What is the third stage of labor
Giving birth - third stage of labour
Giving birth - third stage of labour | Pregnancy Birth and Baby beginning of content6-minute read
Listen
What is the third stage of labour?
The third stage of labour begins when your baby is born. During this stage of labour, the placenta and membranes that supported your baby in your uterus come out through your vagina.
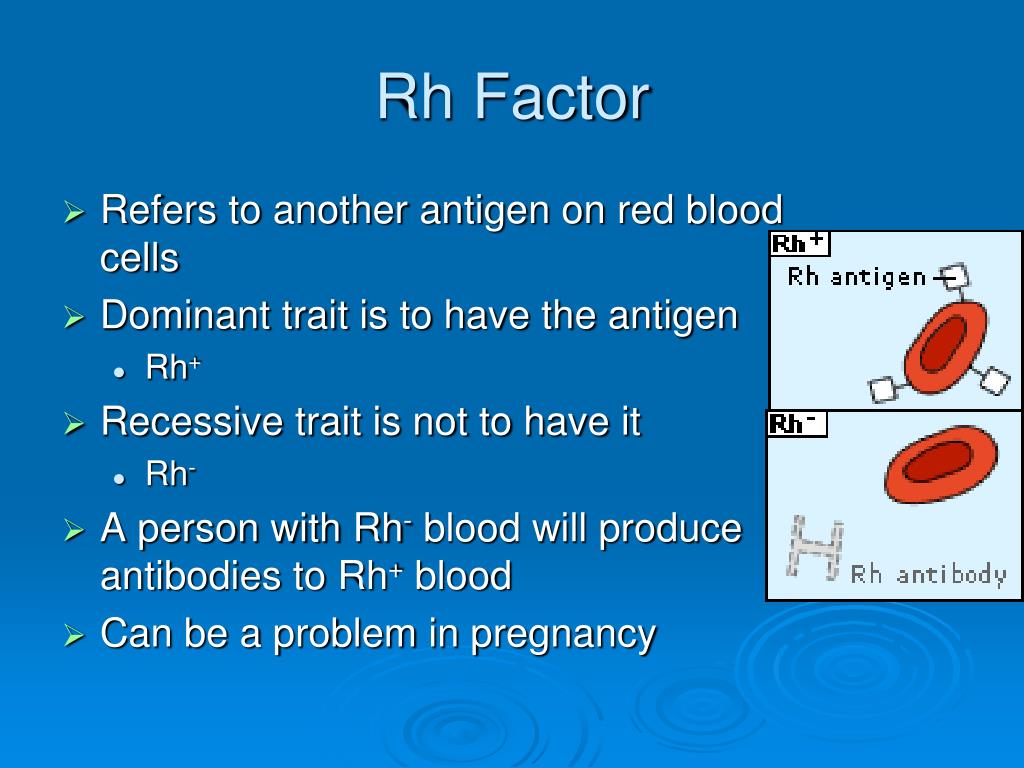
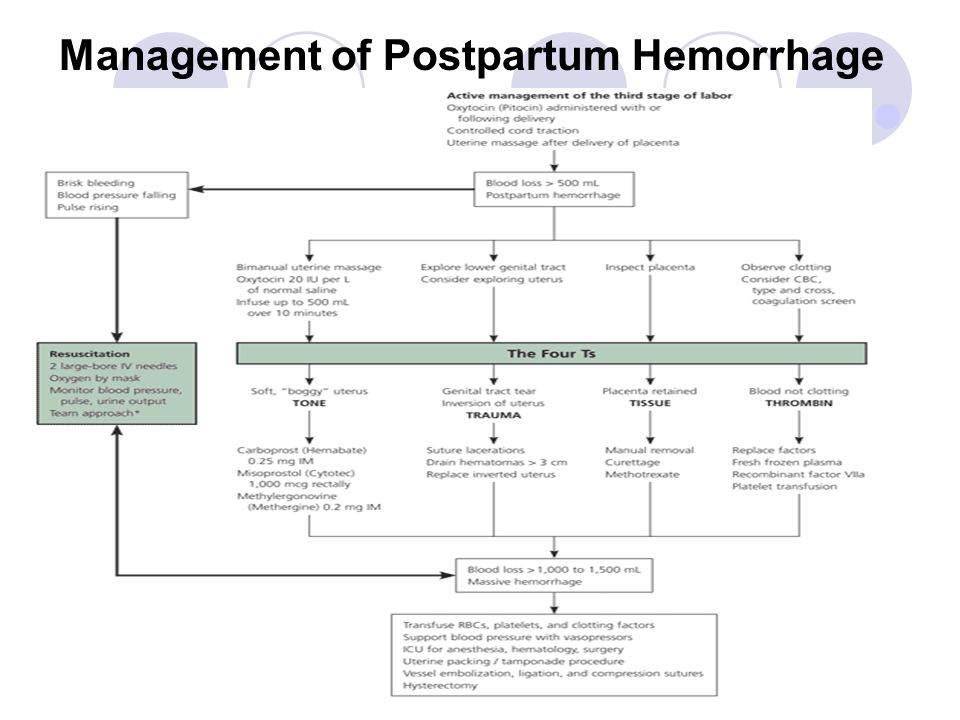
Your midwife can help this to happen by guiding the placenta out and by giving you an injection to help your uterus contract. This is called ‘active management’. Some women prefer to deliver their placenta without medical help. This is called 'physiological management'. It is a good idea to discuss your preferences with your healthcare team during your pregnancy and before the birth.
During the third stage of labour, the umbilical cord, which connected your baby to your placenta, is clamped and cut. If you would like the umbilical cord to be left intact, or to be clamped later, you should let your midwife know so that they can arrange this. If your birth partner would like to cut the cord, let your midwife know. You may also like to add this to your birth plan, if you have one.
How long does it usually last?
The third stage of labour generally lasts about 30 minutes if actively managed. If you decide to use physiological management, meaning that you deliver the placenta without medication or hands-on help from your midwife, the third stage can take up to one hour.
What can I do to help the placenta come out?
You may choose to change positions to help the placenta come out. Pushing gently will also help the placenta come out. You may experience mild contractions as the placenta comes away from your uterus.
How can my midwife support the third stage of labour?
If you are actively managing the third stage of labour, your midwife will offer you an injection of a medicine called oxytocin.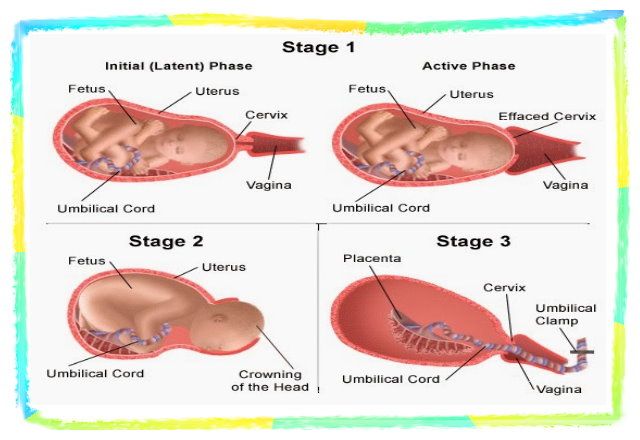 This helps your uterus to contract after birth. This medicine is used to reduce the risk of excessive bleeding (post-partum haemorrhage), and to reduce the risk of needing a blood transfusion after birth.
This helps your uterus to contract after birth. This medicine is used to reduce the risk of excessive bleeding (post-partum haemorrhage), and to reduce the risk of needing a blood transfusion after birth.
Your midwife will support you by checking the position of your uterus and by gently pulling on the umbilical cord when they notice signs that your placenta is ready to come out.
When the placenta begins to come out through your vagina, your midwife will guide the placenta, while gently twisting to make sure all of the membranes come out with it.
Your midwife will also clamp and cut the umbilical cord. This is generally done a few minutes after your baby is born, and after the blood in the umbilical cord has had time to flow into your baby. In some situations, your doctor or midwife may recommend clamping and cutting the umbilical cord immediately after birth. This is usually only needed if you or your baby are very unwell.
Women have different preferences regarding when the umbilical cord should be cut and what should be done with the placenta after delivery. Your health team will do all they can to facilitate and support your decisions, while keeping the health of you and your baby as a top priority.
Your health team will do all they can to facilitate and support your decisions, while keeping the health of you and your baby as a top priority.
Do I need stitches after labour?
After your placenta has come out, your midwife will check the skin around your vagina (your perineum) for tears. Your skin can sometimes tear when it is stretched during birth. Your midwife will check if you have a tear and if so, how deep the tearing is and where it is located. Small, shallow tears may not need to be closed with stitches. However, larger tears should be treated to make sure that they heal properly and to reduce your chance of complications afterwards. If you need stitches, your doctor or midwife will offer you medicine for pain relief before you get them. If you have had an episiotomy, this will also need stitches.
Will my birth partner be with me?
Your birth partner can stay with you throughout this stage of labour if you would like them to be. They will be able to support you, for example by reassuring you and bringing you anything you need.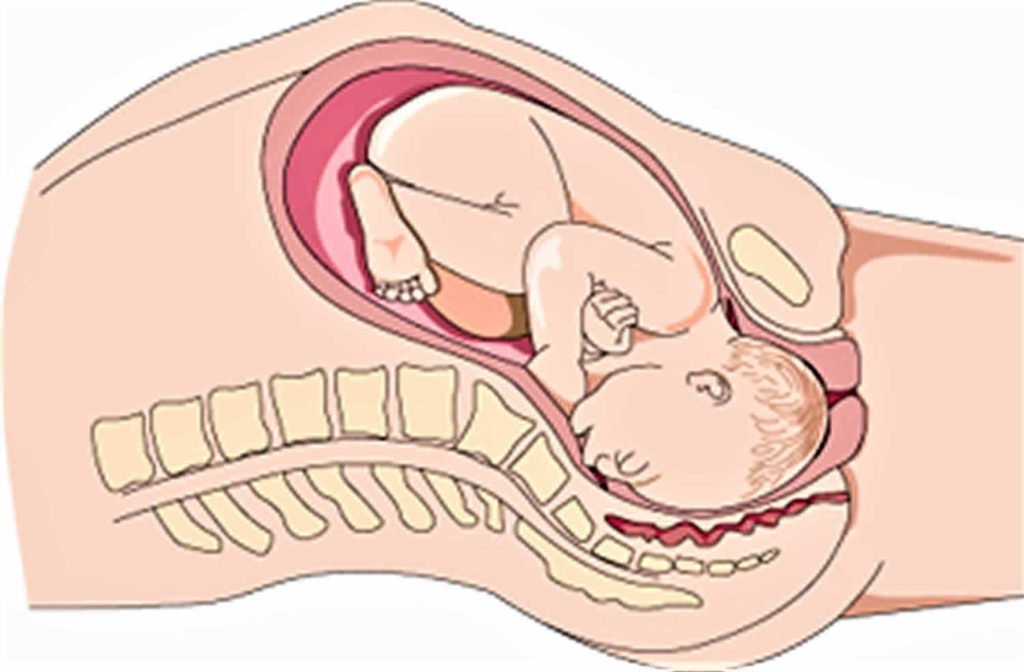 If you would prefer that your birth partner is not with you during any part of your labour, let your midwife know — it’s your choice.
If you would prefer that your birth partner is not with you during any part of your labour, let your midwife know — it’s your choice.
Where is my baby during the third stage of labour?
Your baby will be placed on your chest or stomach after they are born, with their skin directly in contact with yours. This is called ’skin-to-skin’ contact and it is your first opportunity to hold and cuddle your new baby. Your midwife will cover you both with a blanket to keep you warm. They will also check on you and your baby to make sure you are both doing well. Your midwife will need to measure your baby and give them medicines, but there is no rush. This time is for you to meet your baby and enjoy being with them.
This is also a good opportunity to breastfeed your baby for the first time if you would like to. Breastfeeding can shorten the third stage of labour and reduce the amount of bleeding you experience. This is because breastfeeding causes your body to release oxytocin, which naturally contracts your uterus.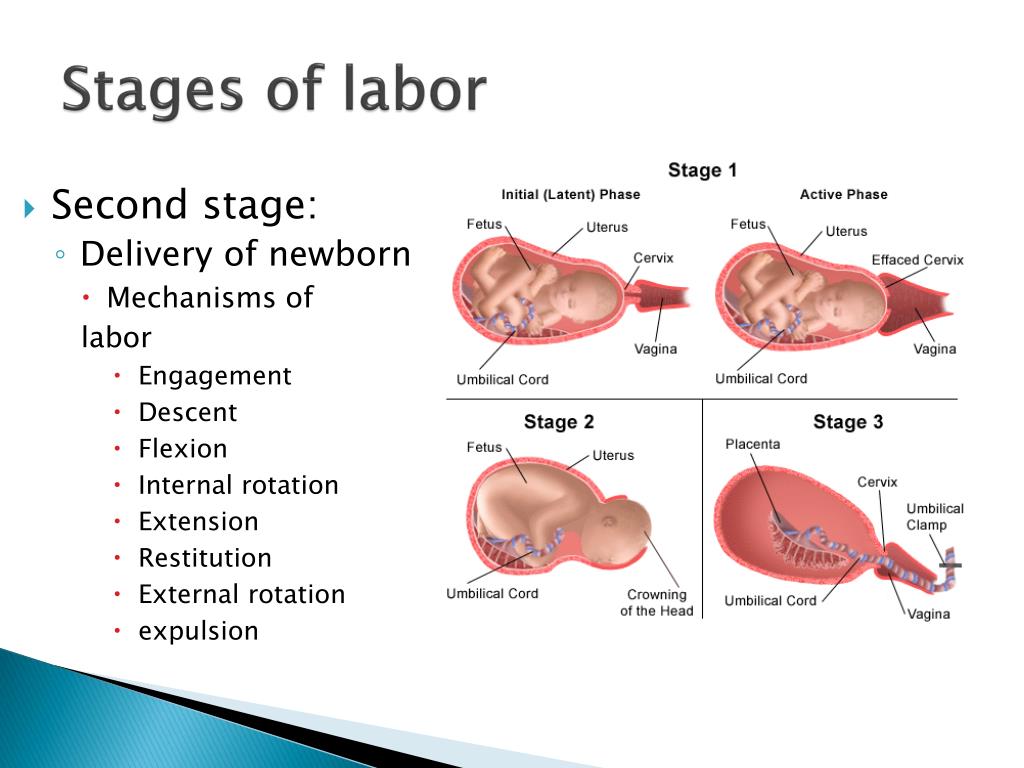 Your midwife will show you how to breastfeed your baby if you would like them to. You can breastfeed your baby right after birth (even if you plan to bottle feed later). Some women find that this a great way to start to bond with their newborn.
