What should my newborns temp be
Fever (0-12 Months)
Is this your child's symptom?
- An abnormal high body temperature
- Fever is the only symptom. Your child has a true fever if:
- Rectal (bottom), Ear or Forehead temperature: 100.4° F (38.0° C) or higher
- Under the arm (armpit) temperature: 99° F (37.2° C) or higher
- Caution: Ear temperatures are not accurate before 6 months of age
- Caution: Forehead temperatures must be digital. Forehead strips are not accurate.
Causes of Fever
- Overview. Almost all fevers are caused by a new infection. Viruses cause 10 times more infections than bacteria. The number of germs that cause an infection are in the hundreds. Only a few common ones will be listed.
- Viral Infections. Colds, flu and other viral infections are the most common cause. Fever may be the only symptom for the first 24 hours. The start of viral symptoms (runny nose, cough, loose stools) is often delayed.
Roseola is the most extreme example. Fever may be the only symptom for 3 to 5 days. Then a rash appears.
- Bacterial Infections. A bladder infection is the most common cause of silent fever in girls.
- Vaccine Fever. Fever with most vaccines begins within 12 hours. It lasts 2 to 3 days. This is normal and harmless. It means the vaccine is working.
- Newborn Fever (Serious). Fever that occurs during the first 3 months of life can be serious. All of these babies need to be seen as soon as possible. The fever may be due to sepsis (a bloodstream infection). Bacterial infections in this age group can get worse quickly. They need rapid treatment.
- Meningitis (Very Serious). A bacterial infection of the membrane that covers the spinal cord and brain. The main symptoms are a stiff neck, headache and confusion. Younger children are lethargic or so irritable that they can't be consoled. If not treated early, can suffer brain damage.

- Overheated. The fever is usually low grade. Can occur during heat waves or from being overdressed. The temp becomes normal in a few hours after moving to a cooler place. Fever goes away quickly with rest and drinking extra fluids.
- Not Due to Teething. Research shows that "getting teeth" does not cause fevers.
Fever and Crying
- Fever on its own shouldn't cause much crying.
- Frequent crying in a child with fever is caused by pain until proven otherwise.
- Hidden causes can be ear infections, kidney infections, sore throats and meningitis.
Normal Temperature Range
- Rectal. A reading of 98.6° F (37° C) is just the average rectal temp. A normal low can be 96.8° F (36° C) in the morning. It can change to a high of 100.3° F (37.9° C) late in the day. This is a normal range.
When to Call for Fever (0-12 Months)
Call 911 Now
- Not moving
- Can't wake up
- Severe trouble breathing (struggling for each breath; can barely speak or cry)
- Purple or blood-colored spots or dots on skin
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Trouble breathing, but not severe
- Great trouble swallowing fluids or spit
- Fever in baby less than 12 weeks old.
 Caution: Do NOT give your baby any fever medicine before being seen.
Caution: Do NOT give your baby any fever medicine before being seen. - Fever over 104° F (40° C)
- Shaking chills (shivering) lasting more than 30 minutes
- Nonstop crying or cries when touched or moved
- Won't move an arm or leg normally
- Dehydration suspected. No urine in over 8 hours, dark urine, very dry mouth and no tears.
