Baby sleep progression
Newborn Sleep Patterns | Johns Hopkins Medicine
What are the sleep patterns of a newborn?
The average newborn sleeps much of the day and night, waking only for feedings every few hours. It is often hard for new parents to know how long and how often a newborn should sleep. Unfortunately, there is no set schedule at first, and many newborns have their days and nights confused. They think they are supposed to be awake at night and sleep during the day.
Generally, newborns sleep a total of about 8 to 9 hours in the daytime and a total of about 8 hours at night. But because they have a small stomach, they must wake every few hours to eat. Most babies don’t begin sleeping through the night (6 to 8 hours) until at least 3 months of age. But this can vary a lot. Some babies don’t sleep through the night until closer to 1 year. In most cases, your baby will wake up and be ready to eat at least every 3 hours. How often your baby will eat depends on what he or she is being fed and his or her age. Make sure you talk with your healthcare provider to figure out if you need to wake your baby for feedings.
Watch for changes in your baby's sleep pattern. If your baby has been sleeping consistently, and suddenly is waking more often, there may be a problem such as an ear infection. Or your baby may be going through a growth spurt and need to eat more often. Some sleep disturbances are simply due to changes in development or because of overstimulation.
What are the different alert phases of a newborn?
Babies are also different in how alert they are during the time they are awake.
Quiet alert phase
When a newborn wakes up at the end of the sleep cycle, there is typically a quiet alert phase. This is a time when the baby is very still, but awake and taking in the environment. During the quiet alert time, babies may look or stare at objects, and respond to sounds and motion. This phase usually progresses to the active alert phase. This is when the baby is attentive to sounds and sights, and moves actively.
Crying phase
After the quiet alert phase is a crying phase. The baby's body moves erratically, and he or she may cry loudly. Babies can easily be overstimulated during the crying phase. It is usually best to find a way of calming the baby and the environment. Holding your baby close or wrapping your baby snugly in a blanket (swaddling) may help calm a crying baby.
It is usually best to feed babies before they reach the crying phase. During the crying phase, they can be so upset that they may refuse the breast or bottle. In newborns, crying is a late sign of hunger.
Caution on swaddling
Swaddling means wrapping newborn babies snugly in a blanket to keep their arms and legs from flailing. This can make a baby feel safe and help him or her fall asleep. You can buy a special swaddling blanket designed to make swaddling easier.
But don’t use swaddling if your baby is 2 months or older, or if your baby can roll over on his or her own. Swaddling may raise the risk for SIDS (sudden infant death syndrome) if the swaddled baby rolls onto his or her stomach.
When you swaddle, give your baby enough room to move his or her hips and legs. The legs should be able to bend up and out at the hips. Don’t place your baby’s legs so that they are held together and straight down. This raises the risk that the hip joints won’t grow and develop correctly. This can cause a problem called hip dysplasia and dislocation.
Also be careful of swaddling your baby if the weather is warm or hot. Using a thick blanket in warm weather can make your baby overheat. Instead use a lighter blanket or sheet to swaddle the baby.
Helping your baby sleep
Babies may not be able to form their own sleeping and waking patterns, especially in going to sleep. You can help your baby sleep by knowing the signs of sleep readiness, teaching him or her to fall asleep on his or her own, and providing the right environment for comfortable and safe sleep.
What are the signs of sleep readiness?
Your baby may show signs of being ready for sleep when you see the following signs:
Rubbing eyes
Yawning
Looking away
Fussing
How can you help your baby fall asleep?
Not all babies know how to put themselves to sleep. When it is time for bed, many parents want to rock their baby to sleep. Newborns and younger infants will fall asleep while breastfeeding. Having a routine at bedtime is a good idea. But if an older baby falls asleep while eating or in your arms, this may become a pattern. Your baby may then begin to expect to be in your arms in order to fall asleep. When your baby briefly awakens during a sleep cycle, he or she may not be able to go back to sleep on his or her own.
