How to speed up early labour
Speeding up labour - BabyCentre UK
In this article
- When does active labour start?
- How long is a normal labour?
- What counts as a slow labour?
- Why might my labour be slow?
- How is labour speeded up?
- Can I speed up labour myself?
- What can help me to cope with a long labour?
When does active labour start?
Midwives and doctors say the active first stage of your labour starts when:
- you are having regular, powerful contractions and
- your cervix is dilating from 4cm (1.6in) onwards (NCCWCH 2014).
This may surprise you, as you may start to have strong tightenings well before reaching this point. You may have been awake all night and feeling as though labour has been under way for a while.
Pacing yourself in early labour may help you cope better when active labour gets under way (RCM 2018). Find out how to get through early labour at home.
How long is a normal labour?
Every labour is different, but there are average times that may help to guide you.
Early labour (before it gets active) often lasts about nine hours to 12 hours (Tilden et al 2019). It’s common for it to be longer for first-time mums, lasting 18 hours or more (Ängeby et al 2018).
The active first stage of labour (when your cervix is dilating from 4cm and you are having regular, powerful contractions) for a first baby is usually about eight hours, but it could be shorter or longer (NCCWCH 2014).
If this isn't your first baby, you may have a shorter labour, though this isn't guaranteed. For women who have given birth before, the active first stage of labour lasts, on average, for five hours (NCCWCH 2014). It's unlikely to last for more than 12 hours (NCCWCH 2014).
The pushing phase of labour (active second stage) shouldn't usually take more than three hours, or two hours if you've had a baby before (NCCWCH 2014).
Bear in mind that a quick labour isn't necessarily better either for you or your baby (Rimmer 2014). Very fast labours can be physically and emotionally challenging (Rimmer 2014). However, a very slow labour can leave you exhausted and unwell (Harper et al 2014).
What counts as a slow labour?
During active labour there may be an hour or so of slow or little progress, followed by periods of faster progress (Ehsanipoor and Satin 2019). What matters is how your labour progresses over several hours.
If your labour is straightforward, your midwife will assess your labour every four hours (NCCWCH 2014). With your permission, she'll carry out a vaginal examination to check how open your cervix is (NCCWCH 2014, RCM 2012a, RCN 2016). She'll also listen to your baby's heartbeat using a hand-held Doppler (a Sonicaid) or an ear trumpet (a Pinard stethoscope).
A four-hourly check gives your midwife a good overview of how you're doing. Assessing you more often than that won't necessarily help her to understand more, and can lead to unnecessary intervention in your labour (NCCWCH 2014).
Assessing you more often than that won't necessarily help her to understand more, and can lead to unnecessary intervention in your labour (NCCWCH 2014).
However, if you've had any health concerns during this or a previous pregnancy you may need continuous monitoring.
Your doctor or midwife will also want to monitor you if you've developed complications, such as meconium (your baby’s first poo) in your waters, or fresh bleeding (NCCWCH 2014).
Your midwife will place two electronic sensors on your bump, one to measure contractions and one to measure your baby's heartbeat. The sensors will remain there throughout your labour. Your midwife will still only check your cervix every four hours, though.
If your cervix isn't dilating at a rate of at least 0.5cm (0.2in) an hour over a four-hour period, speeding up your labour may be an option (NCCWCH 2014). This is also called augmentation of labour. Your midwife will discuss whether or not to speed up your labour with you and your doctor.
Each woman's labour is unique. Your wishes should be taken into account, along with what your midwife and doctor recommend is best for you and your baby (Jackson et al 2014, NCCWCH 2014).
Why might my labour be slow?
Some labours are just slow for no particular reason. However, you may have a slow labour if:
- You're dehydrated or exhausted (NCCWCH 2014).
- The position of your baby is making it harder for your labour to progress (NCCWCH 2014).
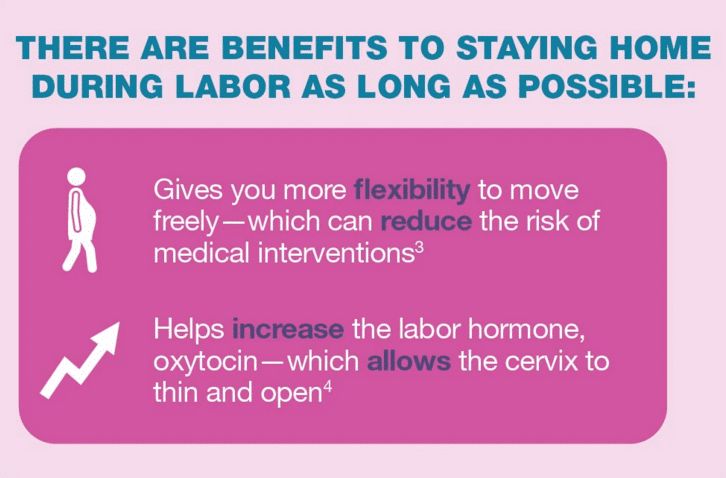
- You feel particularly scared or anxious. These emotions tend to interfere with the release of the hormone oxytocin, which can help labour along (Aral et al 2014, Simkin and Ancheta 2011).
- Your contractions are infrequent, not very strong, or staying at the same intensity rather than getting stronger (NCCWCH 2014).
- You've had interventions that have slowed your contractions. These could include having to stay still for periods of time, or having an epidural (NCCWCH 2014).
Bear in mind that the first 5cm of cervix dilation nearly always takes much longer than the second 5cm (Ehsanipoor and Satin 2019, Jackson et al 2014, Simkin and Ancheta 2011). Your cervix opens more quickly as your contractions get stronger.
How is labour speeded up?
If your midwife asks whether you'd like to have your labour speeded up, take time to consider your options. If your baby is fine, and your cervix is gradually opening up, even if it's happening slowly, it may be best to leave things alone. You may be perfectly happy to take things gently, staying in tune with your body and your baby.
Or you may be so exhausted that you really want your baby to be born quickly. If that's the case, your midwife can help to move things along in the following ways:
Breaking the waters
Your midwife may suggest breaking your waters to speed up your labour (NCCWCH 2014). This isn't usually recommended near the beginning of labour, as it could increase your risk of infection if labour doesn't start right away (NCCWCH 2008).
This isn't usually recommended near the beginning of labour, as it could increase your risk of infection if labour doesn't start right away (NCCWCH 2008).
However, if the active stage of labour slows right down, breaking your waters can help to get things going again. It may shorten labour by about an hour (NCCWCH 2014).
If you agree to the procedure, here's how your midwife will do it. Once you're on the bed, she'll remove the last section of the bed so that your bottom is right at the end. She may ask you to put your legs up in stirrups, or just hold them apart.
Your midwife will then make a small break in the membranes around your baby. She'll use a long thin probe (amnihook) or a medical glove with a pricked end on one of the fingers (amnicot). She'll scratch the membrane until it bursts and the waters flow out into a tray placed underneath the bed.
This procedure isn't painful but it can be very uncomfortable. You'll probably be glad to get up again once it's over.
Your midwife will then check your baby's heartbeat using a Sonicaid or ear trumpet, to make sure that breaking the waters hasn't distressed him.
Your contractions may become much stronger after your waters have been broken (NCCWCH 2014). Be prepared to work hard with breathing and relaxation exercises. Or you can ask your midwife for some pain relief, such as gas and air, if you need extra help.
Hormone drip
If moving around or breaking your waters doesn't speed up your labour, your doctor may suggest a hormone drip to boost your contractions (NCCWCH 2014). This will contain Syntocinon, which is an artificial form of the labour hormone oxytocin.
If you have Syntocinon, your midwife will continuously monitor your baby's heartbeat by strapping electronic sensors to your tummy (NCCWCH 2014).
Your midwife may also recommend attaching a small clip to your baby's head. The clip is called a fetal scalp electrode and it may provide a more accurate reading than placing a sensor on your tummy. It also allows you to move around more easily.
It also allows you to move around more easily.
Continuous monitoring is recommended because Syntocinon can over-stimulate your womb (uterus) (NCCWCH 2014). You may get very strong, frequent contractions, which could distress your baby.
You're also more likely to need help from pain-relieving drugs to cope with these artificially induced contractions. For this reason, your midwife should offer you an epidural before she starts a Syntocinon drip (NCCWCH 2014).
Can I speed up labour myself?
If you'd prefer not to have your waters broken, or a hormone drip, there are some natural techniques you could try to speed up your labour
- If you're lying on the bed, get up! Being upright and mobile may strengthen your contractions, while also helping you to cope with them (Lawrence et al 2013).
- Take a walk to the toilet. A full bladder may slow down your labour by getting in the way of your baby's head descending (Simkin and Ancheta 2011).

- If you have access to one, get into a warm bath or birth pool. This can reduce your need for an epidural or spinal pain relief (Cluett et al 2018).
- If your baby is lying back-to-back, an experienced midwife may advise you to lie on your side or try kneeling or standing lunge positions. This may help your baby to rotate to a better position for birth (Simkin and Ancheta 2011).
- Have some private time with your partner. Turn the lights down low and have a cuddle, with some nipple stroking or breast massage. This may help your body to release oxytocin, the hormone that strengthens your contractions (Simkin and Ancheta 2011).
You could also try acupuncture during your labour (Mollart et al 2015,Simkin and Ancheta 2011). Complementary therapies probably work best if used throughout labour. You may be able to request an acupuncturist if your labour has slowed down. In some areas of the UK, acupuncturists specialising in childbirth work in teams, meaning that a practitioner is always available.