- Weak immune system. Examples are sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
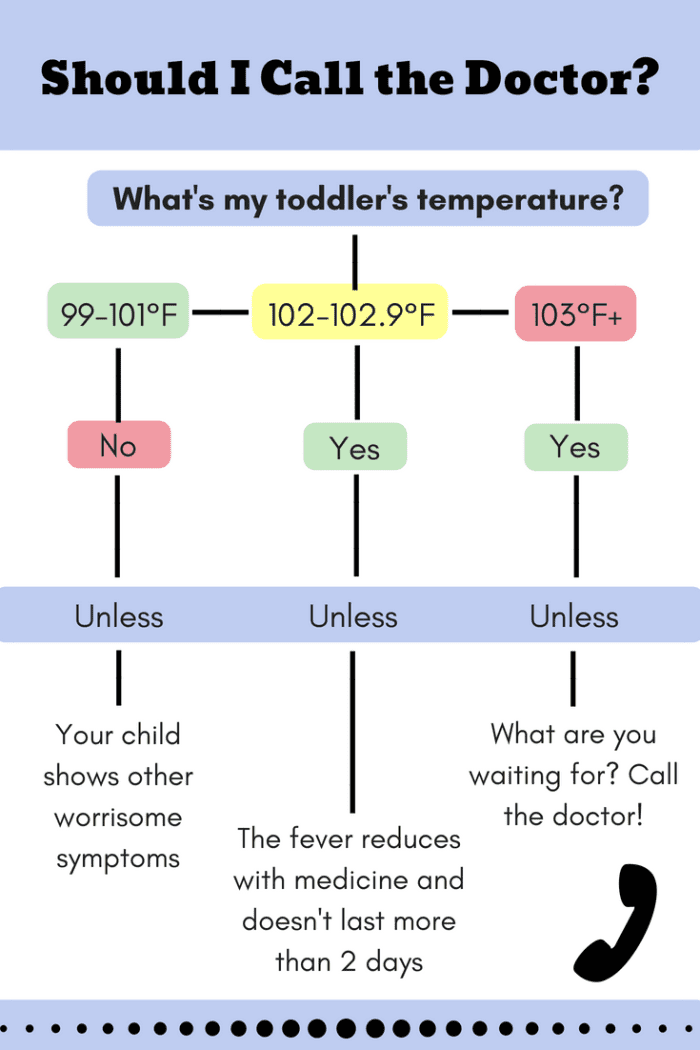
Contact Doctor Within 24 Hours
- Age 3-6 months old with fever
- Age 6-12 months old with fever that lasts more than 24 hours. There are no other symptoms (such as cough or diarrhea).
- Fever lasts more than 3 days
- Fever returns after gone for more than 24 hours
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Fever with no other symptoms and your child acts mildly ill
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Fever
- What You Should Know About Fever:
- Having a fever means your child has a new infection.
- It's most likely caused by a virus.
- You may not know the cause of the fever until other symptoms develop. This may take 24 hours.
- For infants more than 3 months old, most fevers are good for sick children. They help the body fight infection.
- Use the ranges below to help put your child's level of fever into perspective:
- 100° - 102° F (37.8° - 39° C) Low grade fever: helpful, good range. Don't treat.
- 102° - 104° F (39 - 40° C) Average fever: helpful. Treat if causes discomfort.
- Over 104° F (40° C) High fever: causes discomfort, but harmless. Always treat.
- Over 106° F (41.1° C) Very high fever: important to bring it down. Rare to go this high.
- Over 108° F (42.3° C) Dangerous fever: fever itself can be harmful.
- Treatment for All Fevers - Extra Fluids:
- Fluids alone can lower the fever. Reason: being well hydrated helps the body give off heat through the skin.
- For shivering (or the chills), give your child a blanket. Make them comfortable.
- Offer your child extra water or other fluids by mouth. Cold fluids are better. Until 6 months old, only give extra formula or breastmilk.
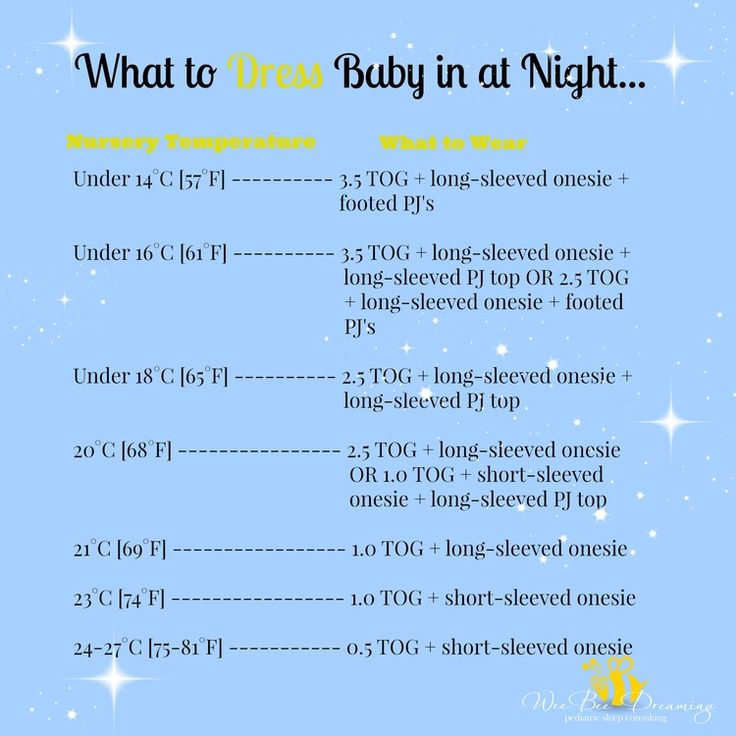
- For all children, dress in 1 layer of light weight clothing, unless shivering.
