When does your baby start getting nutrients from you
When does the placenta form, and what does it do? Learn all about the placenta.
One of the many remarkable things about pregnancy is that you're not only growing a new human being, but also an entirely new organ. And pretty much everything your baby needs to develop and thrive flows through it. Find out all about the amazing placenta, including when it forms and what it does.
What is the placenta?
The placenta is a pancake-shaped organ that develops within the wall of your uterus and connects to your baby though the umbilical cord. By the end of pregnancy, it grows to be about 9 inches in diameter and about an inch thick at the center.
What does the placenta do?
- It delivers oxygen and nutrients (such as vitamins, glucose, and water) from your body to the baby's, and processes the waste products from your baby.
- It produces the hormones that help your baby grow and develop.
- It allows antibodies to pass to your baby from your bloodstream.
These antibodies protect against certain bacterial infections and viral illnesses, like diphtheria and measles, until after your baby is born and old enough to get their first vaccinations.
When does the placenta form?
The placenta starts forming as early as six days after fertilization. At this point your baby-to-be is a hollow ball of several hundred cells called a blastocyst. The blastocyst attaches to the lining of the uterus, usually near the top. This is called implantation, and it's completed by day 9 or 10.
The wall of the blastocyst is one cell thick except in one area, where it's three to four cells thick. In the thickened area, the inner cells develop into the embryo. The outer cells throughout the embryo burrow into the lining of the uterus and develop into the placenta.
The placenta produces several hormones that help maintain the pregnancy, including human Chorionic Gonadotropin (hCG), which prevents the ovaries from releasing eggs and stimulates the ovaries to produce estrogen and progesterone continuously. (Home pregnancy tests measure levels of hCG in your urine.)
(Home pregnancy tests measure levels of hCG in your urine.)
The placenta is fully formed by 18 to 20 weeks but continues to grow throughout pregnancy. At delivery, it weighs about 1 pound.
How the placenta works
The placenta connects to the umbilical cord through thousands of microscopic "fingers" of tissue (chorionic villi) containing a network of blood vessels that connect to the embryo's circulatory system. The villi are formed by 6 weeks of pregnancy, and your blood fills the spaces around them by 12 weeks. When your blood comes in contact with the villi, nutrients are exchanged for waste through the villi walls.
The villi also act as a filter, preventing some viruses and bacteria from reaching your baby, while allowing molecules of everything you ingest as well as antibodies and gases to pass through.
How do babies get nutrients in the womb?
Your baby needs nourishment from the get-go. Until the placenta is developed enough to provide nutrients, your baby receives nutrients from the lining of the uterus, called the endometrium. (These same endometrial cells will quickly multiply to form the placenta.)
(These same endometrial cells will quickly multiply to form the placenta.)
In the early weeks of pregnancy, glands in the uterine lining secrete glucose, which it stores as glycogen. At first, this glycogen is the only source of nourishment for your baby.
At about 8 to 12 weeks into pregnancy, the placenta takes over as a nutrient source for your baby. (And at this point the uterus stops secreting glycogen.) Here's how it works:
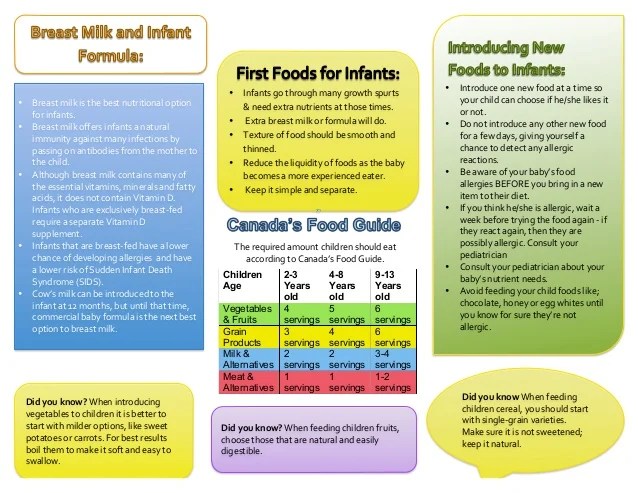
- When you eat, the food travels to your stomach, where it's broken down (digested) into glucose, fats, vitamins, minerals, and protein.
- The nutrients are absorbed into your bloodstream and travel to the placenta.
- Blood vessels in the umbilical cord pass the nutrients from the placenta to vessels that flow from the umbilical cord to the baby. At this point, your baby will begin to gain weight more quickly. The umbilical cord also returns waste products from your baby to the placenta and into your circulation for elimination.
Wondering how fast the food you eat reaches your baby? It depends on how quickly the food is digested and enters your bloodstream. Some foods may take several hours, while substances like caffeine can enter your bloodstream and cross the placenta in a very short time. For more information, watch our video on how food reaches your baby.
Harmful substances that cross the placenta
Along with all the good things that are transferred to your baby, some harmful ones can cross the placenta too. These include alcohol, nicotine, and illegal drugs as well as some medications.
No safe level has been established for alcohol consumption during pregnancy, and experts recommend not drinking any amount while you're expecting. The same goes for smoking and using illegal drugs. Although marijuana is legal in some states, experts recommend against using it during pregnancy.
Use caution when taking prescribed and over-the-counter medications during pregnancy because most cross the placenta. Although many medications are considered safe for your baby, a few are known to cause birth defects. And for many drugs, there simply is not enough research to know their effects on an unborn baby. Your provider can help you determine whether the benefits of a certain drug outweigh the risks in your case.
Although many medications are considered safe for your baby, a few are known to cause birth defects. And for many drugs, there simply is not enough research to know their effects on an unborn baby. Your provider can help you determine whether the benefits of a certain drug outweigh the risks in your case.
Although the placenta acts as a barrier to most bacteria, some viruses and small bacteria can cross it. Many have no effect, but others can be harmful to a developing baby. That's one reason why it's important to get all recommended vaccinations before and during pregnancy, including a flu shot and a Tdap vaccine to protect against tetanus, diphtheria, and pertussis (whooping cough).
Both the flu and pertussis can be life-threatening for babies, and getting these vaccines while you're pregnant enables antibodies to pass through the placenta that will protect your newborn from catching these illnesses. Getting your COVID vaccine and boosters will help protect you from infection and will also provide your baby with antibodies through the placenta (and your breast milk, if you breastfeed).
Here are a few other things you can do to promote a healthy placenta and a healthy baby:
- Go to all your prenatal checkups and work with your healthcare provider to manage any health conditions, such as high blood pressure, which can cause problems with the placenta.
- Don't smoke or use drugs. Placental problems, like placental abruption, are more common in women who smoke, use illegal drugs (like cocaine and heroin), or abuse medications (like opioids).
Delivering the placenta
A few minutes after your baby is born, the placenta detaches from the wall of your uterus and is delivered through your vagina. This is called the "afterbirth."
You'll have a few contractions, but this stage of childbirth usually lasts only about five to 30 minutes and feels more like menstrual cramps than labor pains. (If you're having a c-section, your doctor will remove the placenta manually.)
