When does 2nd trimester of pregnancy start
What To Expect, Development & Tests
What is the second trimester of pregnancy?
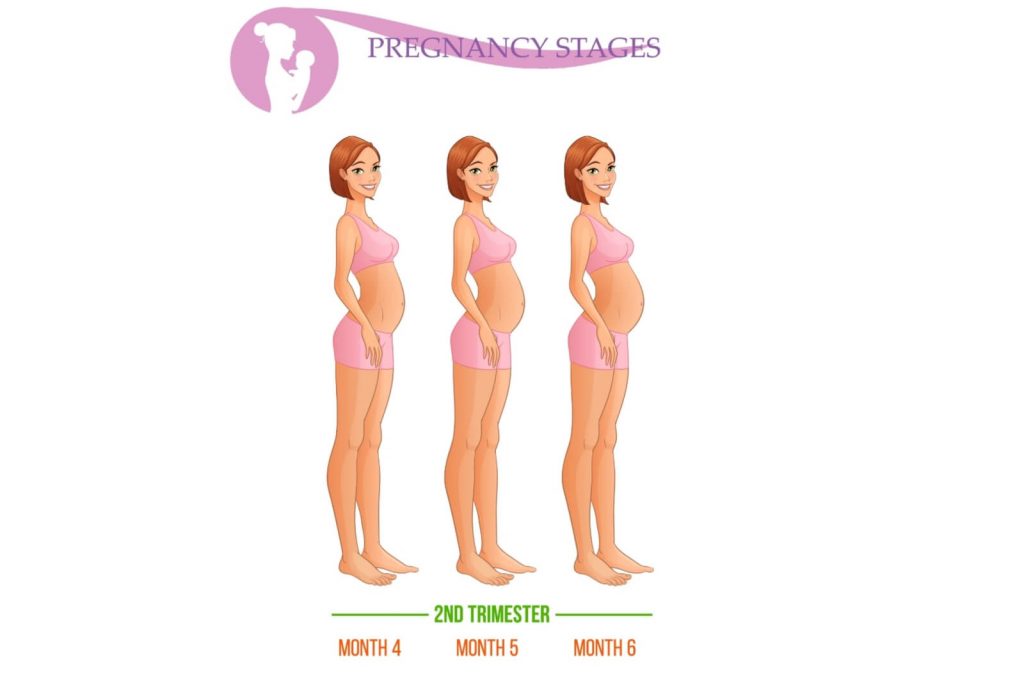
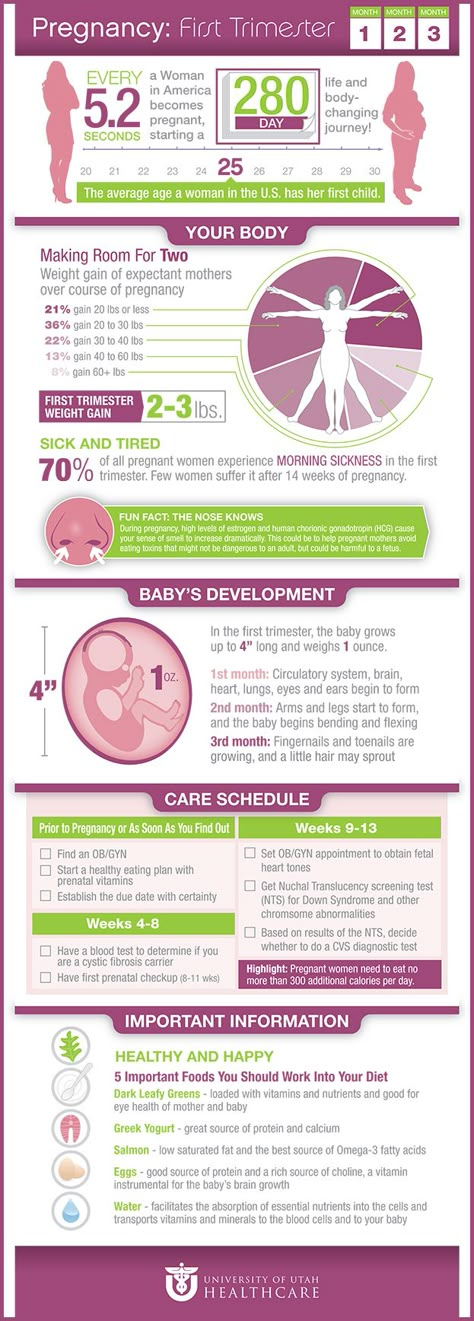
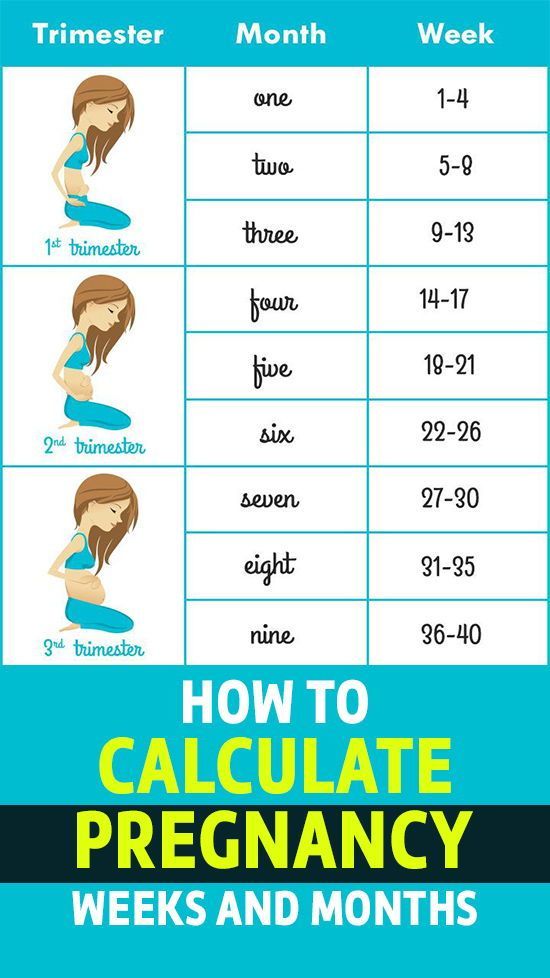
The typical pregnancy lasts about 40 weeks. It’s divided into three periods of time — the first, second and third trimester. Each trimester is roughly 14 weeks long. When you enter your second trimester, you are around 14 weeks pregnant. This middle trimester will last from week 14 to the end of week 27.
During your second trimester of pregnancy, you’ll start looking and feeling more pregnant. For many people, this is the best part of pregnancy because the morning sickness and fatigue of their first trimester fade into the past. Often, any anxiety that went with your first trimester also starts to diminish at this point. You’ll start to feel your fetus move by the end of this trimester, and you might begin to settle into your pregnancy and enjoy it more. Of course, it’s important to remember that pregnancy is different for everyone. Some people never experience negative symptoms like morning sickness in their first trimester. Others might continue to feel sick well into their second trimester of pregnancy.
How does my baby develop during the second trimester of pregnancy?
Your fetus will go through many changes during your second trimester of pregnancy. During this trimester, the fetus starts to look more like a child — with its facial features aligning, and its fingers and toes becoming well-defined. By month four, the fetus will actually have eyelids, eyebrows, eyelashes, nails and hair. The fetus will also be able to stretch, make faces and even suck on its thumb. You’ll soon be able to determine the sex of the fetus on an ultrasound — often around 20 weeks.
At this point, you might also start feeling the fetus move. The movement is often described as a flutter or similar to the feeling of having butterflies in your stomach. The fetus will be doing flips and movements throughout your second trimester. This first movement is called the quickening. If this isn’t your first pregnancy, you might feel the fetus move sooner.
