What to expect with ivf
In vitro fertilization (IVF) - Mayo Clinic
Overview
In vitro fertilization
In vitro fertilization
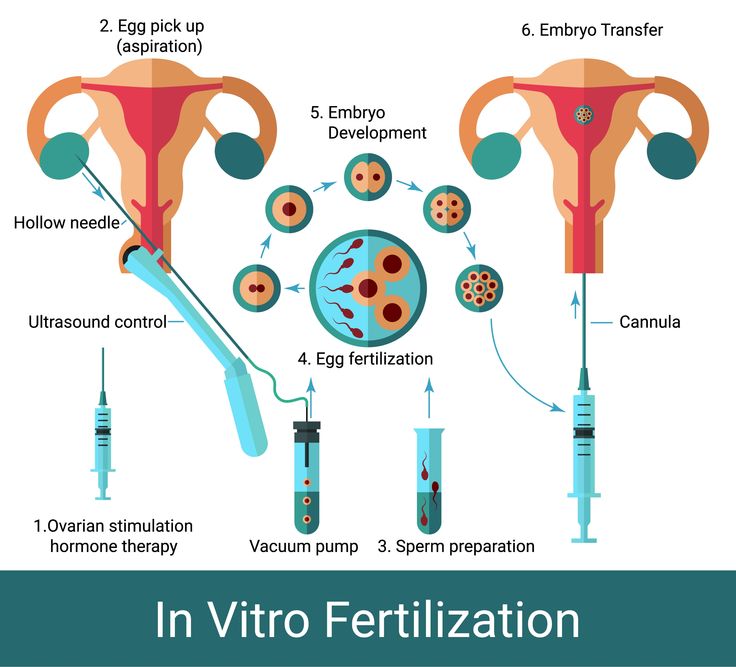
During in vitro fertilization, eggs are removed from mature follicles within an ovary (A). An egg is fertilized by injecting a single sperm into the egg or mixing the egg with sperm in a petri dish (B). The fertilized egg (embryo) is transferred into the uterus (C).
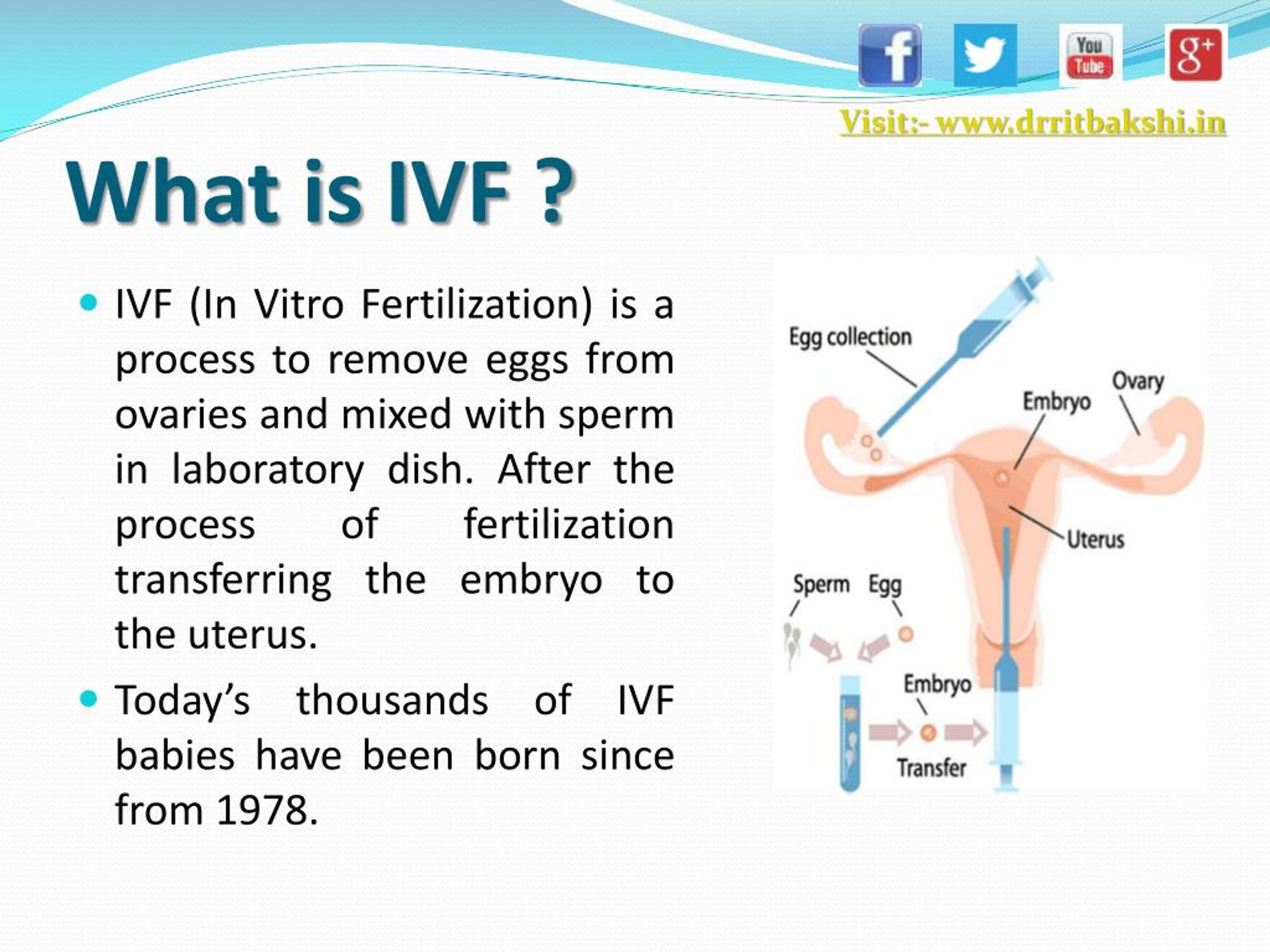
In vitro fertilization (IVF) is a complex series of procedures used to help with fertility or prevent genetic problems and assist with the conception of a child.
During IVF, mature eggs are collected (retrieved) from ovaries and fertilized by sperm in a lab. Then the fertilized egg (embryo) or eggs (embryos) are transferred to a uterus. One full cycle of IVF takes about three weeks. Sometimes these steps are split into different parts and the process can take longer.
IVF is the most effective form of assisted reproductive technology. The procedure can be done using a couple's own eggs and sperm. Or IVF may involve eggs, sperm or embryos from a known or anonymous donor. In some cases, a gestational carrier — someone who has an embryo implanted in the uterus — might be used.
Your chances of having a healthy baby using IVF depend on many factors, such as your age and the cause of infertility. In addition, IVF can be time-consuming, expensive and invasive. If more than one embryo is transferred to the uterus, IVF can result in a pregnancy with more than one fetus (multiple pregnancy).
Your doctor can help you understand how IVF works, the potential risks and whether this method of treating infertility is right for you.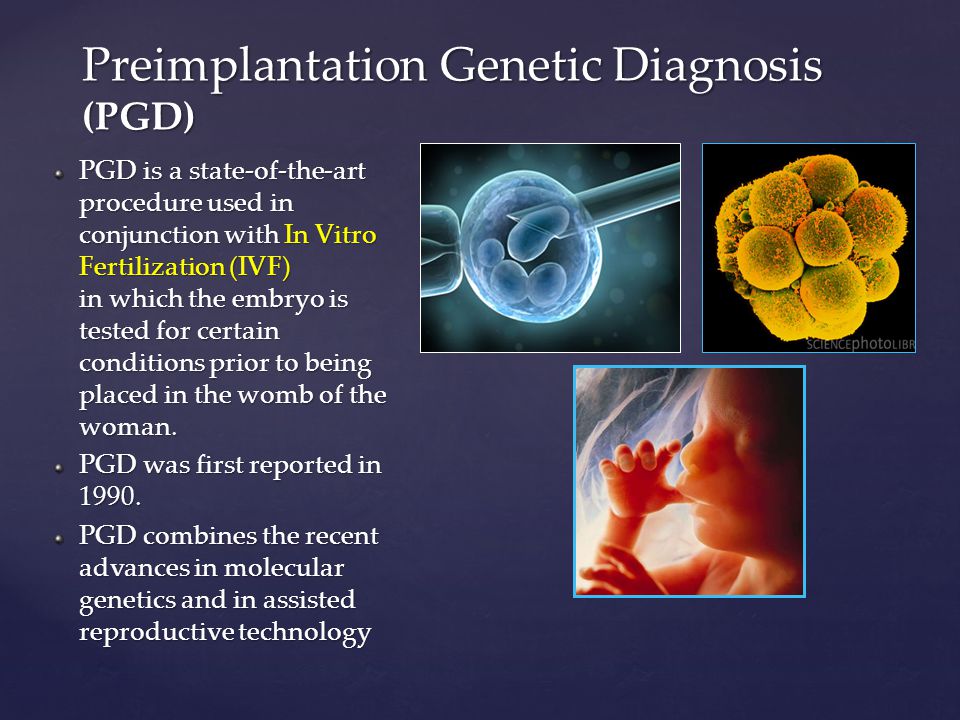
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Book: Mayo Clinic Guide to Fertility and Conception
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
In vitro fertilization (IVF) is a treatment for infertility or genetic problems. If IVF is performed to treat infertility, you and your partner might be able to try less-invasive treatment options before attempting IVF, including fertility drugs to increase production of eggs or intrauterine insemination — a procedure in which sperm are placed directly in the uterus near the time of ovulation.
