When do colostrum starts
What Is It, Benefits & What To Expect
Overview
What is colostrum?
Colostrum (kuh-loss-trum) is the first milk your body produces during pregnancy. It forms in your mammary glands (breasts) and plays an important role in building your baby's immune system. If you plan on breastfeeding (nursing or chestfeeding), it's the first milk your baby will get from your breasts. If you don't want to breastfeed or if your baby is struggling to breastfeed, you can hand express colostrum. It's high in protein, vitamins, minerals and immunoglobulins (antibodies) that help build your baby's immune system. It's often called "liquid gold" because of its rich, golden color and valuable benefits.
What is colostrum made of?
Colostrum is high in protein and low in fat and sugar. It's filled with white blood cells that produce antibodies. These antibodies strengthen your baby's immune system, protecting him or her from infection. Colostrum is highly concentrated and nutrient-dense even in tiny doses, so your baby's tummy doesn't need a lot to reap its benefits.
What kind of nutrients are in colostrum?
Colostrum is rich in nutrients that protect and nourish your baby unlike anything else. It's made up of things like:
- Immunoglobulin A (an antibody).
- Lactoferrin (a protein that helps prevent infection).
- Leukocytes (white blood cells).
- Epidermal growth factor (a protein that stimulates cell growth).
It gets its color from carotenoids (an antioxidant) and vitamin A. Vitamin A plays a vital role in your baby's vision, skin and immune system. Colostrum is rich in magnesium, which supports your baby’s heart and bones, and copper and zinc, which also support immunity.
What's the difference between colostrum and breast milk?
Colostrum is a nutrient-rich first milk produced by your breasts during pregnancy. It changes to transitional breast milk a few days after your baby is born. However, small amounts of colostrum remain in your breast milk for several weeks.
There are distinct differences between colostrum and breast milk:
- Colostrum is filled with immunoglobins to boost your baby's immune system and protect it from illness.
- Colostrum has two times as much protein.
- Colostrum has four times as much zinc.
- Colostrum is lower in fat and sugar so it's easier to digest.
- Colostrum is thicker and more yellow.
What are the stages of breast milk?
There are three different stages of breast milk: colostrum, transitional milk and mature milk.
- Colostrum: Your first milk that lasts between two and four days after birth.
- Transitional milk: Begins approximately four days after birth and lasts about two weeks.
- Mature milk: Milk that lasts from approximately 14 days after birth until you are done producing milk.
When does colostrum turn to milk?
After approximately three or four days, colostrum will turn to transitional milk. This is often referred to as someone's milk "coming in." Your breasts will feel firm, tender and full. It means your milk supply has ramped up. By this time your baby's stomach has expanded and they can drink more milk each feeding. Once your milk supply is established and your body has stabilized, transitional milk changes to mature milk.
Once your milk supply is established and your body has stabilized, transitional milk changes to mature milk.
What makes colostrum turn to breast milk?
The pregnancy hormones created by the placenta help you create colostrum. The hormone progesterone drops significantly when the placenta separates from your uterus (after your baby is born). This drop in progesterone triggers your breasts to create milk.
Function
What is the purpose of colostrum?
The function of your breasts, or mammary glands, is to produce milk to feed your baby. Colostrum is more than the first milk your baby consumes after birth. It's highly concentrated with nutrients and antibodies to fight infection and protect your baby. It provides a powerful, unique immunity that only it can provide. Because your baby only needs a little bit of colostrum, it also helps them learn to suck, swallow and breathe during feeding.
What are the benefits of colostrum?
Colostrum builds your baby's immune system and provides concentrated nutrition. Some of the benefits of colostrum are:
Some of the benefits of colostrum are:
- Helps strengthen your baby's immune system.
- Helps to establish a healthy gut by coating the intestines. This helps keep harmful bacteria from being absorbed.
- Offers ideal nutrition for a newborn.
- Has a laxative effect that helps your baby clear meconium (your baby's first poop) and lessens the chance of jaundice.
- Easy to digest.
- Helps prevent low blood sugar in full-term babies.
Why is colostrum good for newborns?
Colostrum has all the nutrients your baby needs in the first few days of life. It's also packed with nutrients and vitamins to strengthen your baby's immune system.
The flow of colostrum from your nipples is slow so your baby can learn to breastfeed (nurse). Learning how to breastfeed takes practice and requires your newborn to not only learn to suck and swallow but breathe at the same time.
Does leaking colostrum mean labor is close?
Colostrum leaking from your breasts doesn't mean labor is coming. Leaking colostrum is normal and some people notice it as early as the second trimester. Some don't notice any signs of leaking colostrum while others will see dried colostrum on their nipples. If you are leaking colostrum, you can wear disposable or washable breast pads.
Leaking colostrum is normal and some people notice it as early as the second trimester. Some don't notice any signs of leaking colostrum while others will see dried colostrum on their nipples. If you are leaking colostrum, you can wear disposable or washable breast pads.