In the last few weeks of the second trimester, the fetus can also hear you. If you talk to your growing belly, you might notice movement in response.
If your baby was born at the end of your second trimester (premature birth), they would be likely to survive with intensive care.
What happens to my body during the second trimester of pregnancy?
The fetus isn’t the only one growing and changing during your second trimester. You'll notice several changes in your own body during this time. Your uterus — the place where the fetus grows during pregnancy — continues to stretch. This organ will expand throughout your pregnancy as the fetus gets larger. After pregnancy, your uterus will return to its pre-pregnancy size (picture an upside-down pear).
However, your uterus isn’t the only thing growing during the second trimester either. You’ll start gaining weight and might start developing the tell-tale enlarged belly of a pregnant person. Don’t worry if this takes time to develop. Everyone is different, and no two bodies will look exactly the same during pregnancy.
Everyone is different, and no two bodies will look exactly the same during pregnancy.
You might also feel or develop a few new symptoms of pregnancy during your second trimester, including:
- An increased appetite.
- An achy body.
- Some swelling in your hands, feet and ankles.
- Some stretch marks.
If you experienced morning sickness during your first trimester, it’s likely fading away now. The uncomfortable symptoms of early pregnancy (nausea and extreme fatigue, for example) don’t typically continue into your second trimester. This is one reason why many people consider their second trimester of pregnancy to be the best part of pregnancy.
What tests will I have during the second trimester of pregnancy?
Throughout your pregnancy, your healthcare provider will order various tests to check on your health and the health of your developing fetus. During your second trimester, you’ll typically be screened for a few different things, including the Rh factor of your blood and the condition gestational diabetes. You'll also have an ultrasound during your second trimester. This ultrasound is probably best known for telling new parents the sex of the fetus, but it’s mainly used to look at their anatomy.
You'll also have an ultrasound during your second trimester. This ultrasound is probably best known for telling new parents the sex of the fetus, but it’s mainly used to look at their anatomy.
One thing your provider will test for during your second trimester is your Rh factor. Rh factor is an antigen protein found on most people’s red blood cells. If you don’t have the protein, then you are Rh- (negative). You’ll be given an injection of Rh immune globulin (called Rhogam®) during the 28th week of your pregnancy to prevent the development of antibodies that could be harmful to the fetus. You’ll also be given an injection of Rhogam® after delivery if your fetus has Rh+ (positive) blood.
If you are Rh-, you may also receive this injection if you:
- Are having an invasive procedure (such as amniocentesis).
- Had an abdominal trauma.
- Had any significant bleeding during pregnancy.
- Need to have the fetus turned in your uterus (due to breech presentation).

Your provider will also order a test called the oral glucose screening test. This is usually done at the end of your second trimester — often between weeks 24 and 28. The purpose of the glucose screening test is to see if you are developing gestational diabetes. During the test, you’ll be given a syrup-like drink. The healthcare provider administering this test will give you a set amount of time to drink the entire bottle, then you'll be asked to wait nearby for one hour. After the hour is over, you’ll have your blood drawn. Your healthcare provider will then go over your test results with you.
What do I need to prepare or plan for during the second trimester of pregnancy?
There are many things you can start thinking about during your second trimester of pregnancy to prepare for your new family member. Many of these things will center around conversations that you should start having at this point in your pregnancy. It’s good to discuss the type of birth you hope to have and learn about the different ways your child might be born.
A few ways your baby could be born can include:
- Vaginal birth (this could be medicated so that your pain is decreased, or unmedicated).
- Assisted birth (you might need tools like forceps or a vacuum to help with your delivery).
- Cesarean section (C-section).
You can learn more about these types of birth through your own research or in a birth class. This is the time for you to look into educational classes about birth, breastfeeding and parenting of your newborn. These classes can help prepare you for your new role as a parent. Ask your healthcare provider for more information on classes and groups you can join at this point in your pregnancy.
This might also be a good time to take a tour of the hospital where you’ll give birth. A hospital tour is a great way to get familiar with the place where your baby will be born. During the tour, you’ll learn where you should go when you first get to the hospital during labor and what will happen afterward. You’ll typically get to see hospital rooms and learn more about the hospital staff, as well.
You’ll typically get to see hospital rooms and learn more about the hospital staff, as well.
What should I be doing during the second trimester of pregnancy to stay healthy?
Throughout your second trimester, you should continue maintaining a healthy lifestyle. Try to exercise for about 20 minutes a day. Regular exercise is good for you and your developing fetus. Some of the safest types of exercise include walking and swimming; though, there are many other options you can try. Talk to your healthcare provider about the type of exercise you'd like to do beforehand just to be safe. You’ll want to avoid contact sports and activities where you could fall, as these could endanger your pregnancy.
It’s also a good idea to do kegel exercises throughout your entire pregnancy. These exercises will help strengthen your pelvic floor muscles.
Apart from exercise, you should continue eating a healthy diet, taking your prenatal vitamins and attending each of your appointments.
When should I call my doctor during the second trimester of pregnancy?
You’re the person who knows your body the best. If you ever feel like something is wrong, it’s completely OK to reach out to your healthcare provider. It’s also a good idea to call your healthcare provider right away if you have:
- Unusual or severe cramping or abdominal pain.
- Noticeable changes in how much the fetus moves (after 28 weeks of gestation). If you don’t count six to 10 movements in one hour or less, call your provider.
- Difficulty breathing or shortness of breath that seems to be getting worse over time.
You should also reach out to your provider right away if you start having any signs of premature labor. Talk with your provider if you have any of the following signs of premature labor:
- Regular tightening or pain in your lower abdomen or back that occurs more than four times in an hour.
- Any bleeding in your second or third trimester of pregnancy.

- Any fluid leakage. Vaginal discharge often increases as part of the hormonal changes in pregnancy.
- Pressure in your pelvis or vagina.
Second trimester | Pregnancy Birth and Baby
Second trimester | Pregnancy Birth and Baby beginning of content5-minute read
Listen
The second trimester of pregnancy is a time when many women will feel energised and well. You will become visibly pregnant, but you won’t be so heavy that getting around is difficult. This is also a time of rapid growth and development for your baby, and you may find yourself busy with health checks and planning for the birth.
What is the second trimester?
Trimesters are a helpful way to think about pregnancy because the changes that happen to you and your baby fall into 3 broad categories of early, middle and late pregnancy, as reflected in the first, second and third trimesters.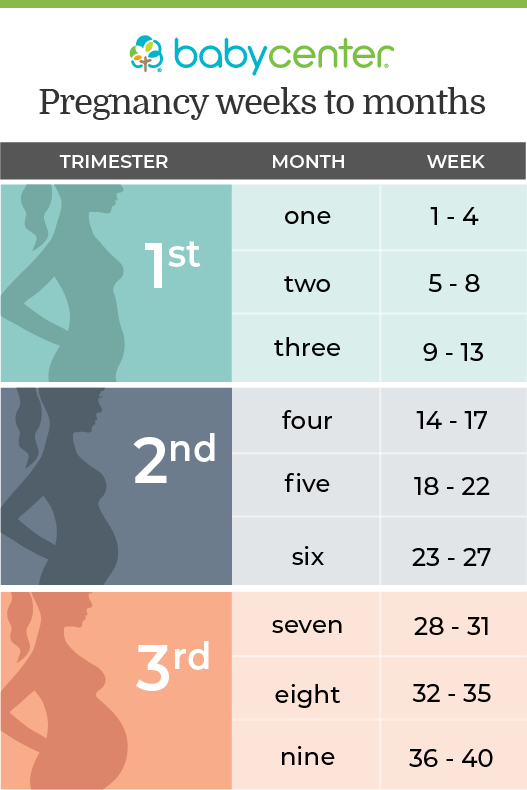
The second trimester represents the middle part of your pregnancy, from weeks 13 to 26. For many women, one of the best things about this trimester is that nausea might begin to settle.