Sometimes, IVF is offered as a primary treatment for infertility in women over age 40. IVF can also be done if you have certain health conditions.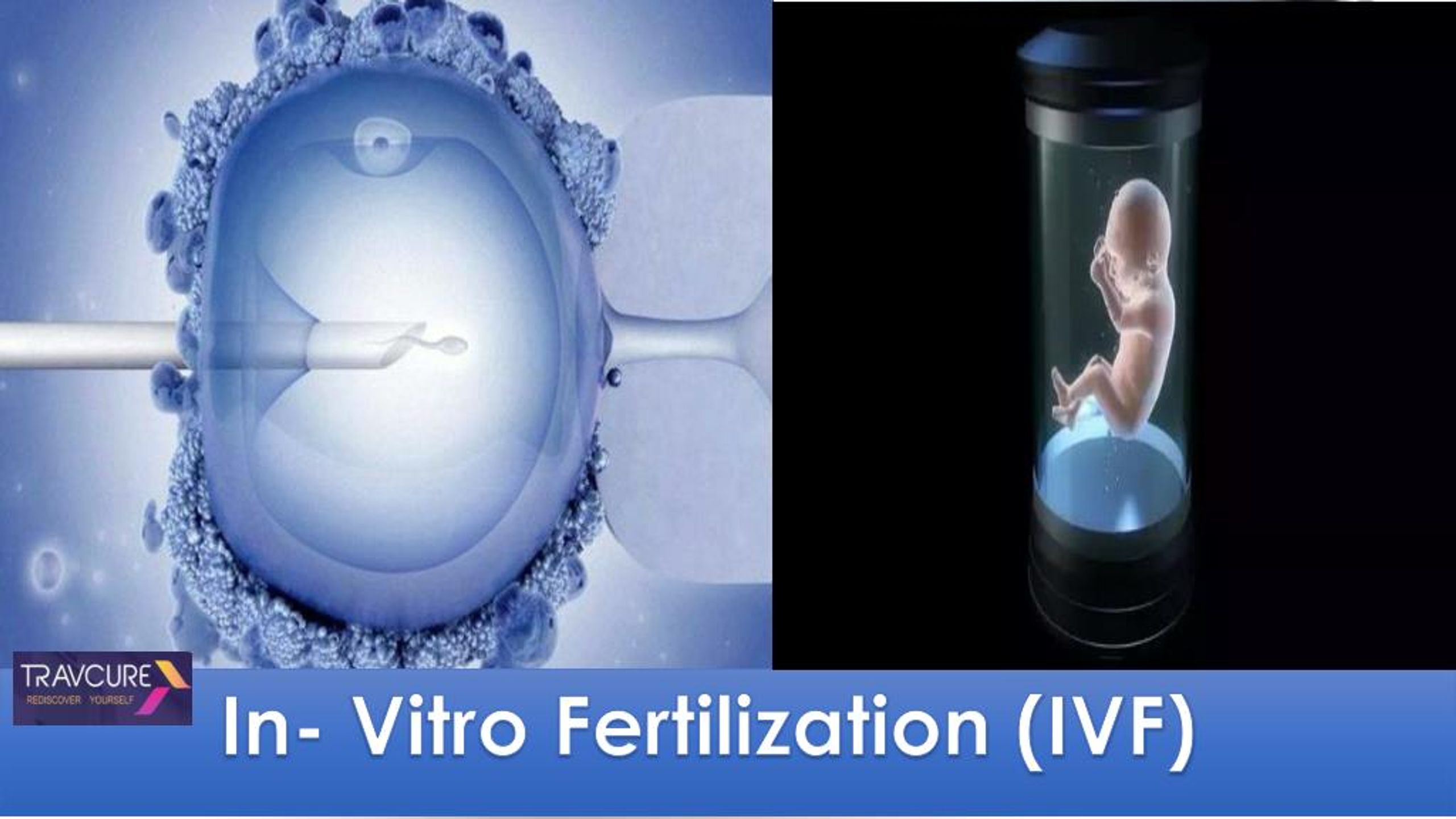 For example, IVF may be an option if you or your partner has:
For example, IVF may be an option if you or your partner has:
- Fallopian tube damage or blockage. Fallopian tube damage or blockage makes it difficult for an egg to be fertilized or for an embryo to travel to the uterus.
- Ovulation disorders. If ovulation is infrequent or absent, fewer eggs are available for fertilization.
- Endometriosis. Endometriosis occurs when tissue similar to the lining of the uterus implants and grows outside of the uterus — often affecting the function of the ovaries, uterus and fallopian tubes.
- Uterine fibroids. Fibroids are benign tumors in the uterus. They are common in women in their 30s and 40s. Fibroids can interfere with implantation of the fertilized egg.
- Previous tubal sterilization or removal. Tubal ligation is a type of sterilization in which the fallopian tubes are cut or blocked to permanently prevent pregnancy.
 If you wish to conceive after tubal ligation, IVF may be an alternative to tubal ligation reversal surgery.
If you wish to conceive after tubal ligation, IVF may be an alternative to tubal ligation reversal surgery. - Impaired sperm production or function. Below-average sperm concentration, weak movement of sperm (poor mobility), or abnormalities in sperm size and shape can make it difficult for sperm to fertilize an egg. If semen abnormalities are found, a visit to an infertility specialist might be needed to see if there are correctable problems or underlying health concerns.
- Unexplained infertility. Unexplained infertility means no cause of infertility has been found despite evaluation for common causes.
- A genetic disorder. If you or your partner is at risk of passing on a genetic disorder to your child, you may be candidates for preimplantation genetic testing — a procedure that involves IVF. After the eggs are harvested and fertilized, they're screened for certain genetic problems, although not all genetic problems can be found.
 Embryos that don't contain identified problems can be transferred to the uterus.
Embryos that don't contain identified problems can be transferred to the uterus. -
Fertility preservation for cancer or other health conditions. If you're about to start cancer treatment — such as radiation or chemotherapy — that could harm your fertility, IVF for fertility preservation may be an option. Women can have eggs harvested from their ovaries and frozen in an unfertilized state for later use. Or the eggs can be fertilized and frozen as embryos for future use.
Women who don't have a functional uterus or for whom pregnancy poses a serious health risk might choose IVF using another person to carry the pregnancy (gestational carrier). In this case, the woman's eggs are fertilized with sperm, but the resulting embryos are placed in the gestational carrier's uterus.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.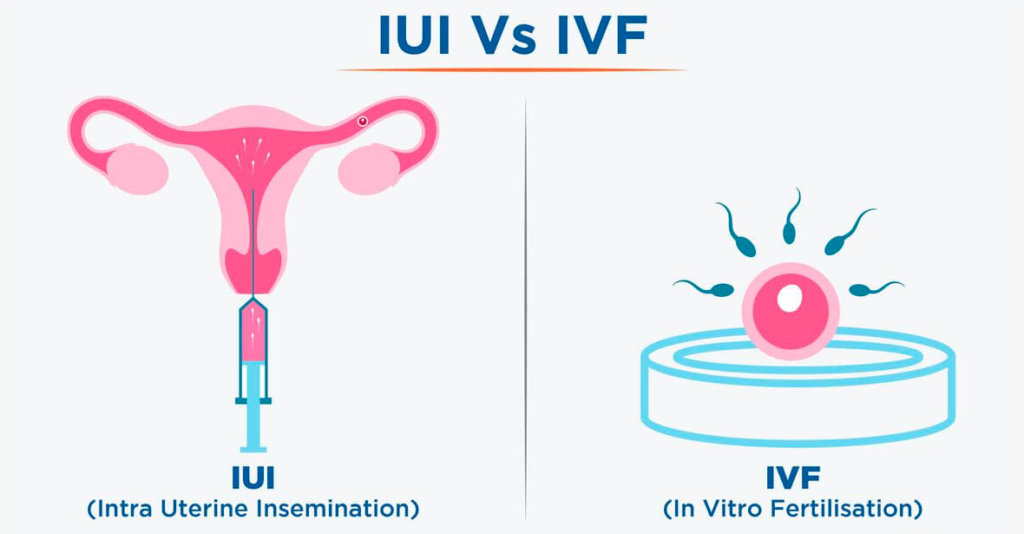
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Risks
Risks of IVF include:
- Multiple births.
