When does baby stop gaining weight in the womb
Weight Gain & Other Changes
The Third Trimester of Pregnancy: Weight Gain & Other ChangesMedically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By The Healthline Editorial Team on May 15, 2017
The 3rd trimester of pregnancy
Your baby changes most rapidly during your third trimester of pregnancy. Your body will also go through significant changes to support your growing fetus. You may have some of the same changes and symptoms you had during your first and second trimesters, but they are often worse in the third trimester, as you get closer to your baby’s arrival.
Rapid weight gain
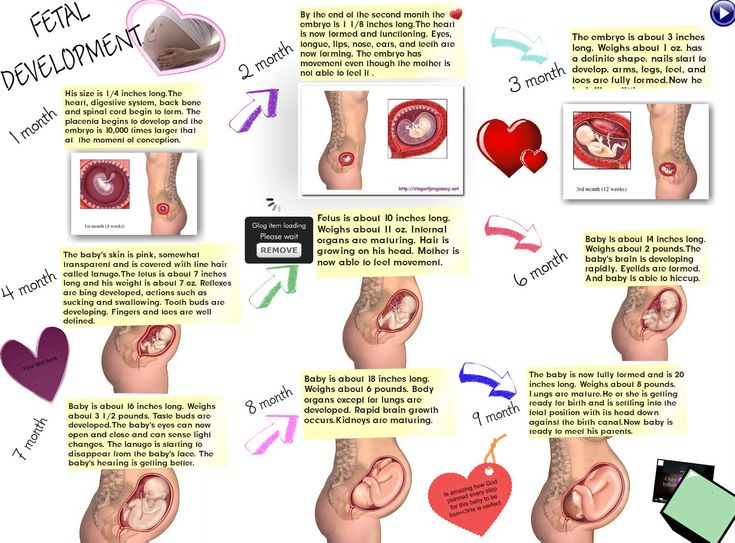
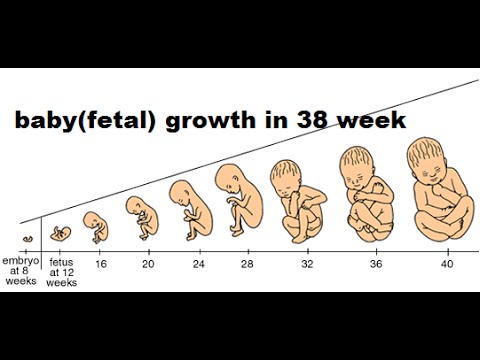
During the final months of pregnancy, your baby gains the most weight. In fact, according to the American Pregnancy Association, a fetus weighs around 2 pounds at 27 weeks, 4 to 4 ½ pounds by 32 weeks, and grows up to between 6 ¾ pounds to 10 pounds, if you have a full-term delivery. Your baby will also grow an average of six more inches during the third trimester.
In addition to baby weight, your body will also gain weight from:
- fluids
- more blood
- amniotic fluid
- a larger uterus
- the placenta
- fat stores
All of these will add a few extra pounds. That’s one reason why doctors and midwives stress that women try not to gain too much weight during the first two trimesters of pregnancy.
While you certainly don’t want to lose weight during the third trimester, it’s also important not to give in to unhealthy food cravings and to be as active as possible. Doing both will help you prevent unnecessaryweight gain. The total amount of weight you should gain depends on how much you weighed pre-pregnancy. Complications of too much weight gain can show up during the third trimester, and may include:
- gestational diabetes
- high blood pressure
- premature birth (baby is born at 37 weeks or earlier)
- heavy birth weight
Leg veins and swelling
Natural weight gain from pregnancy can cause your legs and ankles to swell. The problem can be worse with extra fluid retention, so make sure to drink plenty of water and avoid salty foods. The extra pressure in your lower extremities may lead to spider veins and varicose veins. Take pressure off of your legs by resting with your feet up when you can. You may also consider wearing support stockings if the swelling causes pain.
The problem can be worse with extra fluid retention, so make sure to drink plenty of water and avoid salty foods. The extra pressure in your lower extremities may lead to spider veins and varicose veins. Take pressure off of your legs by resting with your feet up when you can. You may also consider wearing support stockings if the swelling causes pain.
Minor fluid retention is normal, but rapid and painful swelling in your legs and ankles could be a cause for concern. Tell your doctor about any sudden swelling, so they can rule out a potentially life-threatening condition called preeclampsia. It’s marked by extremely high blood pressure, protein in the urine, and sometimes headache and upper-right abdominal pain.
Breast and vaginal changes
It’s normal for breasts to grow larger and more tender during the final weeks of pregnancy. In fact, the Mayo Clinic estimates that women gain an average of 2 pounds of tissue in the breasts during pregnancy. By the third trimester, your breasts may leak colostrum, which is early breast milk that’s yellow in color.
During pregnancy, any significant vaginal changes could be a cause for concern. There’s a small exception during the third trimester. As you near the end of your pregnancy, you may notice some vaginal discharge that looks like mucous and has a spot or two of blood in it. This is a result of your cervix softening to help prepare you for labor. You should call your doctor if you notice:
- excessive discharge
- a discharge that is thick, yellow, green, or cheesy, since this might indicate an infection
- any blood from the vagina
Aches and pains
Your growing baby is starting to get cramped in your belly, so you might start feeling more kicks and other movements. Some of these might be painful from time to time—perhaps your baby is a future soccer star! A growing fetus can cause more body aches for you because of the extra weight you’re carrying. Aches and pains in the back, knees, and neck are common during the third trimester. Rest and put your feet up when you can, and alternate between ice packs and heating pads to ease the pain.
