Posterior pelvic pain
Posterior Pelvic Pain in Pregnant Women
Posterior pelvic pain (PPP) pain felt at or near the sacroiliac joints of your pelvis as a result of sacroiliac joint dysfunction. These are joints located at the 2 dimples of the lower back. The pain often feels deep within your lower back and can occur on one or both sides of your back. In some cases, pain radiates down to the buttock and the back of the thigh.
While pain may begin at any time during pregnancy, PPP on average begins in the 18th week of pregnancy (the middle of the 2nd Trimester) and becomes more intense as the pregnancy progresses. The pain usually spontaneously resolves within 3 months after your pregnancy. But in some cases, it can become chronic and disabling.
What are the Sacroiliac joints?
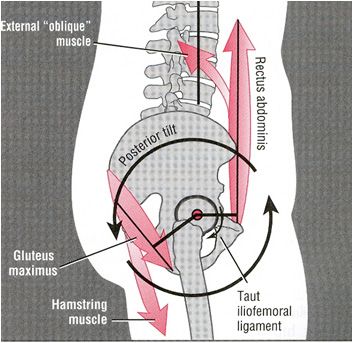
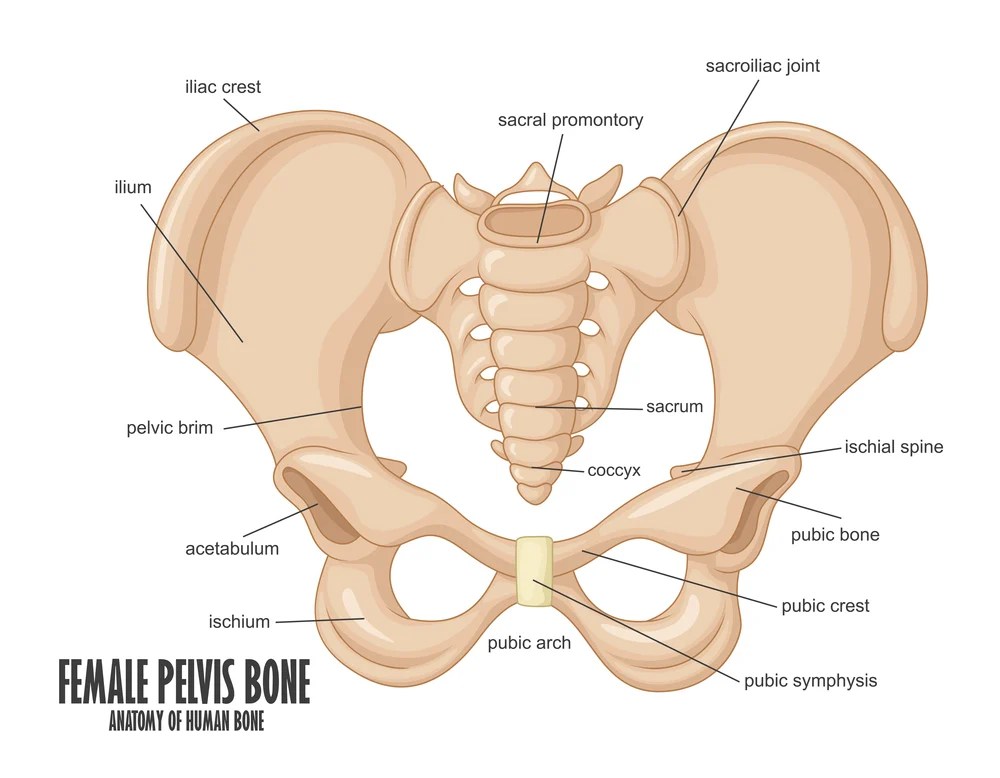
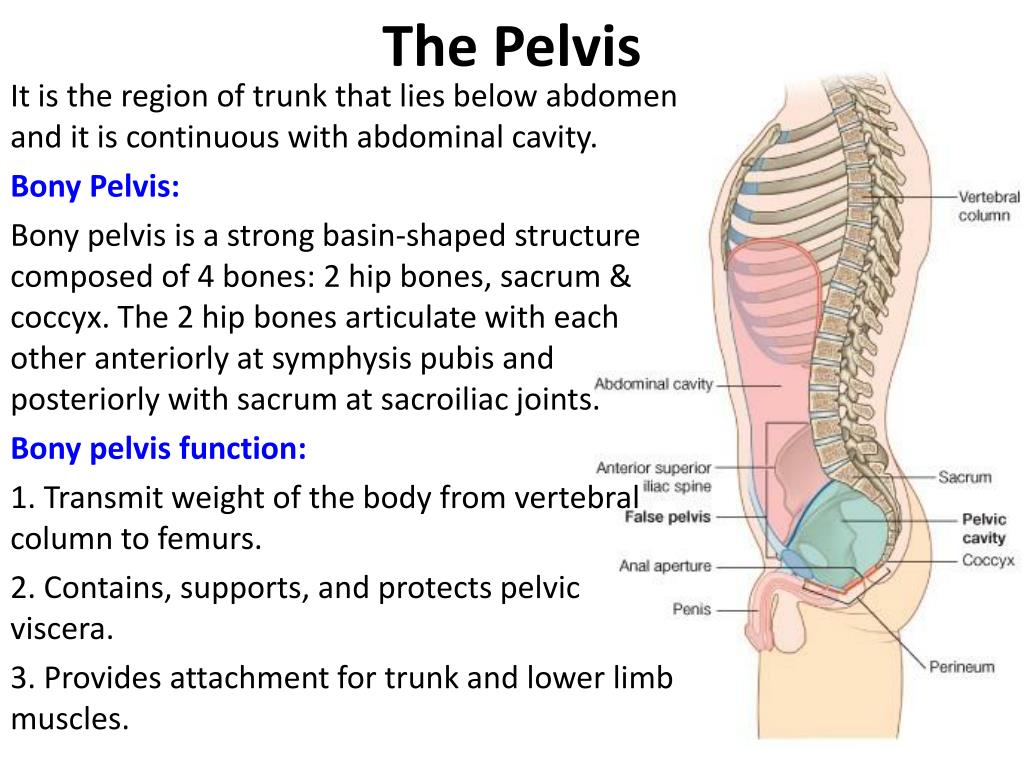
The sacroiliac joints (SIJ) formed between the sacrum, a triangular-shaped bone in the lower portion of the spine, and the right and left ilium of the pelvis. The SIJ is a strong and stable weight-bearing joint that permits very little movement due to its natural structure.
The main role of the SIJ is to allow forces to be transmitted effectively through the body, absorbing impact from the legs to the spine during activities such as walking, running and jumping.
The SIJ is kept stable through two mechanisms:
- Firstly, the rough, groove-like connecting surfaces of the sacrum and ilium interlock and help stabilise the joint, like two pieces of Lego together.
- Secondly, the SIJ is further strengthened by a complex mesh of ligaments and muscles such as the core stabilizers. These core muscles, such as the transversus abdominis and multifidus which surround the SIJ, act as active stabilizers by actively contracting to create a compressive force over the SIJ, gripping the joint firmly together. They act as a natural corset by providing that compression around the lower back and pelvic region -much like wrapping your fingers around the two Lego pieces, keeping them firm and tight.