 IVF increases the risk of multiple births if more than one embryo is transferred to your uterus. A pregnancy with multiple fetuses carries a higher risk of early labor and low birth weight than pregnancy with a single fetus does.
IVF increases the risk of multiple births if more than one embryo is transferred to your uterus. A pregnancy with multiple fetuses carries a higher risk of early labor and low birth weight than pregnancy with a single fetus does. - Premature delivery and low birth weight. Research suggests that IVF slightly increases the risk that the baby will be born early or with a low birth weight.
-
Ovarian hyperstimulation syndrome. Use of injectable fertility drugs, such as human chorionic gonadotropin (HCG), to induce ovulation can cause ovarian hyperstimulation syndrome, in which your ovaries become swollen and painful.
Symptoms typically last a week and include mild abdominal pain, bloating, nausea, vomiting and diarrhea. If you become pregnant, however, your symptoms might last several weeks. Rarely, it's possible to develop a more severe form of ovarian hyperstimulation syndrome that can also cause rapid weight gain and shortness of breath.

- Miscarriage. The rate of miscarriage for women who conceive using IVF with fresh embryos is similar to that of women who conceive naturally — about 15% to 25% — but the rate increases with maternal age.
- Egg-retrieval procedure complications. Use of an aspirating needle to collect eggs could possibly cause bleeding, infection or damage to the bowel, bladder or a blood vessel. Risks are also associated with sedation and general anesthesia, if used.
- Ectopic pregnancy. About 2% to 5% of women who use IVF will have an ectopic pregnancy — when the fertilized egg implants outside the uterus, usually in a fallopian tube. The fertilized egg can't survive outside the uterus, and there's no way to continue the pregnancy.
- Birth defects. The age of the mother is the primary risk factor in the development of birth defects, no matter how the child is conceived.
 More research is needed to determine whether babies conceived using IVF might be at increased risk of certain birth defects.
More research is needed to determine whether babies conceived using IVF might be at increased risk of certain birth defects. - Cancer. Although some early studies suggested there may be a link between certain medications used to stimulate egg growth and the development of a specific type of ovarian tumor, more-recent studies do not support these findings. There does not appear to be a significantly increased risk of breast, endometrial, cervical or ovarian cancer after IVF.
- Stress. Use of IVF can be financially, physically and emotionally draining. Support from counselors, family and friends can help you and your partner through the ups and downs of infertility treatment.
How you prepare
The Centers for Disease Control and Prevention and the Society for Assisted Reproductive Technology provide information online about U. S. clinics' individual pregnancy and live birth rates.
S. clinics' individual pregnancy and live birth rates.
A clinic's success rate depends on many factors. These include patients' ages and medical issues, as well as the clinic's treatment population and treatment approaches. Ask for detailed information about the costs associated with each step of the procedure.
Before beginning a cycle of IVF using your own eggs and sperm, you and your partner will likely need various screenings, including:
- Ovarian reserve testing. To determine the quantity and quality of your eggs, your doctor might test the concentration of follicle-stimulating hormone (FSH), estradiol (estrogen) and anti-mullerian hormone in your blood during the first few days of your menstrual cycle. Test results, often used together with an ultrasound of your ovaries, can help predict how your ovaries will respond to fertility medication.
- Semen analysis. If not done as part of your initial fertility evaluation, your doctor will conduct a semen analysis shortly before the start of an IVF treatment cycle.
- Infectious disease screening. You and your partner will both be screened for infectious diseases, including HIV.
- Practice (mock) embryo transfer. Your doctor might conduct a mock embryo transfer to determine the depth of your uterine cavity and the technique most likely to successfully place the embryos into your uterus.
- Uterine exam. Your doctor will examine the inside lining of the uterus before you start IVF. This might involve a sonohysterography — in which fluid is injected through the cervix into your uterus — and an ultrasound to create images of your uterine cavity. Or it might include a hysteroscopy — in which a thin, flexible, lighted telescope (hysteroscope) is inserted through your vagina and cervix into your uterus.
Before beginning a cycle of IVF, consider important questions, including:
-
How many embryos will be transferred? The number of embryos transferred is typically based on age and number of eggs retrieved.
 Since the rate of implantation is lower for older women, more embryos are usually transferred — except for women using donor eggs or genetically tested embryos.
Since the rate of implantation is lower for older women, more embryos are usually transferred — except for women using donor eggs or genetically tested embryos.Most doctors follow specific guidelines to prevent a higher order multiple pregnancy, such as triplets or more. In some countries, legislation limits the number of embryos that can be transferred. Make sure you and your doctor agree on the number of embryos that will be transferred before the transfer procedure.
-
What will you do with any extra embryos? Extra embryos can be frozen and stored for future use for several years. Not all embryos will survive the freezing and thawing process, although most will.
Having frozen embryos can make future cycles of IVF less expensive and less invasive. Or, you might be able to donate unused frozen embryos to another couple or a research facility. You might also choose to discard unused embryos.

- How will you handle a multiple pregnancy? If more than one embryo is transferred to your uterus, IVF can result in a multiple pregnancy — which poses health risks for you and your babies. In some cases, fetal reduction can be used to help a woman deliver fewer babies with lower health risks. Pursuing fetal reduction, however, is a major decision with ethical, emotional and psychological consequences.
- Have you considered the potential complications associated with using donor eggs, sperm or embryos, or a gestational carrier? A trained counselor with expertise in donor issues can help you understand the concerns, such as the legal rights of the donor. You may also need an attorney to file court papers to help you become legal parents of an implanted embryo.
What you can expect
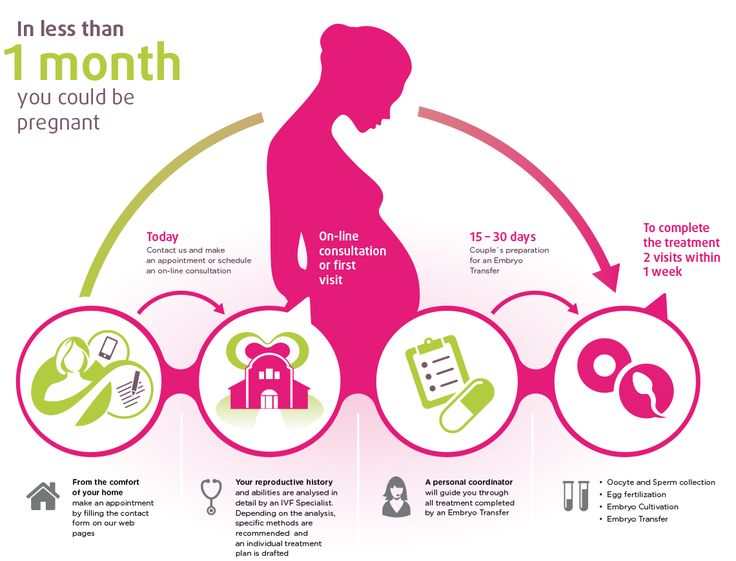
IVF involves several steps — ovarian stimulation, egg retrieval, sperm retrieval, fertilization and embryo transfer. One cycle of IVF can take about two to three weeks. More than one cycle may be needed.
One cycle of IVF can take about two to three weeks. More than one cycle may be needed.
Ovulation induction
The start of an IVF cycle begins by using synthetic hormones to stimulate the ovaries to produce multiple eggs — rather than the single egg that typically develops each month. Multiple eggs are needed because some eggs won't fertilize or develop normally after fertilization.
Several different medications may be used, such as:
- Medications for ovarian stimulation. To stimulate your ovaries, you might receive an injectable medication containing a follicle-stimulating hormone (FSH), a luteinizing hormone (LH) or a combination of both. These medications stimulate more than one egg to develop at a time.
- Medications for oocyte maturation. When the follicles are ready for egg retrieval — generally after eight to 14 days — you will take human chorionic gonadotropin (HCG) or other medications to help the eggs mature.