Can you express colostrum if you're pregnant?
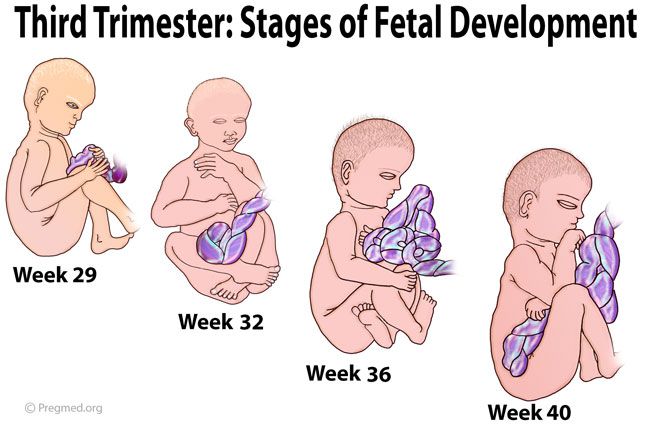
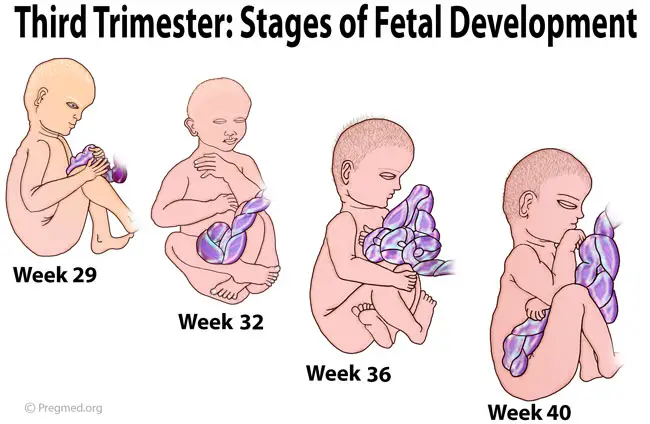
Colostrum can be expressed by about week 37 in pregnancy and is beneficial for some people. Using your hands to compress your breasts in a rhythmic pattern so that milk comes out is called hand expressing. Expressing colostrum before your baby is born carries some risks like contractions or premature labor. It can be beneficial to those at risk for premature birth, low milk supply or when certain health conditions present.
Speak with your healthcare provider before you remove colostrum from your breasts. If you are leaking colostrum, it may be safe to collect and store it for when your baby is born.
Can you pump colostrum?
It's difficult to pump colostrum with a breast pump because of its thick consistency. Most people recommend and prefer using their hands to express colostrum. Hand expressing colostrum usually produces more colostrum than a pump.
Most people recommend and prefer using their hands to express colostrum. Hand expressing colostrum usually produces more colostrum than a pump.
Anatomy
What does colostrum look like?
Colostrum is often a deep, rich yellow or orange color, almost like the yolk of an egg. This is because it contains high levels of beta carotene. It can sometimes appear white, clear or creamy. It's a thicker consistency than breast milk (or cow's milk), but the thickness varies from person to person. Colostrum is often sticky and can contain faint traces of blood (this is normal).
How do I know I am making colostrum?
Your body begins producing colostrum between 12 and 18 weeks in pregnancy. Most people will produce anywhere from a tablespoon to an ounce of colostrum within the first 24 hours of delivery. This slowly increases until transitional milk comes in around the third or fourth day. In most cases, you will not know if you are making colostrum, however, it's very rare to be unable to produce colostrum. You will know if your baby is getting colostrum if he or she is maintaining their weight and wetting diapers.
You will know if your baby is getting colostrum if he or she is maintaining their weight and wetting diapers.
How long do you have colostrum?
Your body produces colostrum for up to about five days after your baby is born. It changes to transitional milk around this time, then changes again to mature milk after about 14 days. Traces of colostrum are present in your breast milk for up to six weeks.
Conditions and Disorders
What happens if you don't produce colostrum?
Most people will produce some colostrum — not producing it is rare. It's normal to feel like nothing is coming out of your breasts and worry that your baby isn't getting enough. Your baby only needs a few teaspoons of colostrum to fill their tiny stomach.
Care
How do you store pumped colostrum?
If you and your healthcare provider decide it's safe to express and store colostrum, there are a few rules to follow. First, you should ensure the colostrum is stored in a sterile container or syringe. It can be kept in your refrigerator for about two or three days. It must be moved to a freezer after three days. Colostrum can be kept in a freezer for at least three months.
It can be kept in your refrigerator for about two or three days. It must be moved to a freezer after three days. Colostrum can be kept in a freezer for at least three months.
Frequently Asked Questions
How much colostrum does a newborn need?
Your newborn's tummy is about the size of a marble. They only need about an ounce of colostrum per day. This equals about a teaspoon each feeding (you can expect to feed your newborn eight to 10 times the first few days). The amount of colostrum (and then transitional milk) your baby needs increases slowly each day as their stomach expands. As your body transitions to producing regular breast milk, your milk production will increase to meet their needs.