Your midwife will show you how to breastfeed your baby if you would like them to. You can breastfeed your baby right after birth (even if you plan to bottle feed later). Some women find that this a great way to start to bond with their newborn.
What happens if something goes wrong?
Every labour is unique, and sometimes things don’t go according to plan. You may have to adjust your birth plan if the situation calls for it. There can be labour complications in which extra medical support is needed. Your midwife will communicate with you and your doctor to guide you to make the best decisions for you and your baby.
Listen to our podcast on understanding your choices when having a baby.
Sources:
Queensland government (Stages of Labour - The Third Stage of Labour), Queensland government (Guideline: Normal Birth), Royal Women's (Stages of labour), The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Provision of routine intrapartum care in the absence of pregnancy complications), Queensland government (Perineal care), Queensland government (Establishing breastfeeding)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: February 2022
Back To Top
Related pages
- Giving birth - second stage of labour
- Giving birth - first stage of labour
- Giving birth - stages of labour
- Giving birth - waters breaking
- Giving birth - contractions
Need more information?
Giving birth - stages of labour
You're unlikely to mistake the signs of labour when the time comes, but if you're in any doubt don't hesitate to contact your midwife.
Read more on Pregnancy, Birth & Baby website
Giving birth - first stage of labour
Find out what happens during the first stage of labour.
Read more on Pregnancy, Birth & Baby website
Giving birth - second stage of labour
The second stage of labour is when you give birth to your baby.
Read more on Pregnancy, Birth & Baby website
Induced labour
Induced labour is a medical treatment to start labour. It may be recommended if your baby needs to be born before labour is due to start naturally.
Read more on Pregnancy, Birth & Baby website
Slow progress in labour
Slow progress in labour is also called failure to progress or prolonged labour. Read what happens when your labour doesn't go as quickly as expected.
Read more on Pregnancy, Birth & Baby website
Labour and birth using water
Information to help you make an informed choice for you and your baby about using water during the first stage of your labour or having a waterbirth.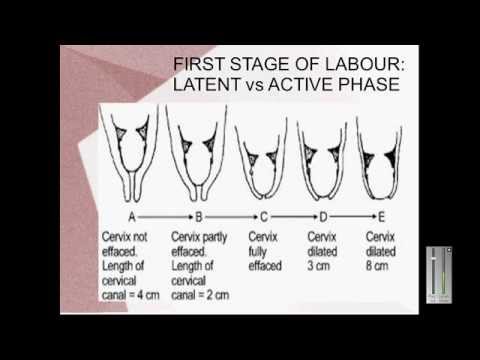
Read more on WA Health website
Pain Relief in Labour and Childbirth
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website
Interventions during labour
An ‘intervention’ is an action taken by a midwife or doctor that literally intervenes in the birthing process. Read about the different types of intervention.
Read more on Pregnancy, Birth & Baby website
Causes - Miracle Babies
Every year in Australia around 48,000 newborn babies require the help of a NICU or SCN, there are many factors linked to premature birth and also many that remain unexplained
Read more on Miracle Babies Foundation website
Shoulder dystocia
Shoulder dystocia happens when a baby's shoulder gets stuck behind the mother’s pubic bone during birth.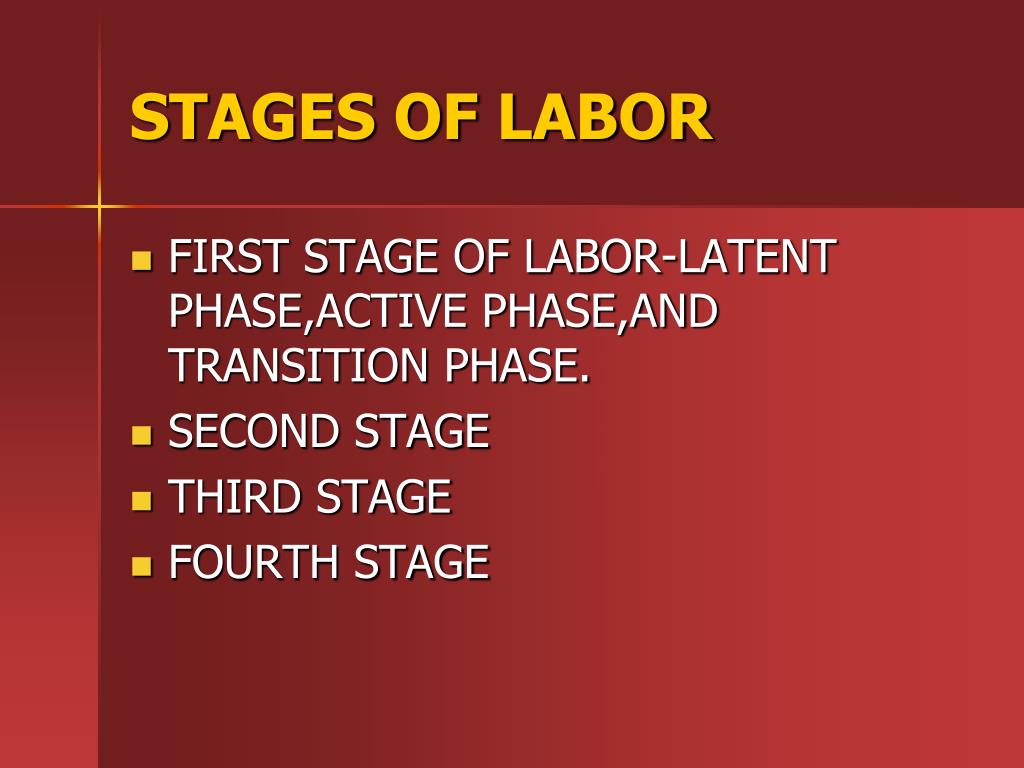 It is a medical emergency that requires immediate intervention. Find out why here.