- Medications to prevent premature ovulation. These medications prevent your body from releasing the developing eggs too soon.
- Medications to prepare the lining of your uterus. On the day of egg retrieval or at the time of embryo transfer, your doctor might recommend that you begin taking progesterone supplements to make the lining of your uterus more receptive to implantation.
Your doctor will work with you to determine which medications to use and when to use them.
Typically, you'll need one to two weeks of ovarian stimulation before your eggs are ready for retrieval. To determine when the eggs are ready for collection, you may have:
- Vaginal ultrasound, an imaging exam of your ovaries to monitor the development of follicles — fluid-filled ovarian sacs where eggs mature
- Blood tests, to measure your response to ovarian stimulation medications — estrogen levels typically increase as follicles develop, and progesterone levels remain low until after ovulation
Sometimes IVF cycles need to be canceled before egg retrieval for one of these reasons:
- Inadequate number of follicles developing
- Premature ovulation
- Too many follicles developing, creating a risk of ovarian hyperstimulation syndrome
- Other medical issues
If your cycle is canceled, your doctor might recommend changing medications or their doses to promote a better response during future IVF cycles.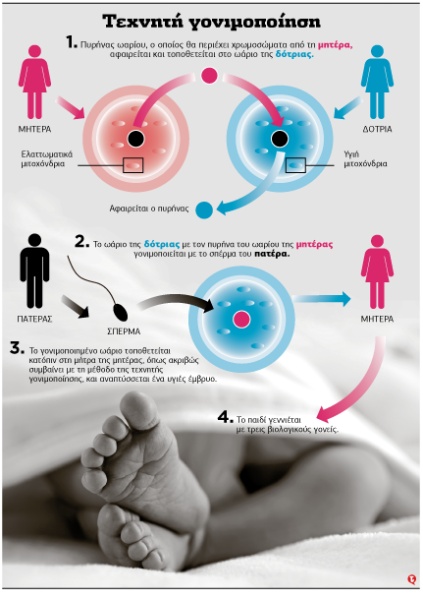 Or you may be advised that you need an egg donor.
Or you may be advised that you need an egg donor.
Egg retrieval
Egg retrieval can be done in your doctor's office or a clinic 34 to 36 hours after the final injection and before ovulation.
- During egg retrieval, you'll be sedated and given pain medication.
- Transvaginal ultrasound aspiration is the usual retrieval method. An ultrasound probe is inserted into your vagina to identify follicles. Then a thin needle is inserted into an ultrasound guide to go through the vagina and into the follicles to retrieve the eggs.
- If your ovaries aren't accessible through transvaginal ultrasound, an abdominal ultrasound may be used to guide the needle.
- The eggs are removed from the follicles through a needle connected to a suction device. Multiple eggs can be removed in about 20 minutes.
- After egg retrieval, you may experience cramping and feelings of fullness or pressure.
- Mature eggs are placed in a nutritive liquid (culture medium) and incubated.
 Eggs that appear healthy and mature will be mixed with sperm to attempt to create embryos. However, not all eggs may be successfully fertilized.
Eggs that appear healthy and mature will be mixed with sperm to attempt to create embryos. However, not all eggs may be successfully fertilized.
Sperm retrieval
If you're using your partner's sperm, a semen sample needs to be provided at your doctor's office or clinic the morning of egg retrieval. Typically, the semen sample is collected through masturbation. Other methods, such as testicular aspiration — the use of a needle or surgical procedure to extract sperm directly from the testicle — are sometimes required. Donor sperm also can be used. Sperm are separated from the semen fluid in the lab.
Fertilization
Fertilization can be attempted using two common methods:
- Conventional insemination. During conventional insemination, healthy sperm and mature eggs are mixed and incubated overnight.
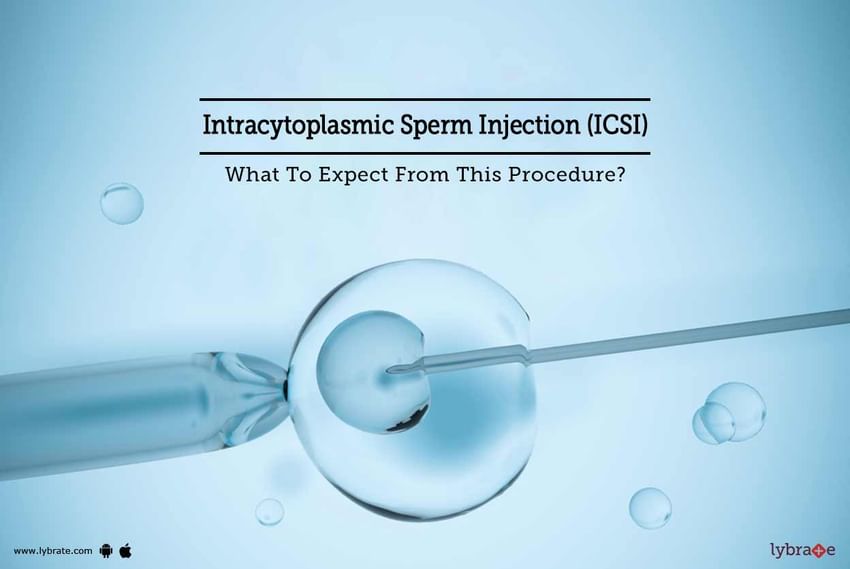
- Intracytoplasmic sperm injection (ICSI). In ICSI, a single healthy sperm is injected directly into each mature egg.
 ICSI is often used when semen quality or number is a problem or if fertilization attempts during prior IVF cycles failed.
ICSI is often used when semen quality or number is a problem or if fertilization attempts during prior IVF cycles failed.
In certain situations, your doctor may recommend other procedures before embryo transfer.
- Assisted hatching. About five to six days after fertilization, an embryo "hatches" from its surrounding membrane (zona pellucida), allowing it to implant into the lining of the uterus. If you're an older woman, or if you have had multiple failed IVF attempts, your doctor might recommend assisted hatching — a technique in which a hole is made in the zona pellucida just before transfer to help the embryo hatch and implant. Assisted hatching is also useful for eggs or embryos that have been previously frozen as the process can harden the zona pellucida.
- Preimplantation genetic testing.
 Embryos are allowed to develop in the incubator until they reach a stage where a small sample can be removed and tested for specific genetic diseases or the correct number of chromosomes, typically after five to six days of development. Embryos that don't contain affected genes or chromosomes can be transferred to your uterus. While preimplantation genetic testing can reduce the likelihood that a parent will pass on a genetic problem, it can't eliminate the risk. Prenatal testing may still be recommended.
Embryos are allowed to develop in the incubator until they reach a stage where a small sample can be removed and tested for specific genetic diseases or the correct number of chromosomes, typically after five to six days of development. Embryos that don't contain affected genes or chromosomes can be transferred to your uterus. While preimplantation genetic testing can reduce the likelihood that a parent will pass on a genetic problem, it can't eliminate the risk. Prenatal testing may still be recommended.
Embryo transfer
Egg-retrieval technique
Egg-retrieval technique
Typically, transvaginal ultrasound aspiration is used to retrieve eggs. During this procedure, an ultrasound probe is inserted into your vagina to identify follicles, and a needle is guided through the vagina and into the follicles. The eggs are removed from the follicles through the needle, which is connected to a suction device.
ICSI
ICSI
In intracytoplasmic sperm injection (ICSI), a single healthy sperm is injected directly into each mature egg.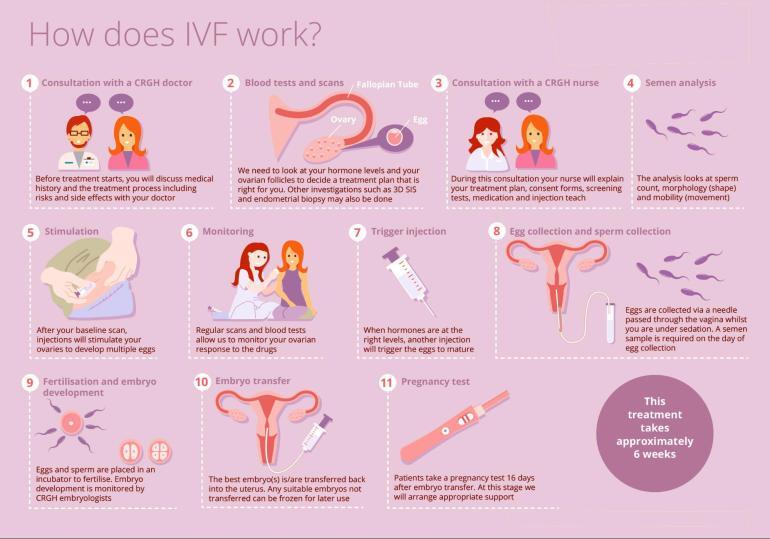 ICSI is often used when semen quality or number is a problem or if fertilization attempts during prior in vitro fertilization cycles failed.