Do I need to supplement?
No, you shouldn't need to supplement. A tiny bit of colostrum goes a long way in filling up your baby. Check with your healthcare provider to make sure your baby is gaining weight. If your baby is wetting diapers and seems pretty happy, supplementing is usually not necessary.
Is it okay to squeeze out colostrum?
Yes, it's usually OK to squeeze out colostrum once you reach full-term pregnancy (37 weeks). Check with your healthcare provider if you wish to do this prior to your baby being born. If you want to hand express colostrum for your newborn, follow these steps:
- Cup your breasts with your hand in a "C" shape. Four fingers should be under your breast and your thumb should be above your nipple.
- Use your thumb and index finger to gently squeeze your areola and nipple.
- Repeat several times and in a pattern. Apply firm pressure but do not slide your fingers. If colostrum doesn't come out, try moving your fingers to another spot.
- Colostrum should slowly flow out within minutes. It's thick and comes out in drops.
- You can repeat this a few times per day.
Please note that expressing colostrum before your baby is born carries risks. Some people can go into premature labor or begin having contractions. Talk to your healthcare provider before you express colostrum.
Talk to your healthcare provider before you express colostrum.
A note from Cleveland Clinic
Colostrum is the first milk produced by your breasts. It's rich in nutrients and high in antibodies and antioxidants. Getting started with breastfeeding can be difficult and usually requires assistance, so don't be ashamed to ask your healthcare provider for help. Breastfeeding early and often is the best way to make sure your baby gets the many benefits from colostrum. Hand expressing colostrum and feeding your baby with a syringe is also an option. Ask your healthcare team for help if feeding your baby colostrum is something you wish to do.
When Does Breast Milk Come In & Signs It’s Coming
The look and feel of your colostrum, or early milk, is much different from your mature, later milk - which often comes in around 2 - 5 days after your baby's birth, though every mama’s timing is different.
Share this content
So, When Does Breast Milk Come In?
Though colostrum production begins as early as 16 weeks pregnant and should begin to be expressed right away after birth (with some moms even experiencing occasional leakage later in pregnancy), its look and composition differs significantly from your later breast milk. This is because colostrum, or your “first milk”, plays a much different role for your baby than your later breast milk, though both forms are incredibly important to your baby’s wellness and development. Though later breast milk may take some time to “come in” after delivery, your milk production has been in the works since early in your pregnancy, so don’t worry, mama – it’ll be here soon enough!
This is because colostrum, or your “first milk”, plays a much different role for your baby than your later breast milk, though both forms are incredibly important to your baby’s wellness and development. Though later breast milk may take some time to “come in” after delivery, your milk production has been in the works since early in your pregnancy, so don’t worry, mama – it’ll be here soon enough!
Moms shouldn’t expect to see large milk volumes in the first few days after birth, though most newborns lose weight during this time. Both of these things are normal and expected, and your colostrum is all your newborn needs until your later milk presents. With that in mind, your later milk – or the breast milk produced as your colostrum transitions to your mature milk – “comes in” about 2 – 5 days after your baby’s birth. “Coming in” refers to the significant increase in volume and changes in composition, though this popular term isn’t necessarily accurate. This is because your colostrum is breast milk and should be fed to your baby as soon as possible after birth. When your mature milk comes in later, however, it is accompanied by some very noticeable symptoms.
When your mature milk comes in later, however, it is accompanied by some very noticeable symptoms.
Signs Milk Is Coming In
Many women, even first-time moms, know exactly when their breast milk has come in, mainly due to common indicators like:
- Breast engorgement, or the feeling of fullness, heaviness, and/or firmness.
- Swelling of the breasts.
- Breast milk leakage, particularly overnight.
- Flattened nipples and/or skin tightening or firmness around the areolas.
This initial engorgement – and the occasional discomfort that may accompany the first time your milk comes in – will dissipate as your body adjusts to a regular nursing and pumping routine. If your breasts are frequently engorged after your milk comes in, this is a sign that your body is working hard to produce milk and you may not be fully emptying your breasts after a nursing session – be sure to have a breast pump and breast milk storage bags on hand, so you can fully empty your breasts after and between breastfeeding your little one. Your pumped breast milk can be stored in the refrigerator or freezer, so you can start a stockpile for your little one – which can be especially helpful if your partner or another person, such as a babysitter, needs to feed the baby. Just be sure to read up on the latest breast milk storage guidelines and use a helpful feeding and pumping log to ensure none of your precious liquid gold goes to waste!
Your pumped breast milk can be stored in the refrigerator or freezer, so you can start a stockpile for your little one – which can be especially helpful if your partner or another person, such as a babysitter, needs to feed the baby. Just be sure to read up on the latest breast milk storage guidelines and use a helpful feeding and pumping log to ensure none of your precious liquid gold goes to waste!