When it is time for bed, many parents want to rock their baby to sleep. Newborns and younger infants will fall asleep while breastfeeding. Having a routine at bedtime is a good idea. But if an older baby falls asleep while eating or in your arms, this may become a pattern. Your baby may then begin to expect to be in your arms in order to fall asleep. When your baby briefly awakens during a sleep cycle, he or she may not be able to go back to sleep on his or her own.
After the newborn period, most experts recommend allowing your baby to become sleepy in your arms, then placing him or her in the bed while still awake. This way your baby learns how to go to sleep on his or her own. Playing soft music while your baby is getting sleepy is also a good way to help create a bedtime routine.
Baby sleep: what to expect at 2-12 months
Baby sleep needs
Babies need sleep to grow and develop well. But babies’ sleep needs vary, just as the sleep needs of older children and adults do.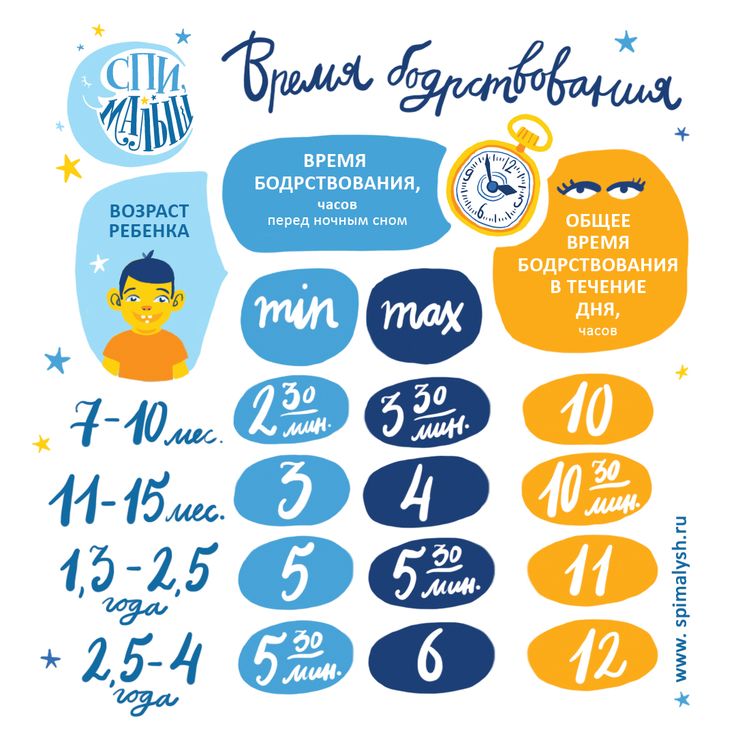 Your baby might be doing well with more or less sleep than other babies the same age.
Your baby might be doing well with more or less sleep than other babies the same age.
Your baby’s mood and wellbeing is often a good guide to whether your baby is getting enough sleep. If your baby is:
- wakeful and grizzly, they might need more sleep
- wakeful and contented, they’re probably getting enough sleep.
How baby sleep changes from 2 to 12 months
As they get older, babies:
- sleep less in the daytime
- are awake for longer between naps
- have longer night-time sleeps and wake less at night
- need less sleep overall.
2-3 months: what to expect from baby sleep
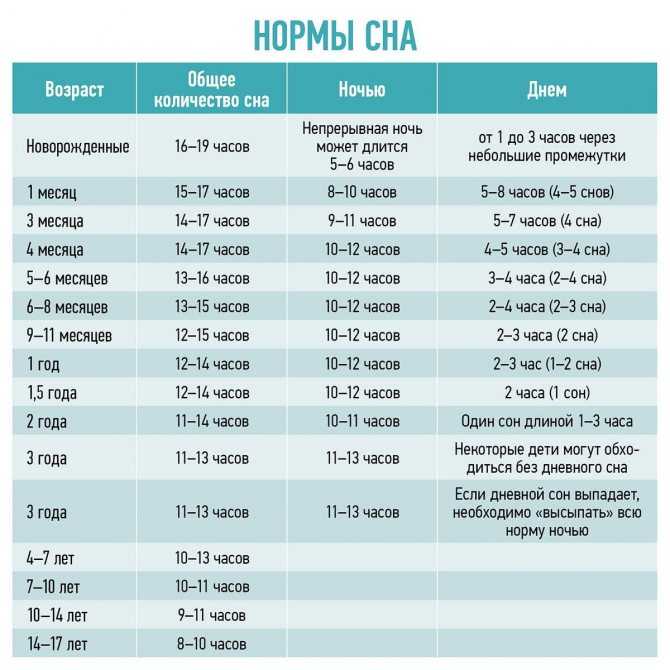
At this age, babies sleep on and off during the day and night. Most babies sleep for 14-17 hours in every 24 hours.