Posterior pelvic pain arises from sacroiliac joint dysfunction, in other words when the stability of SIJ is compromised.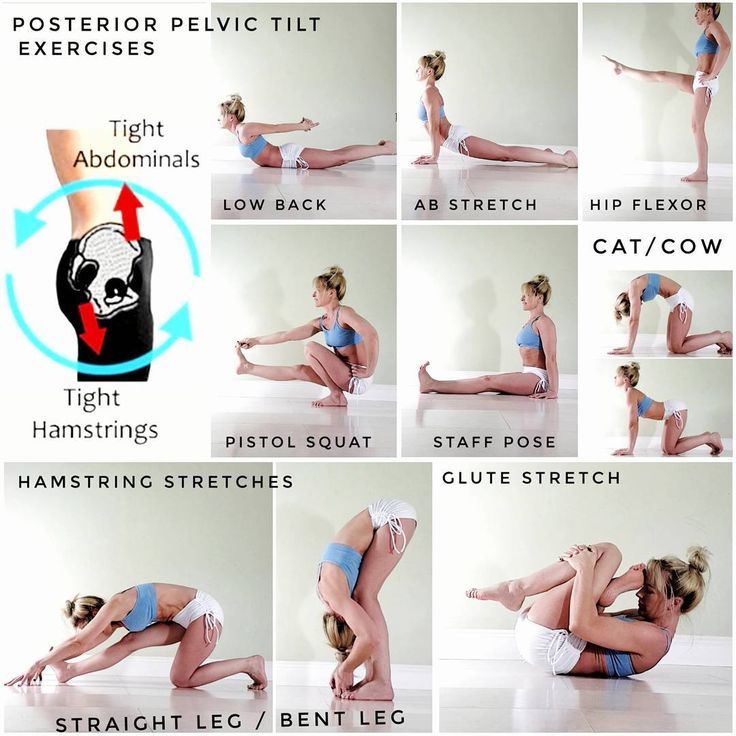
Why does Posterior Pelvic Pain happen during Pregnancy?
During pregnancy, mechanisms stabilising the SIJ affected. This instability allows for increased motion, stressing the SIJ.
- Hormones released during pregnancy relax the ligaments of the body to allow the pelvis to enlarge, in preparation for childbirth
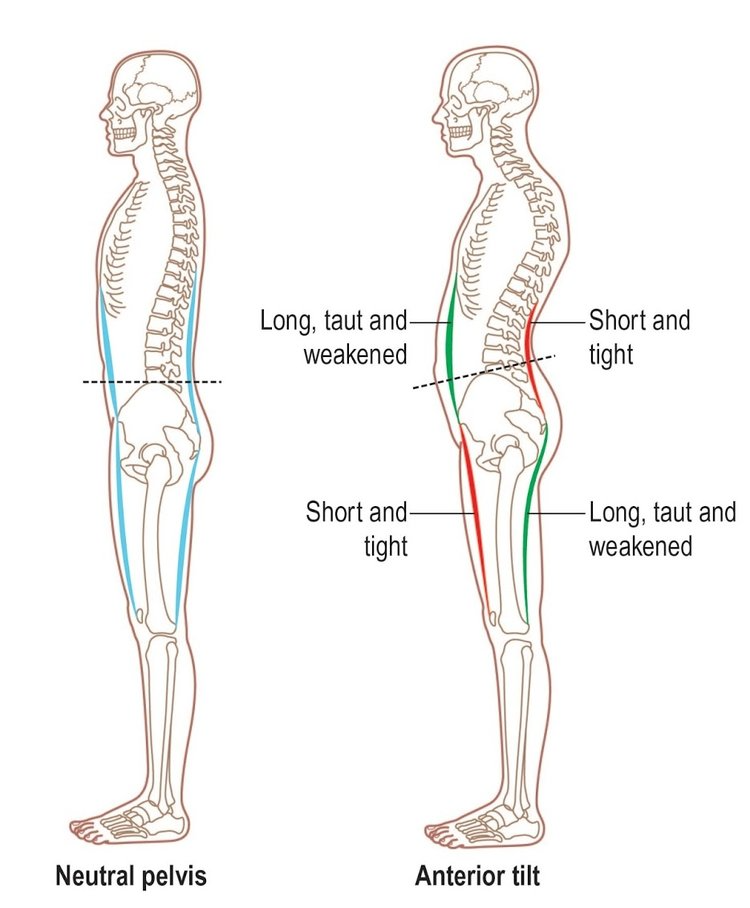
- Due to the growing uterus, some of the core muscles around the pelvis get ‘stretched’ and weakened.
Moreover, the additional weight and altered walking pattern associated with pregnancy can cause significant mechanical strain on the sacroiliac joints, which may result in SIJ inflammation, giving a deep ache in the posterior pelvis.
What are the symptoms of Posterior Pelvic Pain?
Of all the back pains experienced during pregnancy, posterior pelvic pain is the most common – you are four times more likely to experience PPP than lumbar pain.
You may have posterior pelvic pain/sacroiliac joint dysfunction if you have:
- Deep, boring pain in the back of the pelvis (around the sacroiliac joints)
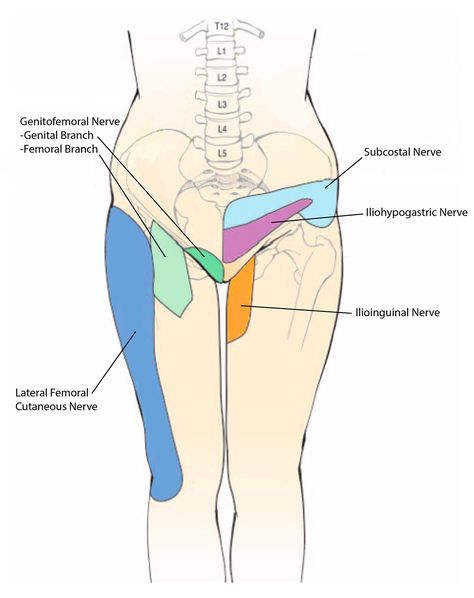
- Pain may occasionally radiate to the groin and thighs.
- The pain is typically worse with standing, walking, climbing stairs, resting on one leg, getting in and out of a low chair, rolling over and twisting in bed, and lifting. The pain improved when lying down.
- If there are inflammation and arthritis in the SI joint, you may experience stiffness and a burning sensation in the pelvis.
Diagnosing Sacroiliac Joint Dysfunction in pregnancy
Your doctor and/or physiotherapist will conduct a thorough history and physical examination to determine the underlying disorders of your pain. That includes a description of symptoms, a series of tests designed to look at the stability, movement, and pain in the sacroiliac joints and surrounding structures.
Imaging, such as computed tomography (CT) scan and X-ray may also help in the diagnosis. Another reliable diagnostic method involves injecting an anaesthetic agent into the SI joint, guided by an X-ray machine, numbing the irritated area, thereby identifying the pain source.
However, due to the concerns of fetal exposure to radiation, diagnostic procedures involving radiation is generally avoided.
