Birth trauma ptsd
What is Birth Trauma? - Birth Trauma Association
Birth trauma is a shorthand phrase for post-traumatic stress disorder (PTSD) after childbirth. We also use it for women who have some symptoms of PTSD, but not enough for a full diagnosis.
PTSD was first identified amongst soldiers returning from the Vietnam War, and most people still think of it as a condition experienced by soldiers. In fact, PTSD can follow any traumatic event – such as being in a car accident, being sexually abused or having a very difficult birth. It can also happen to people who have witnessed a traumatic event, so people who have seen someone else violently killed, for example, often experience PTSD. This is why some partners, and even midwives, experience PTSD after seeing a traumatic birth.
In most cases, what makes birth traumatic is the fear that you or your baby are going to die. We very often see birth trauma in women who have lost a lot of blood, for example, or who had to have an emergency caesarean because their baby’s heartrate suddenly dipped.
You can download our leaflet on coping with a difficult birth here.
Symptoms of birth trauma (postnatal PTSD)
There are four main symptoms:
- Re-experiencing the traumatic event through flashbacks, nightmares or intrusive memories. These make you feel distressed and panicky.
- Avoiding anything that reminds you of the trauma. This can mean refusing to walk past the hospital where you gave birth, or avoiding meeting other women with new babies.
- Feeling hypervigilant: this means that you are constantly alert, irritable and jumpy. You worry that something terrible is going to happen to your baby.
- Feeling low and unhappy (“negative cognition” in the medical jargon). You may feel guilty and blame yourself for your traumatic birth. You may have difficulty remembering parts of your birth experience.
Not everyone who has had a traumatic experience suffers from PTSD, but many do. It’s a completely normal response, and not a sign of weakness.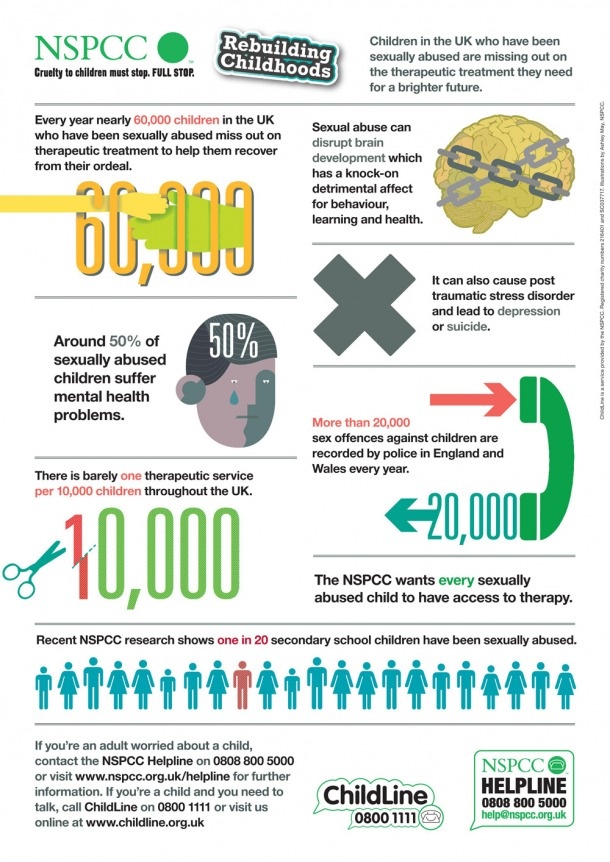 It’s also involuntary: brain scans show a difference between the brains of people with PTSD and those without. PTSD is not something that can be cured by “pulling yourself together” or “focusing on the positive,” despite what other people tell you.
It’s also involuntary: brain scans show a difference between the brains of people with PTSD and those without. PTSD is not something that can be cured by “pulling yourself together” or “focusing on the positive,” despite what other people tell you.
Who gets birth trauma?
Some women experience events during childbirth (as well as in pregnancy or immediately after birth) that would traumatise any normal person.
For other women, it is not always the sensational or dramatic events that trigger childbirth trauma but other factors such as loss of control, loss of dignity, the hostile attitudes of the people around them, feelings of not being heard or the absence of informed consent to medical procedures.
There is still a lot of research to be done, but some of the factors that make birth trauma more likely are:
- Lengthy labour or short and very painful labour
- Induction
- Poor pain relief
- Feelings of loss of control
- High levels of medical intervention
- Forceps births
- Emergency caesarean section
- Impersonal treatment or problems with staff attitudes
- Not being listened to
- Lack of information or explanation
- Lack of privacy and dignity
- Fear for baby's safety
- Stillbirth
- Birth of a baby with a disability resulting from a traumatic birth
- Baby’s stay in the special care baby unit or neonatal intensive care unit
- Poor postnatal care
- Previous trauma (for example, in childhood, with a previous birth or domestic violence)
Finally, people who witness their partner’s traumatic childbirth experience may also feel traumatised as a result.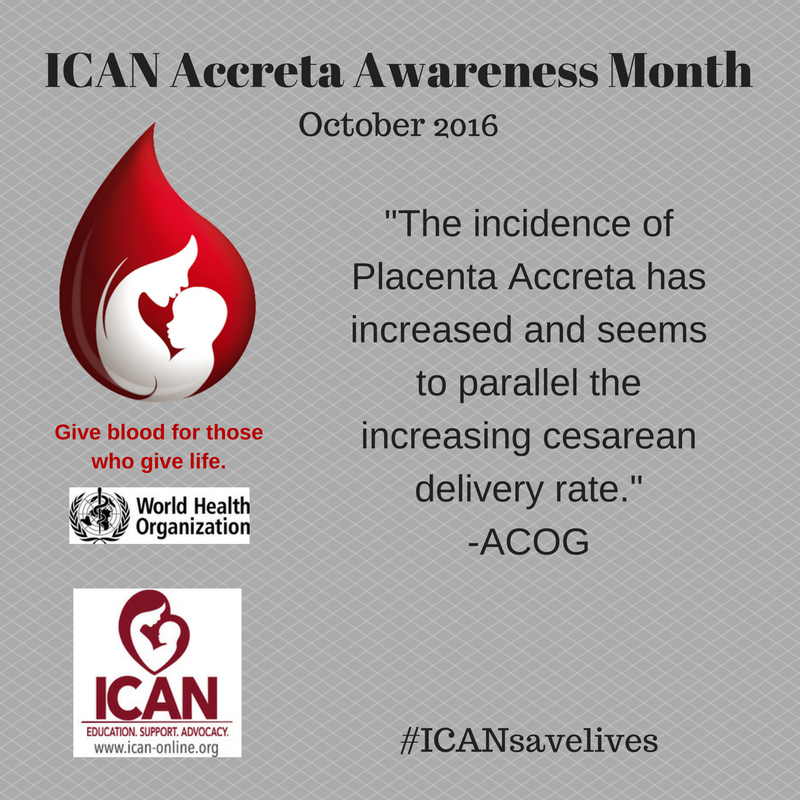 See our partners page for more information.
See our partners page for more information.
What is different about birth trauma?
Women affected by birth trauma often find that there is nowhere to turn for support because even other mothers who have not had traumatising births can find it hard to understand the impact of a traumatic birth. This can make sufferers lonely and depressed as they often feel they are somehow weaker than other women because they are unable to forget their birth experience. They may feel incredibly guilty as a result.
This is a terrible burden to shoulder. The nature of PTSD means it’s impossible to stop constantly thinking about the birth experience, but very few people are aware of this. Even health care professionals don't always understand.
Unfortunately, this lack of support can mean that relationships with friends and family may deteriorate. Many women end up feeling torn between their desire for more children and their determination to avoid another pregnancy. They may also lose interest in sex and these problems can place a great strain on relationships.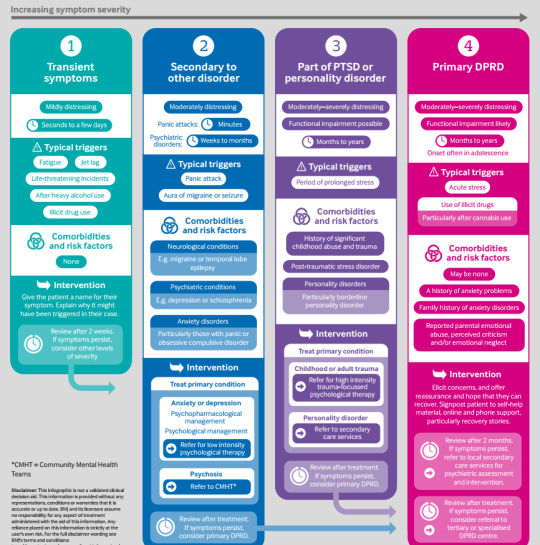
Some women also avoid any medical intervention that reminds them of their birth experience, such as smear tests.
For many women, their greatest concern is the day-to-day difficulties they encounter bonding with their baby who they see as a constant reminder of the trauma they have experienced.
The BTA aims to tackle this isolation by offering women much needed support and showing them that they are far from alone. By working together and providing women with a voice, we hope that we can help change those practices that contribute to birth trauma
What’s the difference between birth trauma and postnatal depression?
Birth trauma can overlap with postnatal depression (PND) as some of the symptoms are the same, but the two illnesses are distinct and need to be treated individually.
Unfortunately, many women are wrongly diagnosed with PND and are prescribed medication that may do little, or nothing, to help their situation. Women tell us that they are frequently told by their health care professionals that they should try and move on with their lives or that they should just be grateful that they have a healthy baby.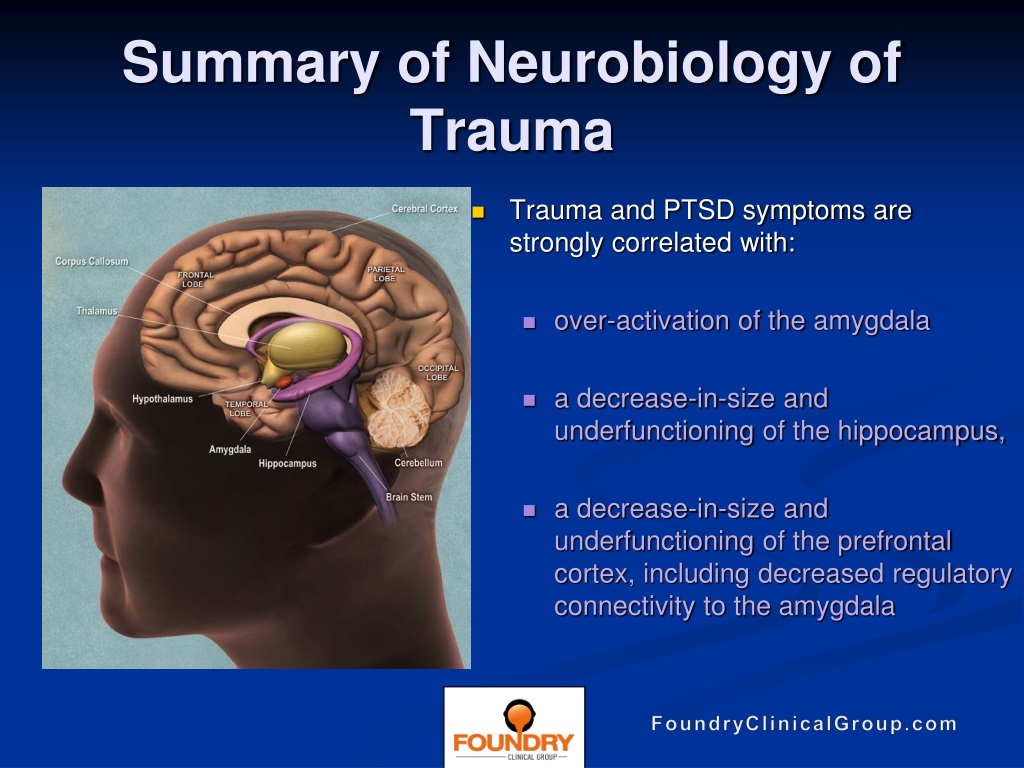 This can exacerbate the feelings of guilt and isolation that women already feel. Women may then end up with prescriptions for anti-depressants, simply because doctors do not understand the disorder.
This can exacerbate the feelings of guilt and isolation that women already feel. Women may then end up with prescriptions for anti-depressants, simply because doctors do not understand the disorder.