 Reason: also helps heat loss from the skin.
Reason: also helps heat loss from the skin. - For shivering (or the chills), give your child a blanket. Make them comfortable.
- Caution: if a baby under 1 year has a fever, never overdress or bundle up. Reason: Babies can get over-heated more easily than older children.
- Fever Medicine:
- Caution: Do not give a baby under 3 months any fever medicine. Most of these babies will need to be seen.
- For fevers 100°-102° F (37.8° - 39°C), fever meds are not needed. Reason: fevers in this range help the body fight the infection. Fevers turn on the body's imune system. Fevers don't cause any discomfort. Fever meds are mainly needed for fevers higher than 102° F (39° C).
- Give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil) if over 6 months old.
- Goal of treatment: keep the fever at a helpful level. Most often, the fever meds lower the fever by 2° to 3° F (1 - 1.
 5° C). They do not bring it down to normal. It takes 1 or 2 hours to see the effect.
5° C). They do not bring it down to normal. It takes 1 or 2 hours to see the effect. - Do not use aspirin. Reason: Risk of Reye syndrome, a rare but serious brain disease.
- Do not use both acetaminophen and ibuprofen together. Reason: Not needed and a risk of giving too much.
- Pain: fever does not cause pain. If your child also has pain, it's from the infection. It may be a sore throat or muscle pain. Treat the pain, if it's more than mild.
- Return to Child Care:
- Your child can return to child care after the fever is gone. Your child should feel well enough to join in normal activities.
- What to Expect:
- Most fevers with viral illnesses range between 101° and 104° F (38.4° and 40° C).
- They may last for 2 or 3 days.
- They are not harmful.
- Call Your Doctor If:
- Your child looks or acts very sick
- Any serious symptoms occur such as trouble breathing
- Fever goes above 104° F (40° C)
- Any fever occurs if less than 12 weeks old
- Fever without other symptoms lasts more than 24 hours
- Fever lasts more than 3 days (72 hours)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 11/03/2022
Last Revised: 09/18/2022
Copyright 2000-2022 Schmitt Pediatric Guidelines LLC.
How to take a newborn’s temperature
Your best bet is to use a digital thermometer. These can be bought inexpensively in any supermarket or pharmacy and can be used to take rectal (in the bottom) or axillary (in the armpit) temperature readings.
Taking a rectal temperature gives the most accurate reading of body temperature in infants and young children. However, if the thought of doing this makes you squeamish, taking an axillary temperature is the next best choice.
Be aware that temperature strips, which are placed on someone's forehead for a reading, have been found to be poor indicators of true body temperature, especially in infants and children, and should be avoided. The digital thermometer is best for temperature taking at home.
The digital thermometer is best for temperature taking at home.
Taking a rectal temperature
- Lubricate the tip of the thermometer with a lubricating jelly. Check the manufacturer's directions to see whether water-soluble jelly or petroleum jelly is recommended.
- Place your baby on a firm, flat surface such as a changing table.
- Using your hand, insert the lubricated thermometer through the anal opening, about one-half to one inch or about 1.25 to 2.5 centimeters into the rectum. Stop at less than ½ inch or about 1.25 centimeters if you feel any resistance.
- Steady the thermometer between your second and third fingers as you cup your hand against your baby's bottom. Soothe your baby and speak to him/her quietly as you hold the thermometer in place.
- Wait until you hear the appropriate number of beeps or other signal that the temperature is ready to be read. Read and record the number on the screen, noting the time of day that the reading was taken.

Taking an axillary temperature
- Remove your child's shirt and undershirt. The thermometer should touch skin only, not clothing.
- Insert the thermometer in your child's armpit. Fold your child's arm across his chest to hold the thermometer in place.
- Wait until you hear the appropriate number of beeps or other signal that the temperature is ready to be read. Read and record the number on the screen, noting the time of day that the reading was taken.
Additional tips
- Never take your baby's temperature right after a bath or if he/she has been bundled tightly for a while — this can affect the temperature reading
- Never leave a child unattended while taking his temperature
- Temperature should be taken only if the baby feels hot or is lethargic
- A baby's normal temperature range:
- Under the arm is 97.5 to 99.3 degrees Fahrenheit or 36.5 to 37.4 degrees Celsius
- Rectal is 100.2 degrees Fahrenheit or less, or 37.