Frequent urination
During the first and second trimesters, you might have needed to urinate more often because of hormonal changes. Now that you’re in the third trimester, it may seem like you have to pee every hour. That’s because all the weight your baby’s gaining puts extra pressure on your bladder. Avoid drinking too many fluids at night to avoid disrupting your sleep.
To prepare for labor, your baby settles into your pelvis. This is called lightening. Once this happens, you might notice being able to breathe more deeply or to eat a bit more food. But your baby’s head is now pushing down even more on your bladder.
Aside from the annoyance, frequent bathroom visits aren’t usually a cause for concern. However, if you notice any blood in your urine or have back pain, call your doctor right away. Both could be signs of a urinary tract infection.
Trouble sleeping at night
Early in your pregnancy you may have wanted to sleep all the time. In your third trimester, you’re more likely to have insomnia. General discomfort is the primary reason why pregnant women can’t sleep. That discomfort can be from needing to urinate or a kicking baby. To make sure you prepare yourself and your bedroom for a good night’s sleep.
In your third trimester, you’re more likely to have insomnia. General discomfort is the primary reason why pregnant women can’t sleep. That discomfort can be from needing to urinate or a kicking baby. To make sure you prepare yourself and your bedroom for a good night’s sleep.
- Avoid exercise in the late afternoon and evening.
- Keep your bedroom cool and dark.
- Avoid late naps or naps longer than an hour.
- Layer your bedding in case you get hot.
- Consider putting a fan at the bedside.
- Leave the TV off in the bedroom. (Even with the sound off, the flickering light can disturb sleep cycles.)
- Take a warm bath before bed.
- Meditate or practice deep breathing exercises.
- Use extra pillows to support your belly.
Other changes
Some mothers-to-be have other changes during the third-trimester, including:
- heartburn
- hemorrhoids
- shortness of breath
- bulging belly button
- Braxton Hicks contractions (These are weak and are not the same as labor contractions.
 )
)
Final preparations for baby
Perhaps the most significant changes you’ll have towards the end of your pregnancy are contractions. Unlike Braxton Hicks contractions, true labor progresses by contractions becoming longer, stronger, and closer together. Congratulations — this is your cue to call your midwife or birth center to prepare for the arrival of your baby!
Last medically reviewed on May 16, 2017
- Parenthood
- Pregnancy
- 3rd Trimester
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Family Doctor Editorial Staff. (2011, February). Changes in your body during pregnancy: Third trimester
familydoctor. org/familydoctor/en/pregnancy-newborns/your-body/changes-in-your-body-during-pregnancy-third-trimester.html
org/familydoctor/en/pregnancy-newborns/your-body/changes-in-your-body-during-pregnancy-third-trimester.html - Fetal development: Third trimester. (2015, August)
americanpregnancy.org/while-pregnant/third-trimester/ - Mayo Clinic Staff. (2014, May 5). Third trimester pregnancy: What to expect
mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/pregnancy/art-20046767 - Stages of pregnancy. (2010, September 27)
womenshealth.gov/pregnancy/youre-pregnant-now-what/stages-pregnancy - Weight gain during pregnancy. (2009, September)
marchofdimes.org/pregnancy/weight-gain-during-pregnancy.aspx
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
May 16, 2017
Written By
The Healthline Editorial Team
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Debra Rose Wilson, PhD, MSN, RN, IBCLC, AHN-BC, CHT
Share this article
Medically reviewed by Debra Rose Wilson, Ph. D., MSN, R.N., IBCLC, AHN-BC, CHT — By The Healthline Editorial Team on May 15, 2017
D., MSN, R.N., IBCLC, AHN-BC, CHT — By The Healthline Editorial Team on May 15, 2017
related stories
How to Predict When Your Baby Will Drop
What Might Go Wrong in the Third Trimester?
How to Dilate Faster During Labor: Is It Possible?
What Do Different Types of Labor Contractions Feel Like?
How to Safely Exercise in the Third Trimester of Pregnancy
Read this next
How to Predict When Your Baby Will Drop
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
Your baby dropping is one of the first signs that your body is getting ready for labor. A registered nurse and mother of four tells you what you need…
READ MORE
What Might Go Wrong in the Third Trimester?
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.
 N., IBCLC, AHN-BC, CHT
N., IBCLC, AHN-BC, CHTWeeks 28 through 40 bring the arrival of the third trimester. This exciting time is definitely the home stretch for expectant mothers, but it’s also a…
READ MORE
How to Dilate Faster During Labor: Is It Possible?
Medically reviewed by Michael Weber, MD
As you approach your due date and delivery, you might be wondering how to speed up the process. Here’s what you need to know about inducing labor and…
READ MORE
What Do Different Types of Labor Contractions Feel Like?
Medically reviewed by Michael Weber, MD
If you’re a first-time mom, you might be wondering what contractions feel like. Here’s a guide to contractions and how to tell if you’re in labor.
READ MORE
How to Safely Exercise in the Third Trimester of Pregnancy
Medically reviewed by Debra Rose Wilson, Ph.
 D., MSN, R.N., IBCLC, AHN-BC, CHT
D., MSN, R.N., IBCLC, AHN-BC, CHTJust 20 minutes a day of low- to moderate-intensity activity can help improve pregnancy symptoms and strengthen your body for delivery. You can still…
READ MORE
Natural Ways to Induce Labor
Medically reviewed by Meredith Wallis, MS, APRN, CNM, IBCLC
There are some natural ways to induce labor. If your due date is here, read this and talk to your doctor about what's right for you.
READ MORE
Inducing Labor Safely: How to Get Your Water to Break
Medically reviewed by Katie Mena, MD
If you’re past your due date, you’re likely anxious to bring your baby into the world. Here’s how to safely induce labor.