If you want, and if you've made prior arrangements with your provider, you can save the placenta.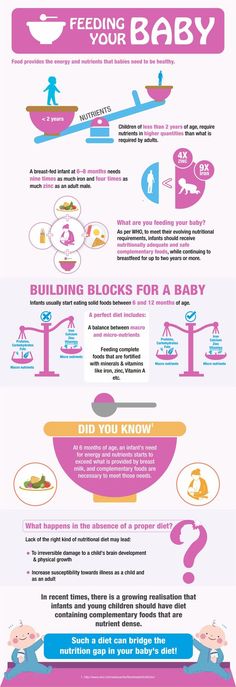 Some women believe that encapsulating and eating the placenta after birth helps them recover faster, though there's no scientific evidence to support this claim.
Some women believe that encapsulating and eating the placenta after birth helps them recover faster, though there's no scientific evidence to support this claim.
Also note that some experts think eating the placenta may be harmful, as there are potential risks, including infection and heavy metal contamination. Be sure to discuss this topic with your provider if it's something you're considering.
Learn more:
Placenta previa
Placenta accreta
Slideshow: Fetal development, week by week
advertisement | page continues below
You Are What You Eat...And Also What Your Mother Ate
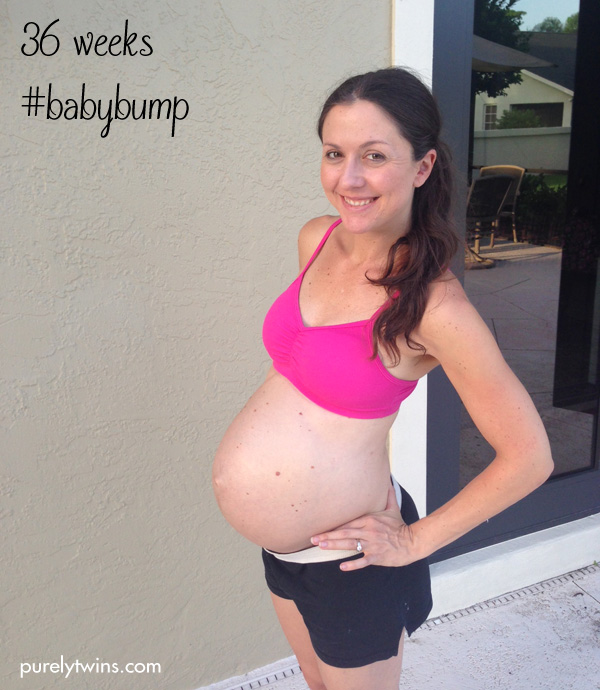
If you feel like you’ve been seeing more pregnant women lately, your eyes are not deceiving you. According to the US Census, August is the month with the highest number of births. During pregnancy, the fetus relies on its mother’s diet to sustain its nutritional needs for growth and development in the womb. For years, scientists have studied the potential long-term effects of prenatal nutrition on the development of adult diseases like hypertension, cardiovascular disease, and diabetes. New research is showing that a mother’s nutrition and health may also contribute to permanent changes in fetal metabolism, even before she knows she’s eating for two.
New research is showing that a mother’s nutrition and health may also contribute to permanent changes in fetal metabolism, even before she knows she’s eating for two.
The Basics of Reproductive Physiology and Early Nutrition
The full-term human fetus develops from a single cell and needs nutrition from the moment of conception. The developing fetus relies primarily on the mother’s placenta for energy, but it takes nearly 12 weeks until growth of the placenta is complete. How are the high-energy needs of a growing baby fueled from day one?
Upon ovulation, a mature female egg (ovum) is released into the fallopian tube. Fertilization takes place within the fallopian tube when a sperm meets the egg, forming a single-celled zygote. Over the next several days, the zygote divides rapidly while traveling to the uterus, relying on energy stored in the egg to fuel its growth. By the time it reaches the uterine cavity, the shape of the cell mass has changed from a solid sphere to a more ring-like shape with an inner cell mass called the blastocyst.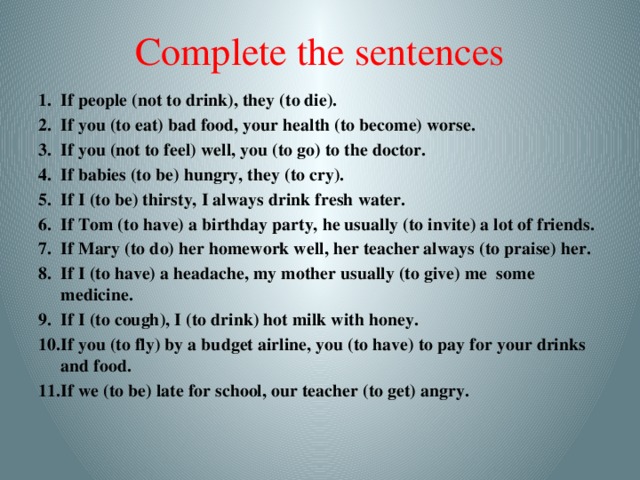 The developing blastocyst remains in the uterine cavity for 4-5 days before implanting in the uterine lining (endometrium), using nutrients from endometrial secretions to meet its energy needs until implantation occurs. The outer cells of the blastocyst, or trophoblast, are the first cells to differentiate and take on specialized tasks. Its first task is to initiate implantation by secreting enzymes that help break down the cells of the endometrium. The trophoblastic cells digest endometrial cells, absorbing the nutrients and transferring them to the blastocyst to provide further sustenance. While some trophoblastic cells break down the endometrium for nutrition, others form cords of cells that reach deeper into the endometrium to allow the blastocyst to attach and implant. Once implantation is complete, around one week post ovulation, the trophoblast and cells from the endometrium proliferate rapidly to form the placenta. The endometrium is the only source of nutrients for the embryo in the first week of implantation and remains a major source of nutrition for 8-12 weeks until the development of the maternal blood supply to the placenta is complete.
