What is the most common neural tube defect
Neural Tube Defects | MedlinePlus
On this page
Basics
- Summary
- Start Here
- Diagnosis and Tests
- Prevention and Risk Factors
- Treatments and Therapies
Learn More
- Related Issues
- Specifics
- Genetics
See, Play and Learn
- No links available
Research
- Statistics and Research
- Clinical Trials
- Journal Articles
Resources
- Find an Expert
For You
- Patient Handouts
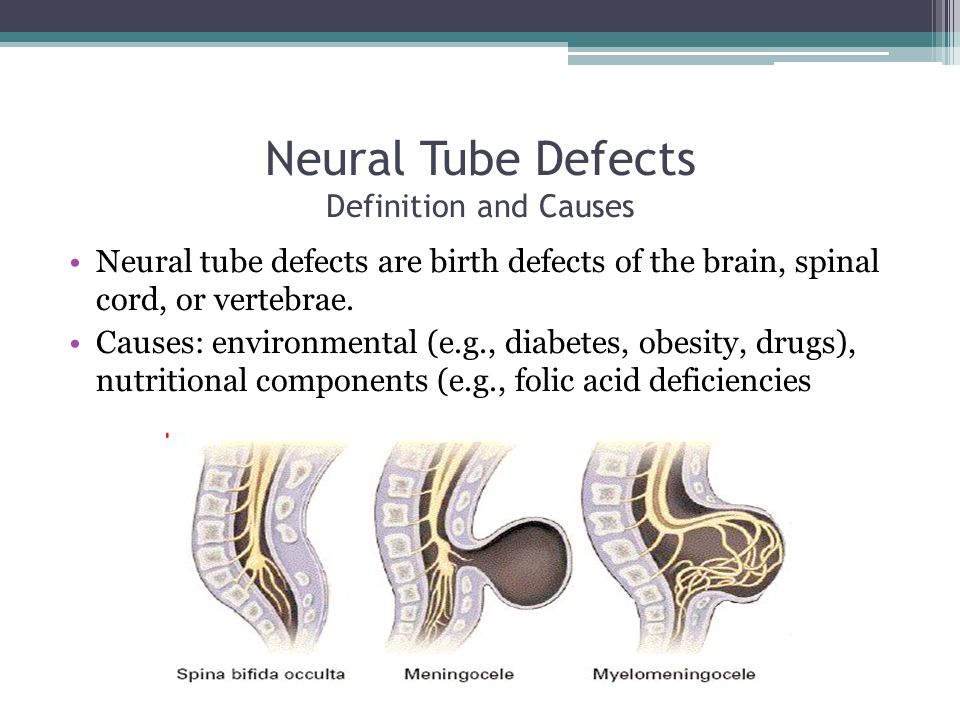
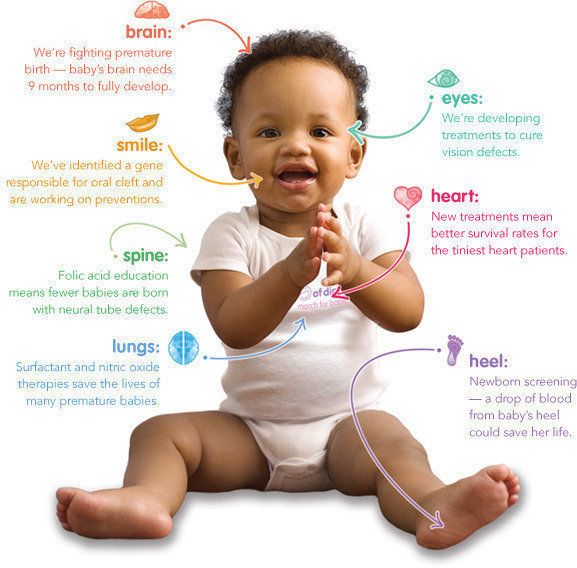
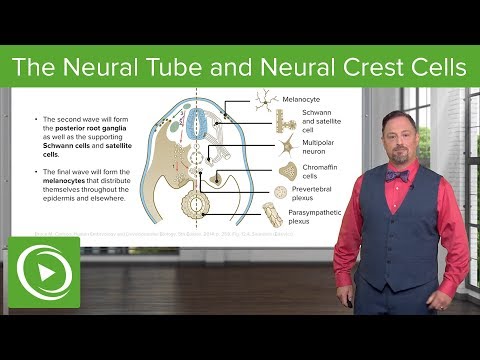
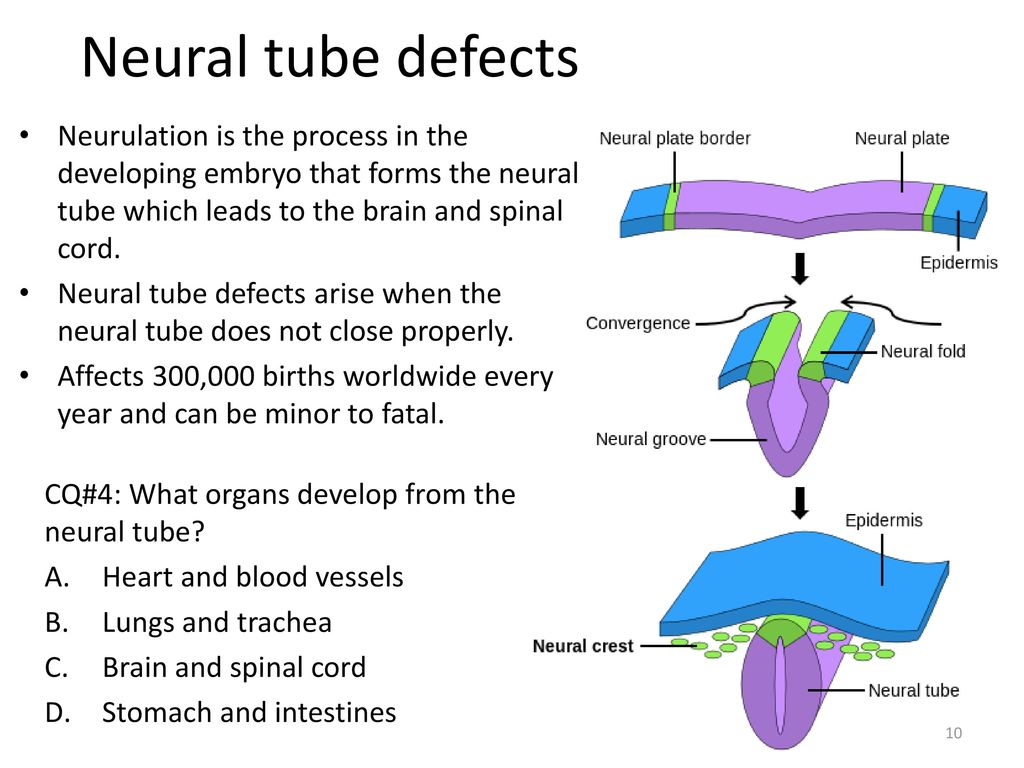
Neural tube defects are birth defects of the brain, spine, or spinal cord. They happen in the first month of pregnancy, often before a woman even knows that she is pregnant. The two most common neural tube defects are spina bifida and anencephaly. In spina bifida, the fetal spinal column doesn't close completely. There is usually nerve damage that causes at least some paralysis of the legs. In anencephaly, most of the brain and skull do not develop. Babies with anencephaly are usually either stillborn or die shortly after birth. Another type of defect, Chiari malformation, causes the brain tissue to extend into the spinal canal.
The exact causes of neural tube defects aren't known. You're at greater risk of having an infant with a neural tube defect if you:
- Have obesity
- Have poorly controlled diabetes
- Take certain antiseizure medicines
Getting enough folic acid, a type of B vitamin, before and during pregnancy prevents most neural tube defects.
Neural tube defects are usually diagnosed before the infant is born, through lab or imaging tests.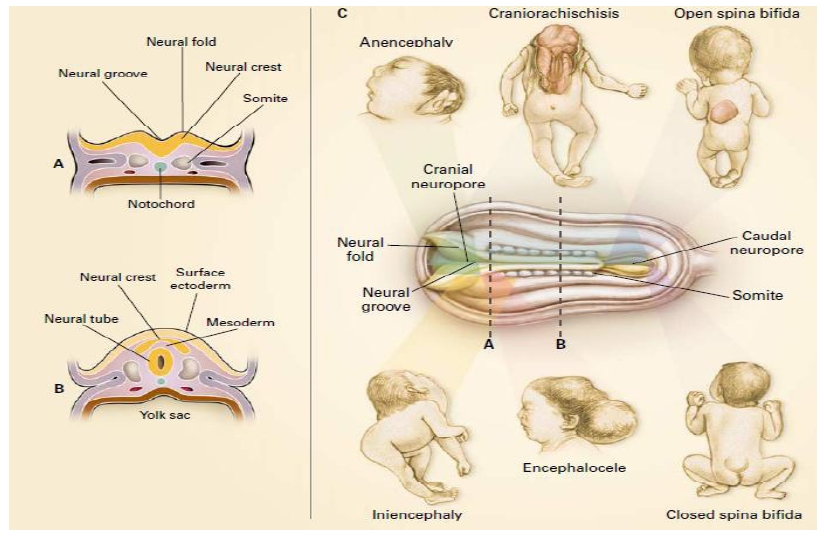 There is no cure for neural tube defects. The nerve damage and loss of function that are present at birth are usually permanent. However, a variety of treatments can sometimes prevent further damage and help with complications.
There is no cure for neural tube defects. The nerve damage and loss of function that are present at birth are usually permanent. However, a variety of treatments can sometimes prevent further damage and help with complications.
NIH: National Institute of Child Health and Human Development
- About Neural Tube Defects (NTDs) (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- Neural Tube Defects (March of Dimes Birth Defects Foundation)
- Alpha-fetoprotein (AFP) Test (National Library of Medicine) Also in Spanish
- How Do Health Care Providers Diagnose Neural Tube Defects (NTDs)? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- What Are the Treatments for Neural Tube Defects (NTDs)? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- Are There Disorders or Conditions Associated with Neural Tube Defects (NTDs)? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- Anencephaly (National Institute of Neurological Disorders and Stroke)
- Cephalic Disorders (National Institute of Neurological Disorders and Stroke) Also in Spanish
- Cephalic Disorders (National Institute of Neurological Disorders and Stroke) - Short Summary
- Encephaloceles (National Institute of Neurological Disorders and Stroke)
- Facts about Anencephaly (Centers for Disease Control and Prevention) Also in Spanish
- Facts about Encephalocele (Centers for Disease Control and Prevention) Also in Spanish
- Hydranencephaly (National Institute of Neurological Disorders and Stroke)
- Iniencephaly (National Institute of Neurological Disorders and Stroke)
- Tethered Spinal Cord Syndrome (National Institute of Neurological Disorders and Stroke)
- How Many People Are at Risk for Neural Tube Defects (NTDs)? (Eunice Kennedy Shriver National Institute of Child Health and Human Development) