Legs during pregnancy
Aching, Painful, Or Heavy Legs During Pregnancy
Having aching legs during pregnancy is the icing on the cake of all of your physical ailments. But contrary to cake, heavy or aching legs are not something to be desired. While things like morning sickness and fatigue can be expected, when leg pain hits, it might catch you off guard.
To help make your leg troubles a little more bearable, we’ll give you some basic information and help you identify the signs, causes, and treatments for your aching and heavy legs.
Blood Circulation And Heavy Or Aching Legs During Pregnancy
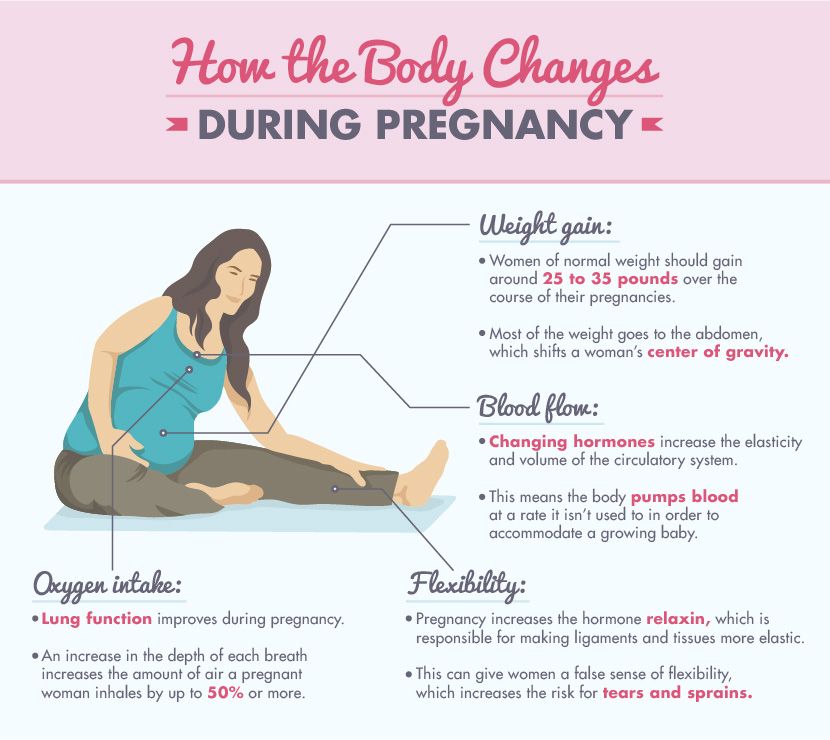
Pregnancy is a period during which the risk of circulatory disruptions becomes particularly high. These disruptions are the consequence of the related increase in body weight and hormonal changes, as seen below:
- As early as the first trimester, the increase in hormones creates circumstances in which the blood in the veins can easily stagnate, weakening vein walls and the firmness of blood vessels.
Estrogen levels can lead to inflammation (edema), and progesterone modifies the vein walls and vessel dilation.
- Throughout pregnancy, the increased volume of the uterus leads to increased pressure on the main vein responsible for returning blood to the heart.
- Finally, an increase in blood weight and volume (of 20% to 30%) contributes to increased pressure on the leg veins, which is doubled or tripled. The valves are separated further from each other by distension of the veins and no longer play their role of impeding blood return.
Blood circulation in the leg veins can be considerably disrupted. The symptoms vary significantly from woman to woman and pregnancy to pregnancy, ranging from simple discomfort to disabling pain.
After delivery, these impairments most often go away on their own within a few weeks.
The Role Of Veins And Vascular Insufficiency
In their normal state, arteries supply the body’s tissues and organs with essential substances for their healthy functioning, such as oxygen. Veins, on the other hand, return blood to the heart.
Veins, on the other hand, return blood to the heart.
Blood pressure and the firmness of vein walls allow blood to flow from the lower to the upper portion of the legs. This blood flow through the veins and back up to the heart is called venous return.
Valves, acting as small flaps, are positioned every 2 to 5 centimeters (0.8 to 2 inches) in the veins. These valves ensure that blood always flows in the same direction without ever “falling” back down the other way.
