Vaginal during pregnancy
How Pregnancy Affects Vaginal Health
Medically reviewed by Patricia Geraghty, MSN, FNP-BC, WHNP — By Annette McDermott on October 4, 2016
During pregnancy, you expect your body to go through many obvious changes, such as larger breasts and a growing abdomen. What you may not know is your vagina goes through changes, too. It’s important to understand how pregnancy affects vaginal health, even after you give birth.
If you know what’s normal for your vagina during pregnancy, you’ll be more likely to head- off potential complications. Here are some ways your vagina is affected by pregnancy:
Increased vaginal discharge
An increase in vaginal discharge is one of the most noticeable vaginal changes during pregnancy. It’s caused by high levels of estrogen and progesterone. An increase in blood volume and blood flow can also contribute to increased vaginal discharge.
Pregnancy discharge should be thin, white, and milky. It may get heavier as your due date approaches. It shouldn’t smell bad, but it may have a mild odor that’s more noticeable than before. If vaginal discharge bothers you, try wearing unscented panty liners or mini pads.
Increased risk of vaginal infections
In some cases, increased vaginal discharge indicates infection. Vaginal infections are common during pregnancy, thanks in part to hormonal changes that alter your vagina’s pH-balance. Common vaginal infections during pregnancy include:
Yeast infections: During pregnancy, vaginal secretions contain more sugar, yeast’s meal of choice. A yeast infection won’t harm your unborn baby, but it’ll make your life uncomfortable. Symptoms of a yeast infection include vaginal itching, vaginal discharge that resembles cottage cheese and smells yeasty, and vaginal burning.
Bacterial vaginosis (BV): According to the American Pregnancy Association, 10 to 30 percent of pregnant women will get bacterial vaginosis. The condition is caused by an imbalance of good and bad vaginal bacteria. The main symptom of BV is a fishy-smelling, gray discharge. Untreated BV is linked to pre-term labor, low birth weight, and miscarriage.
The main symptom of BV is a fishy-smelling, gray discharge. Untreated BV is linked to pre-term labor, low birth weight, and miscarriage.
Trichomoniasis: This infection is transmitted by having sex with an infected person. It may cause serious pregnancy complications, such as your water breaking too soon and premature birth. Symptoms of trichomoniasis include a foul-smelling, yellow-green discharge, vaginal itching and redness, and pain during urination and sex.
Increased vaginal swelling
To support your growing baby, your blood flow increases significantly during pregnancy. It’s not unusual for your labia and vagina to appear swollen and feel fuller. The swelling and increased blood flow may also increase your libido and make you feel easily aroused. Hormonal changes and increased blood flow may also cause your vagina and labia to darken and take on a bluish tint.
In some cases, vaginal swelling is caused by infection. If vaginal swelling is accompanied by redness, burning, and itching, contact your doctor.
Vulvar varicose veins
Your legs aren’t the only place varicose veins can appear during pregnancy. They may also happen in your vulvar and vaginal areas. Vulvar varicose veins are caused by an increase in blood volume, and a decrease in how fast your blood flows from your lower extremities.
Vulvar varicose veins may cause pressure, fullness, and discomfort in your vulva and vagina. You can help relieve symptoms by applying a cold compress, elevating your hips when lying down, and wearing a compression garment. Most vulvar varicose veins go away on their own within several weeks of giving birth.
Vaginal bleeding
Vaginal bleeding during your first trimester isn’t unusual. It may be due to the implantation of the fertilized egg to the lining of your uterus. It may also be caused by increased blood volume. In some cases, vaginal bleeding is a sign of miscarriage, especially if it’s accompanied by severe, menstrual-like cramping, and the passing of tissue through your vagina.
Vaginal bleeding during your second and third trimesters is concerning. You should seek emergency medical care if your vaginal bleeding is caused by:
- placenta abruption (when the placenta peels away from the uterine lining)
- premature opening of the cervix
- preterm labor
- uterine rupture
When labor begins, you may experience vaginal discharge mixed with pink mucous. This is normal and is called bloody show.
No matter what scenario your vagina goes through during birth, there’ll be some swelling, bruising, and pain afterwards. It may be hurt to urinate or have a bowel movement. For most women, these symptoms go away after a few weeks. It may take longer if your vagina tore during birth, or if the skin between your vagina and anus was cut to help get your baby out.
Vaginal bleeding is common for two to six weeks after giving birth. Heavy bleeding that’s bright red and may include blood clots is normal for the first 24 hours after delivery. After that, bleeding should gradually decrease. Even so, you may experience vaginal bleeding for up to six weeks.
After that, bleeding should gradually decrease. Even so, you may experience vaginal bleeding for up to six weeks.
Your vagina will probably feel wide and stretchy after giving birth. It usually regains much of its elasticity within six weeks. Kegel exercises and other pelvic floor exercises performed during and after pregnancy help increase vaginal tone and decrease your risk of organ prolapse into the vagina.
Women who are breastfeeding have lower estrogen levels and are more likely to experience dryness. Water-based lubricants and natural moisturizers may help relieve vaginal dryness symptoms, such as painful sex, vaginal itching, and vaginal burning.
Your vagina plays a key role in pregnancy and childbirth, so it deserves special attention. Here are some tips for keeping your vagina healthy during and after pregnancy:
- Dry your vaginal area with a hair dryer on a low, cool setting after bathing or swimming.
- Wipe from front to back after going to the bathroom.

- Don’t douche or use scented sanitary pads or tampons.
- Avoid feminine hygiene sprays or perfumed personal care products.
- Wear looser clothing or underwear.
- Eat yogurt regularly.
- Reduce your sugar intake.
- Stay hydrated.
- Eat a healthy, balanced diet and get regular exercise.
- Practice responsible sex.
Consult your doctor when in doubt about vaginal discharge or other vaginal concerns. Some vaginal symptoms may be a sign of a serious problem, so it’s best to be cautious.
Pavilion for Women Blog | Pavilion for Women
August 04, 2022 | Sarah Ammons, PT, DPT, OCS, FAAOMPT
Physical therapy plays a vital role in the treatment of women’s pelvic pain.
Once a patient’s underlying medical issues have been addressed, that’s when a physical therapist’s job begins. We provide pelvic floor physical therapy to reduce pain, improve muscle strength and function, and restore quality of life. As physical therapists, we help women build bridges back to the lives they knew before they began experiencing pelvic pain.
Treatment and education
Many people don’t realize that pelvic pain problems can be treated by physical therapy. In some cases, pelvic floor physical therapy treats the main condition causing a woman’s pain. In other cases...
July 20, 2022 | Joseph Nassif, MD, MBA
Uterine fibroids affect most women at some point in their lives.
Fibroids typically don’t cause any symptoms or health problems, but when they do, pelvic pain may be one of them.
Understanding this common condition can help women know what to watch for, when to seek help and what to expect when they do.
What are fibroids?
Fibroids are benign (not cancerous) growths in the uterus. Uterine fibroids are also referred to as leiomyomas. Their cause is unknown.
A woman may have a single fibroid or multiple fibroids. Fibroids can also vary widely in size.
In most cases, they occur in women during their reproductive years – rarely are...
July 19, 2022 | Xiaoming Guan, MD, PhD
Pelvic pain is common, complex and often misdiagnosed, leaving many women suffering and in continued search of relief.
What makes diagnosis so difficult? And what steps can you take to prevent misdiagnosis from happening (or happening again) to you?
A wide range of causes
Much of the challenge stems from the wide range of potential causes of pelvic pain, including underlying conditions unrelated to a woman’s reproductive system.
Common causes include:
- Endometriosis
- Severe menstrual pain (dysmenorrhea)
- Pelvic inflammatory disease (PID)
- Ovarian conditions
- Uterine fibroids
- Gynecologic...
July 18, 2022 | Allison Conn, MD
These little-known conditions are taking their toll on the lives of women of all ages, most of whom have never heard of vulvodynia or vaginismus until they finally get help.
As an OB/GYN specializing in the treatment of these challenging disorders, Dr. Allison Conn knows all too well the suffering they can cause.
“I see a lot of women who have lived in pain for a long time,” says Dr. Conn.
Conn.
What is vulvodynia?