It is a medical emergency that requires immediate intervention. Find out why here.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.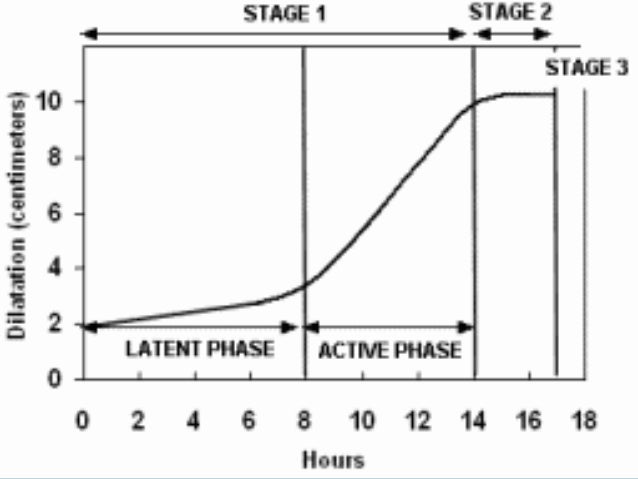
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.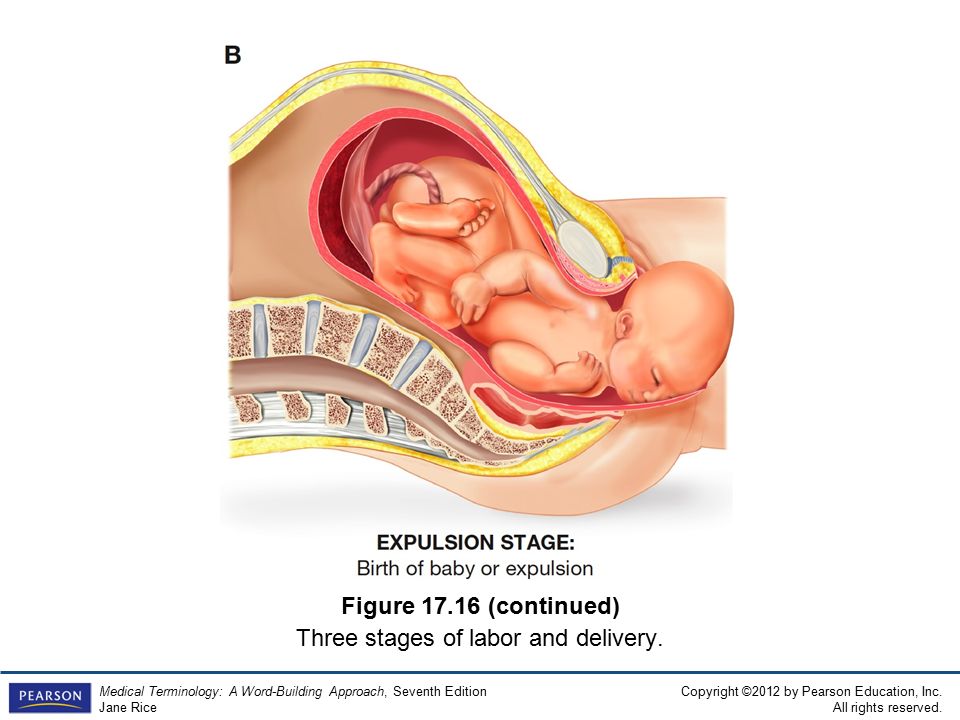
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Active management of the third stage of labor: A brief overview of key issues
1. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin: Clinical Management Guidelines for Obstetrician-Gynecologists Number 76, October 2006: postpartum hemorrhage. Obstet Gynecol. 2006;108:1039–47. [PubMed] [Google Scholar]
2. Rath WH. Postpartum hemorrhage- update on problems of definitions and diagnosis. Acta Obstet Gynecol Scand. 2011;90:421–28. [PubMed] [Google Scholar]
Rath WH. Postpartum hemorrhage- update on problems of definitions and diagnosis. Acta Obstet Gynecol Scand. 2011;90:421–28. [PubMed] [Google Scholar]
3. World Health Organization. WHO guidelines for the management of postpartum haemorrhage and retained placenta. Geneva: World Health Organization. 2009 [Google Scholar]
4. Royal College of Obstetrician and Gynaecologists. Postpartum Hemorrhage: Prevention and Management. 2011 [Google Scholar]
5. Zhu C, Estrada M, White J, Lal M. Heat-stable sublingual oxytocin tablets as a potential needle-free approach for preventing postpartum hemorrhage in low-resource settings. Drug Deliv Transl Res. 2018;8:853–6. [PMC free article] [PubMed] [Google Scholar]
6. Oguz Orhan E, Dilbaz B, Aksakal SE, Altınbas S, Erkaya S. Prospective randomized trial of oxytocin administration for active management of the third stage of labor. Int J Gynecol Obstet. 2014;127:175–9. [PubMed] [Google Scholar]
7. Güngördük K, Asicioglu O, Besimoglu B, Güngördük OC, Yildirm G, Ark C, et al. Using intraumbilical vein injection of oxytocin in routine practice with active management of the third stage of labor: a randomized controlled trial. Obstet Gynecol. 2010;116:619–24. [PubMed] [Google Scholar]
Using intraumbilical vein injection of oxytocin in routine practice with active management of the third stage of labor: a randomized controlled trial. Obstet Gynecol. 2010;116:619–24. [PubMed] [Google Scholar]
8. Gohil JT, Tripathi B. A Study to Compare the Efficacy of Misoprostol, Oxytocin, Methyl-ergometrine and Ergometrine-Oxytocin in Reducing Blood Loss in Active Management of 3rd Stage of Labor. J Obstet Gynaecol India. 2011;61:408–12. [PMC free article] [PubMed] [Google Scholar]
9. McDonald SJ, Abbott JM, Higgins SP. Prophylactic ergometrine-oxytocin versus oxytocin for the third stage of labour. Cochrane Database Syst Rev. 2004:CD000201. [PMC free article] [PubMed] [Google Scholar]
10. Mobeen N, Durocher J, Zuberi N, Jahan N, Blum J, Wasim S, et al. Administration of misoprostol by trained traditional birth attendants to prevent postpartum haemorrhage in homebirths in Pakistan: a randomised placebo-controlled trial. BJOG. 2011;118:353–61. [PMC free article] [PubMed] [Google Scholar]
11. Gulmezoglu AM, Villar J, Ngoc NT, Piaggio G, Carroli G, Adetoro L, et al. WHO multicentre randomised trial of misoprostol in the management of the third stage of labour. Lancet. 2001;358:689–95. [PubMed] [Google Scholar]
Gulmezoglu AM, Villar J, Ngoc NT, Piaggio G, Carroli G, Adetoro L, et al. WHO multicentre randomised trial of misoprostol in the management of the third stage of labour. Lancet. 2001;358:689–95. [PubMed] [Google Scholar]