The developing blastocyst remains in the uterine cavity for 4-5 days before implanting in the uterine lining (endometrium), using nutrients from endometrial secretions to meet its energy needs until implantation occurs. The outer cells of the blastocyst, or trophoblast, are the first cells to differentiate and take on specialized tasks. Its first task is to initiate implantation by secreting enzymes that help break down the cells of the endometrium. The trophoblastic cells digest endometrial cells, absorbing the nutrients and transferring them to the blastocyst to provide further sustenance. While some trophoblastic cells break down the endometrium for nutrition, others form cords of cells that reach deeper into the endometrium to allow the blastocyst to attach and implant. Once implantation is complete, around one week post ovulation, the trophoblast and cells from the endometrium proliferate rapidly to form the placenta. The endometrium is the only source of nutrients for the embryo in the first week of implantation and remains a major source of nutrition for 8-12 weeks until the development of the maternal blood supply to the placenta is complete.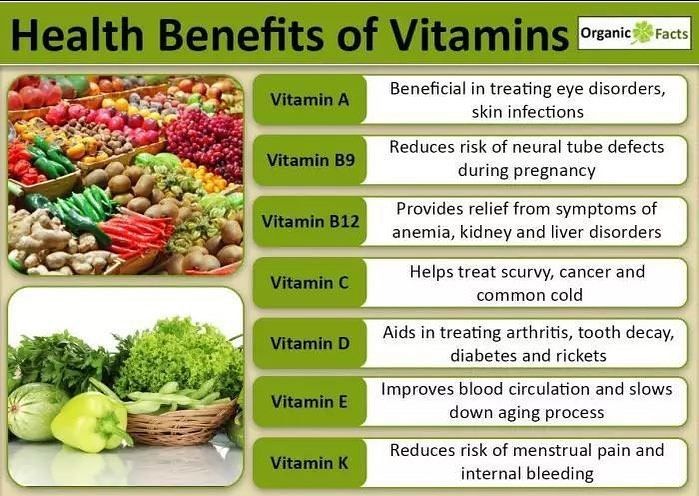
The Roots of the ‘Fetal Origins of Disease’ Theory
In the late 1980s and early 1990s, David Barker, an epidemiologist, and his colleagues at the University of Southampton published a series of groundbreaking studies that found an association between low-birthweight and adult chronic diseases. Barker’s hypothesis posits that malnutrition, even subclinical malnutrition, can adversely affect growth of the fetus. An infant born with a low-birthweight has presumably developed more slowly in the womb. Barker’s studies showed that low-birthweight infants have higher incidences of chronic diseases such as coronary heart disease, type-2 diabetes, hypertension, and stroke as adults.
The connection between low-birthweight and type-2 diabetes is attributed to what Barker calls the “thrifty phenotype”. He hypothesizes that a malnourished fetus adapts its metabolism to a low-nutrient environment in the womb. If that infant is then exposed to an environment of caloric excess during childhood, as is the case in many developed countries, excess nutrients are stored as fat instead of muscle, and this altered body composition can eventually lead to obesity and insulin resistance in adulthood. This hypothesis rests on the assumption that our metabolisms are “hard-wired” during fetal development, and that these systems are therefore unable to adapt to a different degree of food availability during childhood and beyond.
This hypothesis rests on the assumption that our metabolisms are “hard-wired” during fetal development, and that these systems are therefore unable to adapt to a different degree of food availability during childhood and beyond.
The notion that prenatal nutrition could be linked to adult health, dubbed the developmental origins of disease theory, was astounding to the medical and research community at the time. There were many skeptics of his early research, but further studies have continued to show this pattern of birthweight being correlated with adult metabolic disease.
New Research on Prenatal Nutrition and its effect on the Fetal Environment
Barker’s hypothesis is no longer considered controversial, but the mechanism of how maternal nutrition influences long-term health outcomes is still being examined. Last month at the Society for Reproductive Science conference in Pittsburg, PA, new research proposed some explanations for how prenatal nutrition might influence adult health, and highlighted the role of prenatal nutrition at even the very early stages of pregnancy.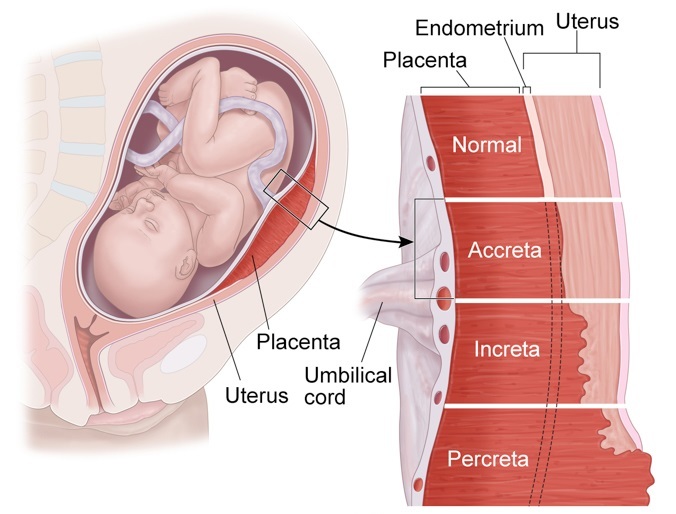
Researchers are finding that nutrition for the blastocyst and even the single-celled zygote may be especially critical. A group of scientists led by Kelle Moley from Washington University has discovered that in mouse studies, the nutritional environment at the zygote stage can produce long-term effects in the developing fetus. The researchers transferred single-celled zygotes from diabetic mice into non-diabetic mice. They found that, compared to normal mice, the zygotes from the diabetic mice had higher rates of growth defects later in fetal development, including neural tube defects, heart defects, and limb deformities. Because the embryos were transferred at the zygote stage, this suggests that maternal nutrition even before this point is important for the health of the offspring. The researchers hypothesize that the high blood sugar of diabetics may cause changes in the mothers’ eggs themselves that eventually lead to changes in a fetus if an egg becomes fertilized, though this will take many more studies to fully investigate.
Another scientist, Tom Fleming from the University of Southampton, presented a mouse study displaying the so-called thrifty phenotype. His team fed mice a low-protein diet during the stages before implantation, followed by normal nutrition for the rest of gestation and postnatally. Mice that were fed a diet low in protein had offspring that were heavier than the controls and showed signs of cardiovascular abnormalities and hypertension as adult mice. Fleming’s lab analyzed a selection of embryos from both mice and found differences in cell development during the early blastocyst stage that eventually produced changes in the trophoblast when these outer cells differentiated. Because the trophoblast plays a significant role in the development of the fetal side of the placenta, this research suggests that the diet programs the offspring’s metabolism early on. The zygote and blastocyst seem to sense a low-nutrient environment, so they boost metabolism to collect as many nutrients as possible during pregnancy, presumably to compensate for the potentially low-nutrient environment outside the womb.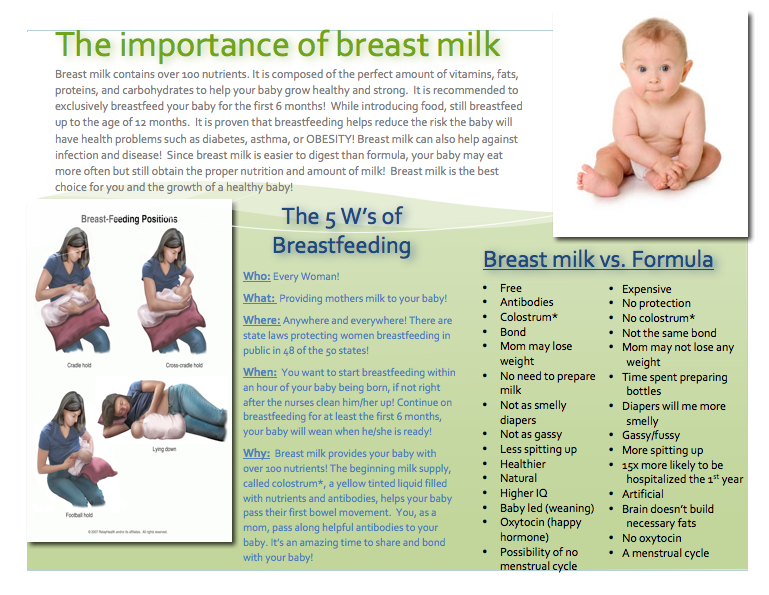 After the mice are born, they still show this type of metabolism that promotes nutrient storage in the form of fat.