Women with vulvodynia have chronic pain, burning, itching or discomfort of the vulva, with no recognized cause. The vulva is the external part of the female genitals, including the labia, the clitoris and the opening of the vagina.
...
July 14, 2022 | Tamisa Koythong, MD
Understanding your options for pelvic pain surgery
If you’re suffering from pelvic pain and medical treatments haven’t been effective, surgery may be recommended — but that doesn’t necessarily mean a hysterectomy.
Today, there are more minimally invasive procedure options than ever before for the surgical treatment of gynecologic conditions — including endometriosis, fibroids and ovarian cysts — that cause pelvic pain.
...
Changes in a woman's body during pregnancy
From the very first days of pregnancy, the body of a pregnant woman undergoes profound transformations. These transformations are the result of the coordinated work of almost all body systems, as well as the result of the interaction of the mother's body with the child's body.
During pregnancy, many internal organs undergo significant restructuring. These changes are adaptive in nature, and, in most cases, are short-lived and completely disappear after childbirth. Consider the changes in the basic systems of the vital activity of a woman's body during pregnancy.
The respiratory system during pregnancy works hard. The respiratory rate increases. This is due to an increase in the need of the mother and fetus for oxygen, as well as in the limitation of the respiratory movements of the diaphragm due to an increase in the size of the uterus, which occupies a significant space of the abdominal cavity.
Cardio The mother's vascular system has to pump more blood during pregnancy to ensure an adequate supply of nutrients and oxygen to the fetus. In this regard, during pregnancy, the thickness and strength of the heart muscles increase, the pulse and the amount of blood pumped by the heart in one minute increase. In addition, the volume of circulating blood increases. In some cases, blood pressure increases. The tone of the blood vessels during pregnancy decreases, which creates favorable conditions for enhanced
to supply tissues with nutrients and oxygen. During pregnancy, the network of vessels of the uterus, vagina, and mammary glands decreases sharply. On the external genitalia, in the vagina, lower extremities, there is often an expansion of the veins, sometimes the formation of varicose veins. Heart rate decreases in the second half of pregnancy. It is generally accepted that the rise in blood pressure over 120-130 and a decrease to 100 mm Hg. signal the occurrence of pregnancy complications. But it is important to have data on the initial level of blood pressure. and changes in the blood system. During pregnancy, blood formation increases, the number of red blood cells, hemoglobin, plasma and bcc increases. BCC by the end of pregnancy increases by 30-40%, and erythrocytes by 15-20%. Many healthy pregnant women have a slight leukocytosis. ESR during pregnancy increases to 30-40. Changes occur in the coagulation system that contribute to hemostasis and prevent significant blood loss during childbirth or placental abruption and in the early postpartum period.
signal the occurrence of pregnancy complications. But it is important to have data on the initial level of blood pressure. and changes in the blood system. During pregnancy, blood formation increases, the number of red blood cells, hemoglobin, plasma and bcc increases. BCC by the end of pregnancy increases by 30-40%, and erythrocytes by 15-20%. Many healthy pregnant women have a slight leukocytosis. ESR during pregnancy increases to 30-40. Changes occur in the coagulation system that contribute to hemostasis and prevent significant blood loss during childbirth or placental abruption and in the early postpartum period.
Kidneys work hard during pregnancy. They secrete decay products of substances from the body of the mother and fetus (the waste products of the fetus pass through the placenta into the mother's blood).
Changes in the digestive system are represented by increased appetite (in most cases), craving for salty and sour foods. In some cases, there is an aversion to certain foods or dishes that were well tolerated before the onset of pregnancy. Due to the increased tone of the vagus nerve, constipation may occur.
In some cases, there is an aversion to certain foods or dishes that were well tolerated before the onset of pregnancy. Due to the increased tone of the vagus nerve, constipation may occur.
The most significant changes, however, occur in the genitals of pregnant women. These changes prepare the woman's reproductive system for childbirth and breastfeeding.