READ MORE
Is It Safe to Use Exercise to Induce Labor?
Medically reviewed by Michael Weber, MD
If you’re pregnant and past your due date, you might wonder if exercising will help induce labor.
 Here’s the truth.
Here’s the truth. READ MORE
Does Evening Primrose Oil Safely Induce Labor?
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
You may hear of women taking evening primrose oil to naturally induce labor. Read about this supplement and its safety and effectiveness.
READ MORE
Your Guide to a Pregnancy-Safe Skin Care Routine
When you're expecting, pregnancy-safe skin care can help ensure the health of you and your baby. We'll tell you what to avoid — and some good…
READ MORE
Weight Gain & Other Changes
The Third Trimester of Pregnancy: Weight Gain & Other ChangesMedically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By The Healthline Editorial Team on May 15, 2017
The 3rd trimester of pregnancy
Your baby changes most rapidly during your third trimester of pregnancy. Your body will also go through significant changes to support your growing fetus. You may have some of the same changes and symptoms you had during your first and second trimesters, but they are often worse in the third trimester, as you get closer to your baby’s arrival.
Your body will also go through significant changes to support your growing fetus. You may have some of the same changes and symptoms you had during your first and second trimesters, but they are often worse in the third trimester, as you get closer to your baby’s arrival.
Rapid weight gain
During the final months of pregnancy, your baby gains the most weight. In fact, according to the American Pregnancy Association, a fetus weighs around 2 pounds at 27 weeks, 4 to 4 ½ pounds by 32 weeks, and grows up to between 6 ¾ pounds to 10 pounds, if you have a full-term delivery. Your baby will also grow an average of six more inches during the third trimester.
In addition to baby weight, your body will also gain weight from:
- fluids
- more blood
- amniotic fluid
- a larger uterus
- the placenta
- fat stores
All of these will add a few extra pounds. That’s one reason why doctors and midwives stress that women try not to gain too much weight during the first two trimesters of pregnancy.
While you certainly don’t want to lose weight during the third trimester, it’s also important not to give in to unhealthy food cravings and to be as active as possible. Doing both will help you prevent unnecessaryweight gain. The total amount of weight you should gain depends on how much you weighed pre-pregnancy. Complications of too much weight gain can show up during the third trimester, and may include:
- gestational diabetes
- high blood pressure
- premature birth (baby is born at 37 weeks or earlier)
- heavy birth weight
Leg veins and swelling
Natural weight gain from pregnancy can cause your legs and ankles to swell. The problem can be worse with extra fluid retention, so make sure to drink plenty of water and avoid salty foods. The extra pressure in your lower extremities may lead to spider veins and varicose veins. Take pressure off of your legs by resting with your feet up when you can. You may also consider wearing support stockings if the swelling causes pain.
Minor fluid retention is normal, but rapid and painful swelling in your legs and ankles could be a cause for concern. Tell your doctor about any sudden swelling, so they can rule out a potentially life-threatening condition called preeclampsia. It’s marked by extremely high blood pressure, protein in the urine, and sometimes headache and upper-right abdominal pain.
Breast and vaginal changes
It’s normal for breasts to grow larger and more tender during the final weeks of pregnancy. In fact, the Mayo Clinic estimates that women gain an average of 2 pounds of tissue in the breasts during pregnancy. By the third trimester, your breasts may leak colostrum, which is early breast milk that’s yellow in color.
During pregnancy, any significant vaginal changes could be a cause for concern. There’s a small exception during the third trimester. As you near the end of your pregnancy, you may notice some vaginal discharge that looks like mucous and has a spot or two of blood in it. This is a result of your cervix softening to help prepare you for labor. You should call your doctor if you notice:
This is a result of your cervix softening to help prepare you for labor. You should call your doctor if you notice:
- excessive discharge
- a discharge that is thick, yellow, green, or cheesy, since this might indicate an infection
- any blood from the vagina
Aches and pains
Your growing baby is starting to get cramped in your belly, so you might start feeling more kicks and other movements. Some of these might be painful from time to time—perhaps your baby is a future soccer star! A growing fetus can cause more body aches for you because of the extra weight you’re carrying. Aches and pains in the back, knees, and neck are common during the third trimester. Rest and put your feet up when you can, and alternate between ice packs and heating pads to ease the pain.