The calf muscles and compression of the instep also play a role in blood flow, particularly when walking.
Contributing Factors
Several factors can increase the risk of vascular insufficiency during pregnancy:
- Heredity: If your mom has had circulatory issues, you run a higher risk of experiencing them yourself.
- Working in a standing position and shuffling. Prolonged sitting can also disrupt venous return.
- A sedentary lifestyle and lack of physical exercise.
- Excess body weight prior to pregnancy, or significant weight gain during pregnancy.

- Previous pregnancies: The risk of venous insufficiency increases with the number of previous pregnancies carried to term — 23 percent for the first pregnancy and 31 percent for the fourth.
Healthy Habits
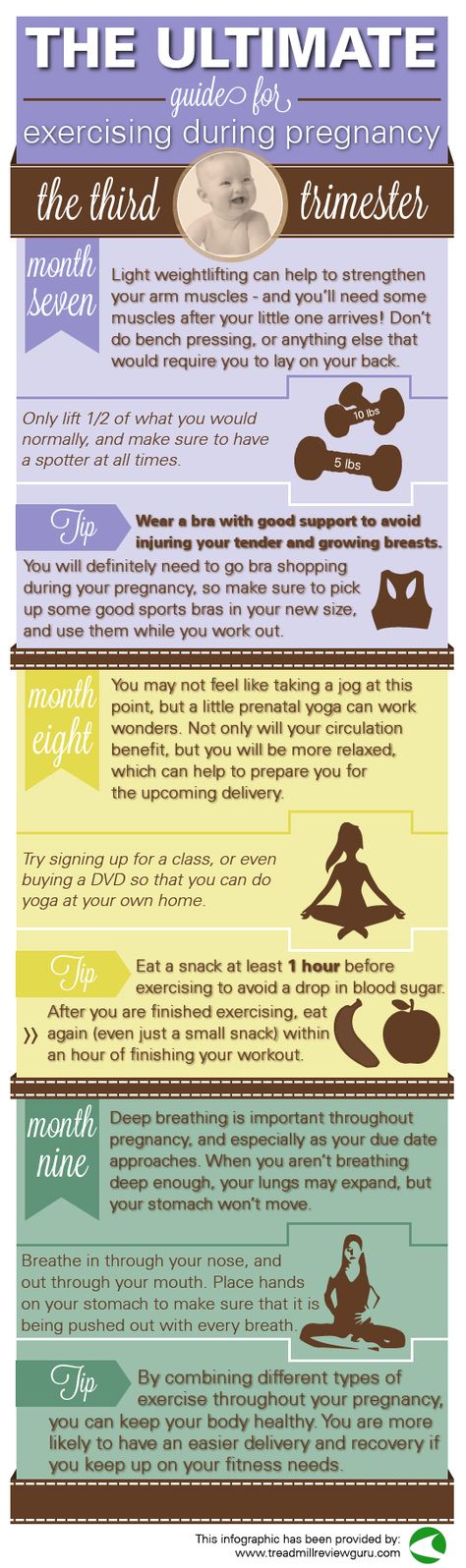
To avoid circulatory impairments during pregnancy, prevention is essential. If you need to, try to lose weight before getting pregnant and then limit your weight gain during pregnancy.
Here are some other healthy habits to help you avoid vascular insufficiency:
- Take walks or do light exercise, which boosts blood flow
- Wear shoes with a small heel that is neither too high nor too flat (3 to 4 cm or 1 to 1.5 inches)
- Avoid tight-fitting clothes and constricting socks
- If you suffer from any plantar arch problems, wear corrective insoles
- In certain cases, wearing compression stockings and taking venotonics may be recommended during pregnancy, starting in the second month
If you experience the sensation of heavy legs despite these measures, try some of these tips to help ease the discomfort:
- Raise your feet from the foot of your bed
- At the end of each shower, spray cold water over your legs in an upward motion from the ankles to the thighs
- Avoid sources of heat (prolonged exposure to the sun, high-temperature baths, underfloor heating, etc.