You can also ask your midwife whether she's certified in any complementary therapies, such as aromatherapy massage, that could help you.
How to help your baby be born
How can you speed up labour and make the birth easier? Discover how to help your baby be born more quickly.More preparing for birth videos
What can help me to cope with a long labour?
These methods may help you:
- Use breathing and relaxation techniques to help you stay calm and focused (NCCWCH 2014). If you've been taking hypnobirthing classes, this is the time to use everything you've learned!
- Ask your birth partner to massage your back, or your feet, if you're sitting in a chair (NCCWCH 2014, Smith et al 2018).
- Listen to your favourite music (NCCWCH 2014).
- Eat and drink when you need to. Have a small snack, such as toast, and water, or an isotonic drink, to stay hydrated (NCCWCH 2014).
- Change your position.
 Later in labour you may not feel like walking around, but your midwife can help you to find a comfortable position (NCCWCH 2014).
Later in labour you may not feel like walking around, but your midwife can help you to find a comfortable position (NCCWCH 2014). - Listen to your body and try different positions (Simkin and Ancheta 2011). Move around or adopt positions that feel most comfortable to you as labour progresses (NCCWCH 2014).
- Ask your midwife to explain what's going on. If you feel involved and in control of your labour, you'll probably feel less anxious and more relaxed. This may make your labour easier to cope with, and you may find it a more positive experience (NCCWCH 2014).
- If your midwife is caring for other women as well as you because the unit is busy, continuous support from a student midwife may help your labour to progress. Your birth partner could ask if there's any extra help available (Bolbol-Haghighi et al 2016).
Learn more about what to expect from each stage of labour.
References
Aral I, Koken G, Bozkurt M, et al. 2014. Evaluation of the effects of maternal anxiety on the duration of vaginal labour delivery. Clin Exp Obstet Gynecol 41(1):32-6
2014. Evaluation of the effects of maternal anxiety on the duration of vaginal labour delivery. Clin Exp Obstet Gynecol 41(1):32-6
Bolbol-Haghighi N, Masoumi SZ, Kazemi F. 2016. Effect of continued support of midwifery students in labour on the childbirth and labour consequences: a randomized controlled clinical trial. J Clin Diagn Res 10(9): QC14–QC17. www.ncbi.nlm.nih.gov [Accessed September 2019]
Cluett ER, Burns E, Cuthbert A. 2018. Immersion in water during labour and birth. Cochrane Database of Systematic Reviews (5): CD000111. www.cochranelibrary.com [Accessed September 2019]
Ehsanipoor MD, Satin AJ. 2019. Normal and abnormal labor progression. UpToDate. www.uptodate.com [Accessed September 2019]
Harper LM, Caughey AB, Roehl KA, et al. 2014. Defining an abnormal first stage of labor based on maternal and neonatal outcomes. Am J Obstet Gynecol (210(6):536.e1-7. www.ncbi.nlm.nih.gov [Accessed September 2019]
Jackson K, Marshall JE, Brydon S. 2014. Physiology and care during the first stage of labour. In: Marshall JE, Raynor MD. eds. Myles Textbook for Midwives. 16th ed. Edinburgh: Churchill Livingstone, 327-66
2014. Physiology and care during the first stage of labour. In: Marshall JE, Raynor MD. eds. Myles Textbook for Midwives. 16th ed. Edinburgh: Churchill Livingstone, 327-66
Lawrence A, Lewis L, Hofmeyr GJ, et al. 2013. Maternal positions and mobility during first stage labour. Cochrane Database of Systematic Reviews (10): CD003934. www.cochranelibrary.com [Accessed September 2019]
Mollart LJ, Adam J, Foureur M. 2015. Impact of acupressure on onset of labour and labour duration: a systematic review. Women Birth 28(3): 199-206
NCCWCH. 2014. Intrapartum care: care of healthy women and their babies during childbirth. National Collaborating Centre for Women's and Children's Health, Clinical guideline, 190. www.nice.org.uk [Accessed September 2019]
RCM. 2012a. Assessing progress in labour. Royal College of Midwives Trust, Evidence based guidelines for midwifery-led care in labour
RCM. 2012b. Rupturing membranes. Royal College of Midwives Trust, Evidence based guidelines for midwifery-led care in labour
RCM. 2018. Midwifery care in labour guidance for all women in all settings. Royal College of Midwives, Midwifery Blue Top Guidance
2018. Midwifery care in labour guidance for all women in all settings. Royal College of Midwives, Midwifery Blue Top Guidance
RCN. 2016. Genital examination in women. Royal College of Nursing. www.rcn.org.uk [Accessed September 2019]
Rimmer A. 2014. Prolonged pregnancy and disorders of uterine action. In: Marshall JE, Raynor MD. eds. Myles textbook for midwives 16th ed. Edinburgh: Churchill Livingstone, 417-33
Simkin P, Ancheta R. 2011. The labor progress handbook: early interventions to prevent and treat dystocia. 3rd ed. Chichester: Wiley Blackwell
Smith CA, Levett KM, Collins CT, et al. 2018. Massage, reflexology and other manual methods for pain management in labour. Cochrane Database of Systematic Reviews (3): CD009290. www.cochranelibrary.com [Accessed September 2019]
Smyth RMD, Markham C, Dowswell T. 2013. Amniotomy for shortening spontaneous labour. Cochrane Database of Systematic Reviews (6): CD006167. www. cochranelibrary.com [Accessed September 2019]
cochranelibrary.com [Accessed September 2019]
Thakar R, Sultan AH. 2014. The female pelvis and the reproductive organs. In: Marshall JE, Raynor MD. eds. Myles Textbook for Midwives. 16th ed. Edinburgh: Churchill Livingstone, 55-80
Show references Hide references
Speeding up labour - BabyCentre UK
In this article
- When does active labour start?
- How long is a normal labour?
- What counts as a slow labour?
- Why might my labour be slow?
- How is labour speeded up?
- Can I speed up labour myself?
- What can help me to cope with a long labour?
When does active labour start?
Midwives and doctors say the active first stage of your labour starts when:
- you are having regular, powerful contractions and
- your cervix is dilating from 4cm (1.6in) onwards (NCCWCH 2014).
This may surprise you, as you may start to have strong tightenings well before reaching this point. You may have been awake all night and feeling as though labour has been under way for a while.
You may have been awake all night and feeling as though labour has been under way for a while.
Pacing yourself in early labour may help you cope better when active labour gets under way (RCM 2018). Find out how to get through early labour at home.
How long is a normal labour?
Every labour is different, but there are average times that may help to guide you.
Early labour (before it gets active) often lasts about nine hours to 12 hours (Tilden et al 2019). It’s common for it to be longer for first-time mums, lasting 18 hours or more (Ängeby et al 2018).
The active first stage of labour (when your cervix is dilating from 4cm and you are having regular, powerful contractions) for a first baby is usually about eight hours, but it could be shorter or longer (NCCWCH 2014).
If this isn't your first baby, you may have a shorter labour, though this isn't guaranteed. For women who have given birth before, the active first stage of labour lasts, on average, for five hours (NCCWCH 2014). It's unlikely to last for more than 12 hours (NCCWCH 2014).
It's unlikely to last for more than 12 hours (NCCWCH 2014).
The pushing phase of labour (active second stage) shouldn't usually take more than three hours, or two hours if you've had a baby before (NCCWCH 2014).
Bear in mind that a quick labour isn't necessarily better either for you or your baby (Rimmer 2014). Very fast labours can be physically and emotionally challenging (Rimmer 2014). However, a very slow labour can leave you exhausted and unwell (Harper et al 2014).
What counts as a slow labour?
During active labour there may be an hour or so of slow or little progress, followed by periods of faster progress (Ehsanipoor and Satin 2019). What matters is how your labour progresses over several hours.
If your labour is straightforward, your midwife will assess your labour every four hours (NCCWCH 2014). With your permission, she'll carry out a vaginal examination to check how open your cervix is (NCCWCH 2014, RCM 2012a, RCN 2016).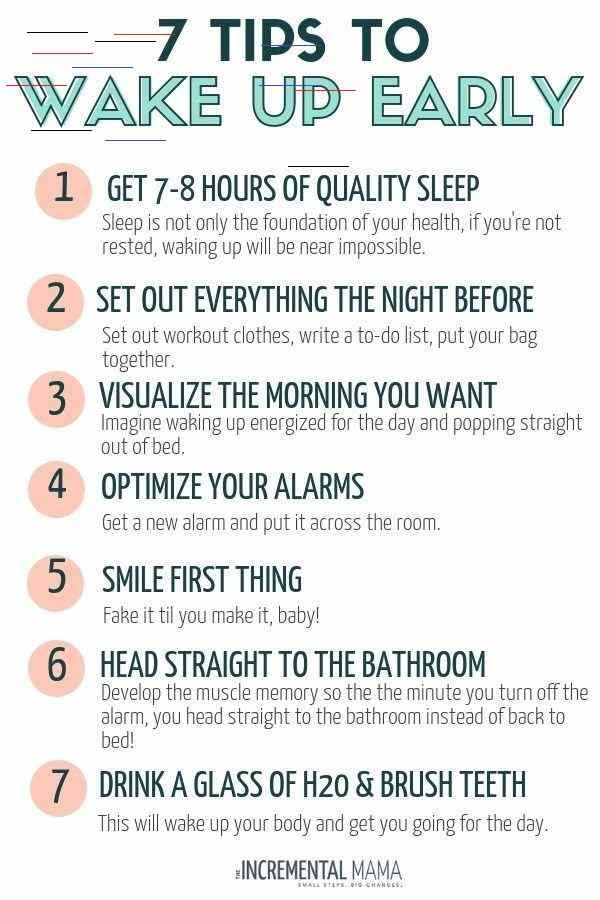 She'll also listen to your baby's heartbeat using a hand-held Doppler (a Sonicaid) or an ear trumpet (a Pinard stethoscope).