Treatment and Management of PPP
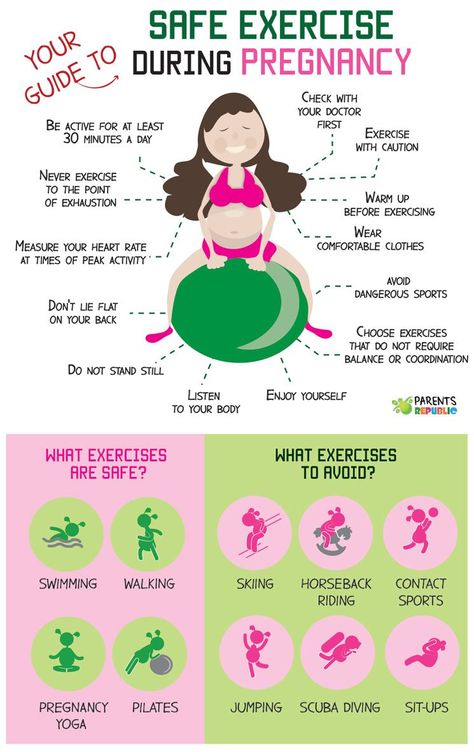
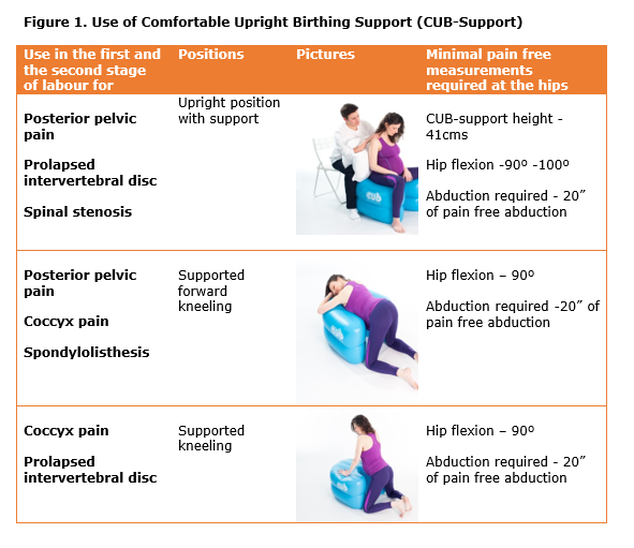
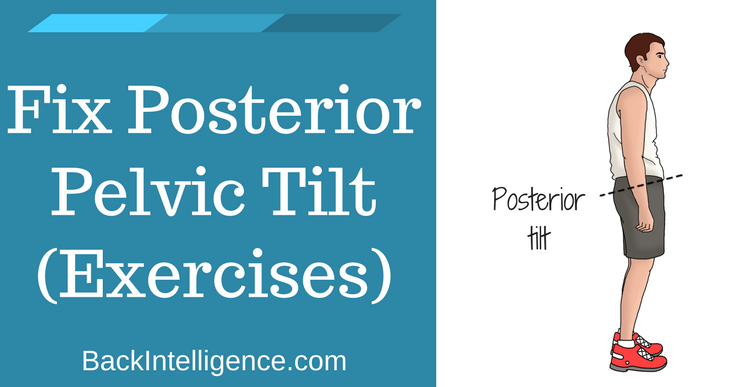
The first-line treatment of pregnancy-related sacroiliac joint dysfunction is physiotherapy and exercises that focus on the core stability of the trunk and pelvic girdle. Sometimes, a sacroiliac belt prescribed to complement the core stability exercises and to give quick pain relief.
Exercises will form a large part of the treatment and in some cases, mobilisation (a gentler form of manipulation) of your hip, back or pelvis may be used to correct any underlying movement dysfunction (Posterior Pelvic Pain – Exercises you can do to relieve the pain).
Other manual techniques include muscle energy technique (MET) and myofascial release. It is vital to engage a physiotherapist who is skilled in treating pregnancy-related pain as she is aware of the studies that support the use of specific stabilizing exercises and other treatment techniques; thereby preventing the dysfunction from escalating into a chronic condition.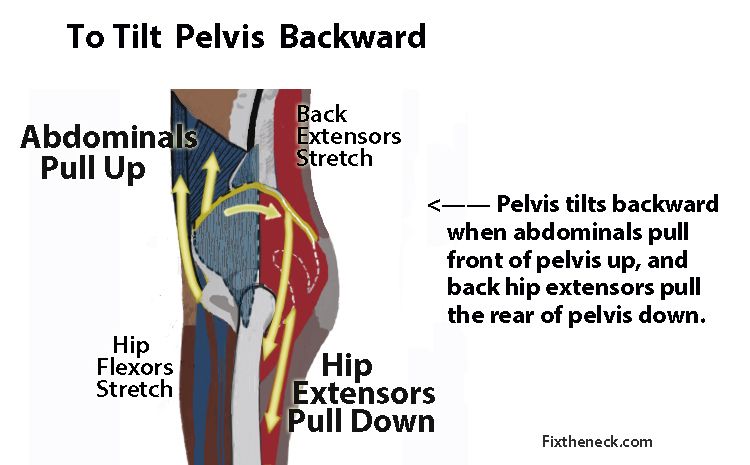
Other alternative treatments include an anaesthetic and steroidal injections into the SIJ that can help in pain relief, which lasts from one day or much more long-term. Oral anti-inflammatory medications are often effective in pain relief as well. However, these two treatments may be contraindicated during pregnancy.
Posterior Pelvic Pain Home Advice during Pregnancy
Here are some tips for expectant women with posterior pelvic pain.
Lying down
- Avoid lying on your back for long periods of time, particularly after the 19th week of your pregnancy.
- Try lying on your side (preferably your left) with a pillow placed between your knees and another under your tummy.
- If your waist sags down into the bed, try placing a small rolled-up towel under your waist.
Turning over in bed
- To turn to your right while lying on your back, arch your lower back, tighten your pelvic floor muscles and lower abdominal muscles and bend both knees one by one.
- Turn your head to the right and take your left arm over to the right of your body. Hold onto the side of your bed if you can.
- To turn, pull with your left hand and take both knees over to the right so that you roll to the right. As soon as possible, bend your knees up as high as they will go – this helps to lock out your pelvis and lessen pain.
- Reverse this to turn to the left.
Getting out of bed
- Roll onto your side with your knees bent up, move your feet over the edge of the bed and push yourself up sideways with your arms.
- Reverse the process when you lie down.
Standing from a sitting position.
- Sit on the edge of the chair.
- Keeping your knees apart slightly and lean forward till your head is directly over your knees, keeping your back straight.
- Stand up by pushing up with your arms, with your back straight and tummy tucked in. This helps to hold your pelvic joints in their most stable position and may reduce your pain significantly.
Experiencing back pain? Click here to find out more about Physiotherapy for back pain relief and how Core Concepts can help.
Reference:
- Fitzgerald CM and Le J. Back pain in pregnancy requires practitioner creativity. Biomechanics. 2007 November
- Ostgaard HC, Andersson GB, Karlsson K. Prevalence of back pain in pregnancy. Spine. 1991; 16:549-552.
- Ostgaard HC, Zetherstrom G, Roos-Hansson E, Svanberg B. Reduction of back and posterior pelvic pain in pregnancy. Spine. 1994; 19:894-900.
