When do you miscarry a blighted ovum
Blighted ovum | Pregnancy Birth and Baby
Blighted ovum | Pregnancy Birth and Baby beginning of content4-minute read
Listen
Key facts
- A blighted ovum is a type of miscarriage that can happen early in a pregnancy.
- A blighted ovum is when a sac and placenta grow, but a baby does not.
- A miscarriage can be extremely upsetting, and you may need support and time to grieve.
- Having a blighted ovum in one pregnancy does not change your chance of having a successful pregnancy in the future.
What is a blighted ovum?
A blighted ovum is a type of miscarriage that can happen early in a pregnancy. It is also called an 'anembryonic pregnancy' as there is no embryo (developing baby). In this type of miscarriage, a sac and placenta grow, but there is no baby. Because a blighted ovum still makes pregnancy hormones, it may still show up as a positive pregnancy test.
A blighted ovum will eventually cause a miscarriage, usually at 7 to 12 weeks of pregnancy. Your body realises that the pregnancy is not developing properly and starts to shed blood and tissue from the uterus. You may notice pain in your lower abdomen, or bleeding from your vagina.
How common is miscarriage?
Miscarriage is very common, and up to 1 in 5 people who know that they are pregnant will miscarry before 20 weeks of gestation. The actual rate of miscarriage is even higher, as a very early miscarriage may happen before you even realise that you’re pregnant.
What causes a blighted ovum?
When the egg is fertilised, cells that make the pregnancy sac and placenta start multiplying. But occasionally, the cells that are supposed to develop into a baby don’t multiply.
The cause isn’t known. It isn’t caused by anything you have done.
It isn’t caused by anything you have done.
How and when is blighted ovum diagnosed?
Sometimes, it is picked up during a routine ultrasound. This can be particularly difficult if you’ve gone for an ultrasound expecting good news.
At other times, there may have been bleeding at the start of the pregnancy and an ultrasound is used to investigate the cause.
How is blighted ovum treated?
Your doctor will discuss the options with you. You might choose to allow a natural miscarriage to happen. Once this starts, it can take days or weeks for the bleeding to finish. If the bleeding is getting heavier, if you are in pain or you feel unwell, see your doctor.
You could also have a termination by taking medicines or by having a type of surgery known as D & C.
Does it affect my chances of having a baby?
No. Having a blighted ovum in one pregnancy does not alter your chance of having a successful pregnancy in the future.
If you have had one miscarriage, your next pregnancy is likely to be normal. If you have had 3 miscarriages in a row, you should see your doctor to rule out any problems.
If you have had 3 miscarriages in a row, you should see your doctor to rule out any problems.
Where can I go for support and information?
Speak with your doctor if you are concerned that you may have a blighted ovum.
A miscarriage can be extremely upsetting. If you’ve experienced a miscarriage you may need support and time to grieve. There is no right way to feel after a miscarriage. Different people react to a miscarriage with different emotions, including anger, guilt or relief.
Pregnancy, Birth and Baby helpline can offer emotional support and trusted advice to anyone who is dealing with pregnancy loss. Call Pregnancy, Birth and Baby on 1800 882 436 anytime of the day or night.
Sources:
Raising Children (Miscarriage : what it is and how to cope), Pink Elephants Network (What is miscarriage?), Red Nose (Reasons for miscarriage)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: June 2022
Back To Top
Related pages
- Fathers and miscarriage
- Emotional support after miscarriage
- Miscarriage
- Pregnancy loss
Need more information?
Reasons for Miscarriage | Red Nose Australia
Read more on Red Nose website
Experiencing a pregnancy loss
Losing a baby at any stage of pregnancy can be devastating. Remember, pregnancy loss is more common than you probably think – and it’s not your fault. This article aims to help you deal with the many emotions you will be feeling.
Read more on Pregnancy, Birth & Baby website
Miscarriage
A miscarriage is the loss of a baby, usually during the first three months or first trimester of pregnancy.
Read more on Pregnancy, Birth & Baby website
Pregnancy: miscarriage & stillbirth | Raising Children Network
Have you experienced a miscarriage or stillbirth? Find articles and videos about coping with the grief of losing a pregnancy or having a stillbirth.
Read more on raisingchildren.net.au website
Miscarriage: a guide for men | Raising Children Network
This Dads Guide to Pregnancy covers miscarriage, the grief men might experience after miscarriage, and how to support partners after pregnancy loss.
Read more on raisingchildren.net.au website
The Pink Elephants Support Network - Supporting Your Physical Wellbeing After Miscarriage
Physical Wellbeing can be an important factor when trying to conceive
Read more on Pink Elephants Support Network website
The Pink Elephants Support Network - Supporting Your Emotional Wellbeing After Miscarriage
It can be challenging to maintain a positive outlook after early pregnancy loss
Read more on Pink Elephants Support Network website
The Pink Elephants Support Network - Holistic Options for Miscarriage Management
Some women may find holistic options can help them feel nurtured and empowered on their journey to future pregnancy
Read more on Pink Elephants Support Network website
The Pink Elephants Support Network - Causes of Miscarriage - Pink Elephants
There are a number of possible reasons that a miscarriage may occur, and often it’s not until extensive testing is done that you may find out why
Read more on Pink Elephants Support Network website
The Pink Elephants Support Network - Pregnancy After Loss - Pink Elephants
Pregnancy after loss is a time that can be fraught with many conflicting emotions
Read more on Pink Elephants Support Network website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Blighted Ovum (Anembryonic Pregnancy): Causes & Symptoms
Overview
A blighted ovum is when the gestational sac containing the embryo is empty.What is a blighted ovum?
A blighted ovum (also called an anembryonic pregnancy) is a type of early miscarriage that occurs when a fertilized egg implants into the uterus but does not develop into an embryo. The embryo will stop growing, but the gestational sac (where the embryo would develop) continues to grow. The placenta and empty gestational sac will release pregnancy hormones — even without an embryo present. This causes you to have early symptoms of pregnancy or even have a positive pregnancy test. Sometimes it occurs so early in pregnancy that you don't know you're pregnant.
Sometimes it occurs so early in pregnancy that you don't know you're pregnant.
When does a blighted ovum happen?
A blighted ovum causes an early miscarriage in the first trimester of pregnancy. During fetal development, a fertilized egg turns into a blastocyte. At around four weeks of pregnancy, this blastocyte implants in the wall of the uterus and develops into an embryo. When you have a blighted ovum, the gestational sac that would hold the embryo continues to grow, even without an embryo present. The following can occur:
- A blighted ovum happens so early in pregnancy, that you never realize you are pregnant.
- You have a positive pregnancy test and signs of pregnancy only to discover a blighted ovum at your first ultrasound.
- You have a positive pregnancy test and signs of pregnancy but then experience a miscarriage.
How common is a blighted ovum pregnancy?
A blighted ovum is the number one cause of first trimester miscarriages.
Symptoms and Causes
What are the symptoms of a blighted ovum?
