infections.
Such a large volume of examination should be clear to the patient: after all, miscarriage, as a rule, is the result of not one, but several causes that have their effect simultaneously or sequentially. In addition, many women who have experienced a spontaneous miscarriage may need the help of a psychotherapist who can provide professional advice to help eliminate the negative psychological consequences of this phenomenon. After the examination, a set of appropriate therapeutic measures is planned, depending on the identified factors of miscarriage. The patient's partner is also examined, which includes the identification of hereditary diseases, clarification of the presence of previously or currently existing diseases of various organs and systems, semen analysis and examination for infections.
Prevention of miscarriage is carried out both before and during pregnancy. Our obstetricians-gynecologists conduct a special examination for all women who have undergone spontaneous abortion and preterm birth, including a targeted history taking, elucidation of the features of menstrual function (by functional diagnostic tests), hysterosalpingography and ultrasound scanning.