- http://www.sidysfunction.com/articles/lumbarbackandposteriorpelvicpain.html
Posterior Pelvic Pain - Exercises you can do to relieve the pain
Table of Contents
Related Articles
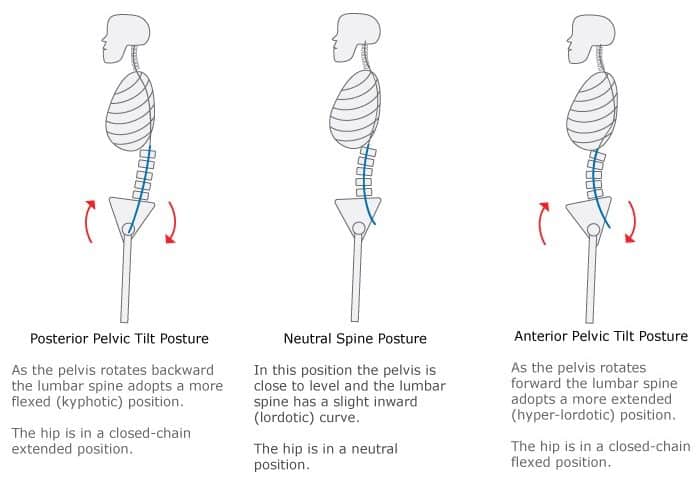
The arched back posture isn’t the only culprit causing lower back pain during pregnancy. A weak and unstable pelvis also contributes to lower back and pelvic pain, often described as Posterior Pelvic Pain.
In the second edition of our Pregnancy & Pain series, our principal physiotherapist, Sylvia Ho shares some strengthening exercises that you can do at home if you have posterior pelvic pain.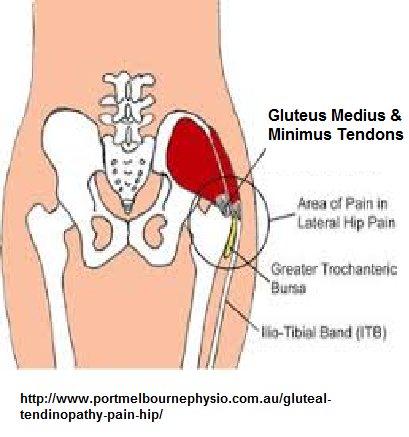 If you are unsure, please seek the advice of a medical professional before commencing on the exercises.
If you are unsure, please seek the advice of a medical professional before commencing on the exercises.
One of the most “invisible” and overlooked ailments faced by expectant mothers is posterior pelvic pain, felt in the lower back and pelvic area caused by a growing load, i.e. your baby. In some cases, the pain extends to the buttocks and the back of the thigh.
The pelvis is made up of three bones: the sacrum bone flanked by two illium bones, held together by ligaments. It is a platform to transfer weight from one leg to the other, with the three bones working as one to facilitate daily activities efficiently, such as walking.
How does posterior pelvic pain occur during pregnancy?Pelvic pain is usually felt in the sacrum — the middle plate — where the joints form. When these ligaments are loose, weight transfer cannot be performed properly, causing pain and imbalance.
During pregnancy, these ligaments become more relaxed due to a hormone relaxin as the body prepares for childbirth.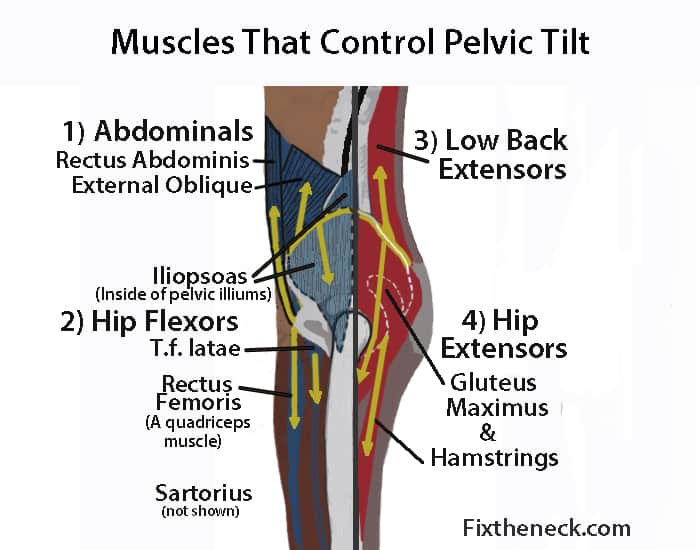 As a result, the pelvis is no longer stable, leading to pain.
As a result, the pelvis is no longer stable, leading to pain.
Thankfully, there are ways to minimise posterior pelvic pain, as long as you start early in your pregnancy. Main exercises, guided by a physiotherapist target and strengthen the transverse abdominus (or corset muscle) and the pelvic belt itself. Stronger muscles increase the stability of the joints, therefore reducing the pain as the muscles are able to support the movement.
Physiotherapy treatment and exercisesIn physiotherapy service for posterior pelvic pain, it is best to consult with a physiotherapist on how to correctly perform these exercises before you conduct them at home.
- Basic position: lie on your back, knees upright, and feet firmly on the ground. Here, you will learn to be aware of your transverse abdominus and perform targeted pelvic exercises.
- Supine march: from the basic position, lift your legs into a 90-degree angle with your shin parallel to the ground.
 Alternate with the other leg, lifting and dropping the suspended leg slowly.
Alternate with the other leg, lifting and dropping the suspended leg slowly. - Leg extensions: from the basic position, lift your legs up perpendicular to the ground and bring them down, activating your pelvic and transverse abdominus muscles to power your movements.
https://youtu.be/tOKnBzJf6H8
References
- Mens, J. M., Vleeming, A., Snijders, C. J., Ronchetti, I., Ginai, A. Z., & Stam, H. J. (2002). Responsiveness of outcome measurements in rehabilitation of patients with posterior pelvic pain since pregnancy. Spine,27(10), 1110-1115.
- Mens, J. M., Vleeming, A., Snijders, C. J., Koes, B. W., & Stam, H. J. (2001). Reliability and validity of the active straight leg raise test in posterior pelvic pain since pregnancy. Spine, 26(10), 1167-1171.
- Wu, W. H., Meijer, O. G., Uegaki, K., Mens, J. M. A., Van Dieen, J. H., Wuisman, P. I. J. M., & Östgaard, H. C. (2004). Pregnancy-related pelvic girdle pain (PPP), I: Terminology, clinical presentation, and prevalence.
 European Spine Journal, 13(7), 575-589.
European Spine Journal, 13(7), 575-589. - Stuge, B., Hilde, G., & Vøllestad, N. (2003). Physical therapy for pregnancy?related low back and pelvic pain: a systematic review. Acta obstetricia et gynecologica Scandinavica, 82(11), 983-990.
Related Articles
Pain in the pelvic area - causes, examination and treatment | Symptoms
Menstrual cramps
Symptoms: Sharp or crampy pains that begin a few days before or during menstruation, are most intense within about 24 hours after the onset of menstruation and subside after 2 to 3 days, often accompanied by headache, nausea, constipation, diarrhea, or frequent urination. urination.