A blighted ovum can occur so early in pregnancy that you never knew you were pregnant. In other cases, you may experience signs of pregnancy such as a missed menstrual period or a positive pregnancy test. You can have symptoms of early pregnancy, such as breast tenderness and morning sickness.
Other times your symptoms will resemble those of a miscarriage:
- Vaginal bleeding: Spotting (light bleeding), bleeding or passing light gray tissue or blood clots.
- Cramping: Mild to moderate cramping in your pelvic and abdominal region.
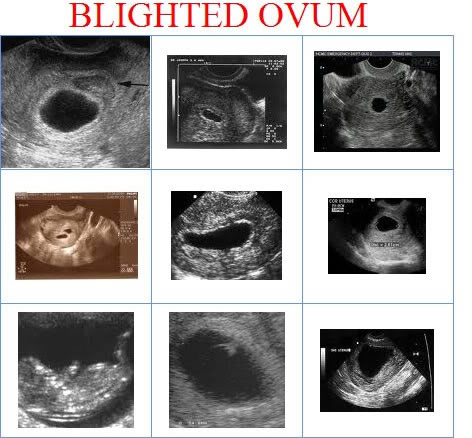
The only way to confirm a blighted ovum is through an ultrasound. It will show a gestational sac that is missing an embryo inside.
What causes a blighted ovum?
A blighted ovum is usually caused by chromosomal or genetic problems during cell division. During conception, the egg will begin to divide shortly after being fertilized by sperm. Around ten days later, the cells have formed an embryo. With a blighted ovum, the embryo never forms or stops growing after it’s formed.
Around ten days later, the cells have formed an embryo. With a blighted ovum, the embryo never forms or stops growing after it’s formed.
How does a blighted ovum miscarriage start?
A blighted ovum miscarriage will cause vaginal bleeding and abdominal cramping. A miscarriage usually feels more intense than your regular menstrual period. You can take an over-the-counter medicine like acetaminophen to relieve cramping. Avoid lifting anything heavy or any strenuous exercise as it can increase your bleeding. You may experience spotting for several weeks after a miscarriage.
Diagnosis and Tests
How is a blighted ovum diagnosed?
Your healthcare provider will diagnose a blighted ovum using transvaginal ultrasound. This happens in the first trimester, usually between seven and nine weeks of pregnancy. An embryo should be visible at this time in pregnancy. With a blighted ovum, the gestational sac will be empty.
- You will lie back on an exam table and place your feet in stirrups like you do for a pelvic exam.
 Your healthcare provider will put an ultrasound wand into your vagina to see the contents of your uterus.
Your healthcare provider will put an ultrasound wand into your vagina to see the contents of your uterus. - A blighted ovum will appear as an empty sac — almost like a bubble.
A blighted ovum is when the gestational sac containing the embryo is empty.
People are often unaware that they have a blighted ovum. This is because your placenta continues to give off hormones, making your body think you are pregnant. This is also why you can still have symptoms of pregnancy, including a positive pregnancy test.
If you’ve already experienced bleeding or signs of a miscarriage, your healthcare provider will use ultrasound to look at the contents of your uterus to diagnose a blighted ovum.
Some healthcare providers will collect a series of blood samples that check the levels of hCG (human chorionic gonadotropin) in your body. HCG is known as the pregnancy hormone because it's only produced if you are pregnant. The level of hCG in your blood increases rapidly in early pregnancy and reaches its peak around weeks eight to ten. If it's not rising quickly, it can indicate a miscarriage or other complication. Your provider may decide to test your hCG levels over the course of several days to evaluate how your hCG levels are rising. This can be an effective tool for diagnosing blighted ovum.
If it's not rising quickly, it can indicate a miscarriage or other complication. Your provider may decide to test your hCG levels over the course of several days to evaluate how your hCG levels are rising. This can be an effective tool for diagnosing blighted ovum.
Management and Treatment
How is a blighted ovum treated?
For some people, there may be no treatment needed, because your body passes the embryo through your vagina (a miscarriage). If your body does not miscarry the embryo, there are other options to remove the contents of your uterus. Your healthcare provider will talk you through possible treatments:
- Dilation & Curettage (D&C): This is a surgical procedure to remove the contents of your uterus. Your healthcare provider will dilate, or open, the cervix and use medical tools and suction to remove the pregnancy tissues from your uterus. This is done under sedation or general anesthesia.
- Natural miscarriage: If it's safe, you may be able to watch and wait to see if your body eventually releases the pregnancy tissues.
 It can sometimes take days or weeks for this to start. Your healthcare provider will let you know if this is an option for you. You will experience cramping, abdominal pain and bleeding once the miscarriage begins.
It can sometimes take days or weeks for this to start. Your healthcare provider will let you know if this is an option for you. You will experience cramping, abdominal pain and bleeding once the miscarriage begins. - Medication-induced miscarriage: You may be given a medication called misoprostol to trigger your body to miscarry. This moves the process along and eliminates the time waiting for a miscarriage to start on its own. You will have cramping, abdominal pain and bleeding within 30 minutes to ten hours of taking the medication.
A follow-up appointment is usually scheduled four to six weeks after a miscarriage or D&C. You may be given another ultrasound to confirm the uterus is empty. Your healthcare provider will check for signs of infection and make sure there were no complications.
What are the complications of a blighted ovum?
Complications of a blighted ovum are uncommon, but the possible complications could include:
- Excessive bleeding or hemorrhage.

- Infection.
- Scarring (from the D&C procedure).
- Tears in the uterus (from the D&C procedure).
How long does it take to recover from a blighted ovum?
Recovering from a blighted ovum miscarriage or D&C can last from one or two weeks to a month. Cramping generally lasts up to a week, but bleeding can last several weeks. Your bleeding should get lighter until it stops completely.
You can resume normal activities when you feel comfortable. Bleeding can increase with strenuous activity or exercise. Hormones may remain in your body and delay your menstrual cycle. Most people will get their period within four to six weeks after a blighted ovum.
It may take longer to recover emotionally from a blighted ovum miscarriage. You may have feelings of sadness, anger or confusion. It’s OK to take time to grieve. Ask your friends and family for support.
Prevention
Can a blighted ovum be prevented?
A blighted ovum can’t be prevented. Some couples may want to do genetic testing on the tissue inside the uterus. This checks for underlying causes of your miscarriage and can be helpful to couples who have experienced multiple pregnancy losses.
Some couples may want to do genetic testing on the tissue inside the uterus. This checks for underlying causes of your miscarriage and can be helpful to couples who have experienced multiple pregnancy losses.
Outlook / Prognosis
How soon after a blighted ovum can I get pregnant again?
Most healthcare providers recommend having one or two regular menstrual cycles before trying to conceive again after any type of miscarriage.
What are my chances of having another blighted ovum?
Your chances of having another blighted ovum are low. Most people go on to have healthy, full-term pregnancies. If you experience more than one blighted ovum, your healthcare provider may suggest testing to determine if there is an underlying cause.
Living With
When should I see my healthcare provider?