Frequent urination
During the first and second trimesters, you might have needed to urinate more often because of hormonal changes. Now that you’re in the third trimester, it may seem like you have to pee every hour.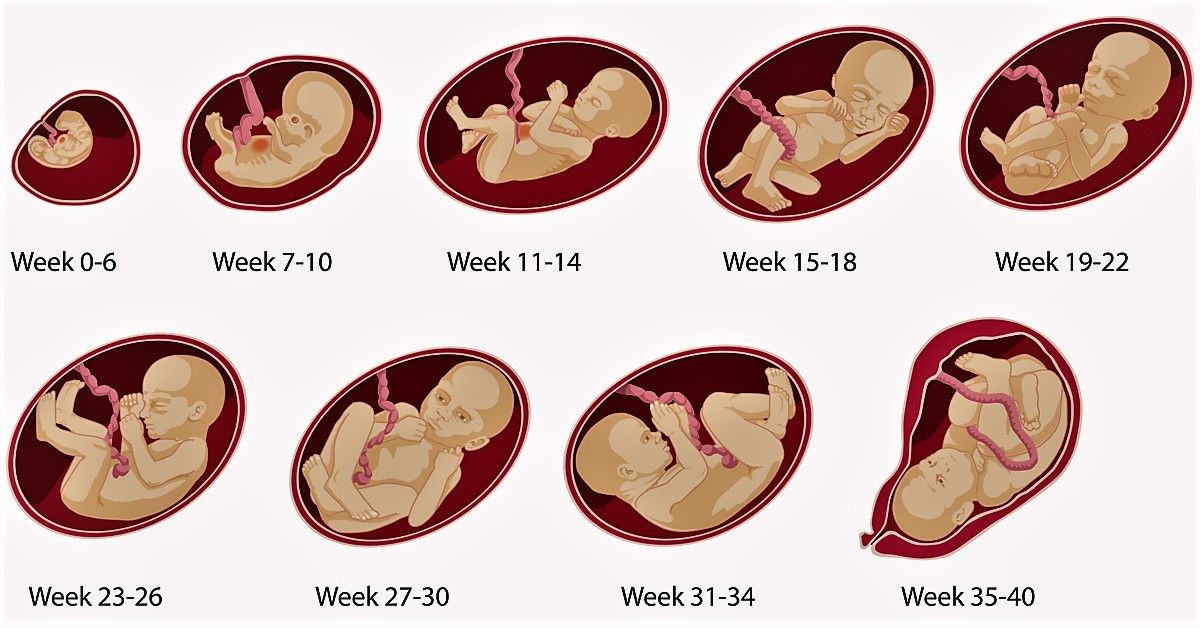 That’s because all the weight your baby’s gaining puts extra pressure on your bladder. Avoid drinking too many fluids at night to avoid disrupting your sleep.
That’s because all the weight your baby’s gaining puts extra pressure on your bladder. Avoid drinking too many fluids at night to avoid disrupting your sleep.
To prepare for labor, your baby settles into your pelvis. This is called lightening. Once this happens, you might notice being able to breathe more deeply or to eat a bit more food. But your baby’s head is now pushing down even more on your bladder.
Aside from the annoyance, frequent bathroom visits aren’t usually a cause for concern. However, if you notice any blood in your urine or have back pain, call your doctor right away. Both could be signs of a urinary tract infection.
Trouble sleeping at night
Early in your pregnancy you may have wanted to sleep all the time. In your third trimester, you’re more likely to have insomnia. General discomfort is the primary reason why pregnant women can’t sleep. That discomfort can be from needing to urinate or a kicking baby. To make sure you prepare yourself and your bedroom for a good night’s sleep.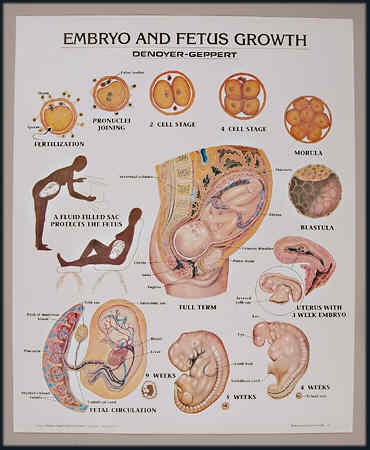
- Avoid exercise in the late afternoon and evening.
- Keep your bedroom cool and dark.
- Avoid late naps or naps longer than an hour.
- Layer your bedding in case you get hot.
- Consider putting a fan at the bedside.
- Leave the TV off in the bedroom. (Even with the sound off, the flickering light can disturb sleep cycles.)
- Take a warm bath before bed.
- Meditate or practice deep breathing exercises.
- Use extra pillows to support your belly.
Other changes
Some mothers-to-be have other changes during the third-trimester, including:
- heartburn
- hemorrhoids
- shortness of breath
- bulging belly button
- Braxton Hicks contractions (These are weak and are not the same as labor contractions.)
Final preparations for baby
Perhaps the most significant changes you’ll have towards the end of your pregnancy are contractions. Unlike Braxton Hicks contractions, true labor progresses by contractions becoming longer, stronger, and closer together. Congratulations — this is your cue to call your midwife or birth center to prepare for the arrival of your baby!
Congratulations — this is your cue to call your midwife or birth center to prepare for the arrival of your baby!
Last medically reviewed on May 16, 2017
- Parenthood
- Pregnancy
- 3rd Trimester
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Family Doctor Editorial Staff. (2011, February). Changes in your body during pregnancy: Third trimester
familydoctor.org/familydoctor/en/pregnancy-newborns/your-body/changes-in-your-body-during-pregnancy-third-trimester.html - Fetal development: Third trimester. (2015, August)
americanpregnancy.org/while-pregnant/third-trimester/ - Mayo Clinic Staff.
 (2014, May 5). Third trimester pregnancy: What to expect
(2014, May 5). Third trimester pregnancy: What to expect
mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/pregnancy/art-20046767 - Stages of pregnancy. (2010, September 27)
womenshealth.gov/pregnancy/youre-pregnant-now-what/stages-pregnancy - Weight gain during pregnancy. (2009, September)
marchofdimes.org/pregnancy/weight-gain-during-pregnancy.aspx
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
May 16, 2017
Written By
The Healthline Editorial Team
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Debra Rose Wilson, PhD, MSN, RN, IBCLC, AHN-BC, CHT
Share this article
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By The Healthline Editorial Team on May 15, 2017
related stories
How to Predict When Your Baby Will Drop
What Might Go Wrong in the Third Trimester?
How to Dilate Faster During Labor: Is It Possible?
What Do Different Types of Labor Contractions Feel Like?
How to Safely Exercise in the Third Trimester of Pregnancy
Read this next
How to Predict When Your Baby Will Drop
Medically reviewed by Debra Rose Wilson, Ph.
 D., MSN, R.N., IBCLC, AHN-BC, CHT
D., MSN, R.N., IBCLC, AHN-BC, CHTYour baby dropping is one of the first signs that your body is getting ready for labor. A registered nurse and mother of four tells you what you need…
READ MORE
What Might Go Wrong in the Third Trimester?
