What to expect after labor
Recovering From Delivery - Postpartum Recovery
Your body has just done one of the most remarkable things it will ever do: grow another human being. After 9 months of waiting, you are probably excited to finally be home with your new baby. Much of your focus and energy during the coming weeks and months will be on baby, but remember that you also need to take care of yourself, too.
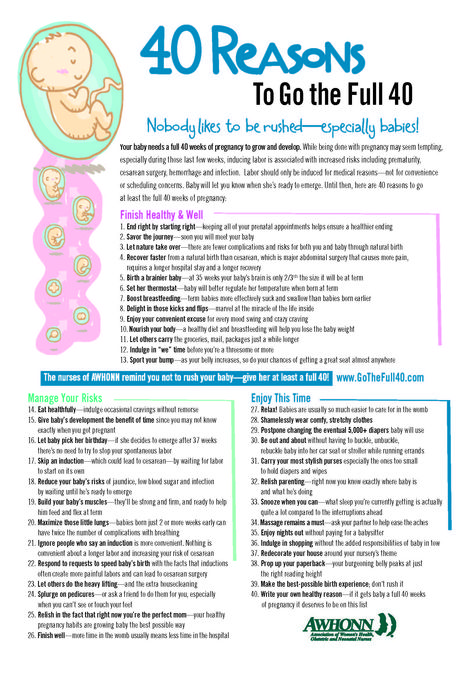
Your delivery may have been complicated or easy. You may have had a cesarean birth (C-section) or vaginal delivery. You may have labored for a few hours or a few days. No matter what your delivery looked like, your body has been through a trauma just the same. It is going to need time to recover.
Your postpartum recovery won’t be just a few days. Fully recovering from pregnancy and childbirth can take months. While many women feel mostly recovered by 6-8 weeks, it may take longer than this to feel like yourself again. During this time, you may feel as though your body has turned against you. Try not to get frustrated. Remember that your body is not aware of your timelines and expectations. The best thing you can do for it is rest, eat well, and give yourself a break.
During this time, your hormones also will be fluctuating. You may not be thinking clearly and will be more emotional. Again, give yourself time for this to pass. However, if at any time you think about hurting yourself or your baby, tell someone.
Path to improved health
It took the better part of a year to grow and have a baby. Take comfort in knowing that, for the most part, you will begin to feel like yourself much sooner than that. In a few months, you should be well on your way to recovery.
That is not to say that postpartum recovery won’t have its challenges. It is very common to feel as though your body is not healing as quickly as you’d like. Remember, the more you can rest your body and let it fully recover, the better you’ll be for it. Even if you can only manage to eat, sleep, and care for your baby, that is enough.
During the first six weeks, pay attention to your body. You’ll be tired and focused on your baby, but try to notice changes with your own body. This is very important as you heal.
As you begin to feel better, resist the temptation to do more. Overdoing things at this point can set you back in your recovery. Concentrate on nourishing your body with good foods, drinking plenty of water (especially if you are breastfeeding), and getting enough rest.
If you’ve had a C-section, you’ll have more restrictions about what you can do in the days and weeks following childbirth. Common don’ts include driving and lifting anything heavier than your baby. Your doctor will let you know when you can resume normal activities.
Here is more of what you can expect during your postpartum recovery.
Abdominal pain. As your uterus shrinks back into its normal size and shape, you will feel pain in your abdomen (lower belly). These pains are called “afterpains.” Most of these pains will be dull, but some will be sharp. You may feel more of these pains as you breastfeed your baby. That is because breastfeeding stimulates a chemical in your body that causes the uterus to contract (tighten). For many women, applying heat to the area helps control the pain. Consider using a heating pad or hot water bottle. Your abdominal pain should ease up over time. If these pains get worse or don’t let up, you should call your doctor.
You may feel more of these pains as you breastfeed your baby. That is because breastfeeding stimulates a chemical in your body that causes the uterus to contract (tighten). For many women, applying heat to the area helps control the pain. Consider using a heating pad or hot water bottle. Your abdominal pain should ease up over time. If these pains get worse or don’t let up, you should call your doctor.
Baby blues. You are so excited and happy to bring baby home. The next minute, though, you are sad. It can be confusing, especially to new moms. Know that many women (70-80%) struggle with feeling sad the first few weeks after having a baby. It is commonly called the “baby blues” and is caused by hormone changes. It is nothing to be ashamed of. In fact, confiding in a friend of family member can often make you feel better. If these feelings last more than a few weeks or you are not able to function because of them, you could have postpartum depression. Postpartum depression is more serious than baby blues. If you have severe feelings of sadness or hopelessness, you should call your doctor.
If you have severe feelings of sadness or hopelessness, you should call your doctor.
Constipation. It is very common to be constipated in the days following childbirth. There are several things that could cause this. If you received any pain-relieving drugs in the hospital, they could slow down your bowels. If you had anesthesia (a pain blocker) for any reason, that also can cause it. Sometimes, postpartum constipation is brought on simply by fear. This is true especially if you have stitches because you had an episiotomy (a surgical cut between the vagina and anus to widen the vaginal opening for childbirth) or tore this area during delivery. You may be afraid of damaging the stitches or be afraid that a bowel movement will cause even more pain in that area. To help ease constipation, drink plenty of water and try to eat foods that offer a lot of fiber. In many cases, you may want to talk to your doctor about prescribing a stool softener (such as Colace or Docusoft). If you haven’t had a bowel movement by four days postpartum, call your doctor.
If you haven’t had a bowel movement by four days postpartum, call your doctor.
Hemorrhoids. You may have developed hemorrhoids (painful swelling of a vein in the rectum) during your pregnancy. If not, you may have gotten them from the strain and pushing during delivery. They can cause pain and bleed after a bowel movement. They also itch. You can get some relief from the pain and itching by applying witch hazel to your hemorrhoids. This is especially effective if you keep the witch hazel in the refrigerator. Your hemorrhoids should shrink over time. If not, contact your doctor.
Hormonal shifts. Besides fueling your mood swings (see “Baby blues,” above), hormones are also responsible for other postpartum symptoms. You may be sweating more, especially at night when you sleep. Just make sure that your sweating is not accompanied by a fever. That could be a sign of infection. Hormonal changes also cause hair loss for many new moms. This is only temporary. When your estrogen levels increase, your hair will return to its normal thickness.
When your estrogen levels increase, your hair will return to its normal thickness.
