What to expect during an induction
Labor induction - Mayo Clinic
Overview
Labor induction — also known as inducing labor — is prompting the uterus to contract during pregnancy before labor begins on its own for a vaginal birth.
A health care provider might recommend inducing labor for various reasons, primarily when there's concern for the mother's or baby's health. An important factor in predicting whether an induction will succeed is how soft and expanded the cervix is (cervical ripening). The gestational age of the baby as confirmed by early, regular ultrasounds also is important.
If a health care provider recommends labor induction, it's typically because the benefits outweigh the risks. If you're pregnant, understanding why and how labor induction is done can help you prepare.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
To determine if labor induction is necessary, a health care provider will likely evaluate several factors. These include the mother's health and the status of the cervix. They also include the baby's health, gestational age, weight, size and position in the uterus. Reasons to induce labor include:
- Nearing 1 to 2 weeks beyond the due date without labor starting (postterm pregnancy).
- When labor doesn't begin after the water breaks (prelabor rupture of membranes).
- An infection in the uterus (chorioamnionitis).
- When the baby's estimated weight is less than the 10th percentile for gestational age (fetal growth restriction).
- When there's not enough amniotic fluid surrounding the baby (oligohydramnios).
- Possibly when diabetes develops during pregnancy (gestational diabetes), or diabetes exists before pregnancy.
- Developing high blood pressure in combination with signs of damage to another organ system (preeclampsia) during pregnancy. Or having high blood pressure before pregnancy, developing it before 20 weeks of pregnancy (chronic high blood pressure) or developing the condition after 20 weeks of pregnancy (gestational hypertension).
- When the placenta peels away from the inner wall of the uterus before delivery — either partially or completely (placental abruption).
- Having certain medical conditions. These include heart, lung or kidney disease and obesity.
Elective labor induction is the starting of labor for convenience when there's no medical need. It can be useful for women who live far from the hospital or birthing center or who have a history of fast deliveries.
A scheduled induction might help avoid delivery without help. In such cases, a health care provider will confirm that the baby's gestational age is at least 39 weeks or older before induction to reduce the risk of health problems for the baby.
As a result of recent studies, women with low-risk pregnancies are being offered labor induction at 39 to 40 weeks. Research shows that inducing labor at this time reduces several risks, including having a stillbirth, having a large baby and developing high blood pressure as the pregnancy goes on. It's important that women and their providers share in decisions to induce labor at 39 to 40 weeks.
It's important that women and their providers share in decisions to induce labor at 39 to 40 weeks.
Request an appointment
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health. Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Risks
Uterine incisions used during C-sections
Uterine incisions used during C-sections
A C-section includes an abdominal incision and a uterine incision. After the abdominal incision, the health care provider will make an incision in the uterus. Low transverse incisions are the most common (top left).
Labor induction carries various risks, including:
- Failed induction. An induction might be considered failed if the methods used don't result in a vaginal delivery after 24 or more hours. In such cases, a C-section might be necessary.
- Low fetal heart rate. The medications used to induce labor — oxytocin or a prostaglandin — might cause the uterus to contract too much, which can lessen the baby's oxygen supply and lower the baby's heart rate.

- Infection. Some methods of labor induction, such as rupturing the membranes, might increase the risk of infection for both mother and baby. The longer the time between membrane rupture and labor, the higher the risk of an infection.
-
Uterine rupture. This is a rare but serious complication in which the uterus tears along the scar line from a prior C-section or major uterine surgery. Rarely, uterine rupture can also occur in women who have not had previous uterine surgery.
An emergency C-section is needed to prevent life-threatening complications. The uterus might need to be removed.
- Bleeding after delivery. Labor induction increases the risk that the uterine muscles won't properly contract after giving birth, which can lead to serious bleeding after delivery.
Labor induction isn't for everyone. It might not be an option if:
- You've had a C-section with a classical incision or major uterine surgery
- The placenta is blocking the cervix (placenta previa)
- Your baby is lying buttocks first (breech) or sideways (transverse lie)
- You have an active genital herpes infection
- The umbilical cord slips into the vagina before delivery (umbilical cord prolapse)
If you have had a C-section and have labor induced, your health care provider is likely to avoid certain medications to reduce the risk of uterine rupture.
How you prepare
Labor induction is typically done in a hospital or birthing center. That's because mother and baby can be monitored there, and labor and delivery services are readily available.
What you can expect
During the procedure
There are various ways of inducing labor. Depending on the circumstances, the health care provider might use one of the following ways or a combination of them. The provider might:
-
Ripen the cervix. Sometimes prostaglandins, versions of chemicals the body naturally produces, are placed inside the vagina or taken by mouth to thin or soften (ripen) the cervix. After prostaglandin use, the contractions and the baby's heart rate are monitored.
In other cases, a small tube (catheter) with an inflatable balloon on the end is inserted into the cervix. Filling the balloon with saline and resting it against the inside of the cervix helps ripen the cervix.
- Sweep the membranes of the amniotic sac.
 With this technique, also known as stripping the membranes, the health care provider sweeps a gloved finger over the covering of the amniotic sac near the fetus. This separates the sac from the cervix and the lower uterine wall, which might help start labor.
With this technique, also known as stripping the membranes, the health care provider sweeps a gloved finger over the covering of the amniotic sac near the fetus. This separates the sac from the cervix and the lower uterine wall, which might help start labor. -
Rupture the amniotic sac. With this technique, also known as an amniotomy, the health care provider makes a small opening in the amniotic sac. The hole causes the water to break, which might help labor go forward.