 )
) - Massage your legs every day, from the ankles to the knees, using a specific treatment cream to increase blood return and stimulate blood flow
Signs Of Heavy Or Aching Legs
Aching or heavy legs first appear as a sensation of discomfort, fatigue, and heaviness in the legs. These sensations can be the first sign of an actual circulation impairment alongside other characteristics, such as having pain:
- In the interior and posterior area of the calf that radiates up the leg toward the inside of the knee
- Most often felt towards the end of the day
- If you remain standing for a long time or if you are in contact with heat (summer temperatures, hot baths, hot-wax treatments, etc.)
- Increase as the pregnancy progresses
- Relieved by cold temperatures, winter climates, rest, elevation of the legs, and walking
- Accompanied by cramps at night, restlessness of the legs (painful discomfort that requires that one move one’s legs for relief), inflammation (edema of the ankles), varicosities, and even varicose veins
If you are experiencing any of these symptoms, talk about it with your doctor at your next visit. Your doctor may be able to prescribe a suitable treatment for you.
Your doctor may be able to prescribe a suitable treatment for you.
Causes Of Aching Or Heavy Legs
Like most expecting moms, you’re probably wondering what’s causing your aching or heavy legs. The sensation of heavy or aching legs is related to a loss of firmness and elasticity of the vein walls, which causes a slowing of blood circulation in the veins. Because of this, the veins dilate and blood pressure increases.
Valves — the small flaps that normally keep blood from flowing back down the leg veins — have difficulty maintaining this pressure and progressively become deficient.
Resistance to leaks weakens and blood stagnates in the lower portion of the veins, which further impairs vein walls. A vicious cycle takes hold.
On top of this, other factors could be causing your aching legs, such as:
- Nerve pressure: When your uterus expands, it puts pressure on certain nerves, which can trigger spasms and cause pain in your legs.
- Dehydration: If your body doesn’t get the right amount of hydration during your pregnancy — and it needs a lot! — it can really suffer.
 Whether you’re dealing with morning sickness, stress, or cramps, drinking water can be the easy answer to all your pregnancy woes. When in doubt, take the water route!
Whether you’re dealing with morning sickness, stress, or cramps, drinking water can be the easy answer to all your pregnancy woes. When in doubt, take the water route! - Increase in your weight: Your legs are carrying around more weight than they’re used to. They’re having to work a little harder each day, so at the end of the day, they’re tired just like you.
- Swelling: Swelling is no stranger to pregnancy, especially in the heat. When your ankles and feet start to swell in the heat, as we’ve mentioned above, circulation gets restricted. This is when your legs start to ache and get heavy. (Note: If you notice consistent swelling in your legs and feet, or your leg starts to feel warm, reach out to your obstetrician right away.)
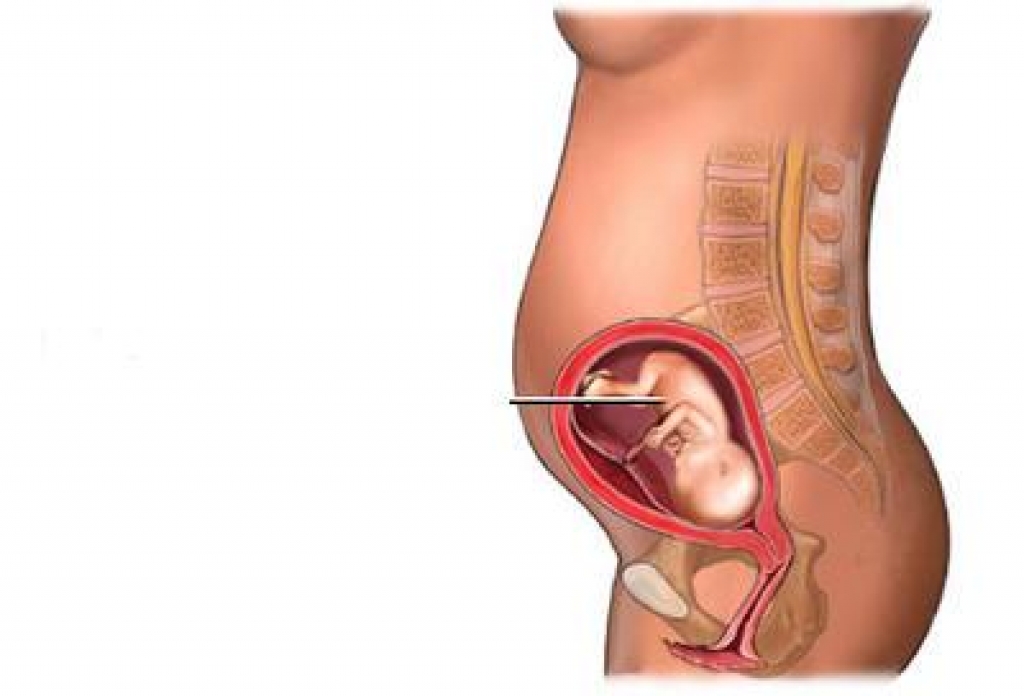
- Changes in your posture as your baby grows: Throughout stages of your pregnancy, your baby has taken different positions inside your uterus. This can take a toll on your body, especially your back.