What happens to your body?
Your body will undergo some major changes during the second trimester. Your uterus will grow, and you may feel some discomfort or aches as uterine ligaments stretch. You will start to feel your skin stretch around your belly and your breasts, which may cause mild itching. Some women get stretch marks in these areas, which tend to fade over time.
Although your baby weighs less than a kilo, your blood volume will increase to meet the demands of all the growth happening inside you, which will mean you will gain some additional weight.
Your emotions
Pregnancy can be a wonderful and exciting time, but it’s also important to expect to feel some occasional days of heightened anxiety or low mood.
Sometimes one or both parents experience difficult emotions during pregnancy, such as being worried about the birth or about coping as a parent.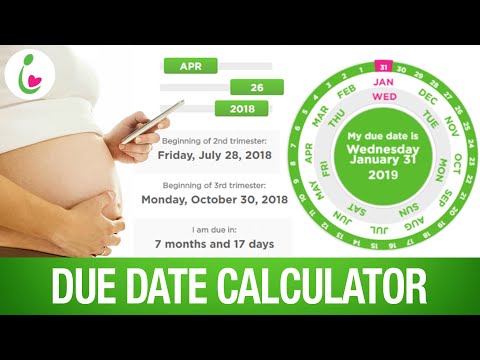
Feelings of anxiety are not uncommon, and some women will experience symptoms of a condition called anxiety disorder. Antenatal depression is a mood disorder that includes intense emotional changes beyond those you might expect during pregnancy.
If you are worried about feelings of anxiety, low mood or depression, you could:
- see your doctor, obstetrician, child health nurse or midwife
- phone Pregnancy, Birth and Baby on 1800 882 436
- call PANDA - Perinatal Anxiety & Depression Australia on 1300 726 306
What happens to the baby?
During the second trimester, your baby will grow from being around 7.5cm, and weighing 30 grams in week 13, to around 23cm and 820 grams at week 26.
Your baby will be able to move freely within the amniotic sac in your uterus. By about week 19 (or sooner if this isn’t your first pregnancy), you may feel this movement – as a faint tickling or fluttering. During these 3 months, your baby’s organs will continue to develop and the liver, pancreas and kidneys all start to function. This is also the time when babies might start to suck their thumb. By week 20 your baby can hear sounds, including the sound of your heartbeat, and they are learning to recognise your voice, although the ears are not yet fully formed.
This is also the time when babies might start to suck their thumb. By week 20 your baby can hear sounds, including the sound of your heartbeat, and they are learning to recognise your voice, although the ears are not yet fully formed.
What can you expect at your antenatal visits?
Regular antenatal visits are an important part of staying healthy and making sure your baby is healthy. How often you see your health professional will depend on your personal circumstances, but for many women, visits will be every 4 to 6 weeks.
At all visits during your second trimester, you will have your blood pressure checked, and your hands and feet will also be checked for swelling. You might be weighed, have blood taken for tests and have your urine checked.
Your doctor or midwife will check your abdomen to monitor your baby’s growth and will listen to your baby’s heartbeat. If you didn’t have an ultrasound in your first trimester, you may be offered one at around 18 to 20 weeks.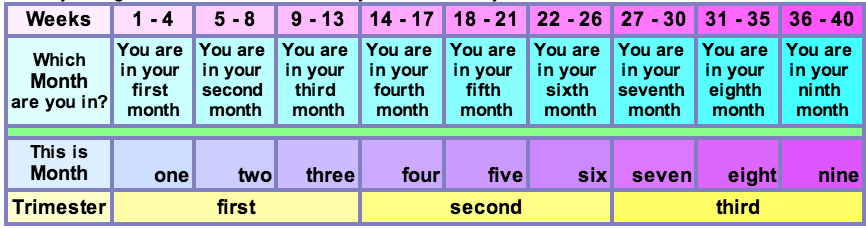
How to stay healthy
Eating well and staying active is as important as ever during pregnancy - it's good for your physical and emotional health, and good for your baby too. Light-to-moderate exercise in pregnancy is usually safe: consider walking, swimming, yoga and stationary cycling in your second trimester. High-impact exercise and activities where there is a risk of falling, getting hurt (especially around the stomach) or overheating are not recommended.
Your choice of food during your pregnancy is also important – but that doesn’t mean ‘eating for two’. What you eat during your pregnancy has been shown to affect how your baby grows as well as your baby’s health later in life.
Things to consider in the second trimester
Parental leave – discuss with your partner and then with your employer:
- How will you share the care of your baby with your partner (or other family members)?
- When do you plan to start your leave?
- When you intend to return to work?
- When is a good time to share your pregnancy news with your employer?
- Will your role at work change after your baby is born?
Antenatal classes:
- Ask your midwife or doctor about antenatal education available in your area.
- Consider going to classes together with your birthing partner – not only will you learn a lot about how to prepare for labour, you’ll meet people who will share their experience of becoming parents.
Your pregnancy journey
Follow your pregnancy week-by-week to find out how your baby is growing and what is happening to your body.
Sources:
NSW Health (Having a baby), Royal Women's Hospital (Pregnancy and birth), Raising Children Network (Pregnancy week-by-week), Women's and Children's Health Network (The first 3 months of pregnancy: the first trimester), Queensland Health (How much weight will I gain during pregnancy?), Healthy WA (Emotional health for parents during pregnancy and after the birth)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2021
Back To Top
Related pages
- Pregnancy week-by-week
- Third trimester
- First trimester
Need more information?
Second trimester of pregnancy: for men | Raising Children Network
Tiredness and morning sickness often ease up in pregnancy’s second trimester. Our guide explains how this can be a special time for men and their partners.
Read more on raisingchildren.net.au website
Pregnancy changes video: second trimester | Raising Children Network
In this video mums and dads describe physical and emotional changes in the second trimester of pregnancy. A midwife says tiredness and nausea might ease.
Read more on raisingchildren.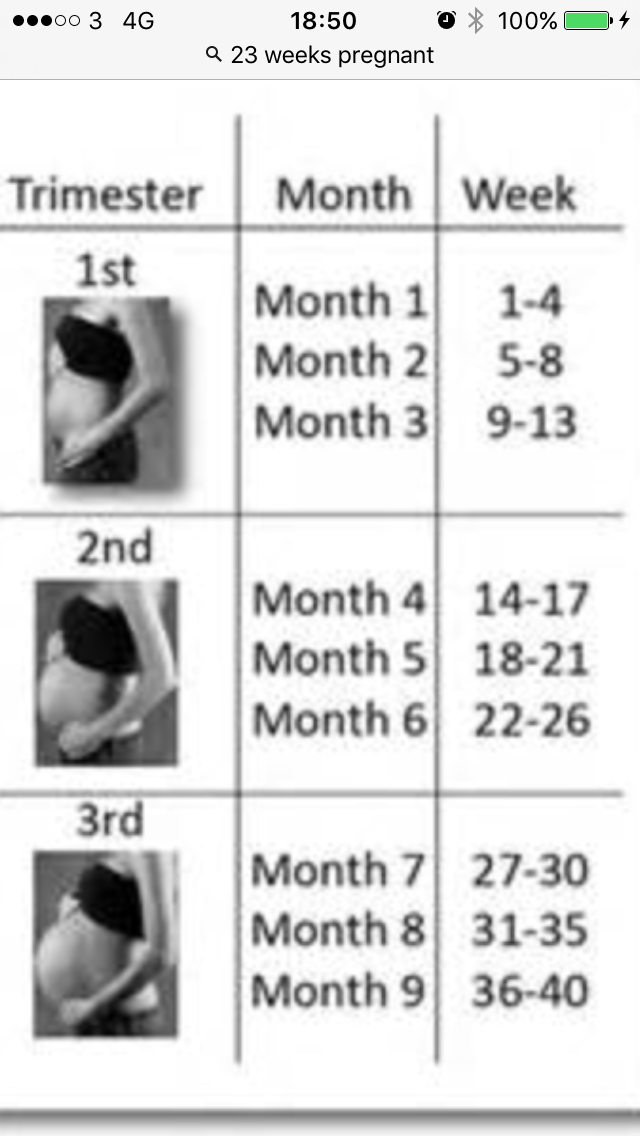 net.au website
net.au website
Exercise in second trimester: dads guide | Raising Children Network
How much exercise is safe for pregnant women in the second trimester? Light to moderate exercise is usually OK. This Dads Guide explains and has tips.