Sometimes PND can go hand in hand with birth trauma, however, and in those cases anti-depressants may be appropriate. If you are concerned that you have been misdiagnosed, do speak to your GP or health visitor. Please show them a copy of our leaflet if they appear to be unaware of birth trauma or the fact that it requires specialised treatment.
The Mothers Who Get PTSD From Childbirth
Health
For some women, the psychological toll of childbirth leads to a form of PTSD—distinct from postpartum depression—that follows them into new motherhood.
By Ilana E. StraussMaxim Shemetov / ReutersWhenever Sarah sees a Facebook post of a smiling friend holding a newborn baby, she breaks down.
It’s not that she dislikes her friends. It’s also not that she envies their motherhood; Sarah has her own healthy baby girl. But she doesn’t have her own postcard-perfect photo like that, capturing the first moments of a new family’s joy. What she has instead are memories that continue to haunt her.
Sarah, a 28-year-old mother from Nebraska, suffers from postpartum post-traumatic stress disorder. Many people, including doctors, confuse postpartum PTSD with postpartum depression, even though the two disorders are quite different: Mothers with postpartum depression generally don’t suffer from the intrusive memories and flashbacks that plague PTSD sufferers. Instead, they most commonly deal with things like sadness, trouble concentrating, difficulty finding joy in activities they once enjoyed, and difficulty bonding with their infants. Postpartum depression is also unique to new mothers, but any traumatic experience can bring on PTSD.
In 2014, Sarah had a traumatic birth, in which her firstborn daughter was born prematurely and had to go to the neonatal intensive-care unit (NICU). The experience took a psychological toll: For months after the birth, Sarah would lie awake at night, suffering through flashbacks of the experience. Sometimes, she’d burst out crying in public.
The experience took a psychological toll: For months after the birth, Sarah would lie awake at night, suffering through flashbacks of the experience. Sometimes, she’d burst out crying in public.
Her condition is more similar to the PTSD experienced by veterans than it is to postpartum depression. Postpartum PTSD sufferers like Sarah experience typical PTSD symptoms like hyper-vigilance, intrusive memories, flashbacks, severe emotional distress, irritability, trouble sleeping, and nightmares, explains Anastasia Pollock, a therapist who specializes in treating trauma. Mothers who suffer from PTSD often end up structuring their lives around their disorder, doing everything they can to avoid triggers that remind them of their trauma.
The traumatic experience can come before or during pregnancy, like a bad reaction to fertility treatment or severe morning sickness, explains Jennifer Zimmerman, the cofounder of Solace for Mothers, an organization that helps women to emotionally heal after traumatic childbirths.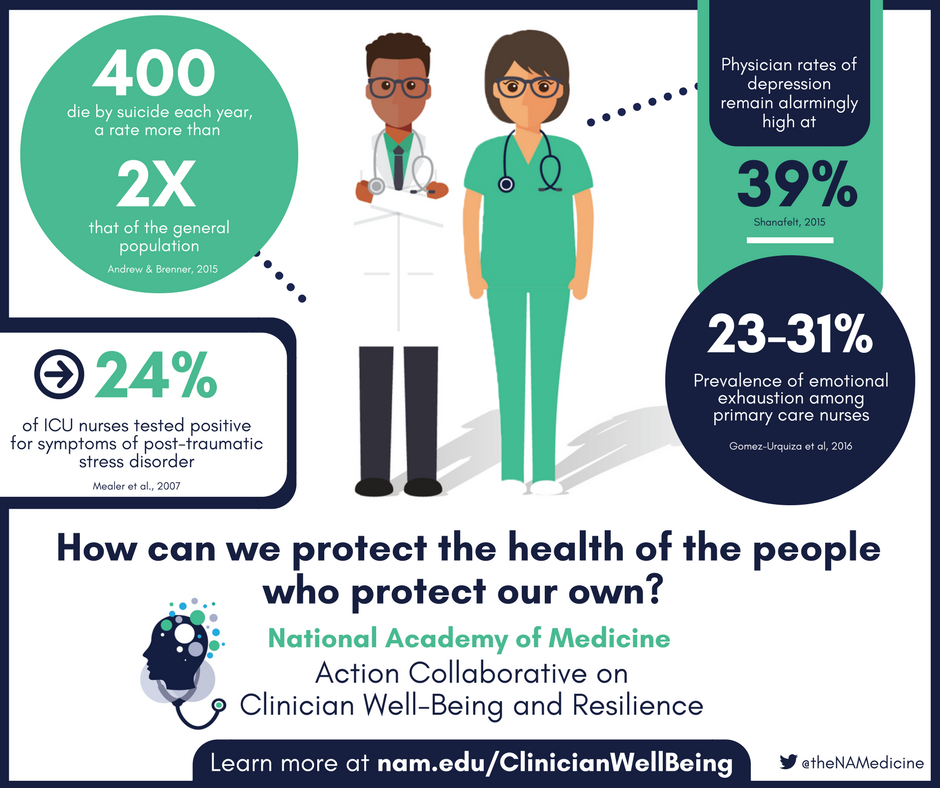
Other times, it can come during labor and delivery: When a newborn has a medical problem, as Sarah’s did, or when a woman feels coerced into undergoing invasive procedures during the birthing process. An experience that may not be a big deal to some women may be traumatic for others, Zimmerman explains:
“What looks like a normal labor and delivery to the outsider can be experienced as traumatic to her.”
* * *
The psychology behind developing PTSD is complicated, but it frequently has a lot to do with expectations. Mothers often don’t anticipate having a problematic birth, so when it happens, it can leave lasting psychological scars.
That certainly seemed to be the case with Sarah.
She had a relatively easy pregnancy—but in her 33rd week, while waiting in the car for her husband to bring her ice cream, her water broke unexpectedly. Her husband rushed her to the hospital, where a whirlwind of doctors and nurses ran tests in the birthing room. A doctor said her baby had underdeveloped lungs.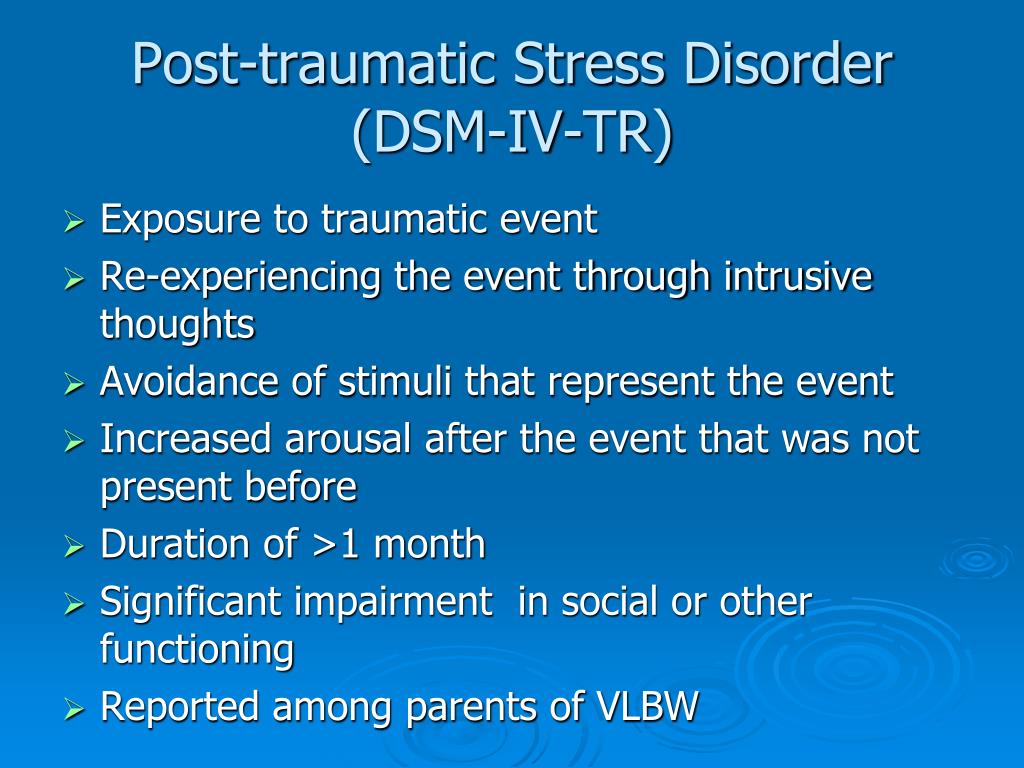
When it came time for Sarah to deliver, the doctors wheeled her out of the birthing room and into a room on the NICU floor so that her newborn could be treated immediately.
Once she gave birth, the doctors whisked the baby girl away before Sarah could hold her, and her husband rushed off with them.
At that moment, Sarah told me, she remembered a couple in her birthing class that had planned the trendiest birth possible, complete with hypnotherapy and a birthing pool. At the time, she had laughed at the idea; now she envied them.
“I didn’t care about low lighting, I didn’t care about Enya playing in the background,” remembers Sarah. “I just wanted to see my daughter when she was born, and I wanted to see my husband’s face. And I didn’t get either."
The doctor cleaned Sarah up, brought her back to her room, and left her alone.
“It was grief and fear when it should have been joy and excitement,” she says.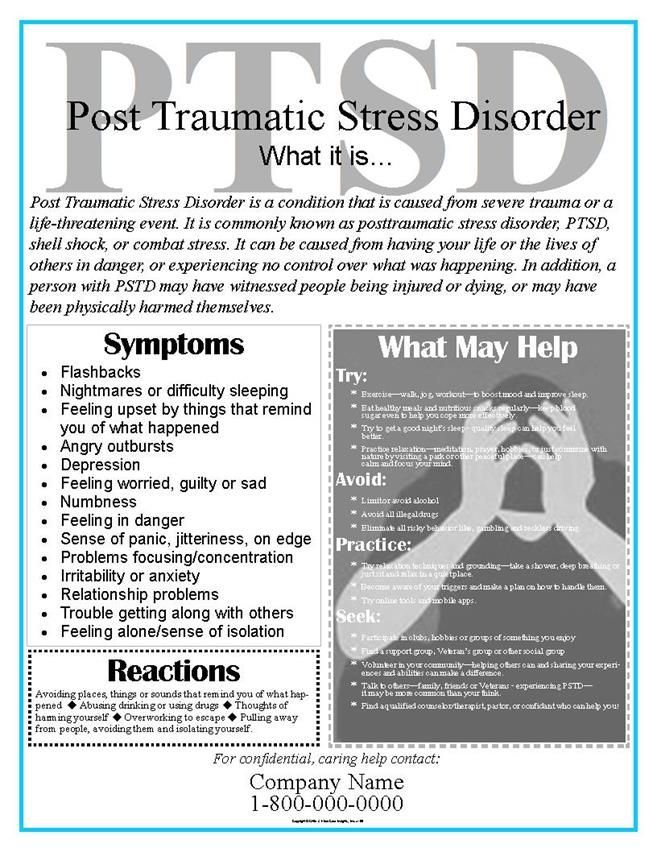 “And it was emptiness.”
“And it was emptiness.”
A couple of hours later, nurses finally wheeled Sarah back to the NICU to see her daughter. At the sight of her baby—wires everywhere, a tube in her mouth—she felt a wave of intense melancholy. She started stroking her daughter, Eloise, but a nurse told her she was doing it wrong, she recalls—the touch was too rough for newborn skin. I can’t even touch my baby right, she thought.
A few days later, after Sarah had been discharged from the hospital, she was finally allowed to hold her daughter for the first time, though she couldn’t yet take her home from the NICU. From then on, Sarah says, she came in every day to hold her daughter for hours, sometimes with her husband but often alone. She lived off the bagels and oatmeal the hospital provided. Nurses eventually told to go home and take care of herself, a task that would turn out to be more difficult than she realized.