ICSI is often used when semen quality or number is a problem or if fertilization attempts during prior in vitro fertilization cycles failed.
Blastocyst
Blastocyst
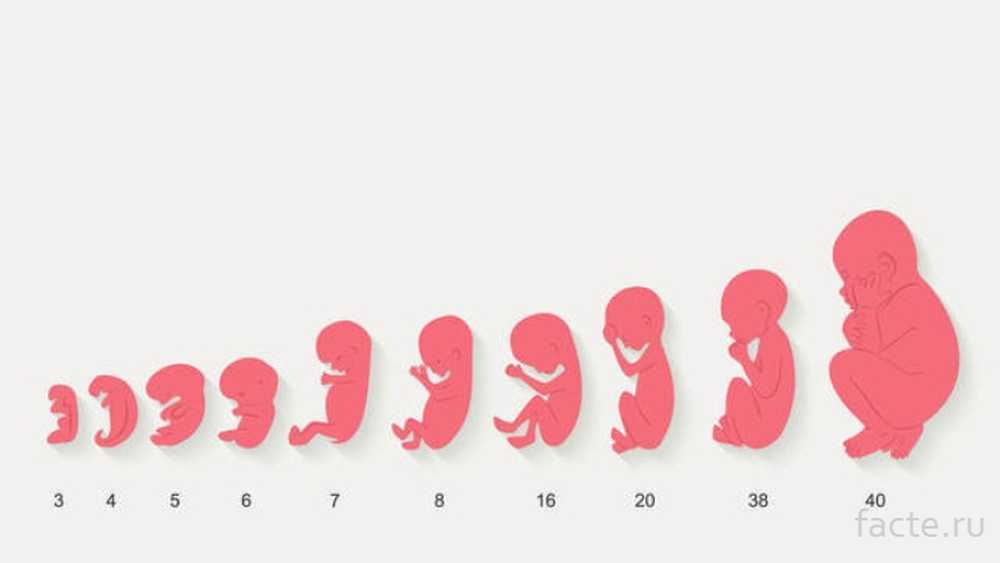
Three days after fertilization, a normally developing embryo will contain about six to 10 cells. By the fifth or sixth day, the fertilized egg is known as a blastocyst — a rapidly dividing ball of cells. The inner group of cells will become the embryo. The outer group will become the cells that nourish and protect it.
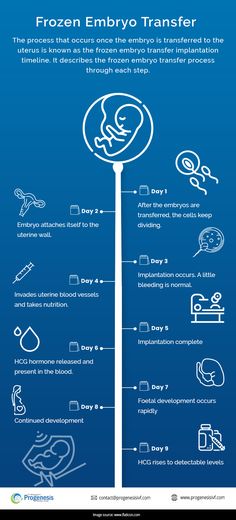
Embryo transfer is done at your doctor's office or a clinic and usually takes place two to five days after egg retrieval.
- You might be given a mild sedative. The procedure is usually painless, although you might experience mild cramping.
- The doctor will insert a long, thin, flexible tube called a catheter into your vagina, through your cervix and into your uterus.
- A syringe containing one or more embryos suspended in a small amount of fluid is attached to the end of the catheter.
- Using the syringe, the doctor places the embryo or embryos into your uterus.
If successful, an embryo will implant in the lining of your uterus about six to 10 days after egg retrieval.
After the procedure
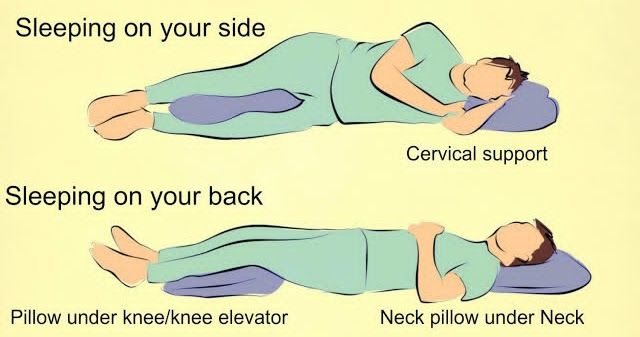
After the embryo transfer, you can resume your usual daily activities. However, your ovaries may still be enlarged. Consider avoiding vigorous activity, which could cause discomfort.
Typical side effects include:
- Passing a small amount of clear or bloody fluid shortly after the procedure — due to the swabbing of the cervix before the embryo transfer
- Breast tenderness due to high estrogen levels
- Mild bloating
- Mild cramping
- Constipation
If you develop moderate or severe pain after the embryo transfer, contact your doctor. He or she will evaluate you for complications such as infection, twisting of an ovary (ovarian torsion) and severe ovarian hyperstimulation syndrome.
Results
About 12 days to two weeks after egg retrieval, your doctor will test a sample of your blood to detect whether you're pregnant.
- If you're pregnant, your doctor will refer you to an obstetrician or other pregnancy specialist for prenatal care.
- If you're not pregnant, you'll stop taking progesterone and likely get your period within a week. If you don't get your period or you have unusual bleeding, contact your doctor. If you're interested in attempting another cycle of in vitro fertilization (IVF), your doctor might suggest steps you can take to improve your chances of getting pregnant through IVF.
The chances of giving birth to a healthy baby after using IVF depend on various factors, including:
- Maternal age. The younger you are, the more likely you are to get pregnant and give birth to a healthy baby using your own eggs during IVF.
 Women age 41 and older are often counseled to consider using donor eggs during IVF to increase the chances of success.
Women age 41 and older are often counseled to consider using donor eggs during IVF to increase the chances of success. - Embryo status. Transfer of embryos that are more developed is associated with higher pregnancy rates compared with less-developed embryos (day two or three). However, not all embryos survive the development process. Talk with your doctor or other care provider about your specific situation.
- Reproductive history. Women who've previously given birth are more likely to be able to get pregnant using IVF than are women who've never given birth. Success rates are lower for women who've previously used IVF multiple times but didn't get pregnant.
- Cause of infertility. Having a normal supply of eggs increases your chances of being able to get pregnant using IVF.
 Women who have severe endometriosis are less likely to be able to get pregnant using IVF than are women who have unexplained infertility.
Women who have severe endometriosis are less likely to be able to get pregnant using IVF than are women who have unexplained infertility. - Lifestyle factors. Women who smoke typically have fewer eggs retrieved during IVF and may miscarry more often. Smoking can lower a woman's chance of success using IVF by 50%. Obesity can decrease your chances of getting pregnant and having a baby. Use of alcohol, recreational drugs, excessive caffeine and certain medications also can be harmful.
Talk with your doctor about any factors that apply to you and how they may affect your chances of a successful pregnancy.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
By Mayo Clinic Staff
Related
Products & Services
What to Expect When You’re Doing IVF Treatments
Take a quick stroll in any Barnes & Noble, or peruse Amazon’s fertility section and you’ll see there is a big disparity between the amount of books about pregnancy versus the books on infertility treatments. While more amazing publications are popping up on what to expect while you’re in the middle of fertility treatments, there is still a lot to be desired. Online forums can be a good place to chat with others who are experiencing similar symptoms or who have blazed the trail before you, however, most content is not medically approved and should not be used for diagnostic purposes. We’ve included a list of the top 10 things you may experience during in vitro fertilization (IVF) treatments at our Connecticut fertility center:
While more amazing publications are popping up on what to expect while you’re in the middle of fertility treatments, there is still a lot to be desired. Online forums can be a good place to chat with others who are experiencing similar symptoms or who have blazed the trail before you, however, most content is not medically approved and should not be used for diagnostic purposes. We’ve included a list of the top 10 things you may experience during in vitro fertilization (IVF) treatments at our Connecticut fertility center:
1. Body changes –
It’s not uncommon for women to gain a little weight during IVF treatments. Hormone injections can affect your weight and also your hunger levels (read # 4). Additionally, depending on how many eggs develop or if you experience any mild ovarian hyperstimulation, you will notice that your stomach will feel bloated and that your jeans feel snug. This is normal and will subside when you start your next period, or within a few weeks of your pregnancy. If you gain weight rapidly (for instance 10 pounds in 2-3 days) call our office immediately.