Call your healthcare provider right away if you have any of these symptoms:
- Excessive bleeding from your vagina.
- Dizziness or fainting.
- Fever that does not go away.
- Symptoms that get worse over time.
- Severe pain that isn’t helped with pain medicine.
When should I go to the ER?
Go to the nearest ER If you experience heavy vaginal bleeding — more than two pads per hour for two consecutive hours — or have symptoms of anemia like dizziness, palpitations or paleness.
What questions should I ask my doctor?
Losing a pregnancy is upsetting and confusing. Do not be embarrassed to ask any questions you have. It's completely normal to have questions and feel emotional during this time. Some questions you may ask are:
- Can I let my body miscarry or should I take medication to induce a miscarriage?
- What are the risks of miscarriage?
- Do I have to have a D&C?
- What are the risks of a D&C?
- How long can I expect to bleed or have cramping?
- Is there any indication this will happen again?
- When can I start trying to conceive?
- Do I need to come back for another ultrasound?
Frequently Asked Questions
Is a blighted ovum considered a miscarriage?
Yes, a blighted ovum is a miscarriage. A miscarriage is a loss of pregnancy before 20 weeks. A blighted ovum is considered an early miscarriage because it occurs before 13 weeks of pregnancy.
A miscarriage is a loss of pregnancy before 20 weeks. A blighted ovum is considered an early miscarriage because it occurs before 13 weeks of pregnancy.
How long can you carry a blighted ovum?
The amount of time you can carry a blighted ovum varies. Your placenta will continue to grow and release hormones without an embryo. For some people, a miscarriage can occur within a few days or weeks. Others may still believe they are pregnant only to discover a blighted ovum at their first ultrasound.
Can a blighted ovum turn into a baby?
No, an empty gestational sac will not turn into an embryo. The formation of the embryo occurs within two weeks of conception. By the time the gestational sac is formed, the cells should have already formed the embryo. Your healthcare provider will be able to examine your gestational sac to confirm that no embryo has developed.
Do hCG levels rise with blighted ovum?
Yes, most of the time hCG levels will rise, giving you a positive pregnancy test and symptoms of pregnancy. This is because the placenta continues to give off hCG even if an embryo is not present. The hormone hCG is sometimes called the pregnancy hormone because it is only produced if you are pregnant.
This is because the placenta continues to give off hCG even if an embryo is not present. The hormone hCG is sometimes called the pregnancy hormone because it is only produced if you are pregnant.
Is a blighted ovum more common with IVF?
A blighted ovum is not more common with IVF (In Vitro Fertilization). Your chances of having a blighted ovum with IVF treatment are about the same as they would be with a natural conception.
A note from Cleveland Clinic
Losing a pregnancy is difficult. If you are struggling after a miscarriage, speak with your healthcare provider so they can recommend support groups or counselors. Finding support may help you get through this hard time. Most people who have had a blighted ovum will go on to have a healthy pregnancy.
What to do after a miscarriage
If a woman has a miscarriage, it is important to take competent measures to restore health. This will help to cope mentally and prepare the ground for a new pregnancy. According to medical statistics, 15-20% of pregnancies end in spontaneous termination for various reasons. The symptoms of what happened rarely go unnoticed, which makes it possible to diagnose the pathology in time, consult a gynecologist, undergo adequate treatment and plan the birth of a child for the future. nine0003
According to medical statistics, 15-20% of pregnancies end in spontaneous termination for various reasons. The symptoms of what happened rarely go unnoticed, which makes it possible to diagnose the pathology in time, consult a gynecologist, undergo adequate treatment and plan the birth of a child for the future. nine0003
Specialists classify spontaneous abortion into two categories:
1. Termination of biochemical pregnancy - the embryo leaves the uterine cavity in the first or third weeks after conception. A woman during this period most often does not suspect that she is carrying a child. Pregnancy becomes known only when testing for the content of hCG in the urine and blood. The blood that has left the body is usually perceived as menstruation, which, for unknown reasons, began outside the scheduled time. Units who carefully monitor their health go to the doctor. nine0003
2. Spontaneous abortion or miscarriage in early pregnancy - up to 22 weeks, when the weight of the embryo does not reach 0. 4 kg.
4 kg.
Medical therapy
Any method is useful to maintain pregnancy. A qualified doctor develops an individual treatment protocol based on the available diagnostic data. Drugs used may include:
- sedatives;
- restorative therapy; nine0022
- hormone stabilizing drugs;
- uterine antispasmodics;
- vitamin and mineral supplements.
The specialist eliminates the threat of miscarriage in the early stages, tells how to prevent a relapse. In the later stages, the cervix is fixed with a special suturing (usually for a period of 16-25 weeks, if there is an ICI).
If an attempt to stop a spontaneous abortion fails, the following treatment tactics are used:
- Waiting – an organism freed from an embryo does not require specialized treatment.
- Drug therapy - the patient is prescribed drugs that complete the removal of foreign tissues from the body.
 By causing severe spasms of the muscular walls of the uterus, the tablets provoke the expulsion of residues from the cavity.
By causing severe spasms of the muscular walls of the uterus, the tablets provoke the expulsion of residues from the cavity. - Surgery - is used in case of complications or inconvenient for the independent exit of the fetus, the bending of the uterus. nine0022
Curettage
Having symptoms of a miscarriage in early pregnancy and faced with the need for a curettage (gynecological cleaning), a woman worries about the state of her reproductive system. It is not worth doing this, the operation takes place in a gentle mode, with maximum delicacy in relation to the patient's childbearing ability. Curettage is performed when there is a risk of incomplete exit of the embryo from the uterine cavity and the development of infection in the pelvic organs due to the elements remaining in it. Ignoring the procedure can lead to blood poisoning and the formation of a pathology that prevents re-conception. nine0003
Vacuum aspiration, however, is performed more frequently, which is more gentle. The complex application of the method with hysteroscopy allows you to carefully examine the internal contents of the uterus in order to prevent poorly cleaned areas on the mucous membrane.
The complex application of the method with hysteroscopy allows you to carefully examine the internal contents of the uterus in order to prevent poorly cleaned areas on the mucous membrane.
Preparation for gynecological cleaning (curettage)
Gynecological cleaning is performed for diagnostic and therapeutic purposes for various indications :
- after childbirth;
- in missed pregnancy, miscarriages; nine0022
- for menstrual irregularities;
- for accurate diagnosis of gynecological disorders.
Curettage is recommended a few days before the onset of menstruation. In this case, blood loss decreases and a favorable prognosis is given for rapid tissue recovery. The operation requires a preliminary examination, testing. This is :
- complete blood count;
- blood coagulation tests; nine0022
- smear for examination of the bacteriological environment;
- STI testing.
Before curettage, you stop taking any medications, dietary supplements that have not been discussed with a specialist. Even plant components that can affect blood clotting and provoke blood loss during surgery can be dangerous. Your healthcare provider should be made aware of the medications you are taking so that they know what risks may arise. nine0003
Rules for preparing for the procedure:
- refrain from sexual intercourse three days before the operation;
- avoid the use of intimate hygiene products (gels, creams, ointments, liquids), suppositories, tablets and vaginal sprays;
- Do not douche;
- Do not eat or drink 10 hours before surgery. This is necessary for high-quality anesthesia.