Perineum soreness. The perineum is the area between your vagina and anus. Many times, this area will tear during childbirth. Other times, your doctor may have to make a small cut in this area to widen your vagina for childbirth. Even if neither of these things happened during your vaginal birth, your perineum will be sore and possibly swollen postpartum. You may feel discomfort in this area for several weeks. While you recover, sitting on an icepack several times a day for 10 minutes will help relieve the pain. This is especially good to do after going to the bathroom. During the first week postpartum, also use a squirt bottle to rinse the perineum with warm water after using the toilet. Notify your doctor if your perineum area does not get less sore each day or you have any sign of infection.
Sore nipples and breasts. The first few days of breastfeeding, it is normal for women to have sore nipples and breasts. If the soreness continues beyond a few days, it could be that the baby isn’t latching correctly. Try changing positions or consult a lactation expert (breastfeeding expert) for help. Do this before your nipples develop painful cracks, which could sideline your breastfeeding. The American Academy of Family Physicians (AAFP) recommends that all babies, with rare exceptions, be breastfed and/or receive expressed human milk exclusively for the first six months of life. Breastfeeding should continue with the addition of complementary foods throughout the second half of the first year.
If the soreness continues beyond a few days, it could be that the baby isn’t latching correctly. Try changing positions or consult a lactation expert (breastfeeding expert) for help. Do this before your nipples develop painful cracks, which could sideline your breastfeeding. The American Academy of Family Physicians (AAFP) recommends that all babies, with rare exceptions, be breastfed and/or receive expressed human milk exclusively for the first six months of life. Breastfeeding should continue with the addition of complementary foods throughout the second half of the first year.
Stitches. If you have stitches due to a torn or cut perineum (see “Perineum soreness,” above), it will take 7-10 days to heal. The stitches will absorb over time. It is important that you keep the stitches from getting infected by gently cleaning them with warm water after each time you use the toilet. Do this by using a squirt bottle to rinse the area and pat it dry. Do not wipe the area with toilet paper or you could irritate the stitched area. No matter how eager you are to check the healing progress, try to keep you hands off the stitches. If the area begins to hurt worse or the stitches seem weepy, contact your doctor. It could be a sign of infection.
No matter how eager you are to check the healing progress, try to keep you hands off the stitches. If the area begins to hurt worse or the stitches seem weepy, contact your doctor. It could be a sign of infection.
If you have stitches from a cesarean birth (C-section), these heal in varying degrees. The stitches in the skin should heal in 5-10 days. The underlying stitches in your muscle layer will take longer to heal. These won’t completely heal for 12 weeks. For the stitches that you can see, make sure to watch for any signs of infection. These signs include if the incision area is red, swollen, or weeping pus; or if you have a fever.
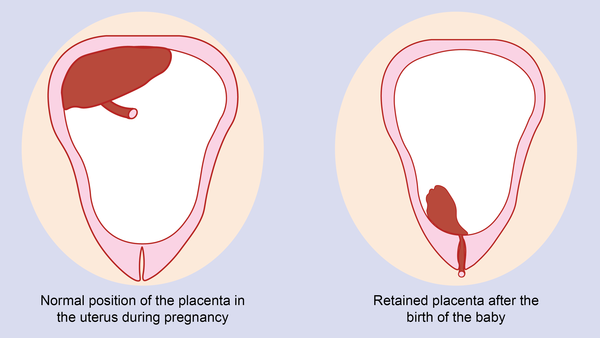
Vaginal bleeding and discharge. After giving birth, it is common that you will have vaginal bleeding and discharge (this is called lochia), even if you had a C-section. This is your body’s way of eliminating the extra blood and tissue that was used to grow and nourish your baby. Expect for this to be heavier at first (up to 10 days), but then taper off. Light bleeding and spotting can last up to six weeks after delivery. It is important that you use only sanitary pads during this time. Using tampons can introduce bacteria and lead to infection. Also expect to pass some clots, especially the first week. If clots are bigger than a quarter, you should contact your doctor.
Light bleeding and spotting can last up to six weeks after delivery. It is important that you use only sanitary pads during this time. Using tampons can introduce bacteria and lead to infection. Also expect to pass some clots, especially the first week. If clots are bigger than a quarter, you should contact your doctor.
Water retention. You may be eager for that swelling you noticed during your pregnancy to go away. It won’t, though, for a while longer. Also known as postpartum edema (swelling), your body will continue to hold on to water because of an increase in a hormone called progesterone. You may notice the swelling in your hands, legs, and feet. It shouldn’t last much longer than a week after delivery. If it does or if it seems to get worse over time, be sure to tell your doctor.
Weight loss. If you were hoping for immediate weight loss after your baby was born, you were probably very disappointed. No mother is that lucky, no matter what you read in the tabloids. You can expect to lose about 6-12 pounds (depending on the size of your baby) during the birth. After that, your weight loss will slow considerably. Depending on how much weight you gained during pregnancy (the average is 25-35 pounds), it may take several months to lose the baby weight. For many women, breastfeeding seems to help promote weight loss. Other moms don’t see weight loss associated with breastfeeding. Try to keep your nutrition consistent while you are breastfeeding and do not get frustrated if it takes longer than you’d hoped to lose the weight.
You can expect to lose about 6-12 pounds (depending on the size of your baby) during the birth. After that, your weight loss will slow considerably. Depending on how much weight you gained during pregnancy (the average is 25-35 pounds), it may take several months to lose the baby weight. For many women, breastfeeding seems to help promote weight loss. Other moms don’t see weight loss associated with breastfeeding. Try to keep your nutrition consistent while you are breastfeeding and do not get frustrated if it takes longer than you’d hoped to lose the weight.
Things to consider
Pay attention to your body after giving birth. If something doesn’t seem right, it probably isn’t. Soreness is to be expected, but too much pain could mean something is seriously wrong. Don’t be so wrapped up in caring for your baby that you ignore your own health.
Just because you’ve made it through delivery, you are not necessarily out of danger for health complications. There are life-threatening problems related to childbirth that can happen days or weeks after delivery.
- Postpartum hemorrhage is rare but can happen. If your postpartum bleeding is filling more than a pad every hour, you should contact your doctor immediately. Without treatment, postpartum hemorrhage can be fatal.
- Headaches that are severe and don’t go away can also signal an underlying problem, especially coupled with high blood pressure. You could be in danger of having a stroke.
- Deep vein thrombosis (a blood clot in a deep vein) is a somewhat uncommon problem (1 in every 1,000 pregnancies) that can occur during or after pregnancy. Symptoms include leg pain or feeling like you have a pulled muscle. Your leg may also be red and hot to the touch. Left untreated, these clots can break away and travel to your lungs. When this happens, it can be life-threatening.