Read more on raisingchildren.net.au website
Pregnancy second trimester: men’s feelings | Raising Children Network
It’s pretty common for men to feel pregnancy is happening at a distance. Even in the second trimester, it might not feel real. Read more in our Dads Guide.
Read more on raisingchildren.net.au website
Pregnancy at week 13
At week 13 of pregnancy, you officially enter your second trimester and hopefully any morning sickness has eased off.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 25
As you are approaching the end of the second trimester, you might be starting to feel a bit uncomfortable as your baby continues to grow.
Read more on Pregnancy, Birth & Baby website
Late term abortion | Marie Stopes Australia
Having a late term abortion, also known as a second trimester abortion, is never easy. Given the often exceptional circumstances and more complex procedure required they require special care and support. We specialise in later term abortions in most states, in line with legal gestation limits.
Read more on MSI Australia website
Maternal screening - Pathology Tests Explained
Why and when to get tested for maternal screening
Read more on Pathology Tests Explained website
Pregnancy at week 16
At week 16, you might begin to feel your baby moving, while hormonal changes may be affecting your libido.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 14
By week 14, your baby’s organs have formed, their face is becoming more recognisable, and you may be feeling more energetic.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Second trimester of pregnancy: 4, 5, 6 months
Second trimester of pregnancy
The second trimester of pregnancy lasts from 12 to 27 weeks. During this period, you will continue to be monitored by a specialist doctor with visits once every 3 weeks, pass a number of necessary tests, in particular, a complete blood count, a biochemical blood test, blood for a coagulogram, a glucose tolerance test, a general urinalysis and bacteriological culture of urine for sterility 1-3 . At a period of 18-21 weeks, an ultrasound of the fetus will be performed with an assessment of its condition.
At a period of 18-21 weeks, an ultrasound of the fetus will be performed with an assessment of its condition.
Second trimester abdomen
The circumference of your abdomen increases markedly, by the end of the second trimester of pregnancy, the increase in the abdomen is more noticeable, and the bottom of the uterus is located at the level of the navel. Wear comfortable clothes, avoid tight belts, elastic bands around the abdomen 1-3 .
Second trimester of pregnancy and pain
In case of sudden pains of a different nature (cramping sharp or monotonous pulling pains) of the abdomen, you should immediately consult a doctor. Pain in the abdomen may be associated with the threat of abortion and other complications. If the 2nd trimester is coming to an end and you have pain in the lumbar region, this may be due to compression of the ureters by the enlarged uterus. It is necessary to pass a urine test and do an ultrasound of the kidneys 1-3 .
Constipation can also cause pain in the abdomen, along the final section of the large intestine (sigmoid colon). Pain during bowel movements, that is, during bowel movements, may be associated with an increase in hemorrhoids, the appearance of anal fissures. To ensure regular bowel movements, follow the drinking regimen and diet 1-3 .
The 2nd trimester of pregnancy may be accompanied by headaches (cephalgia). One of the causes of cephalalgia during pregnancy can be an increase in blood pressure. When a headache occurs, control the level of blood pressure (you need to measure at rest, on both hands at least one measurement on each). Remember that headaches and high blood pressure require urgent medical attention 1-3 .
Fourth month of pregnancy and fetal development
1-3- All your baby's organs are already formed, his height is about 10 cm, and his weight is about 70 grams, he makes active movements in the joints.

- By the end of 4 months, the fetus actively increases in size, its height is about 13 cm, weight is about 140 grams.
- The development of teeth, sweat, salivary glands occurs, the liver begins to produce bile, and the pancreas - insulin.
- The baby begins to move his eyes, blink, and hear sounds well, because the bones of the inner ear are already formed.
- By the end of the fourth month, the woman begins to feel the movements of her baby.
- The liver and spleen form blood cells.
Fifth month of pregnancy and fetal development
1-3- The fetus is actively moving, on ultrasound you can see how the baby sucks his fingers. Weight about 240 grams, height about 15 cm.
- At 5 months, the fetal intestine is formed and individual nutrients can be absorbed, meconium accumulates.
- The immune system is fully formed and blood cells begin to produce bone marrow. The 5th month is coming to an end, and the baby's weight is about 400 grams.

- Your belly at 5 months of pregnancy no longer allows you to wear ordinary trousers and jeans, but dresses from an ordinary wardrobe can still fit, the uterus is just below the level of the navel.
- The breast at the 5th month of pregnancy also increases, usually by 1 size, the areolas of the nipples become more pigmented.
Sixth month of pregnancy and fetal development
1-3- The most intensive growth of the fetus begins, which will continue for only 3 trimesters.
- At the beginning of this period, the weight of the fetus is about 500-600 grams, and by the end of 6 months, the weight of the baby already reaches 900 grams.
- The 6th month of pregnancy is characterized by the formation of the surfactant system and the maturation of your baby's lungs.
- The breast at 6 months of pregnancy continues to increase due to the growth of glandular tissue, the size and pigmentation of the areola increases, the mammary glands prepare for lactation under the influence of estrogens.

2nd trimester of pregnancy:
macro- and micronutrient supplement
Pregnancy and iodine:
- To prevent iodine deficiency, all pregnant and lactating women are advised to take 200 micrograms of potassium iodide daily.
- Optimal absorption of iodides is observed in the morning hours. 4-8
Talk to your doctor about taking potassium iodide.
Pregnancy and calcium:
- The need for calcium increases to 1200-1500 mg per day, calcium salts are most often found in the form of carbonate and citrate, they have good bioavailability.
- Calcium is well absorbed in the evening. 9-11
Discuss the need to take calcium salts with your doctor.
Pregnancy and iron:
- Iron preparations are not recommended for all women, but iron deficiency anemia often accompanies the 2nd trimester of pregnancy 4 .
- If the level of ferritin (an accessible and reliable indicator of iron sufficiency) decreases, iron supplements should be taken at an average dose of 30-60 mg per day 4 .

The decision to prescribe iron supplements is made by your doctor or hematologist.
Pregnancy and vitamin D:
- The requirement for vitamin D throughout pregnancy and lactation is 2000 IU per day 9-11 .
Ask your doctor if you need to take vitamin D.
Second trimester pregnancy and complications
When the above symptoms appear, either alone or in combination, i.e. several symptoms at once, you need to urgently consult a doctor, since the lack of specialized medical care may be associated with a risk to your life and the life of the child.
2nd trimester and gestational diabetes mellitus
12-13 :- The list of mandatory examinations now includes a standard glucose tolerance test. Based on the results of this test, the state of carbohydrate metabolism is judged.
- In the presence of deviations from the norm, you will first of all be advised to follow a diet with a sharp restriction of fast carbohydrates and physical activity in accordance with the general state of health and the characteristics of the course of pregnancy.

- It will be necessary to consult an endocrinologist, nutritionist, physiotherapist.
2nd trimester and preeclampsia
14 :- An increase in blood pressure (may be asymptomatic!), the appearance of protein in the urine and edema are manifestations of preeclampsia.
- It is important to have your blood pressure checked regularly, have a urinalysis, and monitor weight gain.