12. Tuncalp Ö, Hofmeyr GJ, Gülmezoglu AM. Prostaglandins for preventing postpartum haemorrhage. Cochrane Database Syst Rev. 2012:CD000494. [PMC free article] [PubMed] [Google Scholar]
13. WHO. Recommendations for the Prevention and Treatment of Postpartum Haemorrhage. Geneva: World Health Organization. 2012 [Google Scholar]
14. Tan J, Cao Q, He GL, Cai YH, Yu JJ, Sun X, et al. Misoprostol versus ergometrine-oxytocin for preventing postpartum haemorrhage: a systematic review and meta-analysis of randomized controlled trials. J Evid Based Med. 2016;9:194–204. [PubMed] [Google Scholar]
15. Hernández-Castro F, López-Serna N, Treviño-Salinas EM, Soria-López JA, Sordia-Hernández LH, Cárdenas-Estrada E. Randomized double-blind placebo-controlled trial of buccal misoprostol to reduce the need for additional uterotonic drugs during cesarean delivery. Int J Gynaecol Obstet. 2016;132:184–7. [PubMed] [Google Scholar]
Int J Gynaecol Obstet. 2016;132:184–7. [PubMed] [Google Scholar]
16. Sentilhes L, Lasocki S, Ducloy-Bouthors AS, Deruelle P, Dreyfus M, Perrotin F, et al. Tranexamic acid for the prevention and treatment of postpartum haemorrhage. Br J Anaesth. 2015;114:576–87. [PubMed] [Google Scholar]
17. Draxler DF, Medcalf RL. The Fibrinolytic System-More Than Fibrinolysis? Transfus Med Rev. 2015;29:102–9. [PubMed] [Google Scholar]
18. Tengborn L, Blombäck M, Berntorp E. Tranexamic acid--an old drug still going strong and making a revival. Thromb Res. 2015;135:231–42. [PubMed] [Google Scholar]
19. Hinshaw K. Tranexamic acid for post-partum haemorrhage in the WOMAN trial. Lancet. 2017;390:1582–3. [PubMed] [Google Scholar]
20. Li B, Miners A, Shakur H, Roberts I WOMAN Trial Collaborators. Tranexamic acid for treatment of women with post-partum haemorrhage in Nigeria and Pakistan: a cost-effectiveness analysis of data from the WOMAN trial. Lancet Glob Health. 2018;6:222–8.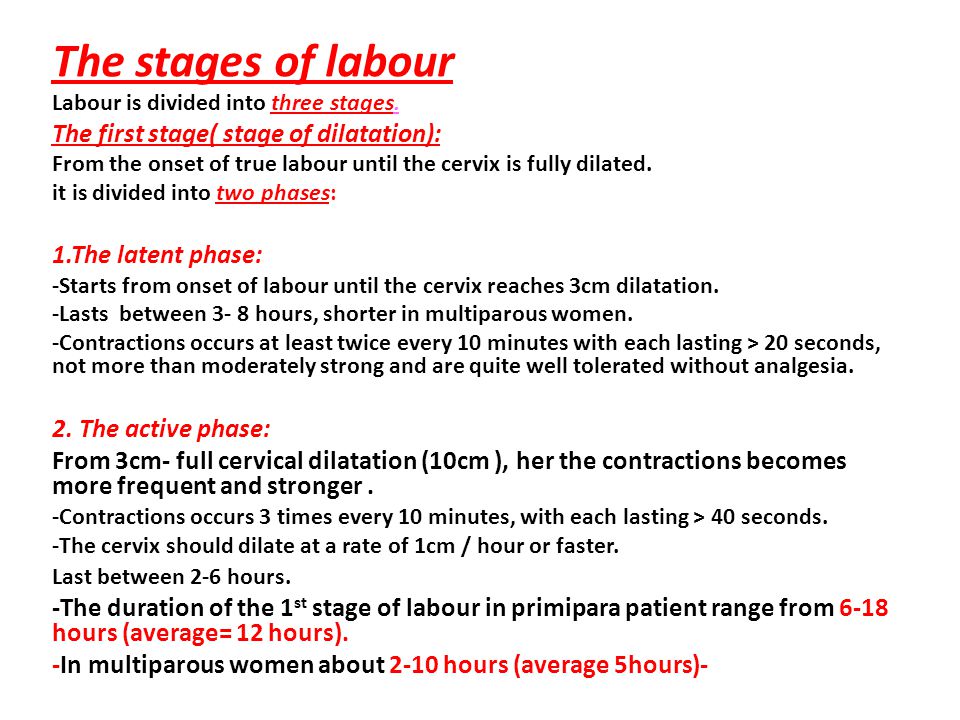 [PMC free article] [PubMed] [Google Scholar]
[PMC free article] [PubMed] [Google Scholar]
21. Gai M, Wu L, Su Q, Tatsumoto K. Clinical observation of blood loss reduced by tranexamic acid during and after caesarean section: a multi-center, randomized trial. Eur J Obstet Gynecol Reprod Biol. 2004;112:154–7. [PubMed] [Google Scholar]
22. Mayur G, Purvi P, Ashoo G, Pankaj D. Efficacy of tranexamic acid in decreasing blood loss during and after caesarean section: a randomized case controlled prospective study. J Obstet Gynecol India. 2007;57:227–30. [Google Scholar]
23. Sekhavat L, Tabatabaii A, Dalili M, Farajkhoda T, Tafti AD. Efficacy of tranexamic acid in reducing blood loss after caesarean section. J Matern Fetal Neonatal Med. 2009;22:72–5. [PubMed] [Google Scholar]
24. Gungorduk K, Yıldırım G, Asıcıoğlu O, Gungorduk OC, Sudolmus S, Ark C. Efficacy of intravenous tranexamic acid in reducing blood loss after elective cesarean section: a prospective, randomized, double-blind, placebo-controlled study. Am J Perinatol.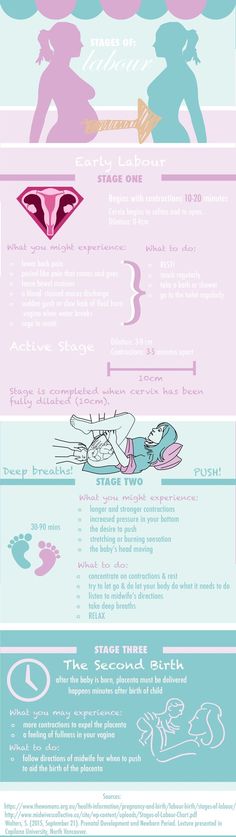 2011;28:233–40. [PubMed] [Google Scholar]
2011;28:233–40. [PubMed] [Google Scholar]
25. Movafegh A, Eslamian L, Dorabadi A. Effect of intravenous tranexamic acid administration on blood loss during and after caesarean delivery. Int J Gynecol Obstet. 2011;115:224–6. [PubMed] [Google Scholar]
26. Xu J, Ju Y. Tranexamic acid for the prevention of postpartum haemorrhage after caesarean section: a double-blind randomization trial. Arch Gynecol Obstet. 2013;287:463–8. [PubMed] [Google Scholar]