- Postpartum preeclampsia is rare and can develop within 48 hours after childbirth or as late as six weeks after childbirth. It is similar to preeclampsia (also called toxemia), which can occur while you’re pregnant.
 Both preeclampsia and postpartum preeclampsia cause your blood vessels to constrict (get smaller). This results in high blood pressure and also distresses your internal organs. Sometimes there are no obvious symptoms, unless you are monitoring your blood pressure. When you do have symptoms, they may include severe headache, swelling of your hands and feet, blurred vision, pain in the upper right portion of your body, and sudden weight gain. If you suspect you may have postpartum preeclampsia, call your doctor immediately.
Both preeclampsia and postpartum preeclampsia cause your blood vessels to constrict (get smaller). This results in high blood pressure and also distresses your internal organs. Sometimes there are no obvious symptoms, unless you are monitoring your blood pressure. When you do have symptoms, they may include severe headache, swelling of your hands and feet, blurred vision, pain in the upper right portion of your body, and sudden weight gain. If you suspect you may have postpartum preeclampsia, call your doctor immediately.
When to see a doctor
When you are recovering from delivery, it is best to err on the side of caution if you feel that something is not right with you or with the baby. You should expect to have some discomfort as you heal. You should not begin to feel worse.
In general, if you have any of these postpartum symptoms, call your doctor.
- Heavy vaginal bleeding that soaks more than one pad per hour or vaginal bleeding that increases each day instead of decreasing.
- Passing large clots (bigger than a quarter).
- Chills and/or a fever of more than 100.4°F.
- Fainting or dizziness.
- Changes to your vision or a severe headache (persistent).
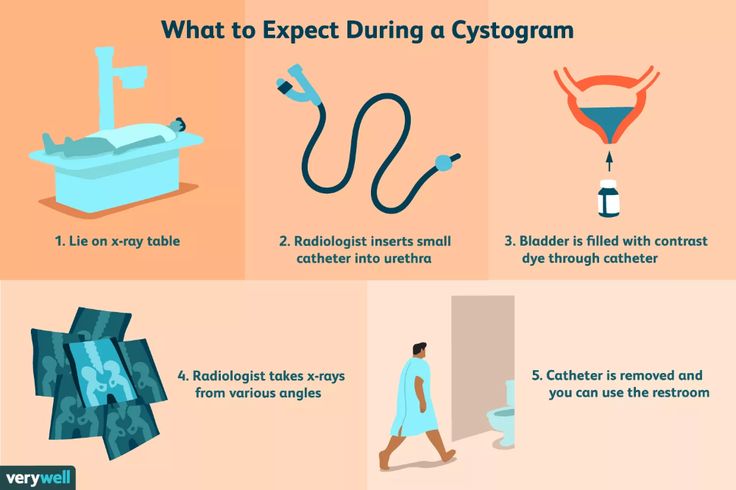
- Painful urination or difficulty urinating.
- Vaginal discharge with a strong odor.
- Heart palpitations, chest pain or difficulty breathing.
- Vomiting.
- Incision from C-section or episiotomy is red, weepy (with pus), or swollen.
- Abdominal (lower belly) pain that is getting worse or new abdominal pain.
- Sore breasts that are red or feel hot to the touch.
- Pain in your legs with redness or swelling.
- Increase in swelling.
Questions to ask your doctor
- How long until I will feel like myself again?
- Why am I still retaining water?
- How many calories should I eat while I’m breastfeeding?
- When can I begin exercising?
- How long should I wait before having sex again?
- Can I get pregnant while I’m breastfeeding?
- Why is my hair falling out?
- Are there foods I shouldn’t eat while breastfeeding?
- Why aren’t I losing weight?
- What are my options for birth control?
- Will my breasts go back to normal?
- Why do I have no interest in sex?
Resources
Centers for Disease Control and Prevention (CDC): Depression Among Women
National Institutes of Health, MedlinePlus: Postpartum Care
Postpartum Support International
U. S. Department of Health and Human Services, Womenshealth.gov: Pregnancy: Recovering from Birth
S. Department of Health and Human Services, Womenshealth.gov: Pregnancy: Recovering from Birth
Postpartum recovery: What to expect
The moment you’ve been waiting for is finally here. After months of nurturing a growing baby in your belly and long hours of childbirth, your little one is part of the outside world now. Congratulations!
You just did an incredibly beautiful and difficult thing. Now comes the transition from pregnancy to postpartum – and chances are you’re going to feel tired, sore and a little anxious. But what exactly can you expect after giving birth?
Your body and emotions are going to experience a lot of changes in the days and weeks following childbirth. Here are some of the key things to expect immediately after giving birth and during the postpartum recovery process.
Postpartum recovery timeline
How long is the postpartum period?
No matter how you delivered your baby, the postpartum recovery period is generally considered to be the first six weeks after childbirth.
This doesn’t mean that at six weeks you’ll magically bounce back to pre-baby condition. Instead, this refers to postpartum healing, which is the physical healing of your body after birth.
How long does it take to heal after giving birth?
By the six-week mark, your vagina, perineum or C-section incision should be healed, and your uterus should be back to its normal size. Throughout those first weeks, you’ll experience a lot of changes – from new levels of tiredness to hormone fluctuations. And you’ll probably continue to see changes in your body and emotions for several weeks after the initial six weeks of recovery.
Your postpartum body: How your body will feel and change after giving birth
Postpartum hormone changes
Hormones are your body’s chemical messengers that tell your body how to do something and when to do it. During pregnancy, your hormones changed to help support your growing baby and prepare your body for childbirth. After giving birth, your hormones are on a new mission to help you heal, bond with your baby and breastfeed your baby if you choose to.
The first postpartum hormone changes your body will go through are:
- Estrogen and progesterone levels decrease when your baby and the placenta are delivered.
- Oxytocin – known as the bonding hormone – surges and contributes to the strong parental instinct you’ll feel.
- Prolactin increases to signal milk production.
Bleeding and vaginal discharge
As your uterus sheds that thick lining it maintained during your pregnancy, you’ll experience some vaginal bleeding and discharge – which is known as lochia. Even if you had a cesarean (C-section), you’ll experience bleeding and discharge.
Lochia will start out as bright red for a day or two before gradually fading to pink, and then light brown or light yellow. Bleeding and discharge will be the heaviest within the first several days after having your baby, but will become lighter as time goes on. Typically, lochia can last 4-6 weeks, with discharge continually decreasing.
How much bleeding is too much?
Early on, it may seem like you’re bleeding a lot – similar to having a very heavy period. This is totally normal, but there are a few signs to watch for.