What Else Should I Know?
Though your body’s breast milk production is kicked into high gear within 30 – 40 hours after you deliver the placenta, your later milk coming in is dictated by the hormonal changes taking place in your body during this time. Because every woman – and every pregnancy – is different, there is a range of days during which breast milk may come in. With that in mind, there is evidence that skin to skin contact, initiating breastfeeding within 30 – 60 minutes after birth, and continuing to nurse early and often (or pumping or hand expressing your colostrum to feed your baby, if there are latching challenges) can positively impact your breast milk production.
If your breasts are very engorged, it can be more difficult for your baby to latch properly. Try softening your breasts before a feeding, such as by taking a warm shower, applying a warm compress to each breast, and/or hand expressing a small volume of milk. You can also apply a cold compress – think a bag of frozen vegetables or an ice pack wrapped in a towel – to reduce swelling and discomfort. Prevent engorgement and reduce your risk of developing mastitis or encountering eventual breast milk supply issues by nursing or pumping frequently.
If you have questions about your breast milk coming in, concerns about supply, or are experiencing difficulties getting into a regular breast milk feeding routine, talk to a lactation consultant right away. The sooner you can address any issues you may be facing, the easier it will be to minimize impact on your future breast milk production. Remember, mama, it’s common to encounter early breast milk feeding challenges – especially if you’re a first-time mom – and it may take some time for your body and hormones to adjust. After all, you just did an amazing thing by welcoming your little one into the world! The most important thing to remember is to persevere and continue finding ways to ensure your baby receives all that great liquid gold that your body is making – whether by pumping, nursing, or a combination of both. As your milk comes in and you adapt to life with a newborn, you and your baby will eventually get into a regular feeding routine. Congratulations on your new bundle of joy – and be sure to enjoy this unique bonding time together!
After all, you just did an amazing thing by welcoming your little one into the world! The most important thing to remember is to persevere and continue finding ways to ensure your baby receives all that great liquid gold that your body is making – whether by pumping, nursing, or a combination of both. As your milk comes in and you adapt to life with a newborn, you and your baby will eventually get into a regular feeding routine. Congratulations on your new bundle of joy – and be sure to enjoy this unique bonding time together!
Breast changes from the beginning of pregnancy to the end of breastfeeding
Medela's experts explain the changes that occur in the breast from the beginning of pregnancy to the end of breastfeeding, as well as tips for taking care of your breasts throughout this period.
Share this information
From the moment of conception, your body begins to prepare for the birth of your baby. This applies not only to the uterus - the anatomy of the breast also changes radically. This article will tell you what to expect in each trimester, during and after breastfeeding.
This article will tell you what to expect in each trimester, during and after breastfeeding.
First trimester breast changes
Early in pregnancy, many women notice changes in their breasts. Moreover, often they become the first signs of pregnancy. Fluctuations in hormone levels and changes in the structure of the mammary glands can cause increased sensitivity and soreness of the nipples and breasts as early as the third or fourth week. For some pregnant women, breast tenderness persists until childbirth, but for most it goes away after the first trimester.
“Sometimes during pregnancy, breasts grow very quickly in the first weeks, and sometimes their size increases gradually,” says Dr. Jacqueline Kent, a leading lactation specialist at the University of Western Australia. “All women are different. For some, breast size may not change much until childbirth or even after them. In general, we can say that by the time the milk arrives, the breast will most likely become one and a half times larger than before pregnancy! 1
As soon as your regular bras start to feel tight (usually around 12 weeks), it's time to buy a maternity bra. The most comfortable, according to many women, are seamless models with wide straps made of soft, breathable fabric. It is best to avoid underwired bras as they can put pressure on the developing milk ducts.
The most comfortable, according to many women, are seamless models with wide straps made of soft, breathable fabric. It is best to avoid underwired bras as they can put pressure on the developing milk ducts.
It is important to take your measurements correctly in order to find the right bra with a good fit. Take measurements every couple of months, as you may need a different size bra as your baby grows and your breasts get bigger.
Breast changes in the second trimester
From about the 15th week of pregnancy, newly formed cells that produce milk are activated in the breast, and by about the 22nd week, production begins. 1 But don't worry - most of this milk will be absorbed by the body without going out, as pregnancy hormones prevent it from being overproduced or excreted.
“During the second trimester, you may notice that the nipples and areolas (the areas of skin around the nipples) become darker and larger,” says Dr. Daniel Prime, Medical Research Associate at Medela. tubercles - the so-called glands of Montgomery. They secrete oil that moisturizes the nipples and will protect them from inflammation and infection when you start to feed. Scientists believe that the smell of this fat is similar to the smell of amniotic fluid and helps the newborn baby find the nipple.” 2
tubercles - the so-called glands of Montgomery. They secrete oil that moisturizes the nipples and will protect them from inflammation and infection when you start to feed. Scientists believe that the smell of this fat is similar to the smell of amniotic fluid and helps the newborn baby find the nipple.” 2
Do not use harsh soap for breast hygiene and do not rub hard with a towel as this can damage this natural lubricant. Just wash your breasts with warm water and pat dry. And if someone tells you to pinch or rub your nipples to prepare them for breastfeeding, don't listen to them!