She'll also listen to your baby's heartbeat using a hand-held Doppler (a Sonicaid) or an ear trumpet (a Pinard stethoscope).
A four-hourly check gives your midwife a good overview of how you're doing. Assessing you more often than that won't necessarily help her to understand more, and can lead to unnecessary intervention in your labour (NCCWCH 2014).
However, if you've had any health concerns during this or a previous pregnancy you may need continuous monitoring.
Your doctor or midwife will also want to monitor you if you've developed complications, such as meconium (your baby’s first poo) in your waters, or fresh bleeding (NCCWCH 2014).
Your midwife will place two electronic sensors on your bump, one to measure contractions and one to measure your baby's heartbeat. The sensors will remain there throughout your labour. Your midwife will still only check your cervix every four hours, though.
If your cervix isn't dilating at a rate of at least 0.5cm (0. 2in) an hour over a four-hour period, speeding up your labour may be an option (NCCWCH 2014). This is also called augmentation of labour. Your midwife will discuss whether or not to speed up your labour with you and your doctor.
2in) an hour over a four-hour period, speeding up your labour may be an option (NCCWCH 2014). This is also called augmentation of labour. Your midwife will discuss whether or not to speed up your labour with you and your doctor.
Each woman's labour is unique. Your wishes should be taken into account, along with what your midwife and doctor recommend is best for you and your baby (Jackson et al 2014, NCCWCH 2014).
Why might my labour be slow?
Some labours are just slow for no particular reason. However, you may have a slow labour if:
- You're dehydrated or exhausted (NCCWCH 2014).
- The position of your baby is making it harder for your labour to progress (NCCWCH 2014).
- You feel particularly scared or anxious. These emotions tend to interfere with the release of the hormone oxytocin, which can help labour along (Aral et al 2014, Simkin and Ancheta 2011).
- Your contractions are infrequent, not very strong, or staying at the same intensity rather than getting stronger (NCCWCH 2014).

- You've had interventions that have slowed your contractions. These could include having to stay still for periods of time, or having an epidural (NCCWCH 2014).
Bear in mind that the first 5cm of cervix dilation nearly always takes much longer than the second 5cm (Ehsanipoor and Satin 2019, Jackson et al 2014, Simkin and Ancheta 2011). Your cervix opens more quickly as your contractions get stronger.
How is labour speeded up?
If your midwife asks whether you'd like to have your labour speeded up, take time to consider your options. If your baby is fine, and your cervix is gradually opening up, even if it's happening slowly, it may be best to leave things alone. You may be perfectly happy to take things gently, staying in tune with your body and your baby.
Or you may be so exhausted that you really want your baby to be born quickly. If that's the case, your midwife can help to move things along in the following ways:
Breaking the waters
Your midwife may suggest breaking your waters to speed up your labour (NCCWCH 2014). This isn't usually recommended near the beginning of labour, as it could increase your risk of infection if labour doesn't start right away (NCCWCH 2008).
This isn't usually recommended near the beginning of labour, as it could increase your risk of infection if labour doesn't start right away (NCCWCH 2008).
However, if the active stage of labour slows right down, breaking your waters can help to get things going again. It may shorten labour by about an hour (NCCWCH 2014).
If you agree to the procedure, here's how your midwife will do it. Once you're on the bed, she'll remove the last section of the bed so that your bottom is right at the end. She may ask you to put your legs up in stirrups, or just hold them apart.
Your midwife will then make a small break in the membranes around your baby. She'll use a long thin probe (amnihook) or a medical glove with a pricked end on one of the fingers (amnicot). She'll scratch the membrane until it bursts and the waters flow out into a tray placed underneath the bed.
This procedure isn't painful but it can be very uncomfortable. You'll probably be glad to get up again once it's over.
Your midwife will then check your baby's heartbeat using a Sonicaid or ear trumpet, to make sure that breaking the waters hasn't distressed him.
Your contractions may become much stronger after your waters have been broken (NCCWCH 2014). Be prepared to work hard with breathing and relaxation exercises. Or you can ask your midwife for some pain relief, such as gas and air, if you need extra help.
Hormone drip
If moving around or breaking your waters doesn't speed up your labour, your doctor may suggest a hormone drip to boost your contractions (NCCWCH 2014). This will contain Syntocinon, which is an artificial form of the labour hormone oxytocin.
If you have Syntocinon, your midwife will continuously monitor your baby's heartbeat by strapping electronic sensors to your tummy (NCCWCH 2014).
Your midwife may also recommend attaching a small clip to your baby's head. The clip is called a fetal scalp electrode and it may provide a more accurate reading than placing a sensor on your tummy. It also allows you to move around more easily.
It also allows you to move around more easily.
Continuous monitoring is recommended because Syntocinon can over-stimulate your womb (uterus) (NCCWCH 2014). You may get very strong, frequent contractions, which could distress your baby.
You're also more likely to need help from pain-relieving drugs to cope with these artificially induced contractions. For this reason, your midwife should offer you an epidural before she starts a Syntocinon drip (NCCWCH 2014).
Can I speed up labour myself?
If you'd prefer not to have your waters broken, or a hormone drip, there are some natural techniques you could try to speed up your labour
- If you're lying on the bed, get up! Being upright and mobile may strengthen your contractions, while also helping you to cope with them (Lawrence et al 2013).
- Take a walk to the toilet. A full bladder may slow down your labour by getting in the way of your baby's head descending (Simkin and Ancheta 2011).

- If you have access to one, get into a warm bath or birth pool. This can reduce your need for an epidural or spinal pain relief (Cluett et al 2018).
- If your baby is lying back-to-back, an experienced midwife may advise you to lie on your side or try kneeling or standing lunge positions. This may help your baby to rotate to a better position for birth (Simkin and Ancheta 2011).
- Have some private time with your partner. Turn the lights down low and have a cuddle, with some nipple stroking or breast massage. This may help your body to release oxytocin, the hormone that strengthens your contractions (Simkin and Ancheta 2011).
You could also try acupuncture during your labour (Mollart et al 2015,Simkin and Ancheta 2011). Complementary therapies probably work best if used throughout labour. You may be able to request an acupuncturist if your labour has slowed down. In some areas of the UK, acupuncturists specialising in childbirth work in teams, meaning that a practitioner is always available.
You can also ask your midwife whether she's certified in any complementary therapies, such as aromatherapy massage, that could help you.
How to help your baby be born
How can you speed up labour and make the birth easier? Discover how to help your baby be born more quickly.More preparing for birth videos
What can help me to cope with a long labour?
These methods may help you:
- Use breathing and relaxation techniques to help you stay calm and focused (NCCWCH 2014). If you've been taking hypnobirthing classes, this is the time to use everything you've learned!
- Ask your birth partner to massage your back, or your feet, if you're sitting in a chair (NCCWCH 2014, Smith et al 2018).
- Listen to your favourite music (NCCWCH 2014).
- Eat and drink when you need to. Have a small snack, such as toast, and water, or an isotonic drink, to stay hydrated (NCCWCH 2014).
- Change your position.
 Later in labour you may not feel like walking around, but your midwife can help you to find a comfortable position (NCCWCH 2014).
Later in labour you may not feel like walking around, but your midwife can help you to find a comfortable position (NCCWCH 2014). - Listen to your body and try different positions (Simkin and Ancheta 2011). Move around or adopt positions that feel most comfortable to you as labour progresses (NCCWCH 2014).
- Ask your midwife to explain what's going on. If you feel involved and in control of your labour, you'll probably feel less anxious and more relaxed. This may make your labour easier to cope with, and you may find it a more positive experience (NCCWCH 2014).
- If your midwife is caring for other women as well as you because the unit is busy, continuous support from a student midwife may help your labour to progress. Your birth partner could ask if there's any extra help available (Bolbol-Haghighi et al 2016).
Learn more about what to expect from each stage of labour.