An amniotomy is done only if the cervix is partially dilated and thinned, and the baby's head is deep in the pelvis. The baby's heart rate is monitored before and after the procedure.
- Inject a medication into a vein. In the hospital, a health care provider might inject a version of oxytocin (Pitocin) — a hormone that causes the uterus to contract — into a vein. Oxytocin is more effective at speeding up labor that has already begun than it is as at cervical ripening.
 The provider monitors contractions and the baby's heart rate.
The provider monitors contractions and the baby's heart rate.
How long it takes for labor to start depends on how ripe the cervix is when the induction starts, the induction techniques used and how the body responds to them. It can take minutes to hours.
After the procedure
In most cases, labor induction leads to a vaginal birth. A failed induction, one in which the procedure doesn't lead to a vaginal birth, might require another induction or a C-section.
By Mayo Clinic Staff
Related
Products & Services
What to Expect and What to Ask
Labor induction, also known as inducing labor, is the jumpstarting of uterine contractions before natural labor occurs, with the goal of a healthy vaginal delivery.
Healthcare providers, doctors, and midwives might suggest inducing labor for a number of reasons — both medical and nonmedical (elected).
Here’s what you need to know in order to prepare for labor induction.
A healthcare provider, doctor, or midwife will evaluate your health and the health of your baby at all prenatal appointments. This includes examining your baby’s gestational age, size, weight and position in your uterus.
This includes examining your baby’s gestational age, size, weight and position in your uterus.
At later appointments, this may include checking your cervix and considering the overall picture to determine whether or not you or baby are at risk and labor induction is needed.
How does your cervix rate?
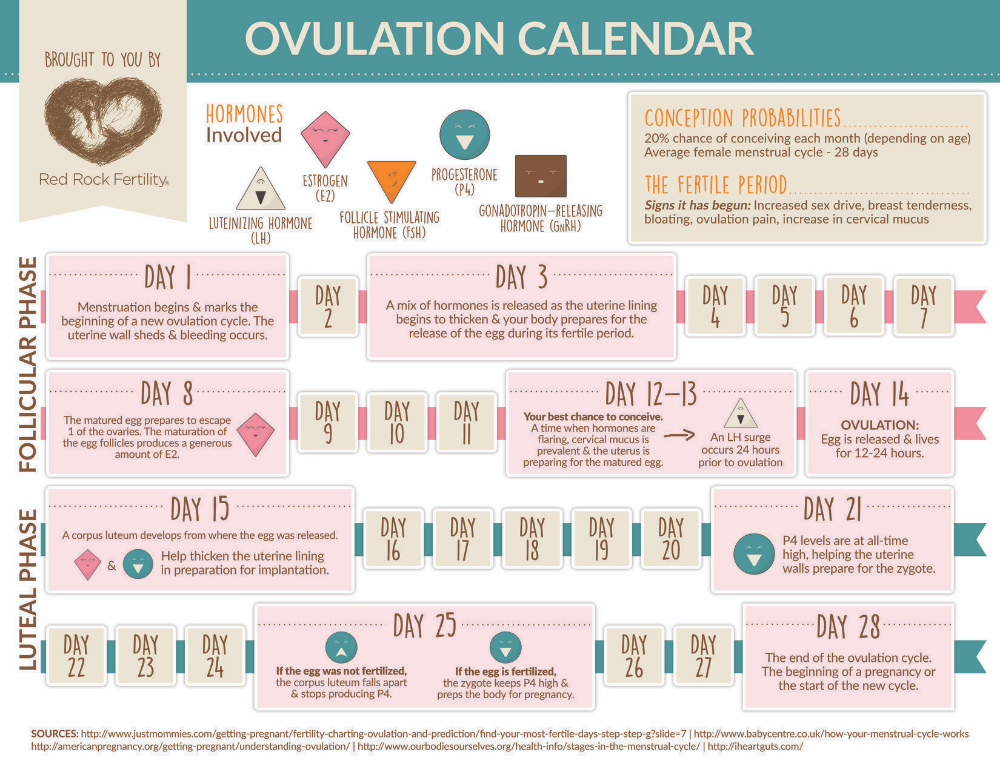
The cervix begins to ripen (soften), thin out, and open as it prepares for labor and delivery. To determine the readiness of the cervix, some doctors use the Bishop score. Rating the readiness on a scale from 0 to 13, your cervix gains points based on dilation, texture, placement, angle, and length.
Was this helpful?
A labor induction may be suggested if there’s cause for concern regarding the health of you or your baby. Or perhaps you live a far distance from your hospital, and it would be prudent to control the timing of your labor and delivery.
Other reasons include:
- Predicted due date has come and gone.
- Gestational diabetes.

- Chorioamnionitis (an infection in the uterus).
- Baby is growing too slowly.
- Oligohydramnios (low or leaking amniotic fluid).
- Placental obstruction or abruption.
- Broken water, but no contractions.
- History of speedy, short deliveries.
Women with certain medical conditions should not be recommended for induction, so it’s important to ask questions (see below) and discuss all of the options, benefits, and potential risks of a labor inducing procedure with your healthcare provider.
Did you know?Women spend more time in labor now than they did 50 years ago!
Was this helpful?
There are many methods of labor induction, and what works for one woman or one delivery, may not work for another.