2nd trimester and pyelonephritis
1-3 :- With an increase in the duration of pregnancy, the risk of developing pyelonephritis increases, this is due to a violation of the outflow of urine due to compression of the ureters by the growing uterus.
- Sitting and supine position contribute to urinary obstruction.
- Motor activity, knee-elbow position make urine outflow optimal.
- 1. National guidance. Gynecology. 2nd edition, revised and enlarged. M., 2017.
 446 p.
446 p. - 2. Guidelines for outpatient care in obstetrics and gynecology. Edited by V.N. Serov, G.T. Sukhikh, V.N. Prilepskaya, V.E. Radzinsky. 3rd edition, revised and expanded. M., 2017. S. 545-550.
- 3. Obstetrics and gynecology. Clinical guidelines. — 3rd ed., rev. and additional / G.M. Savelyeva, V.N. Serov, G.T. Dry. — M.: GEOTARMEDIA. 2013. - 880 p.
- 4. WHO antenatal care guidelines for a positive pregnancy experience. 2017.196 s. ISBN 978-92-4-454991-9
- 5. Dedov I.I., Gerasimov G.A., Sviridenko N.Yu. Iodine deficiency diseases in the Russian Federation (epidemiology, diagnosis, prevention). Toolkit. — M.; 1999.
- 6. Iodine deficiency: current state of the problem. N.M. Platonov. Clinical and experimental thyroidology. 2015. Volume 11, No. 1. S. 12-21.
- 7. Melnichenko G.A., Troshina E.A., Platonova N.M. Iodine deficiency diseases of the thyroid gland in the Russian Federation: the current state of the problem. Analytical review of publications and official state statistics (Rosstat).
 Consilium Medicum. 2019; 21(4):14–20. DOI: 10.26442/20751753.2019.4.19033
Consilium Medicum. 2019; 21(4):14–20. DOI: 10.26442/20751753.2019.4.19033 - 8. Clinical guidelines: diagnosis and treatment of (multiple) nodular goiter in adults. 2016. 9 p.
- 9. National program for optimizing the feeding of children in the first year of life in the Russian Federation (4th edition, revised and supplemented) / Union of Pediatricians of Russia [et al.]. — M.: Pediatr, 2019. — 206 p.
- 10. National program Vitamin D deficiency in children and adolescents of the Russian Federation: modern approaches to correction / Union of Pediatricians of Russia [et al.]. — M.: Pediatr, 2018. — 96 s.
- 11. Pigarova E.A., Rozhinskaya L.Ya, Belaya Zh.E., et al. Clinical guidelines of the Russian Association of Endocrinologists for the diagnosis, treatment and prevention of vitamin D deficiency in adults // Problems of Endocrinology. - 2016. - T.62. — No. 4. — P. 60-84.
- 12. Russian national consensus "Gestational diabetes mellitus: diagnosis, treatment, postpartum care" / Dedov I.
 I., Krasnopolsky V.I., Sukhikh G.T. On behalf of the working group//Diabetes mellitus. —2012. -No4. —S.4-10.
I., Krasnopolsky V.I., Sukhikh G.T. On behalf of the working group//Diabetes mellitus. —2012. -No4. —S.4-10. - 13. Clinical guidelines. Algorithms of specialized medical care for patients with diabetes mellitus. 9th edition (updated). 2019. 216 p.
- 14. Adamyan L.V., Artymuk N.V., Bashmakova N.V., Belokrinitskaya T.E., Belomestnov S.R., Bratishchev I.V., Vuchenovich Yu.D., Krasnopolsky V.I. , Kulikov A.V., Levit A.L., Nikitina N.A., Petrukhin V.A., Pyregov A.V., Serov V.N., Sidorova I.S., Filippov O.S., Khodzhaeva Z.S., Kholin A.M., Sheshko E.L., Shifman E.M., Shmakov R.G. Hypertensive disorders during pregnancy, childbirth and the postpartum period. Preeclampsia. Eclampsia. Clinical guidelines (treatment protocol). M.: Ministry of Health of Russia; 2016.
Pregnancy by trimesters: 2nd and 3rd trimester
The first trimester is behind us with its anxiety, morning sickness, constant sleepiness and other problems. If you count by weeks, the II trimester starts from the 13th week and is considered the easiest and calmest.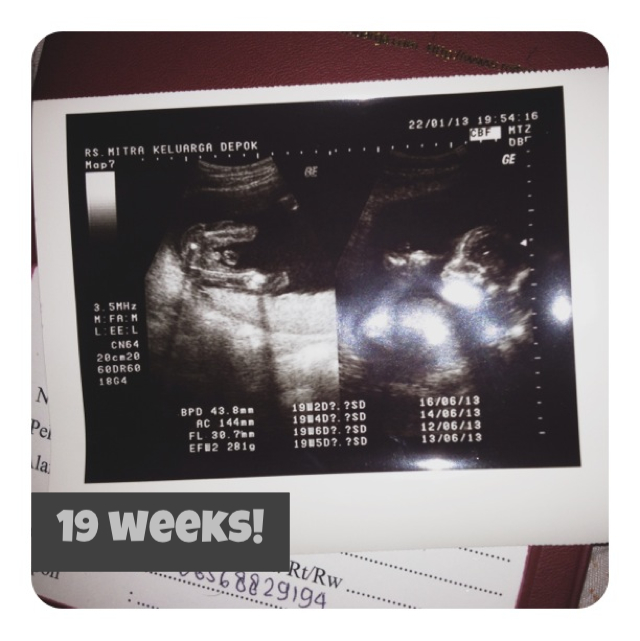 The future mother, both psychologically and physically, has already adapted to her status, but it seems that motherhood is not yet close. However, there is also a lot of research to be done.
The future mother, both psychologically and physically, has already adapted to her status, but it seems that motherhood is not yet close. However, there is also a lot of research to be done.
A full range of laboratory tests is available at DILA: Program 185 "Examination of a pregnant woman at 22-24 weeks of pregnancy", prenatal screening of the II trimester, prenatal non-invasive screening (NIPT, basic), as well as a number of other screening programs and mono-studies. All of them are aimed at determining the general state of health, the work of the main systems and organs of a pregnant woman in the second and third trimesters of pregnancy. Regular monitoring will allow early detection of various complications that may arise and provide the necessary treatment. Thus, the chances of a normal pregnancy and the birth of a healthy child are increased.
Second trimester examinations
The second (II) trimester of pregnancy includes the period between 13 and 26 weeks. It is during this time period, closer to the 16th week, that all organs and systems of the fetus are already finally laid down, but all the organs and systems of the fetus continue to develop, the placenta is formed, and after the 23rd week the fetus is already considered fully viable and formed. Clinical laboratory diagnostics of a number of biochemical indicators of this period reflects not only the state of health of a pregnant woman and the features of the work of the main organs and systems, but also makes it possible to detect diseases and possible complications.
It is during this time period, closer to the 16th week, that all organs and systems of the fetus are already finally laid down, but all the organs and systems of the fetus continue to develop, the placenta is formed, and after the 23rd week the fetus is already considered fully viable and formed. Clinical laboratory diagnostics of a number of biochemical indicators of this period reflects not only the state of health of a pregnant woman and the features of the work of the main organs and systems, but also makes it possible to detect diseases and possible complications.
So, Program 185 "Examination of a pregnant woman at 22-24 weeks of pregnancy" includes the following studies:
- Complete blood count. It is aimed at a basic assessment of the general state of health: the hematopoietic system, the presence of inflammatory, infectious (including viral), oncological diseases, as well as allergic processes in the body.
- Urinalysis. Allows you to assess the state of the urinary tract and some extrarenal diseases, to identify the presence of preeclampsia.
- Glucose tolerance test, which makes it possible to evaluate carbohydrate metabolism disorders (including latent forms).
- HIV 1/1o/2 to detect HIV infection.