After the mice are born, they still show this type of metabolism that promotes nutrient storage in the form of fat.
It’s not just undernutrition that affects long-term changes: both animal and human studies show that obesity during pregnancy can also affect fetal metabolism, though more studies need to be done on the cellular and molecular level to examine how this happens. Preliminary research shows that offspring of obese mothers tend to show insulin resistance and have decreased functioning of the pancreas: their pancreases produce lower amounts of several hormones necessary for metabolism. These offspring also had higher rates of developmental anomalies similar to those of diabetic mothers such as neural tube defects, abnormalities in the functioning of arteries, and increased susceptibility to high blood pressure.
Barker’s work, the studies described above, and work by many other researchers, has established that the nutritional environment during early gestation influences adult metabolism. But exactly how, at the molecular level, are these changes mediated? One potential mechanism by which nutrients can influence metabolism is through changes in gene expression, or the amount or type of protein made from a particular gene. The amount and type of products made from genes define how cells in the body function. While differences in gene expression can be hereditary, they can also be due to factors in the environment like nutrient availability. While these studies suggest that this is indeed occurring, what is exactly happening at the genetic level still needs to be examined.
But exactly how, at the molecular level, are these changes mediated? One potential mechanism by which nutrients can influence metabolism is through changes in gene expression, or the amount or type of protein made from a particular gene. The amount and type of products made from genes define how cells in the body function. While differences in gene expression can be hereditary, they can also be due to factors in the environment like nutrient availability. While these studies suggest that this is indeed occurring, what is exactly happening at the genetic level still needs to be examined.
The role of maternal nutrition seems well-established, but what about the paternal nutrition? While the father’s nutrition has been examined for its role in infertility, it has not been studied extensively for its influence in embryonic development.
Life-style or Fetal Origins of Disease?
Scientific evidence suggests that adult metabolic diseases may be the result of the nutritional environment both before conception and throughout gestation. But we shouldn’t point fingers at moms just yet. Prenatal nutrition is just one factor among many that may influence human development and metabolism. It is clear that adult lifestyle factors such as smoking, diet, and exercise also contribute to chronic disease risk. Thus, metabolic disease is likely caused by a combination of prenatal development and adult lifestyle factors. Maintaining a healthy weight and eating a nutritious diet with complete vitamins and minerals is therefore important for mothers, fathers, and children alike.
But we shouldn’t point fingers at moms just yet. Prenatal nutrition is just one factor among many that may influence human development and metabolism. It is clear that adult lifestyle factors such as smoking, diet, and exercise also contribute to chronic disease risk. Thus, metabolic disease is likely caused by a combination of prenatal development and adult lifestyle factors. Maintaining a healthy weight and eating a nutritious diet with complete vitamins and minerals is therefore important for mothers, fathers, and children alike.
–Megan Lee, Harvard School of Public Health Alumna
Your baby was born prematurely | Regional Perinatal Center
Premature babies
If your baby is born too early, the joy of having a baby can be overshadowed by health concerns and thoughts about the possible consequences.
Instead of returning home with the baby, holding him and caressing him, you will have to stay in the department, learn to cope with the fear of touching the baby, realize the need for treatment and various manipulations, get used to the complex equipment that surrounds him.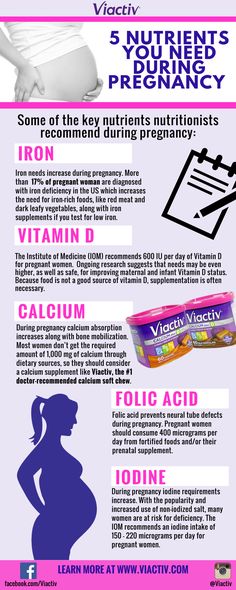
In this situation, not only your baby needs help, you need it too! The best assistants are your loved ones, their love and care, as well as professional advice and recommendations from doctors and psychologists. This section of articles will help you improve your knowledge of preterm infant care, development and nutrition.
Your help for the baby
Previously, parents were often not allowed into the neonatal unit and, especially, into the intensive care unit because of the fear of infection of the baby, but now the contact of the parent with the child is recognized as desirable and is prohibited only in exceptional cases (for example, if parents have acute infections)
Close communication between you and your baby is very important from the first days of his life. Even very immature premature babies recognize the voices and feel the touch of their parents.
The newborn needs this contact. Studies have shown that it greatly contributes to the faster adaptation of an immature child to new conditions and the stabilization of his condition. The baby's resistance to therapy increases, he absorbs large amounts of food and quickly begins to suck on his own. Contact with the child is important for parents. Taking part in the care of the baby, they feel their involvement in what is happening and quickly get used to a new role, especially when they see how he reacts to their presence.
The baby's resistance to therapy increases, he absorbs large amounts of food and quickly begins to suck on his own. Contact with the child is important for parents. Taking part in the care of the baby, they feel their involvement in what is happening and quickly get used to a new role, especially when they see how he reacts to their presence.
By constantly and attentively observing the baby, parents can notice the smallest changes in his condition before others. In addition, communication in the hospital is a good practice that will undoubtedly come in handy after discharge. For parents, early physical contact with the baby is very valuable, because it allows them to feel him, despite the incubator and other obstacles, and show him their love.
Treatment in the neonatal intensive care unit requires parents to have full confidence in all medical staff.
Nursing premature babies in the hospital
Many premature babies cannot breathe, suckle and regulate their body temperature sufficiently after birth. Only in the last weeks of pregnancy is the maturation of the lungs, gastrointestinal tract, kidneys, brain, which regulates and coordinates the work of all organs and systems.
Only in the last weeks of pregnancy is the maturation of the lungs, gastrointestinal tract, kidneys, brain, which regulates and coordinates the work of all organs and systems.
Fluid loss due to the immaturity of the skin of premature babies and the insufficiency of thermoregulation processes require constant attention. Modern approaches focused on nursing premature babies help to cope with these problems.
Heat regulation incubator
Premature babies are very susceptible to temperature fluctuations. At the same time, clothing can interfere with the monitoring of the baby's condition and its treatment. That is why an incubator is used to provide the conditions necessary for premature babies. It maintains a certain temperature and humidity, which change as the child grows. When the body weight of a premature infant reaches 1500-1700 g, he can be transferred to a heated bed, and after reaching a weight of 2000, most premature babies can do without this support. There are no strict rules here: when nursing children with low body weight, doctors are guided by the severity of the condition of each premature baby and its degree of maturity.