References
Aral I, Koken G, Bozkurt M, et al. 2014. Evaluation of the effects of maternal anxiety on the duration of vaginal labour delivery. Clin Exp Obstet Gynecol 41(1):32-6
2014. Evaluation of the effects of maternal anxiety on the duration of vaginal labour delivery. Clin Exp Obstet Gynecol 41(1):32-6
Bolbol-Haghighi N, Masoumi SZ, Kazemi F. 2016. Effect of continued support of midwifery students in labour on the childbirth and labour consequences: a randomized controlled clinical trial. J Clin Diagn Res 10(9): QC14–QC17. www.ncbi.nlm.nih.gov [Accessed September 2019]
Cluett ER, Burns E, Cuthbert A. 2018. Immersion in water during labour and birth. Cochrane Database of Systematic Reviews (5): CD000111. www.cochranelibrary.com [Accessed September 2019]
Ehsanipoor MD, Satin AJ. 2019. Normal and abnormal labor progression. UpToDate. www.uptodate.com [Accessed September 2019]
Harper LM, Caughey AB, Roehl KA, et al. 2014. Defining an abnormal first stage of labor based on maternal and neonatal outcomes. Am J Obstet Gynecol (210(6):536.e1-7. www.ncbi.nlm.nih.gov [Accessed September 2019]
Jackson K, Marshall JE, Brydon S. 2014. Physiology and care during the first stage of labour. In: Marshall JE, Raynor MD. eds. Myles Textbook for Midwives. 16th ed. Edinburgh: Churchill Livingstone, 327-66
2014. Physiology and care during the first stage of labour. In: Marshall JE, Raynor MD. eds. Myles Textbook for Midwives. 16th ed. Edinburgh: Churchill Livingstone, 327-66
Lawrence A, Lewis L, Hofmeyr GJ, et al. 2013. Maternal positions and mobility during first stage labour. Cochrane Database of Systematic Reviews (10): CD003934. www.cochranelibrary.com [Accessed September 2019]
Mollart LJ, Adam J, Foureur M. 2015. Impact of acupressure on onset of labour and labour duration: a systematic review. Women Birth 28(3): 199-206
NCCWCH. 2014. Intrapartum care: care of healthy women and their babies during childbirth. National Collaborating Centre for Women's and Children's Health, Clinical guideline, 190. www.nice.org.uk [Accessed September 2019]
RCM. 2012a. Assessing progress in labour. Royal College of Midwives Trust, Evidence based guidelines for midwifery-led care in labour
RCM. 2012b. Rupturing membranes. Royal College of Midwives Trust, Evidence based guidelines for midwifery-led care in labour
RCM. 2018. Midwifery care in labour guidance for all women in all settings. Royal College of Midwives, Midwifery Blue Top Guidance
2018. Midwifery care in labour guidance for all women in all settings. Royal College of Midwives, Midwifery Blue Top Guidance
RCN. 2016. Genital examination in women. Royal College of Nursing. www.rcn.org.uk [Accessed September 2019]
Rimmer A. 2014. Prolonged pregnancy and disorders of uterine action. In: Marshall JE, Raynor MD. eds. Myles textbook for midwives 16th ed. Edinburgh: Churchill Livingstone, 417-33
Simkin P, Ancheta R. 2011. The labor progress handbook: early interventions to prevent and treat dystocia. 3rd ed. Chichester: Wiley Blackwell
Smith CA, Levett KM, Collins CT, et al. 2018. Massage, reflexology and other manual methods for pain management in labour. Cochrane Database of Systematic Reviews (3): CD009290. www.cochranelibrary.com [Accessed September 2019]
Smyth RMD, Markham C, Dowswell T. 2013. Amniotomy for shortening spontaneous labour. Cochrane Database of Systematic Reviews (6): CD006167. www. cochranelibrary.com [Accessed September 2019]
cochranelibrary.com [Accessed September 2019]
Thakar R, Sultan AH. 2014. The female pelvis and the reproductive organs. In: Marshall JE, Raynor MD. eds. Myles Textbook for Midwives. 16th ed. Edinburgh: Churchill Livingstone, 55-80
Show references Hide references
How to induce labor naturally
There are at least seven ways to induce labor that are supported by science. Let's take a look at each of these "evidence-based" methods.
1. Sexual intercourse
Many women manage to induce natural childbirth through sex. This is because semen contains prostaglandins, the same hormone-like compounds found in cervical ripening drugs such as Cervidil.
The key to having sex for natural induction is not to do it once. With this natural method of labor induction, "3 times is the way to go." It is assumed that three ejaculations contain the same amount of prostaglandins as Cervidil.
Of course, at 40+ weeks of pregnancy, frequent sex is definitely not what the expectant mother dreams of, but it is definitely the best alternative to cervidil and pitocin, which can lead to more painful contractions and even rupture of the membranes or fetal distress.
2. Nipple stimulation
Nipple stimulation can actually help induce labor or hasten a stalled or slow labor. You should stimulate the entire breast, not just the nipples. Try a slow, rhythmic breast massage behind the areola.
You can do this yourself or ask your partner to help you.
3. Evening Primrose Oil
Evening Primrose Oil contains prostaglandins that help prepare the cervix for childbirth. However, there is limited research on the efficacy and safety of evening primrose oil. Evening primrose oil can actually prolong labor by several hours when used vaginally. It can also cause early rupture of membranes, meaning your waters break before contractions begin.
Although many mothers claim that oil speeds up labor, there is still a risk, so it should be considered as a last resort.
4. Castor oil
Castor oil causes the intestines to contract, which can stimulate uterine contractions. But like evening primrose oil, this method should also be used with caution and only with the approval of your midwife or doctor.
But like evening primrose oil, this method should also be used with caution and only with the approval of your midwife or doctor.
Although many mothers have used it with great success and no other interventions. Yet it should be remembered that intestinal contractions cause terrible diarrhea. At best, this can be inconvenient; at worst, it can cause dehydration. If you and your birthing team decide to try this method, be sure to drink at least 500 ml of water to keep yourself hydrated and maintain healthy electrolyte levels.
5. Red raspberry leaf tea
Red raspberry leaf tea is a great way to tone the uterus during pregnancy and can also help induce labor.
Due to its stimulating effect, most midwives do not recommend drinking until the second trimester. For labor induction, increase the dose of this tea.
6. Eating dates
Research shows that eating dates during pregnancy helps women achieve greater cervical dilation, intact membranes, and more spontaneous labor when the time comes for delivery. Oxytocin use was significantly lower in women who consumed dates, and the average duration of the first stage of labor was shorter in women who consumed dates. As the study concludes, “dating dates during the last 4 weeks before delivery significantly reduced the need for labor induction and induction and resulted in more favorable labor.”
Oxytocin use was significantly lower in women who consumed dates, and the average duration of the first stage of labor was shorter in women who consumed dates. As the study concludes, “dating dates during the last 4 weeks before delivery significantly reduced the need for labor induction and induction and resulted in more favorable labor.”
What else can help induce labor?
While not backed by science, many moms claim these natural or "anecdotal" ways to induce labor.
1. Pamper yourself
Pamper yourself is a great way to relax and focus before having a baby. Sure, prenatal massage is great, but you might want to focus on the feet, which have special trigger points that can induce labor. A foot massage, reflexology, or even just a pedicure can be rewarding and definitely an enjoyable pastime.
2. Guided Relaxation
Soothing affirmations, guided meditation, and deep breathing can do wonders to help your body relax and prepare to welcome your baby. Fearful thoughts and anxiety can lead to the release of adrenaline and other stress hormones that stop the birth process.
Fearful thoughts and anxiety can lead to the release of adrenaline and other stress hormones that stop the birth process.
It is interesting that before giving birth, cats go to a dark, quiet place. Darkness helps bypass stress hormones and increases levels of melatonin, a key hormone that can help trigger hormonal cascades. You can try this by turning off the lights, closing your eyes and focusing on your body and the amazing feat you are about to accomplish.
3. Nutrition
Follow your ideal pregnancy diet and remember to drink water. Childbirth is hard work and you will need all the support you can get. Although nutrition may not stimulate labor, it will definitely help you feel strong, prepared, and calm when labor actually begins.
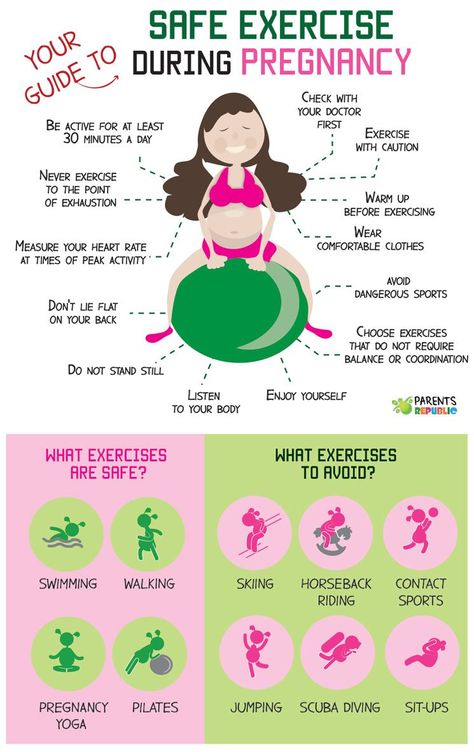
4. Exercise
Moderate exercise is fantastic throughout pregnancy, and some women have been lucky enough to induce labor by walking, cycling, swimming, or other exercise. By moving our body, we can help the baby into its birth position and open up our pelvis for a faster delivery. However, the main thing is not to overdo it. You don't want to be tired when labor starts.
By moving our body, we can help the baby into its birth position and open up our pelvis for a faster delivery. However, the main thing is not to overdo it. You don't want to be tired when labor starts.
5. Acupuncture, acupressure and chiropractic
In addition to mental readiness, you and your child need to be physically ready, and acupuncture, acupressure and chiropractic can help with this. Acupuncture is a potentially useful way to induce labor, but there isn't a lot of solid research on this topic. However, acupuncture and acupressure have been used for many years to induce labor and are trusted by many women.
The idea of acupressure is that acupuncture and acupressure help to unblock any stagnant energy, which can help the child to get into the correct position. Specifically, acupuncture points for inducing labor are found on the feet, arms, and back. They stimulate the thyroid, digestive and reproductive systems.
Chiropractic induction methods are based on the same idea. Opening and balancing the pelvis with chiropractic helps your baby get into the correct, deep position and stimulates your body for labor.
Opening and balancing the pelvis with chiropractic helps your baby get into the correct, deep position and stimulates your body for labor.
Find a suitable pregnancy acupuncturist or contact a local mums group for recommendations.
6. Pineapple
The bromelain in pineapple and other tropical fruits is said to induce labor by stimulating the uterus. On the other hand, it may just be the stimulation of the intestines from eating a large amount of pineapple, which causes labor. Either way, it's a delightful way to induce labor naturally.