In addition to natural inducing methods (both proven and unproven), such as sexual intercourse, castor oil, hot baths, breast and nipple stimulation, acupuncture, herbal supplements, and eggplant casseroles, there are many medical/surgical techniques too.
A doctor or midwife can use medicines and other means to assist in opening the cervix and stimulate contractions. Some methods include:
- Amniotomy, or “breaking the water,” where your healthcare provider pokes a small hole in your amniotic sac. This will also make your uterine contractions stronger.
- Pitocin, also called oxytocin, which is a hormone that speeds up labor. Pitocin is delivered through an IV in your arm.
- Cervical ripening, performed by taking medicine orally or by inserting a medicine (prostaglandin analogs) into the vagina to stretch, soften, and expand the cervix.
- Insertion of catheter or balloon by your healthcare provider, which then expands, such as a Foley bulb induction.
- Stripping membranes, where your healthcare provider uses a gloved finger to separate the thin tissue of amniotic sac from the uterine wall.
From time to time, a doctor will use more than one method to induce labor and delivery.
Every labor progresses at its own pace. If your cervix is soft and ripe, a gentle push may be all you need to jumpstart those contractions. If your cervix needs more time, it may take days before delivery occurs.
If your cervix is soft and ripe, a gentle push may be all you need to jumpstart those contractions. If your cervix needs more time, it may take days before delivery occurs.
An induced labor can last anywhere from a few hours to a few days. Sometimes, labor induction doesn’t work at all, or the method used has to be repeated. It all depends on how ripe the cervix is at time of induction and how well your body responds to the method chosen for induction.
Contractions can start within 30 minutes of taking oxytocin, and most women will begin labor within hours after their water breaks.
All healthcare providers should allow you 24 hours or more of the early phase of labor before considering the induction a bust and moving forward with other interventions.
If you and your baby are healthy and doing well after a failed induction, you might be sent home and asked to reschedule the induction for a later date. (Yes, that can actually happen.)
As with everything in life, labor induction comes with some risks.
- You may experience stronger, more painful and frequent contractions.
- You may have increased risk of postpartum depression, according to one 2017 study.
- You may have a failed induction and need a cesarean delivery (this comes with its own list of concerns, including a longer recovery time).
A first-time mother whose cervix is not ready for labor has an increased chance of the induction leading to a cesarean delivery, according to the American College of Obstetricians and Gynecologists. This is why asking questions (see below) — especially about the condition of your cervix — is so important.
Throughout the induction process, your healthcare provider, doctor, or midwife will monitor you and your baby to determine whether or not an assisted vaginal delivery or cesarean delivery is necessary.
Other potential risks of induction include:
- Infection. Certain methods of induction, such as rupturing membranes, pose an increased risk for infection in both mom and baby.
- Uterine rupture. This is especially true for women who have had a previous cesarean delivery or another uterine surgery.
- Complications with fetal heart rate. Too many contractions can lead to changes in the baby’s heart rate.
- Fetal death.
It’s important to discuss the potential risks for you and your baby during induction in detail with a healthcare provider, doctor, or midwife before agreeing to any procedure.
Ask questions
Before you agree to be induced, consider finding out the following from your healthcare provider:
- What’s the reason for the induction?
- What are the signs that make you a good candidate for induction?
- What types of induction is your healthcare provider considering?
- What’s your due date? (Confirm that the induction date is indeed set for after the 39th week of pregnancy.)
- What’s the condition of your cervix?
- What is the baby’s position?
- How many times has your doctor or midwife performed this procedure?
- Will you be able to move around?
- What are the risks and benefits of each induction procedure being considered?
- Will it require constant or occasional monitoring?
- Will it hurt? What are your options for pain relief?
- What is the doctor or midwife’s plan if the chosen method for induction fails?
- At what point might you be sent home, with another induction rescheduled?
- Will your doctor or midwife be available during the entire procedure?
- If the procedure takes a very long time, will you be able to use the restroom?
- Do you have a prior medical condition or consideration that will affect this induction?
You’ll also want to know where the labor induction will take place, typically a hospital or birthing center. However, a home delivery with natural induction methods may sometimes be an option.
However, a home delivery with natural induction methods may sometimes be an option.
Set realistic expectations
Maybe an induction isn’t what you had in mind. Well… try to keep an open mind! Induced labor is very different than a naturally occurring labor, but that doesn’t mean you have to throw your entire birth plan out the window.
Take a moment to consider how you think and feel about your labor and delivery plan. The mental and emotional aspects of labor and delivery are complicated enough, and getting induced has its own benefits and risks.
Pack entertainment
This may be happening, but it’s not always fast.Don’t let the waiting time get to you. Load an electronic device with movies, on-demand shows, and books and add them to your hospital bag.
Pack a journal and plan on taking a few minutes to jot down your in-the-moment labor and delivery thoughts. Make a playlist of music for when you need calming and for the You Can Do This Oomph and Push.
Don’t forget to pack chargers for all electronic devices, a pair of headphones, and comfortable, loose clothing.
Eat something light and then try to go poo
Most practitioners say no food once contractions begin. Don’t stop at your favorite fast food place on the way to the hospital. You don’t want the runs during this business.
Before heading to the hospital, eat a light meal at home… and then give the ol’ porcelain bowl a good visit. You’ll feel much better.
Give your partner permission to scoot
If the induction lasts longer than 12 to 24 hours, consider allowing your partner some fresh air. A bored induction partner can turn into an annoying labor and delivery companion, so allow your partner to pack their own hospital bag.
