Oral thrush infant treatment
Thrush in newborns Information | Mount Sinai
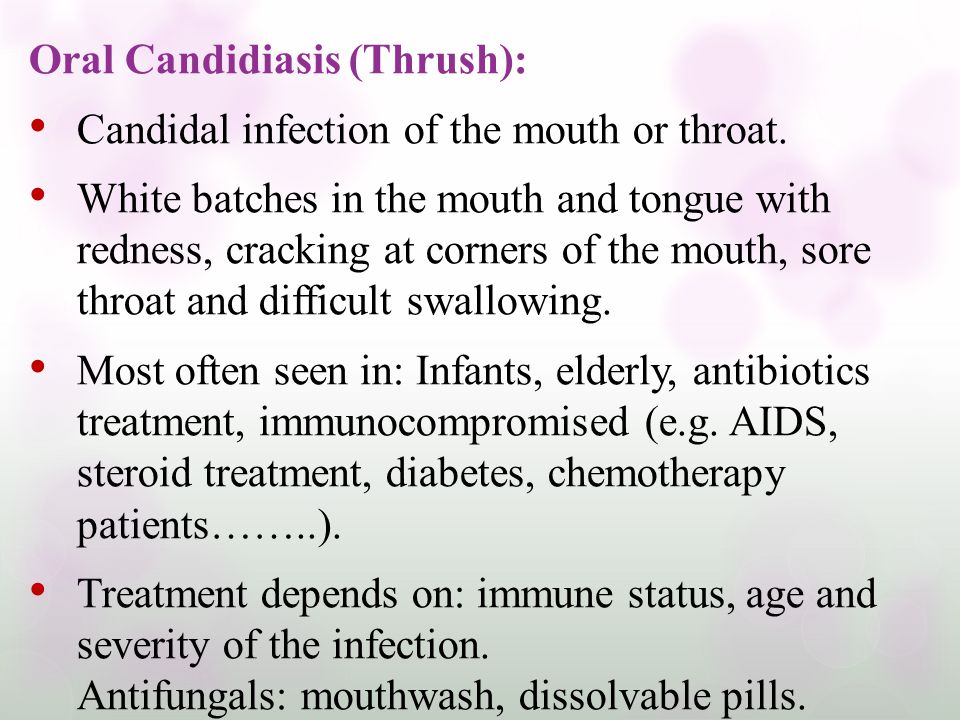
Candidiasis - oral - newborn; Oral thrush - newborn; Fungal infection - mouth - newborn; Candida - oral - newborn
Thrush is a yeast infection of the tongue and mouth. This common infection can be passed between a mother and baby during breastfeeding.
Causes
Certain germs normally live in our bodies. While most germs are harmless, some can cause infection.
Thrush occurs when too much of a yeast called Candida albicans grows in a baby's mouth. Germs called bacteria and fungi naturally grow in our bodies. Our immune system helps keep these germs in check. But babies do not have fully-formed immune systems. That makes it easier for too much yeast (a type of fungus) to grow.
Thrush often occurs when mother or baby has taken antibiotics. Antibiotics treat infections from bacteria. They can also kill "good" bacteria, and this allows yeast to grow.
The yeast thrives in warm, moist areas. The baby's mouth and the mother's nipples are perfect places for a yeast infection.
Babies can also get a yeast infection on the diaper area at the same time. The yeast gets in the baby's stool and can cause a diaper rash.
Symptoms
Symptoms of thrush in the baby include:
- White, velvety sores in the mouth and on the tongue
- Wiping the sores may cause bleeding
- Redness in the mouth
- Diaper rash
- Mood changes, such as being very fussy
- Refusing to nurse because of soreness
Some babies may not feel anything at all.
Symptoms of thrush in the mother include:
- Deep-pink, cracked, and sore nipples
- Tenderness and pain during and after nursing
Exams and Tests
Your health care provider can often diagnose thrush by looking at your baby's mouth and tongue. The sores are easy to recognize.
Treatment
Your baby might not need any treatment. Thrush often goes away on its own in a few days.
Thrush often goes away on its own in a few days.
Your provider may prescribe antifungal medicine to treat thrush. You paint this medicine on your baby's mouth and tongue.
If you have a yeast infection on your nipples, your provider may recommend an over-the-counter or prescription antifungal cream. You put this on your nipples to treat the infection.