7. Spicy food
Some mothers use spicy food to induce labor. Like castor oil, spicy foods stimulate the intestines. Keep in mind that spicy foods can cause stomach upset, a side effect that is best avoided during childbirth.
8. Eggplant Parmesan
Scalinis Restaurant near Atlanta, Georgia, claims to have helped more than 300 women go into labor within 48 hours with its famous eggplant parmesan. Don't live near a restaurant? Dish you can try at home:
Don't live near a restaurant? Dish you can try at home:
Ingredients:
3 medium eggplants
0.5 cup flour
6 eggs, beaten
2 cups Italian breadcrumbs
1L cups marinara sauce
1/2 cup grated romano cheese
1/2 cup grated parmesan cheese
200 gr mozzarella cheese, grated
2 cups ricotta cheese
How to cook:
After washing the eggplants, cut them into slices.
Lay the eggplant slices on a layer of paper towels and sprinkle with a little salt, then cover with another layer of paper towels and press down with something heavy. This will remove excess moisture. Let them sit for about an hour.
Working with one eggplant slice at a time, dust it with flour, then dip in beaten eggs, then coat well in breadcrumbs. Fry in hot olive oil on both sides until golden brown.
In a baking dish, alternate layers of marinara sauce, eggplant slices, ricotta, Parmesan, and Romano cheese until the baking dish is filled. Sprinkle with grated mozzarella cheese and bake for 25 minutes at 375°C. Let stand 10 minutes before serving.
Sprinkle with grated mozzarella cheese and bake for 25 minutes at 375°C. Let stand 10 minutes before serving.
Note. For a gluten-free option, use chickpea or buckwheat flour in place of flour and almond flour or semolina in place of breadcrumbs.
9. Homeopathic remedies
Homeopathic remedies are generally considered safe during pregnancy. Common homeopathic remedies used to induce labor include Pulsatilla 200C, Caullophyllum 200C, and Cimicifuga 200C. Some midwives recommend alternating all three times every three days until labor begins. Consult your gynecologist for dosage.
For more information on homeopathic remedies during pregnancy and childbirth, read Homeopathic Medicines for Pregnancy and Childbirth by Richard Moskowitz and Homeopathy for Pregnancy, Childbirth and Your Baby's First Year by Miranda Castro.
10. Special Exercises
This chart helps misplaced babies get into the ideal birthing position, which puts pressure on the cervix and stimulates labor.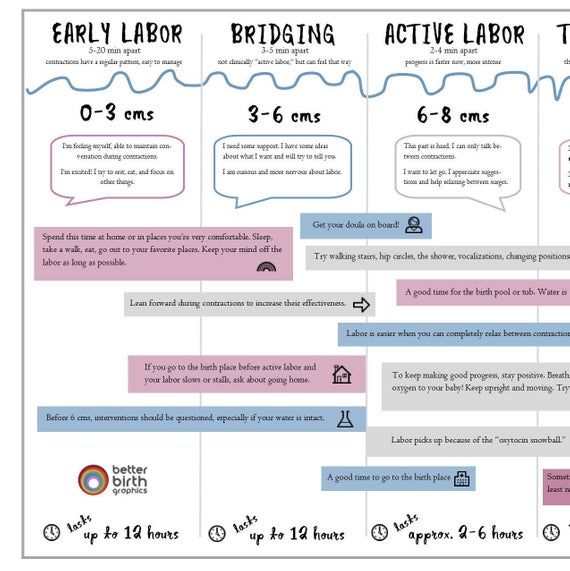
This simple procedure has three parts, including:
1, Start in cat/cow pose with knees wide apart, then lower chest as low as possible and buttocks as high as possible. Swing while maintaining this position for 30 minutes. This helps the baby move out of the pelvis a little, allowing him to rotate and change his head position.
2. Roll onto your left side, straighten your bottom leg, then lift your top leg as high as you can. Roll forward using pillows for support. Maintain this position for 30 minutes.
Do your best to move for at least 30 minutes. Lunges, walking up and down stairs in twos, sideways, sitting on a birth ball, and hula hoops are especially helpful because they put your pelvis in an asymmetrical position.
Which food induces labor?
As noted above, when it comes to food to induce labor, dates are the best choice. Research shows that dates reduce the need for induction and shorten labor.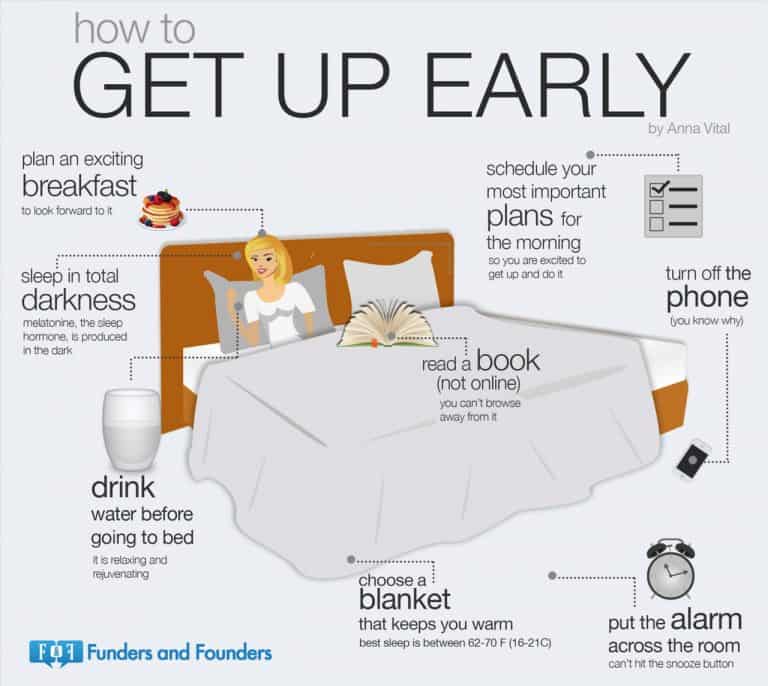 Pineapple and spicy foods can also help induce labor, although there isn't much evidence to support these theories, only a lot of anecdotal evidence.
Pineapple and spicy foods can also help induce labor, although there isn't much evidence to support these theories, only a lot of anecdotal evidence.
How long does it take to have a baby after induction?
As with most aspects of childbirth, there is no hard and fast rule. Every woman is different: for some mothers, induction of labor can take only a few hours, for others it can take several days. And sometimes induction doesn't work at all.
Why does induction cause more pain?
Our body naturally produces oxytocin, a hormone that stimulates contractions. During induction, a woman is usually given a synthetic form of oxytocin, such as pitocin, to speed up contractions. This can cause labor to start too quickly, resulting in stronger and more intimate contractions.
What are the risks of induction?
The risks of induction vary depending on the method of induction, but the biggest risk is that the induction will fail. In 25% of cases, the induction failed - this may mean that the mother is in labor for a long time, but eventually a caesarean section may be required. It can be physically taxing and emotionally draining for a mom.
In 25% of cases, the induction failed - this may mean that the mother is in labor for a long time, but eventually a caesarean section may be required. It can be physically taxing and emotionally draining for a mom.
Other risks include:
Low fetal heart rate: The strong, frequent contractions caused by pitocin may cause discomfort to the baby.
Uterine rupture: The strong, frequent contractions caused by Pitocin can cause the uterus to rupture. This is most common in mothers who have previously had uterine surgery.
Excessive bleeding in the mother after childbirth: When stimulated, the uterus may not contract properly after childbirth.
Infection: Rupture of membranes can put mother and baby at increased risk of infection.
What if I miss my due date? Should I induce labor?
Absolutely not! You have the right to refuse anything that does not suit you, including induction of labor.
At 40 weeks gestation, there is no evidence that induction is necessary in a normal healthy pregnancy. Remember that your due date is determined by a number of factors, including the average length of pregnancies in your family, the accuracy of your due date calculation, and your individual child. Your baby and body are the ones who initiate labor and usually know when they are ready.
Remember that your due date is determined by a number of factors, including the average length of pregnancies in your family, the accuracy of your due date calculation, and your individual child. Your baby and body are the ones who initiate labor and usually know when they are ready.
If you have passed 41 weeks of pregnancy
There is no reason to consider induction in a normal healthy pregnancy before 41 weeks, and you may want to wait even longer before trying any of these methods. If you choose to go through 41 weeks without trying to induce labor, your healthcare provider will likely keep a close eye on you.
If you have passed 42 weeks of pregnancy
Natural induction of labor is still a priority and may increase the likelihood of other labor interventions. If mom and baby are healthy, it is perfectly reasonable and scientifically justified to give birth at 42 weeks.
How did other mothers induce labor?
I asked moms on my Facebook page about ways to induce labor naturally. Here are some of their responses:
Here are some of their responses:
- My water broke but my contractions didn't start. That night I went for acupuncture and two hours later I had a nice steady contraction rhythm! — Jill B.
- Massage of painful points, sex, walks. — Norma O.
- I massaged the pressure points on my feet and around my ankles that are supposed to induce labor. That night I went into labor, that is, a week before the expected date of delivery! I also started drinking 1 cup of red raspberry leaf tea a day at 32 weeks pregnant and gradually increased it to 4 cups by the time I was due. — Jennifer B.
- A friend told me that she had read that pineapple can induce labor. Without thinking, the next day I ate almost a whole pineapple. That night I went into labor, a week early. — Stephanie N.
- With both of my kids, I've tried everything - spicy food, pineapple, even scrubbing floors/lunges vigorously. But both times the trick was to have sex with my husband and make him ejaculate inside me.