* * *
When a person goes through trauma, the mind goes into an unusually hyper-aroused, fight-or-flight state, explains Sharon Dekel, an instructor at Harvard Medical School who is currently researching postpartum PTSD.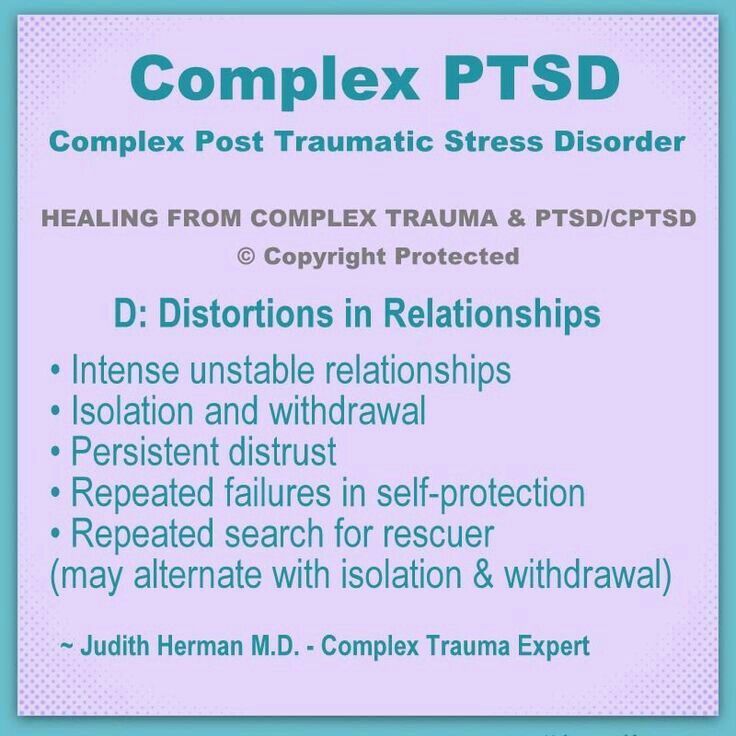 The brain’s amygdala, which normally helps store memories, becomes hyper-responsive, leading to an exaggerated sense of fear. Parts of the brain that normally inhibit the amygdala stop working. When something reminds a sufferer of her traumatic experience, her unusually terrifying memories feel like more than memories; they feel like they’re still happening.
The brain’s amygdala, which normally helps store memories, becomes hyper-responsive, leading to an exaggerated sense of fear. Parts of the brain that normally inhibit the amygdala stop working. When something reminds a sufferer of her traumatic experience, her unusually terrifying memories feel like more than memories; they feel like they’re still happening.
Four months after Eliose’s birth, Sarah’s niece was born prematurely and ended up in the NICU. Visiting her at the hospital, she saw the baby hooked up to all the same machines her daughter had been. When Sarah was out of sight of her brother and sister-in-law, she collapsed into her husband, sobbing.
“It all came back,” Sarah says. That’s when she realized something wasn’t right. Sarah began experience anxiety, flashbacks, and other PTSD symptoms, even bursting out crying in her church group.
“I have never gotten over being terrified that my daughter will stop breathing,” she said.
Now, anything that sounds like a monitor—an alarm clock, an oven alarm—puts her brain in panic mode.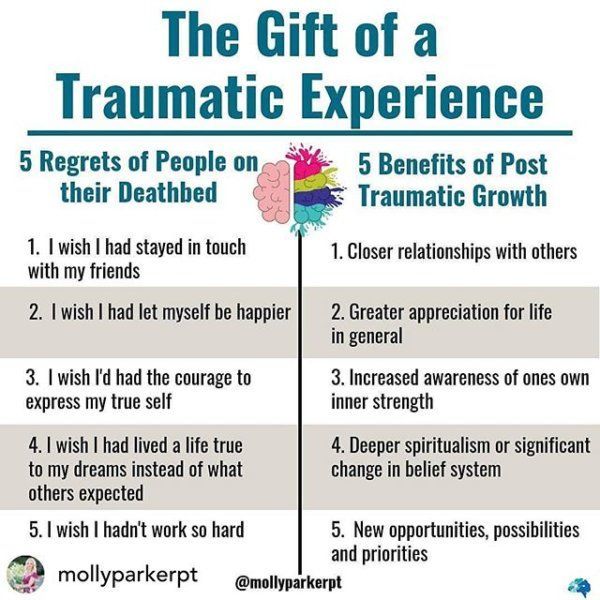
The fear is common among women suffering from postpartum PTSD. After her son was born prematurely and rushed to the NICU in 2011, Alicia, a first-time mother, grew “paranoid to pieces,” she says. Thanks to his precarious birth, she was constantly stuck in a mental moment where she felt like her son was in danger. For 14 months after he was born, she was too afraid of outdoor hazards to bring her son out of her house. When she finally mustered up the courage to take him with her to Walmart, she had a panic attack when a shopper sneezed.
She had to get rid of her coffee maker because it sounded too much like one of the hospital machines.
* * *
Having a particularly complicated birth, such as one when the baby ends up in the NICU, makes postpartum PTSD more likely, but even mothers who have troublesome childbirths usually don’t develop the disorder.
Dekel says personal history may be one reason why some women are more susceptible than others. A woman who has experienced trauma in the past, such as sexual abuse, is much more likely to get postpartum PTSD.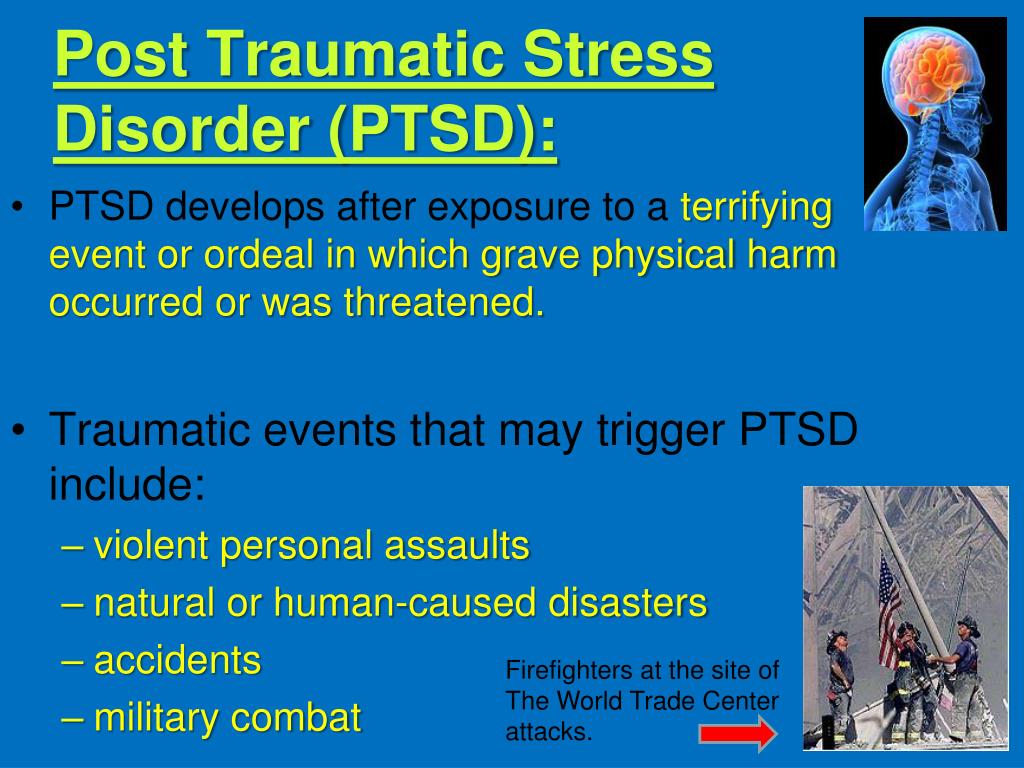 She also believes that neurohormonal factors could be involved, though research is still fuzzy.
She also believes that neurohormonal factors could be involved, though research is still fuzzy.
No one knows for sure how common the condition actually is: According to Dekel, an estimated 1-3 percent of new mothers suffer from full-blown postpartum PTSD, but around 25 percent have one or more symptoms of it. Other researchers estimate that postpartum PTSD may affect up to 17 percent of new mothers.
While there’s been plenty of research on PTSD in veterans, literature on postpartum PTSD is sparse; doctors only began researching the disorder around 2006.
It’s hard to say why postpartum PTSD has gone unstudied for so long, though both Dekel and Pollock suspect that stigma may have something to do with it: Mothers have kept their symptoms to themselves, and so the condition has remained largely invisible. Pollock has one client in her 70s who has been carrying around her PTSD since she had her baby over 40 years ago. She only started getting treatment recently.
When your own child is an emotional trigger, bonding can be all but impossible.
And because doctors only started recognizing postpartum PTSD recently, many women who have the condition aren’t diagnosed. Doctors can be quick to label suffering mothers with the better-known postpartum depression instead.
The good news: Research on the topic has been gaining speed in the last five years. Dekel is currently following a large number of women through pregnancy and beyond, hoping to identify factors that could lead to postpartum PTSD. Eventually, she hopes that mothers will be able to know their risk before giving birth.
“When we know more, we can offer better treatment,” Dekel explains. She stresses that treatment is not just important for mothers. It matters for their children, too—when your own child is an emotional trigger, bonding can be all but impossible.
* * *
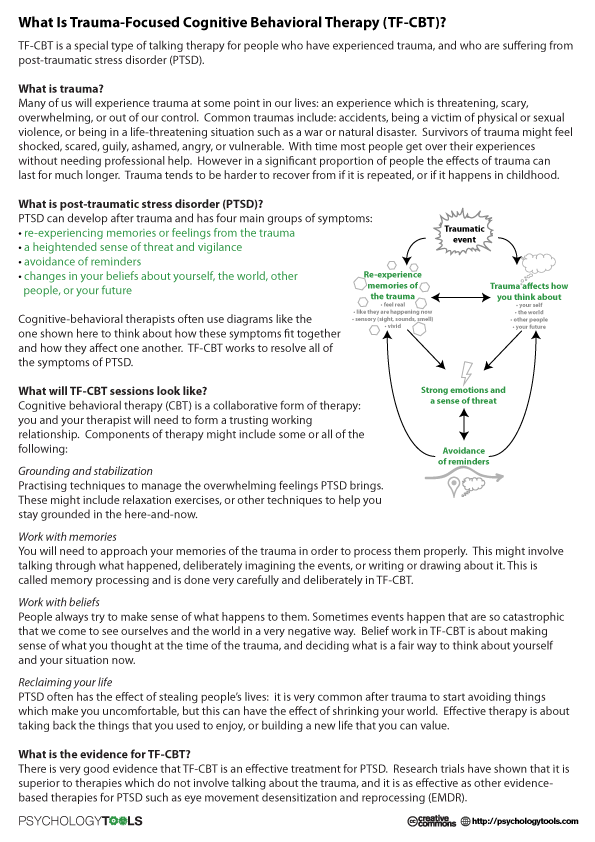
Postpartum PTSD is generally treated like any other type of PTSD, with therapy, peer support groups, and medication. Zimmerman points out that many women she works with also seek alternative therapies, such as healing through writing, art, music, or dance.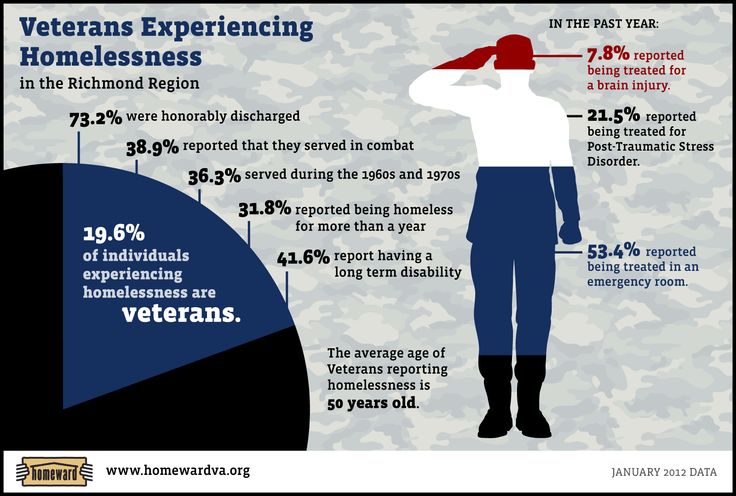
“Each woman’s path to healing is unique, and there is no one thing that works for everyone,” says Zimmerman. “It can be a process of trial and error to find what may relieve one’s symptoms, and often it just takes time to heal."
Pollock prefers to treat her PTSD patients with EMDR, a new treatment that has shown promising preliminary results. In this treatment, patients think about the source of their trauma while Pollock does things like tap on their knees and play beats, which helps patients’ brains remember that they’re in the present, not the world of their flashbacks. This helps their brains come “back online,” she says, to reinterpret their memories and put them where they belong: in the past.