Cleaning
Curettage is carried out in a hospital, the woman is placed on the gynecological chair of the operating room. The doctor removes the upper layer of the mucous lining the uterine cavity from the inside. The exclusion of pain involves anesthesia. If there were signs of miscarriage in the early stages of pregnancy or at a later period, after which it spontaneously terminated, the dilated cervix allows for curettage without anesthesia. For anesthesia, intravenous administration of the drug is used, selected individually, taking into account the characteristics of the patient's body. A few seconds after the injection, the woman falls into a shallow sleep, the discomfort disappears, which makes the doctor's actions painless. nine0003
The exclusion of pain involves anesthesia. If there were signs of miscarriage in the early stages of pregnancy or at a later period, after which it spontaneously terminated, the dilated cervix allows for curettage without anesthesia. For anesthesia, intravenous administration of the drug is used, selected individually, taking into account the characteristics of the patient's body. A few seconds after the injection, the woman falls into a shallow sleep, the discomfort disappears, which makes the doctor's actions painless. nine0003
A dilator inserted into the cervix straightens the walls of the organ, facilitating access to the internal cavity. Holding the neck, the specialist inserts a rounded probe with a small diameter, after which he replaces it with a more voluminous analogue. A special video camera attached to the end of the probe allows for hysteroscopy - examination of the cavity before curettage. Cleaning is done with a curette, shaped like a small spoon on a long handle. Carefully collected tissues are stored in a specialized sterile tube, which is later sent to the laboratory for histological examination. nine0003
nine0003
The procedure rarely takes more than one hour, usually 20 minutes is enough for the doctor. Together with the cavity, the cervical canal is cleaned. Manipulations are called RDV - separate diagnostic curettage. Collected samples are placed separately. Histology is used to identify the structure of tissues in order to exclude the presence of atypical cells in them, indicating cancerous lesions, precancerous conditions. The study is carried out within two weeks, after receiving the results, the woman revisits the gynecologist for a follow-up examination. nine0003
Curettage is often carried out for diagnostic purposes to determine the symptoms of pathological conditions in the functioning of the organs of the reproductive system. These can be:
- irregular cycle;
- voluminous discharge and painful menstruation;
- bleeding during menopause;
- difficulties in conceiving in the absence of visible causes of pathology;
- suggestion of developing uterine cancer.

Possible complications
Complications can occur, as after any surgical intervention. A serious consequence is the discovery of uterine bleeding. In order to prevent it, oxytocin is used - injections stimulate the cessation of abnormal blood flow. Oxytocin will help if the bleeding is due to insufficient contraction of the uterus. In violation of blood clotting, it is ineffective.
Another complication of is hematometra, when blood clots accumulate in the uterine cavity, which can cause an inflammatory process in the tissues. It is caused by a spasm of the cervix that occurred immediately after cleaning, which interferes with the evacuation of blood. Experts recommend the use of antispasmodics that relax the muscles of the organ and contribute to the normal outflow of blood. A woman should be alerted by pulling pains in the lower abdomen and a sharp cessation of discharge. nine0003
After cleansing, endometritis may occur when inflammation affects the lining of the uterus. A measure of therapy for a dangerous diagnosis is a course of antibiotics. Pain in the abdomen and a sharp increase in body temperature testify to the pathology. Any dangerous change in condition should be reported to the doctor immediately. In this case, countermeasures will be taken in a timely manner, which will eliminate the risks of developing more formidable complications.
A measure of therapy for a dangerous diagnosis is a course of antibiotics. Pain in the abdomen and a sharp increase in body temperature testify to the pathology. Any dangerous change in condition should be reported to the doctor immediately. In this case, countermeasures will be taken in a timely manner, which will eliminate the risks of developing more formidable complications.
How to behave after a miscarriage
A miscarriage that has occurred requires a certain tactic of behavior. Among the measures recommended by doctors:
- It is advisable to postpone a new pregnancy attempt for 3-6 months . Otherwise, the risk of repeating the undesirable development of events is high. If pregnancy occurs before the expiration date, there is no need to panic. The main thing is the supervision of a specialist.
- If you are waiting for , ask for advice on effective contraception. nine0022
- Follow your doctor's advice .
- Pass the necessary examinations , take tests.
Ask about the effect of the drugs you take on the fetus if you become pregnant during therapy. Find out after what period of time you can fearlessly try to conceive a child.
How to detect genetic pathologies during repeated pregnancy
If a miscarriage of the first pregnancy occurs due to a genetic factor, it is especially scary to decide on a second one. But you should not be afraid of this, with a well-designed therapy, the chances of success are more than great. Diagnostic procedures today are highly accurate and allow you to identify pathology in the early stages. Examination in this case is mandatory, as well as the following:
- who are over 35;
- has screening changes;
- who had markers of chromosomal pathologies and malformations of the embryo;
- who already have children with chromosomal abnormalities.
Ultrasound diagnostics can detect malformations in 80-85% of cases. However, the technology is not impeccably reliable, as it misses pathologies in 20% of situations. Biochemical screening, invasive examinations have valid data. The latest version of the study allows you to identify up to 99% anomalies.
However, the technology is not impeccably reliable, as it misses pathologies in 20% of situations. Biochemical screening, invasive examinations have valid data. The latest version of the study allows you to identify up to 99% anomalies.
When planning a new pregnancy, it is imperative to visit a geneticist. Screening diagnostics for the detection of abnormal genes will help eliminate the risks of possible pathologies, the factor of heredity and genetic failure during conception. Sometimes the threat of miscarriage in the early stages exists in almost healthy carriers. The examination will allow you to find out about the anomaly in advance and undergo treatment.
What is a miscarriage like
A miscarriage that occurs is complete when all parts of the embryo come out of the uterine cavity together with membranes and amniotic fluid. If parts of the fetus remain in the uterus, they speak of an incomplete miscarriage, which occurs more often in the early stages of pregnancy. To neutralize the negative consequences, to prevent the development of an infectious process in the tissues, the product of conception is evacuated from the uterine cavity by the methods of medical interruption, gynecological curettage, and vacuum aspiration. Therapy may include the use of drugs aimed at contracting the uterus and pushing the contents out. Ultrasound examination is considered to be the control method of diagnostics. nine0003
To neutralize the negative consequences, to prevent the development of an infectious process in the tissues, the product of conception is evacuated from the uterine cavity by the methods of medical interruption, gynecological curettage, and vacuum aspiration. Therapy may include the use of drugs aimed at contracting the uterus and pushing the contents out. Ultrasound examination is considered to be the control method of diagnostics. nine0003
Why the body rejects the embryo
The causes of miscarriage often lie in the presence of chromosomal abnormalities in the fetus. Among the factors that provoke rejection of embryos are also:
- Heredity and genetic failure at the stage of fertilization of the egg by the sperm.
- A non-viable fetus may appear as a result of various risk factors - environmental conditions, occupational hazards, viral illness of parents. It is impossible to neutralize these factors.
 The only way out of the situation is to reduce the likelihood of their manifestation by protecting the expectant mother from dangers during gestation. nine0022
The only way out of the situation is to reduce the likelihood of their manifestation by protecting the expectant mother from dangers during gestation. nine0022 - Hormonal imbalance caused by disruption of the endocrine system. The situation can be affected by an insufficient amount of progesterone in the mother's body or an excess of testosterone. With early detection of a failure of the hormonal system, a woman undergoes specially organized therapy before pregnancy.
- The presence of tumors , neoplasms in the pelvic organs.
- Isthmic-cervical insufficiency when the isthmus and cervix dilate prematurely, unable to cope with the increasing pressure caused by the growing fetus in the body. nine0022
- There is a risk of miscarriage in the presence of anomalies in the work of the cardiovascular and renal systems.
- Drug addiction , alcohol addiction, substance abuse of mother and father.
- Depressive conditions , stress, nervous stress of a pregnant woman.
- Mechanical stress , blows, bruises, excessive physical labor of the future woman in labor.
- X-ray examination - radiation can cause miscarriage. nine0022
- Drug use . In the first trimester, you can not use potent medicinal formulas. Drugs can cause the development of defects in the embryo. Some decoctions of herbs are also contraindicated - parsley, tansy, cornflower, nettle, St. John's wort. It is forbidden to self-medicate. Each drug is agreed with the attending physician.
- Infectious and viral process in the body. Any sexually transmitted infection can provoke a miscarriage, which must be cured before pregnancy, otherwise there is a high risk of infection of the fetus in the womb. A great threat of miscarriage in the early stages exists due to viral infections and inflammation of the internal organs.
 A dangerous symptom is the high temperature of the mother, accompanied by intoxication of the body. At the stage of pregnancy planning, it is important to stop chronic diseases. nine0022
A dangerous symptom is the high temperature of the mother, accompanied by intoxication of the body. At the stage of pregnancy planning, it is important to stop chronic diseases. nine0022 - History of abortion , unsuccessful surgery, unprofessionalism of the doctor and unfortunate circumstances.
- Immunological factors .
The list of causes of miscarriage in the early stages of pregnancy and in the later period may be more extensive, in each case, doctors identify the pathology individually.
Isthmic-cervical insufficiency (ICI)
One of the most common causes of spontaneous miscarriage during pregnancy is CSI - dilatation of the cervix and isthmus of the uterus as a result of increasing pressure from the growing fetus. Pre-pregnancy manipulations with the uterus (cervical dilation due to abortion, childbirth or curettage) affect the condition of the muscle ring. Damaged areas are tightened by scar tissue that does not have elasticity, is not amenable to stretching and contraction. ICI also has a functional nature when there is a hormonal imbalance. nine0003
ICI also has a functional nature when there is a hormonal imbalance. nine0003
ICI occurs in the period from the 11th to the 27th week after conception, when the embryo begins to produce androgens in the mother's body with the launch of the adrenal glands. Taking into account the mother's hormones, their indicator can be exceeded - this softens the cervix, opens and shortens it. Harmful bacteria and microorganisms penetrate into the formed channel, infecting the fetal egg. The initial stages of ICI do not have obvious symptoms, since they do not entail the tone of the uterine muscles. With the loss of strength of the membranes, amniotic fluid pours out. There are no pain sensations. nine0003
If a woman has had a miscarriage that started with amniotic fluid, she should report it to her doctor when monitoring a subsequent pregnancy.
Treatment of isthmic-cervical insufficiency
Endocrine disorders are corrected by prescribing hormonal drugs. An assessment of the condition of the uterus is carried out by a doctor a couple of weeks after the start of taking medications. They say about positive dynamics when the opening is suspended and no further expansion of the neck is observed. In the absence of the planned effect, surgical intervention is prescribed. Similar measures are used for the traumatic nature of the neck deformity. You should not be afraid of the operation, the doctor acts delicately, without causing additional injuries to the patient, without causing discomfort to the baby growing in the womb. The procedure is most effective in the early stages of pregnancy. Suturing can significantly reduce the risk of infection of the embryo through the lower edge of the cavity. nine0003
They say about positive dynamics when the opening is suspended and no further expansion of the neck is observed. In the absence of the planned effect, surgical intervention is prescribed. Similar measures are used for the traumatic nature of the neck deformity. You should not be afraid of the operation, the doctor acts delicately, without causing additional injuries to the patient, without causing discomfort to the baby growing in the womb. The procedure is most effective in the early stages of pregnancy. Suturing can significantly reduce the risk of infection of the embryo through the lower edge of the cavity. nine0003
Surgical intervention takes place in a hospital. Before the operation, the pregnant woman is examined. After the procedure, the vagina is sanitized, for which the suturing site is treated with chlorhexidine and furatsilin for three days. The patient needs to undergo a weekly follow-up examination with the attending physician, where he assesses the situation, making adjustments to the therapeutic protocol if necessary. The sutures are removed at the 38th week of pregnancy. During this time, the neck matures, preparing the birth canal for the passage of the fetus. Many women in labor worry that they will need a caesarean section if they have stitches, but this is not true. In most cases, women give birth on their own. nine0003
The sutures are removed at the 38th week of pregnancy. During this time, the neck matures, preparing the birth canal for the passage of the fetus. Many women in labor worry that they will need a caesarean section if they have stitches, but this is not true. In most cases, women give birth on their own. nine0003
Immediate action is recommended if the amniotic sac prolapses (falls out) into the cervix between 16 and 24 weeks. The suturing of the neck obliges the woman to observe bed rest, strictly follow the daily routine, avoid physical exertion, and do not skip taking medications. In rare cases, complications occur. Among them, the eruption of sutures through the tissues, provoked by the frequent tension of the muscles of the uterus. To prevent tone, tocolytics are prescribed - medicines to prevent premature birth. The expectant mother should be prepared for frequent examinations and smears, which may be caused by the likelihood of accumulation of pathological microflora on the suture threads. nine0003
nine0003
It is also important to conduct psychological therapy, where a woman is taught relaxation techniques. The behavior of the future mother is a decisive factor in the successful bearing of the fetus in case of pregnancy complications. Panic and fuss create an unfavorable prognosis in stabilizing the situation. If a spontaneous abortion occurred for reasons of ICI, when you can get pregnant after a miscarriage, the doctor will say. Ideally, the period should be at least two years. The specialist must also take measures to prevent a repeated situation of losing a child. nine0003
In addition to the suture, ICI correction is also carried out using an obstetric pessary. An alternative method is the imposition of a special ring of hypoallergenic materials on the cervix. Silicone is the most commonly used. The ring creates additional support, preventing the opening of the neck.