There are no strict rules here: when nursing children with low body weight, doctors are guided by the severity of the condition of each premature baby and its degree of maturity.
In incubators, very young premature babies are placed in special "nests" - soft hemispheres in which the baby feels comfortable and assumes a position close to intrauterine. It must be protected from bright lights and loud noises. For this purpose, special screens and coatings are used.
Critical treatments during the first days of life of premature babies with low and very low birth weight:
Use of an incubator or heated bed.
Oxygen supply for respiratory support.
If necessary, artificial ventilation of the lungs or breathing using the CPAP system.
Intravenous administration of various drugs and fluids.
Carrying out parenteral nutrition with solutions of amino acids, glucose and fat emulsions.
Don't worry: not all premature babies need such extensive treatment!
Mechanical ventilation and CPAP for respiratory support
When it comes to nursing, oxygen supply is of the utmost importance for premature babies. In a child born before the 34-35th week of pregnancy, the ability of the lungs to work independently is not yet sufficiently developed. The use of a constant flow of air with oxygen, which maintains a positive airway pressure (CPAP), leads to an increase in blood oxygen saturation.
In a child born before the 34-35th week of pregnancy, the ability of the lungs to work independently is not yet sufficiently developed. The use of a constant flow of air with oxygen, which maintains a positive airway pressure (CPAP), leads to an increase in blood oxygen saturation.
This new method made it possible for the majority of even very immature children to do without mechanical ventilation. The need for intubation of children has disappeared: during treatment with CPAP, oxygen is supplied through short tubes - cannulas that are inserted into the nasal passages. CPAP or mechanical ventilation is continued until the lungs can function at full capacity on their own.
In order for the lungs to expand and remain in such a state in the future, a surfactant is needed - a substance that lines the alveoli from the inside and reduces surface tension. Surfactant is produced in sufficient quantities starting from the 34-35th week of pregnancy. Basically, it is by this time that the formation of the lungs is completed. If the baby was born earlier, modern technologies allow the introduction of surfactant into the lungs of premature babies immediately after their birth.
If the baby was born earlier, modern technologies allow the introduction of surfactant into the lungs of premature babies immediately after their birth.
Parenteral nutrition - administering nutrient solutions by vein
Premature babies, especially those born weighing less than 1500 g, are not able to get and absorb enough nutrients, even when fed through a tube. For the rapid growth of the baby, a large amount of nutrition is needed, and the size of the stomach is still very small, and the activity of digestive enzymes is also reduced. Therefore, such children are given parenteral nutrition.
Special nutrients are injected into a vein using infusion pumps that deliver solutions slowly at a predetermined rate. In this case, amino acids necessary for building proteins, fat emulsions and glucose, which are sources of energy, are used. These substances are also used for the synthesis of a number of hormones, enzymes and other biologically active substances.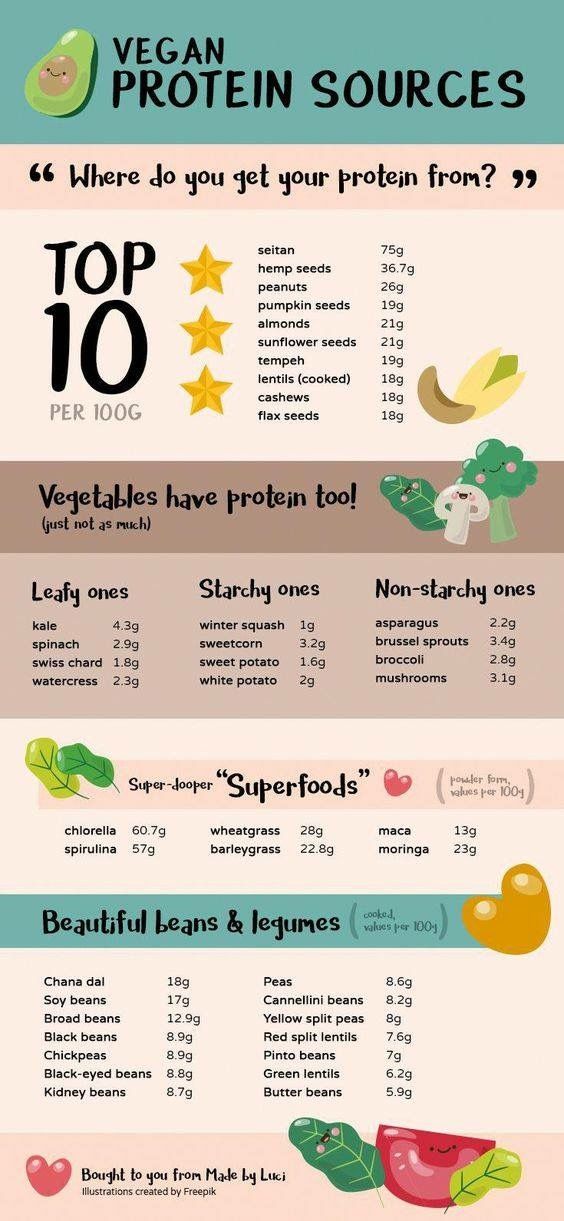 Additionally, minerals and vitamins are introduced.
Additionally, minerals and vitamins are introduced.
Gradually, the volume of enteral nutrition increases, and parenteral nutrition decreases until it is completely canceled.
Premature infants with gastrointestinal disease require parenteral nutrition for a longer period of time.
By the time your grown baby is discharged from the hospital, everything should be well prepared at home. And this applies not only to the environment, clothes and means of caring for the child.
All family members must be ready to receive the baby. Of course, the main care will fall on the shoulders of the parents. Although you have already gained some experience in the hospital, it is important to feel the support of others, especially in the early days.
Older children can also help. The discharge of your baby is a great joy that you want to share with all your relatives.
While you are getting used to your new role, it is important that nothing distracts you from communicating with your child.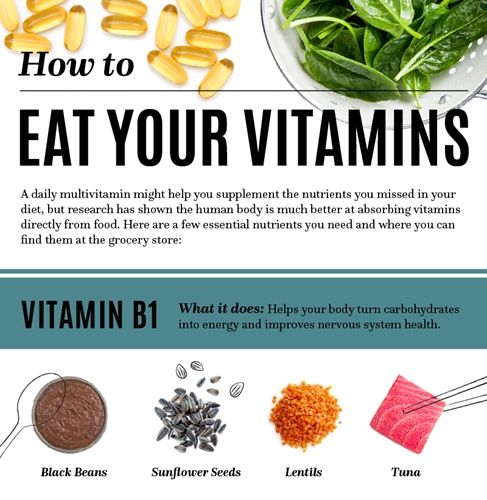 Now all the care and responsibility for the baby lies entirely with you. Everything you need to take care of him should be at hand.
Now all the care and responsibility for the baby lies entirely with you. Everything you need to take care of him should be at hand.