This is totally normal, but there are a few signs to watch for.
If you’re soaking through one pad an hour for more than two hours, call the nurse line or your care provider right away. Also, if you continue to have bloody discharge or pass blood clots for more than four weeks, call your care provider.
Increased bleeding after your lochia starts to decrease can be a sign you’re overdoing it and need more rest. Seeing ongoing clots could mean your uterus is having trouble getting back to its pre-pregnancy size. In either case, it’s always best to call.
When can you expect your first postpartum period?
Several factors can affect when you get your first period after giving birth. One of the biggest factors is whether you’ve chosen to breastfeed your baby and if your breastmilk is their only food source.
Typically, those who do not breastfeed may expect their period to return sooner than those who do – anywhere from four weeks to three months after giving birth. For those that do breastfeed, some may get their period within that same timeframe – but many may not get their period until they’ve begun to wean or stopped breastfeeding entirely.
For those that do breastfeed, some may get their period within that same timeframe – but many may not get their period until they’ve begun to wean or stopped breastfeeding entirely.
Vaginal and perineum soreness
Both your vagina and your perineum (the area between your vagina and rectum) will feel very tender and sore from the strain of childbirth.
If you gave birth vaginally, it’ll probably take you a few weeks to heal, especially if your perineum tore or you had an episiotomy. If you labored or pushed at all, but eventually gave birth by C-section, it’s very likely that you’ll still be sore.
In our “Postpartum essentials” section below, we’ll talk about what you can do to relieve postpartum vaginal pain, and promote healing.
After-birth pains (contractions)
Contractions after birth, also called after-birth pains, might be uncomfortable at times but nothing like what you may have experienced during labor. Actually, contractions after birth are signaling something good.
After-birth contractions help reduce uterine bleeding, and help shrink your uterus back to its usual, pre-baby size.
You may notice after-birth pains the most if you breastfeed. This is because breastfeeding causes your body to release oxytocin, a hormone that causes uterine contractions.
Engorged breasts
Your breasts have been changing since the beginning of your pregnancy. And around the third or fourth day after giving birth, you’ll notice the next big change as your breasts will start filling with milk. Your breasts may become engorged and feel firm, swollen and sore.
That initial tightness and soreness will wear off whether you choose to breastfeed or not. But if you choose to breastfeed, your breasts will usually feel full before feeding or pumping sessions. And you may experience more of that tender, heavy feeling if your next session is a little overdue.
Sore or cracked nipples
Blood flow to your nipples increases throughout your pregnancy, so you’ve probably noticed some tenderness for several months. But the first few days after giving birth brings that blood flow to a new height, making them particularly sensitive. And naturally, if you choose to breastfeed, that will have an impact, too.
But the first few days after giving birth brings that blood flow to a new height, making them particularly sensitive. And naturally, if you choose to breastfeed, that will have an impact, too.
As your baby learns how to properly latch on to your breast, it’s common to experience a little pain at first. But once baby gets a good latch, that should go away. A little discomfort as baby gets into a rhythm is normal, but feeling constant pain throughout your feeding is not.
If you find that you have breastfeeding problems, a lactation consultant can be a big help – and you can ask for one right in the hospital.
Sore muscles
You’ve just finished the mother of all workouts, so it's normal to feel some muscle soreness throughout your body following birth. And you may feel the aftereffects of your hard work for a few days.
You can expect to feel especially sore anywhere you held a lot of tension during labor, such as in your arms, neck or jaw.
Tiredness
Fatigue is another perfectly normal postpartum symptom. Again, your body has just gone through (and is still going through) a lot, so it’s important to get as much rest as you need.
Again, your body has just gone through (and is still going through) a lot, so it’s important to get as much rest as you need.
Many care providers recommend sleeping whenever your baby does. You and your baby’s well-being are the most important things right now. Eating healthy and staying hydrated will also help you restore and maintain your energy levels over time.
Night sweats
Many people experience postpartum night sweats due to changing hormones. While they can be uncomfortable, they aren’t anything to worry about. Just make sure you’re drinking enough water and try to stay cool. Night sweats should subside in a couple weeks.
Lower abdominal pain on and near your incision (if you had a C-section)
After a C-section, you’re going to feel pain and tenderness on and near your incision, especially for the first few days and weeks as you recover.
C-section recovery timeline
The postpartum recovery process after a C-section tends to be a bit longer than a vaginal birth. You’ll likely stay in the hospital for an extra day, and you’ll have certain restrictions on bending and lifting. You may also be prescribed pain medication to take for one to two weeks after delivery.
You’ll likely stay in the hospital for an extra day, and you’ll have certain restrictions on bending and lifting. You may also be prescribed pain medication to take for one to two weeks after delivery.
Before you go home, you’ll get detailed instructions for how to care for your incision and promote healing. Your incision should be healed around six weeks after giving birth.
Caring for your C-section incision
When taking care of your incision, it’s important to be as gentle as possible while keeping it clean and dry. This may mean:
- Cleaning your incision once or twice a day with mild soap. Either run soap and water over it in the shower, or gently use a washcloth or bath sponge.
- Dabbing away excess water with a clean towel, then air drying the rest.
- Wearing gauze bandages to absorb drainage and protect your clothes, and changing the gauze daily or if it gets wet.
How your mood, attitude and emotions can change after childbirth
Having a new baby can bring a wide range of emotions along with it. Of course, it’s going to be beautiful and exciting, but it’s also going to put new pressures on you, your time and your energy. Here are a couple changes you can expect.
Of course, it’s going to be beautiful and exciting, but it’s also going to put new pressures on you, your time and your energy. Here are a couple changes you can expect.
You’re very likely to experience some baby blues
After all the excitement and beauty of birth, it can be surprising and confusing to suddenly feel bouts of sadness, anxiety or irritability. But this isn’t just normal, it’s incredibly common.
In fact, about 80% of new moms experience a range of emotions or mood swings during their first days with their baby. This is what’s known as the baby blues. The baby blues may also give you insomnia or make you feel overwhelmed at times. But they usually go away on their own within two weeks.
During this time, it’s important to be particularly kind to yourself. It can help to talk to your partner or loved ones about how you feel. Share how you’re feeling so they can support you and help you get through it.
If your baby blues last more than two weeks or your symptoms become more severe, call your care provider. You may be experiencing postpartum depression.
You may be experiencing postpartum depression.
Your interest in sex may decrease
There are several reasons you may not feel like being intimate with your partner after giving birth. You’re tired and spending a lot of time and energy on being a great parent. Your body may still be healing or experiencing hormonal shifts.