27. Sentürk MB, Cakmak Y, Yildiz G, Yildiz P. Tranexamic acid for caesarean section: a double-blind, placebo-controlled, randomized clinical trial. Arch Gynecol Obstet. 2013;287:641–5. [PubMed] [Google Scholar]
28. Shahid A, Khan A. Tranexamic acid in decreasing blood loss during and after caesarean section. J Coll Physicians Surg. 2013;23:459–62. [PubMed] [Google Scholar]
29. Abdel-Aleem H, Alhusaini TK, Abdel-Aleem MA, Menoufy M, Gülmezoglu AM. Effectiveness of tranexamic acid on blood loss in patients undergoing elective caesarean section: randomized clinical trial.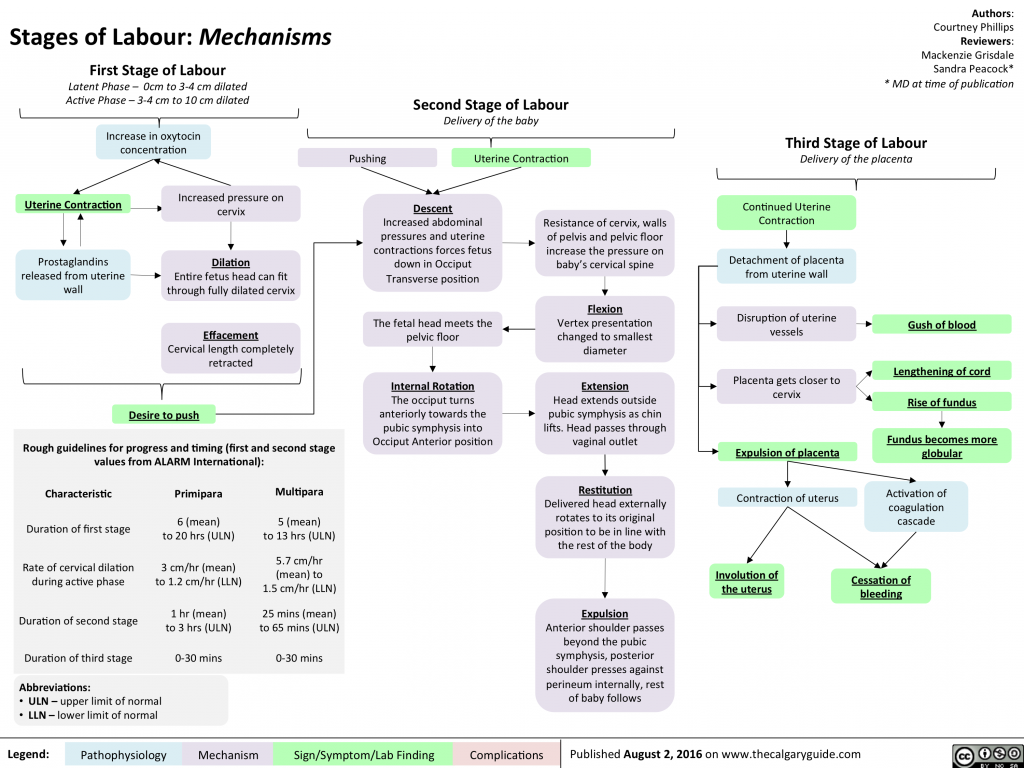 J Matern Fetal Neonatal Med. 2013;26:1705–9. [PubMed] [Google Scholar]
J Matern Fetal Neonatal Med. 2013;26:1705–9. [PubMed] [Google Scholar]
30. Goswami U, Sarangi S, Gupta S, Babbar S. Comparative evaluation of two doses of tranexamic acid used prophylactically in anemic parturients for lower segment caesarean section: A double-blind randomized case control prospective trial. Saudi J Anaesth. 2013;7:427–31. [PMC free article] [PubMed] [Google Scholar]
31. Ahmed MR, Sayed Ahmed WA, Madny EH, Arafa AM, Said MM. Efficacy of tranexamic acid in decreasing blood loss in elective caesarean delivery. J Matern Fetal Neonatal Med. 2015;28:1014–8. [PubMed] [Google Scholar]
32. Yang H, Zheng S, Shi C. Clinical study on the efficacy of tranexamic acid in reducing postpartum blood lose: a randomized, comparative, multicenter trial. Zhonghua Fu Chan Ke Za Zhi. 2001;36:590–2. [PubMed] [Google Scholar]
33. Mirghafourvand M, Mohammad-Alizadeh S, Abbasalizadeh F, Shirdel M. The effect of prophylactic intravenous tranexamic acid on blood loss after vaginal delivery in women at low risk of postpartum haemorrhage: a double-blind randomised controlled trial.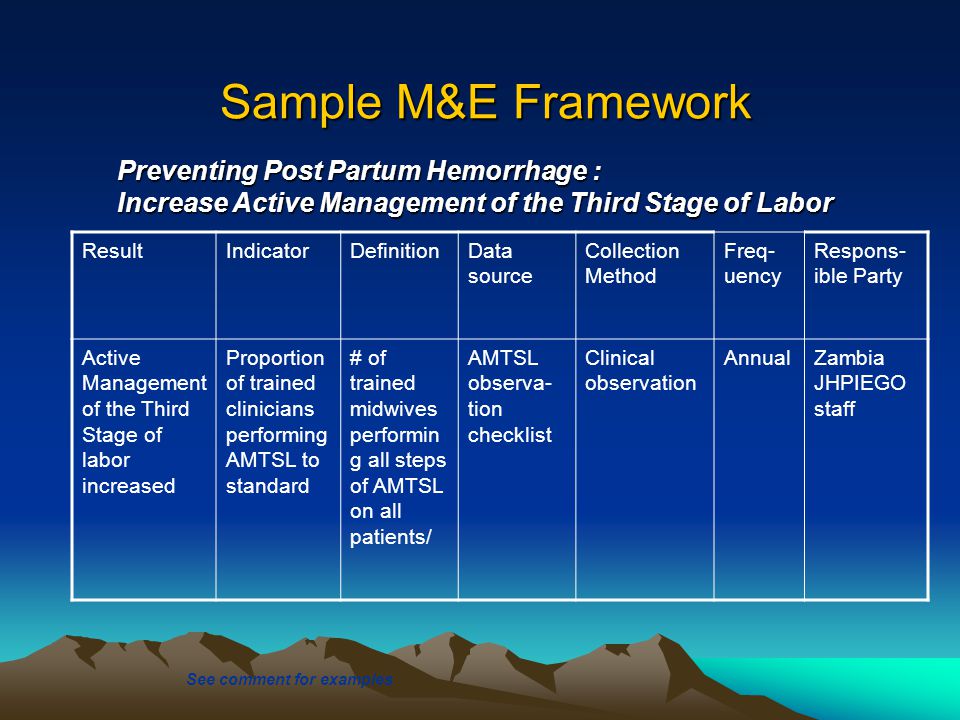 Aust N Z J Obstet Gynaecol. 2015;55:53–8. [PubMed] [Google Scholar]
Aust N Z J Obstet Gynaecol. 2015;55:53–8. [PubMed] [Google Scholar]
34. Ducloy-Bouthors AS, Jude B, Duhamel A, Huissoud C, Keita-Meyer H, Mandelbrot L, et al. High-dose tranexamic acid reduces blood loss in postpartum haemorrhage. Crit Care. 2011;15:117. [PMC free article] [PubMed] [Google Scholar]
35. Gungorduk K, Asıcıoglu O, Yıldırım G, Ark C, Tekirdag Aİ, Besımoglu B. Can intravenous injection of tranexamic acid be used in routine practice with active management of the third stage of labor in vaginal delivery? A randomized controlled study. Am J Perinatol. 2013;230:407–13. [PubMed] [Google Scholar]
36. Hofmeyr GJ, Mshweshwe NT, Gülmezoglu AM. Controlled cord traction for the third stage of labour. Cochrane Database Syst Rev. 2015;1:CD008020. [PMC free article] [PubMed] [Google Scholar]
37. Güngördük K, Asicioglu O, Celikkol O, Olgac Y, Ark C. Use of additional oxytocin to reduce blood loss at elective caesarean section: A randomised control trial. Austr N Z J Obstet Gynaecol. 2010;50:36–9. [PubMed] [Google Scholar]
2010;50:36–9. [PubMed] [Google Scholar]
38. Chen M, Chang Q, Duan T, He J, Zhang L, Liu X. Uterine massage to reduce blood loss after vaginal delivery: a randomized controlled trial. Obstet Gynecol. 2013;122:290–5. [PubMed] [Google Scholar]
39. Begley CM, Gyte GM, Devane D, McGuire W, Weeks A. Active versus expectant management for women in the third stage of labour. Cochrane Database of Syst Rev. 2015:CD007412. [PubMed] [Google Scholar]
Important to know - Health of a Petersburger
The total duration of childbirth and their course