The uterus of a pregnant woman increases significantly in size. Its mass increases from 50 g - at the beginning of pregnancy to 1200 g - at the end of pregnancy. The volume of the uterine cavity by the end of pregnancy increases by more than 500 times! The blood supply to the uterus is greatly increased. In the walls of the uterus, the number of muscle fibers increases. The cervix is filled with thick mucus that clogs the cavity of the cervical canal. The fallopian tubes and ovaries also increase in size. In one of the ovaries, there is a "corpus luteum of pregnancy" - a place for the synthesis of hormones that support pregnancy.
The walls of the vagina will loosen and become more elastic.
External genitalia (labia minor and major) also increase in size and become more elastic. The tissues of the perineum are loosened. In addition, there is an increase in mobility in the joints of the pelvis and a divergence of the pubic bones. The changes in the genital tract described above are of extremely important physiological significance for childbirth. Loosening the walls, increasing the mobility and elasticity of the genital tract increases their throughput and facilitates the movement of the fetus through them during childbirth.
Skin in the genital area and in the midline of the abdomen usually becomes darker in color. Sometimes "stretch marks" form on the skin of the lateral parts of the abdomen, which turn into whitish stripes after childbirth.
Mammary glands increase in size, become more elastic, tense. When pressing on the nipple, colostrum (first milk) is released. Changes of the bone skeleton and muscular system . An increase in the concentration of the hormones relaxin and progesterone in the blood contributes to the leaching of calcium from the skeletal system. This accomplishes two goals. On the one hand, this helps to reduce the rigidity of the joints between the pelvic bones (especially the pubic joint) and increase the elasticity of the pelvic ring. Increasing the elasticity of the pelvis is of great importance in increasing the diameter of the internal bone ring in the first stage of labor and further reducing the resistance of the birth tract to fetal movement in the second stage of labor. Secondly, calcium, washed out of the mother's skeletal system, is used to build the skeleton of the fetus.
Changes of the bone skeleton and muscular system . An increase in the concentration of the hormones relaxin and progesterone in the blood contributes to the leaching of calcium from the skeletal system. This accomplishes two goals. On the one hand, this helps to reduce the rigidity of the joints between the pelvic bones (especially the pubic joint) and increase the elasticity of the pelvic ring. Increasing the elasticity of the pelvis is of great importance in increasing the diameter of the internal bone ring in the first stage of labor and further reducing the resistance of the birth tract to fetal movement in the second stage of labor. Secondly, calcium, washed out of the mother's skeletal system, is used to build the skeleton of the fetus.
It should be noted that calcium compounds are washed out of all bones of the maternal skeleton (including the bones of the foot and spine). As shown earlier, a woman's weight increases during pregnancy by 10 -12 kg. This additional load against the background of a decrease in bone stiffness can cause foot deformity and the development of flat feet. A shift in the center of gravity of the body of a pregnant woman due to an increase in the weight of the uterus can lead to a change in the curvature of the spine and the appearance of pain in the back and pelvic bones. Therefore, for the prevention of flat feet, pregnant women are advised to wear comfortable shoes with low heels. It is advisable to use insoles that support the arch of the foot. For the prevention of back pain, special physical exercises are recommended that can unload the spine and sacrum, as well as wearing a comfortable bandage. Despite an increase in calcium loss by the bones of the skeleton of a pregnant woman and an increase in their elasticity, structure and bone density (as is the case with osteoporosis in older women).
A shift in the center of gravity of the body of a pregnant woman due to an increase in the weight of the uterus can lead to a change in the curvature of the spine and the appearance of pain in the back and pelvic bones. Therefore, for the prevention of flat feet, pregnant women are advised to wear comfortable shoes with low heels. It is advisable to use insoles that support the arch of the foot. For the prevention of back pain, special physical exercises are recommended that can unload the spine and sacrum, as well as wearing a comfortable bandage. Despite an increase in calcium loss by the bones of the skeleton of a pregnant woman and an increase in their elasticity, structure and bone density (as is the case with osteoporosis in older women).
Changes in the nervous system . In the first months of pregnancy and at the end of it, there is a decrease in the excitability of the cerebral cortex, which reaches its greatest degree by the time of the onset of childbirth. By the same period, the excitability of the receptors of the pregnant uterus increases. At the beginning of pregnancy, there is an increase in the tone of the vagus nerve, in connection with which various phenomena often occur: changes in taste and smell, nausea, increased salivation, etc.