Uterine hypertonicity - risk prevention
Uterine contractions before natural delivery is called hypertonicity. The condition is not an independent disease, it signals a malfunction in the body, often manifesting itself in the early stages of pregnancy. The causes of the pathological phenomenon are:
The condition is not an independent disease, it signals a malfunction in the body, often manifesting itself in the early stages of pregnancy. The causes of the pathological phenomenon are:
- Hormonal disorders caused by insufficient function of the placenta, ovaries, problems with the adrenal glands, causing imbalance.
- Genital infantilism organ defects.
- Neoplasms , tumors in the uterus that are not necessarily malignant (eg, fibroids).
- During pregnancy infectious processes, viral diseases. nine0021 CCI - opening of the cervix under increasing pressure created by the growing embryo.
- Immunological problems .
- Chronic diseases of the body (cardiovascular disorders, renal insufficiency).
- Past miscarriages early pregnancy, symptoms of which may recur, induced abortions.

In addition to physiological causes, psychological factors are of no small importance. A woman who is in a depressed state can provoke hypertonicity in herself. nine0003
You can feel the tension of the muscles of the uterus on your own, without the help of a specialist. This is evidenced by the heaviness that appears in the lower abdomen, pulling pains in the lumbar region. Symptoms are similar to painful menstruation. Arising in the first trimester, the condition provokes spontaneous abortion, missed pregnancy, death of the fetal egg. In the subsequent period, premature birth due to hypertonicity is likely.
Why does the tension of the walls of the uterus cause irreversible consequences? The reason is the disturbed blood supply to the placental tissues, the occurrence of hypoxia of the embryo and the slowdown in the development of the emerging child. Following the contraction of the muscles of the uterus, the placenta does not contract, which causes its detachment and provoking the release of the fetal bladder. nine0003
nine0003
Hypertonicity is diagnosed during a scheduled visit to a specialist. Stabilization of the situation requires the appointment of sedative drugs and antispasmodics. A strengthening effect is provided by therapy with the inclusion of vitamin B6, magnesium. In most cases, the measures taken are sufficient to neutralize the risks. Self-treatment, which can cause irreversible consequences, is strictly prohibited. With hypertonicity, the main rule for a pregnant woman is calmness and lack of physical activity. Some women who have had a successful delivery say they "didn't get up" during their entire pregnancy. With hypertonicity, sexual intercourse is also excluded. nine0003
If the threat cannot be neutralized, hospitalization is recommended. It is especially dangerous when severe cramping pain is complemented by spotting. To lie down "for preservation" is an adequate measure in the struggle for the birth of a healthy and strong baby. In the hospital walls, a pregnant woman is prescribed a vaginal examination, ultrasound. If necessary, a woman takes urine and blood tests, checks the hormonal background, and is examined for the presence of STIs.
If necessary, a woman takes urine and blood tests, checks the hormonal background, and is examined for the presence of STIs.
At the onset of labor activity before the 34th week, the condition is tried to be stabilized with tocolytics. The most dangerous period is from the 25th to the 28th week, when the woman is recommended the maximum possible bed rest. After that, the fetus has every chance of survival. In order to quickly form the pulmonary system of the embryo, allowing it to survive with an early birth, hormones are prescribed. nine0003
Having an unfavorable prognosis for miscarriage and the threat of miscarriage, it is necessary to take up prevention at the stage of conception planning.
Stages of spontaneous abortion
There are certain signs that attract attention and divide the course of a miscarriage into specific stages:
- Threat - having noticed factors threatening pregnancy, you can take measures to restore the situation, normalize the mother's well-being.
 nine0022
nine0022 - Start of abortion - at this stage, the doctor can apply life-saving manipulations and give recommendations to the pregnant woman.
- Miscarriage in progress – the condition is irreversible, it is impossible to stop the pathology. The death of the fetal egg begins, which leaves the uterine cavity.
- Completed abortion - the uterus gets rid of the residual tissues of the embryo, cleanses, restores its original parameters. It is important to prevent the remnants of foreign fibers inside, otherwise the organ becomes infected with decaying residues and toxins go into the bloodstream. nine0022
Symptoms of miscarriage - how not to miss the threat
If there is a threat of miscarriage in the early stages, the following symptoms may occur: The pain may be monotonous or come in waves.
 Bright scarlet blood can stand out, it is often confused with menstruation. nine0022
Bright scarlet blood can stand out, it is often confused with menstruation. nine0022 A woman who does not know how an early miscarriage occurs should listen to her inner state.
Should alert:
- spasmodic pain impulses;
- Drawing pain in the lumbar region.
In the later stages, the above symptoms are added:
- liquid discharge from the vagina, which may indicate damage to the amniotic sac; nine0022
- pain when urinating;
- internal bleeding, which warns of a deterioration in the general condition, fainting, dizziness, pallor of the skin. All this is an indication for emergency hospitalization of a pregnant woman.
The beginning of an abortion is characterized by more pronounced symptoms of a miscarriage - contraction-like pain, severe dizziness, loss of strength. Instead of smearing discharges, clot-like ones appear, abundantly manifested during movement. Pregnancy can be saved if the area of detachment of the fetal egg is small and the fetal heartbeat is determined. nine0003
Pregnancy can be saved if the area of detachment of the fetal egg is small and the fetal heartbeat is determined. nine0003
The third stage is useless for saving the fetus. There is girdle pain in the lower back and abdomen. Together with abundant blood loss, a fetal egg comes out of the uterus. Incomplete miscarriage requires curettage of the uterine cavity if parts of the embryo or membranes of the fetal egg remain in it, otherwise there is a high risk of complications that will endanger the life of the mother.