Talking about what you’re experiencing with your partner can help them better understand your feelings. Also, knowing when sex is considered safe again is important for setting the right expectations for yourself and your partner.
How long after giving birth can you have sex?
Typically, you can begin having sex – if you feel comfortable and your care provider says it’s okay – around six weeks after giving birth. Keep in mind that hormonal changes can cause your vagina to feel dry and tender, especially if you’re breastfeeding. Using a personal lubricant will help ease discomfort.
It’s also possible to get pregnant in the postpartum period, even if you’re breastfeeding and haven’t noticed your period yet. It’s hard to know when ovulation will return after giving birth, so be sure to use protection. Your postpartum visit is a great time to discuss birth control options.
It’s hard to know when ovulation will return after giving birth, so be sure to use protection. Your postpartum visit is a great time to discuss birth control options.
You may notice changes in your relationship with your partner
You and your partner probably know that your relationship is going to change with your baby’s arrival, but it may still come as a shock. It’s perfectly normal. Your lives are both different now, and it’s going to take some getting used to. Open and honest communication is going to be your best tool as you both adjust to your new life together as parents.
Postpartum essentials: What you’ll need on hand as you recover
Your care team will make sure you have what you need to begin the postpartum healing process during your hospital stay. (And they may even send you home with a few things.) But there are several postpartum necessities you should have on hand at home for when you return from the hospital.
- Pain relief medication – Acetaminophen (Tylenol) or ibuprofen (Advil) can both help relieve aches and pains.
 Your care provider may even recommend alternating between the two medications during the first few days of recovery. Just make sure you follow their instructions and ask any questions you may have. If you’ve had a C-section, your care provider may prescribe a pain relief medication for you to take during the first couple of weeks post-delivery.
Your care provider may even recommend alternating between the two medications during the first few days of recovery. Just make sure you follow their instructions and ask any questions you may have. If you’ve had a C-section, your care provider may prescribe a pain relief medication for you to take during the first couple of weeks post-delivery. - Postpartum belly band – Belly bands use light compression to help ease some of the aches and pains as you heal. Bands wrap around your abdomen, from your hips up to your ribs. Some women find that wearing a band reduces their back pain, supports their pregnancy-stretched core muscles and takes some of the pressure off their incision if they had a C-section. You may be given a postpartum belly band at the hospital if you have a C-section.
- Absorbent maxi pads – Tampons will be off limits until you’ve fully recovered, so you’ll need comfortable yet absorbent maxi pads for the bleeding and discharge you’ll experience.
- 100% cotton underwear – Cotton is breathable and can wick away moisture. Since you’ll be bleeding on and off for several weeks – and more heavily at first – choose underwear you’ll be okay with throwing away if it becomes stained. You can also find disposable cotton underwear, similar to what the hospital will provide for you. (Tip: Ask for a few extra pairs of disposable undies from the hospital. Many people find them to be incredibly comfortable, especially the first few days after having a baby.)
- Ice packs – Ice packs in various forms will be an effective way to get relief from pain and inflammation. You can even get wearable ice pads for your perineal and vaginal areas. But the classic ice pack wrapped in a towel will still do wonders. Ice packs can also reduce discomfort from sore or engorged breasts.
- Peri rinse bottle – As your vagina and perineum recover, use a peri bottle or spray bottle filled with warm water to promote healing and protect any stitches.
 The warm water is soothing and will enable you to gently rinse off your perineal area after you go to the bathroom. You’ll receive a peri bottle in the hospital that you can take home.
The warm water is soothing and will enable you to gently rinse off your perineal area after you go to the bathroom. You’ll receive a peri bottle in the hospital that you can take home. - Sitz bath – A sitz bath, which is when you sit in warm, shallow water, can also be used both to soothe irritation and clean your perineum. You can take a sitz bath in your bathtub or buy a kit with a plastic bowl that fits onto your toilet.
- Witch hazel pads – Witch hazel pads are great for soothing postpartum hemorrhoids, but they can also help ease perineal soreness.
- Hemorrhoid spray with lidocaine – Lidocaine is a local anesthetic and is used as an ingredient in certain sprays. These sprays can give you fast, cooling relief from pain and irritation caused by postpartum hemorrhoids.
- Stool softener – You may experience constipation in the weeks following birth. A stool softener can be a gentle way to help things move along smoothly, and put less strain on your vaginal and perineal areas – especially if you’ve received stitches.
- Nursing bras for day and night – Nursing bras are designed to give you comfort and support without irritating sensitive areas. They also come with flaps that open to make it easy for your baby to feed without having to remove your bra. Even if you aren’t breastfeeding, a snug, comfortable bra that provides firm support will do wonders. Wear bras that do not have an underwire.
- Lanolin and nipple creams – These special creams are a go-to treatment for sore, dry or cracked nipples. They can be applied any time you’re feeling discomfort. And many creams are made with baby-safe ingredients, so that you don’t have to wash them off before you breastfeed. HealthPartners’ Health and Care Stores carry an organic, herbal salve that our lactation consultants recommend, along with other helpful breastfeeding products.
- Nursing pads – If you’re breastfeeding, it’s common to experience some milk leakage between feedings. Even if you’re not breastfeeding, you may still leak a little colostrum or milk from your breasts early on.
 Nursing pads fit comfortably inside your bra to soak up leaks and help prevent a wet shirt. You can get reusable pads or disposables depending on your preference. Both need to be changed throughout the day.
Nursing pads fit comfortably inside your bra to soak up leaks and help prevent a wet shirt. You can get reusable pads or disposables depending on your preference. Both need to be changed throughout the day. - Heating pad – As far as self-care tools go, the heating pad is a classic. Resting against a source of gentle, focused heat can help with a variety of aches and pains, from your lower back to your breasts.
- Help – Your partner, family and friends can be good resources for you as you recover. You have an important job to do, so be ready to ask for and accept help with chores, meals and anything else.
Get answers to all your postpartum recovery questions
During your postpartum healing period, you’ll experience a lot of physical and emotional changes, and some may surprise you no matter how prepared you are. Just know that we’re here for you if you have questions or need help. Our nurse lines are staffed with experienced nurses who are available 24/7.
HealthPartners patients can call 800-551-0859. Park Nicollet patients can call their clinic directly during business hours, and 952-993-4665 after hours. And if you have questions or need advice about taking care of your new baby, our BabyLine is also available 24/7 at 612-333-2229.
And if you’re looking for more resources, check out our pregnancy and parenting resources guide that connects you with helpful information no matter where you are in your journey.