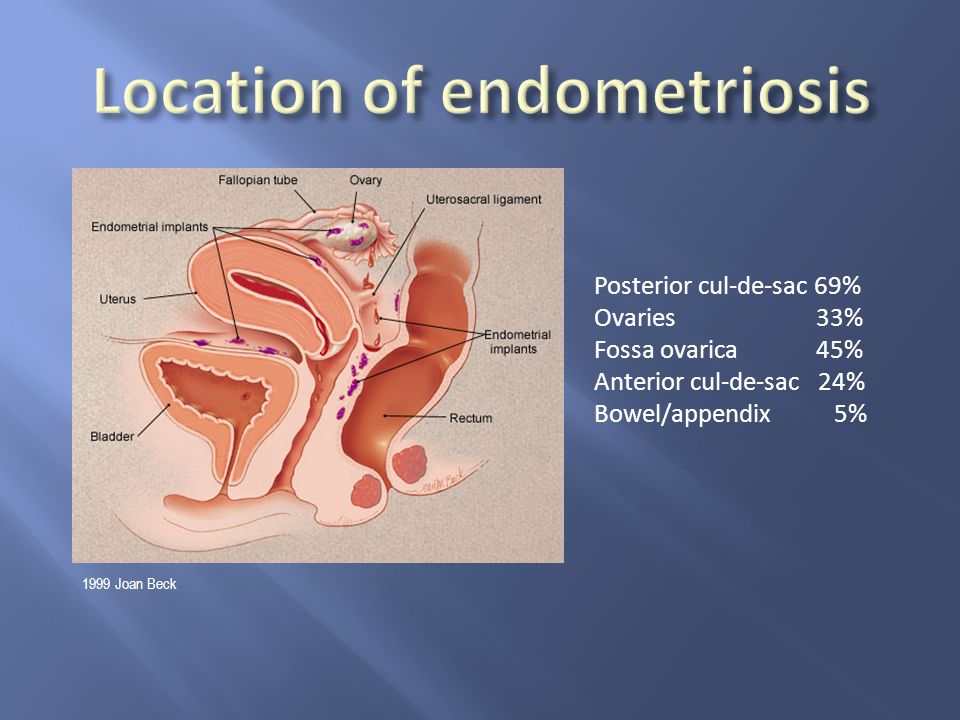
Endometriosis
Signs: Sharp or crampy pain that occurs before and during the first days of menstruation, often pain during intercourse and / or bowel movements. It can eventually lead to pain that is not related to the menstrual cycle.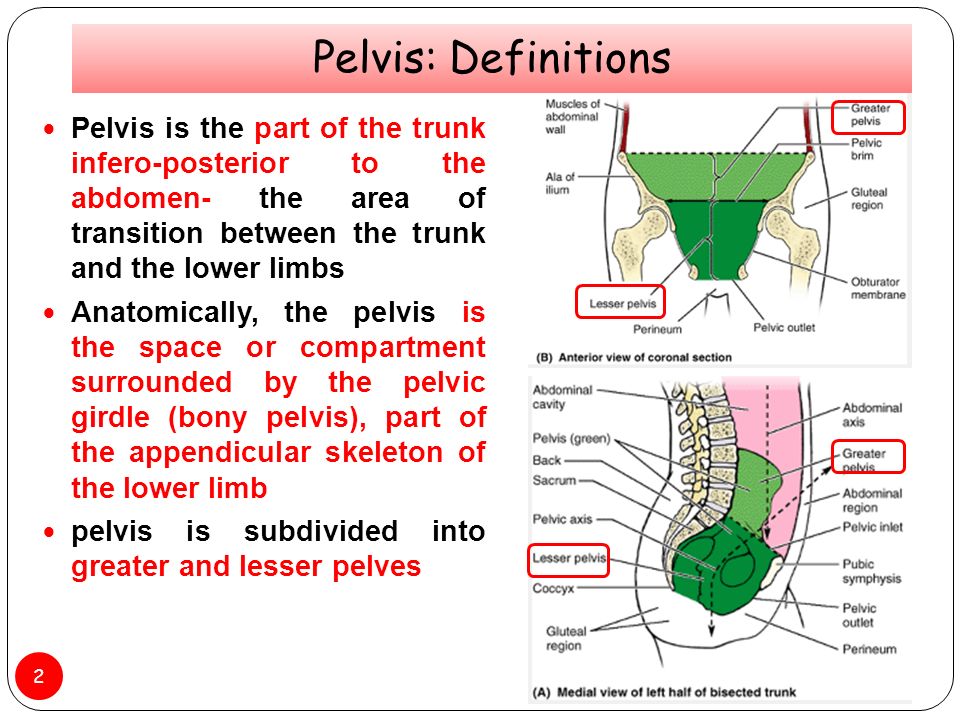
Pain in the middle of the menstrual cycle
Signs: Severe, sharp pain that starts suddenly; can occur on either side, but only on one side each time, occurs at the same time during the menstrual cycle, usually in the middle of the cycle between periods (when the egg is released), most intense at the beginning, but then decreases over 1-2 days, there is often slight bleeding.
Pelvic inflammatory disease
Signs: Aching pain in the pelvic area, which can be felt on one or both sides. Usually a vaginal discharge that is sometimes foul-smelling and can become pus-like and yellow-green in color as the infection progresses. Sometimes pain during urination and/or intercourse, fever or chills, nausea or vomiting.
Rupture of an ovarian cyst
Signs: Pain that starts suddenly is initially limited to one area in the lower abdomen. Sometimes dizziness, fainting, slight vaginal bleeding, nausea, or vomiting occur.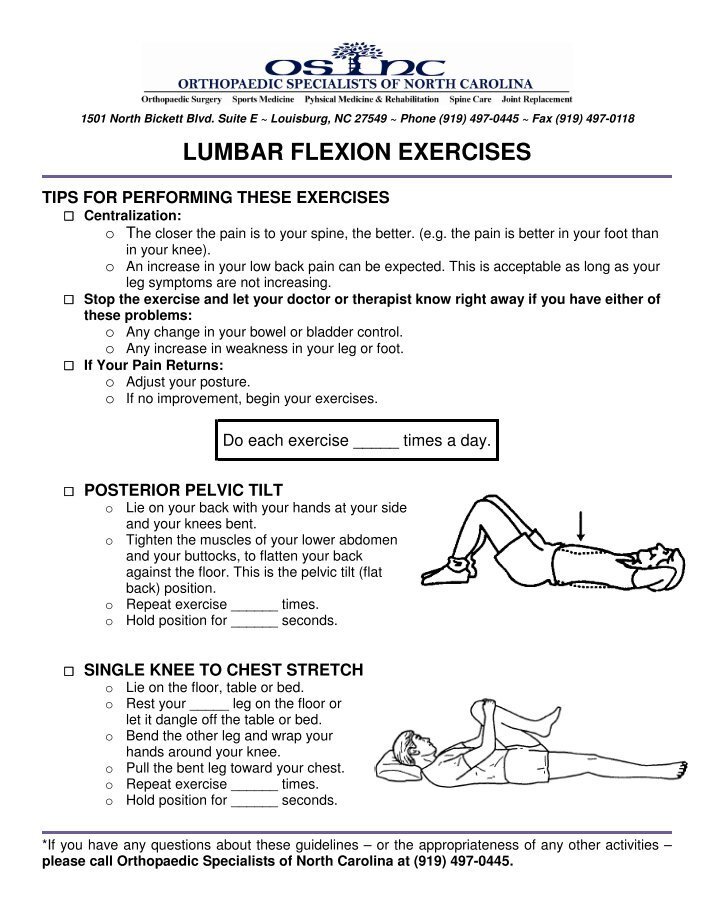
Ectopic pregnancy
Signs: Persistent (not spasmodic) pain that starts suddenly, is initially limited to one area in the lower abdomen. Often slight vaginal bleeding, sometimes dizziness, fainting, fast heartbeat, or dangerously low blood pressure (shock) caused by severe internal bleeding.
Sudden degeneration fibromas in uterus
Symptoms: Sudden pain. It is most common during the first 12 weeks of pregnancy, after childbirth or abortion. Vaginal bleeding may occur.