If both you and your baby have the infection, you both need to be treated at the same time. Otherwise, you can pass the infection back and forth.
Outlook (Prognosis)
Thrush in babies is very common and can easily be treated. Let your provider know if thrush keeps coming back. It may be a sign of another health issue.
When to Contact a Medical Professional
Contact your provider if:
- Your baby has symptoms of thrush
- Your baby refuses to eat
- You have symptoms of a yeast infection on your nipples
Prevention
You may not be able to prevent thrush, but these steps may help:
- If you bottle feed your baby, clean and sterilize all equipment, including nipples.

- Clean and sterilize pacifiers and other toys that go in baby's mouth.
- Change diapers often to help prevent yeast from causing diaper rash.
- Be sure to treat your nipples if you have a yeast infection.
Balest AL, Riley MM, O'Donnell B, Zarit JS. Neonatology. In: Zitelli BJ, McIntire SC, Nowalk AJ, Garrison J, eds. Zitelli and Davis' Atlas of Pediatric Physical Diagnosis. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 2.
Harrison GJ. Approach to infections in the fetus and newborn. In: Cherry JD, Harrison GJ, Kaplan SL, Steinbach WJ, Hotez PJ, eds. Feigin and Cherry's Textbook of Pediatric Infectious Diseases. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 66.
Last reviewed on: 12/12/2021
Reviewed by: Neil K. Kaneshiro, MD, MHA, Clinical Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Oral thrush (mouth thrush) - NHS
Oral thrush is usually harmless. It's common in babies and older people with dentures. It can be easily treated with medicines bought from a pharmacy.
Check if it's oral thrush
Adults
Your mouth is red inside and you have white patches.Credit:
DR P. MARAZZI/SCIENCE PHOTO LIBRARY https://www.sciencephoto.com/media/459245/view
When you wipe off the white patches, they leave red spots that can bleed.Credit:
DR P. MARAZZI/SCIENCE PHOTO LIBRARY https://www. sciencephoto.com/media/633814/view
sciencephoto.com/media/633814/view
Other symptoms in adults are:
- cracks at the corners of the mouth
- not tasting things properly
- an unpleasant taste in the mouth
- pain inside the mouth (for example, a sore tongue or sore gums)
- difficulty eating and drinking
Oral thrush in adults is not contagious.
Babies
A white coating on the tongue like cottage cheese – this cannot be rubbed off easily.Credit:
DR M.A. ANSARY/SCIENCE PHOTO LIBRARY https://www.sciencephoto.com/media/251590/view
Sometimes there are white spots in their mouth.Credit:
DR P. MARAZZI / SCIENCE PHOTO LIBRARY https://www.sciencephoto.com/media/252476/view
MARAZZI / SCIENCE PHOTO LIBRARY https://www.sciencephoto.com/media/252476/view
Other symptoms in babies are:
- they do not want to feed
- nappy rash
Babies can pass oral thrush on through breastfeeding. This can cause nipple thrush in mothers.
If you're not sure it's oral thrush
Look at other causes of a white or sore tongue.
A pharmacist can help with oral thrush
Oral thrush can be easily treated with a mouth gel bought from a pharmacy. The gel is suitable for adults, children and babies over the age of 4 months.
Ask your pharmacist for advice. Always follow the instructions on the medicine packet.
If you leave oral thrush untreated, the infection can spread to other parts of the body.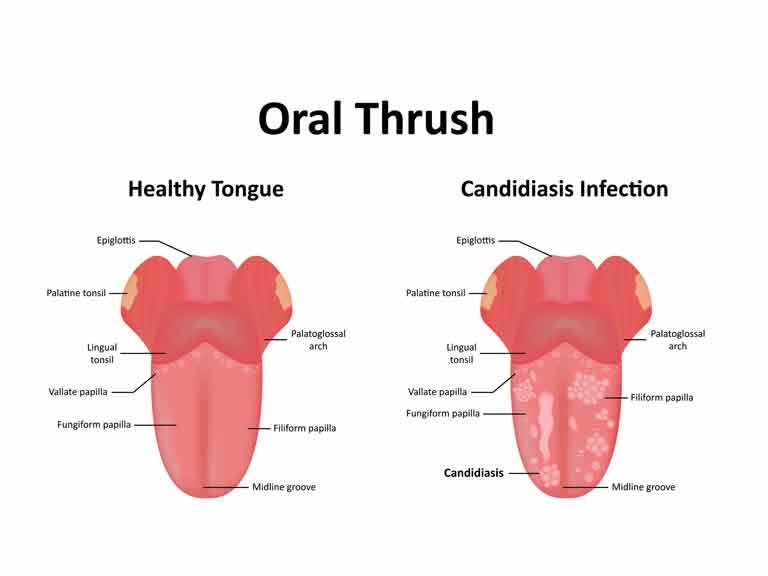
Non-urgent advice: See a GP if:
- your baby is under 4 months and has signs of oral thrush
- you do not see any improvement after 1 week of treatment with a mouth gel
- you have difficulty or pain swallowing
How you can prevent oral thrush
Thrush is an infection caused by a fungus called Candida. Some things can make the fungus grow more than usual.