 Your posture starts to change throughout your pregnancy without you even noticing at times, but your legs are sure to take notice of the change. Your legs have to support you throughout these different stages, and it can impact them.
Your posture starts to change throughout your pregnancy without you even noticing at times, but your legs are sure to take notice of the change. Your legs have to support you throughout these different stages, and it can impact them. - Fluid retention: Your growing uterus puts pressure on the veins that carry blood back from your lower body, which partially blocks blood flow. As a result, fluid remains in your legs and feet.
- Joint laxity: As we’ve discussed, when you’re carrying the extra weight from your precious baby, it’s a lot for your legs — but it’s also a lot for your joints. Your joints can easily become stressed from the added pressure. Your joints may seem a little loose and you might even waddle when you walk!
At-Home Treatment
Most often, your leg aches can be relieved at home. That’s something to shout about because we know leg aches can really be a Debby Downer as you wrap up your day!
Here are a few ideas to relieve your leg aches and heavy legs at the end of the day:
- Stretch your calf muscles by flexing and releasing each foot a few times
- Take short walks throughout the day to boost blood flow
- Avoid standing or sitting with your legs crossed for long periods
- Take a warm bath before bed (After getting out of a relaxing bath, don’t forget to apply Stretch Marks Oil to help limit the appearance of stretch marks! It leaves your skin restored, refreshed, and noticeably smoother.
 )
) - Massage your legs throughout the day and especially before bed (Try using our Body Firming Gel to give your legs a little massage. It hydrates your skin, giving it a firmer look and overall feel.)
- Take a calcium supplement (with the go-ahead from your doctor)
- Drink a glass of milk before bed
- Prop your legs up on a pillow (make sure your legs are elevated above your heart)
- Wear compression leggings or socks
- Increase your potassium intake
Medical Treatment
If your legs are painful and you see no improvement after trying the recommended measures outlined in the previous section, do not hesitate to see a doctor. They can prescribe suitable treatment for your condition.
Various methods — from medicinal to physical to surgical — may be considered, depending on the severity of your circulatory impairments:
- Compression via pantyhose, stockings, or socks is the basic treatment for anyone experiencing venous insufficiency.
 Different models are available depending on the strength of compression necessary. Significant progress has been made in improving the esthetics of these garments. The cost of some of these compression methods may be eligible for Social Security reimbursement.
Different models are available depending on the strength of compression necessary. Significant progress has been made in improving the esthetics of these garments. The cost of some of these compression methods may be eligible for Social Security reimbursement. - Venotonics have anti-inflammatory properties, stimulating muscle tone and protecting the elasticity of the vein walls. They must be taken for an extended period of time in order to be effective.
- Kinesitherapy and exercises to build up the leg muscle also have a role to play. Walking, swimming and biking are the best types of activity. Spa treatments, massages, and manual lymphatic drainage can also provide valuable relief.