Tell them to pack some snacks (nothing smelly!) and a good pillow. Once at the hospital, communicate your feelings as best as possible, and then tell them to go find you some ice cream for after.
Accept that it may take longer than you’d like, and may be more challenging than you imagine. It will be okay! Talk with friends and family members who have had induced labors and at some point, and try to stop googling. It’s normal to feel excited and nervous.
It will be okay! Talk with friends and family members who have had induced labors and at some point, and try to stop googling. It’s normal to feel excited and nervous.
Just remember: You have options and choices.
Induction of labor in women with normal pregnancies of 37 weeks or more
Does a policy of inducing labor at 37 weeks or more of gestation reduce the risks for infants and their mothers compared with a policy of waiting until a later gestational age or until Will there be indications for labor induction?
This review was originally published in 2006 and subsequently updated in 2012 and 2018.
What is the problem?
The average pregnancy lasts 40 weeks from the start of a woman's last menstrual period. Pregnancies lasting more than 42 weeks are described as "post-term" and therefore the woman and her doctor may decide to give birth by induction. Factors associated with postnatal pregnancy and delayed delivery include obesity, first birth, and maternal age over 30 years.
Why is this important?
Protracted (term) pregnancy may increase risks for infants, including greater risk of death (before or shortly after birth). However, induction (stimulation or induction) of labor can also pose risks to mothers and their babies, especially if the woman's cervix is not ready for delivery. Current diagnostic methods cannot predict risks to babies or their mothers per se, and many hospitals have specific policies regarding how long a pregnancy can last.
What evidence did we find?
We searched for evidence (July 17, 2019) and identified 34 randomized controlled trials in 16 different countries involving more than 21,500 women (mostly at low risk of complications). The trials compared a policy of induction of labor after 41 completed weeks of gestation (>287 days) with a policy of waiting (expectant management).
Labor induction policies were associated with fewer perinatal deaths (22 trials, 18 795 babies). Four perinatal deaths occurred in the induction policy group compared with 25 perinatal deaths in the expectant management group. Fewer stillbirths occurred in the induction group (22 trials, 18,795 infants): two in the induction group and 16 in the expectant management group.
Four perinatal deaths occurred in the induction policy group compared with 25 perinatal deaths in the expectant management group. Fewer stillbirths occurred in the induction group (22 trials, 18,795 infants): two in the induction group and 16 in the expectant management group.
Women in the induction of labor groups in the included studies were probably less likely to deliver by caesarean section than in the expectant management groups (31 studies, 21,030 women), and there was probably little or no difference when compared with assisted vaginal delivery (22 studies, 18,584 women).
Fewer infants were admitted to the neonatal intensive care unit (NICU) in the induction policy group (17 trials, 17,826 infants; high-certainty evidence). A simple test of the baby's health status (Apgar score) at five minutes after birth was likely to be more favorable in the induction groups than expectant management (20 trials, 18,345 infants).
An induction policy may make little or no difference for women who have had a perineal injury, and likely has little or no effect on the number of women with postpartum hemorrhage or breastfeeding at hospital discharge. We are uncertain about the effect of induction or expectant management on length of stay in the maternity hospital due to the very low certainty of the evidence.
We are uncertain about the effect of induction or expectant management on length of stay in the maternity hospital due to the very low certainty of the evidence.
Among newborns, the number of children with trauma or encephalopathy was similar in both groups (moderate and low-certainty evidence, respectively). None of the studies reported the development of neurodevelopmental problems during follow-up of children and postpartum depression in women. Only three trials reported some measure of maternal satisfaction.
What does this mean?
An induction policy compared to expectant management is associated with fewer infant deaths and probably fewer caesarean sections; and probably has little or no effect on assisted vaginal delivery. Determining the best time to offer induction of labor to women at 37 weeks' gestation or more requires further study, as well as further study of women's risk profiles and their values and preferences. Discussing the risks of induction of labor, including benefits and harms, can help women make an informed choice between induction of labor, especially if the pregnancy lasts more than 41 weeks, or expectant management—waiting and/or waiting until labor is induced. Women's understanding of induction, procedures, their risks and benefits is important to influence their choice and satisfaction.
Discussing the risks of induction of labor, including benefits and harms, can help women make an informed choice between induction of labor, especially if the pregnancy lasts more than 41 weeks, or expectant management—waiting and/or waiting until labor is induced. Women's understanding of induction, procedures, their risks and benefits is important to influence their choice and satisfaction.
Translation notes:
Translation: Alekseeva Lada Igorevna. Editing: Prosyukova Ksenia Olegovna and Ziganshina Lilia Evgenievna. Russian translation project coordination: Cochrane Russia - Cochrane Russia, Cochrane Geographic Group Associated to Cochrane Nordic. For questions related to this translation, please contact us at: [email protected]
Labor induction. When is it really needed?
Sokolova Elena
Published: 02/14/2023
Reading time: 7 minutes
3686
When should labor be induced?
Most pregnant women are set for spontaneous delivery. But what to do if the date of birth is approaching, has come, or even passed, and the birth has not begun. Or the doctor talks about the need for delivery, and the delivery date is still far away. In this article we will talk about the stimulation of the birth act. We will analyze the indications and discuss why induction of labor is performed.