Torsion (twisting) of the ovarian adnexa
Signs: Severe pain that starts suddenly, occurs on one side, grows rapidly. As well as intermittent pain that comes and goes (when the ovary twists and unwinds). Often occurs in pregnant women, after the use of drugs for the treatment of infertility or with an increase in the ovaries.
Ovarian cancer / Endometrial cancer
Signs: Gradually increasing pain.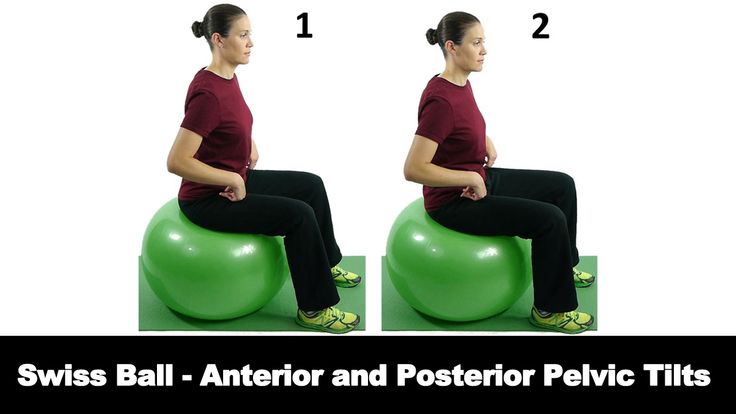 Brown or bloody discharge from the vagina. Abnormal vaginal bleeding (bleeding after menopause or bleeding between periods), sometimes weight loss.
Brown or bloody discharge from the vagina. Abnormal vaginal bleeding (bleeding after menopause or bleeding between periods), sometimes weight loss.
Spikes
Signs: Pain in the pelvic area, which gradually increases, often becomes chronic. As well as pain during intercourse. No vaginal bleeding or discharge. Sometimes nausea and vomiting (suggesting intestinal blockage). In women who have had abdominal surgery or in women with a pelvic infection.
Miscarriage
Signs: Spasmodic pain in the pelvis or back, accompanied by vaginal bleeding. Other signs of early pregnancy such as breast tenderness, nausea, and missed periods.
Appendicitis
Signs: Pain that usually occurs in the lower right side of the abdomen. Loss of appetite and usually nausea and vomiting. Often fever.
Bladder infection
Signs: Pain just above the pubic bone. Sometimes an urgent need to urinate, more frequent urination, or burning when urinating.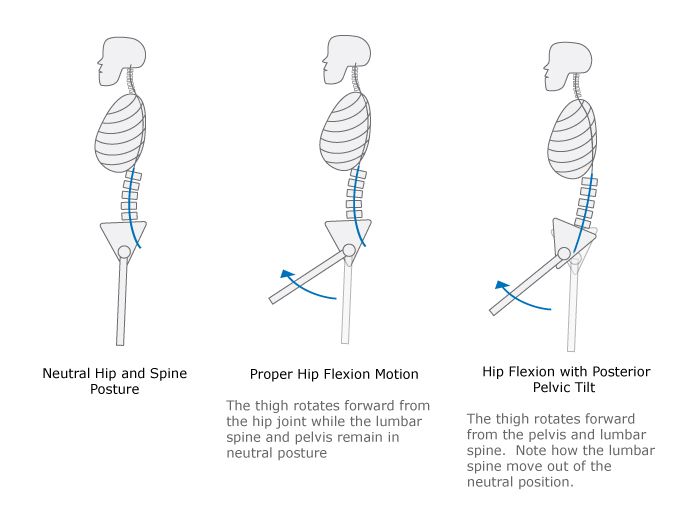
Diverticulitis
Signs: Pain or tenderness in the left lower abdomen, fever.
Inflammatory bowel disease (including Crohn's disease and ulcerative colitis)
Signs: Cramping pain in the abdomen, diarrhea, in ulcerative colitis often with blood in the stool, loss of appetite and weight loss.
Stones in the urinary tract
Signs: Excruciating intermittent pain in the lower abdomen, side or lower back, depending on the location of the stone, nausea and vomiting, blood in the urine.
Gastrointestinal disorders (gastroenteritis, constipation, accumulation of pus; colon cancer)
Musculoskeletal disorders (pubic bone dehiscence after childbirth, fibromyalgia and abdominal muscle tension)
Psychological factors (stress and depression)
Pelvic pain. Women's Health Clinic in Barcelona
El pelvic pain it can be a symptom or a pathology itself. At the Women's CD Gynecology Clinic in Barcelona, we have a dedicated department for the treatment of pelvic pain, given its importance and presence in various gynecological conditions. If a symptom persists for more than six months, it must be evaluated from both a somatic and psychosocial point of view, as described in the Spanish Pain Society.
At the Women's CD Gynecology Clinic in Barcelona, we have a dedicated department for the treatment of pelvic pain, given its importance and presence in various gynecological conditions. If a symptom persists for more than six months, it must be evaluated from both a somatic and psychosocial point of view, as described in the Spanish Pain Society.
Dr. Francisco Carmona is one of the leading experts and authorities in the field of pelvic pain associated with gynecology, along with Dr. Oriol Porta.
Both gynecologists, together with the CD women's team and especially Dr. Dra. Lara Quintas, constitute one of the most important groups in Europe dealing with this pathology. The goal of our gynecological clinic is to offer top notch treatment, especially when it comes to complex problems such as pelvic pain.
Pelvic Pain Unit
In this video, Dr. Oriol Porta, Head of Pelvic Pain, explains some aspects of pelvic pain.
Index
- Pelvic Pain Department
- What is pelvic pain?
- What causes this?
- Symptoms
- Pain during bowel movements
- Pain during urination
- Pain in the ovaries
- Treatment of pelvic pain
- We can help you get rid of pain
- Hear from our patients
- Pelvic Pain Association
- Pelvic Pain Awareness Month
- Latest articles on our Gynecology Blog
- Meet Our Pelvic Pain Experts
What is Pelvic Pain?
El chronic pelvic pain o chronic pelvic pain syndrome (SDPC) is localized pain in the pelvis (area below the navel and above the hips) more than 6 months of evolution, which occurs cyclically or acyclically, continuously or intermittently, and which causes functional disability or limits people's daily activities.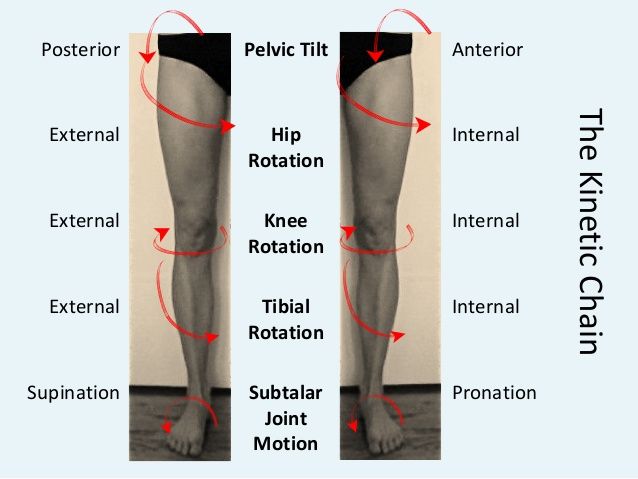 It may be a symptom of another disease or the condition itself.
It may be a symptom of another disease or the condition itself.
What causes this?
There are several conditions that can cause this symptom. However, sometimes pelvic pain develops for no apparent reason, and the underlying cause is diagnosed. Many psychological factors have been described that may contribute to the development of pain ; to this it should be added that the emotional impact of suffering pain Over a long period of time without reliable knowledge of the cause, this contributes to the deterioration of its perception.