Preparing for discharge from the hospital
Before discharge, you must make sure that:
- Prepared the crib, bath for bathing and a place for changing clothes, preferably a changing table. A crib should be placed in the parents' bedroom, the child should not be left alone even at night. A stroller is also required. you have baby milk that was recommended by the doctor before discharge (if the child is on mixed or artificial feeding). As a rule, this is a specialized medical product. You need a certain number of small bottles and teats of the appropriate size, as well as a sterilizer. All premature babies will need pacifiers.
- You have fully mastered breastfeeding or bottle feeding.
- If your baby is not suckling all the required amount of milk from the breast and is supplementing from a bottle, you have purchased a breast pump that you have learned to use; you may also need it if you have a lot of breast milk.

- You have asked your doctor how often your child's weight should be monitored.
- If your baby still needs medication, you have the required amount at home. And you know exactly how and when to give them to your child.
- You know which warning signs to look out for.
- After the baby is discharged, a pediatrician and a neonatologist will look after the baby, to whom you will give the discharge summary from the hospital.
- You know how the hospital from which your child is being discharged will provide follow-up care after discharge.
- You know which specialists and how often should examine your baby (oculist, neuropathologist, etc.).
- All the emergency phone numbers you need are at your fingertips.
When can a child go home
This question is very difficult to answer because all children are different. The stay in the hospital can last from 6 days to 6 months, depending on the degree of prematurity of the child, the severity of his condition, as well as the presence of certain complications.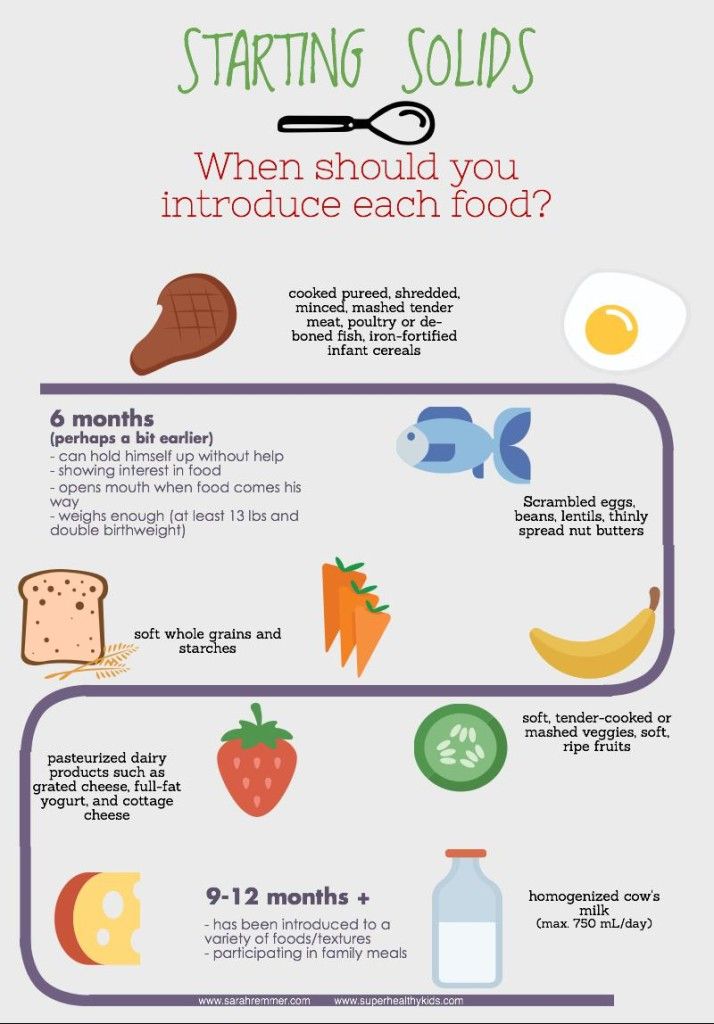
Of course, all parents look forward to the moment when the baby can be brought home. Long-term nursing of a premature baby is often a difficult test for you. But we must not forget that safety comes first, and the baby can be discharged home only when the doctors are confident in the stability of his condition. It is certainly in your interest as well.
The rate of increase in body weight and length
Weight gain is the main indicator of the growth of the baby and the adequacy of the treatment. The weight of the child, especially in the first days and weeks of life, is influenced by a number of factors: the presence of milk in the stomach (immediately after feeding), the time of bowel movement, the degree of filling of the bladder, the presence of edema. Therefore, if an edematous child does not gain weight for several days, and perhaps even loses it, do not worry. It should be remembered that children grow unevenly and periods of high weight gain alternate with lower ones. It is better to focus not on weight gain per day, but on the dynamics of this indicator over several days or a week.
It is better to focus not on weight gain per day, but on the dynamics of this indicator over several days or a week.
It is currently accepted that in the interval corresponding to 28-34 weeks of pregnancy, the normal weight gain of the child is 16-20 g/kg per day. Then it is reduced to 15 g/kg.
It is also important to take into account the rate of increase in body length. With malnutrition, at first the child gains less weight (or even loses it), and with a more pronounced deficiency of nutrients, his growth is also disturbed.
The weight must not only increase at a certain rate, but must also correspond to the length of the baby. An important parameter characterizing the development of the baby is an increase in the circumference of the head. The brain most actively increases in size during the first 12–18 months of life. But an excessively rapid increase in head circumference, as well as a slowdown in its increase, indicate neurological disorders.
A premature baby can be discharged from the hospital if:
- he is able to independently maintain the required body temperature;
- does not need breathing support and constant monitoring of the work of the respiratory and cardiovascular systems;
- can suck out the required amount of nutrition on its own;
- does not need round-the-clock monitoring and frequent determination of biochemical or other indicators;
- supportive care can be provided at home;
- he will be under the supervision of a local pediatrician and neonatologist at the place of residence.
The decision to discharge home is made for each patient individually. In addition to the state of health of the baby, the degree of preparedness of parents, their ability to provide high-level care for a premature baby is also taken into account.
Feeding a premature baby after discharge
Breastfeeding is the ideal way to feed premature babies.
However, if the baby was born much prematurely and his birth weight did not exceed 1800-2000 g, his high nutritional requirements cannot be met by breastfeeding. The growth rate will be insufficient. Moreover, over time, the content of many nutrients, including protein, in milk decreases. And it is the main material for building organs, and primarily brain tissue. Therefore, proteins must be supplied to the body of a premature infant in the optimal amount.