If you gain weight rapidly (for instance 10 pounds in 2-3 days) call our office immediately.
2. Feeling emotional –
If additional hormones in your body aren’t enough to make you feel emotional, the experience of a first IVF treatment can feel overwhelming for some patients. Expect to feel emotional. It’s allowed.
3. Feeling distracted –
We’ve heard some women say that they feel like they have “pregnancy brain” while doing IVF. It’s not surprising considering many patients juggle careers and other obligations, in addition to treatments and thinking about treatment results. Being distracted or forgetful is fairly common.
4. Increased appetite–
This doesn’t happen to everyone, but some patients may experience an increase in hunger. While some of the medications may increase your hunger, more often an increased desire to eat is more emotionally driven. Just remember to eat healthily.
5. Shots –
You will be required to inject follicle stimulating and ovulation regulating hormones each day via small needles. The amount of medication and frequency of shots is different for each patient. Also, during visits you may have your blood drawn to get a clear analysis of your hormone levels. Most patients are surprised at how painless the daily shots actually are.
The amount of medication and frequency of shots is different for each patient. Also, during visits you may have your blood drawn to get a clear analysis of your hormone levels. Most patients are surprised at how painless the daily shots actually are.
6. Oral medications –
In addition to shots, you may have to take oral medication. Dr. Levi will adjust your dosages after appointments and may recommend additional medications as needed.
7. Gastrointestinal changes –
Constipation or loose stools are all common complaints of people who are in the process of IVF. Make sure to drink plenty of water and to eat foods that are high in fiber to combat digestive issues.
8. Some waiting –
We do our best at Park Avenue Fertility to keep your in-office wait to a minimum, however occasionally there will be some waiting, especially for blood test results. We always make sure to return calls and share your results with you as quickly as possible.
9. Feelings of stress or frustration –
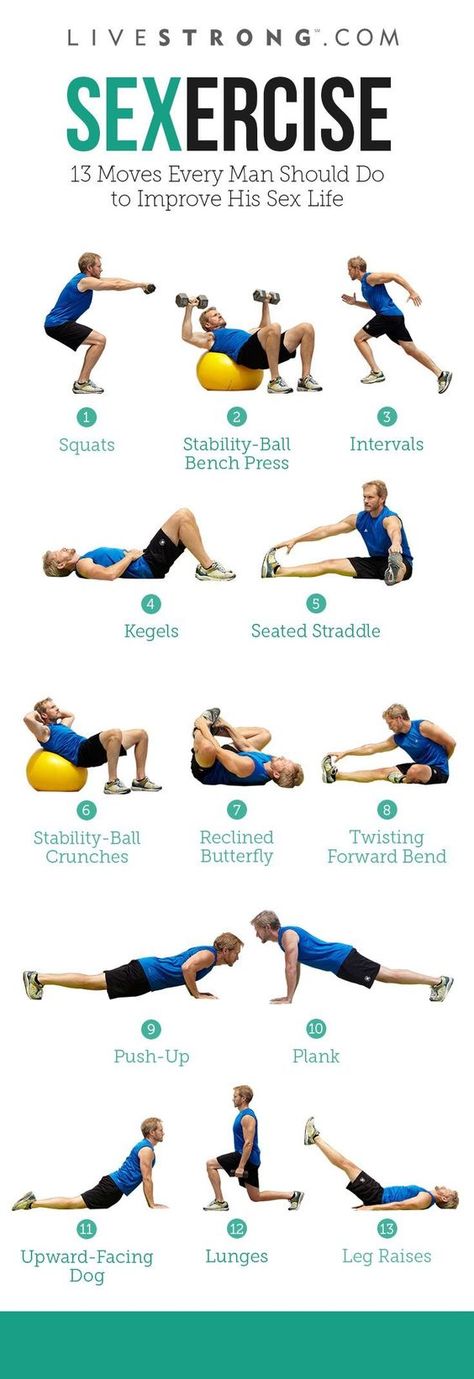
Fertility treatments can be stressful for some patients and can be frustrating if you are physically feeling the effects of your medications.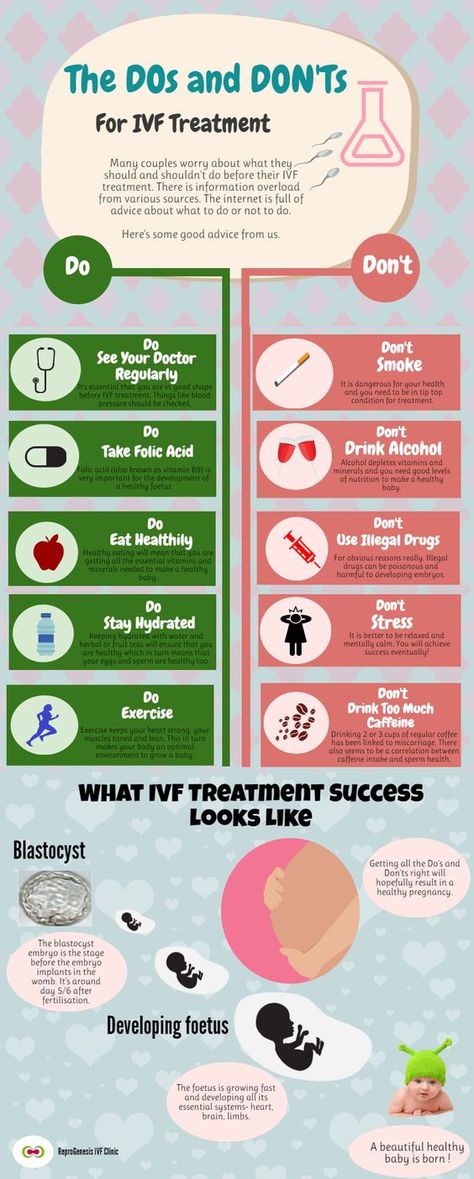 Utilizing stress relieving practices like light yoga, meditation, or acupuncture can help alleviate anxieties.
Utilizing stress relieving practices like light yoga, meditation, or acupuncture can help alleviate anxieties.
10. Surprises –
Fertility treatments are different for each patient and there really is no “average” experience. Don’t be surprised if you find you’re hungrier during treatments. Don’t be surprised if you need more sleep each night. And don’t be surprised if you find that this process is considerably easier than you expected. As they say, “expect the unexpected.”
Fertility treatments have provided an amazing opportunity for patients who have struggled with infertility to experience pregnancy. Additionally, the process of follicle stimulation involved in IVF is also the same procedure used during egg donation. To learn more about how IVF works, scan our website for more in-depth information or call our office at 855-901-BABY to set up an appointment at one of our Norwalk, Fairfield, or Trumbull locations with renowned Connecticut fertility specialist Dr. Levi.
Fomin Clinic - a network of multidisciplinary clinics
There are many conflicting rumors around IVF: some consider it a panacea, while others, on the contrary, are sure that this procedure is deadly for mother and baby. Let's look at what IVF is, who really needs it, and how high the risks associated with this method of infertility treatment are.
In vitro fertilization (IVF) is a complex and high-tech method of infertility treatment, which includes several stages:
Consultation and examination. An obstetrician-gynecologist (reproductologist) tells a couple about the technique, explains its advantages and risks. If the future parents agree, they are invited to undergo an examination and pass the necessary tests. If there are no contraindications to the procedure, the couple is offered to enter the IVF protocol - that is, to begin treatment.
Ovarian stimulation. During the monthly cycle, one mature egg is released from the ovaries. To increase the chances of conception, a woman can be prescribed drugs that "force" to mature several eggs - this increases the chances of successful fertilization.
To increase the chances of conception, a woman can be prescribed drugs that "force" to mature several eggs - this increases the chances of successful fertilization.
Sometimes it is possible to do without drug stimulation of the ovaries - this technique is called "IVF in a natural cycle". Unfortunately, "natural" IVF is not suitable for everyone, so the choice of technique should be entrusted to the doctor. The doctor will take into account the results of examinations and analyzes and select the IVF method that is right for you.
Egg collection. When the eggs are mature, the doctor will remove them from the ovary with a special needle. This is a small but complete operation, which is carried out in a small operating room under anesthesia.
Oocyte fertilization and embryo culture. Both of these steps take place in the laboratory.
A lab worker will take a sperm sample from the future father and add it to the eggs for fertilization to occur.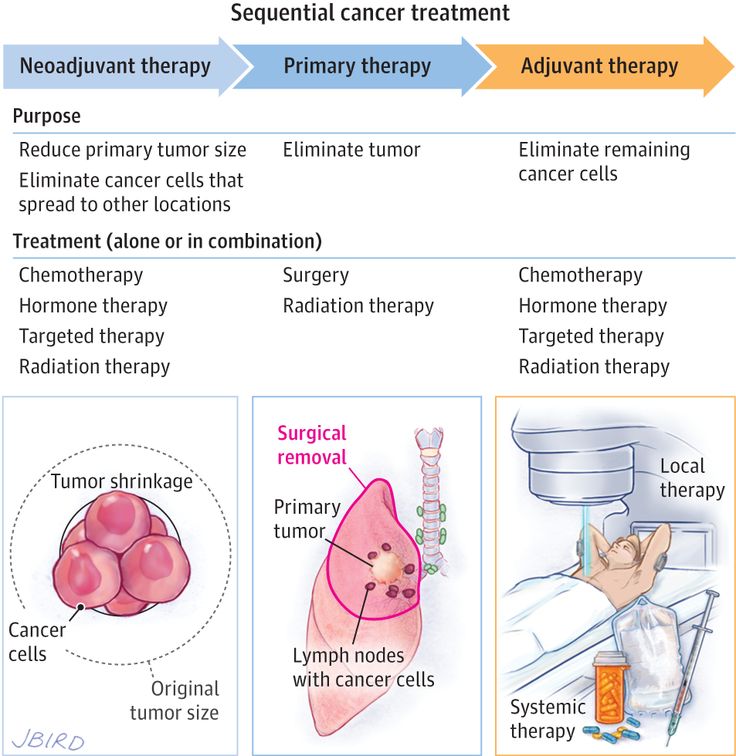 If the spermatozoa are not active enough or have an irregular shape, they can be “helped” by introducing them into the egg with a special needle. The procedure is called intracytoplasmic sperm injection, or ICSI.
If the spermatozoa are not active enough or have an irregular shape, they can be “helped” by introducing them into the egg with a special needle. The procedure is called intracytoplasmic sperm injection, or ICSI.
If fertilization is successful, the cell will divide and grow. 3-4 days after fertilization, expectant parents may be offered pre-implantation genetic diagnosis (PGD). This will make sure that everything is fine, and the embryo can be transferred to the mother.
Embryo transfer to the uterus. 3-5 days after fertilization, the embryo is placed in the mother's uterus. This procedure is also performed in a small operating room, anesthesia is usually not needed.
Now all we have to do is wait. Two weeks after the embryo transfer, you will need to take a blood test for human chorionic gonadotropin (hCG). This hormone is produced by the shell of the embryo (chorion), and appears in the blood only after the successful implantation of the embryo into the uterine cavity. If the hCG level is high, the procedure was successful!
If the hCG level is high, the procedure was successful!
After successful implantation of the embryo, pregnancy and childbirth proceed in the same way as after conception "naturally". The baby born into the world, as a rule, is almost no different from other babies.
IVF is a last resort, which is resorted to if other methods of infertility treatment have not helped. At the same time, a woman must be healthy enough to undergo IVF without serious complications.
In our country, the procedure for selecting patients for IVF is described in the order of the Ministry of Health of the Russian Federation of August 30, 2012 No. 107n. According to the order, IVF is recommended for couples who have not been helped:
- laparoscopic and hysteroscopic correction;
- ovulation stimulation;
- treatment of male factor infertility.
Treatment is considered ineffective if pregnancy has not occurred within 9-12 months. True, this does not apply to women over 35 years old - in this case, the doctor can refer you to IVF earlier. If there are no obstacles to IVF, the procedure can be done free of charge under the CHI policy.
True, this does not apply to women over 35 years old - in this case, the doctor can refer you to IVF earlier. If there are no obstacles to IVF, the procedure can be done free of charge under the CHI policy.
The list of IVF contraindications is quite large. Among them are infectious and non-infectious diseases, diseases of the nervous system and circulatory system, diseases of the endocrine system and metabolic disorders, oncological diseases and many other diseases. The full list is in order No. 107n.
If the disease is curable, then IVF can be done after recovery. That is why before the procedure it is very important to undergo an examination and pass all the tests that the doctor will prescribe. If cured in time, the probability of conception as a result of IVF will be much higher, and the risk for mother and child is much lower.
Risks for the mother. According to international studies, the maternal morbidity and mortality rate directly associated with IVF is low - but still somewhat higher than in women who conceived a child "naturally".
Researchers believe that this is because IVF is more often used by older people who may have diseases other than infertility. In addition, the statistics are "spoiled" by women with multiple pregnancies - IVF often results in twins, which are more difficult to endure than one child.
In addition, some risk is associated with hormonal stimulation of the ovaries and the stage of egg retrieval. Stimulation can cause ovarian hyperstimulation syndrome, and the egg retrieval phase increases the risk of thrombosis, abdominal bleeding, infection, and anesthesia complications, just like any other surgical procedure.
However, according to available data, IVF does not cause cancer. There was no significant association between IVF, breast and cervical cancer.
Risk for baby. The most well-known health risk associated with IVF is Angelman syndrome. This is a very rare genetic defect - the estimated risk with IVF is 2-5 cases per 15,000 people, while with a "natural" conception, the risk will be 1 case per 15,000 people.
A large national study in Norway found that children conceived through assisted reproductive technology have a higher risk of developing leukemia and Hodgkin's lymphoma compared to "normal" children. However, these diseases are also rare - so the real chance that a particular child will get sick is very small.
In general, the risks of birth defects with IVF are associated with the underlying cause of infertility, and smaller size and frailty with multiple pregnancies, so that the risks of IVF are only marginally higher than the risks of "natural" conception.
But what is known for sure is that IVF does not affect the mental abilities of children. The researchers studied the school performance of such children and found that they study even better than peers conceived "naturally". True, IVF has nothing to do with it: it’s just that people who could afford an expensive procedure were usually richer and had a higher level of education, so they tried to put their children in the best school and paid a lot of attention to their development.
- IVF is an effective method of infertility treatment, but it is not suitable for everyone. It is worth thinking about IVF if other methods of infertility treatment have not helped to get pregnant within a year.
- Before IVF, both future parents must undergo examinations and pass the necessary tests. The decision on IVF should be made carefully, taking into account all the advantages and risks of this method.
- Although IVF has certain risks for mother and baby, the overall risk is not much higher than with "natural" conception.
Follow us
IVF methods
ECO
In vitro fertilization (IVF) is now considered one of the most effective ways to solve the problem of infertility. IVF primarily helps people who have not been able to conceive a child naturally. The IVF procedure assumes that the sperm and egg are not found in the woman's body, but in an extracorporeal way, in the laboratory, and then, after fertilization, the embryo is placed in the uterine cavity.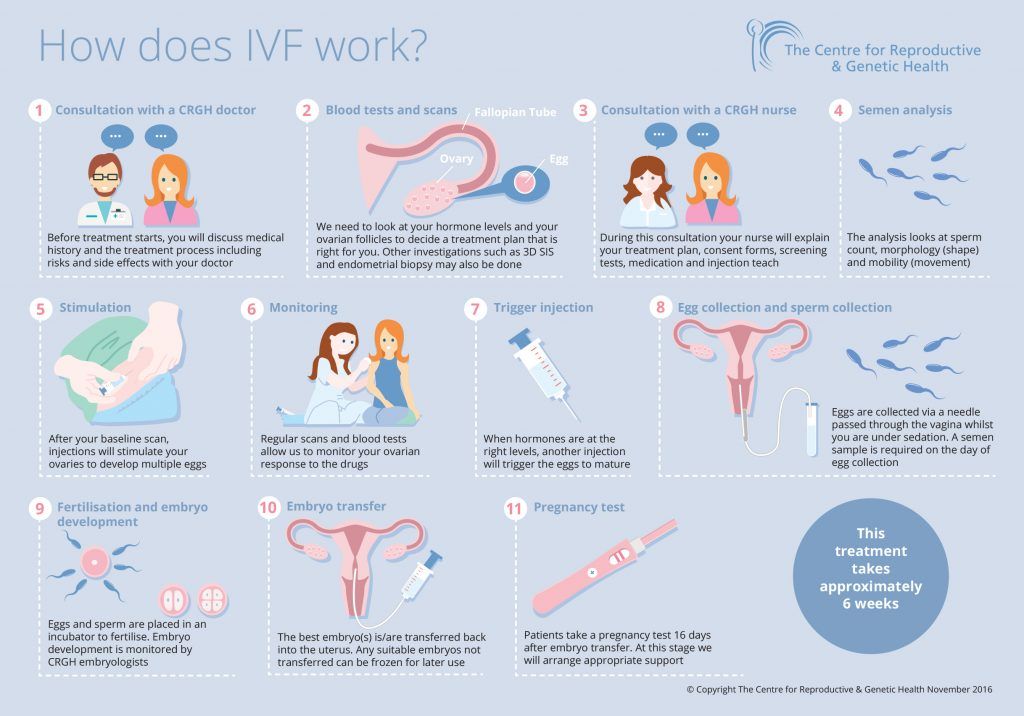 At the moment, different methods of artificial insemination are used in medical practice, while the goal of each of them is the same - the onset of pregnancy.