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
Weeks 28 through 40 bring the arrival of the third trimester. This exciting time is definitely the home stretch for expectant mothers, but it’s also a…
READ MORE
How to Dilate Faster During Labor: Is It Possible?
Medically reviewed by Michael Weber, MD
As you approach your due date and delivery, you might be wondering how to speed up the process. Here’s what you need to know about inducing labor and…
READ MORE
What Do Different Types of Labor Contractions Feel Like?
Medically reviewed by Michael Weber, MD
If you’re a first-time mom, you might be wondering what contractions feel like.
 Here’s a guide to contractions and how to tell if you’re in labor.
Here’s a guide to contractions and how to tell if you’re in labor.READ MORE
How to Safely Exercise in the Third Trimester of Pregnancy
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
Just 20 minutes a day of low- to moderate-intensity activity can help improve pregnancy symptoms and strengthen your body for delivery. You can still…
READ MORE
Natural Ways to Induce Labor
Medically reviewed by Meredith Wallis, MS, APRN, CNM, IBCLC
There are some natural ways to induce labor. If your due date is here, read this and talk to your doctor about what's right for you.
READ MORE
Inducing Labor Safely: How to Get Your Water to Break
Medically reviewed by Katie Mena, MD
If you’re past your due date, you’re likely anxious to bring your baby into the world.
 Here’s how to safely induce labor.
Here’s how to safely induce labor.READ MORE
Is It Safe to Use Exercise to Induce Labor?
Medically reviewed by Michael Weber, MD
If you’re pregnant and past your due date, you might wonder if exercising will help induce labor. Here’s the truth.
READ MORE
Does Evening Primrose Oil Safely Induce Labor?
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
You may hear of women taking evening primrose oil to naturally induce labor. Read about this supplement and its safety and effectiveness.
READ MORE
Your Guide to a Pregnancy-Safe Skin Care Routine
When you're expecting, pregnancy-safe skin care can help ensure the health of you and your baby. We'll tell you what to avoid — and some good…
READ MORE
Fetal growth retardation (FGR)
Gynecology
It happens that expectant mothers hear a frighteningly incomprehensible abbreviation - ZRP at the appointment with the attending physician or in the ultrasound room.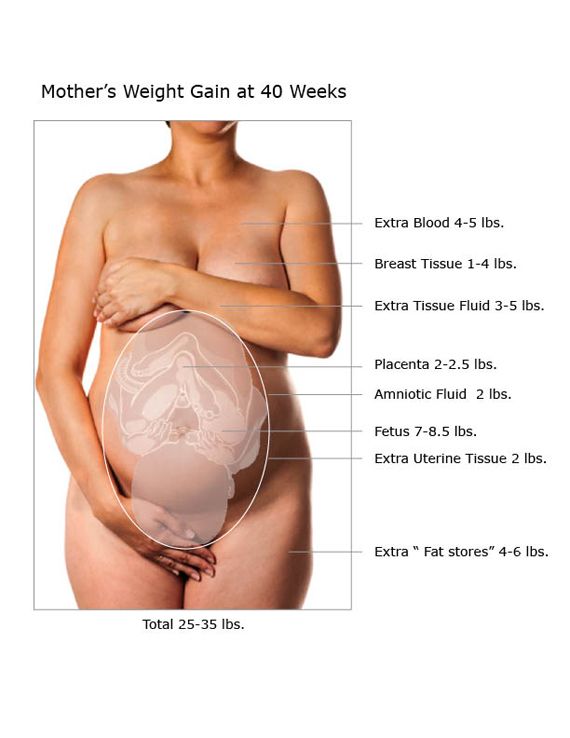 Its decoding is even more frightening: "delayed fetal development." A pregnant woman faced with a similar diagnosis is tormented by many questions. How dangerous is this condition? How will it affect the health of the baby? Will he be able to catch up?
Its decoding is even more frightening: "delayed fetal development." A pregnant woman faced with a similar diagnosis is tormented by many questions. How dangerous is this condition? How will it affect the health of the baby? Will he be able to catch up?
Adult people are not alike, and among the many external differences, they differ in height and weight. Even the same person at different periods of his life can lose weight or gain weight, and this does not cause alarm in anyone. Very young children are another matter: clear criteria are calculated for them, a deviation from which indicates that something is wrong with the baby. And the smaller the child, the more important is the correspondence of his physical development to certain norms. And to assess the state of intrauterine development of the fetus, its size is the most objective criterion.
The weight of a child at birth is very important for his development, especially in the first year of life, and affects his health later on.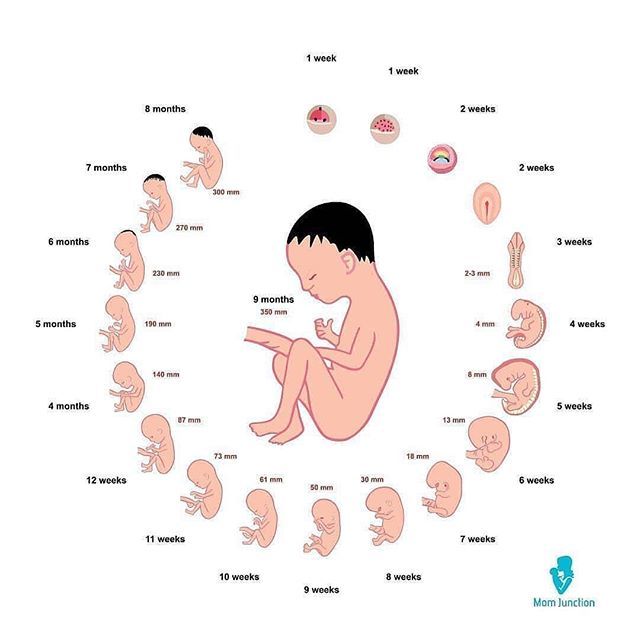 Children born with low body weight (up to 2500 grams) are more prone to obstetric complications: they tolerate childbirth worse, they develop hypoxia and even asphyxia more often than children with normal weight, and neurological disorders also occur.