In addition, premature babies have a significantly increased need for calcium and phosphorus, which are essential for bone formation.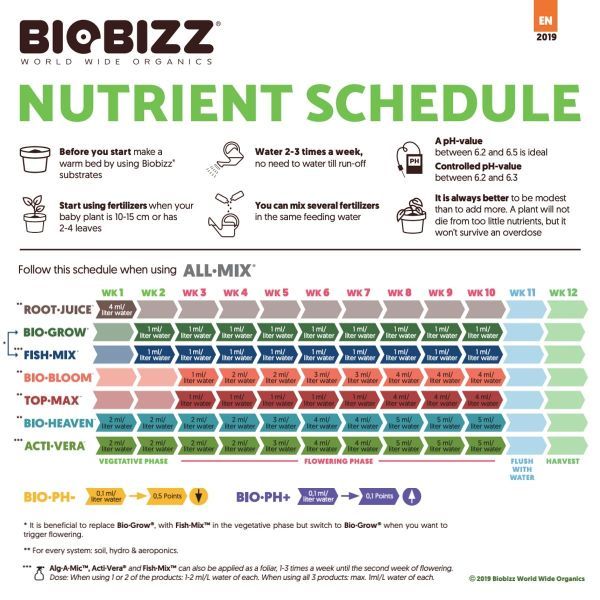
In order for the baby's nutrition to be complete even after being discharged from the hospital, special additives - "enrichers" are introduced into breast milk in a certain amount, already less than in the hospital. They make up for the lack of protein in it, as well as some vitamins and minerals. As a result, the child receives them in the optimal amount. The duration of their use will be determined by your doctor. If there is not enough milk or it does not exist at all, children born prematurely should be transferred to artificial feeding. Complementary feeding of premature babies is carried out with special children's dairy products designed for children with low birth weight. This baby milk is ideally suited to both the ability of immature children to digest and assimilate nutrients, and their needs.
Premature infant milk contains more protein, fat and carbohydrates than term infant milk, resulting in a higher calorie content. In specialized baby milk, the concentration of many minerals is higher, especially iron, zinc, calcium, phosphorus, as well as vitamins, including vitamin D. Long-chain polyunsaturated fatty acids of the Omega-3 and Omega-6 classes are introduced into such products, which are necessary for proper development of the brain and organ of vision, as well as nucleotides that contribute to the optimal development of immunity. However, when the child reaches a certain weight (2000-2500 g), you should gradually switch to feeding with standard baby milk, but not completely. Specialized baby milk can be present in the diet of a premature baby for several months. This time, as well as the volume of the product, will be determined by the doctor. He will answer all your questions about how to feed your baby.
Long-chain polyunsaturated fatty acids of the Omega-3 and Omega-6 classes are introduced into such products, which are necessary for proper development of the brain and organ of vision, as well as nucleotides that contribute to the optimal development of immunity. However, when the child reaches a certain weight (2000-2500 g), you should gradually switch to feeding with standard baby milk, but not completely. Specialized baby milk can be present in the diet of a premature baby for several months. This time, as well as the volume of the product, will be determined by the doctor. He will answer all your questions about how to feed your baby.
At present, specialized children's dairy products have been developed and are being used to feed premature babies after discharge from the hospital. In its composition, it occupies an intermediate position between a specialized product for premature babies and regular baby milk. Your baby will be transferred to such baby milk while still in the hospital. You will continue to give it to your child at home, and the doctor, watching him, will tell you when it will be possible to switch to regular standard baby milk. If the baby was born with a very low body weight or is poorly gaining weight, special baby milk can be used for a long time - up to 4 months, 6 or even 9months. The beneficial effect of such children's dairy products on the growth and development of the child has been proven in scientific studies.
You will continue to give it to your child at home, and the doctor, watching him, will tell you when it will be possible to switch to regular standard baby milk. If the baby was born with a very low body weight or is poorly gaining weight, special baby milk can be used for a long time - up to 4 months, 6 or even 9months. The beneficial effect of such children's dairy products on the growth and development of the child has been proven in scientific studies.
Feeding needs for premature babies
Higher caloric intake because they need to gain weight faster than term babies.
More protein as premature babies grow faster.
More calcium and phosphorus for bone building.
More trace elements and vitamins for growth and development.
A premature baby grows faster than a term baby. Nutrition for such children is calculated taking into account body weight at birth, the age of the baby and its growth rate. As a rule, the calorie content of the daily diet is about 120-130 calories per 1 kg of body weight.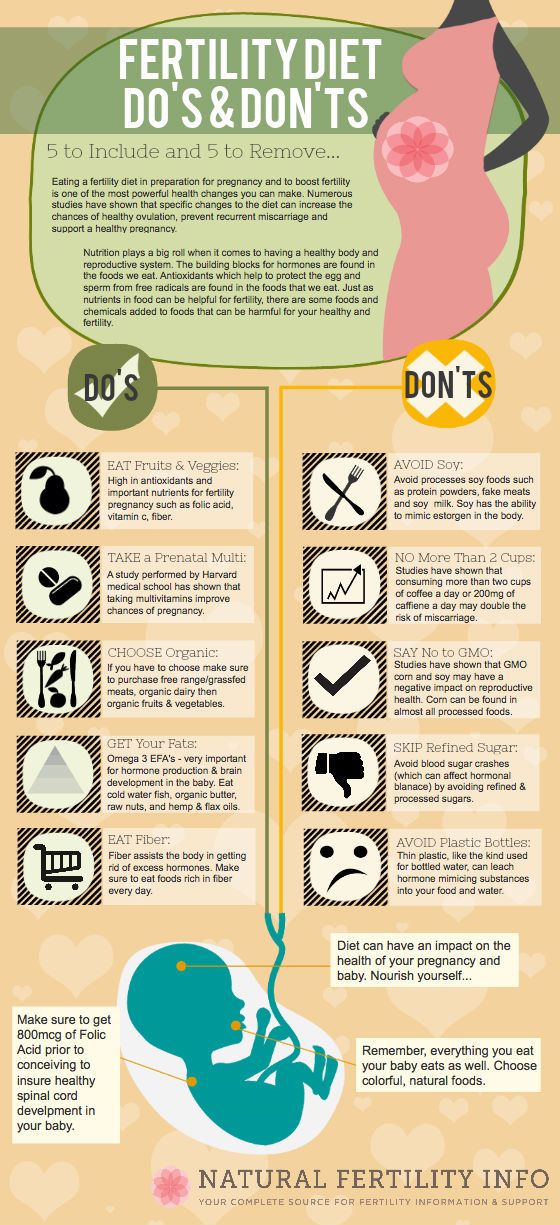
It is very important that your baby continues to gain weight quickly and grow in length after discharge. To do this, feeding premature babies must be carried out using a specialized fortified diet prescribed by a doctor.
when children learn to eat carefully, why it is important not to rush a child
Published: 08/13/2020
Reading time: 4 min.
Number of reads: 18759
Author of the article: Ponomareva Yulia Vladimirovna
Pediatrician, Candidate of Medical Sciences, Allergist-Immunologist
Nutrition is one of the most important functions of a person, which is absolutely necessary for his life. But the growth and harmonious development of the child depend not only on the provision of nutrients, but also determined by the proper organization of food intake.