Recovery after childbirth - where to start
MainLibraryWomen's HealthRecovery after childbirth: terms, specialists, procedures
Childbirth is over, you have become a mother. And ahead is a new life: with new emotions, sensations, new questions and, first of all, with a new perception of oneself. But how can one feel this incomparable happiness if the body hurts, it is unpleasant to move, it is impossible to sit, every now and then it throws you into a fever and for some reason not everything is as smooth and joyful as you would like? nine0003
This is normal. These changes are necessary and important. What happens to the female body during this - the postpartum period, for which nature has given us 6-8 weeks? Within a few hours (!) after childbirth, the nervous, cardiovascular and other systems of the female body begin to rebuild, and hormones are tuned to a new stage - lactation. At the same time, a woman needs to comprehend what happened, get used to new feelings and sensations - this is also an important psychological stage. This is a multi-stage and difficult process, on the “quality” of which the psycho-emotional stability of the mother depends. And her condition, in turn, affects the adaptation and development of the child (for example, some psychotherapists believe that certain areas of our brain are formed in the first six months of life and directly depend on the emotional relationship with the mother in these months). nine0003
These changes are necessary and important. What happens to the female body during this - the postpartum period, for which nature has given us 6-8 weeks? Within a few hours (!) after childbirth, the nervous, cardiovascular and other systems of the female body begin to rebuild, and hormones are tuned to a new stage - lactation. At the same time, a woman needs to comprehend what happened, get used to new feelings and sensations - this is also an important psychological stage. This is a multi-stage and difficult process, on the “quality” of which the psycho-emotional stability of the mother depends. And her condition, in turn, affects the adaptation and development of the child (for example, some psychotherapists believe that certain areas of our brain are formed in the first six months of life and directly depend on the emotional relationship with the mother in these months). nine0003
Previously, it was believed that after giving birth, the mother should not be disturbed, she is tired, she needs to rest, she has to adapt to a new life, she has no time for doctors, procedures, etc. ...
...
Significant changes are taking place in a woman's body, and they are a big burden on the body. Therefore, if in the very first postpartum week you gently and correctly “intervene” in the restructuring process, then the postpartum period will be much easier. You have to listen to your body and prioritize correctly. nine0003
“In my opinion, recovery after childbirth should be started as early as possible - in the very first days after the hospital,” says obstetrician-gynecologist and hirudotherapist Nina Alexandrovna Antonova. – A woman experiences this restructuring not only at the physiological level, she lives through it very emotionally. In Israel, studies were conducted: mothers asked the same questions - immediately after childbirth and 20 years later. The only question, the answer to which has not changed over the years, sounded like this - “what day in motherhood do they consider the most difficult?”. All mothers both times answered so - this is "the day of return from the hospital. " To overcome the many stressful situations of postpartum life, we will show you what is going on and which specialists can be helpful. nine0003
" To overcome the many stressful situations of postpartum life, we will show you what is going on and which specialists can be helpful. nine0003
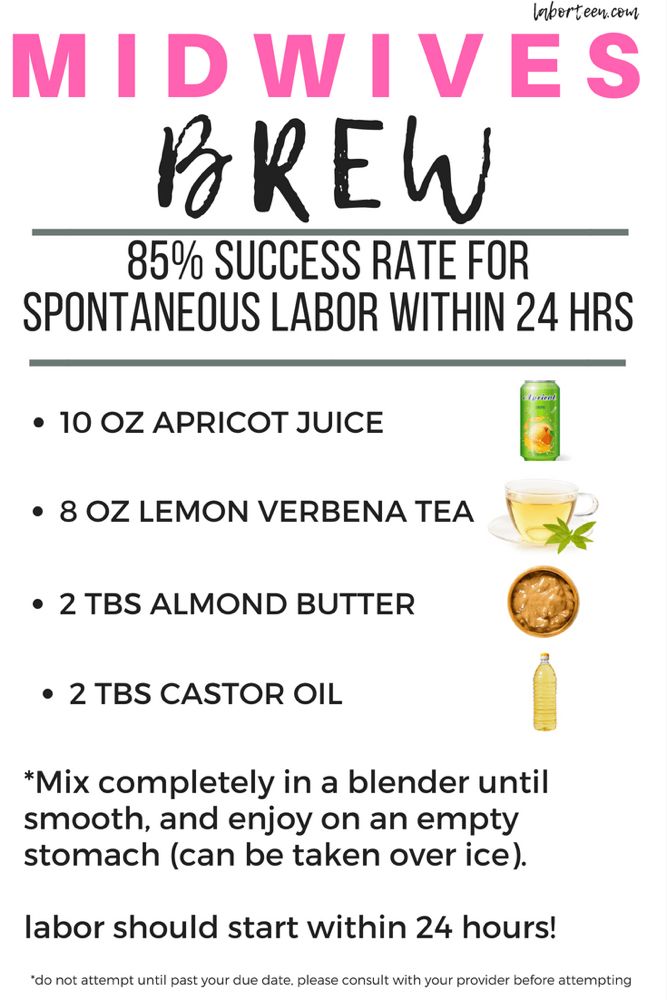
1. The uterus shrinks and returns to its original size, its mucous membrane is restored (after childbirth, the uterus weighs 1000 grams, and after 6-8 weeks - 50-60 grams). For successful contraction of the uterus, it is very important to attach the newborn to the breast within the first hour after birth, and frequent feedings after (once every 2 hours during the day, and a little less often at night). Breastfeeding stimulates the production of oxytocin, which helps the uterus contract, which, by the way, a mother can even feel during feedings - when sensations resembling contractions appear in the lower abdomen. Herbal preparations of shepherd's purse, nettle, yarrow or birch leaves can also help reduce the size of the uterus. Until it has decreased, one must be very careful with physical activity, exercises - not all of them will benefit.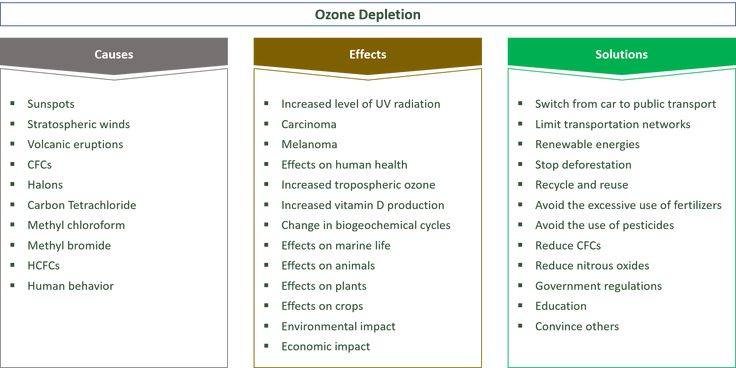 Do not strive to regain your former harmony in the very first postpartum weeks - now you and your body have completely different tasks. nine0003
Do not strive to regain your former harmony in the very first postpartum weeks - now you and your body have completely different tasks. nine0003
Who can I contact?