 I went into labor less than 12 hours after two times. — Lisa S.
I went into labor less than 12 hours after two times. — Lisa S. - The first child was "delayed" by 3 days, so I stimulated naturally with evening primrose oil (oral and vaginal) and castor oil. That day, I started having contractions! — Sarah L.
- Acupuncture! I came in with very weak, irregular contractions and left with active labour, intense contractions 6 minutes apart. She gave birth 10 hours later. — Sherry M.
- I worked every day of both my births (throughout all pregnancies). I also had sex. — Susan B.
- Acupuncture, chiropractor and pumping (nipple stimulation). — Angela G.
Original - here
Premature birth - Juno
Premature birth: article content
What is preterm birth
The birth of a baby weighing more than 0.5 kg from 22 to 37 weeks is considered early. According to statistics, 15 million babies are born prematurely around the world.
In our country, until 2012, babies were registered who were born at 28 weeks, and all those born earlier - a week later. The development of obstetrics made it possible to nurse critically premature babies and increased their survival statistics.
The development of obstetrics made it possible to nurse critically premature babies and increased their survival statistics.
Who is at risk
Any pregnant woman can give birth prematurely. Some expectant mothers have a higher chance of preterm birth. The risk zone includes pregnant women:
- under 17 and over 35;
- have more than one fetus;
- have structural features of the uterus or its cervix;
- use harmful substances - drugs, alcohol, smoke;
- have heavy physical activity;
- have a history of preterm birth;
- work in hazardous production;
- are subjected to sexual, emotional abuse, stress, mental stress.
At risk are expectant mothers who are not registered during the gestation period or ignore ultrasound, screenings, laboratory tests.
The threat of early preterm birth is more common with diagnoses: diabetes mellitus, anemia, hypertension, genitourinary infections, hypothyroidism, problems with weight before conception (deficiency or obesity), thrombophilia, vaginal bleeding. There is also a risk when conceiving through IVF, with congenital malformations of the fetus.
There is also a risk when conceiving through IVF, with congenital malformations of the fetus.
If a woman has previously given birth to a child ahead of schedule, the chances of premature birth remain in subsequent pregnancies. The same applies to the weight of the crumbs: if the firstborn was born with a lack of body weight, then his brother or sister may be underweight.
Risk factors
Doctors point to a number of factors that take place long before the conception of a child. These include:
- Gynecological diseases suffered in childhood or adolescence;
- Early initiation of intimate life;
- Hereditary factor;
- Pathologies of previous pregnancy: preeclampsia, fetoplacental insufficiency, premature birth;
- Excessive uterine distension in multiple pregnancies, polyhydramnios;
- Threat of early miscarriage.
Another risk factor is surgery or trauma to the abdominal organs during the gestation period.
Risk of preterm birth at different times
The birth of a child prematurely has many negative consequences for him. It depends on the trimester in which the pregnancy ended.
The most severe consequence is the death of the infant. With early preterm birth in the period of 22-24 weeks, the threat is the highest - up to 80% of babies die. This occurs against the background of intracranial hemorrhage of 3-4 degrees, cardiopulmonary insufficiency, intrauterine infection of the fetus.
Among those born in the period of 25 - 26 weeks, 40% of babies die, in 27 - 28 - about 20%, in 29 - 32 - no more than 10%, and in 33 - 34 - 2% of newborns are at risk.
Modern medicine is able to provide care for a premature baby and save his life. But no one can guarantee a full healthy life. Such a child can subsequently be given disappointing diagnoses: cerebral palsy, mental retardation, retinopathy of prematurity. He may suffer all his life from problems with the digestive and respiratory systems, impaired vision, hearing, delayed mental and physical development.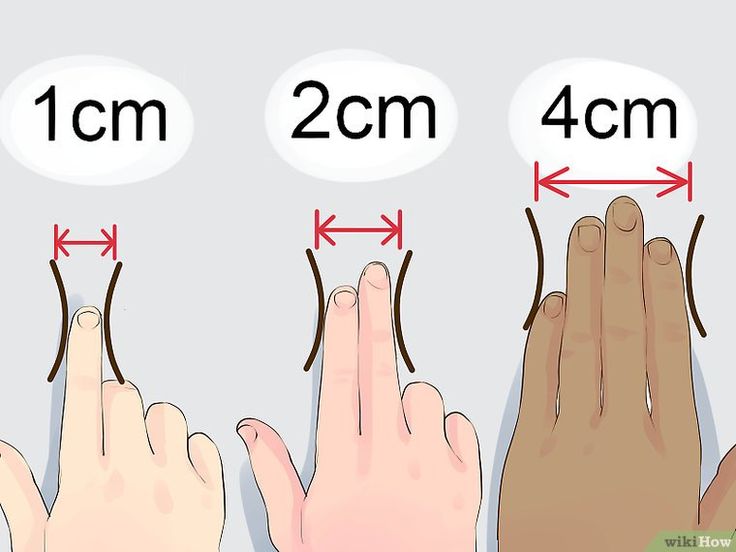 Diagnosis implies disability.
Diagnosis implies disability.
For a woman in labor, preterm labor is usually not dangerous. Without concomitant pathologies, the mother's body does not care how long the child is born. There are only psychological problems: stress, fear and worries about the baby. It is better for a mother to tune in that her child, in case of severe prematurity, will be taken to the intensive care unit for nursing, so she will not see him immediately.
A newly minted mother needs rehabilitation. Therapy is prescribed, depending on the cause of the pathology: a complex of vitamins, antioxidants, hormones.
Why preterm birth is dangerous
Infants are immature: their body is covered with a large amount of cheese-like lubricant, there is a deficiency of subcutaneous fatty tissue, few hairs on the head and fluff on the body, cartilage on the ears and nose are soft, the nails do not go beyond the fingertips, the navel is located closer to the pubis.
Babies are underweight. Depending on the weight of the crumbs, 4 degrees of prematurity are distinguished: at the 1st degree, the baby weighs from 2500 to 2001 g, the 2nd - from 2000 to 1500 g, the 3rd - from 1500 to 1001 g, the 4th - 1000 g and below .
Depending on the weight of the crumbs, 4 degrees of prematurity are distinguished: at the 1st degree, the baby weighs from 2500 to 2001 g, the 2nd - from 2000 to 1500 g, the 3rd - from 1500 to 1001 g, the 4th - 1000 g and below .
The development of the genital organs has not been completed: the testicles in boys are not lowered into the scrotum, and in girls the large labia do not cover the small and clitoris.
Children have immature lungs. They cannot breathe adequately - often they need help. The cry is weak. There are also problems with digestion. The body cannot absorb all the components from mother's milk.
Extrauterine life for children becomes a strong stress. It's hard to deal with him. They poorly resist infections, quickly lose heat, thermoregulation is impaired. They are subject to hemorrhages against the background of fragile vessels. Especially dangerous are hemorrhages in the cervical spinal cord and ventricles of the brain.
Among the complications of preterm birth are intracranial hemorrhages, asphyxia, intrauterine growth retardation.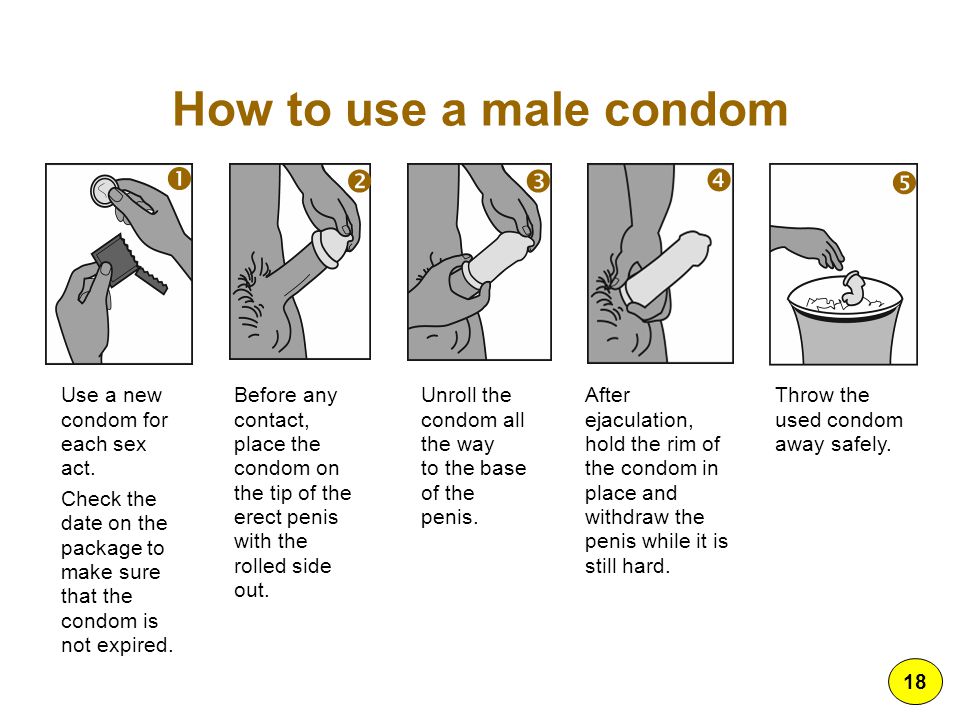
Types of preterm birth
Several classifications have been adopted. Let's consider them.