If you have flat or inverted nipples, your pregnancy is over 32 weeks, and your pregnancy is normal, you can try inserting special nipple formers* into your bra in consultation with your doctor. They help to gently pull out the nipples so that it is easier for the newborn to grasp them. Consult your healthcare professional or read our article on flat and inverted nipples to learn more.
If breast size increases dramatically during pregnancy, breast skin may itch and stretch marks may appear on it. A good moisturizer can help soothe itching. The appearance of stretch marks usually depends on genetics and skin type. If you have a predisposition to stretch marks, it is unlikely that you will be able to prevent them, but, fortunately, over time they will become lighter and less noticeable.
Breast changes in the third trimester
In the last trimester, you may again experience soreness and heaviness in your chest. A sleep bra will keep you comfortable at night, while a supportive sports bra will help you avoid soreness and ligament damage during exercise.
Don't forget to buy a pair of nursing bras one month before your baby is born. If possible, consult a specialist in the store or study the online guide to select the appropriate model and size. Every woman is different, but usually cups of a nursing bra are chosen one or two sizes larger than before pregnancy.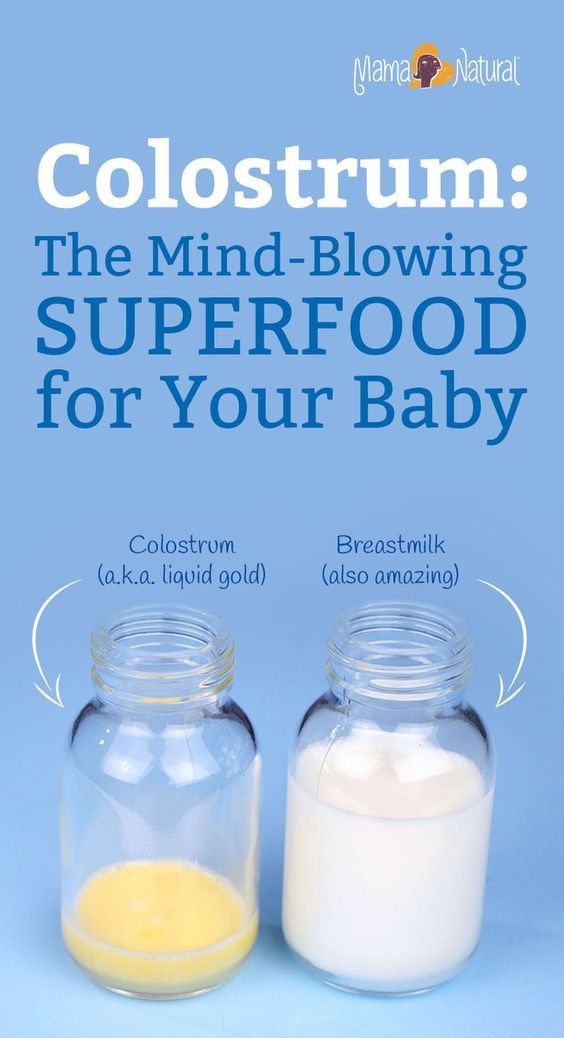 The underbust girth may also increase as the ribcage expands to provide enough room for the baby. The sales assistant should choose the size of your bra, taking into account the appearance of milk after childbirth. Models with fasteners that can be unfastened with one hand make it easier to attach the baby to the breast.
The underbust girth may also increase as the ribcage expands to provide enough room for the baby. The sales assistant should choose the size of your bra, taking into account the appearance of milk after childbirth. Models with fasteners that can be unfastened with one hand make it easier to attach the baby to the breast.
Surprising but true: milk appears in the breast even before the baby is born. This is why your nipples may start to produce some colostrum (the first breast milk), which will be quite thick and sticky. Sometimes this happens as early as 14 weeks, but more often it still happens in late pregnancy. To avoid the appearance of stains and smudges on clothes, you can use special bra pads.
“If you have diabetes or have been diagnosed with gestational diabetes, your doctor may tell you to express some colostrum by hand and freeze it. A recent study showed that after the 36th week it is quite safe if the pregnancy does not have other complications, 3 , says Dr. Prime, “Storing colostrum can come in very handy because babies with diabetic mothers are at higher risk of hypoglycemia (low blood sugar) and frequent colostrum feeding is the best remedy. . However, be prepared for the fact that there will be very little colostrum. You may only be able to express a few drops at first, and that’s perfectly fine.”
Prime, “Storing colostrum can come in very handy because babies with diabetic mothers are at higher risk of hypoglycemia (low blood sugar) and frequent colostrum feeding is the best remedy. . However, be prepared for the fact that there will be very little colostrum. You may only be able to express a few drops at first, and that’s perfectly fine.”