- The gynecologist (in the first month) will check the contraction of the uterus, see if there are any blood clots left, possibly an ultrasound.
- A hirudotherapist will also help to speed up the healing of injured soft tissues, reduce edema, and raise the general (and local) immunity of the mother
2. Due to hormonal changes, ligaments change their elasticity after childbirth, so bones and joints become less mobile. After them, the internal organs, which were displaced due to the large size of the uterus (stomach, lungs, intestines, bladder, etc.), take their former position. All these changes can be accompanied by pain, and in the future, pathological fixation may occur, leading to a constant feeling of discomfort, for example, in the back. nine0003
Who can I contact?
Osteopathic appointment is useful for any woman after childbirth for full recovery and lactation, we especially recommend visiting him if there was a long or rapid labor, if a large child was born, there were gaps in labor or pain persists, there is pain in the sacrum.
An osteopath will also help a mother with lactostasis (and a newborn - with an inability to properly grasp the nipple when sucking). nine0003
3. There are changes in the endocrine system: the work of hormones is now aimed primarily at ensuring breastfeeding. But it often happens that by the end of the first week milk does not come in sufficient quantities. Or disappears in a month at all (the so-called lactation crises, which not everyone manages to survive). Or, on the contrary, there is so much of it that mastopathy threatens.
Who can I contact?
Breastfeeding consultant will help to improve lactation, tell you how to stimulate milk production, teach you how to put the baby to the breast so that there are no cracks on the nipples, that is, help organize feeding in such a way that it would bring joy and satisfaction to mother and baby. The psychologist will consult on the main psychological aspects of the postpartum period, breastfeeding, the first year of your child's life, and the features of relations with your spouse after childbirth. nine0003
nine0003
4. Mom's emotional state changes: postpartum euphoria can be replaced by irritability or unreasonable sadness, indifference or, on the contrary, impulsiveness. If a mother cries or regrets something on the first day after birth, then, according to perinatal psychologists, this may be a manifestation of postpartum depression. Emotions during this period have a great influence on the process of postpartum recovery - help him or, conversely, slow him down.
Who can I contact? nine0018
A homeopath will help you balance your emotional mood and harmonize your general state. The psychologist will tell you what's new with the body, with the mother's psyche, what tasks are relevant at this stage. What needs to be done to prevent postpartum depression, where, in what or "in whom" to look for resources for recovery. And if depression does come, it will help to cope with your condition and return to a full life.
Meetings with specialists or lectures on children's issues will help you switch to solving new pressing issues: how to organize a daily routine, how to learn how to relax, how to travel with a baby, as well as solve a number of "pediatric" problems (from vaccinations to hardening or treatment non-drug means - for example, our "School of moms and dads"). Although an active social life is recommended no earlier than 3 months after giving birth, when you can easily leave the house with your baby using a sling. nine0003
Although an active social life is recommended no earlier than 3 months after giving birth, when you can easily leave the house with your baby using a sling. nine0003
You can use various types of assistance - both classical medical, psychological and organizational, and turn to more ancient methods of treatment leading to general recovery. Now you can choose and, most importantly, do it consciously!
Ten tips on how to recover after childbirth
During pregnancy and childbirth, your body has undergone great changes. With your new lifestyle, remember to take the time to take care of yourself as well. East-Tallinn Central Hospital physiotherapist Triin Ershov, who specializes in childbirth recovery, gives advice on how to support your body. nine0018
After childbirth, the mother's attention is usually focused on the newborn, and she forgets about herself. However, at this time it is very important to give the body a rest and follow the ergonomics of everyday life so that the body can recover normally.
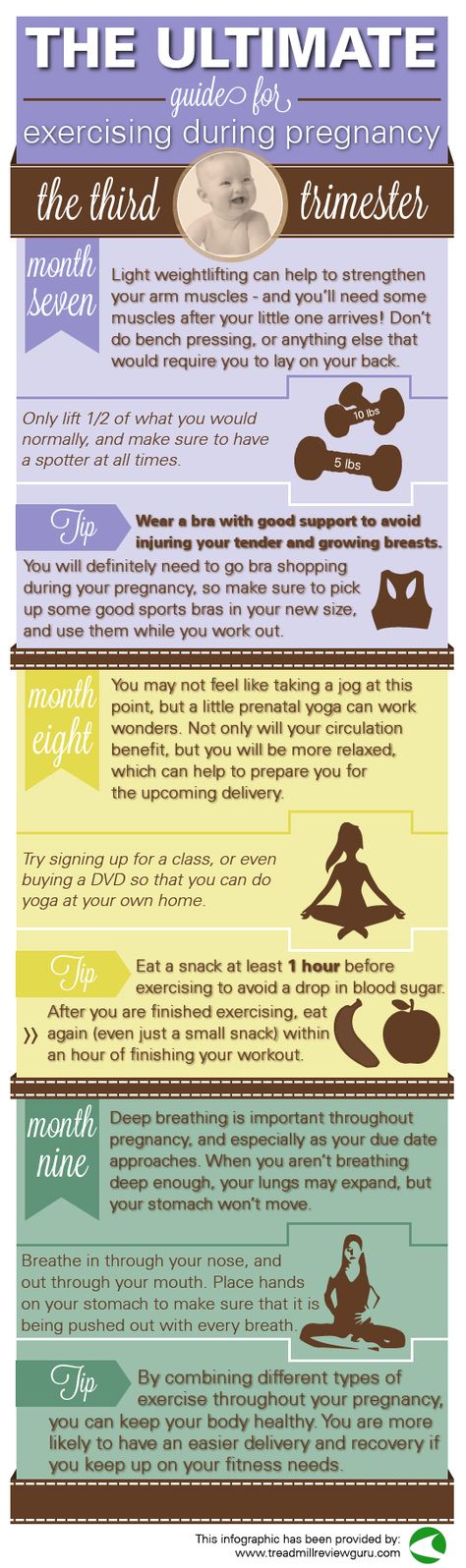
The body's natural recovery time after childbirth is six to eight weeks. During this period, it is not recommended to start training, as the muscles are not yet ready for this. However, you can gradually begin to restore the muscles of the pelvic floor and abdomen, as well as take short walks. It is important to listen to your body and give it enough rest. nine0003
- Get out of bed and lie down through the side lying position.