Transition
Once complementary foods are introduced, the baby begins to adapt to foods other than breastmilk, getting used to foods and learning eating habits that will be ingrained and implemented for the rest of his life. It is in the second half of life that the baby begins to eat on his own, his gradual socialization and transition to a common family table take place. Focusing on the eating behavior of the mother and other close relatives, the baby tries to imitate, seeks to try adult food, gains his own experience and forms taste preferences. This stage is very important in human development. It determines taste preferences in the future, the attitude to the procedure for eating, and in case of unfavorable developments, it can be the cause of persistent appetite disorders.
It is in the second half of life that the baby begins to eat on his own, his gradual socialization and transition to a common family table take place. Focusing on the eating behavior of the mother and other close relatives, the baby tries to imitate, seeks to try adult food, gains his own experience and forms taste preferences. This stage is very important in human development. It determines taste preferences in the future, the attitude to the procedure for eating, and in case of unfavorable developments, it can be the cause of persistent appetite disorders.
A difficult period
None of us was born with the ability to use a spoon, fork and drink from a cup. These skills are acquired with the help of adults, and it is their behavior that determines how quickly and successfully, and most importantly, how psychologically comfortable a child will master the difficult science of behavior at the table. Parents should be patient, show respect for the child and understand that it will take a long time before the baby masters the skills of eating. Of course, at first, a little researcher will study food by touch, try to smear it on the table and turn the plate over. Be calm about his experiments, but continue to teach him persistently, helping him use tableware and educating him by your own example. The more confident children begin to use a spoon, the less difficulty they have in eating, and the more successfully their diet expands.
Of course, at first, a little researcher will study food by touch, try to smear it on the table and turn the plate over. Be calm about his experiments, but continue to teach him persistently, helping him use tableware and educating him by your own example. The more confident children begin to use a spoon, the less difficulty they have in eating, and the more successfully their diet expands.
Preparatory stage
For self-feeding, the child should have a specially equipped place - the most popular and convenient highchairs for feeding. Initially, the child will eat at his table, and then by the end of the first year of life, you can move the high chair to the family table.
This is important! To successfully master the skills of eating, children should have their own comfortable spoon and stable plate. It is advisable to use a medium-sized spoon, shallow, with a non-slip thickened handle. The first cutlery should not have sharp edges so that the baby does not hurt the gums. Dishes must be selected from environmentally friendly and safe materials.
Dishes must be selected from environmentally friendly and safe materials.
A number of modern spoons have temperature-sensitive sensors, which can be useful for monitoring the temperature of food. Use a plate with a high rim to help your child scoop up food more easily. To make the dishes less slippery, choose plates with a wide base or use special devices in the form of a rubber bottom or suction cups.
See also: At what age should a child be introduced to complementary foods? This will be a positive reinforcement in his learning. Mom needs to sit directly facing the child and offer a spoon, trying to make him take it with his leading hand. While holding the baby's wrist and elbow, try scooping up some food and directing it towards the mouth. Then return the spoon to the plate. As practice and learning improves, gradually decrease your help by moving your supporting hand away from the child's wrist toward the child's elbow, and then let the child try to do without assistance.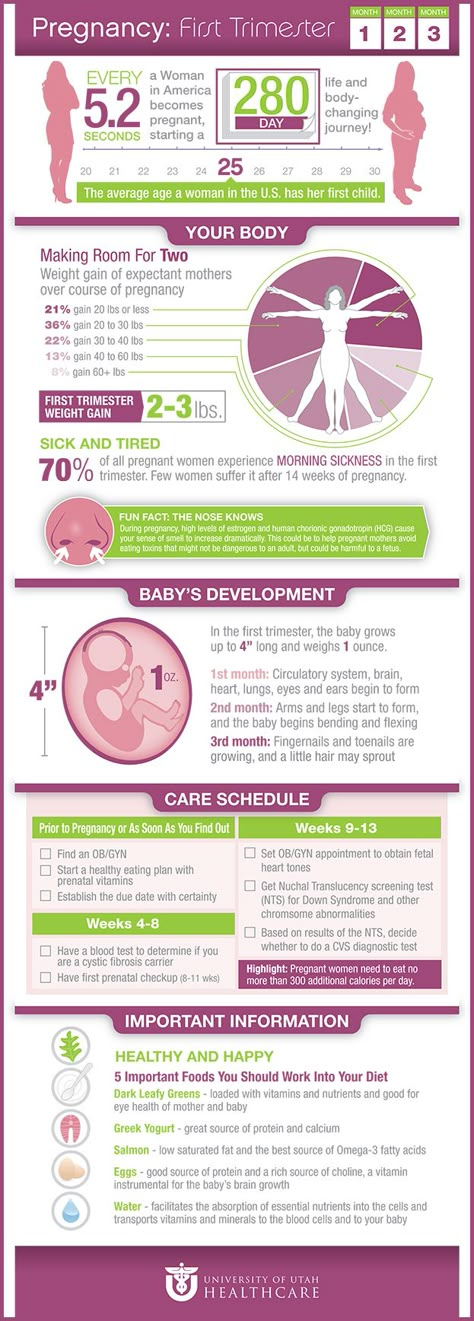
Of course, not everything will work out right away. For a long time, the baby will try to eat with his hands, put food in a spoon with his fingers, or help with the other hand to bring the spoon to his mouth. Praise and openly rejoice in his success.
IMPORTANT! Remember that children experience great emotional stress when they learn to eat on their own, so do not keep them at the table for a long time and even scold them for slowness and untidiness. Another very important point is to encourage independence. Do not take the spoon away from the child in an attempt to speed up the process. And do not be afraid that the baby will eat less - after a while he will get hungry again and happily eat the next portion.
Drinks
The modern market of goods is replete with various devices for feeding babies: from bottles to various drinkers. However, child nutrition experts recommend teaching your child to drink from a cup. In the first year of life, a child has a pronounced sucking reflex, so when using a bottle or drinker, he can drink more than he needs. The glass or cup should be lightweight and made of materials that do not crack or break. Some kids prefer to drink with their hands around a glass, others are more comfortable holding on to the handle of a mug - try different options, choosing the most convenient one. At the initial stage, the adult brings the cup to his mouth and, leaning it against his lips, slowly tilts it. Pour liquid only a third of the volume - the child will not choke, but there will be no need to throw back his head. The next step is to help the baby - hold his wrists and direct his hands with a glass to his mouth. Teach him to keep his head upright while drinking. And the next step is to try drinking on your own.
The glass or cup should be lightweight and made of materials that do not crack or break. Some kids prefer to drink with their hands around a glass, others are more comfortable holding on to the handle of a mug - try different options, choosing the most convenient one. At the initial stage, the adult brings the cup to his mouth and, leaning it against his lips, slowly tilts it. Pour liquid only a third of the volume - the child will not choke, but there will be no need to throw back his head. The next step is to help the baby - hold his wrists and direct his hands with a glass to his mouth. Teach him to keep his head upright while drinking. And the next step is to try drinking on your own.
Simple rules
- It is very important to create the right nutritional stereotype for the child. Before eating, remove toys from sight, do not turn on the TV.
- Try to create a calm and friendly atmosphere at the table. Eating should not be associated with stress and negative emotions.