You might get thrush if you're:
- taking antibiotics over a long time
- using asthma inhalers
- getting cancer treatment like chemotherapy
There are some things you can do to help prevent oral thrush:
Do
-
take care of your teeth: brush twice a day, clean your dentures, and go for regular check-ups even if you have dentures
-
brush your gums and tongue with a soft toothbrush if you do not have any teeth
-
sterilise dummies regularly
-
sterilise bottles after each use
-
rinse your mouth after eating or taking medicine
-
go to regular check-ups if you have a long-term condition like diabetes
Page last reviewed: 08 July 2020
Next review due: 08 July 2023
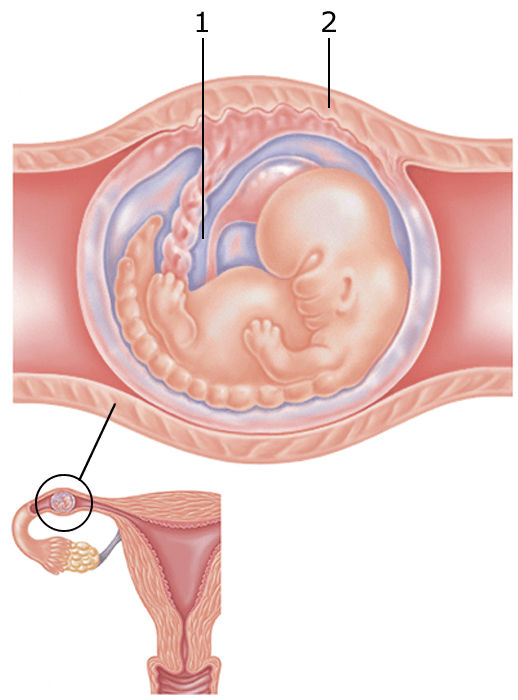
Candidiasis in the mouth of a child
Contents
What kind of disease is candidiasisSymptomsCausesTreatmentMethods of therapyPreventive measures
Many parents are aware of such a common problem in children as thrush, which is characterized by the appearance of white plaque on the tissues of the oral cavity.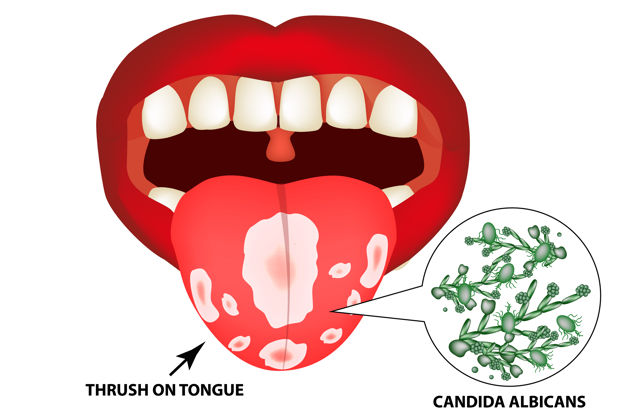 In medicine, this pathological condition has the term "candidiasis" and refers to fungal diseases.
In medicine, this pathological condition has the term "candidiasis" and refers to fungal diseases.
Most often, candidiasis develops in the mouth of a child in the first year of life. Symptoms of thrush greatly disturb the baby, but timely treatment allows you to quickly and without consequences get rid of the fungus.
What kind of disease is candidiasis
According to statistics, about 30% of infants are faced with candidiasis. The causative agent of the disease is the Candida fungus. These specific microorganisms are normally present in the body of every person, even in the absence of health problems, but only in small quantities.