- If varicose veins developed during your pregnancy and are still present after delivery, vein sclerotherapy or surgery may be considered. These techniques can be performed under local anesthesia, requiring neither an epidural nor general anesthesia, and the patient can go home the same day as treatment, or the following day.

A Comfortable Pregnancy
Aching and heavy legs can be caused by a variety of factors, as we listed above. Although these unpleasant sensations usually disappear on their own after delivery, they should not be taken lightly.
Heavy legs can turn into vascular pathologies that can sometimes be disabling. Monitor your heavy legs closely and give them the appropriate care from the very first signs to limit the risk of complications.
But keep in mind that most often, it’s not a cause for concern or harmful to your baby. Use at-home treatments to ease your leg aches and heavy legs. You may have to try a few before you find what works for you.
And while you’re at it, continue taking care of yourself during your pregnancy by treating your skin. Using the right products that have been clinically proven to effectively help expecting mothers, like our Stretch Marks Cream, will make for one comfortable pregnancy!
5 ways to manage swollen legs and feet during pregnancy | Your Pregnancy Matters
×
What can we help you find?Refine your search: Find a Doctor Search Conditions & Treatments Find a Location
Appointment New Patient Appointment
or Call214-645-8300
MedBlog
Your Pregnancy Matters
September 14, 2021
Your Pregnancy Matters
Robyn Horsager-Boehrer, M. D. Obstetrics and Gynecology
D. Obstetrics and Gynecology
Of all the body parts you expect to get bigger during pregnancy, feet might not be at the top of your list. But most pregnant women experience swelling in their lower legs and feet.
If your ankles appear puffy and your shoes don’t feel quite right, you’re not imagining things. The additional fluid and blood your body creates to support healthy fetal growth also slows down blood circulation. That can cause blood to accumulate in your lower extremities, causing swelling.
During pregnancy, you also produce more relaxin, a hormone that helps your tendons, ligaments, joints, and muscles – you guessed it – relax. While relaxin helps your pelvis open to give birth, it also loosens the tendons and ligaments in your feet.
While relaxin helps your pelvis open to give birth, it also loosens the tendons and ligaments in your feet.
The combination of extra weight and hormones during pregnancy can cause your feet not only to widen but also flatten and lengthen. Leg or ankle swelling likely will decrease a week or two after your baby is born, but your feet may never be the same again.
Studies have shown that pregnancy can cause a permanent decrease in your arch and increase in foot length – typically only after a woman’s first pregnancy.
While more research is needed to determine whether these structural changes can be prevented, there are a few things you can do throughout your pregnancy to reduce swelling and feel more comfortable.
Coping with swollen legs and feet during pregnancy
1. Wear compression socks
Wearing 15-20mmHG compression socks that end at your knee can help alleviate achiness. The socks gradually increase pressure in your legs and move some of the excess fluid back into your blood vessels and the rest of your body.
Avoid socks with a tight band at the top. The tightness might worsen swelling by blocking blood return. That can increase your risk of developing a blood clot – which is already five times higher during pregnancy. You don’t need to purchase medical-grade socks, but you can find a good pair of compression socks for $10-$20.
Compression socks also can prevent the formation of new varicose veins, which occur in 15% of pregnant women for the same reason that causes swelling. The risk doubles after your first pregnancy and is four times higher in women over 35. These veins start out as little bumps under your skin; the socks squeeze them just enough to prevent backward blood flow and bulging. Existing varicose veins aren’t likely to shrink, but compression socks can reduce the pain and discomfort they cause.
2. Rest efficiently
You can easily improve blood circulation during downtime and sleep:
- Elevate your legs above heart level while reading, watching TV, or doing other seated activities.
 The simple change in body position decreases pressure on your veins, which no longer have to work against gravity to send blood to your heart. Use cushions for comfort and elevate in 15- to 20-minute intervals a few times a day.
The simple change in body position decreases pressure on your veins, which no longer have to work against gravity to send blood to your heart. Use cushions for comfort and elevate in 15- to 20-minute intervals a few times a day. - Sleep on your left side. While you can safely sleep on either side during pregnancy, the left side is often recommended to avoid putting pressure on the inferior vena cava, a large vein that carries blood from your lower extremities to your heart.