Young babies sleep in cycles that last 50-60 minutes. In young babies, each cycle is made up of active sleep and quiet sleep. Babies move around and grunt during active sleep, and sleep deeply during quiet sleep.
At the end of each cycle, babies wake up for a little while. They might grizzle or cry. They might need help to settle for the next sleep cycle.
At 2-3 months, babies start developing night and day sleep patterns. This means they tend to start sleeping more during the night.
Around 3 months: what to expect from baby sleep
Babies keep developing night and day sleep patterns.
Their sleep cycles consist of:
- light sleep, when baby wakes easily
- deep sleep, when baby is sound asleep and very still
- dream sleep, when baby is dreaming.
Sleep cycles also get longer, which might mean less waking and resettling during sleep. At this age, some babies might regularly be having longer sleeps at night – for example, 4-5 hours.
Most babies still sleep for 14-17 hours in every 24 hours.
3-6 months: what to expect from baby sleep
At this age, most babies sleep for 12-15 hours every 24 hours.
Babies might start moving towards a pattern of 2-3 daytime sleeps of up to two hours each.
And night-time sleeps get longer at this age. For example, some babies might be having long sleeps of six hours at night by the time they’re six months old.
But you can expect that your baby will still wake at least once each night.
6-12 months: what to expect from baby sleep
Babies sleep less as they get older. By the time your baby is one year old, baby will probably sleep for 11-14 hours every 24 hours.
Sleep during the night
From about six months, most babies have their longest sleeps at night.
Most babies are ready for bed between 6 pm and 10 pm. They usually take less than 40 minutes to get to sleep, but some babies take longer.
At this age, baby sleep cycles are closer to those of grown-up sleep – which means less waking at night. So your baby might not wake you during the night, or waking might happen less often.
But many babies do wake during the night and need an adult to settle them back to sleep. Some babies do this 3-4 times a night.
Sleep during the day
At this age, most babies are still having 2-3 daytime naps that last for between 30 minutes and 2 hours.
6-12 months: other developments that affect sleep
From around six months, babies develop many new abilities that can affect their sleep or make them more difficult to settle:
- Babies learn to keep themselves awake, especially if something interesting is happening, or they’re in a place with a lot of light and noise.
- Settling difficulties can happen at the same time as crawling. You might notice your baby’s sleep habits changing when baby starts moving around more.
- Babies learn that things exist, even when they’re out of sight. Now that your baby knows you exist when you leave the bedroom, baby might call or cry out for you.
- Separation anxiety is when babies get upset because you’re not around.
 It might mean your baby doesn’t want to go to sleep and wakes up more often in the night. As babies mature they gradually overcome this worry.
It might mean your baby doesn’t want to go to sleep and wakes up more often in the night. As babies mature they gradually overcome this worry.
6-12 months: night-time feeding
From around six months of age, if your baby is developing well, it’s OK to think about night weaning and phasing out night feeds. But if you’re comfortable with feeding your baby during the night, there’s no hurry to phase out night feeds.
You can choose what works best for you and your baby.
A rollover feed is a late feed somewhere between 10 pm and midnight. Some parents find that rollover feeds help babies sleep longer towards morning. If this works for you and your baby, it’s fine to give baby a rollover feed.
Concerns about baby sleep
If you’re concerned about your baby’s sleep, it can be a good idea to track your baby’s sleep for a week or so. This can help you get a clear picture of what’s going on.