Oral candidiasis in children is much more common, since the immune system of babies is not yet formed and is not able to withstand pathogenic microorganisms and the effects of negative external factors.
With a weakened immune system and the concomitant effect of provoking factors, the fungus begins to actively multiply, affecting the mucous membranes. Without therapeutic treatment, candidiasis is eliminated in exceptional cases. If thrush is not treated, complications arise, and the infection itself spreads throughout the body.
Without therapeutic treatment, candidiasis is eliminated in exceptional cases. If thrush is not treated, complications arise, and the infection itself spreads throughout the body.
Symptoms
Oral candidiasis in children can have a different form of manifestation and severity of symptoms: mild, moderate and severe. As a rule, each form corresponds to the stage of development of the disease. If therapy is not carried out in a timely manner, then the signs of a fungal infection become more intense and the number of symptoms increases.
With a mild form of the disease, a red rash appears on the oral mucosa, which is covered with a white coating on top. At the next stage, the child has swelling of the tissues and the formation of localized white spots with a touch of curd consistency. Gradually, these spots merge into a large affected area. When plaque is removed, bleeding sores open. If the thrush starts, then the fungus already spreads to the entire oral cavity, including the lips, tongue and throat. All fabrics are completely covered with cheesy bloom.
All fabrics are completely covered with cheesy bloom.
Common symptoms of candidiasis in children include:
-
burning sensation and itching in the mouth;
-
discomfort and pain when eating;
-
frequent spitting up in babies;
-
the formation of cracks in the corners of the lips;
-
temperature rise.
Children of the first two years of life report their condition with refusal to eat, constant whims and causeless crying. It is not difficult to see signs of candidiasis, so if a child has a sharp rise in temperature or refuses to eat, pediatricians and dentists recommend checking the oral cavity for white plaque. If you suspect thrush, it is undesirable to delay a visit to a specialist, since the fungal infection progresses rapidly.
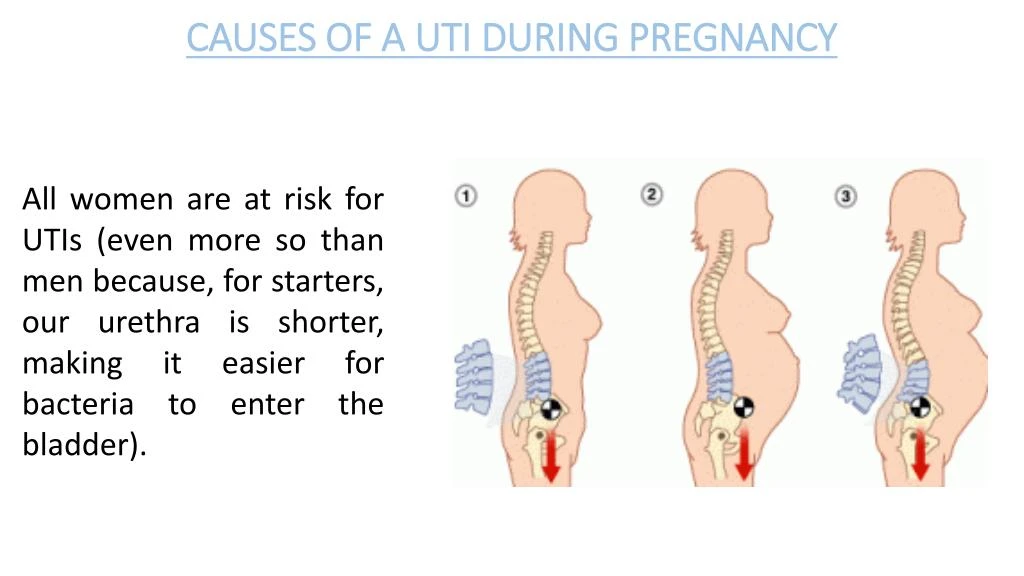
Reasons
The main reason for the development of candidiasis of the oral mucosa in children is a weakened immune system.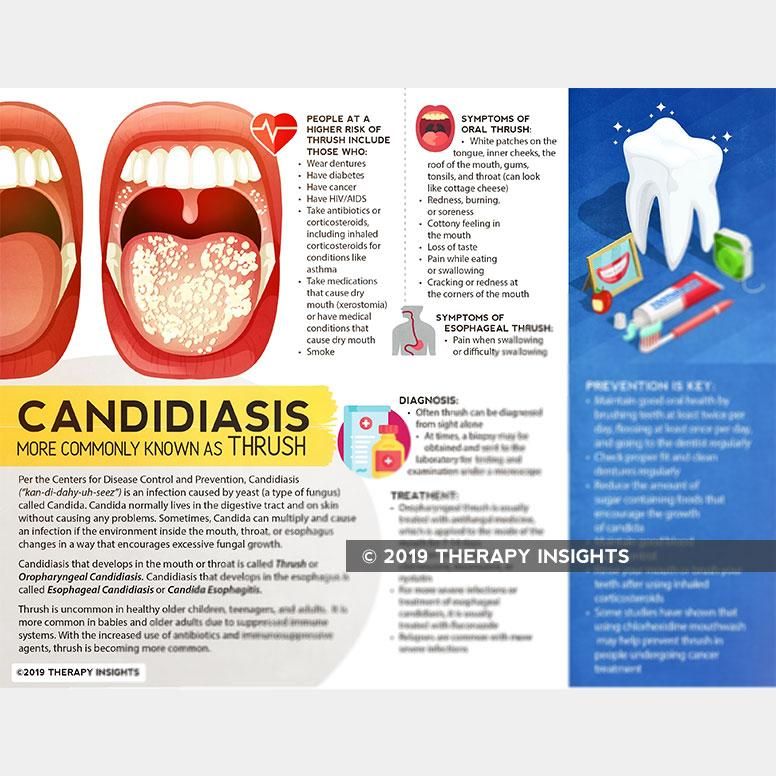 If a child is born prematurely, then the likelihood of having thrush is very high. Children who are breastfed or have congenital pathologies are also often exposed to fungal infection.
If a child is born prematurely, then the likelihood of having thrush is very high. Children who are breastfed or have congenital pathologies are also often exposed to fungal infection.
Provoking factors include:
-
the presence of vaginal candidiasis in the mother during pregnancy - the child can become infected when passing through the birth canal;