Complete blood count with leukocyte count and ESR (erythrocyte sedimentation rate) and urinalysis should preferably be performed once a month.
Clinical blood test makes it possible to study the qualitative and quantitative composition of blood by key indicators: erythrocytes and their specific indicators, leukocytes and their varieties in absolute and percentage terms, platelets. The detection of deviations in these markers may indicate the presence of pathological processes in the body of a pregnant woman. A decrease in the level of erythrocytes and hemoglobin in erythrocytes is a sign of anemia in pregnant women. This can lead to placental insufficiency - the main reason for miscarriage, the birth of small children and fetal death.
Changes in the leukocyte formula may indicate a wide range of changes in the body of pregnant women in the 2nd trimester.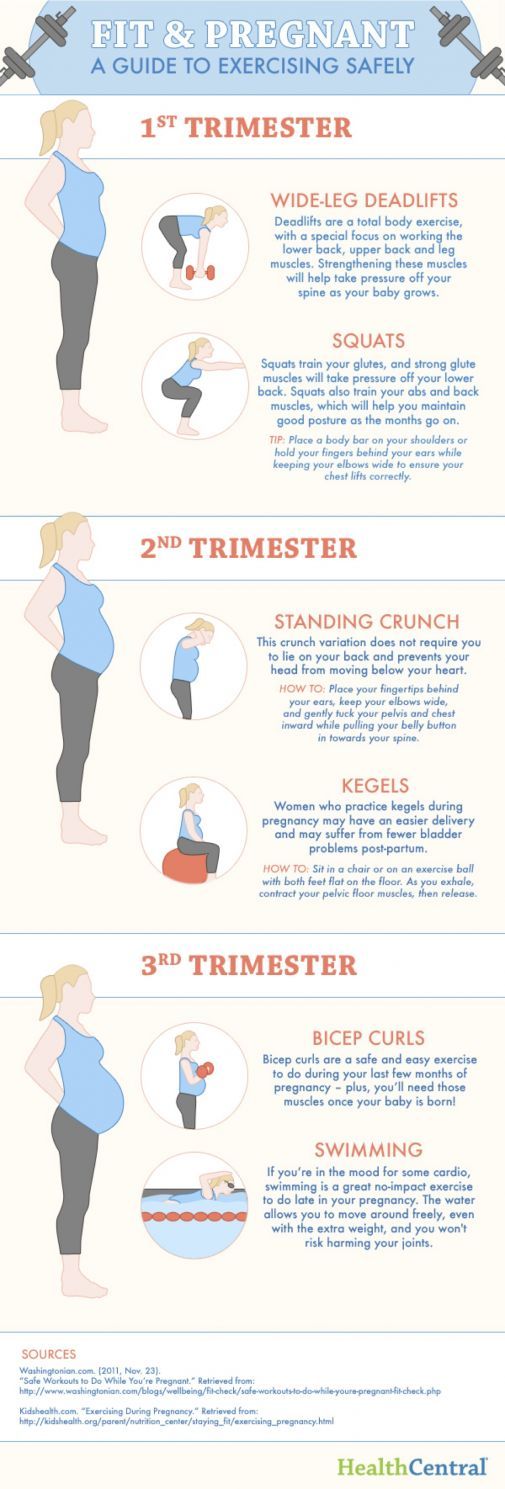 They can act as laboratory signs of previously undiagnosed inflammatory and infectious processes, which requires a more extensive additional examination - both instrumental and laboratory. The content of platelets during physiological pregnancy may slightly decrease, but significant changes in this indicator, including developing thrombocytopenia, require special observation, since they may be indirect signs of a violation of the blood coagulation system, as well as DIC (disseminated intravascular coagulation syndrome), which are severe pregnancy complications.
They can act as laboratory signs of previously undiagnosed inflammatory and infectious processes, which requires a more extensive additional examination - both instrumental and laboratory. The content of platelets during physiological pregnancy may slightly decrease, but significant changes in this indicator, including developing thrombocytopenia, require special observation, since they may be indirect signs of a violation of the blood coagulation system, as well as DIC (disseminated intravascular coagulation syndrome), which are severe pregnancy complications.
A change in the erythrocyte sedimentation rate (ESR) can be observed in acute and chronic inflammatory pathologies, infectious diseases, as well as oncological and autoimmune processes. At the same time, in pregnant women, the erythrocyte sedimentation rate slightly increases in the norm.
General analysis of urine allows you to evaluate the general properties of urine, its physico-chemical properties, the presence of metabolic products, to detect the quantitative and qualitative content of certain organic compounds. This study reflects the functional state of the kidneys, urinary tract, allows you to evaluate the overall metabolic processes, suggest the presence of infectious and inflammatory processes. The detection of glucose and ketone bodies in the urine may indicate the development of impaired carbohydrate tolerance, diabetes mellitus, "pregnancy diabetes". If protein is found in the urine, this may be evidence of developing kidney pathology in pregnant women, as well as a sign of the development of a severe complication during pregnancy - preeclampsia for more than 20 weeks.
This study reflects the functional state of the kidneys, urinary tract, allows you to evaluate the overall metabolic processes, suggest the presence of infectious and inflammatory processes. The detection of glucose and ketone bodies in the urine may indicate the development of impaired carbohydrate tolerance, diabetes mellitus, "pregnancy diabetes". If protein is found in the urine, this may be evidence of developing kidney pathology in pregnant women, as well as a sign of the development of a severe complication during pregnancy - preeclampsia for more than 20 weeks.
The glucose tolerance test detects gestational diabetes (“diabetes in pregnancy”). If this deviation is detected, a woman needs to control her sugar levels throughout pregnancy and after childbirth. Early detection of gestational diabetes is very important to prevent a number of undesirable consequences, including the birth of a large fetus and the risk of prenatal complications.
HIV test . To reduce the risk of infection of the fetus, it is very important to detect the human immunodeficiency virus in a pregnant woman in a timely manner. The detection of HIV infection is an indication for the prevention of mother-to-child transmission of HIV, and not for termination of pregnancy. Without preventive measures, the risks of transmission of HIV infection from mother to fetus are 20-40%, while the use of special preventive measures reduces the likelihood of transmission of infection to 1-2%. Most cases of infection occur when the fetus passes through the natural birth canal. In addition, there is a high risk of infection during breastfeeding.
To reduce the risk of infection of the fetus, it is very important to detect the human immunodeficiency virus in a pregnant woman in a timely manner. The detection of HIV infection is an indication for the prevention of mother-to-child transmission of HIV, and not for termination of pregnancy. Without preventive measures, the risks of transmission of HIV infection from mother to fetus are 20-40%, while the use of special preventive measures reduces the likelihood of transmission of infection to 1-2%. Most cases of infection occur when the fetus passes through the natural birth canal. In addition, there is a high risk of infection during breastfeeding.
We have only described the possibilities of Program 185 "Examination of a pregnant woman at 22-24 weeks of pregnancy", but there are a number of other important studies.