You can do this by drawing up a simple chart with columns for each day of the week. Divide the days into hourly blocks, and colour the intervals when your baby is asleep. Keep your chart for 5-7 days.
Divide the days into hourly blocks, and colour the intervals when your baby is asleep. Keep your chart for 5-7 days.
Once completed, the chart will tell you things like:
- when and how much sleep your baby is getting
- how many times your baby is waking during the night
- how long your baby is taking to settle after waking.
You can also record how you tried to resettle your baby and what worked or didn’t work.
Then you can compare the information in your chart with the general information about baby sleep needs above:
- How does your child compare to other babies the same age? If your baby is wakeful and grizzly and getting much less sleep than others, your baby might need more opportunities for sleep.
- How many times is your baby over six months old waking up during the night? If it’s 3-4 times a night or more, you might be feeling very tired. You might want to think about phasing out some of your baby’s sleep habits.

If you decide you need to see a professional for help with your baby’s sleep, take your chart with you.
If you’re concerned about your baby’s sleep, it’s a very good idea to see a child health professional for help. You could start by talking with your GP or child and family health nurse.
How baby sleep patterns affect grown-ups
Babies and grown-ups need sleep for wellbeing, but babies sleep differently from adults. Most parents of babies under six months of age get up in the night to feed and settle their babies. For many, this keeps going after six months.
Some parents are OK with getting up a lot at night as long as they have enough support and they can catch up on sleep at other times. For others, getting up in the night over the long term has a serious effect on them and their family lives.
The quality of your sleep can affect your health and your mood. Being exhausted can make it hard to give your baby positive attention during the day. And your relationship with your baby and the time and attention you give baby during the day can affect the quality and quantity of baby’s sleep.
And your relationship with your baby and the time and attention you give baby during the day can affect the quality and quantity of baby’s sleep.
So it’s important that you get some help if you’re not getting enough sleep. You could start by asking family or friends for help. And if you feel that lack of sleep is affecting you mentally or emotionally, it’s a very good idea to talk with your GP or another health professional.
There’s a strong link between baby sleep difficulties and symptoms of postnatal depression in women and postnatal depression in men. But the link isn’t there if parents of babies with sleep difficulties are getting enough sleep themselves.
Languages other than English
- Arabic (PDF: 471kb)
- Dari (PDF: 469kb)
- Karen (PDF: 298kb)
- Persian (PDF: 420kb)
- Simplified Chinese (PDF: 502kb)
- Vietnamese (PDF: 324kb)
What is insomnia, causes and treatment
Insomnia (insomnia) is a sleep disorder in which a person cannot fall asleep, fully relax and recuperate. According to world medical statistics, more than 35% of women and almost 30% of men suffer from this disease. In children, insomnia is diagnosed less often - about one in four.
According to world medical statistics, more than 35% of women and almost 30% of men suffer from this disease. In children, insomnia is diagnosed less often - about one in four.
Many patients do not pay attention to the disease or try to cope with it on their own. As a result, a persistent sleep disorder develops - chronic insomnia, which is difficult to treat and causes many health problems. In the presence of such a disease, the patient should seek an initial consultation with a general practitioner.
What is considered insomnia
A healthy person needs at least 6-10 hours of sleep per day for a good rest. During this time, the body recovers, the brain processes the information received during the day. The period of immersion in sleep takes no more than 15 minutes.
It is impossible to do without rest for more than 200 hours. If sleep is insufficient, a person feels a breakdown, irritability. With chronic lack of sleep, a decrease in immunity, lethargy, and the development of mental disorders are possible.
Insomnia is a violation not only of the quantity but also of the quality of sleep. Even with severe fatigue in the evening, a person goes to bed and tries for a very long time to find a comfortable position, to relax. Sleep becomes interrupted. In the morning the patient with insomnia still feels tired. Insomnia is diagnosed when there are three or more episodes every week for a month.
Causes of pathology
There are many factors that can affect sleep.