Children born with low body weight (up to 2500 grams) are more prone to obstetric complications: they tolerate childbirth worse, they develop hypoxia and even asphyxia more often than children with normal weight, and neurological disorders also occur.
As a result, these babies do not adapt well to a new life. In infancy, they suffer from hyperexcitability, increased or, conversely, decreased muscle tone, sluggishly suck and often spit up food, gain weight poorly, and may lag behind their peers in psychomotor development. Even at the age of 7-8 years, such children are hyperactive, clumsy and do not know how to concentrate on the necessary subject for a long time. The difference between healthy babies and small babies only blurs by 9-10 years, although in height and weight they catch up with their peers by the age of two. However, the consequences of the transferred condition can “come around” already in adulthood. Recent studies have shown an association between low birth weight and an increased risk of developing cardiovascular disease, obesity, diabetes mellitus and elevated blood lipids, all of which are associated with congenital endocrine disorders seen in low birth weight infants. Therefore, such a pathology as " Fetal growth retardation " (FGR or fetal malnutrition) deserves special attention.
Therefore, such a pathology as " Fetal growth retardation " (FGR or fetal malnutrition) deserves special attention.
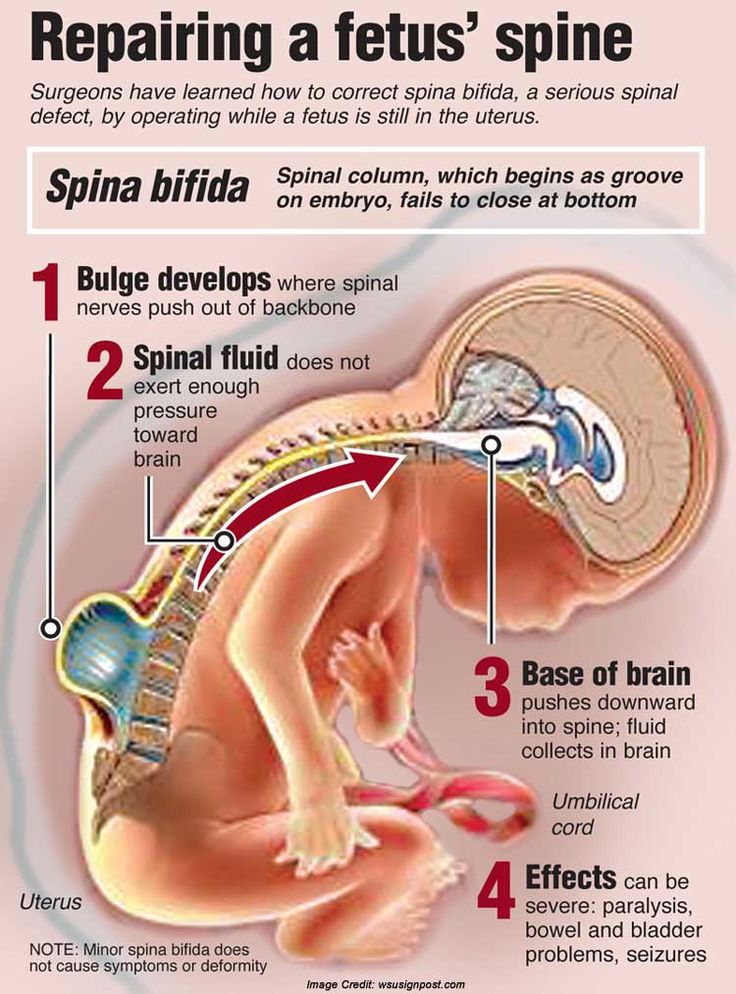
FGR can be symmetrical, when all organs are evenly reduced, and asymmetric, when the brain and skeleton correspond to the gestational age, and the internal organs lag behind in development. The reasons for this are smoking, alcohol consumption, chromosomal abnormalities, infections, but most often - fetoplacental insufficiency and other conditions that lead to circulatory disorders: high or low blood pressure, toxicosis of the second half of pregnancy, diabetes mellitus with vascular damage, kidney disease, etc.
The development of fetal malnutrition is influenced by the age of the mother . The fact is that the body of very young mothers (16-18 years old) is simply not yet ready for the upcoming stresses, while older mothers (32-40 years old) most often already have a “baggage” of chronic diseases. Smoking, addiction to alcohol and any drugs clearly contribute to the development of malnutrition, as they cause pronounced vasoconstriction and reduce uteroplacental blood flow. Alas, quite often hypotrophy is observed during multiple pregnancies, since two or even three twins have to share, literally brotherly, the nutrients received from the mother.
Alas, quite often hypotrophy is observed during multiple pregnancies, since two or even three twins have to share, literally brotherly, the nutrients received from the mother.
One of the simplest methods of monitoring fetal development is to measure the size of the uterus. As soon as it can be easily felt above the womb - approximately at the fourth month of pregnancy, at each visit, the doctor will measure the height of the fundus of the uterus, and in the second half of pregnancy, the circumference of the abdomen at the level of the navel. This will allow the doctor to roughly judge the size of the fetus. Obviously, these indicators are not objective enough, because their value is influenced by the thickness of the anterior abdominal wall, the amount of amniotic fluid, and the physique of the woman.