 9 degrees Celsius or less
9 degrees Celsius or less
- These are the American Academy of Pediatrics recommended ranges. If you have questions or concerns, be sure to discuss them with your baby's healthcare provider
Download the printable version of this page (PDF)
"What should be the temperature of a newborn?" - Parents.ru
Health
- Photo
- Getty Images/Caiaimage
What is the normal temperature for a 10 day old baby? My son's temperature ranges from 36.7 to 37.1-37.2°C during the day. This is fine?
Daria, Moscow
neonatologist, head of the neonatal department of the maternity hospital of the Federal State Budgetary Institution "Central Clinical Clinical Hospital" of the Office of the President of the Russian Federation
The child spends 9 months in the mother's stomach, where the temperature is higher than outside. Accordingly, in the future baby, this figure exceeds the usual 36.6 ° C for us. After birth, the body begins to adapt to new conditions, so up to a year the temperature in the baby can fluctuate quite widely. The normal temperature in a newborn (the first month of life) is 36.6–37.2 ° C. Subfebrile temperature (above 37°C) is associated with very high growth rates of newborns. If the thermometer reads less than 36.6°C, your baby probably needs extra warmth. Pay attention to the temperature in the room and how the child is dressed. Maybe he needs to put on a hat, socks, cover with a blanket. If the newborn, on the contrary, overheated, screamed for a long time, or dehydration occurred, the thermometer can rise above 38 ° C. Fever is also an important symptom of infectious and inflammatory diseases. In this case, you should definitely contact your pediatrician.
Accordingly, in the future baby, this figure exceeds the usual 36.6 ° C for us. After birth, the body begins to adapt to new conditions, so up to a year the temperature in the baby can fluctuate quite widely. The normal temperature in a newborn (the first month of life) is 36.6–37.2 ° C. Subfebrile temperature (above 37°C) is associated with very high growth rates of newborns. If the thermometer reads less than 36.6°C, your baby probably needs extra warmth. Pay attention to the temperature in the room and how the child is dressed. Maybe he needs to put on a hat, socks, cover with a blanket. If the newborn, on the contrary, overheated, screamed for a long time, or dehydration occurred, the thermometer can rise above 38 ° C. Fever is also an important symptom of infectious and inflammatory diseases. In this case, you should definitely contact your pediatrician.
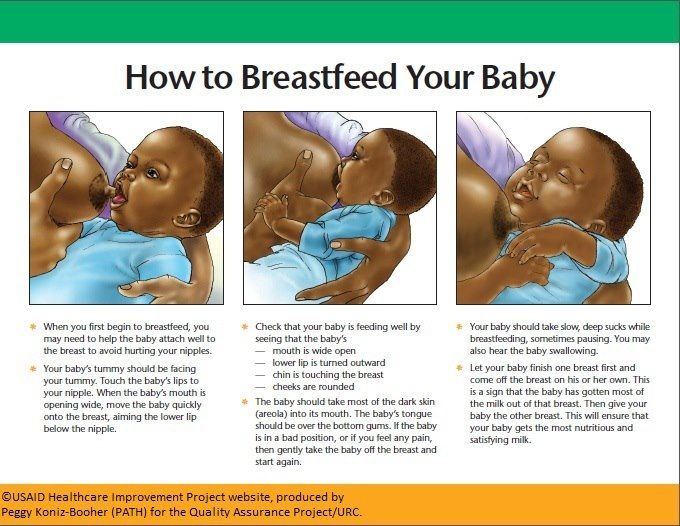
How often should a three-week-old baby be breastfed? How many night feeds do you need? My mother says that at night it is better to feed him once, and then give him water to drink if he wakes up. Otherwise, then it will be, waking up, to demand breasts.
Otherwise, then it will be, waking up, to demand breasts.
Inna, Sochi
Infants in the first month of life should be breastfed on demand. The mode is set by the child himself. Each baby is individual: someone eats 7 times a day, someone - 12. When breastfeeding, it is permissible to feed every two hours. Some children take a six-hour break once a day, most often during a night's sleep. There is no need to wake the child. Wait until he gets hungry. Then he will suckle the breast with great pleasure. Water can be offered between feedings, although breast milk for a newborn is both food and drink.
When formula-feeding, it is better to use an orthodontic nipple, the shape of which resembles the nipple of a woman's breast. She has a wide soft base, so when sucking, the lower jaw moves more actively.