At the moment, different methods of artificial insemination are used in medical practice, while the goal of each of them is the same - the onset of pregnancy.
ECO+ICSI
As part of the ICSI technique, a single spermatozoon is selected and then it is introduced into the egg using special microsurgical instruments. This technique is relevant for families faced with the problem of male infertility. For such couples, ICSI becomes the only effective method of fertilization against the background of a decrease in the spermogram of the male partner. This technique contributes to obtaining a genetically native child with azoospermia. Embryos obtained through ICSI are exactly the same as embryos that are typical for standard IVF.
ECO+IMSI
In the course of this technique, the best spermatozoa according to morphological criteria are selected for fertilization by means of their clearer visualization. Spermatozoa are collected in specialized institutions and using professional equipment. As part of the IMSI methodology, the emphasis is on the quality indicators of sperm, which are evaluated, which helps to increase the likelihood of pregnancy in IVF cycles and reduce the risk of miscarriage. The technique is especially effective in the treatment of infertility in couples suffering from such a pathology of men's health as a severe disorder of spermatogenesis.
As part of the IMSI methodology, the emphasis is on the quality indicators of sperm, which are evaluated, which helps to increase the likelihood of pregnancy in IVF cycles and reduce the risk of miscarriage. The technique is especially effective in the treatment of infertility in couples suffering from such a pathology of men's health as a severe disorder of spermatogenesis.
IVF with donor eggs
Egg donation is chosen when female infertility is diagnosed, which makes it impossible to achieve pregnancy through the use of one's own eggs. In order to obtain eggs from a donor, just like from an ordinary patient, reproductologists organize hormonal stimulation of the ovaries in the IVF cycle. After the maturation of the eggs (oocytes) has occurred, they are collected by transvaginal puncture. Then the embryologists carry out the process of fertilization of the received donor eggs with the sperm of the patient's husband and the cultivation of the embryos in the laboratory.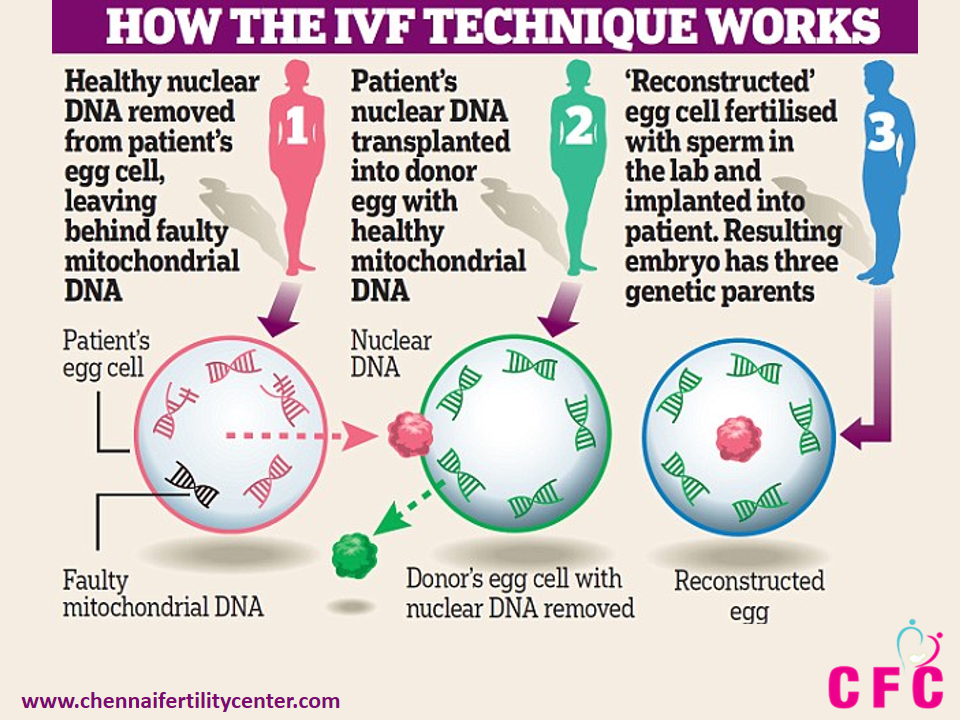 In parallel with this, the endometrium of the patient's uterus is prepared for the purpose of implanting embryos with estradiol and progesterone. On the third or fifth day, the embryologists decide on the best embryos to place in the woman's uterine cavity.
In parallel with this, the endometrium of the patient's uterus is prepared for the purpose of implanting embryos with estradiol and progesterone. On the third or fifth day, the embryologists decide on the best embryos to place in the woman's uterine cavity.
IVF with IVM
IVF is a relatively new fertilization technique. The difference between this technique and traditional IVF is that the work is done with immature eggs obtained from a woman's ovaries. They are placed in a special medium containing hormones in the embryological laboratory for maturation. In this case, the action of hormones extends only to the eggs. The hormonal effect on a woman's body is minimal or not present at all. On average, the maturation of eggs is 1-2 days. The process of cultivation - fertilization and crushing - is similar to ordinary in vitro fertilization. Next, experts transfer the embryo, as in standard IVF.
What is PGD and why should it be done?
So let's talk about pre-implantation genetic diagnosis.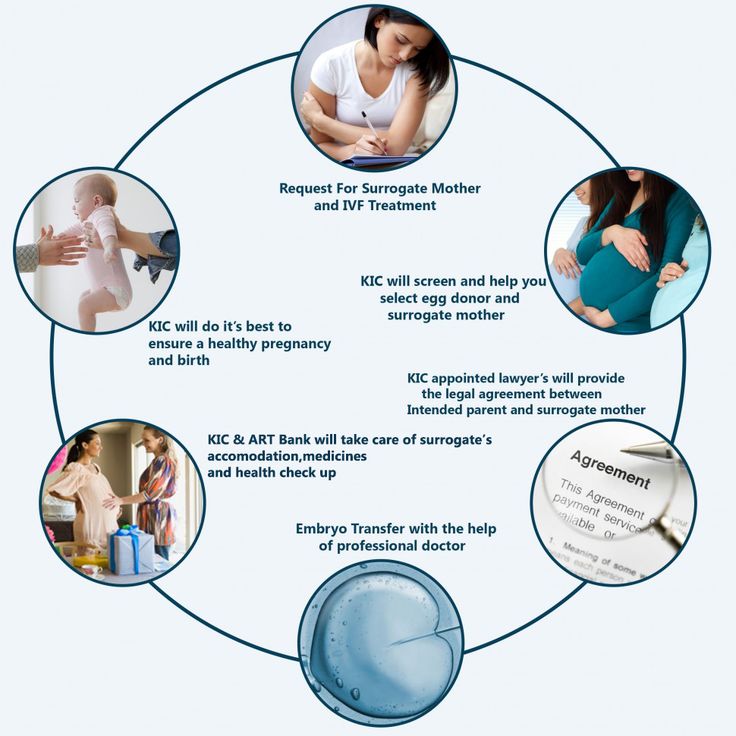 This term refers to a technique aimed at selecting embryos without genetic abnormalities. The technique is recommended for couples who want to increase the likelihood of having a healthy child, as well as for couples with a high risk of having children with genetic diseases.
This term refers to a technique aimed at selecting embryos without genetic abnormalities. The technique is recommended for couples who want to increase the likelihood of having a healthy child, as well as for couples with a high risk of having children with genetic diseases.
What is PESA, TESE, micro-TESE, TESA?
These methods consist in the fact that the receipt of spermatozoa from the appendages will occur surgically. The resulting sperm can then be used to fertilize the egg. Such techniques are recommended in cases where there are no spermatozoa in the semen. A specific technique will be recommended by an andrologist.
What is the effect of ovarian stimulation?
For a healthy female body, it is normal that one egg matures approximately by the middle of the menstrual cycle. The main task in IVF is to increase the chances of success by obtaining several eggs at once.
Is IVF performed without stimulation?
There are diseases in which hormonal stimulation of the ovaries is prohibited, while it is possible to perform IVF in a natural cycle.