Among the main causes of insomnia:
- genetic predisposition;
- taking certain medications;
- alcohol abuse;
- overeating before bed;
- thyroid dysfunction;
- depressions, neuroses;
- increased emotional excitability;
- adverse environmental conditions during falling asleep: cold, heat, hard mattress, etc.;
- parkinsonism, other neurological disorders;
- arthritis, arthrosis, pathologies with severe pain syndrome;
- diseases of the kidneys and bladder, causing frequent urge to urinate;
- restless leg syndrome.

Occasionally, insomnia may occur due to flights between time zones or work schedule changes (eg night work). After the elimination of the provoking factor, rest is restored.
Insomnia in a woman is often caused by menstrual irregularities, pregnancy or the onset of menopause.
Elderly patients and people in difficult life situations are also at risk.
Types of insomnia
According to the type of provoking factors, insomnia happens:
- Adaptive. Symptoms of insomnia appear on the background of severe stress, for example, moving to a different climate zone. Adaptive insomnia does not require serious treatment and can go away on its own within a few weeks.
- Psychophysiological. The patient is afraid in advance that he will not be able to sleep. By evening, the tension intensifies, the fear grows.
- Idiopathic. Insomnia develops from childhood.
 Often it is not possible to establish the exact cause of the violation.
Often it is not possible to establish the exact cause of the violation. - Behavioral. This type of insomnia usually affects young children who are accustomed to certain rituals. For example, if a child who has always been rocked is simply put in a crib, he will be capricious and spin for a very long time. Behavioral insomnia can occur while weaning a baby from the breast or pacifier.
- Based on mental disorders. More than 70% of cases of insomnia are diagnosed in patients with neuropsychiatric diseases.
- On the basis of a violation of sleep hygiene. The cause of insomnia is a person's inattention to his daily routine, work and rest schedule. Coffee before bedtime, bright noise and light are also provoking factors.
- Caused by somatic disease. Any health problem can be the cause: abdominal pain due to gastritis, sleep apnea, cough due to bronchitis, etc.
- Pseudoinsomnia.
 A person's sleep remains normal both in quality and duration, but the patient feels sleep deprivation. It seems to him that he rested less time than actually elapsed.
A person's sleep remains normal both in quality and duration, but the patient feels sleep deprivation. It seems to him that he rested less time than actually elapsed.
According to the duration of manifestations, insomnia is:
- Transient. Sleep disturbances are of short duration, lasting several days. Transient insomnia is caused by changes in the environment, such as moving or depression.
- Sharp. Sleep disturbances are regular, but last no more than a month. Acute insomnia is more often associated with stress. Patients have difficulty falling asleep, sleep becomes short, intermittent.
- Chronic. Insomnia lasts for several months and is triggered by various factors. Patients note periods of deterioration and improvement in their condition.
Symptoms of insomnia
Sleep disorders cannot be confused with another disease. At night, a person cannot rest, and during the day he becomes distracted and irritable. I want to sleep all the time. Insomnia does not allow you to focus on the performance of job duties, causes a decline in motivation. Additionally, it is possible to develop headaches, indigestion.
I want to sleep all the time. Insomnia does not allow you to focus on the performance of job duties, causes a decline in motivation. Additionally, it is possible to develop headaches, indigestion.
Insomnia in children
The timing of sleep varies widely among children. One child needs a long rest, another 6 hours is enough to feel full of energy. If at the same time the children are active, cheerful, then doctors recommend not to worry. Both options can be considered the norm - both long and short sleep.
As the child grows older, they may sleep less and less. The reason for concern should be the capriciousness, irritability of the child, his active unwillingness to go to bed in the evening. Nervousness makes sleep "torn". The child does not sleep well on his own and does not allow his parents to rest.
It is important not to miss the first manifestations of insomnia, when children's sleep is still quite easy to correct. To do this, the process of preparing for the rest must be made pleasant and relaxing. You can bathe the child, give him warm milk, allow him to take his favorite toy to bed. Do not insist on daytime sleep if the baby does not want to, and do not let him fall asleep early in the evening: distract him with a book, cartoons, a walk.
You can bathe the child, give him warm milk, allow him to take his favorite toy to bed. Do not insist on daytime sleep if the baby does not want to, and do not let him fall asleep early in the evening: distract him with a book, cartoons, a walk.
You should not go to bed with your child and wait for him to fall asleep. If joint rest becomes a habit, it will be difficult to get rid of it. Ignore whims, gently but persistently put the child alone, and over time he will learn to fall asleep on his own.
Diagnosis of insomnia
When the first problems with a night's rest appear, it is necessary to make an appointment with a doctor. To diagnose insomnia, a special assessment technique has been developed - the Epworth scale. With its help, the severity of symptoms is assessed and treatment is prescribed. It is also important to establish the cause of insomnia in a man or woman and eliminate the factor.
At the first consultation, the doctor takes an anamnesis. Finds out how long ago the problems with sleep began, what factors could provoke them. The patient is advised to keep a special diary. Every day, the time of falling asleep and waking up, the number of sleep interruptions during the night are entered into the notebook. The patient should describe his feelings in the morning. Based on the diary information, the doctor evaluates the quality and duration of sleep. Data are also needed to select the appropriate treatment.
Finds out how long ago the problems with sleep began, what factors could provoke them. The patient is advised to keep a special diary. Every day, the time of falling asleep and waking up, the number of sleep interruptions during the night are entered into the notebook. The patient should describe his feelings in the morning. Based on the diary information, the doctor evaluates the quality and duration of sleep. Data are also needed to select the appropriate treatment.
An alternative to the diary is the actigraphy procedure. The patient is given a special measuring device that must be worn on the wrist for a week. Actigraphy is performed on an outpatient basis.
If insomnia is caused by a medical condition, a diagnosis is made to determine the underlying cause. Treatment of the underlying pathology eliminates sleep problems.
Treatment of insomnia
It is important not to self-medicate. Uncontrolled intake of sleeping pills and any other drugs, at best, will not bring the expected result, and at worst, it will provoke side effects. Insomnia will progress, and medications will negatively affect your overall health. Be sure to see a doctor.
Insomnia will progress, and medications will negatively affect your overall health. Be sure to see a doctor.
The treatment of insomnia is complex, including consultations of related specialists, taking medications and other auxiliary methods.
Psychotherapy
The doctor helps to overcome crisis situations, cope with neurosis, stress, apathy. The course of psychotherapy includes several sessions at the discretion of the specialist.
One of the methods of treatment is hypnosis. The technology is used for severe violations.
Paradoxical intention technique
A special treatment method aimed at changing perception (cognitive reframing technique). The patient is advised not to think about a night's sleep, but, on the contrary, to make every effort to stay awake. The method is effective in most applications.
Medical treatment
There are many drugs available to improve the quality of sleep. The medicine is selected individually, taking into account the state of health, the severity of symptoms, the patient's lifestyle. Proper treatment should help in the normalization of sleep, but at the same time not create serious side effects and not interfere with daily activities.
The medicine is selected individually, taking into account the state of health, the severity of symptoms, the patient's lifestyle. Proper treatment should help in the normalization of sleep, but at the same time not create serious side effects and not interfere with daily activities.
More often doctors opt for herbal preparations. Medicines have a cumulative effect and are not addictive. Synthetic sleeping pills are taken in a strictly calculated dosage and for a limited period. In most cases, depressants are prescribed (Doxepin, Amitriptyline and others). Means have a quick sedative effect, help regulate sleep, exhibit antiadrenergic, antihistamine, anticholinergic properties. Antidepressants promote falling asleep, increase the total duration of rest.
It is possible to prescribe drugs based on melatonin, the sleep hormone. The drug is effective against chronic insomnia, especially in the elderly. The remedy is prescribed for 3 weeks, after which it is necessary to take a break.
Important: hormonal preparations have many contraindications. For example, Melatonin should not be given to pregnant women and adolescent girls. In each case, the medication must be agreed with the gynecologist.
Massage
Reflex massage has no contraindications, and you can do it yourself. Just 15-20 minutes before bed will help improve the patient's condition. There are various massage techniques that are aimed at stimulating biologically active points on the ears, neck, abdomen, and feet.