There are orange spots on the diaper. The child is seven days old. The doctor said that nothing needs to be done, but I'm still worried.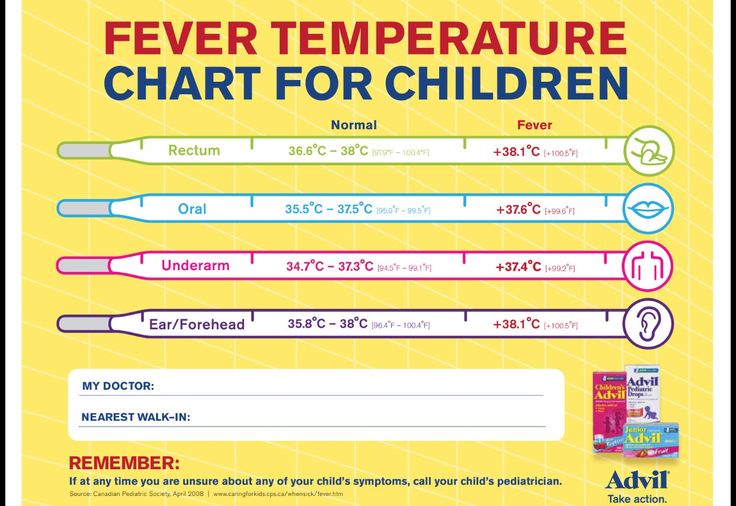
Margarita, Saratov
The first seven days of life is a period of adaptation (adaptation) to autonomous extrauterine existence. This period is characterized by transitional (transient, that is, temporary) states. These include uric acid infarction of the kidneys. It sounds scary, but there is nothing threatening the health of the baby here. Because your doctor is right: no treatment is required. The orange spots on the diaper that we see are uric acid salts that have precipitated. This phenomenon is associated with the peculiarity of metabolism in children during the first seven days of life. Usually this does not affect the well-being of the baby. By the tenth day, when the kidneys get used to the new living conditions, everything returns to normal on its own.
More useful and interesting materials about the health of newborn babies - in our channel on Yandex.Zen.
Love Coming
Tags
- Question to the pediatrician
Read
,Camilla reported Charlotte, and Megan smiled: the new facts about the funeral of Queen Elizabeth II
“The Paul of your son is a girl”: 44-year-old: 44-year-old: 44-year-old: 44-year Olga Orlova answered the question about the future child
The first official photo: the Romanov Imperial House showed the “heir to the throne”0003
Live stream and sunset funeral: 8 features of the burial of Elizabeth II
"It's like a hurricane": Meghan Markle described a typical morning with children
Temperature and humidity in the newborn room: guidelines
temperature for the newborn. It is important not to disturb the thermoregulation of the baby, not to overheat it or, on the contrary, to supercool it. We hold on to the "golden mean".
It is important not to disturb the thermoregulation of the baby, not to overheat it or, on the contrary, to supercool it. We hold on to the "golden mean".
Contents (click to close)
- Features of thermoregulation of the newborn
- Symptoms of newborn overheating
- Symptoms of newborn hypothermia
- Air temperature in the newborn
- temperature baby
- Temperature control
- 0063
- What humidity should be in a child's room? The task of parents is to monitor the correct temperature in the room for the entire first year of a baby’s life.
It is important to understand that a child's thermoregulation disorder is not so easy to detect. A striking sign: constantly high or low body temperature. Or regular fluctuations up or down. Chills, dizziness, weakness are possible.
Parents can help their child by solving two problems:
- Create an optimal temperature regime in the room.
- Dress your newborn correctly.
It is not necessary to wrap up the child when the room is cool or, on the contrary, leave it naked when it is hot. It is necessary to maintain a comfortable temperature in the apartment, at which it will be enough for the baby to put on a vest and sliders.
Symptoms of overheating of the newborn
Systematic overheating of the newborn leads to dehydration, disruption of the nervous and cardiac systems.
The main signs of overheating in a newborn:
- rapid heartbeat;
- reddening of the skin;
- perspiration on the body;
- child's body is hotter than usual;
- lethargy, weakness.
How can I keep my baby from overheating when the room temperature is above 22°C?
- Wear the minimum number of clothes for your baby.
- Give water to drink.
- Bathing a baby.
Symptoms of hypothermia in a newborn
Signs of hypothermia in a newborn:
- cold body, hands, feet;
- pale face, possibly blue;
- blue lips;
- hiccups;
- refusal to eat;
- delayed action.