In rare cases, complications and serious health consequences can occur after a spontaneous abortion. But in the majority of situations, the body independently copes with what happened, expelling the parts remaining in the uterine cavity with a natural contraction of the muscles. An early spontaneous miscarriage does not always occur, a dangerous condition can also occur in the later stages. Some women try to provoke the release of the fetus with decoctions of herbs and medications. This is fraught with complications, including sepsis, dysfunction of the reproductive organs, after which pregnancy becomes impossible. nine0003
This is fraught with complications, including sepsis, dysfunction of the reproductive organs, after which pregnancy becomes impossible. nine0003
Methods of diagnosis
The symptoms of a threatened miscarriage at an early stage will be determined by a doctor during a visit to the antenatal clinic. The specialist will check the size of the uterus, determine the tone of its muscles, the condition of the cervix, and examine the discharge from the genital organs. A reliable method to identify the existing threat is transvaginal ultrasound diagnostics. The doctor draws attention to segmental muscle contractions of the uterus, detachment of the fetal egg. Genetic testing will help analyze the likely causes of a miscarriage. The patient's history is carefully collected. nine0003
Planning a new pregnancy
The medical community is unanimous in the issue of planning a new pregnancy after a spontaneous abortion. Conception is not recommended for at least 3-6 months. During this period, the woman's body will recover and gain strength to bear the fetus. Observation by a doctor, harmonization of hormonal levels, examination of parents to identify possible pathologies are important. In order not to become pregnant in the first months, it is recommended to use contraceptive methods prescribed by your doctor. nine0003
Observation by a doctor, harmonization of hormonal levels, examination of parents to identify possible pathologies are important. In order not to become pregnant in the first months, it is recommended to use contraceptive methods prescribed by your doctor. nine0003
Examination after a miscarriage includes blood and urine tests, examination of the microflora of the vagina with a smear, detection of overt and latent genital infections, glucose and hormone tests, examination of partners for biological compatibility. Planning is an important step towards having a healthy baby. After the studies, the woman is prescribed strengthening therapy. It is important to completely reconsider eating habits, to exclude factors that are harmful to well-being. Vitamins, folic acid are used. Fast food, food containing carcinogens and preservatives are excluded from the diet. Subject to the rules recommended by the doctor, a successful pregnancy with a favorable outcome is likely. nine0003
It is not uncommon for a pregnancy test to show two lines after a miscarriage. This is due to the restructuring of the body, the organs of the reproductive system. It is important to report the incident to your doctor. The presence of remnants of embryonic tissue in the uterus can provoke a positive test result. In this case, immediate curettage is necessary, which neutralizes the risk of inflammation and infection. To accurately determine her condition, a woman needs to undergo an ultrasound diagnosis, take tests to determine hCG in the blood. nine0003
This is due to the restructuring of the body, the organs of the reproductive system. It is important to report the incident to your doctor. The presence of remnants of embryonic tissue in the uterus can provoke a positive test result. In this case, immediate curettage is necessary, which neutralizes the risk of inflammation and infection. To accurately determine her condition, a woman needs to undergo an ultrasound diagnosis, take tests to determine hCG in the blood. nine0003
The question of whether it is possible to get pregnant after a miscarriage worries many parents. The answer is unequivocal - yes, if you follow the recommendations of experts, carefully plan a new conception, monitor your well-being and state of your health.
Components of success after a miscarriage
Spontaneous abortion can provoke not only the health of the patient, but failure to follow simple rules can be a threat. To reduce the risk of losing a child during pregnancy, you need to:
1. Keep calm – it is important for a mother to eliminate all factors that make her nervous from her life. Irritation is not the best way to normalize the condition. In order to stabilize the emotional background, rest is recommended, the use of soothing teas with the permission of the doctor. Good results are given by decoctions of chamomile, lemon balm, mint.
Keep calm – it is important for a mother to eliminate all factors that make her nervous from her life. Irritation is not the best way to normalize the condition. In order to stabilize the emotional background, rest is recommended, the use of soothing teas with the permission of the doctor. Good results are given by decoctions of chamomile, lemon balm, mint.
2. Avoid taking unnecessary medicines and preparations. But it is unacceptable to stop the therapy prescribed by the doctor on your own. Each step must be discussed with the gynecologist. nine0003
3. Eliminate harmful occupational factors. Work in the chemical industry and other hazardous facilities can create an undesirable background in the body, which prevents normal gestation. It is important to understand what is of great value to the mother - the birth of a healthy baby or a career factor. Many refuse to work to increase the chance of having a baby.
4.![]() Eliminate bad habits. It is unacceptable for a woman who has experienced miscarriage to drink alcohol and smoke. It is forbidden to do this and the future father. This negatively affects the quality of spermatozoa, provokes difficulties with conception and risks of deviations in the development of the embryo. nine0003
Eliminate bad habits. It is unacceptable for a woman who has experienced miscarriage to drink alcohol and smoke. It is forbidden to do this and the future father. This negatively affects the quality of spermatozoa, provokes difficulties with conception and risks of deviations in the development of the embryo. nine0003
5. Take vitamin complexes, specially designed to prepare the body for pregnancy, the formation of basic conditions for its favorable course.
6. Eat right. A complete, balanced diet works wonders. With a lack of weight, a nutritionist will develop an adequate diet for a woman with the inclusion of a large amount of protein foods rich in vitamins and trace elements of vegetables, fruits, and cereals. Recommended fats contained in fish, seeds, nuts, avocados, olives. nine0003
7. Get rid of extra pounds. Obesity adversely affects the development of pregnancy. Science has proven that enhanced nutrition during this period is not required. The main thing is its balance.
The main thing is its balance.
Infections during pregnancy
Infectious processes transferred before pregnancy develop immunity in the mother to similar agents of influence. Primary infection poses a great threat, so vaccination will be useful before planning conception. Perinatal diagnosis allows you to detect the infectious process at the initial stage and prevent its harmful effects. This is possible if the pregnant woman is registered from an early date. nine0003
Infection may develop due to an infection transmitted by airborne droplets. It is the most dangerous, since it is almost impossible to prevent it. This applies to mumps, measles, rubella. HIV and hepatitis infect the body through sexual contact, similar to chlamydia. Listeriosis is transmitted with poor-quality products. A pregnant woman can pass infections to a developing baby. Pathology is determined by profile tests of latent infection.
Routine pregnancy monitoring involves regular testing. Sexual infections are determined using a smear, ultrasound shows deviations in the development of the baby, and KGT is aimed at listening to the work of the fetal heart muscle. If there is a suspicion of a serious infection of the embryo, blood sampling from the umbilical cord and amniotic fluid analysis are practiced. nine0003
Sexual infections are determined using a smear, ultrasound shows deviations in the development of the baby, and KGT is aimed at listening to the work of the fetal heart muscle. If there is a suspicion of a serious infection of the embryo, blood sampling from the umbilical cord and amniotic fluid analysis are practiced. nine0003
Infection of a child also depends on concomitant factors. The speed of diagnosis, the literacy of the treatment, the type of pathogen, the duration of the pregnancy are taken into account. The following infectious processes deserve special attention:
1. Viral etiology - a huge number of viruses poses a danger to a pregnant woman. The threat is genital herpes, rubella, infectious type erythema, cytomegalovirus, hepatitis B, measles, mumps, chickenpox. nine0003
2. Bacterial infections, detected during the analysis of biological materials (feces, urine, blood), examination of certain organs of the body. Active reproduction provokes a rapid growth in the number of bacteria in the vagina. Not all microorganisms pose a threat to the child. Dangerous candidiasis, streptococcus, chlamydia, bacterial vaginosis, cystitis.
Active reproduction provokes a rapid growth in the number of bacteria in the vagina. Not all microorganisms pose a threat to the child. Dangerous candidiasis, streptococcus, chlamydia, bacterial vaginosis, cystitis.