“It helps them think “I’m here and now, not there and then,” explains Pollock.
Pollock treats both women with postpartum PTSD and veterans with PTSD, and she uses EMDR for both. But she also helps new mothers bond with their infants and find a new normal. While soldiers can leave combat behind, new mothers can’t just avoid triggers by avoiding their children.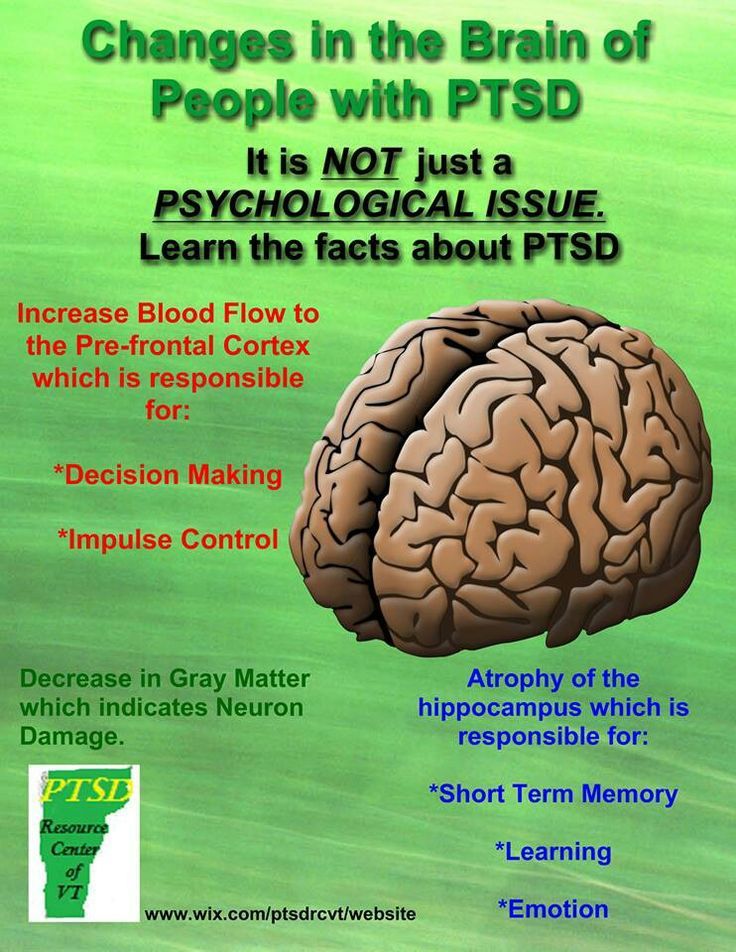
Since getting diagnosed and starting therapy, Sarah says, she’s been slowly improving. Sleeping is still tough, and she still gets regular flashbacks, but she’s better equipped to react to them—they consume her mind for a few seconds, rather than a few hours.
Recently, she joined a Facebook group for mothers whose babies had been in the NICU. It made her feel better to know there are other women out there who had the same experience.
“I just think about how hard it’s been for me,” she says, “and I’m one of the lucky ones.”
Birth trauma of newborns. What is birth trauma in newborns?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Birth trauma of newborns - various injuries to the fetus that occur during the birth act.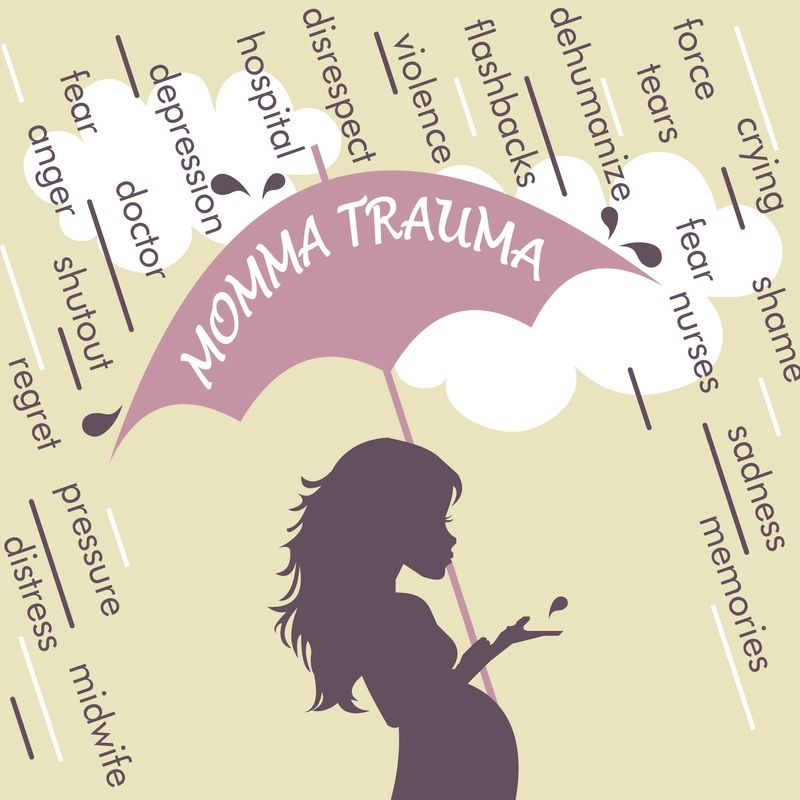 Among the birth injuries of newborns, there are injuries to soft tissues (skin, subcutaneous tissue, muscles), the skeletal system, internal organs, and the central and peripheral nervous systems. Birth trauma in newborns is diagnosed taking into account the mother's obstetric and gynecological history, characteristics of the course of labor, examination data of the newborn and additional studies (EEG, ultrasound, radiography, ophthalmoscopy, etc.). Treatment of birth injuries of newborns is carried out differentially, taking into account the type and severity of the injury. nine0006
Among the birth injuries of newborns, there are injuries to soft tissues (skin, subcutaneous tissue, muscles), the skeletal system, internal organs, and the central and peripheral nervous systems. Birth trauma in newborns is diagnosed taking into account the mother's obstetric and gynecological history, characteristics of the course of labor, examination data of the newborn and additional studies (EEG, ultrasound, radiography, ophthalmoscopy, etc.). Treatment of birth injuries of newborns is carried out differentially, taking into account the type and severity of the injury. nine0006
- Classification of birth injuries of newborns
- Causes
- Different types of neonatal injuries
- Birth injuries of soft tissues
- Birth injuries of the skeletal system
- Birth injuries of internal organs
- Birth injuries of the central and peripheral nervous system
- Prophylaxis
- Prices for treatment
General
Under the birth trauma of newborns understand the violation of the integrity of the tissues or organs of the child, due to the mechanical forces acting in the process of childbirth. Birth injuries are diagnosed in 8-11% of newborns. Birth injuries of newborns are often combined with birth injuries of the mother (ruptures of the vulva, vagina, perineum, uterus, urogenital and vagina-rectal fistulas, etc.). Birth injuries of newborns can have a serious impact on the further physical health and intellectual development of the child. All this makes birth traumatism one of the most urgent problems of obstetrics and gynecology, neonatology and pediatrics, pediatric neurology and traumatology. nine0006
Birth injuries are diagnosed in 8-11% of newborns. Birth injuries of newborns are often combined with birth injuries of the mother (ruptures of the vulva, vagina, perineum, uterus, urogenital and vagina-rectal fistulas, etc.). Birth injuries of newborns can have a serious impact on the further physical health and intellectual development of the child. All this makes birth traumatism one of the most urgent problems of obstetrics and gynecology, neonatology and pediatrics, pediatric neurology and traumatology. nine0006
Birth trauma in newborns
Classification of birth injuries of newborns
Depending on the location of the damage and the predominant dysfunction, the following types of birth trauma of newborns are distinguished:
1. Birth injuries of soft tissues (skin, subcutaneous tissue, muscles, birth tumor, cephalohematoma).
2. Birth injuries of the osteoarticular system (cracks and fractures of the clavicle, humerus and femurs; traumatic epiphyseolysis of the humerus, subluxation of the C1 and C2 joints, damage to the bones of the skull, etc.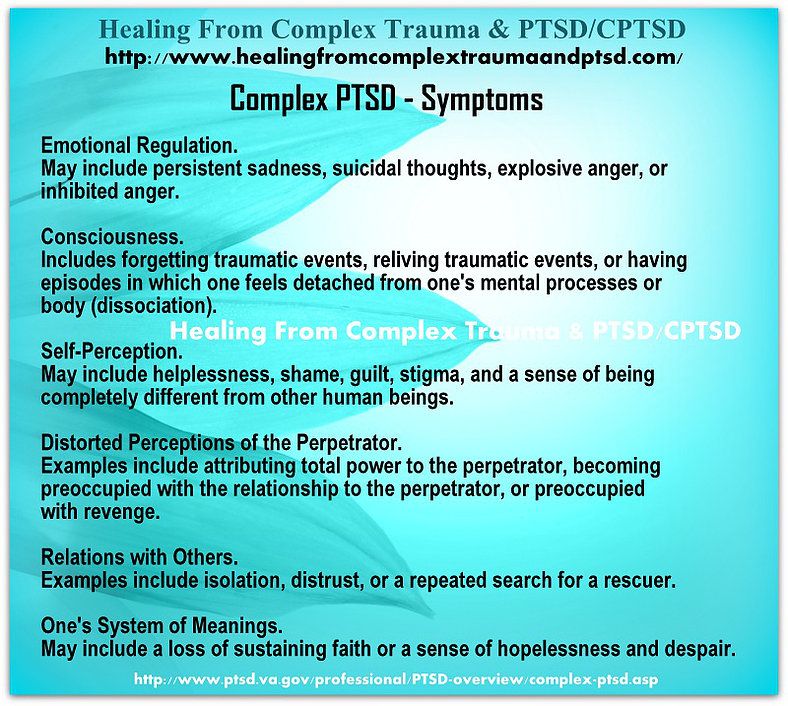 ). nine0006
). nine0006
3. Birth injuries of internal organs (hemorrhages in internal organs: liver, spleen, adrenal glands).
4. Birth injuries of the central and peripheral nervous system in newborns:
- intracranial birth trauma (epidural, subdural, subarachnoid, intraventricular hemorrhages)
- birth injury of the spinal cord (bleeding into the spinal cord and its membranes)
- birth injury of the peripheral nervous system (damage to the brachial plexus - Duchenne-Erb paresis/paralysis or Dejerine-Klumpke palsy, total paralysis, paresis of the diaphragm, damage to the facial nerve, etc.). nine0012
Causes
An analysis of the causes of birth trauma in newborns allows us to identify three groups of factors that increase the likelihood of its occurrence: those related to the mother, to the fetus, as well as to the course and management of childbirth.
Predisposing "maternal" factors may be early or late reproductive age, gestosis, narrow pelvis, hypoplasia or hyperanteflexia of the uterus, diseases of the pregnant woman (cardiovascular, endocrine, gynecological, etc.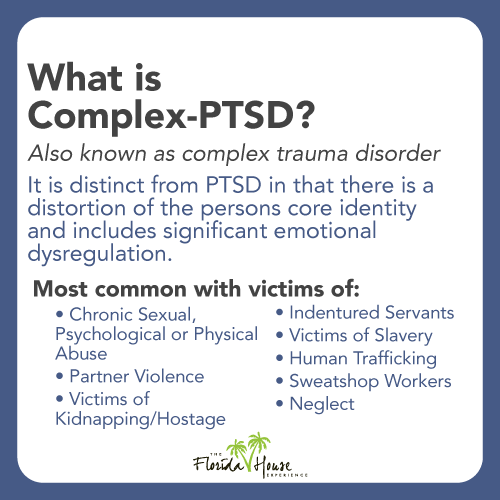 ), post-term pregnancy, occupational hazards, etc. nine0006
), post-term pregnancy, occupational hazards, etc. nine0006
The most extensive group of causes leading to birth trauma in newborns is the circumstances associated with the fetus. Birth injury can be provoked by breech presentation of the fetus, oligohydramnios, incorrect (asynclitic or extensor insertion of the head), prematurity, large fetal size, fetal abnormalities, intrauterine hypoxia and asphyxia, etc.