Breathing exercises
Rhythmic inhalations and exhalations stimulate blood circulation in the tissues of the brain, improve the functioning of internal organs. Breathing exercises help elderly people cope well with insomnia, but even children can easily master simple exercises. It is important that classes bring pleasure and do not create additional stress. A set of exercises will be selected by the doctor.
The patient must remember that breathing should be through the nose with a short and strong inhalation and a long exhalation. You can mentally keep score so that the exercises are rhythmic.
You can mentally keep score so that the exercises are rhythmic.
Spa treatment
Regular courses have a beneficial effect not only on sleep, but also on the general state of human health. It is recommended to relax in sanatoriums at least once a year. In the institution, patients observe a sleep schedule, receive a set of therapeutic and restorative procedures, undergo massage courses, herbal medicine, mud baths, etc.
Prevention of insomnia
In most cases, insomnia can be corrected at the first manifestation and prevent its recurrence. It is necessary to think over the daily routine, in which at least 8 hours are allotted for sleep.
To reduce the symptoms of insomnia, the following actions will help:
1. Go to bed at the same time every day. Warm tea, a herbal bath, favorite pajamas help many people relax - do not break the usual rituals.
2. Give up alcohol, smoking. Alcohol can have a short-term sedative effect and speed up falling asleep, but it negatively affects the deep sleep phase. A person can suddenly get up at night and can no longer sleep.
A person can suddenly get up at night and can no longer sleep.
3. Give up coffee or keep it to a minimum. Caffeine is able to linger in the cells during the day. Undesirable substances are also found in chocolate, strong tea. You can eat such foods only in the morning.
4. Read medication instructions carefully and consult your doctor. Many over-the-counter medications that are taken for colds or headaches contain ephedrine. The substance has a stimulating effect on the body. If the medication affects sleep, ask your doctor to change the dosage or change the medication.
5. Do not overeat before bed. A full stomach will work all night and send signals to the brain - in the morning there will be a feeling of fatigue. To satisfy your hunger, you can drink a glass of kefir, milk or a cup of herbal tea.
6. Take a warm bath. Some are helped by water procedures 2 hours before bedtime, some just before going to bed. Time is determined individually. Flavored foams, herbal decoctions can be added to the bath.
7. Exercise in the morning. A few simple exercises will help you tone up and create moderate physical activity. Regular exercise contributes to better falling asleep in the evening.
8. Practice good sleep hygiene. The room should be dark, quiet and cool enough - + 15 ... + 18 ° С. It is better to choose a mattress that is dense, but not hard, on which the body feels comfortable. Some people find it difficult to fall asleep in silence, they use "background" noises, such as turning on the air conditioner or soft instrumental music.
9. Avoid long naps. Short rest periods of 20 minutes will have an invigorating effect on the body, but longer daytime sleep contributes to insomnia.
10. Contrary to the stereotype, counting sheep is not worth it. When a person is focused on any action, active processes take place in the brain that interfere with sleep.
Diagnosis and treatment of insomnia in Moscow
MedEx Personal Medicine Clinic invites you to a consultation on the causes and treatment of insomnia. Experienced doctors will help find a solution in the most difficult cases. Call us to make an appointment with a neurologist.
Experienced doctors will help find a solution in the most difficult cases. Call us to make an appointment with a neurologist.
Treatment and diagnosis of obstructive sleep apnea syndrome at the St. Petersburg Hospital of the Russian Academy of Sciences
Obstructive sleep apnea syndrome (OSA, “sleep apnea disease”) is a condition in which snoring suddenly stops during sleep and a frightening cessation of breathing occurs, after which the sleeping person snores loudly , sometimes tossing and turning and then starts breathing again. Depending on the severity of the syndrome, from several to 400-500 stops of breathing can be observed during sleep, primarily during the night. Breathing disorders in a sleeping person lead to a serious deterioration in the quality of sleep and create conditions for the development and progression of many serious complications and diseases.
Causes of OSA
- Weakness of the tone of the muscles of the pharynx, as a result of which, during sleep, the airways collapse with a violation of their air permeability.