- By term: critically early - up to 28 weeks, significantly early - from 28 to 32 weeks, moderately early or late - from 32 to 37 weeks;
- By the mechanism of attack: induced and spontaneous. Induced cause artificially for medical reasons. Occurs in 40% of cases. Spontaneous in 60% of cases begin with contractions, in 40% - with a rupture of the membranes;
- By the nature of the course: spontaneous, with regular labor activity, without it and artificially provoked. In 80% of cases, preterm labor begins spontaneously. At the same time, the fetal bladder can be intact - and then the contractions are regular, growing. Or amniotic fluid may pour out, labor activity is chaotic. For medical reasons, early delivery can be artificially induced. For example, in case of danger to the life of the mother, intrauterine death of the fetus, or defects that are incompatible with life;
- According to symptoms: threatening, incipient and incipient.
 With threatening early premature birth, the lower abdomen and lower back hurt, the tone rises. Her neck remains unchanged, the external os is closed. When the process begins, pains appear in the lower abdomen. Regular contractions may begin. The neck is flattened or shortened. The main symptom of the onset of preterm labor is regular labor activity. The cervix opens by 2 - 3 cm, it happens quickly.
With threatening early premature birth, the lower abdomen and lower back hurt, the tone rises. Her neck remains unchanged, the external os is closed. When the process begins, pains appear in the lower abdomen. Regular contractions may begin. The neck is flattened or shortened. The main symptom of the onset of preterm labor is regular labor activity. The cervix opens by 2 - 3 cm, it happens quickly.
In 40% of women in labor, water breaks, 35% gave birth quickly and quickly. The active phase lasts less than when the baby appears on time. The contractions are monotonous, long and painful, the pauses between them are small.
Causes of preterm labor
Doctors indicate the main causes of the pathology:
- Early activity of the fetal endocrine system;
- Infections and inflammatory processes - ureaplasmosis, mycoplasmosis, pyelonephritis, bacterial vaginosis. They stimulate the production of prostaglandins. Hormones affect the uterine muscles - cause contractions and premature birth;
- Placental bleeding.
 They occur with incorrect presentation or detachment. The situation is serious, there is a threat to the life of the mother. Therefore, with presentation, hospitalization is indicated;
They occur with incorrect presentation or detachment. The situation is serious, there is a threat to the life of the mother. Therefore, with presentation, hospitalization is indicated; - Neck weakness. In 20% of cases, it leads to preterm birth. This also includes such factors: the interval between the current and previous gestation is less than 2 years, the woman is expecting 4 children or more;
- Isthmic-cervical insufficiency. The cervix opens itself - a miscarriage or premature birth occurs. It is possible to open mechanically - when scraping after a miscarriage, IVF, abortion;
- Pathologies on the part of the baby - intrauterine infection, malformations of internal organs.
Chronic ailments, dental problems, angina, health status during gestation, genetic factors are all common reasons for early delivery. Sometimes it is impossible to determine. Although this is important for the development of effective means of preventing pathology.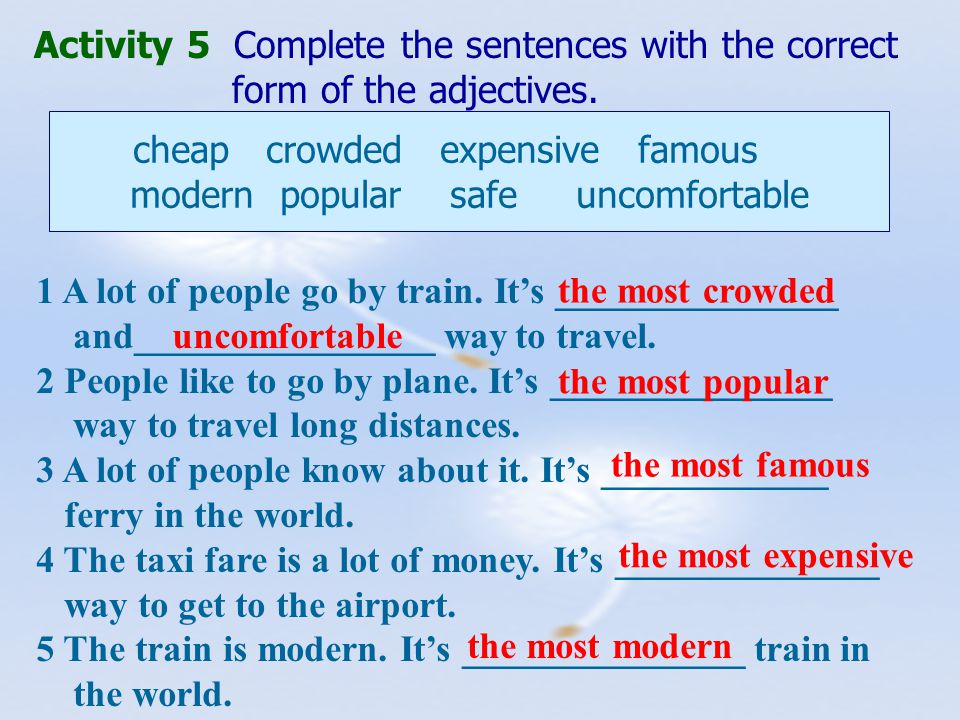
Symptoms of preterm labor
We list the signs by which you may suspect that the baby is in a hurry to be born ahead of time.
Spasms over the pubis. They are similar to pain during menstruation.
Pain, pressure and discomfort in the genitals, thighs, pelvis. There is a dull pain in the lumbar region.
Feeling of pressure, pressure in the back.
Diarrhea, spasms and pain in the intestines.
Vaginal discharge - they get worse. May be watery, pink, brown, bloody.
Contractions of varying intensity. Touch your stomach with your fingertips - you will feel the contraction and relaxation of the uterus. Counted more than 4 contractions in 60 minutes? Call an ambulance - you need an urgent examination by an obstetrician.
The following symptoms are also dangerous: sudden blurred vision, flashes and “flies” before the eyes, incessant migraine, swelling of the face or hands, temperature of 38º C and above, painful urination, abdominal trauma, decreased fetal activity in the 3rd trimester (less than 10 movements in 12 hours).
Any of the above symptoms indicate the risk of preterm birth. Seek medical attention.
Diagnosis of preterm birth
Includes several stages.
Transvaginal ultrasound. The length of the cervix is measured, fetal fibronectin is determined - a kind of "biological glue" that binds the fetal sac to the uterine mucosa.
Gynecological examination. Allows you to assess the degree of opening of the neck, its length.
Rapid test for the determination of phosphorylated protein-1. The test determines the possibility of preterm birth. In the future, this helps prevent iatrogenic complications.
When diagnosing, 2 parameters are evaluated:
- Regularity of contractions;
- Neck changes - shortening and smoothing. informative method. For example, with a neck length of 3 cm, the risk of preterm birth in the next week is 1%. The patient is not admitted to the hospital, there is no danger to her and the fetus.

Differential
Its goal is to correctly diagnose. The early birth of a baby is accompanied by cramps in the lower abdomen, diarrhea, pain in the lumbar region. These same symptoms are characteristic of other conditions: appendicitis, colitis, cystitis, pyelonephritis.
When complaining of pain in the lower abdomen, the patient is examined for the consistency of the scar after the previous cesarean section, for example. When the temperature rises, flu, sore throat, viral infection are excluded.
Diagnosis
Preterm birth is stated based on the clinical picture. Doctors are guided by such markers.
The first is the length of the neck - less than 2 - 2.5 cm.
The second is the determination of phosphorylated protein-1.
The third is the regularity of contractions. There should be at least 4 in 20 minutes.
Fourth - neck changes in dynamics.
Fifth - assessment of the degree of maturity of the neck. Determined by the level of PSIFR-1 in the cervical canal.
Determined by the level of PSIFR-1 in the cervical canal.
Usually the process begins rapidly, suddenly and intensely.
Treatment for preterm birth
The goal is to reduce the tone of the myometrium, reduce uterine contractions. This is achieved by blocking oxytocin receptors - it is the hormone oxytocin that triggers the birth process.
Such antagonists of oxytocin receptors are tocolytics. One of the modern representatives of this group of drugs is atosiban.
The remedy is effective, but has contraindications. It is forbidden to treat pregnant women for less than 24 and more than 33 weeks, with uterine bleeding, growth retardation, distress or fetal death, severe preeclampsia, with rupture of the fetal membrane after 30 weeks, placenta previa or its detachment.
5 steps preterm labor
The first stage is forecasting their onset. Depends on the situation: the process is starting, has begun, or it is a threat.
Stage two - prevention of respiratory distress syndrome in a child. Doctors stimulate the maturation of the lungs. Apply funds from the group of glucocorticoids.
Stage three - prolongation of pregnancy. Doctors try to delay preterm labor by giving the baby's lungs and placenta time to mature. For this, tocolytics are used - they inhibit the contractile activity of the uterus. Usually prophylaxis is carried out - tocolysis is carried out before contractions. When started, therapy is ineffective. The duration of treatment is a maximum of 48 hours.
Stage four - preparation for the birth of a premature baby. The woman in labor is transferred to a higher-level hospital. The physiology of preterm labor does not differ from the birth of a child at term. But close attention is required from doctors to minimize complications for mom and baby.
The fifth stage is the prevention of infections and their complications. At risk are women in labor whose waters have broken. If the patient gives birth before 34 weeks, she can be pierced with a course of dexamethasone. It accelerates the maturation of the placenta and internal organs of the baby, reduces the risk of complications.
If the patient gives birth before 34 weeks, she can be pierced with a course of dexamethasone. It accelerates the maturation of the placenta and internal organs of the baby, reduces the risk of complications.