Anomalies of labor activity can lead to the birth trauma of a newborn: prolonged or rapid labor, labor stimulation with weak labor activity, discoordinated or excessively strong labor activity. A serious group of causes of birth injuries in newborns is the incorrect or unreasonable use of obstetric aids (turning the fetus on a leg, applying obstetric forceps, using a vacuum extractor, performing a caesarean section, etc.). nine0006
As a rule, when birth injuries occur in newborns, there is a combination of a number of adverse factors that disrupt the normal biomechanics of childbirth.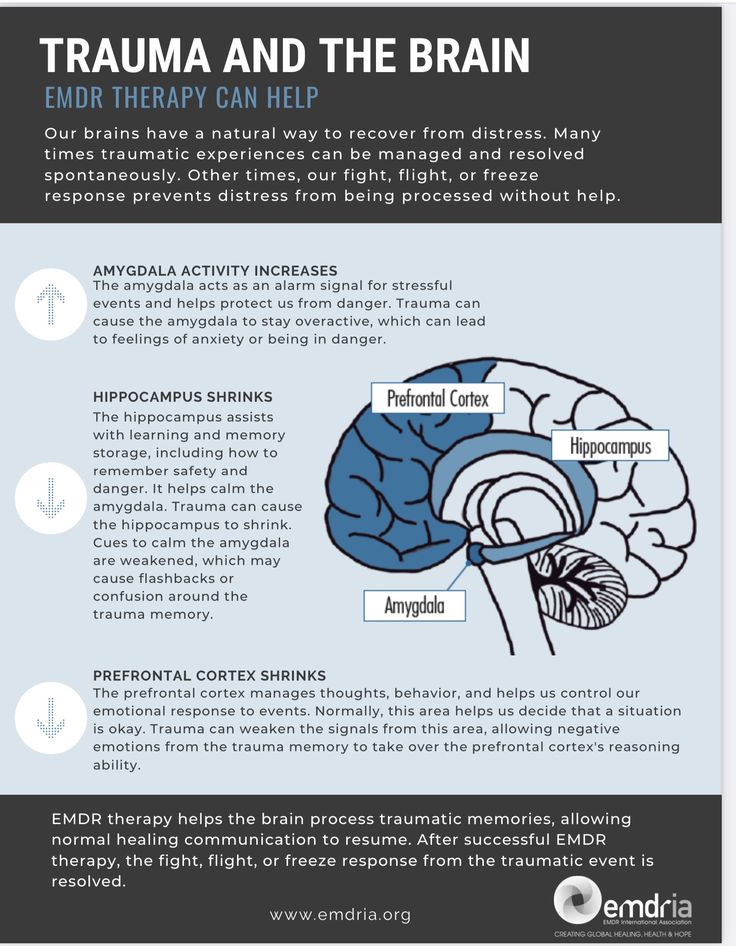
Various types of neonatal injuries
Birth injuries of soft tissues
The most common manifestations of birth trauma in newborns are damage to the skin and subcutaneous tissue. These include scratches, abrasions, petechiae, ecchymosis in various parts of the body. Such damage is detected during a visual examination of the newborn by a neonatologist; usually they are not dangerous and require only local antiseptic treatment and the application of an aseptic dressing. Minor birth injuries of soft tissues disappear by the end of the first week of a newborn's life. nine0006
A type of birth trauma in newborns is a birth tumor, which is characterized by local swelling of the soft tissues of the head. The birth tumor has a soft elastic consistency, cyanotic color with multiple petechiae and ecchymosis. Its occurrence is usually associated with prolonged labor in the cephalic presentation or the imposition of obstetric forceps. The birth tumor does not require treatment, it disappears on its own after 1-3 days.
A more severe type of birth injury in newborns is damage (hemorrhage, rupture) of the sternocleidomastoid muscle, usually its lower third. In this case, a small tumor of moderately dense or doughy consistency is determined at the site of damage. Damage to the sternocleidomastoid muscle may not be detected immediately, but after about a week, when the child develops torticollis. In the treatment of a birth injury of the sternocleidomastoid muscle in newborns, a corrective head position is used with the help of rollers, dry heat, potassium iodide electrophoresis, massage; in case of inefficiency - surgical correction. nine0006
Cephalhematoma, as a kind of birth trauma of newborns, is characterized by hemorrhage under the periosteum of the parietal or occipital bones of the skull. Typical signs of cephalohematoma are an elastic consistency, absence of pulsation, painlessness, fluctuation, and the presence of a roller along the periphery. In the future, newborns with cephalohematoma may experience jaundice caused by increased extravascular production of bilirubin. Cephalhematoma decreases in size by 2-3 weeks of life, and completely resolves by the end of 6-8 weeks. Complications of subperiosteal birth trauma of newborns include anemia, calcification and suppuration of cephalohematoma. Children with large (more than 6 cm in diameter) cephalohematomas need an X-ray of the skull to rule out bone fractures. Since cephalohematomas in premature babies are often associated with intrauterine mycoplasmosis, PCR or ELISA diagnostics is required. nine0006
Cephalhematoma decreases in size by 2-3 weeks of life, and completely resolves by the end of 6-8 weeks. Complications of subperiosteal birth trauma of newborns include anemia, calcification and suppuration of cephalohematoma. Children with large (more than 6 cm in diameter) cephalohematomas need an X-ray of the skull to rule out bone fractures. Since cephalohematomas in premature babies are often associated with intrauterine mycoplasmosis, PCR or ELISA diagnostics is required. nine0006
In most cases, birth injuries of soft tissues in newborns pass without consequences.
Birth injuries of the skeletal system
Among birth injuries of the osteoarticular system in newborns, injuries of the clavicle and bones of the extremities are more common. They always refer to purely obstetric types of damage. Subperiosteal fractures of the clavicle without displacement are usually detected 3-4 days after delivery by the presence of a fusiform dense swelling - forming callus.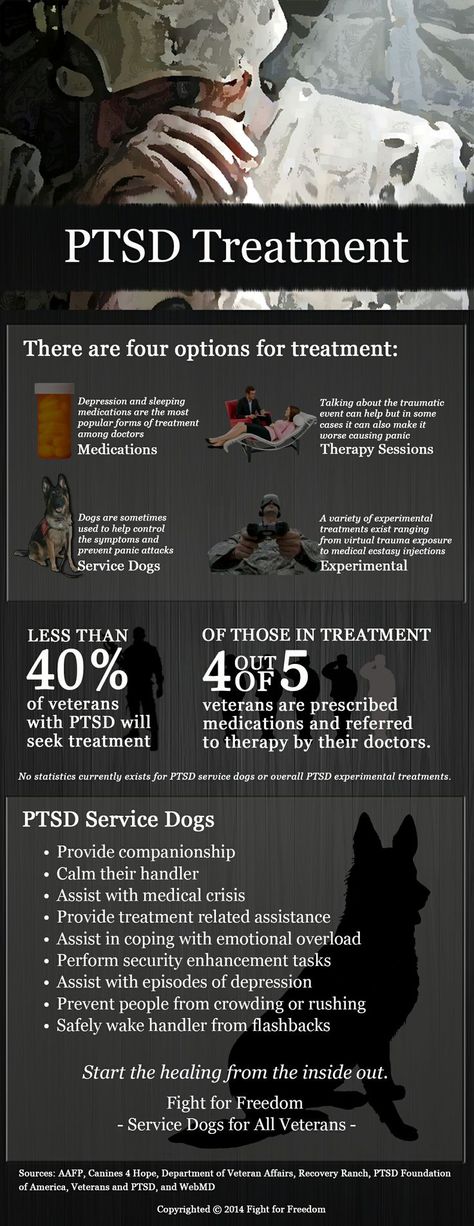 A fracture of the clavicle with displacement is accompanied by the inability to perform active movements, pain, crying with passive movement of the arm, swelling and crepitus over the fracture site. nine0006
A fracture of the clavicle with displacement is accompanied by the inability to perform active movements, pain, crying with passive movement of the arm, swelling and crepitus over the fracture site. nine0006
With a fracture of the humerus or femur, there are no active movements in the limbs, there is a pain reaction to passive movements, there is swelling, deformity and shortening of the damaged limb. For all types of fractures, newborns need to consult a pediatric traumatologist, conduct x-ray diagnostics (radiography of the collarbone, radiography of tubular bones). In case of a clavicle fracture, a short-term immobilization of the arm is performed by applying a Dezo bandage or tight swaddling. In case of fractures of the humerus and femur, the bones of the upper or lower limb are repositioned and a plaster cast is applied (if necessary, traction). nine0006
A type of birth trauma of the skeletal system of newborns is traumatic epiphysiolysis of the humerus.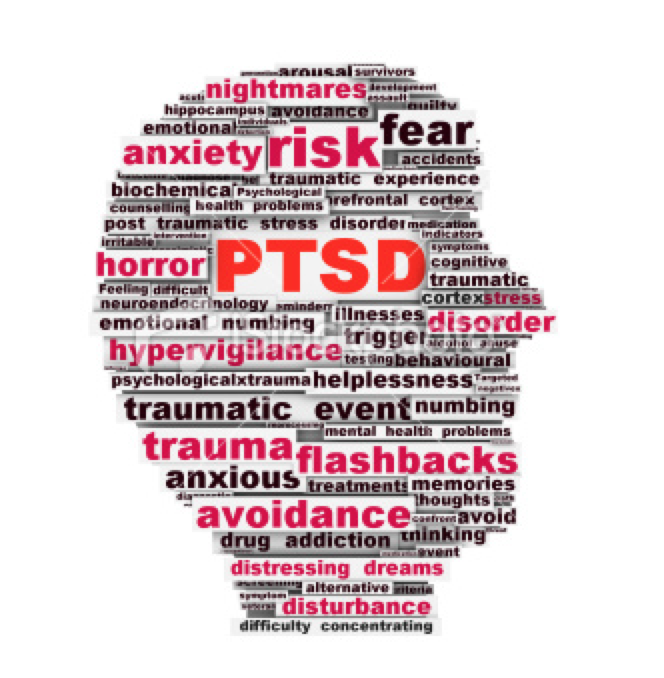 Its manifestations are pain, swelling and crepitus in the area of the shoulder or elbow joints, limited range of motion in the affected arm. The outcome of such an injury may be paresis of the radial nerve, the formation of flexion contracture in the joints. Treatment consists of immobilization of the limb, physiotherapy, massage.
Its manifestations are pain, swelling and crepitus in the area of the shoulder or elbow joints, limited range of motion in the affected arm. The outcome of such an injury may be paresis of the radial nerve, the formation of flexion contracture in the joints. Treatment consists of immobilization of the limb, physiotherapy, massage.
Birth injuries of internal organs
Damage to internal organs occurs as a result of mechanical impact on the fetus during an abnormal course of childbirth. The most common hemorrhages are in the liver, spleen and adrenal glands. Clinical manifestations of birth trauma of internal organs in newborns develop on the 3rd-5th day due to internal bleeding. When a hematoma ruptures, abdominal distention occurs, intestinal paresis develops, muscular hypotension (or atony), inhibition of physiological reflexes, arterial hypotension, persistent regurgitation and vomiting. nine0006
If a birth injury of the internal organs is suspected, the newborn is given a survey radiography of the abdominal cavity, ultrasound of the abdominal organs and ultrasound of the adrenal glands.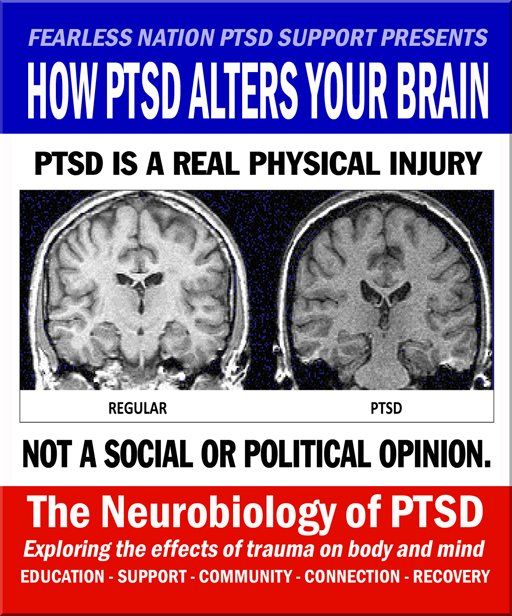 Treatment consists in carrying out hemostatic and symptomatic therapy; if necessary - laparoscopy or laparotomy with revision of internal organs.