2nd trimester prenatal screening - "triple test", including the determination of the total unit of beta-hCG, AFP and unconjugated (free) estriol.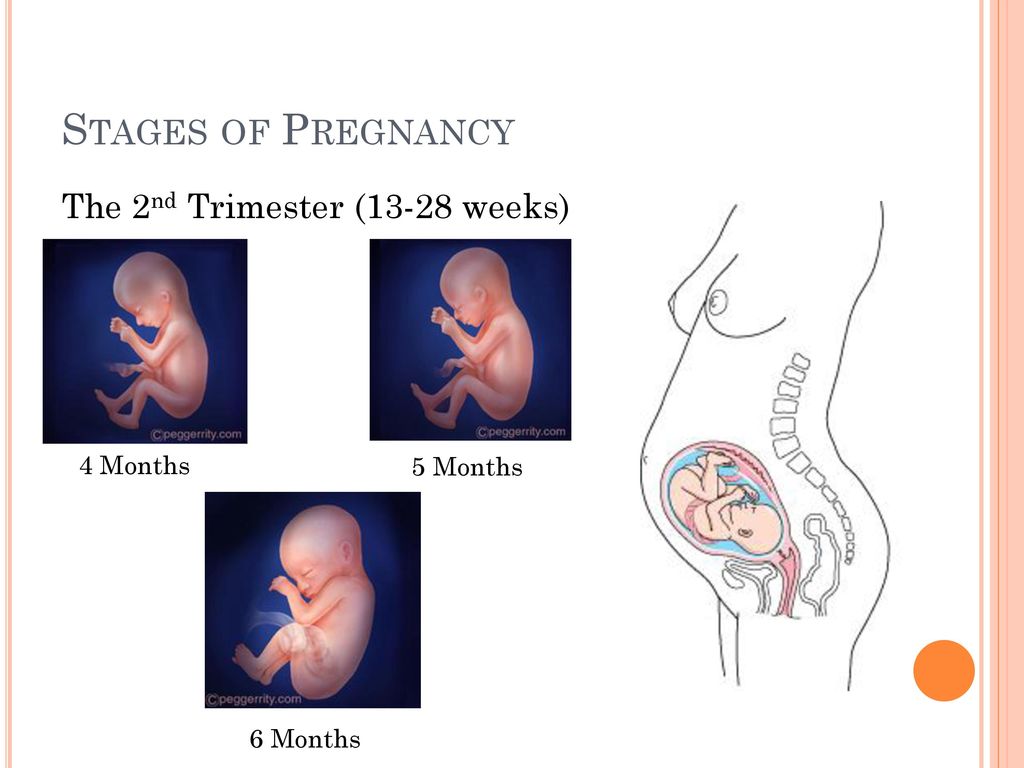 It is carried out for the purpose of biochemical screening of a pregnant woman to assess the risks of certain fetal chromosomal abnormalities:
It is carried out for the purpose of biochemical screening of a pregnant woman to assess the risks of certain fetal chromosomal abnormalities:
- Down syndrome. Violation is accompanied by characteristic features of appearance, mental retardation, defects of internal organs, short stature.
- Edwards syndrome. Most children with this syndrome die before the age of 3 months, only 5-10% survive to a year. The survivors are profoundly mentally retarded.
- Patau Syndrome. Accompanied by severe congenital malformations.
Also, prenatal screening of the second trimester makes it possible to assess the risk of malformations of the neural tube of the fetus.
The test is performed between 14 and 21 weeks, optimally between 16 and 18 weeks of pregnancy. Down, Edwards and Patau syndromes are the most common chromosomal disorders. The ability to detect these disorders in the early stages allows you to timely assess the genetic health of the fetus.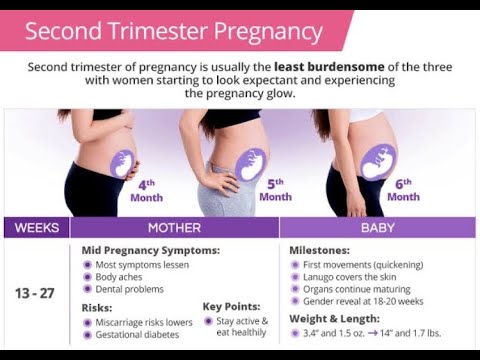
An alternative to biochemical prenatal screening is the NIPT test. It is more accurate than biochemical, and neither the course of pregnancy, nor the drugs taken, nor the woman's somatic diseases affect its results. The difference from biochemical screening is that NIPT is a direct method that allows you to examine the DNA of the fetus, while biochemistry is an indirect method. Biochemical screening has an accuracy of 70-80%, while NIPT has an accuracy of more than 99.9%.
Another important laboratory marker in the 2nd trimester is thyroid-stimulating hormone (TSH). This hormone is produced by the pituitary gland and is responsible for regulating the synthesis of the thyroid hormones thyroxine and triiodothyronine according to the “feedback system”, which allows maintaining a stable concentration of these hormones in the blood. Despite the fact that the thyroid hormone systems of a pregnant woman and the fetus do not depend on each other, her health and, accordingly, the course of the entire pregnancy depend on the normal functioning of the thyroid system of a woman.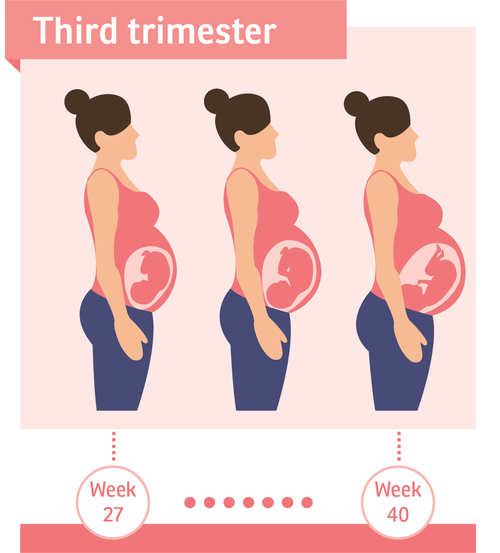 During pregnancy, TSH blood levels often remain stable. TSH is important for the normal development of the fetus, in particular for the normal formation of the central nervous system. In iodine deficiency conditions, the development of compensatory hyperplasia of the thyroid gland of the fetus is possible.
During pregnancy, TSH blood levels often remain stable. TSH is important for the normal development of the fetus, in particular for the normal formation of the central nervous system. In iodine deficiency conditions, the development of compensatory hyperplasia of the thyroid gland of the fetus is possible.
In the second and third trimesters of pregnancy, it is important to assess the risk of one of the most serious pregnancy complications, preeclampsia. Placental growth factor (PLGF), a marker of preeclampsia, has angiogenic properties and is essential for the normal development of the placental vascular system. Normally, the concentration of PlGF gradually increases up to 30 weeks of pregnancy. In the case of preeclampsia, there is a decrease in PLGF. Timely detection of increased risk allows you to predict the optimal tactics of pregnancy and childbirth.
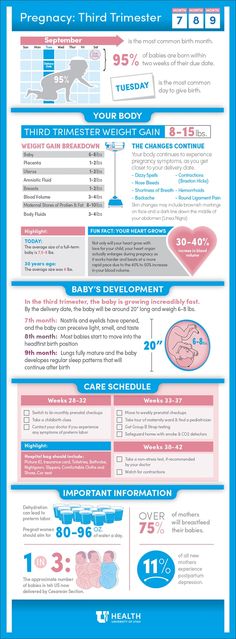
What tests should be done in the third trimester
The third trimester of pregnancy includes the period between 27 and 40 weeks.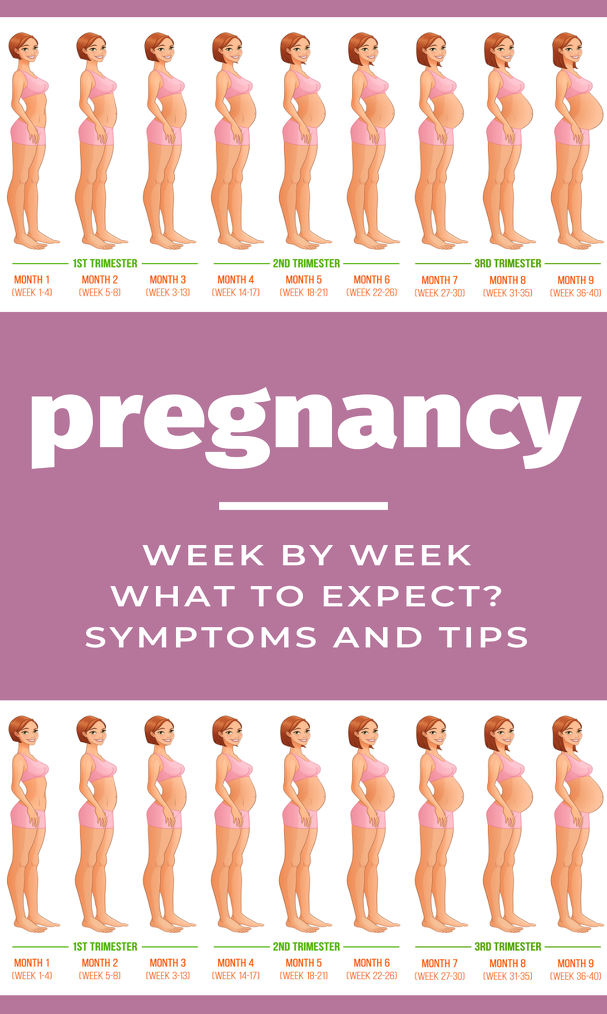 This period is characterized by the active growth of the fetus, the improvement of organ systems, in particular the respiratory system, the development of the sense organs, and the maturation of the nervous system. Clinical laboratory diagnostics of the III trimester is aimed at assessing the functioning of the main organs and systems, in particular the liver, kidneys, blood coagulation system, endocrine system of a pregnant woman, as well as infection control during pregnancy.