What happens to the breast after childbirth
Approximately two to four days after the baby is born (sometimes later if there was a caesarean section or a traumatic delivery), you will feel your breasts becoming heavier and firmer - this means that the milk has come. 4
“This breast fullness is not only due to excessive milk production – there is also an increase in the amount of blood circulating around the breast and the volume of lymphatic fluid,” explains Dr. Prime, “All this is the result of a gradual decrease in pregnancy hormone levels that began after the birth of a child and which allows the hormones responsible for the production of milk to enter into work.
During this period, you may experience soreness and discomfort in your breasts, a condition called breast swelling. This is quite common and usually resolves after a few days, during which time breastfeeding must continue. Read on for our tips on how to relieve swelling and discomfort, and if the problem persists, see a lactation consultant or healthcare provider.
What happens to the breast during lactation
For about the first three months of breastfeeding, your breasts are likely to fill up a lot before feeding. Over time, you may notice that your breasts become less full, but this does not mean at all that your milk production has decreased. If you are breastfeeding your baby exclusively and on demand, and at the same time he is growing well, then everything is in order with the amount of milk.
“Be prepared for the fact that after six months of breastfeeding, your breast size will begin to decrease,” Dr. Kent explains, “This is not a sign that your body is producing less milk. Most likely, the amount of adipose tissue in the breast simply decreased. By the time your baby is 15 months old, your breasts may be back to their pre-pregnancy size, but not smaller. However, whether you continue breastfeeding or not, you may still produce 100 to 300 ml of milk per day.”
Most likely, the amount of adipose tissue in the breast simply decreased. By the time your baby is 15 months old, your breasts may be back to their pre-pregnancy size, but not smaller. However, whether you continue breastfeeding or not, you may still produce 100 to 300 ml of milk per day.”
This may be due to the start of more efficient milk production after six months of breastfeeding, which, according to Dr. Kent's research, may be the result of redistribution of breast tissue. 5
How your breasts change after you stop breastfeeding
When you finally stop breastfeeding—be it after three weeks, three months, or three years—the breast changes associated with lactation disappear. “After the complete cessation of breastfeeding, the breasts, as a rule, return to the size that they were before pregnancy. This usually happens in about three months, and for someone else while breastfeeding,” Dr. Kent explains, “If you get pregnant again, the whole process starts all over again. ”
”
Literature
1 Cox DB et al. Breast growth and the urinary excretion of lactose during human pregnancy and early lactation: endocrine relationship. Exp Physiol . 1999;84(2):421-434. - Cox D.B. et al., "Breast growth and urinary lactose excretion during pregnancy and lactation: an endocrine relationship." Exp Physiol. 1999;84(2):421-434.
2 Doucet S et al. The secretion of areolar (Montgomery’s) glands from lactating women elicits selective, unconditional responses in neonates.PLoS One . 2009;4(10): e 7579. - Doucet S. et al., "Papillary gland secretion (Montgomery's glands) in lactating women induces a selective unconditioned response in the newborn." PLOS One. 2009;4(10):e7579.
3 Forster DA et al. Advising women with diabetes in pregnancy to express breastmilk in late pregnancy (Diabetes and Antenatal Milk Expressing [DAME]): a multicentre, unblinded, randomized controlled trial. Lancet. 2017;389(10085):2204-2213. - Forster D.A. et al., "Women with Gestational Diabetes are Recommended to Express Milk Late in Pregnancy (Diabetes and Antenatal Pumping [ DAME ]): A Multicenter, Open, Randomized, Controlled Trial. Lancet (Lancet). 2017;389(10085):2204- 2213.
Lancet. 2017;389(10085):2204-2213. - Forster D.A. et al., "Women with Gestational Diabetes are Recommended to Express Milk Late in Pregnancy (Diabetes and Antenatal Pumping [ DAME ]): A Multicenter, Open, Randomized, Controlled Trial. Lancet (Lancet). 2017;389(10085):2204- 2213.
4 Infant and young child feeding: model chapter for textbooks for medical students and allied health professionals, Geneva : World Health Organization ; 2009. AVAILABLE FROM : https://www.ncbi.nlm.nih.gov/NBKS/NBK148965/ - "POSTICION" POSTICION "POSTRISS" POSTRIMENT "POST textbook for students of medical and related professions. Geneva: World Health Organization, 2009. Article cited: https://www.ncbi.nlm.nih.gov/books/NBK148965/
5 Kent JC et al. Breast volume and milk production during extended lactation in women. Exp Physiol. 1999;84(2):435-447. - Kent J.S. et al., "Amount and production of breast milk during long-term lactation in women". Ex Physiol. 1999;84(2):435-447.
Breast volume and milk production during extended lactation in women. Exp Physiol. 1999;84(2):435-447. - Kent J.S. et al., "Amount and production of breast milk during long-term lactation in women". Ex Physiol. 1999;84(2):435-447.