3. Get your feet wet
Immersing your feet and ankles in cool water for 20 minutes a few times a week can minimize swelling, whether you use a pool, bathtub, or even a large bowl. Bonus: It’s also a great way to deal with the Texas heat if you’re pregnant during the summer.
Be sure the water temperature is moderate and not ice cold. Cooler temperatures cause the smaller blood vessels close to your skin to constrict, which reduces blood flow to and swelling within the affected area. Water that is too cold can have the opposite effect. Whether you stand and sway or sit and dangle your feet, water therapy is a great way to relieve stress and pain.
Water that is too cold can have the opposite effect. Whether you stand and sway or sit and dangle your feet, water therapy is a great way to relieve stress and pain.
Related reading: Water immersion during labor
4. Invest in supportive shoes that fit.
Unsupportive and uncomfortable shoes can cause even more leg and foot pain, plus backaches. Even if your feet return to their pre-pregnancy size, you’ll feel more comfortable in shoes that fit your feet and support your additional body weight. The American College of Obstetricians and Gynecologists recommends wearing shoes that:
- Have a low heel but are not flat
- Provide good arch support, such as athletic shoes
Many patients prefer shoes that have mesh, which allow their feet to breathe, and can easily slip on and off to limit bending over while pregnant. More shoe brands are merging comfort and style, so even the most fashionable patients will have no problem finding footwear they feel good about wearing.
5. Visit a podiatrist or pedicurist.
Another reason to wear shoes that fit: Stress from tight shoes can cause ingrown toenails, and so can infrequent nail trimming. In the first two trimesters you probably won’t have any difficulty trimming your toenails. But once you reach the third trimester, it might get more challenging.
Try propping up your feet on a stool or ask your partner to help trim your toenails. Nail salon gift cards are a great item to add to your baby shower (or sprinkle!) registry, too.
Seeing a podiatrist is another option to prevent or treat painful foot conditions, such as ingrown toenail, bunions, or plantar warts.
When swelling becomes serious
While gradual swelling in your lower and upper extremities is normal, sudden or severe swelling in your face, hands, or feet might be a symptom of preeclampsia. This pregnancy complication involves very high blood pressure.
If you have preeclampsia, you may need to stay in the hospital until you give birth. Delivery is the only way to “treat” preeclampsia. Left untreated, the condition can cause seizures, kidney or liver damage, and in rare cases, death.
Delivery is the only way to “treat” preeclampsia. Left untreated, the condition can cause seizures, kidney or liver damage, and in rare cases, death.
Related reading: Postpartum hypertension: When a new mom's blood pressure is too high
Talk with your doctor about foot and leg swelling, as well as any other pregnancy symptoms. The more we know about your current condition, the more we can help reduce your risk of future complications.
While we can’t fully prevent foot and leg swelling, we can recommend ways to reduce your risk, such as:
- Regular exercise
- Good-quality sleep
- A healthy diet rich in fruits and vegetables
Discomfort during pregnancy is to be expected, but our goal is to partner with you to minimize it – as well as the risk of more serious conditions.
To discuss your pregnancy concerns or symptoms with an expert, call 214-645-8300 or request an appointment online.
More in: Your Pregnancy Matters
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
January 10, 2023
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
December 20, 2022
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
December 13, 2022
Pediatrics; Your Pregnancy Matters
- Jessica Morse, M.
 D.
D.
December 6, 2022
Your Pregnancy Matters
- Shivani Patel, M.D.
November 22, 2022
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
November 15, 2022
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
November 7, 2022
Mental Health; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
October 11, 2022
Prevention; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
October 4, 2022
More Articles
Edema during pregnancy
Edema during pregnancy- Phlebology Center >
- Pregnancy and varicose veins >
- Edema during pregnancy
Article content:
- Pregnancy and edema
- Why does swelling appear during pregnancy?
- When does edema occur during pregnancy?
- What factors can affect the appearance of edema during pregnancy
nine0003 What can be done to get rid of edema during pregnancy?- Questions from patients about edema and pregnancy
Pregnancy and Edema
Swelling during pregnancy is normal because the body produces approximately 50% more blood and body fluids to meet the needs of a developing baby.