But what to do if the date of birth is approaching, has come, or even passed, and the birth has not begun. Or the doctor talks about the need for delivery, and the delivery date is still far away. In this article we will talk about the stimulation of the birth act. We will analyze the indications and discuss why induction of labor is performed.
To begin with, let's understand what is the induction (stimulation) of labor. Under the induction of labor understand the artificial stimulation of the onset of labor. That is, the launch of labor activity, which occurs after the introduction of drugs, the use of measures. An important factor that is assessed before induction is the assessment of the degree of maturity of the cervix (assessed by the doctor during a vaginal examination). After all, the cervix indicates the readiness of the woman's body for childbirth. Well, if the body is ready, and there is no time to wait for the spontaneous start of the start of labor, then you can start it.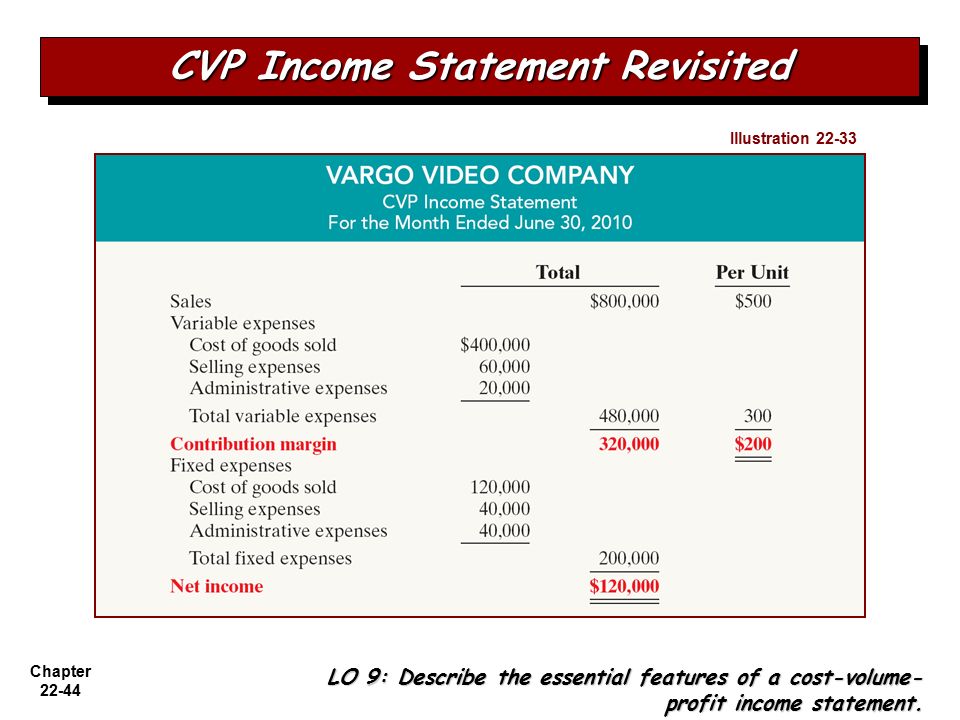
But what to do if there are indications for delivery, there are no contraindications for vaginal delivery, and the cervix is immature? Simply put, it is necessary to give birth, but the body is not yet ready. Caesarean section cannot be considered as an alternative to spontaneous delivery. There are strict indications for it. After a caesarean section, the recovery period increases, the risk of complications increases, a scar remains on the uterus, there is no breastfeeding for the first day (separation of mother and child), a belated arrival of primary milk is often noted. The answer is simple. In such situations, activities are carried out aimed at accelerating the maturation of the cervix - pre-induction of childbirth.
Naturally, all activities are carried out only with the written consent of the pregnant woman. Before suggesting labor induction, the physician always states the reason why this management option is being considered. Indications, contraindications, individual factors are taken into account. If you feel like saying no, I'll wait for spontaneous labor to develop, stop. Ask your doctor to tell you more about the indication for labor induction in your case. Specify what can happen to you and the baby if you refuse and continue to wait. Make a decision carefully, without unnecessary emotions.
If you feel like saying no, I'll wait for spontaneous labor to develop, stop. Ask your doctor to tell you more about the indication for labor induction in your case. Specify what can happen to you and the baby if you refuse and continue to wait. Make a decision carefully, without unnecessary emotions.
Before deciding whether to induce labor, the doctor evaluates the situation:
-
The patient's history (operations on the uterus, cervix, the number of pregnancies and their outcome, the presence of somatic diseases ...). Since often a complicated anamnesis is a contraindication to induction of labor.
-
Recalculates the gestational age (the doctor once again makes sure that the gestational age is accurate). The tendency to overbearing remains the most common reason for induction of labor. Therefore, the exact determination of the gestational age is fundamentally important in this matter.
-
Interprets the result of CBC, OAM, hemostasiograms, blood biochemical parameters.
 Changes in laboratory parameters often require additional examination, consultation of narrow specialists, and decision on management tactics only after the final diagnosis is made.
Changes in laboratory parameters often require additional examination, consultation of narrow specialists, and decision on management tactics only after the final diagnosis is made. -
Obstetric examination allows to determine the position of the fetus, the presenting part, the height of the presenting part. With the pelvic, oblique and transverse position of the fetus, high standing of the presenting part, induction of labor is not carried out.