The successful course of pregnancy is threatened by intestinal infections, often activated in the summer. Their carriers can be animals and poorly processed food before consumption. Of particular danger are listeriosis, salmonellosis, toxoplasmosis. nine0003
Prevention of infections during pregnancy
Infection of the mother poses a threat to the life of the fetus. From the 3rd to the 12th week, the infected organism responds with a miscarriage or the formation of malformations of the child. From the 11th to the 25th - developmental delay. At a later date, organs are deformed and prerequisites for premature birth are created. In order to prevent intrauterine infection, it is recommended to apply a number of rules:
- be examined for the detection of STIs; nine0021 examine blood, determine the presence of antibodies to infection carriers, pathogens;
- avoid contact with sick people, visits to crowded places where there is a possibility of infection by airborne droplets;
- screen pets for dangerous infections, treat them if necessary, or remove them from the home until the threat is eliminated;
- exclude fast food, store-bought semi-finished products from the diet, thoroughly heat treat meat, fish; nine0022
- remove from the diet sushi and other culinary delights purchased in restaurants, cafes;
- thoroughly wash hands, fruits, vegetables with special disinfectants that are not capable of harming the pregnant woman and the child;
- it is planned to visit a gynecologist, undergo examinations recommended by a doctor, take tests, take vitamins;
- register at the first sign of pregnancy;
- prepare for conception, cure infections, vaccinate.
 nine0022
nine0022
It is also important for the child's father to follow most of the recommended rules. If only the mother undergoes treatment, a relapse is likely during sexual intercourse, neutralizing the beneficial effect of therapy.
A woman who has had a miscarriage in the past should be alert to any deviations from the norm in her state of health. It is important to pay attention to ailments, pain, weakness, dizziness. Accounting for an early consultation will create conditions for the bearing of the fetus and the birth of a child. There is no need to be afraid that a miscarriage will forever deprive the joy of motherhood. nine0003
Having completed a course of examinations, passing tests and following the measures prescribed by the doctor to treat imbalances in the body, you will create all the conditions for a favorable pregnancy outcome. Tune in to the positive, protect yourself from worries, worries, stress. Feel the support of loved ones, hope for the best! Get advice from good specialists to rule out any unfavorable prognosis before conception or take steps to neutralize them. Health and prosperity to you, your families and loved ones! nine0003
Health and prosperity to you, your families and loved ones! nine0003
Causes of miscarriage - Health Clinic 365 Yekaterinburg
Miscarriage. Symptoms
Questions to the doctor about miscarriage
Diagnosis of miscarriage
Treatment and prevention of miscarriage
The causes are usually pathologies at the gene or chromosome level. Most miscarriages occur due to abnormal development of the fetus. Deviations that occur in a child at the gene or chromosome level are the result of disorders in cell division or embryo development, and are not transmitted from parents. nine0003
Anembryonic pregnancy. Anembryonic pregnancy is quite common and is the main cause of miscarriage for up to 12 weeks. It happens when a placenta and amniotic membranes form from a fertilized egg, but not a fetus.
Intrauterine fetal death. The death of the embryo occurred before any signs of pregnancy began to appear. Intrauterine fetal death may also be associated with genetic abnormalities of the fetus. nine0003
nine0003
Blistering mole. Mole, also called trophoblastic disease, is less common - about one case in 1000. This is an abnormality of the placenta, caused by the occurrence of violations during fertilization. If the fetus is in this mass, it cannot develop and dies.
Sometimes a miscarriage happens because of the health of the mother.
In some cases, maternal health problems can cause miscarriage, for example:
- Uncontrolled diabetes
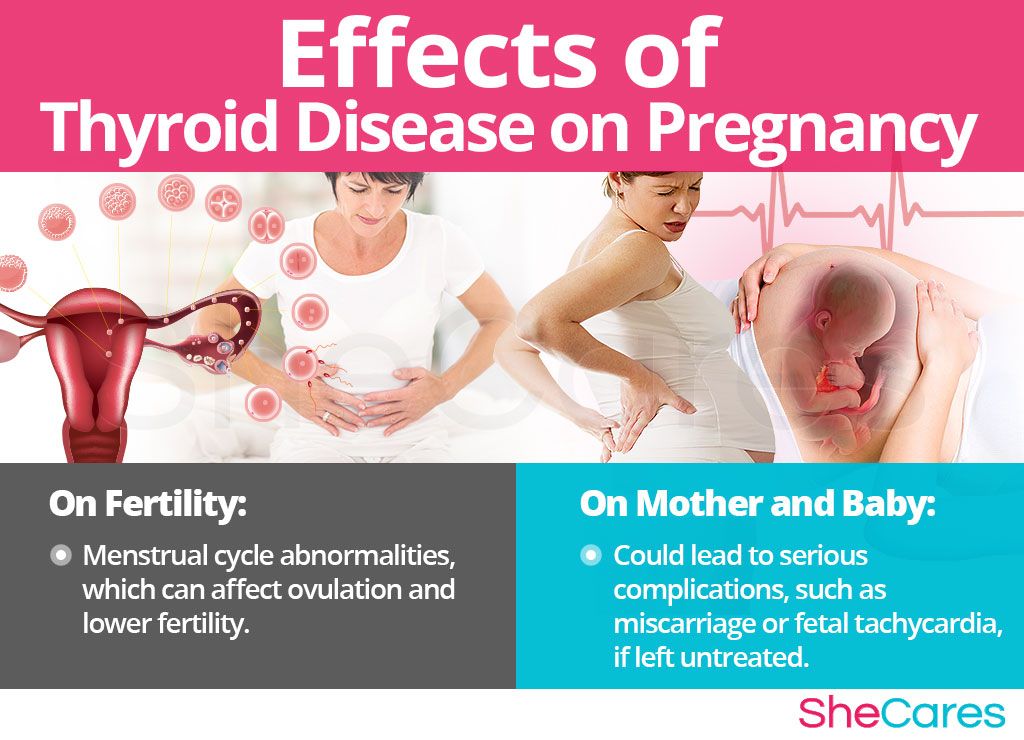
- Diseases of the thyroid gland
- Infections
- Hormonal disorders
- Diseases of the uterus or cervix
Miscarriage is NOT caused by:
- Sports
- Heavy lifting or exercise
- Sexual activity
- Labor activity, if the work is not related to chemicals
Risk factors. nine0008
Various factors increase the risk of miscarriage, for example:
Age. Women over 35 have a higher risk of miscarriage than younger women. At age 35, the risk is about 20%, at age 40, about 40%, and at age 45, about 80%. The age of the father may also play a role. According to some studies, the risk of miscarriage is higher if the father is over 35 years old, and the older the age, the higher the risk.
Women over 35 have a higher risk of miscarriage than younger women. At age 35, the risk is about 20%, at age 40, about 40%, and at age 45, about 80%. The age of the father may also play a role. According to some studies, the risk of miscarriage is higher if the father is over 35 years old, and the older the age, the higher the risk.
More than two miscarriages in the past. The risk of miscarriage is higher in women who have had two or more miscarriages. After one miscarriage, the risk of another is the same as for women who have never had a miscarriage. nine0003
Chronic diseases. Women with chronic conditions, such as thyroid disease or diabetes, are at a higher risk of miscarriage.
Pathology of the uterus or cervix. Certain uterine pathologies and a weak or short cervix increase the risk of miscarriage.
Smoking, alcohol and drug use. Women who smoke or drink alcohol during pregnancy have a higher risk of miscarriage than women who do not smoke or drink alcohol.