This period is characterized by the active growth of the fetus, the improvement of organ systems, in particular the respiratory system, the development of the sense organs, and the maturation of the nervous system. Clinical laboratory diagnostics of the III trimester is aimed at assessing the functioning of the main organs and systems, in particular the liver, kidneys, blood coagulation system, endocrine system of a pregnant woman, as well as infection control during pregnancy.
To check the state of health in the 3rd trimester, complex examinations are available in DILA Program 186 “Examination of a pregnant woman at 28-29 weeks of gestation” and Program 187 “Examination of a pregnant woman at 32-35 weeks of gestation”, as well as individual programs.
Risk of bleeding . In the third trimester of pregnancy, it is important to monitor the state of the blood coagulation and fibrinolysis system. The prothrombin time test is used to evaluate the extrinsic coagulation pathway.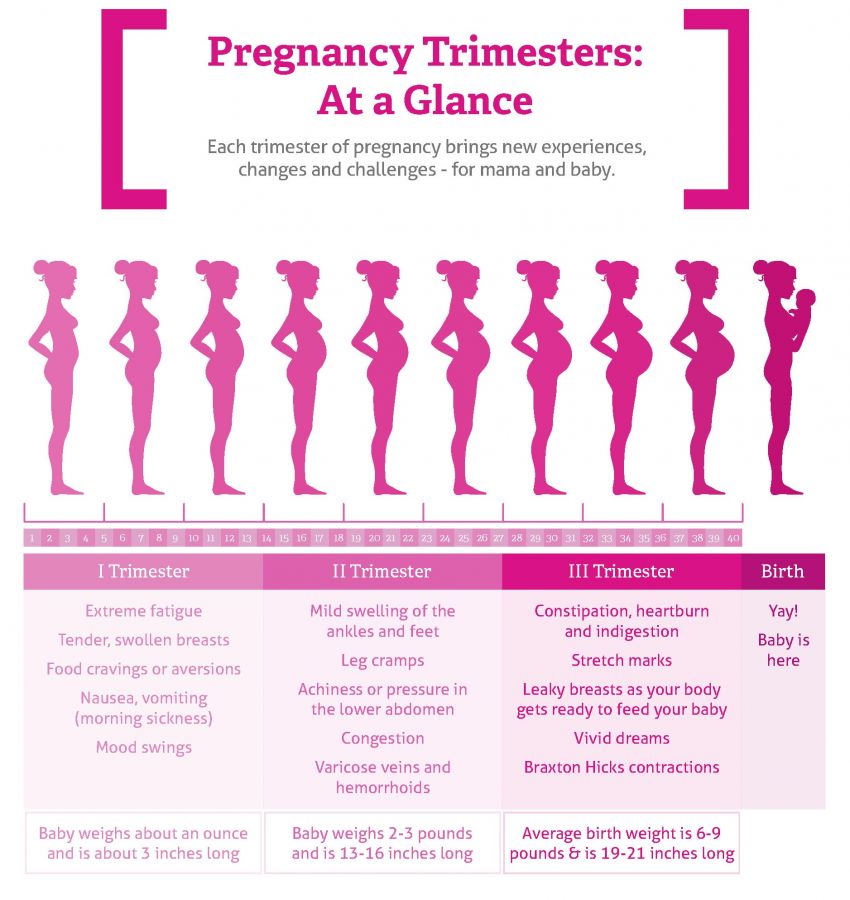 The test results are Quick prothrombin time and international normalized ratio. These indicators make it possible to assess the state of the liver, the main pathways of the blood coagulation system and the functional state of its basic components. The determination of these markers has a high diagnostic value for predicting thrombosis during pregnancy, diagnosing DIC, a dangerous complication accompanied by massive blood loss.
The test results are Quick prothrombin time and international normalized ratio. These indicators make it possible to assess the state of the liver, the main pathways of the blood coagulation system and the functional state of its basic components. The determination of these markers has a high diagnostic value for predicting thrombosis during pregnancy, diagnosing DIC, a dangerous complication accompanied by massive blood loss.
Normally, the levels of prothrombin and fibrinogen in the third trimester of pregnancy slightly increase, but a significant increase in these indicators requires close monitoring and the appointment of the necessary treatment. The concentration of D-dimer also increases during the physiological course of pregnancy, especially at 35-40 weeks, however, a sharp increase in the concentration of this protein may indicate a large number of blood clots, which is often associated with venous thromboembolism or DIC.
Infections . In the third trimester of pregnancy, it is also recommended to re-examine for:
- hepatitis B;
- hepatitis C;
- HIV infection;
- syphilis - antibodies to Treponema pallidum.

Because the incubation period for some infectious diseases varies greatly, negative test results taken early in pregnancy may change by the 3rd trimester or remain negative as well. This is necessary to prevent infection of the fetus during childbirth, prescribe the necessary treatment or a planned caesarean section.
Screening for group B streptococcus is now a mandatory test, essential at 36 +0 -37+ 6 weeks of pregnancy.
There is a group of infections that are very dangerous for pregnant women - these are TORCH infections. Their peculiarity lies in the fact that during the primary infection (if the woman has not yet been ill with them) during pregnancy, they can adversely affect all systems and organs of the fetus, especially its central nervous system. Infection with TORCH-group infections increases the likelihood of miscarriage, stillbirth and congenital malformations of the baby, up to disability. Program 134 "Extended screening for TORCH infections" from DILA allows you to assess the immune status (the presence of immune memory) to pathogens that are part of the TORCH complex group. Screening will help to adequately assess the risks of developing intrauterine infections, receive recommendations regarding subsequent pregnancy management and lifestyle changes to reduce the likelihood of primary infection during this critical period.
Screening will help to adequately assess the risks of developing intrauterine infections, receive recommendations regarding subsequent pregnancy management and lifestyle changes to reduce the likelihood of primary infection during this critical period.
Biochemical indicators (alanine aminotransferase, aspartate aminotransferase total bilirubin and direct bilirubin fraction, total protein in serum), which are part of Program 151 "Blood Biochemistry", allow assessing the functional state of the liver. A significant increase in the content of transaminases in the blood may indicate the presence of liver damage, hepatitis, the development of preeclampsia. A decrease in the level of total protein in the blood serum, along with the loss of protein in the urine and with an increase in blood pressure, can also be a sign of developing preeclampsia. To exclude gestational diabetes and the development of complications, in particular diabetic nephropathy, it is important to determine the level of glucose in the blood plasma.