The most accurate diagnostic method is the ultrasound biometry used in our Clinic , which measures and evaluates several fetal parameters. The most traditional is the measurement of the head, tummy and femur, but if the doctor has doubts, he will also take additional measurements. The accuracy of the diagnosis is ensured by the high qualification of the doctor conducting the study, the excellent resolution of our Sonix OP ultrasound scanner and the possibility of conducting a Doppler study. Ultrasound also controls the amount of amniotic fluid, reveals signs of placental dysfunction, as well as changes in blood flow in it, which helps the doctor to accurately make a preliminary diagnosis and begin treatment. To clarify the diagnosis, we carry out Doppler study of the vessels of the placenta, umbilical cord and large vessels of the fetus, as well as cardiotocography (CTG), , which allows you to register the fetal heartbeat and the nature of changes in the frequency of its heartbeats in response to movements or uterine contractions. It is important that normal Doppler and CTG data - even in the presence of low weight, indicate the well-being of the baby. If the examination did not reveal any deviations, then it becomes clear that we are talking about a healthy, low-weight fetus.
The accuracy of the diagnosis is ensured by the high qualification of the doctor conducting the study, the excellent resolution of our Sonix OP ultrasound scanner and the possibility of conducting a Doppler study. Ultrasound also controls the amount of amniotic fluid, reveals signs of placental dysfunction, as well as changes in blood flow in it, which helps the doctor to accurately make a preliminary diagnosis and begin treatment. To clarify the diagnosis, we carry out Doppler study of the vessels of the placenta, umbilical cord and large vessels of the fetus, as well as cardiotocography (CTG), , which allows you to register the fetal heartbeat and the nature of changes in the frequency of its heartbeats in response to movements or uterine contractions. It is important that normal Doppler and CTG data - even in the presence of low weight, indicate the well-being of the baby. If the examination did not reveal any deviations, then it becomes clear that we are talking about a healthy, low-weight fetus. In this case, we simply observe the woman without any therapy.
In this case, we simply observe the woman without any therapy.
The first signs of IGR can be detected in such a study as early as 24-26 weeks, and its symmetrical form is more often noted. The occurrence of malnutrition after 32 weeks is more typical for the asymmetric form, and fetal hypoxia usually also joins it.
Identified fetal growth retardation should be treated. The goal of treatment in this case is not to “fatten the baby”, but to normalize metabolic processes and support the vital functions of the fetus. Of course, the success of treatment largely depends on how timely it is started. A large arsenal of medicines is used to treat malnutrition. It should be individual, taking into account the cause that caused IGR in this particular case and aimed at treating both the woman's diseases and pregnancy complications. For expectant mothers who are carrying a small child, it is very important to have a good diet rich in vitamins and animal proteins, as well as a regimen with limited physical activity. Although you should not overeat, remembering that excesses in the diet do not at all lead to a proportional increase in the amount of nutrients taken by the placenta for the fetus.
Although you should not overeat, remembering that excesses in the diet do not at all lead to a proportional increase in the amount of nutrients taken by the placenta for the fetus.
Depending on the severity of the condition of the fetus, the treatment is carried out on an outpatient basis, for example, in our day hospital, or in the maternity hospital. Although, as you know, houses and walls help, but in severe cases it is better not to refuse hospitalization. In the hospital, it is easier to monitor the condition of the mother and baby, and therefore provide more effective assistance. The effect of therapeutic measures must be constantly monitored using ultrasound and CTG, which are usually prescribed at intervals of 2 weeks, and if necessary, more often. FGR treatment almost always produces good results. In most cases, it is possible to observe adequate fetal growth: for example, in 7-10 days, the size of the fetus increases accordingly, and does not lag even further, which is considered a completely satisfactory result.
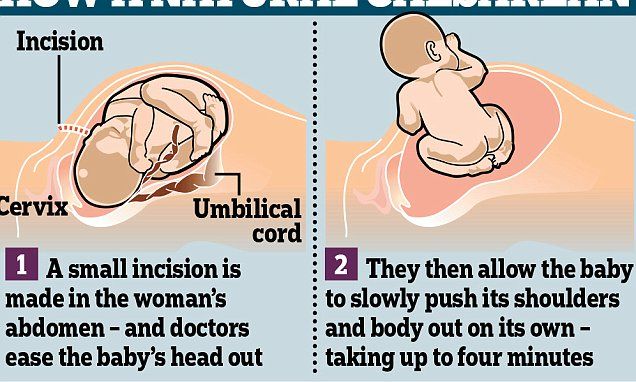
The method and timing of delivery largely depend on the condition of the fetus. If the treatment of FGR is successful and the baby is growing, then it makes no sense to rush things, because by the end of pregnancy it can reach quite a decent size. If, despite all efforts, the child does not gain weight or has any other problems, then they resort to early delivery. At a gestational age close to full-term and ready-made birth canal, natural labor is usually stimulated. At the same time, childbirth is carried out under close medical supervision. However, if the baby is so weak that ordinary childbirth will be too big a test for him, then they resort to a caesarean section. Women who are diagnosed with fetal hypotrophy need to choose a maternity hospital, on the basis of which a modern nursing service for small children is organized, because it is important for such a child to provide qualified assistance from the first minutes of life.