OB sequence
When registering a patient with preterm birth, the doctor gets acquainted with the exchange card, studies the general, gynecological and infectious anamnesis, and the results of examinations. Clarifies complaints and evaluates the condition of the woman in labor. He examines her, measures the pulse and respiration rate, temperature, pressure, abdominal circumference and the height of the uterus.
Clarifies data on the fetus: movements, measures heart rate by auscultation - listening to the heart through the mother's stomach through the device. To assess the condition of the crumbs, the doctor performs cardiotocography. The device records the heart rate.
Ultrasound is performed to assess the condition of the child and mother's organs.
A gynecological examination is carried out: with intact membranes - external, with their rupture - internal. This is necessary to determine the position and position of the child, to assess the degree of disclosure.
Conduct a laboratory examination. They take a smear from the vagina: culture for β-hemolytic streptococcus, bacteriological culture, take blood and urine for a general analysis.
According to the results of the examination, the obstetrician confirms or refutes preterm birth, their stage.
The expectant mother is informed about her condition, forecasts for the child. At the slightest opportunity, they try to prolong the pregnancy. If the child is ready to be born in the near future, the doctor determines the tactics of assistance, coordinates the issue of anesthesia with the woman in labor.
In the absence of indications for a caesarean section, they give birth naturally. This is the best way - it is less traumatic for the baby.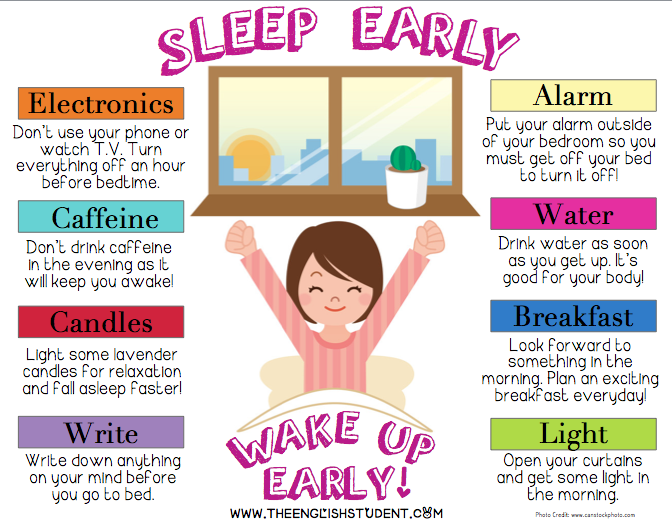 A gentle approach is what a weak newborn needs.
A gentle approach is what a weak newborn needs.
Preterm birth care policy
The woman in labor is provided with continuous psychological support. Describe the current obstetric situation.
With head presentation, they give birth naturally.
With pelvic - take into account clinical indications. Caesarean section is not the only effective method in this case. The operation does not improve the prognosis for a premature baby, but it puts an additional burden on the mother's body: it increases infection, morbidity, and complications.
With foot presentation, only a caesarean section is done.
Anesthesia is carefully selected. Avoid opiates - they depress the respiratory center, which is dangerous for premature babies.
At the birth of a baby before 34 weeks, vacuum aspiration is prohibited. It increases the risk of neonatal morbidity. Dosed episiotomy, exit forceps for the birth of the head and epidural anesthesia are performed.
The umbilical cord is clamped at least 1 minute after the baby is born. This tactic reduces the frequency of intraventricular hemorrhage in preterm pregnancies up to 37 weeks of gestation.
Control the state of the crumbs. CTG is done every hour for 40 minutes, auscultation - periodically.
General recommendations for prevention
You need to think about it from the first trimester. If you want to inform the baby, follow the advice of gynecologists.
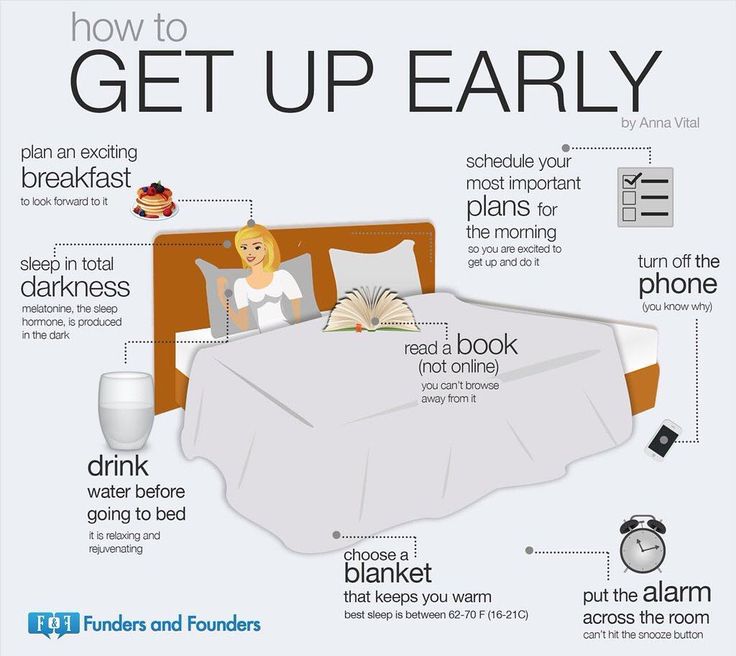
- Take care of yourself. Rest, avoid nervous overload. Sleep at least 7 hours;
- Eat well. Eat foods rich in vitamins, exclude fast food, fatty, fried, spicy and salty foods from the diet. Give up coffee and strong tea;
- Observe the drinking regimen. Try not to feel thirsty - drink water every 2 hours. If you don't want to - don't force yourself;
- Avoid physical activity. Active training, hard work, general cleaning alone are taboo for a pregnant woman.
 Try not to go outside on ice - you may fall, you will strain your muscles - this can increase your tone and provoke premature birth;
Try not to go outside on ice - you may fall, you will strain your muscles - this can increase your tone and provoke premature birth; - Maintain personal hygiene. Wash your face after a bowel movement. Always wash and dry from front to back. This way you will not bring bacteria from the intestine into the vagina. Infections are provocateurs of premature birth;
- Lead a healthy lifestyle. Alcohol and cigarettes are taboo. Smoking pregnant women are predisposed to preterm labor. If you take medications on a regular basis, tell your gynecologist about it. Walk outdoors. Cancel active workouts in favor of leisurely walks in the park;
- Register at the antenatal clinic in the first trimester - at 6 ‒ 8 weeks. Visit a gynecologist, listen to him, take tests, undergo ultrasound, screenings;
- Be careful with sex. In the first trimester, it is better to limit or abstain from it as much as possible - the embryo must be fixed. With placenta previa and other pathologies, the gynecologist may forbid you to have intimate contacts - listen to him;
- Learn to understand your body.
 In the 2nd trimester, start listening to the baby: his movements, activity. Fix any changes, strange and unpleasant sensations - and talk about them to the doctor. In case of acute pain, contractions, spasms, blood, urgently call an ambulance - this may be a premature birth;
In the 2nd trimester, start listening to the baby: his movements, activity. Fix any changes, strange and unpleasant sensations - and talk about them to the doctor. In case of acute pain, contractions, spasms, blood, urgently call an ambulance - this may be a premature birth; - Maintain bed rest. A gynecologist can advise you to rest. For example, with increased uterine contractions, tone;
- Rest every hour. Sit in a chair, lift your legs up. This will relax the muscles, eliminate swelling;
- Be aware of the signs of preterm labor. In case of their threat, you will not miss a moment and consult a doctor. Perhaps the process can be stopped with the help of drugs. Treatment minimizes complications in the premature baby.
Preterm birth prevention
It is divided into 2 stages: before conception and after.
Preventive measures before conception
It is advisable to carry them out to mothers from the risk zone. The gynecologist limits intrauterine manipulations, such as curettage. During IVF, the number of embryos for transfer is regulated taking into account the age of the expectant mother and her health. Inform about the possibility of premature birth at conception through reproductive technologies.
The gynecologist limits intrauterine manipulations, such as curettage. During IVF, the number of embryos for transfer is regulated taking into account the age of the expectant mother and her health. Inform about the possibility of premature birth at conception through reproductive technologies.
Hydration is shown - enhanced drinking regimen. It improves fetoplacental blood flow and reduces the risk of preterm birth.
Eliminate infections. It is advisable to do this at the planning stage, since antibiotic treatment during gestation harms the fetus.
It is recommended to postpone the conception of a child soon after the birth of an older brother or sister. Mommy's body needs to recover from the previous pregnancy. It takes him at least 2 years to do this. During this time, the uterus will return to its previous state, strength, vitamin reserves and body reserves will be restored.
Vitamin complexes are prescribed for predisposition to preterm birth for planning and expectant mothers. Protein-rich dietary supplements are helpful. They strengthen the immune system, improve blood circulation, protect the pregnant woman from infections - and hence the child.
Protein-rich dietary supplements are helpful. They strengthen the immune system, improve blood circulation, protect the pregnant woman from infections - and hence the child.
Secondary prevention of early delivery
With the threat of premature birth, the condition of the pregnant woman is monitored at critical periods: from 2 to 12 and from 18 to 22 weeks. During these periods, it is better to stay in the hospital of the perinatal center. Doctors prescribe drugs to maintain and prolong pregnancy.
Therapy is selected on an individual basis.
With a short neck from 1 to 2.5 cm, progesterone suppositories are prescribed vaginally. The hormone is also shown in previous preterm births. This tactic reduces their risk by 35%. This is a natural hormone. It is efficient and safe. It is prescribed in the first trimester. Synthetic hormone is harmful: it can provoke gestational diabetes.
If there is a threat of early birth of the crumbs, sutures are placed on the neck.