By the same period, the excitability of the receptors of the pregnant uterus increases. At the beginning of pregnancy, there is an increase in the tone of the vagus nerve, in connection with which various phenomena often occur: changes in taste and smell, nausea, increased salivation, etc.
Active endocrine glands there are significant changes that contribute to the proper course of pregnancy and childbirth. Changes in body weight. By the end of pregnancy, a woman's weight increases by about 10-12 kg. This value is distributed as follows: fetus, placenta, membranes and amniotic fluid - approximately 4.0 - 4.5 kg, uterus and mammary glands -1.0 kg, blood - 1.5 kg, intercellular (tissue) fluid - 1 kg , an increase in the mass of adipose tissue of the mother's body - 4 kg.
Conclusion. Summarizing the facts concerning changes in a woman's body during pregnancy, it is worth emphasizing that these changes reflect the processes of physiological adaptation of the mother's body to the process of intrauterine development of the fetus.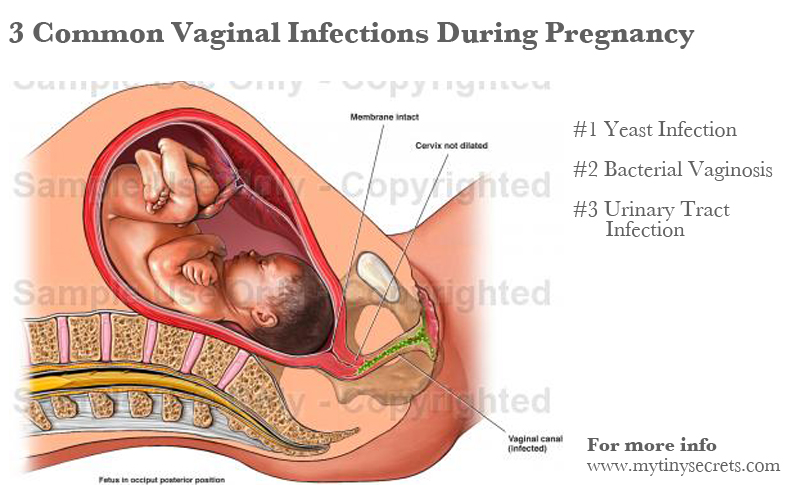 Therefore, measures aimed at preventing the pathology of pregnancy should be, first of all, natural, physiological. This is a proper and balanced diet, smoking cessation, a sufficient level of physical activity and fluid intake. In a healthy woman, such approaches ensure the normal course of pregnancy and adequate preparation of the mother's body for childbirth and breastfeeding.
Therefore, measures aimed at preventing the pathology of pregnancy should be, first of all, natural, physiological. This is a proper and balanced diet, smoking cessation, a sufficient level of physical activity and fluid intake. In a healthy woman, such approaches ensure the normal course of pregnancy and adequate preparation of the mother's body for childbirth and breastfeeding.
Prepared by: Head of the Pregnancy Pathology Department Teressa Ivanovna Vorobieva.
Changes in the cervix during pregnancy
Pregnancy is always pleasant, but sometimes not planned. And not all women have time to prepare for it, to be fully examined before its onset. And the detection of diseases of the cervix already during pregnancy can be an unpleasant discovery.
The cervix is the lower segment of the uterus in the form of a cylinder or cone. In the center is the cervical canal, one end of which opens into the uterine cavity, and the other into the vagina. On average, the length of the cervix is 3–4 cm, the diameter is about 2.5 cm, and the cervical canal is closed. The cervix has two parts: lower and upper. The lower part is called the vaginal, because it protrudes into the vaginal cavity, and the upper part is supravaginal, because it is located above the vagina. The cervix is connected to the vagina through the vaginal fornices. There is an anterior arch - short, posterior - deeper and two lateral ones. Inside the cervix passes the cervical canal, which opens into the uterine cavity with an internal pharynx, and is clogged with mucus from the side of the vagina. Mucus is normally impervious to infections and microbes, or to spermatozoa. But in the middle of the menstrual cycle, the mucus thins and becomes permeable to sperm.