-
insufficient hygiene of the female breast during breastfeeding - the fungus is often localized precisely on the nipples because of the favorable environment for it;
-
poor processing of the child's initial things - bottles, nipples, and so on;
-
the habit of parents to lick the nipples - even if the adult does not have signs of thrush, a fungus may be present in the mouth, which will be transmitted to the child;
-
long-term use of drugs of the "antibiotics" group - drugs help to reduce one's own immunity;
-
frequent regurgitation in infants - after regurgitation, an increased acidic environment, favorable for the fungus, remains inside the oral cavity;
-
excessive and frequent dry mouth - the absence of saliva, as a protective agent against the activity of pathological microorganisms.

Infection with Candida fungus in children older than 2 years can occur as a result of unwashed foods, raw milk or running water. If a child over 3 years of age has suddenly developed signs of thrush, one should be examined not only for a fungal infection, but also for other possible diseases that may be accompanied by a “fading” of the immune system.
Treatment
Children's fungal diseases can be dealt with by a pediatrician, infectious disease specialist or dermatologist. If we are talking about the treatment of thrush of the oral cavity, then the dentist can also carry out therapy.
The diagnosis of "candidiasis" is determined in most cases on the basis of a specialist examination of the oral cavity. If there is any doubt, the doctor directs the patient for additional examinations. To confirm the disease, a laboratory method is used to study a smear taken from the mouth for the presence of a fungus.
Treatment of thrush in children involves an integrated approach. If the disease is not advanced, then local therapy is carried out in combination with the adoption of measures to strengthen the immune system. In severe form, oral candidiasis in children is treated with systemic drugs, local remedies and compliance with preventive recommendations.
If the disease is not advanced, then local therapy is carried out in combination with the adoption of measures to strengthen the immune system. In severe form, oral candidiasis in children is treated with systemic drugs, local remedies and compliance with preventive recommendations.
Methods of therapy
Treatment of candidiasis begins with the treatment of the oral cavity. The first procedure is already performed at the reception. Antiseptic agents are used to remove plaque. The doctor may then apply an antifungal agent.
The parent should carefully monitor the actions of the dentist, as in the future they will have to independently process the oral cavity at home. The necessary drugs will be prescribed by a specialist. Local antifungal agents are dangerous in case of overdose, especially for the child's body, so you must strictly follow the doctor's recommendations.