But the best way to prevent this problem is prevention.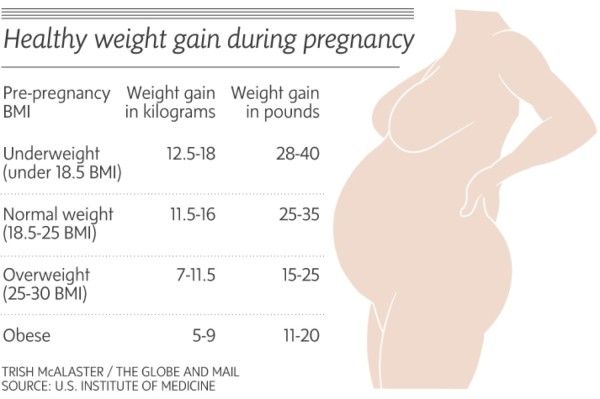 When planning a pregnancy, it is necessary to undergo a thorough examination by specialists, sanitize foci of chronic infection, and say goodbye to bad habits. Sometimes for pregnant women at high risk for FGR, we recommend courses of drug prophylaxis for up to 12 weeks, at 20-23 and 30-32 weeks, which include vasodilators and vitamins.
When planning a pregnancy, it is necessary to undergo a thorough examination by specialists, sanitize foci of chronic infection, and say goodbye to bad habits. Sometimes for pregnant women at high risk for FGR, we recommend courses of drug prophylaxis for up to 12 weeks, at 20-23 and 30-32 weeks, which include vasodilators and vitamins.
Fetal growth retardation, the fetus does not gain weight, what to expect? Part 2 - Family Clinic
In one of the previous articles, we discussed the topic of fetal growth retardation. We got acquainted with some competent terms, and came to the conclusion that the diagnosis is made on the basis of ultrasound parameters, when certain indicators are less than normal.
In this article, we will consider the norms for the size of the fetus, what are they?
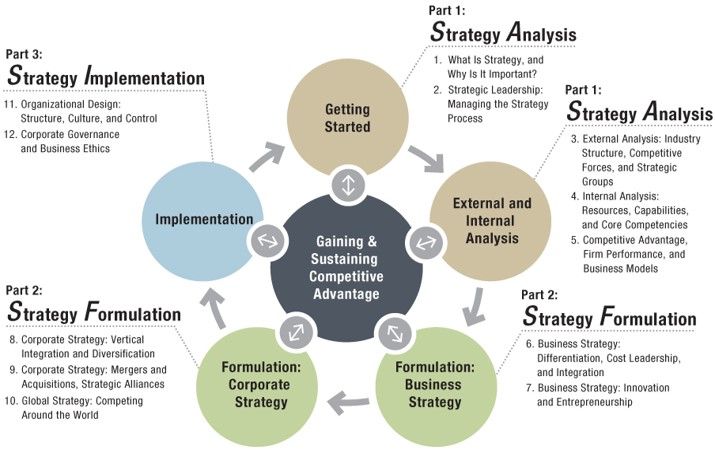
Each doctor who performs ultrasound during pregnancy has a special table (it can be in paper or electronic form) that indicates the parameters, weeks of gestation, and percentiles: namely the 10th percentile, 50th percentile and 9th percentile0th percentile. A percentile is a statistic. The number of percentiles can change, as well as the number of parameters. It is important to understand that the fetus does not grow according to a textbook, but according to its genetic program, and the tasks of an obstetrician-gynecologist with an ultrasound doctor should be understood in dynamics: is it an individual feature of the baby of such intrauterine growth or, indeed, due to placental insufficiency, he lags behind in growth. There are a number of malformations and chromosomal diseases, due to which the fetus is stunted, but then the doctor will suspect this on an ultrasound scan and send it for additional examination.
A percentile is a statistic. The number of percentiles can change, as well as the number of parameters. It is important to understand that the fetus does not grow according to a textbook, but according to its genetic program, and the tasks of an obstetrician-gynecologist with an ultrasound doctor should be understood in dynamics: is it an individual feature of the baby of such intrauterine growth or, indeed, due to placental insufficiency, he lags behind in growth. There are a number of malformations and chromosomal diseases, due to which the fetus is stunted, but then the doctor will suspect this on an ultrasound scan and send it for additional examination.
So, an example of a table of indicators of intrauterine dimensions of the fetus. Let's take the example of 33 weeks pregnant. This line is highlighted in red. Percentiles indicate the relative position of an individual in the standardization sample. These are some average statistical indicators that help, first of all, doctors navigate between the norm and pathology. If your gestational age is 33 weeks, and all indicators of fetometry (sizes of different parts of the fetal body) fit into this line, highlighted in red, then there is no cause for alarm. "According to the textbook" is the 50th percentile (the most common indicator of the norm in the population). But the fetus can be larger or smaller. Remember how at school age you lined up in physical education classes, who is taller, who is lower, but all the good guys turned out to be. In percentiles, the same logic, someone is larger (then the doctor will say the phrase: the biparietal size corresponds to 90 percentile for 33 weeks gestation), someone smaller (then the doctor will say the phrase: the size of the femur corresponds to the 10 percentile for 33 weeks gestation). Both of these are normal, and there is no cause for alarm.
If your gestational age is 33 weeks, and all indicators of fetometry (sizes of different parts of the fetal body) fit into this line, highlighted in red, then there is no cause for alarm. "According to the textbook" is the 50th percentile (the most common indicator of the norm in the population). But the fetus can be larger or smaller. Remember how at school age you lined up in physical education classes, who is taller, who is lower, but all the good guys turned out to be. In percentiles, the same logic, someone is larger (then the doctor will say the phrase: the biparietal size corresponds to 90 percentile for 33 weeks gestation), someone smaller (then the doctor will say the phrase: the size of the femur corresponds to the 10 percentile for 33 weeks gestation). Both of these are normal, and there is no cause for alarm.
As in the previous article on fetal growth retardation, let's repeat the main fetometric indicators that guide us when assessing intrauterine growth of the fetus: biparietal size, head circumference, abdominal circumference, femur length.