Edema during pregnancy
Edema during pregnancy occurs on the hands, face, legs, ankles and feet. nine0014
Why does swelling occur during pregnancy?
This extra fluid retention is needed to soften the body, allowing it to expand as the baby develops. The extra fluid also helps prepare the pelvic joints and tissues for reopening for childbirth. Additional fluids make up approximately 25% of a woman's weight gain during pregnancy.
When does swelling occur during pregnancy?
Swelling can appear at any stage of pregnancy, but it usually starts around the fifth month and may worsen while you are in the third trimester.
What factors can affect the appearance of edema during pregnancy
The following factors can also affect edema during pregnancy:
- Varicose disease
- Summer heat
- Standing for a long time nine0003 Prolonged physical activity
- Low potassium diet
- High caffeine intake
- High sodium intake
Moderate swelling occurs during normal pregnancy, however, if you feel a sudden swelling of the hands and face, this may be a sign of preeclampsia.
Pregnancy and thrombosis
Severe swelling of the distal lower extremities may be due to thrombosis. In these cases of sudden swelling, it is important to see a doctor immediately. nine0014
What can I do to get rid of swelling during pregnancy?
Swelling during pregnancy can be reduced by eating high potassium foods such as bananas, dried apricots, prunes and by limiting caffeine.
Here are some more helpful tips for managing swelling during pregnancy:
- Avoid prolonged standing.
- Minimize your time outside in hot weather. nine0003 Rest with your legs elevated.
- Wear comfortable shoes, avoiding high heels if possible.
- Wear special compression stockings or stockings.
Pregnancy Compression Stockings
- Avoid clothing that is tight around your wrists or ankles.
- Relax or take a dip in the pool.
- Use cold compresses on swollen areas.

- Drink water that stimulates the kidneys and helps reduce water retention. nine0004
- Minimize sodium (salt) intake and avoid adding salt to food.
Pregnancy Swelling Prevention
These simple guidelines will help reduce swelling during pregnancy and make this period more comfortable and safe.
Questions from patients about edema and pregnancy
What to do with swelling of the legs during pregnancy?
Edema during pregnancy is most often a physiological phenomenon, but often a sign of serious clinical situations. It is important to tell your doctor, a gynecologist, about the edema that bothers you. It makes sense to consult a phlebologist in order to exclude the pathology of the veins of the lower extremities. nine0014
How to deal with swelling during pregnancy?
Combating edema during pregnancy will help adhere to a certain regimen, indicated above. It is also necessary to follow the recommendations of your obstetrician-gynecologist and phlebologist.
It is also necessary to follow the recommendations of your obstetrician-gynecologist and phlebologist.
Can swelling be avoided during pregnancy?
It is almost impossible to completely avoid swelling during pregnancy. You should pay attention to the regimen and follow the recommendations of your doctor. Also, it is useful to pay attention to the dynamics of edema, its symmetry. If in doubt, voice them to the doctor. nine0014
Which doctor should I go to if swelling occurs during pregnancy?
If edema occurs during pregnancy, you need to contact an obstetrician-gynecologist, as well as a phlebologist.
Are swelling during pregnancy dangerous?
Physiological swelling is inevitable during pregnancy. However, swelling should be kept under control and if in doubt seek medical attention.
Pregnancy and your feet article on the website of the Preobrazhenskaya Clinic
Pregnancy causes many different changes in a woman's body. Many women during pregnancy present the same complaints.
Many women during pregnancy present the same complaints.
One of these complaints, which is practically not taken into account, is the complaint of pain in the legs.
Due to the natural weight gain during pregnancy, the body's center of gravity shifts forward. This causes a redistribution of the load on the limbs and an increase in pressure in the knee joints and feet.
Pregnant women have two main problems, they are overpronation of the foot and swelling of the legs. nine0014
These changes can cause pain in the heels, arch, or metatarsus. Many women experience leg cramps and varicose veins. Therefore, all pregnant women need to have the necessary information about their health and, in particular, about the function of the legs, so that the nine-month pregnancy period is more comfortable for them.