-
Cervical maturity is assessed by vaginal examination. This is an important and separately assessed factor during the decision to induce labor. The degree of maturity of the cervix is assessed according to the Bishop scale:
| Points | ||||
|---|---|---|---|---|
| 0 | 1 | 2 | 3 | |
| Neck opening (cm) | closed | 1-2 | 2-4 | Over 4 |
| Cervical length | 4 | 2-4 | 1-2 | 1 |
| Head position | -3 | -2 | -1-0 | +1+2 |
| Neck consistency | Thick | Moderately softened | Soft | Soft |
| Neck position | Deviated backwards | Pelvic or anterior | Pelvic Axis | Pelvic Axis |
Obtaining a test result of 8 or more points indicates a mature cervix.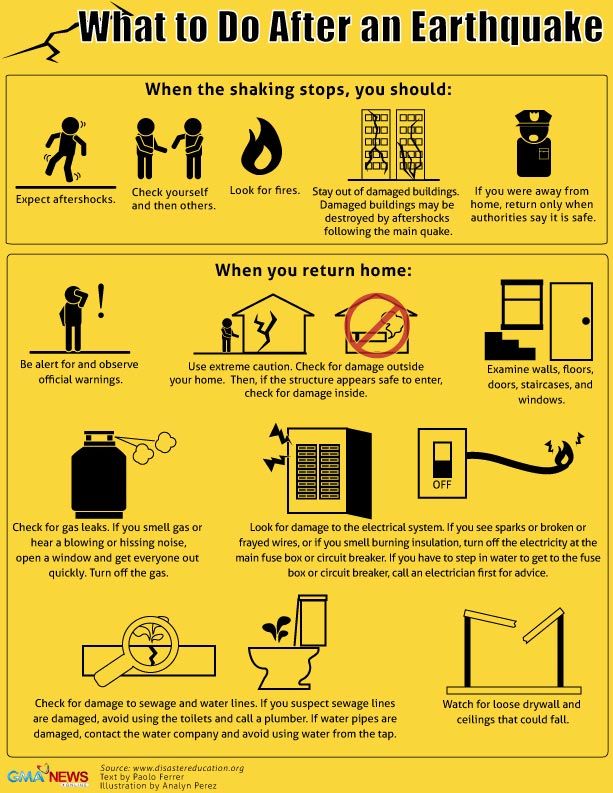 The mature cervix is shortened to 1-2 cm, passes a finger to the internal os in primiparas and beyond the internal os in multiparous, soft, located along the axis of the pelvis, the fetal head is pressed. An insufficiently mature cervix is estimated at 6-7 points. About an immature cervix say 5 or less points (the body is not ready for childbirth) - the cervix is long, dense, the cervical canal is closed or misses the tip of a finger in a multiparous woman, is rejected backwards.
The mature cervix is shortened to 1-2 cm, passes a finger to the internal os in primiparas and beyond the internal os in multiparous, soft, located along the axis of the pelvis, the fetal head is pressed. An insufficiently mature cervix is estimated at 6-7 points. About an immature cervix say 5 or less points (the body is not ready for childbirth) - the cervix is long, dense, the cervical canal is closed or misses the tip of a finger in a multiparous woman, is rejected backwards.
Vaginal examination also evaluates the integrity of the amniotic sac, the capacity of the pelvis, and the nature of the discharge. With an opened fetal bladder, the doctor individually approaches the tactics of managing the patient, taking into account a combination of factors. With a decrease in the capacity of the pelvis, the doctor faces the task of additional examination in order to resolve the issue of the possibility of delivery through the natural birth canal. The presence of pathological discharge is always alarming and gives rise to further examination.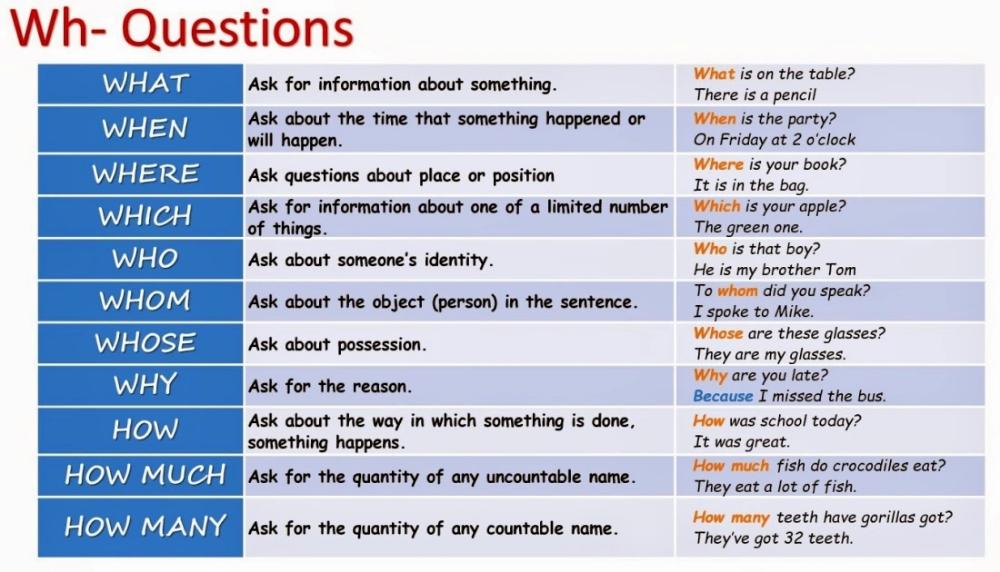
-
A smear is taken for the flora and the degree of purity of the vagina to exclude an infectious and inflammatory process.