On average, the length of the cervix is 3–4 cm, the diameter is about 2.5 cm, and the cervical canal is closed. The cervix has two parts: lower and upper. The lower part is called the vaginal, because it protrudes into the vaginal cavity, and the upper part is supravaginal, because it is located above the vagina. The cervix is connected to the vagina through the vaginal fornices. There is an anterior arch - short, posterior - deeper and two lateral ones. Inside the cervix passes the cervical canal, which opens into the uterine cavity with an internal pharynx, and is clogged with mucus from the side of the vagina. Mucus is normally impervious to infections and microbes, or to spermatozoa. But in the middle of the menstrual cycle, the mucus thins and becomes permeable to sperm.
Outside, the surface of the cervix has a pinkish tint, it is smooth and shiny, durable, and from the inside it is bright pink, velvety and loose.
The cervix during pregnancy is an important organ, both in anatomical and functional terms. It must be remembered that it promotes the process of fertilization, prevents infection from entering the uterine cavity and appendages, helps to "endure" the baby and participates in childbirth. That is why regular monitoring of the condition of the cervix during pregnancy is simply necessary.
It must be remembered that it promotes the process of fertilization, prevents infection from entering the uterine cavity and appendages, helps to "endure" the baby and participates in childbirth. That is why regular monitoring of the condition of the cervix during pregnancy is simply necessary.
During pregnancy, a number of physiological changes occur in this organ. For example, a short time after fertilization, its color changes: it becomes cyanotic. The reason for this is the extensive vascular network and its blood supply. Due to the action of estriol and progesterone, the tissue of the cervix becomes soft. During pregnancy, the cervical glands expand and become more branched.
Screening examination of the cervix during pregnancy includes: cytological examination, smears for flora and detection of infections. Cytological examination is often the first key step in the examination of the cervix, since it allows to detect very early pathological changes that occur at the cellular level, including in the absence of visible changes in the cervical epithelium. The examination is carried out to identify the pathology of the cervix and the selection of pregnant women who need a more in-depth examination and appropriate treatment in the postpartum period. When conducting a screening examination, in addition to a doctor's examination, a colposcopy may be recommended. As you know, the cervix is covered with two types of epithelium: squamous stratified from the side of the vagina and single-layer cylindrical from the side of the cervical canal. Epithelial cells are constantly desquamated and end up in the lumen of the cervical canal and in the vagina. Their structural characteristics make it possible, when examined under a microscope, to distinguish healthy cells from atypical ones, including cancerous ones.
The examination is carried out to identify the pathology of the cervix and the selection of pregnant women who need a more in-depth examination and appropriate treatment in the postpartum period. When conducting a screening examination, in addition to a doctor's examination, a colposcopy may be recommended. As you know, the cervix is covered with two types of epithelium: squamous stratified from the side of the vagina and single-layer cylindrical from the side of the cervical canal. Epithelial cells are constantly desquamated and end up in the lumen of the cervical canal and in the vagina. Their structural characteristics make it possible, when examined under a microscope, to distinguish healthy cells from atypical ones, including cancerous ones.
During pregnancy, in addition to physiological changes in the cervix, some borderline and pathological processes may occur.
Under the influence of hormonal changes that occur in a woman's body during the menstrual cycle, cyclic changes also occur in the cells of the epithelium of the cervical canal. During the period of ovulation, the secretion of mucus by the glands of the cervical canal increases, and its qualitative characteristics change. With injuries or inflammatory lesions, sometimes the glands of the cervix can become clogged, a secret accumulates in them and cysts form - Naboth follicles or Naboth gland cysts that have been asymptomatic for many years. Small cysts do not require any treatment. And pregnancy, as a rule, is not affected. Only large cysts that strongly deform the cervix and continue to grow may require opening and evacuation of the contents. However, this is very rare and usually requires monitoring during pregnancy.
During the period of ovulation, the secretion of mucus by the glands of the cervical canal increases, and its qualitative characteristics change. With injuries or inflammatory lesions, sometimes the glands of the cervix can become clogged, a secret accumulates in them and cysts form - Naboth follicles or Naboth gland cysts that have been asymptomatic for many years. Small cysts do not require any treatment. And pregnancy, as a rule, is not affected. Only large cysts that strongly deform the cervix and continue to grow may require opening and evacuation of the contents. However, this is very rare and usually requires monitoring during pregnancy.