Treatment consists in carrying out hemostatic and symptomatic therapy; if necessary - laparoscopy or laparotomy with revision of internal organs.
With a hemorrhage in the adrenal glands, the child may develop acute or chronic adrenal insufficiency. The prognosis for birth trauma of internal organs in newborns is determined by the volume and severity of the lesion, the timeliness of detection of damage. nine0006
Birth injuries of the central and peripheral nervous system
Damage to the nervous system in newborns is the most extensive group of birth injuries. As part of this review, we will focus on birth trauma of the spinal cord and peripheral nervous system; a detailed description of intracranial birth injuries of newborns will be given in the corresponding article.
Birth injuries of the spinal cord in newborns may include hemorrhage, sprain, compression, or rupture of the spinal cord at various levels, associated with or without a spinal fracture.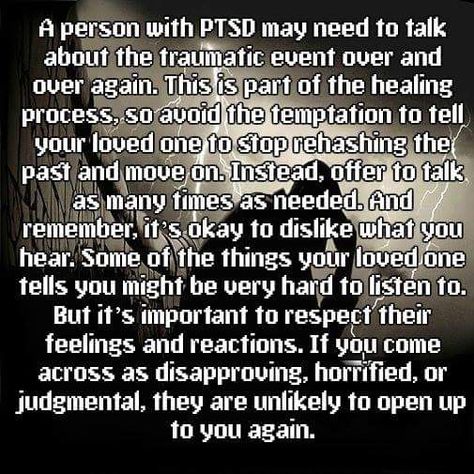 Severe injuries are characterized by the clinic of spinal shock: lethargy, muscular hypotension, areflexia, weak cry, diaphragmatic breathing. The death of children can come from respiratory failure. In more favorable cases, there is a gradual regression of the phenomena of spinal shock; hypotension is replaced by spasticity; autonomic disorders develop (vasomotor reactions, sweating), trophic changes in muscle and bone tissue. Mild birth injuries in newborns are accompanied by transient neurological symptoms: changes in muscle tone, reflex and motor reactions. nine0006
Severe injuries are characterized by the clinic of spinal shock: lethargy, muscular hypotension, areflexia, weak cry, diaphragmatic breathing. The death of children can come from respiratory failure. In more favorable cases, there is a gradual regression of the phenomena of spinal shock; hypotension is replaced by spasticity; autonomic disorders develop (vasomotor reactions, sweating), trophic changes in muscle and bone tissue. Mild birth injuries in newborns are accompanied by transient neurological symptoms: changes in muscle tone, reflex and motor reactions. nine0006
Diagnosis is facilitated by examination of the child by a pediatric neurologist, X-ray or MRI of the spine, electromyography, lumbar puncture, and examination of cerebrospinal fluid. Treatment of a birth injury of the spinal cord in newborns includes immobilization of the damaged area, dehydration and antihemorrhagic therapy, restorative measures (orthopedic massage, exercise therapy, electrical stimulation, physiotherapy).
Birth injuries of the peripheral nervous system in newborns combine damage to the roots, plexuses, peripheral and cranial nerves. nine0006
Given the localization, the paresis of the brachial plexus (obstetric paresis) can be upper (proximal), lower (distal) or total. Upper Duchenne-Erb paresis is associated with damage to the plexuses and roots originating in the C5-C6 segments, which is accompanied by dysfunction of the proximal upper limb. In this case, the child takes a characteristic position with the arm brought to the body, extended at the elbow joint, turned inward at the shoulder and pronated at the forearm; with a hand bent in the palm and a head tilted to the sore shoulder. nine0006
With lower obstetric paresis of Dejerine-Klumpke, plexuses or roots originating from C7-T1 are affected, resulting in dysfunction of the distal arm. Manifestations include muscle hypotonia, hypesthesia, limitation of movements in the wrist and elbow joints, fingers, a symptom of "clawed paw".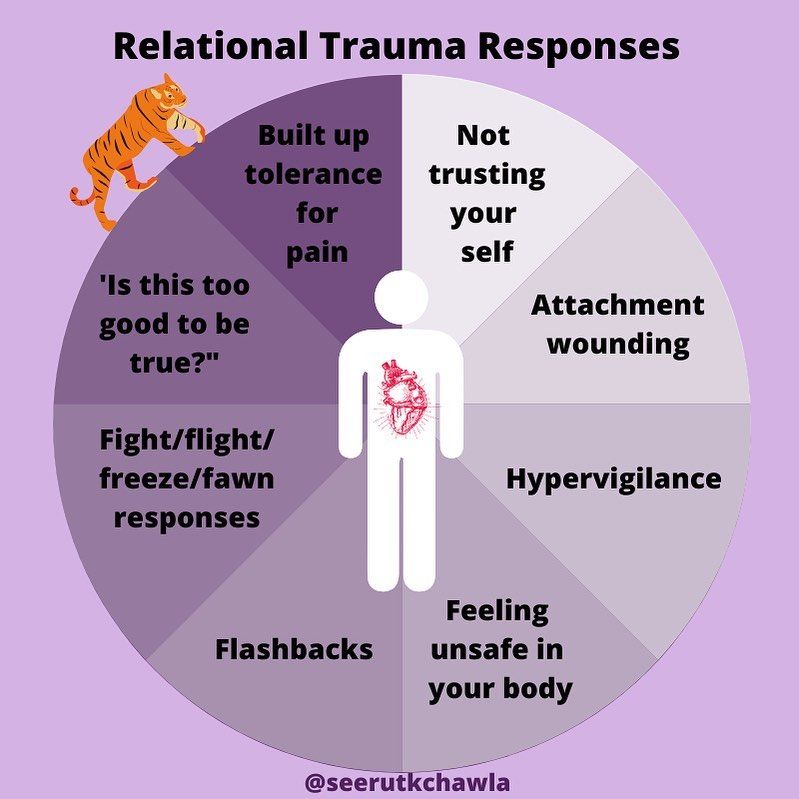 With a total type of obstetric paresis, the arm is completely inactive, muscle hypotension is pronounced, and muscle atrophy develops early.
With a total type of obstetric paresis, the arm is completely inactive, muscle hypotension is pronounced, and muscle atrophy develops early.
Diagnosis and localization of damage is specified using electromyography. Treatment of a birth injury of the brachial plexus in newborns consists in immobilizing the arm with a splint, performing massage, exercise therapy, physiotherapy (ozocerite, paraffin, electrical stimulation, electrophoresis), and drug therapy. nine0006
With paresis of the diaphragm, the newborn develops shortness of breath, paradoxical breathing, cyanosis, bulging of the chest on the affected side. The detection of paresis is facilitated by fluoroscopy and chest x-ray, which determine the high standing and inactivity of the dome of the diaphragm. Against this background, congestive pneumonia can develop in children. Treatment of birth trauma consists of transcutaneous stimulation of the phrenic nerve; if necessary - mechanical ventilation until adequate spontaneous breathing is restored.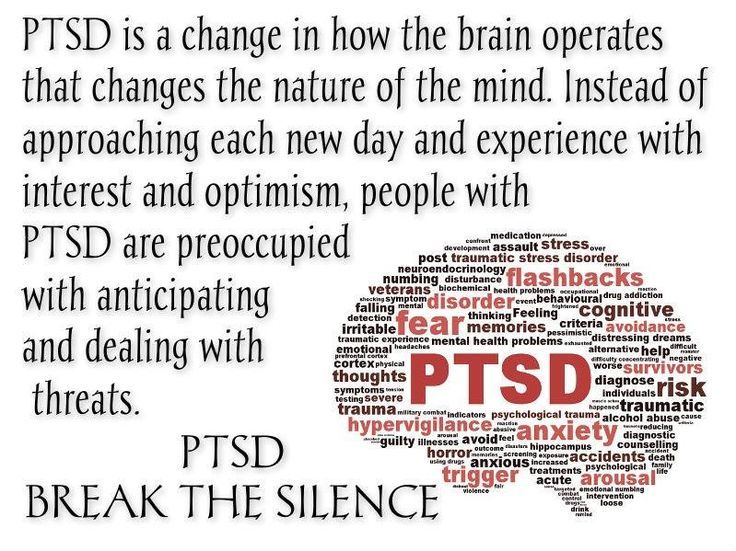 nine0006
nine0006
Paresis of the facial nerve is associated with damage to the trunk or branches of the facial nerve. In this case, the child has facial asymmetry, lagophthalmos, upward displacement of the eyeball when crying, asymmetry of the mouth, and difficulty in sucking. Birth trauma in newborns is diagnosed on the basis of clinical signs, electroneurography, registration of evoked potentials. Often, paresis of the facial nerve resolves without special treatment; in other cases, thermotherapy, drug therapy is carried out. nine0006
Rare types of birth injuries of newborns include injuries of the pharyngeal, median, radial, sciatic, peroneal nerve, lumbosacral plexus.
Prophylaxis
Prevention of birth injuries in newborns involves an assessment of the degree of risk of their occurrence even at the stage of pregnancy, the most careful attitude towards the child during childbirth, the rejection of unreasonable use of benefits for the extraction of the fetus and operative delivery. nine0006
nine0006
Sources
- In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Birth injury. What is birth trauma? nine0001
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.Birth trauma is a collective concept that includes various damage to tissues and organs of a woman in labor or a newborn, caused by the action of birth forces. Among the birth injuries of the mother, there are hematomas, ruptures of the vulva, perineum and vagina, damage to the uterus, the formation of urogenital and enterogenital fistulas, and deformities of the pelvic bones.