In advanced cases, medications are prescribed in the form of solutions, drops or tablets.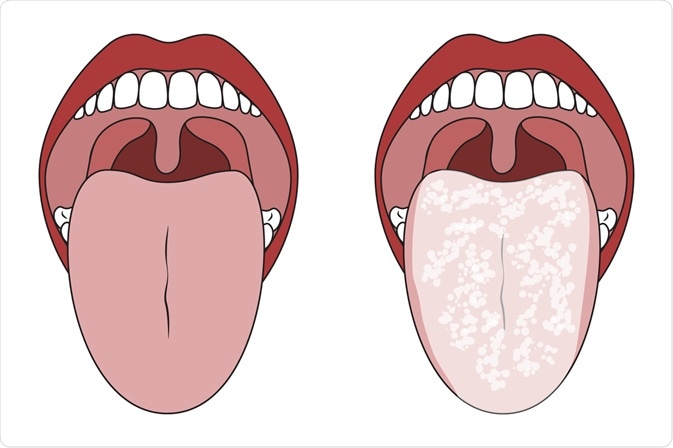 There are only a few drugs for the treatment of candidiasis in children. Replacing them with adult counterparts is dangerous. The dosage must be strictly observed.
There are only a few drugs for the treatment of candidiasis in children. Replacing them with adult counterparts is dangerous. The dosage must be strictly observed.
A mandatory addition to the main therapy is hygiene, good sleep, proper nutrition and taking measures to strengthen immunity (eating healthy foods, if necessary, pharmacy vitamins, walking.
Preventive measures
In order to prevent and even shorten the course of therapy, it is recommended to rinse the mouth (if the child is older than 3-4 years), or use antiseptic sprays several times a day.
It is not difficult to prevent oral candidiasis in children. The responsible approach of parents to the health of the child from the moment of planning conception and pregnancy will help to avoid fungal infections in babies.
Candidiasis (thrush) of the oral cavity - symptoms and treatment
Oral candidiasis is an inflammatory disease that develops against the background of damage to the mucous membranes by fungi of the genus Candida. This is usually associated with a deterioration in local and general immunity. According to studies, up to 90% of the adult population is carriers of this fungus, but the disease most often does not develop, since under normal conditions the pathogen does not act aggressively.
This is usually associated with a deterioration in local and general immunity. According to studies, up to 90% of the adult population is carriers of this fungus, but the disease most often does not develop, since under normal conditions the pathogen does not act aggressively.
Causes of candidiasis
Thrush in the mouth in an adult is a mucosal lesion that may indicate serious health problems. For the reproduction of the fungus, special conditions are necessary. Most often, the disease occurs in patients who neglect oral hygiene. The presence of caries, inflammatory gum disease increases the chances of developing fungal inflammation. This is due to the fact that a large number of pathogenic microorganisms depletes the defense mechanisms.
The second group of reasons is the weakening of the immune system due to a number of diseases and conditions:
-
HIV, diabetes mellitus;
-
oncological diseases;
-
dystrophy, deficiency of vitamins, minerals;
-
surgeries, severe infections, etc.
There are also specific reasons for the development of thrush. It may appear after prolonged and powerful antibiotic therapy. The use of antibiotics leads to the destruction of beneficial flora and imbalance. This causes the active reproduction of Candida.
Oral candidiasis also develops against the background of inhaled corticosteroids. Usually the lesion has the appearance of erythema and appears in areas where the drug has come into contact with the mucosa: in the palate, tongue.
Features of the diet affect the likelihood of developing candidiasis. So, the predominance of carbohydrates predisposes to the activity of the fungus. The growth of Candida and its attachment to the mucosa are enhanced in the presence of sugars.
Bad habits increase the chances of developing leukoplakia, lichen planus and other diseases. Especially when it comes to smoking. Candidiasis often develops in patients with tongue piercings.
The presence of removable dentures is also a risk factor if the patient does not follow the rules of hygiene. In the absence of high-quality cleansing, the prosthesis is covered with a biofilm, which contains a lot of fungi. Disinfection is the main measure for the prevention of the disease and part of the complex treatment for progressive oral candidiasis. If the patient does not remove the structure at night, this also increases the likelihood of developing the disease. The mucous membrane remains without oxygen for a long time, is not washed by saliva - these conditions are suitable for the development of fungi and anaerobic microorganisms. The prosthesis can injure the mucous membranes if it does not fit. Microtraumas weaken local defenses and contribute to the onset of the development of a fungal infection. Injuries can also be associated with sharp chipped teeth and fillings, chemical and thermal burns.