Among the possible pathological causes we can find:
-
Muscle tension pelvic floor : The pelvic floor muscles may suffer from contractures and spasms causing chronic pelvic pain.
-
Pelvic inflammatory disease : after transfer pelvic inflammatory disease (usually caused by a sexually transmitted infection) there may be adhesions or scars affecting organs basin .
-
Ovarian cysts : Cysts may periodically develop in the ovaries causing pain
-
Fibroids : These are benign tumors that grow from the muscles of the uterus. Its growth can cause a feeling of pressure or heaviness, as well as pain in the lower abdomen. In rare cases, they produce acute pain when they lose their adequate blood supply and begin to necrotize internally (degeneration of the fibroids)
-
Irritable bowel syndrome : symptoms associated with irritable bowel (bloating, constipation, diarrhea ...) can cause discomfort and pelvic pressure.
-
Interstitial cystitis : This is a condition associated with chronic inflammation of the bladder, which is usually associated with frequent urination. This can happen when the bladder is full pelvic pain which usually improves after emptying
-
Pelvic congestion syndrome : the presence of varicose veins around the uterus and / or ovaries may lead to pelvic pain .
 However, in many cases, varicose veins of the pelvis are completely asymptomatic.
However, in many cases, varicose veins of the pelvis are completely asymptomatic. -
Psychological factors - Depression, chronic stress or sexual abuse may cause or exacerbate chronic pelvic pain . Emotional distress intensifies pelvic pain In turn, pelvic pain creates emotional distress and creates a vicious cycle.
Depending on the origin, the following classification according to the type of pelvic pain can be made:
- Cyclic and non-cyclic gynecological : episiotomy, endometriosis, adhesions, congestive syndromes, pelvic pain associated with sexual disease or pregnancy, vaginal pain syndrome, vulvodynia , interstitial cystitis, vulvodynia or vestibulodynia, dyspareunia, clitoral pain syndrome, neoplasms of the ovaries and uterus.
- gastrointestinal : irritable bowel syndrome, anorectal pain syndrome or chronic proctalgia, fugax proctalgia, inflammatory bowel disease, abdominal hernia, anal fissures .
 ..
.. - Musculoskeletal : pyramidal syndrome, levator ani hypertension, myofascial syndrome, pelvic girdle hypermobility, pelvic floor dysfunction, coccydynia ...
- Neurological : entrapment of the pudendal nerve by a scar or fascia.
- Psychological : Anxiety, somatic problems, sexual dysfunctions, sleep disturbances, past sexual abuse, drug use ...
Symptoms
El chronic pelvic pain It can present in many ways, some of the most common symptoms are:
- Severe pain and maintained
- Intermittent pain or change in intensity and unpredictability.
- Sharp pain and colic .
- Feeling of internal heaviness in pelvis
Pain associated with other activities:
- Pain during sexual intercourse ( dyspareunia )
- Pain refers to stool
- Pain with defecation ( Disquecia ) or urinate ( urinary disorder )
Standing for a long period of time may increase pain and improve when lying down.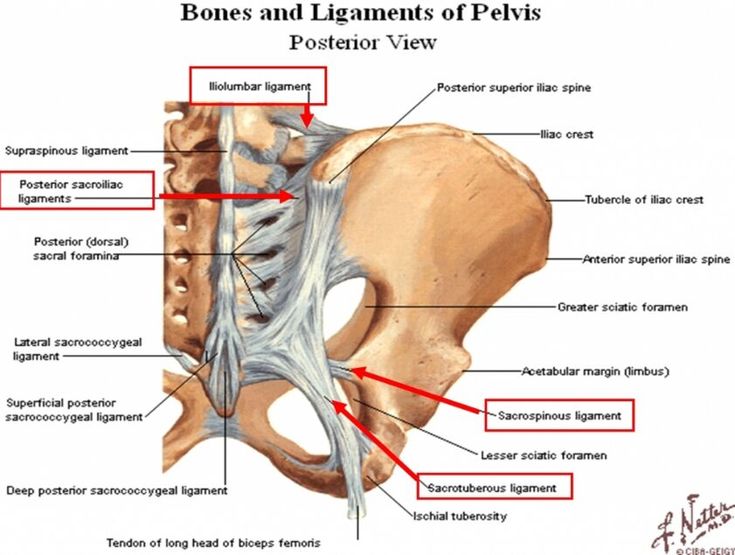 The intensity that the patient perceives pain It can be mild or so strong that it interferes with the patient's daily activities (work, study), disturbs sleep or interferes with sports.
The intensity that the patient perceives pain It can be mild or so strong that it interferes with the patient's daily activities (work, study), disturbs sleep or interferes with sports.
Pain during defecation
In the section on pain, we must highlight pain during defecation , which, as already mentioned, was called Disquecia . This is important because the causes can be confused and a correct diagnosis must be made so as not to increase the time during which the patient does not know what is the cause of her problem.
Pain when urinating
Pain when urinating is called urinary disorder and it can also have a different etiology, so it is necessary to diagnose it and know if it is caused by the same factor that causes this symptom.
Ovarian pain
This is one common way of referring to pelvic pain as one of the causes of ovarian pain this may be due to the presence of ovarian cysts .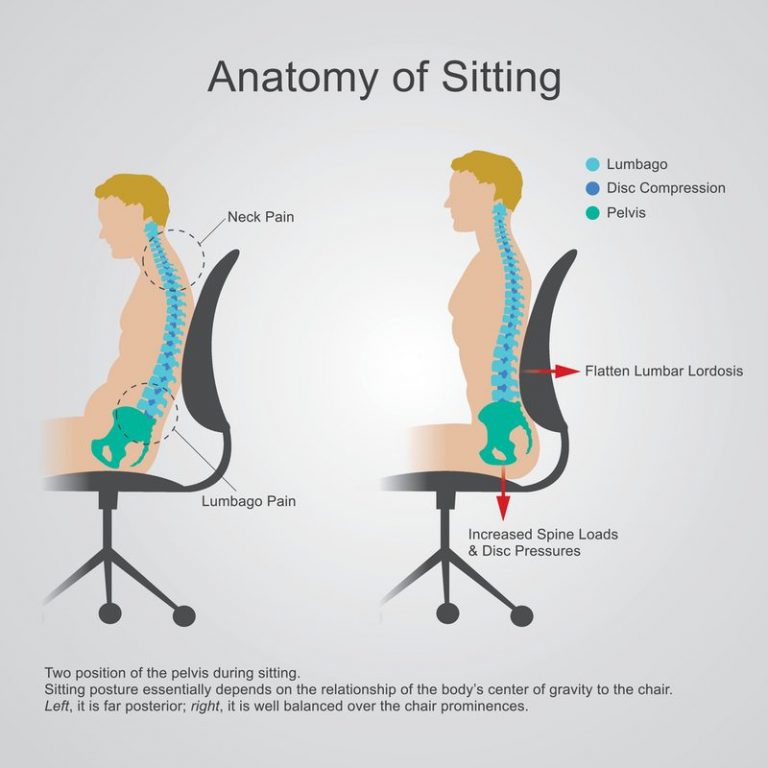
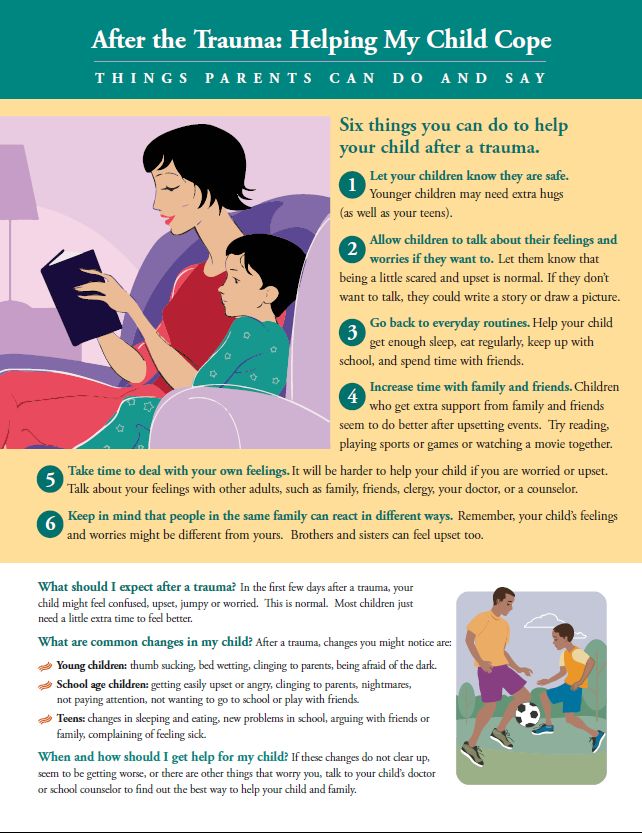
Treatment for pelvic pain
Once the cause of the pelvic pain is identified, treatment will be directed towards treating it.