- Developmental anomalies resulting in narrow airways (eg, small mandible, large tongue).
- Anatomical defects at the level of the nose and pharynx (polyps, deviated nasal septum, enlarged tonsils, adenoids (pathological growth of the nasopharyngeal tonsil), tumor formations).
- Obesity.
- Endocrine diseases: for example, hypothyroidism (causes swelling of the pharyngeal structures), acromegaly - all this prevents the normal passage of air through the respiratory tract.
- Neurological diseases leading to a decrease in muscle tone (stroke - an acute violation of cerebral circulation with the death of a section of brain tissue; myopathy, myodystrophy).
- Violation of the tone of the muscles of the pharynx due to the influence of alcohol, certain drugs (hypnotics, tranquilizers).
- Chronic obstructive pulmonary disease - characterized by narrowing of the airways and impaired airflow (bronchial asthma, chronic obstructive pulmonary disease (COPD)).
- Smoking.
- Allergy.
Symptoms of OSA:
- Restless sleep, during sleep there is excessive motor activity (often roll over from side to side).
- Lack of vigor after sleep, there is a feeling of morning fatigue and weakness after waking up.
- Sleepiness during the day, tendency to fall asleep during work breaks, while driving.
- Morning headaches.
- Increased arterial (blood) pressure (mainly at night and in the morning).
- Frequent nighttime urination (>2 times per night).
- Reduced potency.
- Depression, irritability, decreased concentration and memory.
- Palpitations (tachycardia), heart rhythm disorders - arrhythmias
COAC classification
Based on Apnea Index (AI) value.
Apnea - complete cessation of breathing for at least 10 seconds.
Apnea index (AI) - the frequency of apnea attacks per 1 hour of sleep.
By severity:
- Mild: AI - 5-14.
- Moderate course: AI - 15-29.
- Severe course: AI - 29 or more. In severe forms, up to 300-500 stops of breathing can be observed during sleep, lasting up to 3-4 hours in total.
OSA diagnostics
- ECG Holter monitoring (assesses the work of the heart) with simultaneous registration of pneumogram (recording of respiratory movements), blood oxygen saturation, air flow.
- Cardiorespiratory monitoring is a test that evaluates snoring, respiration, blood oxygen saturation, respiratory movements of the chest and abdominal wall. The device is portable, which makes it possible to conduct research at home.
- Pulse Oximetry - Measures the oxygen saturation curve during sleep.

- Polysomnography is a method of long-term recording of various functions of the human body during a night's sleep: snoring, breathing, blood oxygen saturation, respiratory movements of the chest and abdominal wall, patient's body position, electroencephalogram (registration of brain activity), electrooculogram (registration of eye movements) , electromyogram (registers the tone of the chin muscles, movements of the lower extremities), continuous video recording throughout the patient's sleep. The study allows you to make an accurate diagnosis, evaluate changes in the cardiovascular and nervous systems and determine the optimal treatment tactics. It is carried out only in specialized departments.
Complications and consequences of OSA
- Increased arterial (blood) pressure.
- Arrhythmias.
- Myocardial infarction.
- Stroke (acute cerebrovascular accident).
- Progressive obesity.

- Worsening of the course of type 2 diabetes mellitus.
- Reduced potency.
- Increased risk of accidents and accidents at work. In some countries, OSA is included in the list of diseases for which the issuance of a driver's license is prohibited !!!.
- Sudden death during sleep.
Treatment of obstructive sleep apnea
- Weight loss - following a low-calorie, vitamin-rich diet with a significant reduction in fat and carbohydrates.
- Do not eat 3-4 hours before bedtime.
- Stop smoking and alcohol 2 hours before bedtime.
- Ensuring normal air humidity and hypoallergenic environment in the bedroom (do not use feather and down pillows and blankets, woolen carpets, etc.).
- Ensuring the optimal position of the head and body during sleep. Respiratory disorders are most pronounced when a person is lying on his back, since there is a maximum convergence of the structures of the respiratory tract.