-
If necessary, other methods of examination are carried out, narrow specialists are invited for consultation.
-
CTG of the fetus, dopplerography is performed
-
Based on the data obtained, the doctor will decide on further tactics of pregnancy management, preparation for childbirth, method of delivery, delivery.
Let's find out when the doctor suggests labor induction. That is, consider the indications:
-
Immature cervix at 41 weeks and 4-5 days of gestation (this is the most common indication). Further expectant management increases the percentage of complications in childbirth, both on the part of the mother and the fetus.
-
Premature rupture of amniotic fluid. Prolonged lack of development of labor activity increases the risk of complications.

-
Moderate pre-eclampsia
-
Isosensitization by Rh factor or ABO system. Prolongation of pregnancy increases the risk of fetal complications against the background of the progression of the conflict.
-
Mother's diseases, including oncological ones, against which prolongation of pregnancy is inappropriate.
-
Fetal death
There are also contraindications to labor induction (mainly these are conditions in which vaginal delivery is impossible or is accompanied by an increased risk for the mother and (or) fetus):
-
Anatomically narrow pelvis grade 2-3 (or 1 with a pelviography result of a discrepancy between the size of the pelvis and the size of the fetal head)
-
Transverse, oblique, pelvic presentation of the fetus 070
-
Multiple pregnancies
-
Multiparous (5 or more births in history)
-
Operations on the uterus and (or) cervix
-
Tumors of the uterus, cervix, vagina, preventing the passage of the fetus through the natural birth canal
-
Somatic diseases of the mother in the stage of decompensation
-
Subcompensated or decompensated fetoplacental insufficiency, progressive hypoxia of the fetus indications for delivery through natural birth ways
Ways to induce labor
At the stage of vaginal examination, the doctor determines the maturity of the cervix and evaluates the results on the Bishop scale. This is what will be fundamental in resolving the issue of the need for pre-induction (methods aimed at accelerating the maturation of the cervix) or induction (methods aimed at starting labor).
This is what will be fundamental in resolving the issue of the need for pre-induction (methods aimed at accelerating the maturation of the cervix) or induction (methods aimed at starting labor).
The purpose of pre-induction is to ripen the cervix. For pre-induction, medical methods and dilators of the cervical canal are used.
Medical methods include the synthetic progesterone antagonist mifepristone. All women are well aware, and many have taken progesterone preparations during pregnancy (utrogestan, duphaston). The action of progesterone is aimed at maintaining pregnancy. But the time of childbirth comes, and hence the change of the dominant hormone. We need a hormone of the opposite action - a progesterone antagonist. The action of Mifepristone is aimed at the maturation of the cervix and the start of labor. It is prescribed only by the attending physician for an immature or insufficiently mature cervix in a hospital setting.
Preparations of the prostaglandin group also belong to the medical pre-induction of labor.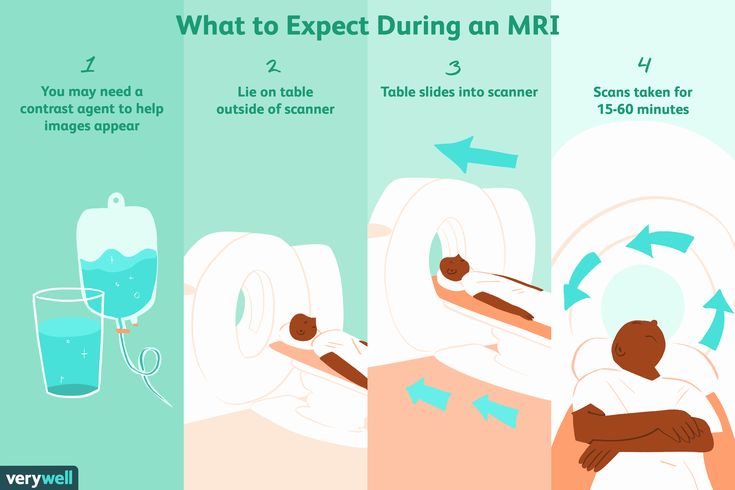 Gel Dinoprostone. What are prostaglandins? These are polyunsaturated fatty acids derived from arachidonic acid. Contains arachidonic acid in red meat, poultry, fish, oils. This is a note to you and a reminder of the importance of a balanced diet. Prostaglandins contribute to the maturation of the cervix, stimulate the contractile activity of the uterus. The level of prostaglandins rises before childbirth, but especially in childbirth. Dinoprostone is administered intravaginally (into the posterior fornix of the vagina) for an immature cervix and intracervically (into the cervical canal) for an insufficiently mature cervix. The gel is prescribed and administered only by an obstetrician-gynecologist.
Gel Dinoprostone. What are prostaglandins? These are polyunsaturated fatty acids derived from arachidonic acid. Contains arachidonic acid in red meat, poultry, fish, oils. This is a note to you and a reminder of the importance of a balanced diet. Prostaglandins contribute to the maturation of the cervix, stimulate the contractile activity of the uterus. The level of prostaglandins rises before childbirth, but especially in childbirth. Dinoprostone is administered intravaginally (into the posterior fornix of the vagina) for an immature cervix and intracervically (into the cervical canal) for an insufficiently mature cervix. The gel is prescribed and administered only by an obstetrician-gynecologist.