In the absence of high-quality cleansing, the prosthesis is covered with a biofilm, which contains a lot of fungi. Disinfection is the main measure for the prevention of the disease and part of the complex treatment for progressive oral candidiasis. If the patient does not remove the structure at night, this also increases the likelihood of developing the disease. The mucous membrane remains without oxygen for a long time, is not washed by saliva - these conditions are suitable for the development of fungi and anaerobic microorganisms. The prosthesis can injure the mucous membranes if it does not fit. Microtraumas weaken local defenses and contribute to the onset of the development of a fungal infection. Injuries can also be associated with sharp chipped teeth and fillings, chemical and thermal burns.
Dryness of the oral cavity due to decreased salivation, changes in the viscosity of saliva, its composition is one of the causes of candidiasis. This may be due to other diseases, so it is important to find out the causes of dryness in order to effectively deal with the consequences.
Oral candidiasis is more common in children. The immaturity of the immune system, the colonization of the oral cavity by Candida from the vaginal canal of the mother during natural childbirth lead to the fact that the disease develops in early infancy. However, older children can also suffer from an illness, which is associated with a weakening of the immune forces.
Types of oral candidiasis and symptoms
Manifestations of oral candidiasis may vary from patient to patient. This is due to the degree of damage to the mucous membranes, as well as the specific type of disease. There are four forms:
-
acute pseudomembranous;
-
acute atrophic;
-
chronic atrophic;
-
chronic hyperplastic.
Despite the fact that the treatment regimen for all forms is almost the same, the symptoms can vary significantly. Let's consider them in more detail.
Acute pseudomembranous candidiasis
This form of oral candidiasis may be asymptomatic. There is slight discomfort due to a white film or small plaques rising above the mucosa. With a mild course, one or more plaques appear, they are easily removed by scraping, and the mucosal area under them has a bright red color. In severe cases, large plaques appear in large numbers. They can merge, forming large areas of damage. Sometimes the symptoms cover the entire mucous membrane. When the plaques thicken, their removal becomes problematic. A severe course is more typical for infants, as well as in adult patients after antibiotic therapy, corticosteroids, immunosuppressants.
There is slight discomfort due to a white film or small plaques rising above the mucosa. With a mild course, one or more plaques appear, they are easily removed by scraping, and the mucosal area under them has a bright red color. In severe cases, large plaques appear in large numbers. They can merge, forming large areas of damage. Sometimes the symptoms cover the entire mucous membrane. When the plaques thicken, their removal becomes problematic. A severe course is more typical for infants, as well as in adult patients after antibiotic therapy, corticosteroids, immunosuppressants.
Acute and chronic atrophic candidiasis
Acute atrophic candidiasis is accompanied by severe burning. There may be no white plaque, and the mucous membrane becomes bright red. Many patients report a metallic, sour, salty, or bitter taste in their mouths. A characteristic manifestation of the disease is dry mouth. This form of the disease is often associated with drug therapy.
In chronic atrophic candidiasis, redness and burning are less pronounced. Usually the disease develops against the background of the installation and wearing of prostheses.
Usually the disease develops against the background of the installation and wearing of prostheses.
Chronic hyperplastic candidiasis
This form of the disease is characteristic of adults. Oral thrush can spread to the mucous membranes of the cheeks, the corners of the mouth and lips, the back of the tongue, and the soft palate. One of the symptoms is the appearance of white plaques that tend to merge with each other. As the disease progresses, their surface becomes rough, rough. Over time, the elements may turn yellow. Formations merge with mucous membranes and it is impossible to remove them.
Diagnostic methods
Treatment by a general dentist. Diagnosis begins with an examination and a detailed survey: the doctor will find out what drugs you have taken recently, whether there are chronic and infectious diseases. A cytological examination of plaque taken from the mucosa is mandatory. This is important because the accumulation of non-fungal flora can be easily confused with a fungal infection.
Scraping is performed in the morning, on an empty stomach, it is not necessary to brush your teeth before the procedure. On the eve, it is important to refuse to eat foods rich in carbohydrates so as not to provoke the growth of pathogenic flora. Studies allow not only to accurately determine the pathogen and type of Candida fungus, but also to find out the sensitivity of fungi to the main antifungal drugs. Based on the results of the tests, the doctor will determine the fungus in the oral cavity and prescribe medication.
Features of treatment
The basis of treatment is systemic and local antifungal drugs. Today they are widely represented on the pharmaceutical market, but it is important to know that the level of Candida fungus resistance to fixed assets is growing every year. For example, resistance to drugs such as Fluconazole is almost complete. Previously, this remedy was used in almost all cases of the disease, but today doctors are forced to revise standard treatment regimens.
Treatment of thrush in the mouth in adults is selected individually. The choice of a systemic antifungal agent is based on the type of pathogen, the patient's condition and the individual characteristics of his health. There are agents to which the infection has minimal resistance. The doctor may prescribe drugs based on nystatin, imidazole derivatives, etc.
In addition, local funds must be used:
-
mouth rinses;
-
gels and suspensions for application to affected areas;
-
topical lozenges and lozenges;
-
irrigation solutions and aerosols;
-
ointments for laying in the oral cavity on a cotton-gauze swab, etc.
Your healthcare provider may prescribe an over-the-counter antiseptic or mild saline rinse. Usually, solutions based on iodine, chlorhexidine, potassium permanganate, gentian violet, sodium tetraborate in glycerin are used. Some pills the doctor may recommend laying on the cheek.
Conditions for effective treatment
Effective treatment for oral thrush involves addressing the underlying cause. It is very important to sanitize the oral cavity: to cure teeth destroyed by caries, to remove non-viable teeth and roots that can no longer be restored. These are chronic foci of inflammation, so simultaneous sanitation will shorten the treatment time. Tartar and plaque should also be removed. This is especially true in cases of candidal stomatitis associated with trauma to the gums with sharp edges of hard dental deposits.
Patients with removable dentures should be retrained in hygiene and disinfection of prosthetic structures. If the time of using the prosthesis comes to an end, it is important to replace it in a timely manner. Treatment of candidiasis will be useless if a person uses the prosthesis incorrectly and again creates conditions for the reproduction of fungi in the oral cavity.
Unsuitable crowns, bridges and other structures are also subject to replacement. It is also important to eliminate enamel chips, which become a source of injury to the gums, mucous membranes of the cheeks and tongue.
It is also important to eliminate enamel chips, which become a source of injury to the gums, mucous membranes of the cheeks and tongue.
Smokers should, if possible, reduce their smoking episodes or give up smoking habits. If the disease developed while taking corticosteroids, it is important to explain the rules of treatment: you should rinse your mouth with plenty of warm water after spraying the drug.
In the treatment of oral candidiasis that has developed against the background of antibiotic therapy, measures should be taken to restore the normal microflora of the intestine and oral cavity. It may be necessary to consult another narrow specialist or therapist: you will need to take probiotics and prebiotics.
For all patients treated for candidiasis, a few general guidelines apply:
-
maintaining oral hygiene;
-
refusal of food rich in carbohydrates;
-
Refusal of sugary drinks.
It is necessary to exclude from the diet foods that can irritate the mucous membranes: dishes prepared with vinegar, marinades, spicy, peppery foods, smoked meats, sour fruits and berries. Also, you can not eat confectionery, pastries with yeast, sugar. It is better to give preference to warm dishes. It is necessary to observe such a diet for another 1.5-2 months after recovery.
Also, you can not eat confectionery, pastries with yeast, sugar. It is better to give preference to warm dishes. It is necessary to observe such a diet for another 1.5-2 months after recovery.
In some cases, it is advisable to use toothpastes with glucose oxidase, lysozyme, lactoferrin. They improve the protective forces of the oral mucosa and can be part of a comprehensive prevention of inflammation. The choice of toothpaste must be agreed with the doctor, he will recommend the best remedy, and also tell you which brush is suitable.
Prevention of candidiasis
Specific prophylaxis of oral candidiasis is performed only in the presence of HIV infection, the patient undergoing radiation therapy, immunosuppressive or antibiotic therapy. In the absence of these risk factors, the doctor will make recommendations for a specific case.
Prevention of fungal diseases in patients with diabetes mellitus, bronchial asthma, chronic systemic diseases involves control of the underlying pathology.