The total duration of childbirth depends on many factors: age, physique and physical condition of the woman, her psychological mood, the speed of cervical dilatation, first pregnancy or repeated, the size of the child, the type of presentation and a number of other points.
Labor activity proceeds differently for all women, but the main periods of childbirth are clearly distinguished: 1st period - the period of contractions, the longest and most intense, 2nd period - the direct birth of a baby, 3rd period - the birth of the afterbirth (placenta).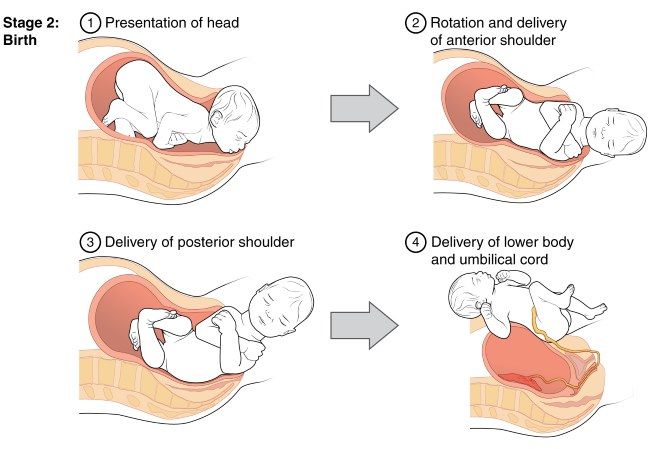
First stage of labor (opening period)
As the name implies, during this period there is a gradual opening of the cervix as a result of regular contractions of the uterine muscles. Contractions occur with a decreasing interval, but they themselves become longer and more frequent.
The dilation period is the time elapsed from the onset of regular contractions until the cervix is fully dilated. During this period, the birth canal is prepared for the passage of the fetus through them with all the fetal formations.
Cervical dilatation occurs gradually: at first the cervix is smoothed out, then the pharynx opens up to 3-4 cm and at the end of the first stage of labor up to 10 cm. This is already a complete dilatation of the cervix. With it, during contractions, the fetal bladder becomes tense and bursts at the height of one of them, the anterior portion of amniotic fluid is poured out.
The first stage of labor is the longest and consists of three phases:
1. Latent phase (lasts 5-6 hours). It is characterized by the establishment of regular contractions, with an interval between them of 10-15 minutes. Latent, or hidden, this phase is called because the contractions of the uterus during it are painless or slightly painful. By the end of the phase, the cervix is definitively flattened and opens about 4 cm.
Latent phase (lasts 5-6 hours). It is characterized by the establishment of regular contractions, with an interval between them of 10-15 minutes. Latent, or hidden, this phase is called because the contractions of the uterus during it are painless or slightly painful. By the end of the phase, the cervix is definitively flattened and opens about 4 cm.
2. Active phase (lasts 3-4 hours). Contractions become more intense, last at least 20 seconds, and the interval between them is reduced to 5-6 minutes. Normally, during the active phase, amniotic fluid is poured out, which contributes to a faster full disclosure of the uterine pharynx. By the end of the phase, the uterus opens by 8 cm. This phase is not always clearly manifested, but it is nevertheless distinguished due to the usual weakening of contractions during disclosure from 8 to 10 cm. The child's head descends and stands in the narrow part of the small pelvis, which necessitates a slower and smoother process. Already in the transitional phase, the woman in labor feels the desire to push, to push the baby out. But in order for the head to pass through the birth canal without the risk of injury, it is necessary to achieve cervical dilatation up to 10 cm.
But in order for the head to pass through the birth canal without the risk of injury, it is necessary to achieve cervical dilatation up to 10 cm.
Second stage of labor (exile period)
The period of exile is the time from the moment of full opening of the pharynx until the birth of the fetus.
It is the second stage of childbirth that is their culmination, because for a short time (compared to contractions) the long-awaited birth of the baby takes place.