Non-pharmacological methods include Dilapan-S dilator. It is a dense synthetic gel in the form of a rod. The gel is injected into the cervical canal. The action of the gel is based on the absorption of fluid from the cervix. The diameter of the rod gradually increases, mechanically expanding the cervical canal.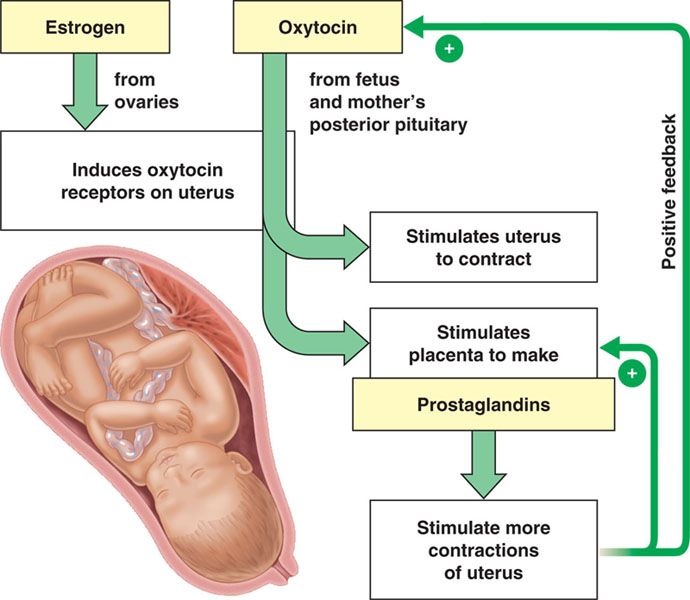 Against the background of tissue stretching, a cascade of reactions is triggered, leading to the maturation of the cervix and the development of labor.
Against the background of tissue stretching, a cascade of reactions is triggered, leading to the maturation of the cervix and the development of labor.
Foley catheters. Based on mechanical pressure. A catheter is inserted through the cervical canal. The catheter balloon is filled with isotonic saline. Under the action of mechanical pressure, the cervix opens, the production of prostaglandins increases, the maturation of the cervix and the development of regular labor activity are stimulated.
Against the background of activities aimed at maturation of the cervix (pre-induction), there is a high probability of the development of regular labor activity. The birth act starts.
Induction of labor (stimulation of labor) is performed on the mature cervix. The cervix may be mature initially upon admission to the hospital or mature during pre-induction.
When should one think about labor induction (labor stimulation)?
Naturally, only if there are indications, no contraindications, the written consent of the woman and against the background of a mature cervix.
Time passes, the cervix is mature, there are indications for induction, there are no contraindications, the woman signed the consent - it's time for induction of labor.
In the modern world, induction of labor is not seen as something extraordinary. Timely induction of labor allows avoiding a number of complications both from the side of the mother and from the side of the fetus, to give birth to a baby through the natural birth canal, which is undoubtedly the most favorable. So how can a doctor help start labor
-
Amniotomy (opening the membranes of the membranes of the membranes) is one of the methods of labor induction. It is carried out by an obstetrician-gynecologist and is absolutely painless for a pregnant woman. During and after the amniotomy, the production of oxytocin, prostaglandins increases, the presenting part is pressed against the internal pharynx, making mechanical pressure. All this leads to the launch of labor activity (usually after a few hours).
-
Administration of oxytocin. Oxytocin is a hormone that is produced in the hypothalamus, enters the pituitary gland, and then into the bloodstream. Its concentration in the blood increases before childbirth. The action of oxytocin is aimed at increasing the contractility of the myometrium, which leads to the development of regular labor activity. With a reduced concentration of the hormone in the blood, the development of labor activity is delayed. The introduction of synthetic oxytocin (an exact analogue of natural) leads to the development of regular labor activity. It is prescribed only by an obstetrician-gynecologist and is carried out under the monitoring of the fetus and mother.
-
Combination of amniotomy and oxytocin. After the amniotomy is completed, oxytocin is administered intravenously.
How long does labor induction last?
When will it start? This question is asked by all women who are preparing the cervix and stimulating labor.
Many schemes have been developed to induce labor and prepare the cervix. This may be the effect of one drug, method, or a combination of them. When choosing a scheme, the obstetrician-gynecologist considers an individual approach in each case. It depends on the degree of maturity of the cervix, indications and contraindications, the obstetric situation, the woman's consent to the events.
In some situations, the waiting time for the development of regular labor activity can be limited to a day, for example, in case of premature rupture of amniotic fluid and there are no indications for an emergency caesarean section. In others, you can wait 3 days or add other methods of induction (pre-induction), for example, with a tendency to overbearing in the absence of indications for operative delivery in a particular situation.
The majority of pregnant women develop regular labor even during the preparation of the cervix.
If the cervical ripening method fails, the doctor will consider another method (combined method) or a caesarean section.
If combined approaches to the maturation of the cervix do not give a positive effect, then the option of delivery remains caesarean section.
With a positive effect from the preparation of the cervix (the cervix is characterized as mature), the doctor recommends and performs (naturally after the written consent of the patient) labor induction.
The development of regular labor activity against the background of preparation and (or) stimulation of labor does not always guarantee delivery through the natural birth canal. Emergency indications for operative delivery may appear, as in women whose childbirth began spontaneously.
Conclusions
-
There are clear indications and contraindications for labor induction.
-
Before you make a decision, ask the doctor all the questions you are interested in, specify why you are offered this option. And only after receiving full information, make decisions.