Read instructions before use. Consult a specialist about possible contraindications.
* RU № ФСЗ 2010/07352 of 07/19/2010
Colostrum during pregnancy | Medela
Colostrum is sometimes called liquid gold, and not only because of its color. We will tell you why this first food is so important for a newborn baby.
Share this information
Colostrum, the first milk produced at the start of breastfeeding, is the ideal nutrition for a newborn. It is very concentrated and rich in proteins and nutrients, so even in small quantities it saturates the tiny tummy of a newborn for a long time. Colostrum is low in fat and easy to digest, yet provides the baby with all the essential ingredients for an optimal developmental start. And perhaps most importantly, it plays a decisive role in the formation of the baby's immune system.
And perhaps most importantly, it plays a decisive role in the formation of the baby's immune system.
Colostrum looks thicker and yellower than mature milk. Its composition also differs in accordance with the special needs of the newborn.
Colostrum fights infections
Almost two-thirds of the cells in colostrum are white blood cells, which not only protect the baby's body from infections, but also teach them to fight them themselves. 1 “White blood cells are very important for the development of immunity. They provide protection and counteract pathogenic microbes,” says Professor Peter Hartmann of the University of Western Australia, a leading lactation expert.
After giving birth, your body no longer protects the baby, and he must confront the new dangers of the world on his own. The white blood cells found in colostrum produce antibodies that can neutralize bacteria and viruses. These antibodies are especially good at dealing with indigestion and diarrhea, which is very important for very young children, whose intestines are not yet fully developed.
Colostrum supports the baby's immune system and intestinal function
Colostrum is especially rich in secretory immunoglobulin A -
is the most important antibody that protects the child from diseases, but not through the circulatory system, but as a protective coating of the mucous membrane of the gastrointestinal tract. 2 “The molecules that provide the mother's immune defenses enter the mother's bloodstream into the breast, where they combine to form secretory immunoglobulin A, which is then transferred to the baby along with colostrum,” explains Professor Hartmann. “Secretory immunoglobulin A accumulates on the mucous membranes of the intestines and respiratory system of the child and protects him from diseases that the mother has already had.”
Colostrum also contains many other immunological components and growth factors that stimulate the development of protective mucous membranes in the intestines of the child, and the prebiotics contained in it contribute to the formation of beneficial microflora. 3
3
Colostrum prevents jaundice
Colostrum not only protects against indigestion, but also has a laxative effect. This helps newborns to empty the intestines frequently, removing from it everything that was digested there in the prenatal state, in the form of meconium - dark and viscous feces.
Frequent stools in newborns also reduce the risk of jaundice. A baby is born with a high level of red blood cells that absorb oxygen from the air. As these cells break down, the liver helps to process them, producing a by-product called bilirubin. If the child's liver is not yet sufficiently formed to process it, bilirubin begins to be deposited in the body, causing jaundice. 4 The laxative properties of colostrum help the baby to remove bilirubin from the body along with the stool.
Colostrum contains vitamins and minerals
Carotenoids and vitamin A give colostrum its characteristic yellow color. . 7 Babies are usually born with a low supply of vitamin A, 8 and colostrum helps to replenish it.
"The first three days are especially important for establishing breastfeeding"
In addition, colostrum is rich in minerals such as magnesium, which is good for the baby's heart and bones, and copper and zinc, which are involved in the development of the immune system. 9.10 Zinc also contributes to the development of the brain, and there is almost four times more zinc in colostrum than in mature milk, 10 because the brain of a newborn must develop rapidly.
Colostrum helps your baby grow and develop
Colostrum contains many other ingredients that help your baby grow and develop. The role of some of them is still unknown to scientists.
“Colostrum retains its composition for about 30 hours after the baby is born,” says Prof. Hartmann. - It contains quite a lot of proteins, because all the antibodies in its composition are essentially proteins. It is relatively low in lactose [milk sugar] and has a different fat composition than mature milk.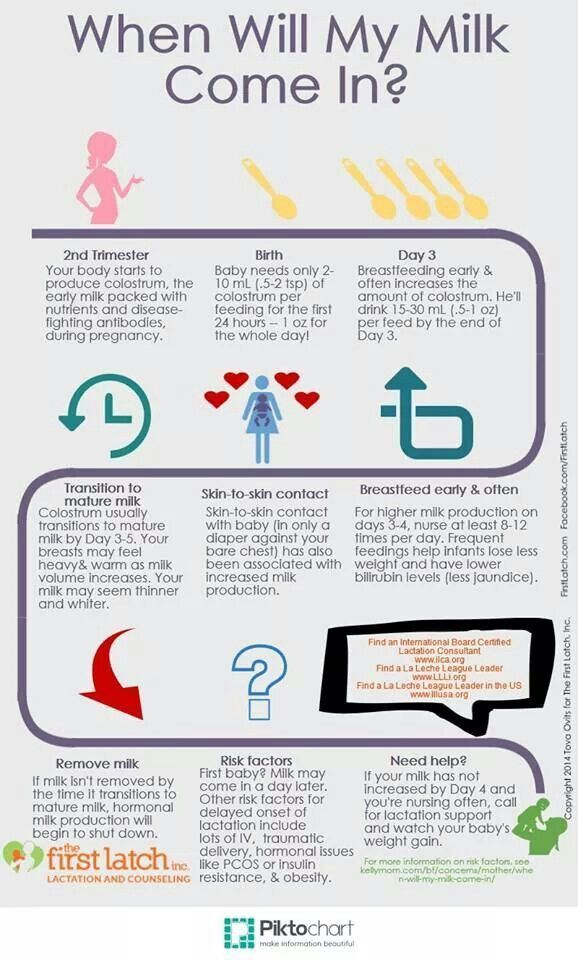 ”
”
In addition, colostrum is close in composition to the amniotic fluid that your baby swallowed and excreted while in the womb, making it ideal for adapting to the outside world. 11
Transition from colostrum to mature milk
Breast milk usually begins to arrive two to four days after birth. The breasts become firmer and fuller, and instead of colostrum, transitional milk is excreted, which is whiter in color and creamier in consistency.
“The first three days are especially important for establishing breastfeeding,” says Prof. Hartmann. “If everything is done correctly during this period, lactation is likely to be good, and the baby will be able to grow normally.”
It seems unbelievable now, but in just one year your baby will be able to walk and maybe even talk. Colostrum is produced for only a few days, but makes an invaluable contribution to the development of the baby during the first 12 months, and the resulting benefits remain with him for life.
Would you like to know more? Read our free e-book Surprising Breast Milk Facts and article What is Transitional Milk?.
Literature
1 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl Immunology. 2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3. 2 Pribylova J et al. Colostrum of healthy mothers contains broad spectrum of secretory IgA autoantibodies. J Clin Immunol. 2012;32(6):1372-1380. - Pribylova J. et al., "Healthy mother's colostrum contains a broad spectrum of secretory autoimmune antibodies to immunoglobulin A". W Clean Immunol. 2012;32(6):1372-1380. 3 Bode L. Human milk oligosaccharides: every baby needs a sugar mama. 4 Mitra S, Rennie J. Neonatal jaundice: aetiology, diagnosis and treatment. Br J Hosp Med (Lond). 20172;78(12):699-704. - Mitra S, Rennie J, Neonatal Jaundice: Etiology, Diagnosis, Treatment. Br J Hosp Med (Lond). 20172;78(12):699-704. 5 Patton S et al. Carotenoids of human colostrum. Lipids. 1990;25(3):159-165. - Patton S. et al., Carotenoids in Maternal Colostrum Lipids. 1990;25(3):159-165. 6 Gilbert C , Foster Childhood blindness in the context of VISION 2020--the right to sight. Bull World Health Organ. 2001;79(3):227-232. 7 Bates CJ. Vitamin A. Lancet. 1995;345(8941):31-35. — Bates S.J., "Vitamin A". Lancet (Lancet) 1995;345(8941):31-35. 8 World Health Organization. e-Library of Evidence for Nutrition Actions (eLENA) [Internet]. Geneva , Switzerland : WHO ; 2018 [ Accessed : 05/14/2018]. Available from Evidence-based electronic library on WHO nutrition activities ( eLENA ) [Internet]. Geneva, Switzerland: WHO; 2018 [visited 14 May 2018] Article at: [ www.who.int/elena/titles/vitamina_infants/en/ ] 9 Kulski JK, Hartmann PE. Changes in human milk composition during the initiation of lactation. Glycobiology. 2012;22(9):1147-1162. - Bode L., "Oligosaccharides in breast milk: a sweet mother for every baby." Glycobiology (Glycobiology). 2012;22(9):1147-1162.
Glycobiology. 2012;22(9):1147-1162. - Bode L., "Oligosaccharides in breast milk: a sweet mother for every baby." Glycobiology (Glycobiology). 2012;22(9):1147-1162.  - Gilbert S., Foster A., "Childhood Blindness in Context VISION 2020 - the right to see". Bull World Health Organ. 2001;79(3):227-232.
- Gilbert S., Foster A., "Childhood Blindness in Context VISION 2020 - the right to see". Bull World Health Organ. 2001;79(3):227-232.  Aust J EXP Biol
Aust J EXP Biol
10 Casey CE Studies in human lactation: zinc, copper, manganese and chromium in human milk in the first month of lactation. Am J Clin Nutr 1985;41(6):1193-1200. - Casey S.I. et al., Female Lactation Study: Zinc, Copper, Magnesium, and Chromium in Breast Milk in the Early Months of Lactation. Am J Clean Nutr. 1985;41(6):1193-1200.
11 Marlier L et al. Neonatal responsiveness to the odor of amniotic and lacteal fluids: a test of perinatal chemosensory continuity. Child Dev .