Actions of parents in case of hypothermia of a newborn
- Put on a warm sleepsuit and socks for the baby.
- Place in an insulated envelope or wrap in a blanket.
- Give a warm drink, breast milk is best.
Air temperature in the newborn home
The optimal temperature in the newborn baby's room ensures the correct functioning of the baby's thermoregulation system. Warm, dry and stagnant air weakens the body's resistance to infectious diseases.
Violation of thermoregulation leads to overheating or hypothermia, which negatively affects the entire body as a whole.
At a comfortable room temperature, the newborn's skin will be warm, dry, of normal color, and breathing will be regular.

How to ventilate a room with a newborn
Be sure to ventilate the room:
- in cold weather 3-4 times a day for 5-15 minutes in the absence of a child;
- in the warm season, the window can be left open during the day, just remember to cover it with a mosquito net.
Newborn room temperature
The World Health Organization recommends that the temperature in the newborn room be 18-21°C.
A hygrometer helps control the air parameters. It is necessary to humidify the dry air in the room during the operation of the central heating. To do this, you can purchase a special device - a humidifier. As an alternative, there are vessels with water placed around the room or clean, wet diapers hung out.
Several thermometers can be purchased for convenience: one for the child's room, the other for measuring the temperature in the bathroom and bathing water.
Dr. Komarovsky about what should be the air in the children's roomComfortable temperature for sleep
For a child to sleep peacefully, the temperature in the room should be below daytime. The optimal temperature for sleeping is 18-21°C. At this room temperature, the child will sleep better.
How do you make sure your child is not overheated or cold?
It is enough to touch the baby's belly or the back of the head - they should be warm. Attention! Not hot and not cold! Don't worry if your baby's hands and feet are cool as this is completely normal.

In case of overheating, it is worth lowering the temperature in the children's room, and if the baby is cold, dress him and / or make the air in the room warmer.
Temperature in the bathroom
The child should be bathed daily. Room temperature should be +18-22°C, water +37°C.
The temperature in the room for a premature baby
Thermoregulation in a premature baby is imperfect. Children quickly cool down and just as quickly overheat. In the maternity ward, immediately after the birth of a premature baby, they are dried and placed in an incubator.
The climate regime in the ward for premature babies is +24-25 °C (on the recommendation of doctors from +25 to +28 °C), humidity is 60%. The room should not be stuffy, the room must be ventilated.
Home environment
- The brightest, dryest and warmest room or part of it is suitable for a premature baby.
- Regularly ventilate the room during the cold season 3-4 times a day, leave the windows open for the whole day during the warm season.

- Take the baby to another room while ventilating the nursery on cold days.
Temperature
During the first two months of life, most preterm infants require a higher ambient temperature than usual.
A premature baby may get cold during bathing, daily toileting, outdoor activities, especially during the cold season. Therefore, changing clothes, performing care procedures should be done as quickly as possible and preferably near an electric heater.
Signs of cooling:
- pallor,
- rare breathing,
- cold skin,
- body temperature below 36.5 °C.
Signs of overheating:
- red face;
- hot skin;
How to maintain the optimal temperature in the newborn room
First of all, install a thermometer in the baby's room.
 You need to focus on + 22-24 ° C, this is the optimal air temperature for a newborn. In the event that centralized heating does not warm the room air to a comfortable temperature, an additional heater is installed. If the room is hot, then it is necessary to ventilate more often. Where it is hot, the air is drier, and accordingly, there is a need for air humidification.
You need to focus on + 22-24 ° C, this is the optimal air temperature for a newborn. In the event that centralized heating does not warm the room air to a comfortable temperature, an additional heater is installed. If the room is hot, then it is necessary to ventilate more often. Where it is hot, the air is drier, and accordingly, there is a need for air humidification. What humidity should be in the children's room
Exhaled air has body temperature and 100% humidity. The drier the inhaled air, the more fluid the baby's body spends on moisturizing it. Air heating reduces the optimum humidity by an average of two times. The drier the air in the room for a newborn, the higher the likelihood of health problems in the baby.
Effects of dry room air on a child:
- difficult breathing;
- dry skin;
- dry mucous membranes, hence crusting in the nose.
Optimum humidity in a newborn room is 50-70%. You can achieve a normal level of humidity in an apartment using old, proven methods - frequent wet cleaning, airing the room, as well as modern ones - climate control, air humidifiers.