 Many birth injuries can be life threatening. Diagnosis of birth injuries is based on external examination, gynecological examination, instrumental methods. Treatment of maternal birth injuries, as a rule, requires emergency surgical assistance and the involvement of narrow specialists (urologists, proctologists, traumatologists). nine0006
Many birth injuries can be life threatening. Diagnosis of birth injuries is based on external examination, gynecological examination, instrumental methods. Treatment of maternal birth injuries, as a rule, requires emergency surgical assistance and the involvement of narrow specialists (urologists, proctologists, traumatologists). nine0006 ICD-10
P10-P15 Birth injury
- Common causes of maternal birth injuries
- Birth injuries of the vulva and vagina
- Vulvar and vaginal hematomas
- Tears of the vulva and vagina
- Birth injuries of the perineum
- Perineal tear symptoms
- Diagnosis and treatment of perineal tears
- Birth trauma of the uterus
- Uterine ruptures
- Classification of uterine ruptures
- Symptoms of uterine rupture
- Uterine rupture emergency
- Cervical tears
- Symptoms of cervical rupture
- Diagnosis and treatment of cervical tears
- Other birth injuries
- Uterine eversion
- Sprains and ruptures of the pelvic joints
- Urogenital and rectovaginal fistulas
nine0011 Prevention of birth injuries
- Prices for treatment
General
Childbirth is a difficult test for the newborn fetus and mother.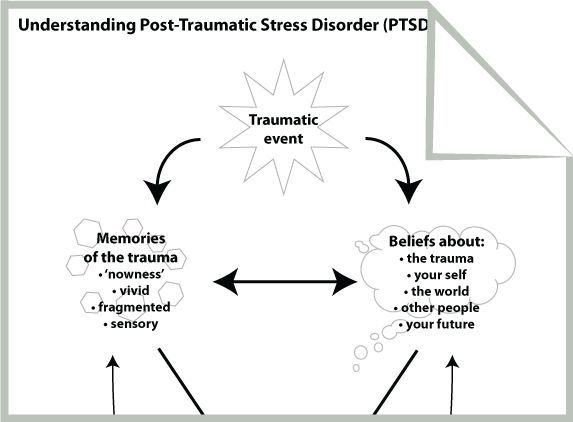 Therefore, after the birth of a child, experts often state the presence of various birth injuries and postpartum disorders in a woman in labor and a newborn. In obstetrics and gynecology, maternal and child birth injuries are distinguished. Birth injuries of a newborn include damage to the peripheral and central nervous systems of various nature and severity, injuries to bones and soft tissues, and internal organs. As part of this review, the main birth injuries that occur in women will be considered. nine0006
Therefore, after the birth of a child, experts often state the presence of various birth injuries and postpartum disorders in a woman in labor and a newborn. In obstetrics and gynecology, maternal and child birth injuries are distinguished. Birth injuries of a newborn include damage to the peripheral and central nervous systems of various nature and severity, injuries to bones and soft tissues, and internal organs. As part of this review, the main birth injuries that occur in women will be considered. nine0006
Significant stretching of the mother's birth canal during childbirth often leads to their damage. These injuries - birth injuries, can be superficial, non-rough in nature (for example, abrasions, cracks) and heal on their own in the early postpartum period, and remain unrecognized. In some cases, birth injuries are so significant that they can lead to serious postpartum complications, disability and even death of a woman. Among birth injuries of the mother there are hematomas; ruptures of the vulva, perineum, vagina, body and cervix; inversion of the uterus; sprains and ruptures of the joints of the pelvis; urogenital and enterogenital fistulas. nine0006
nine0006
Birth injury
Common causes of maternal birth injuries
The variety of variants of maternal birth injuries can be caused by various mechanical and histopathic causes. The mechanical factors in the occurrence of birth injuries include violent or discoordinated labor activity, the provision of operational aids during childbirth (the application of forceps, vacuum extraction of the fetus, manual separation of the placenta, fruit-destroying operations), excessive labor stimulation, irrational management of the straining period, inadequate protection of the perineum, etc. e. Post-term pregnancy, transverse position of the fetus, breech presentation of the fetus, premature birth, narrow pelvis, polyhydramnios, multiple pregnancy, placenta previa can contribute to birth injuries. nine0006
Histopathic causes of birth injuries are due to a burdened obstetric and gynecological history of the woman in labor.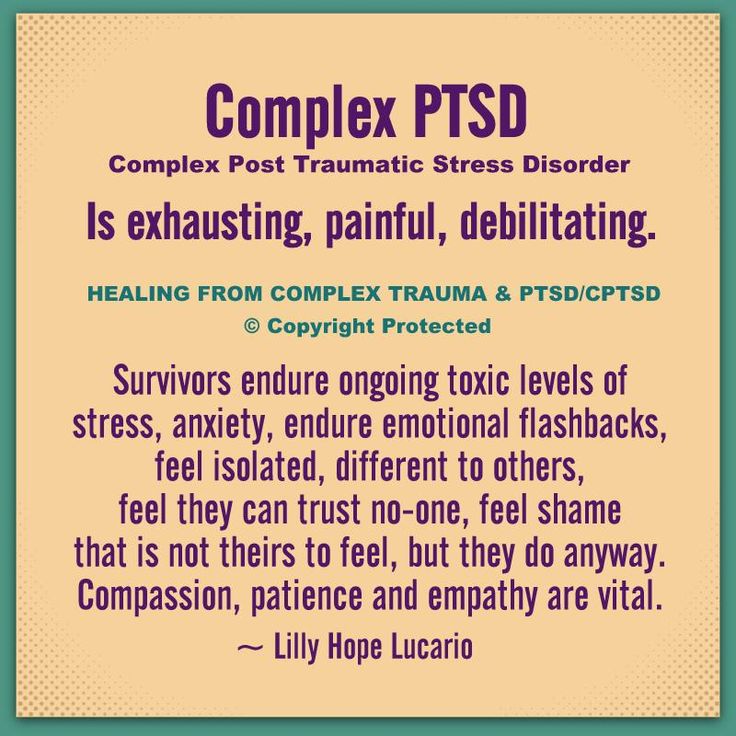 So, the causes of birth injuries of the uterus can be surgical interventions in the past (caesarean section, metroplasty, conservative myomectomy, complete or partial perforation of the uterus during abortion, etc.), which lead to the formation of a scar on the uterus and, as a result, inadequate contractility of the myometrium in childbirth.
So, the causes of birth injuries of the uterus can be surgical interventions in the past (caesarean section, metroplasty, conservative myomectomy, complete or partial perforation of the uterus during abortion, etc.), which lead to the formation of a scar on the uterus and, as a result, inadequate contractility of the myometrium in childbirth.
The likelihood of birth canal injuries increases in the presence of anatomical defects of the genitals (intrauterine septum, uterine hypoplasia, bicornuate uterus), cervical rigidity in late primiparas, uterine hyperanteflexia. Also, birth injuries can be caused by cervicitis, adenomyosis, endometritis, colpitis, cystic drift and chorionepithelioma. In the etiopathogenesis of birth trauma, there are often several aggravating factors. nine0006
Birth injuries of the vulva and vagina
Hematomas of the vulva and vagina
Hematomas of the vulva and vagina are caused by stretching and rupture of blood vessels in the thickness of the soft tissues with intact integuments.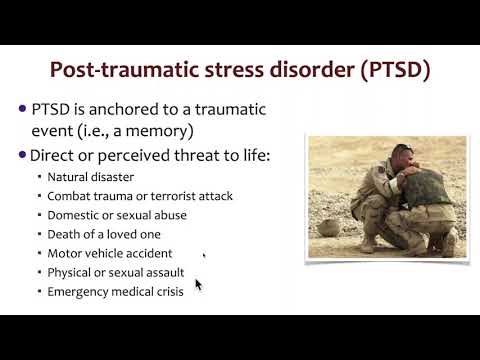 In this case, the blood pouring out of the damaged vessel accumulates in the fiber and under the mucosa, forming a hematoma.
In this case, the blood pouring out of the damaged vessel accumulates in the fiber and under the mucosa, forming a hematoma.
With birth injuries of soft tissues in the vulva and vagina, a blue-purple tumor appears, the size of which can reach the head of a newborn. Hematomas cause a feeling of discomfort (bursting, pressure), soreness. Large progressive hematomas extend to the pelvic tissue and may be accompanied by the development of hemorrhagic shock. Small hemorrhages usually resolve on their own; with large hematomas, their suppuration is possible. Recognition of birth injuries of soft tissues occurs during external examination and gynecological examination. nine0006
Surgical tactics are indicated for large (more than 4-5 cm in diameter) and progressive hematomas. At the same time, the tissues above the hematoma are opened, the accumulated blood is removed, the bleeding vessel is isolated and tied up, the wound is sewn up tightly. With an infected hematoma, the wound is not sutured. With a progressive hematoma, abdominotomy is sometimes required.
With a progressive hematoma, abdominotomy is sometimes required.
Tears of the vulva and vagina
Birth injuries of the vulva and vagina are most common in primiparas. Mild cracks and tears are usually asymptomatic and do not require intervention. Tears in the clitoris, urethra, vagina are accompanied by the formation of hematomas, massive bleeding, hemorrhagic shock. nine0006
Birth injuries of the vagina can be spontaneous and violent. In the latter case, the causes of birth injuries are various obstetric operations. Vaginal tears can occur in its upper, middle, or lower sections; be superficial or deep, reaching the tissue of the small pelvis and abdominal cavity.
Birth injuries of the tissues of the vulva are detected during examination. To exclude internal tears, it is necessary to examine the walls of the vagina with the help of mirrors. nine0006
Treatment of birth injuries of the vulva and vagina is exclusively surgical. After catheterization of the bladder with a metal catheter, the tears are sutured with catgut sutures. In the postoperative period, antimicrobial therapy and vaginal baths with antiseptics are prescribed. Unrecognized vaginal tears may heal uncomplicated or become infected. Deep tears can subsequently lead to secondary vaginal atresia, necessitating vaginoplasty. nine0006
After catheterization of the bladder with a metal catheter, the tears are sutured with catgut sutures. In the postoperative period, antimicrobial therapy and vaginal baths with antiseptics are prescribed. Unrecognized vaginal tears may heal uncomplicated or become infected. Deep tears can subsequently lead to secondary vaginal atresia, necessitating vaginoplasty. nine0006
Birth injuries of the perineum
Birth injuries of the perineum include violent or spontaneous ruptures of the skin, fiber and muscle-fascial tissues of the pelvic floor. Birth injuries of the perineum occur in 7-15% of women in labor, and much more often in primiparas. Perineal ruptures are often combined with birth injuries of the vagina.
Protrusion and cyanosis of the tissues of the pelvic floor, swelling and luster of tissues, cracks testify to the threat of birth injury of the perineum. If there is a threat of birth injury of the perineum, they resort to a median dissection of tissues - perineotomy or a lateral incision - episiotomy, followed by suturing.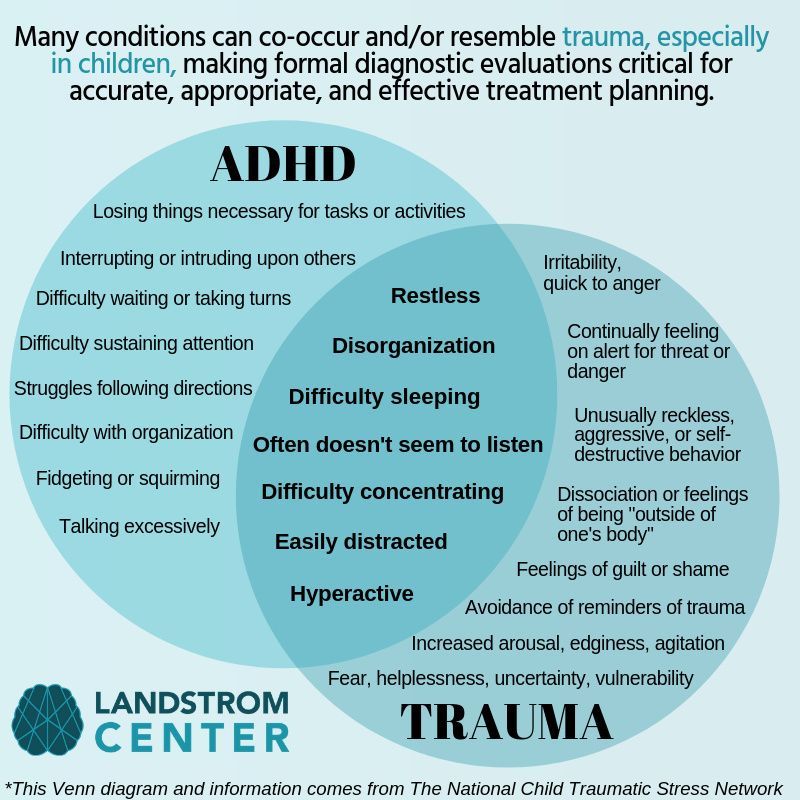 nine0006
nine0006
Perineal tear symptoms
Depending on the depth of the birth injury, 3 degrees of perineal ruptures are distinguished.
With a rupture of the perineum of the 1st degree, the integrity of the skin and subcutaneous tissue in the region of the posterior commissure is violated. II degree of perineal rupture is characterized by additional injuries of the pelvic floor muscles (including the muscles that lift the anus), the back or side walls of the vagina. With a birth injury of the perineum of the III degree, the rupture of the external sphincter, and sometimes the walls of the rectum, joins the above injuries. nine0006
Birth injuries of the perineum are manifested by a violation of the integrity of tissues and bleeding.
Diagnosis and treatment of perineal tears
Birth injuries of the perineum are recognized after the birth of the placenta. To do this, the obstetrician-gynecologist spreads the genital gap, examines the walls of the vagina and the cervix. More often damage to the perineum during childbirth occurs not along the midline, but extramedially, but there is also a central gap between the posterior commissure and the muscle that lifts the anus. nine0006
More often damage to the perineum during childbirth occurs not along the midline, but extramedially, but there is also a central gap between the posterior commissure and the muscle that lifts the anus. nine0006
Restoration of the integrity of the tissues of the perineum is performed by suturing under local infiltration or general anesthesia. Separate catgut sutures are placed on the damaged walls of the vagina and rectum, pelvic floor muscles, subcutaneous tissue and perineal skin. In the postpartum period, sutures are processed, a thorough toilet of the wound after each defecation and urination, and constipation is prevented.