To turn over in bed, bend your legs one at a time while lying on your back while supporting your stomach with your hands. Rotate your shoulders, hips, and knees to the side at the same time to avoid twisting your body.
When lying down in bed, sit on the edge of the bed and place both hands on the edge of the bed. Slowly lie on your back, leaning on your forearm and then on your shoulder. Raise both legs up on the bed and turn your entire body to the side. nine0003
To get out of bed, bend your knees while lying on your back and then roll over onto your side. Leaning on your forearm, and then on your hand, simultaneously lower your legs down over the edge of the bed.
Leaning on your forearm, and then on your hand, simultaneously lower your legs down over the edge of the bed.
- Always change positions when carrying a child
Carrying a child is often carried with one hand, which overloads the muscles of one half of the body. When carrying a child, constantly alternate sides of the body and position. For spitting up, put the baby on one shoulder, then on the other. Wash the child under the tap alternately with the right and left hand. nine0003
Lift your child in an ergonomic way. (Julia-Maria Linna)
- When lifting a child, do not forget about ergonomics
For the first few months after giving birth, avoid heavy lifting and do not lift anything heavier than your baby! For the first three weeks, you should not lift the child with the cradle chair, so as not to create a load on the muscles of the abdomen and pelvic floor. When lifting the child, keep him close to the body, and the back is straight (lift with the help of the legs).
- Changing table must be at the level of the pelvis
When changing diapers in bed, kneel down. (Julia-Maria Linna)
To give your back muscles a rest, avoid activities that require you to sit in a reclining position for a long time. When bathing a baby, set the bathtub at a suitable height. Make sure the top of the changing table is at the level of the pelvis. When changing diapers on a low table or in bed, kneel down instead.
- Give your body a rest!
Especially in the first three weeks, the baby should be fed lying on its side - this way you will rest yourself and give rest to the muscles. If it is still impossible to sit due to perineal tears, it is better to rest lying down. At first, during the child’s sleep, it is better, if possible, to take a nap too - so the body can calmly recover.
- Rest in various positions
If you are lying on your back, place a pillow under your knees to help relax your back muscles. nine0003
nine0003
If you are lying on your side, place a pillow between your knees to relax your back muscles. During breastfeeding, you can lie next to the baby on your side.
When feeding in a seated position, place pillows under the lower back and the baby. (Julia-Maria Linna)
Place a pillow under your lower back when feeding in a sitting position. Place pillows under your baby while breastfeeding so he is at chest level so you don't have to lean forward and your baby can suckle more comfortably. nine0003
- Drink plenty of fluids
To restore bladder function, drink at least two to three liters of fluid a day and go to the bathroom every two to three hours. This will help prevent overstretching of the bladder, as the bladder may fill faster after pregnancy. Restoring normal bladder sensation may take time. Sitting on the toilet, rest your feet on the floor - so the muscles of the pelvic floor will relax better. nine0003
- Watch your diet
To restore bowel function, go to the toilet when you have a strong urge.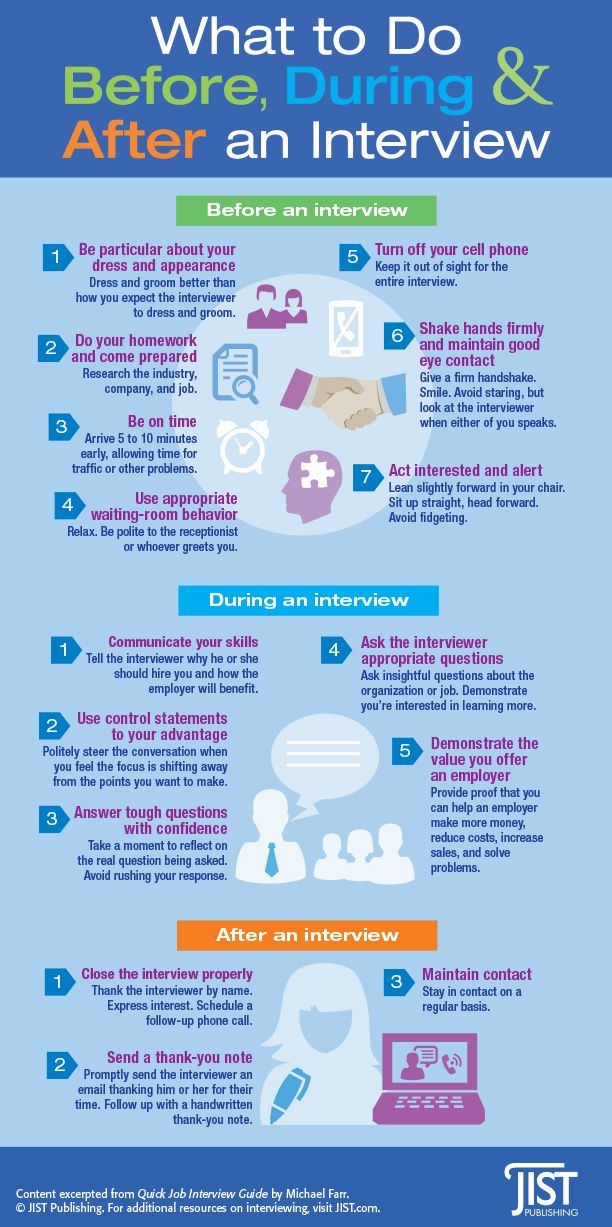 In no case should you postpone going to the toilet. Eat fresh fruits and vegetables, avoid processed foods. Avoid constipation and strong pressure on the pelvic floor. Sitting on the toilet, rest your feet on a small stool, and place your hands or forearms on your hips and relax your abdominal muscles.
In no case should you postpone going to the toilet. Eat fresh fruits and vegetables, avoid processed foods. Avoid constipation and strong pressure on the pelvic floor. Sitting on the toilet, rest your feet on a small stool, and place your hands or forearms on your hips and relax your abdominal muscles.
- Support your back muscles with a brace
After childbirth, it is recommended to wear a special bandage every day for the first 6-8 weeks. The tummy support helps maintain proper posture and reduces discomfort in the abdomen and lower back. Of course, you also need to do exercises and observe ergonomics.
- Start light exercise
After giving birth, start doing pelvic floor strengthening exercises and simple hip lift exercises. Light muscle contractions improve blood circulation and reduce swelling. In resting postures, you can gently tighten your abdominal muscles and practice belly breathing.