However, in the case of chronic pain, in many cases it is not possible to find an organic cause. Pain is not always associated with harm.
Emotions matter, context too. Chronic pain needs to be considered and treated comprehensively, globally, in accordance with a biopsychosociological point of view.
A multimodal and interdisciplinary approach is offered, involving different professionals from different disciplines, with different points of view and experience, interested in helping to provide people-centered care.
The first step should always be focused (whether the cause is found or not) on relieving pain . As discussed above, frustration caused by pain itself, lack of sleep, and life disturbances caused by pain can aggravate it significantly, so it is highly recommended to manage the psychological symptoms caused by pain.
-
Painkillers and antihyperalgesics: according to the WHO therapeutic scale, these will be indicated from non-steroidal anti-inflammatory drugs to basic opioids, as well as ancillary drugs.
-
Stress Management Techniques: Several methods for managing anxiety are described, such as breath control, meditation practice, increasing physical activity, and improving sleep. Programs and methods of cognitive behavioral therapy are used to increase resilience.
-
Nerve blockade: for neuropathic pain in which the nerve trunk is suspected to be affected.
La Department of Physiotherapy de Women's Barcelona uses not only methods aimed at restoring the functions of muscles and joints, but also on the central nervous system, stimulating endogenous pathways pain relief rebalancing the activity of the autonomic nervous system as a modulator of possible neurogenic inflammation; and at the vascular level, activating the lymphatic system with myofascial therapy, manual lymphatic drainage .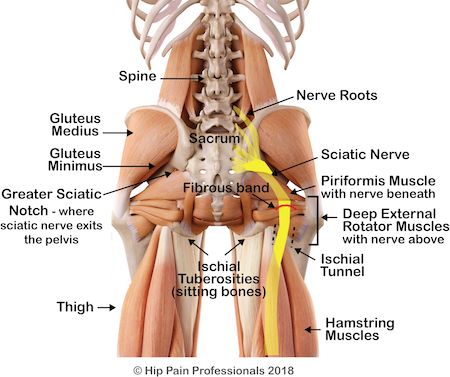 ..
..
El chronic pelvic pain it includes a large number of organic structures linked together in various ways. Therefore, the team of professionals in the Department of Physiotherapy works multidisciplinary with other departments to evaluate and determine the most appropriate therapeutic treatment for each patient.
We can help you get rid of your pain
Don't wait any longer, this pathology is treated and we have a multidisciplinary team in the women's department who will be in charge of finding the best solution for your problem. Pelvic pain .
Our team of professionals will perform the necessary tests and investigations to determine the cause of the pain and determine the most appropriate treatment.
Spain also has an association Chronic pelvic pain in the perineum (ADOPEC), which aims to bring together patients with this pathology in Spain. More information on your adopec.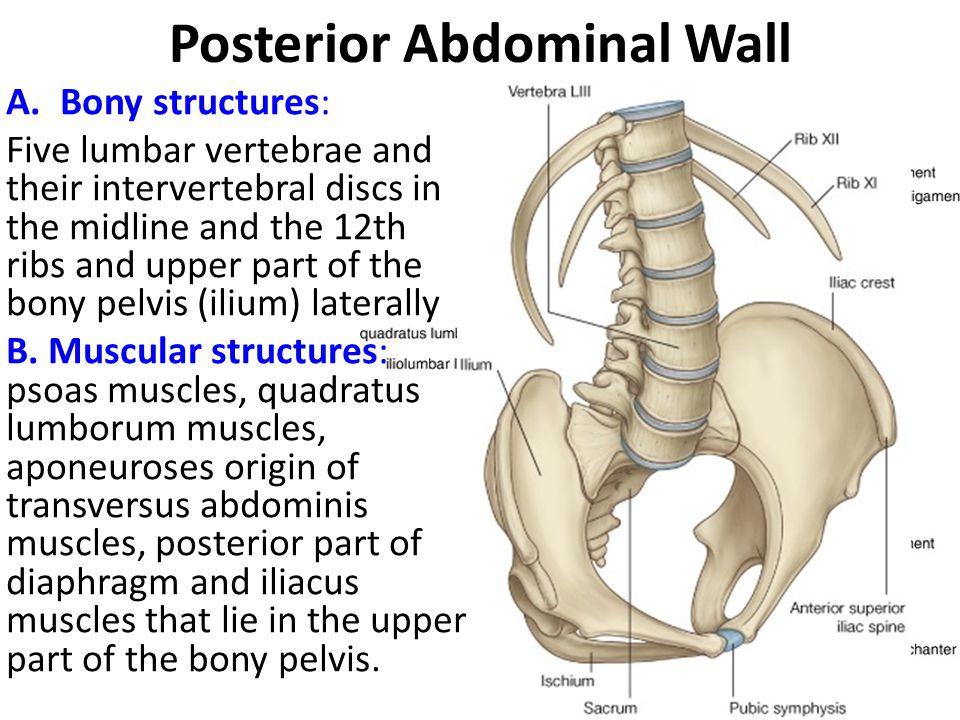 org website.
org website.
Ask our patients
Maria Antolines Thank you very much doctor, I wish there were more doctors like you who remember us and the great indescribable suffering we went through.
Vanesa Gutiérrez Thank you so much doctor for everything you do and for reporting this damn disease that is killing so many people! And thank you personally for helping me and doing your job, my life has now changed! Thank you!
Sylvie Gonzalez Thank you so much for all the struggle you put in for us, I'm having a hard day of pain today and what you're doing gives me strength.
Association of Patients with Pelvic Pain
Recently, in 2016, Association Chronic Pelvic Perineal Pain (ADOPEC) with the aim of collecting and informing all patients about this pathology in Spain. This is a non-profit association that operates throughout the country, its website is adopec.