Birth injuries of the uterus
Uterine ruptures
Uterine rupture is one of the most severe birth injuries and occurs in 0.015% -0.1% of the total number of births. When the uterus ruptures, the integrity of the walls of its body is violated. The lethality of women with birth trauma of the uterus from shock, anemia and septic complications reaches 3-4%.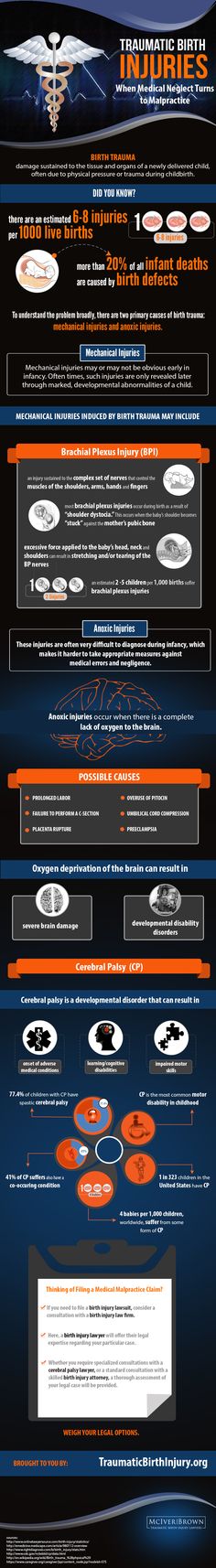 Many women who have had uterine rupture develop hypoxic encephalopathy later on. Fetal death in uterine rupture is close to 100%. nine0006
Many women who have had uterine rupture develop hypoxic encephalopathy later on. Fetal death in uterine rupture is close to 100%. nine0006
Classification of uterine ruptures
There are uterine ruptures that occurred during pregnancy and during childbirth. According to the pathogenetic signs of birth trauma, spontaneous (mechanical, histopathic and mechanical-histopathic) and violent (traumatic, mixed) uterine ruptures are distinguished. According to the birth trauma clinic, uterine ruptures can be threatening, begun, completed.
According to the degree of damage to the walls of the uterus, a birth injury can take the form of a crack, incomplete rupture and complete rupture penetrating into the abdominal cavity. By localization, there is a rupture of the bottom of the uterus, its body, the lower segment, as well as a complete separation of the uterus from the vaginal vaults (colpoporexis) in the transverse position of the fetus. nine0006
Symptoms of uterine rupture
The clinic of birth trauma of the uterus depends on the causes, stage, degree, localization of the rupture.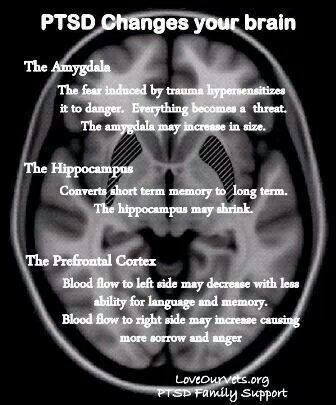 The severity of manifestations and consequences are largely due to the accompanying background - in the presence of somatic diseases of the woman in labor, gestosis, physical and mental exhaustion, infection, etc., irreversible changes quickly develop in the body.
The severity of manifestations and consequences are largely due to the accompanying background - in the presence of somatic diseases of the woman in labor, gestosis, physical and mental exhaustion, infection, etc., irreversible changes quickly develop in the body.
For threatening rupture of the uterus, excessive labor activity with painful strong contractions, deformity of the uterus in the form of an hourglass, development of edema of the cervix, vagina and vulva, difficulty urinating, anxiety of the woman in labor are typical. With the onset of uterine rupture, the listed symptoms are supplemented by convulsive contractions, the appearance of sanious or bloody discharge from the vagina, and hematuria. nine0006
With the completed rupture of the uterus, after a sharp pain and burning sensation in the abdomen, labor activity stops, the woman in labor calms down, becomes depressed, apathetic. Due to the development of hemorrhagic and painful shock, pallor of the skin, hypotension, tachycardia rapidly increase, cold sweat, nausea and vomiting appear. After rupture of the uterus, parts of the fetus are partially or completely palpated in the abdominal cavity, there is no fetal heartbeat. External bleeding with this birth injury can be significant or scanty, depending on the size and location of uterine rupture. nine0006
After rupture of the uterus, parts of the fetus are partially or completely palpated in the abdominal cavity, there is no fetal heartbeat. External bleeding with this birth injury can be significant or scanty, depending on the size and location of uterine rupture. nine0006
Uterine rupture emergency
If there is a threat of uterine rupture, it is necessary to immediately stop labor and complete labor by surgery - caesarean section or fruit-destroying surgery. With the onset or completed uterine rupture, cerebrosection is performed, the fetus and placenta are removed, amniotic fluid and blood are removed, and hemostasis is performed. The volume of intervention for these birth injuries ranges from supravaginal amputation to hysterectomy. Uterine suturing is possible in young patients with recent and small ruptures of a linear nature, the absence of infection. nine0006
At the same time, it is necessary to carry out adequate replenishment of blood loss, anti-shock infusion-transfusion therapy, and correction of hemocoagulation.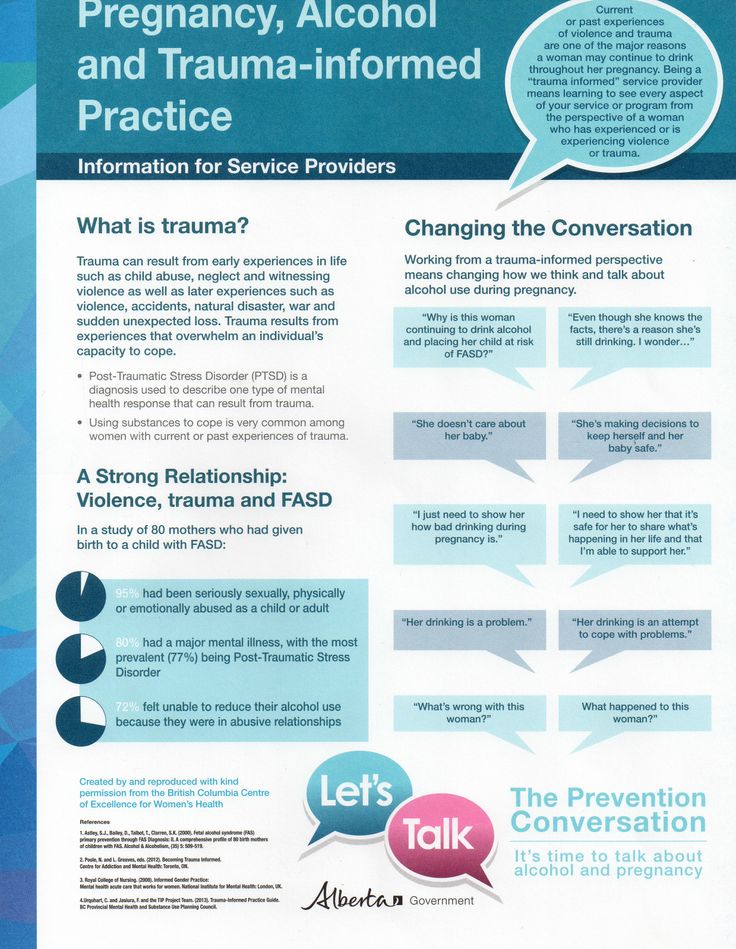 If birth injuries of the uterus were not recognized, bleeding or peritonitis may develop, as well as the death of the puerperal. With infectious complications, laparotomy, removal of the uterus with appendages (panhysterectomy), drainage of the abdominal cavity, and massive antibiotic therapy are undertaken.
If birth injuries of the uterus were not recognized, bleeding or peritonitis may develop, as well as the death of the puerperal. With infectious complications, laparotomy, removal of the uterus with appendages (panhysterectomy), drainage of the abdominal cavity, and massive antibiotic therapy are undertaken.
Cervical tears
This type of birth injury occurs according to various authors in 3-60% of women in labor. Cervical ruptures (violent or spontaneous) are divided into 3 degrees according to the depth of damage: I - a defect of no more than 2 cm; II - defect more than 2 cm, but not reaching the vaginal vaults; III - a defect that reaches the vaults and passes to them. Cervical ruptures are usually localized in the lateral sections, more often on the left.
Symptoms of cervical tears
Birth injuries of the cervix are manifested by postpartum bleeding from the vagina after the birth of the placenta and contraction of the uterus. Blood flowing from the genital tract has a scarlet color, is released in a continuous stream or in the form of a large number of clots in the absence of external damage to the birth canal. Sometimes there is little or no bleeding. If the branches of the uterine arteries are damaged, there is a massive outpouring of blood or the formation of hematomas in the paracervical tissue, a clinic of hemorrhagic shock. nine0006
Blood flowing from the genital tract has a scarlet color, is released in a continuous stream or in the form of a large number of clots in the absence of external damage to the birth canal. Sometimes there is little or no bleeding. If the branches of the uterine arteries are damaged, there is a massive outpouring of blood or the formation of hematomas in the paracervical tissue, a clinic of hemorrhagic shock. nine0006
If cervical ruptures remain unrecognized, in the future this can lead to the development of postpartum ulcers, parametritis, pelvioperitonitis, spontaneous abortions, and cervical dysplasia.
Diagnosis and treatment of cervical tears
To recognize birth injuries of the cervix, all puerperas need to be examined with the help of mirrors immediately after the completion of childbirth, and also 6-48 hours after the reduction of edema and tissue stretching.
Detected ruptures of the cervix are subject to suturing immediately or delayed, no later than 2 days after birth. The sutures are applied to the ruptures of the neck through all layers of tissues, starting from the upper corner of the defect in the direction of the external pharynx. Due to unfavorable conditions (the presence of lochia, edema, crushing of tissues), birth injuries of the cervix often heal by secondary intention. nine0006
The sutures are applied to the ruptures of the neck through all layers of tissues, starting from the upper corner of the defect in the direction of the external pharynx. Due to unfavorable conditions (the presence of lochia, edema, crushing of tissues), birth injuries of the cervix often heal by secondary intention. nine0006
Other birth injuries
Uterine eversion
The development of acute uterine inversion is due to improper management of the afterbirth period, weakness of the uterine ligaments, and atony of the uterus. Distinguish between partial and complete eversion of the uterus. This birth injury proceeds with the phenomena of pain shock.
Treatment of uterine inversion consists in anti-shock measures and reduction of the uterus to its anatomical site under general anesthesia.
Sprains and ruptures of the pelvic joints
These birth injuries develop with excessive softening of the joints of the pelvis (symphysiopathy, symphysitis), childbirth with a premature or large fetus, obstetric benefits. In this case, the pubic bones are stretched and separated at a distance of more than 0.5 cm from each other. Rupture of the pubic joint is often accompanied by displacement of bones, damage to the bladder, urethra, and clitoris. Stretching of the sacroiliac joints leads to hemorrhages and subsequent inflammation of the joints.
In this case, the pubic bones are stretched and separated at a distance of more than 0.5 cm from each other. Rupture of the pubic joint is often accompanied by displacement of bones, damage to the bladder, urethra, and clitoris. Stretching of the sacroiliac joints leads to hemorrhages and subsequent inflammation of the joints.
The clinic of birth injuries of the pelvic joints is manifested by pain in the womb, coccyx, sacrum, aggravated by abduction of the legs, walking; gait disturbance, skin hyperemia and swelling of surrounding tissues.
Birth injuries of the pelvic region are detected during the consultation of a traumatologist during examination, palpation, radiography of the pubic, sacroiliac joint, and pelvis. Treatment of sprains of the pelvic joints requires rest, tight bandaging, wearing special corsets. A rupture of the pubic symphysis or a significant divergence of the pelvic bones requires surgical intervention. nine0006
Urogenital and rectovaginal fistulas
Birth injuries with the formation of fistulas are caused by prolonged (more than 2 hours) standing of the child's head in one plane, as a result of which a violation of blood circulation in tissues develops with their subsequent necrosis. Sometimes urogenital and rectal-vaginal fistulas are formed as a result of intraoperative damage to the walls of the bladder or rectum.
Sometimes urogenital and rectal-vaginal fistulas are formed as a result of intraoperative damage to the walls of the bladder or rectum.
Fistulas are manifested by the release of urine or gases and feces through the vagina outside the acts of urination and defecation. Such disorders are always accompanied by the development of a local inflammatory reaction in the vagina (colpitis). nine0006
Diagnosis of urogenital fistulas is made during a gynecological examination, cystoscopy; rectal-vaginal fistulas are recognized by digital rectal examination, irrigoscopy, fistulography, and rectoscopy. When detecting urogenital and rectovaginal fistulas, their surgical closure (fistuloplasty) is usually required.
Birth injury prevention
Prevention of birth injuries of the uterus requires the study of the gynecological history of the pregnant woman in the early stages, ultrasound monitoring of the state of scars on the uterus during pregnancy, hospitalization of pregnant women with the threat of traumatism during childbirth.