Quite often, in pregnant women, during a mirror examination of the vaginal part, polyps cervix. The occurrence of polyps is most often associated with a chronic inflammatory process. As a result, a focal proliferation of the mucosa is formed, sometimes with the involvement of muscle tissue and the formation of a pedicle. They are mostly asymptomatic. Sometimes they are a source of blood discharge from the genital tract, more often of contact origin (after sexual intercourse or defecation). The size of the polyp is different - from millet grain rarely to the size of a walnut, their shape also varies. Polyps are single and multiple, their stalk is located either at the edge of the external pharynx, or goes deep into the cervical canal. Sometimes during pregnancy there is an increase in the size of the polyp, in some cases quite fast. Rarely, polyps first appear during pregnancy. The presence of a polyp is always a potential threat of miscarriage, primarily because it creates favorable conditions for ascending infection. Therefore, as a rule, more frequent monitoring of the cervix follows. The tendency to trauma, bleeding, the presence of signs of tissue necrosis and decay, as well as questionable secretions require special attention and control. Treatment of cervical polyps is only surgical and during pregnancy, in most cases, treatment is postponed until the postpartum period, since even large polyps do not interfere with childbirth.
They are mostly asymptomatic. Sometimes they are a source of blood discharge from the genital tract, more often of contact origin (after sexual intercourse or defecation). The size of the polyp is different - from millet grain rarely to the size of a walnut, their shape also varies. Polyps are single and multiple, their stalk is located either at the edge of the external pharynx, or goes deep into the cervical canal. Sometimes during pregnancy there is an increase in the size of the polyp, in some cases quite fast. Rarely, polyps first appear during pregnancy. The presence of a polyp is always a potential threat of miscarriage, primarily because it creates favorable conditions for ascending infection. Therefore, as a rule, more frequent monitoring of the cervix follows. The tendency to trauma, bleeding, the presence of signs of tissue necrosis and decay, as well as questionable secretions require special attention and control. Treatment of cervical polyps is only surgical and during pregnancy, in most cases, treatment is postponed until the postpartum period, since even large polyps do not interfere with childbirth.
The most common pathology of the cervix in women is erosion . Erosion is a defect in the mucous membrane. True erosion is not very common. The most common pseudo-erosion (ectopia) is a pathological lesion of the cervical mucosa, in which the usual flat stratified epithelium of the outer part of the cervix is replaced by cylindrical cells from the cervical canal. Often this happens as a result of mechanical action: with frequent and rough sexual intercourse, desquamation of the stratified squamous epithelium occurs. Erosion is a multifactorial disease. The reasons may be:
- genital infections, vaginal dysbacteriosis and inflammatory diseases of the female genital area;
- is an early onset of sexual activity and frequent change of sexual partners. The mucous membrane of the female genital organs finally matures by the age of 20-23. If an infection interferes with this delicate process, erosion is practically unavoidable;
- is an injury to the cervix.
 The main cause of such injuries is, of course, childbirth and abortion;
The main cause of such injuries is, of course, childbirth and abortion; - hormonal disorders;
- , cervical pathology may also occur with a decrease in the protective functions of immunity.
The presence of erosion does not affect pregnancy in any way, as well as pregnancy on erosion. Treatment during pregnancy consists in the use of general and local anti-inflammatory drugs for inflammatory diseases of the vagina and cervix. And in most cases, just dynamic observation is enough. Surgical treatment is not carried out throughout the entire pregnancy, since the excess of risks and benefits is significant, and after treatment during childbirth, there may be problems with opening the cervix.
Almost all women with various diseases of the cervix safely bear and happily give birth to beautiful babies!
Attention! Prices for services in different clinics may vary. To clarify the current cost, select a clinic
Clinical Hospital of IDKClinic "Mother and Child" Entuziastov Samara
All directionsSpecialist consultations (adults)Specialist consultations (children's)Laboratory of molecular geneticsGeneral clinical examinationsProcedural roomOther gynecological operationsTelemedicine for adultsTherapeutic examinationsUltrasound examinations for adults
01.