Reason:
Excessive stress on the feet and swelling of the legs are the most common problems during pregnancy.
Overload occurs because the arch of the foot flattens under the weight.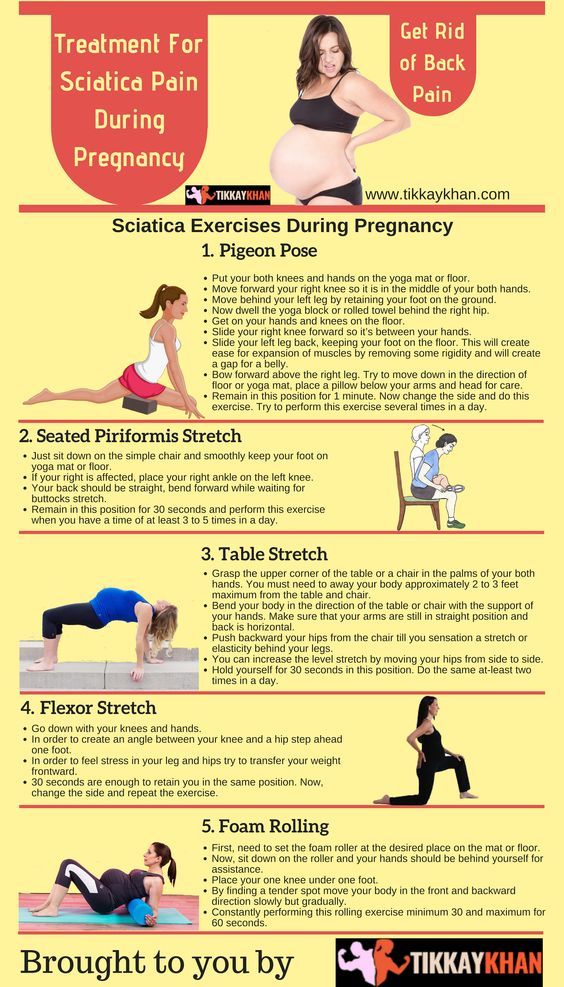 This can cause congestion and inflammation of the plantar fascia that runs from the heel to the toes. nine0014
This can cause congestion and inflammation of the plantar fascia that runs from the heel to the toes. nine0014
Excessive stress on the feet can make walking painful due to increased stress on the legs, calves and spine.
Edema, or swelling of the legs, usually occurs in the second half of pregnancy.
Edema is caused by obstruction of the outflow of blood due to the pressure of the enlarging uterus on the veins of the lower extremities. In a woman's body, the total volume of fluid in the body remains the same as before pregnancy, but its distribution changes. Swollen legs become bluish. nine0014
During pregnancy, an extra volume of fluid accumulates in the body, which contributes to an increase in edema.
If the hands or face swell, the pregnant woman should immediately consult a doctor.
Treatment
There are effective ways to deal with deformity and swelling of the feet during pregnancy.
Foot deformities can be treated with ready-made orthotics . These orthotics must have sufficient arch and hindfoot support. It remains important to choose the right footwear. A pregnant woman should choose comfortable shoes with proper foot support and cushioning. nine0014
These orthotics must have sufficient arch and hindfoot support. It remains important to choose the right footwear. A pregnant woman should choose comfortable shoes with proper foot support and cushioning. nine0014
Foot deformity should be treated not only to relieve pain, but also to avoid complications such as plantar fasciitis, heel spurs, inflammation of the posterior tibial muscle, or deformity of the toes.
Pregnant women can be given the following advice:
- Raise your legs as often as possible. If you have to stay in a sitting position for a long time, set up a small stool and place your feet on it. nine0003 Wear rational footwear. Too narrow and short shoes impede blood flow in the lower extremities.
- Measure the circumference of the lower leg and thigh, as well as the size of the foot, several times during pregnancy. These numbers are subject to change.
- Wear seamless socks that don't restrict blood flow.
- If you drive for a long time, take regular breaks to stretch your legs.