After the discharge of amniotic fluid, contractions temporarily stop. The volume of the uterine cavity decreases, the uterine cavity and vagina appear as a single birth canal. Contractions reappear and become more intense. They are joined by attempts - contractions of the muscle press (abdominal wall, diaphragm and pelvic floor). The frequency and intensity of contractions and attempts are constantly increasing. The head descends and compresses the nerves of the sacral plexus. A woman has a strong desire to squeeze the head out of the birth canal, she is looking for supports for her arms and legs to strengthen her efforts.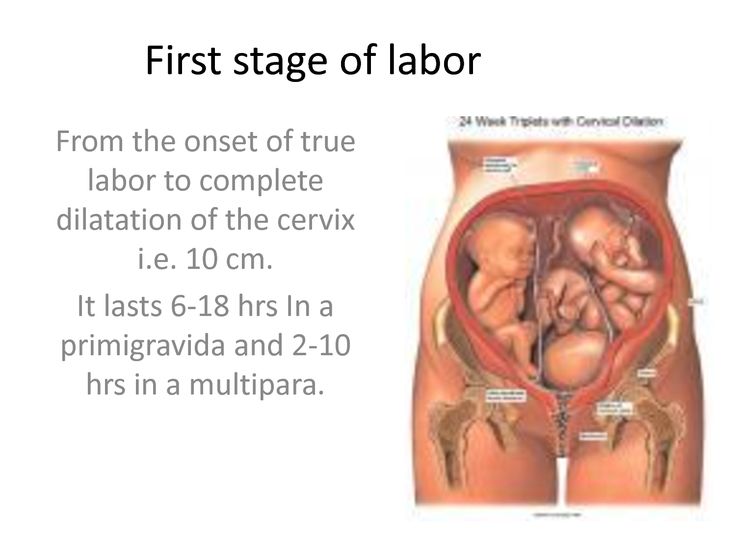
Pushing is a lot of physical work. During attempts, a woman experiences maximum physical stress (blood pressure rises, pulse and respiration become more frequent). During the attempts, the woman holds her breath, and in the intervals between them she rests and "gathers her strength for a new attempt."
In the process of one of the attempts, the head is born. Next, the shoulders are born (first the front, then the back) and the torso. Following the fetus, the posterior amniotic fluid is poured out with an admixture of cheese-like lubricant.
A woman in labor, having experienced severe fatigue, rests after hard work (pulse and respiration rate decrease).
Third stage of labor (postpartum period).
The afterbirth period is the time from the birth of the fetus to the birth of the placenta. During this period, the placenta separates from the walls of the uterus and the birth of the placenta (placenta with membranes and umbilical cord).
In the process of separation of the placenta from the walls of the uterus, the uteroplacental vessels are damaged, which is normally accompanied by blood loss in the amount of 100-200 ml, without adversely affecting the woman's condition.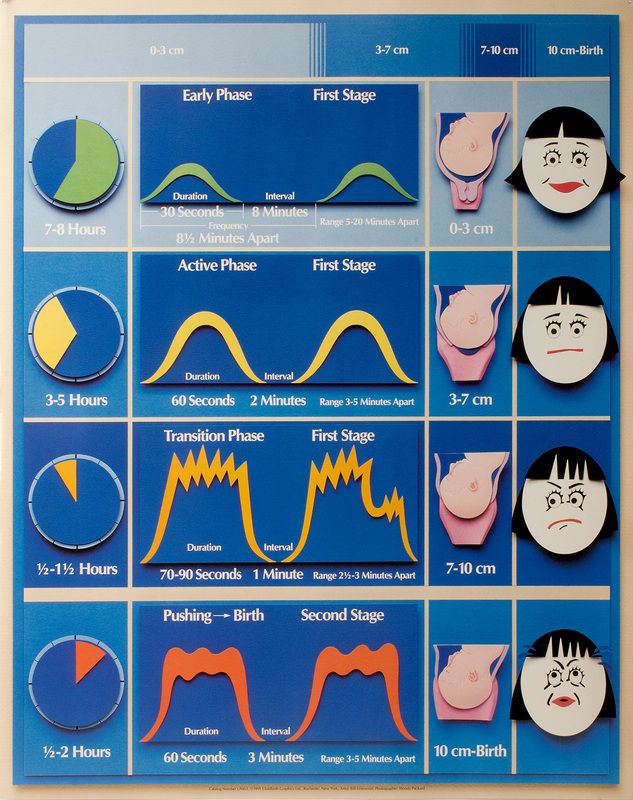 After the birth of the placenta, the uterus contracts sharply, becomes dense, which is necessary to stop bleeding in the area of the placental site; its bottom is in the middle between the womb and the navel.
After the birth of the placenta, the uterus contracts sharply, becomes dense, which is necessary to stop bleeding in the area of the placental site; its bottom is in the middle between the womb and the navel.
During this period, the woman's pulse and respiration normalize. Her demeanor is calm. Chills can sometimes be observed (as a reaction to the transferred strong physical stress).
The third period is no longer as exciting and tense as the previous two. The child was born and the matter remains for the small - the separation of the placenta, or placenta. Nature provides for the resumption of contractions a few minutes after the birth of the baby, necessary for effective exfoliation from the uterus of tissues that nourished the fetus during pregnancy (placenta, membranes, umbilical cord).
Three periods of physiological labor - the natural end of a nine-month wait. Most likely, during the birth process itself, the woman in labor will not care what the period or phase of childbirth is now, but it is still desirable to know about them, at least for greater certainty before going to the hospital.
Sitemap
State Autonomous Professional
educational institution
Republic of Bashkortostan
Salavat Medical College
453261 Republic of Bashkortostan
Salavat, st. Furmanova, 4
Phone/fax: (3476)-38-78-83
e-mail: [email protected]
- College Information
- Basic information
- Structure and governing bodies of the college
- Documents
- Education
- Educational standards and requirements
- Manual. Teaching staff
- Logistics and equipment of the educational process
- Scholarships and other financial support
- Paid educational services
- Financial and economic activities
- Vacancies for reception (transfer)
- Personal data processing
- Anti-corruption
- Legal framework for combating extremism and terrorism
- Vacancies
- Information security
- Olympics
- Mentoring
- Available environment
- International cooperation
- Applicant
- Applicant
- Control figures for the reception of citizens
- Admission Rules
- Individual Achievement Regulations
- Local regulations
- List of specialties
- Document acceptance schedule
- Terms of admission under contracts for the provision of paid educational services
- Information on the need for applicants to undergo a mandatory preliminary medical examination (examination)
- Exemplary entrance tests
- Features of conducting entrance examinations for the disabled and persons with disabilities
- Information about the possibility of filing documents by mail
- Submission of documents by e-mail
- List and deadlines for submission of documents
- Information on the availability of a hostel and the number of places in hostels allocated for nonresident applicants
- Enrollment Orders
- Number of applications submitted
- Filing and reviewing appeals
- College Application
- Citizens' appeal on admission issues
- Targeted training
- Consent to the processing of personal data
- Entrance examinations
- Rating of applicants
- student
- Fundamentals
- Regulations
- Culture and sports
- Dormitory
- Student Council
- Life safety
- Teaching materials
- Employment of graduates
- Graduate Accreditation
- Page of educational psychologist
- Student Union
- Scholarship of the Head of the Republic of Bashkortostan
- teacher
- Reference information
- Educational work
- Additional education
- Republican information and training pedagogical seminars
- Contacts
- Hotline
- Feedback
- Contacts of controlling organizations
This page does not exist.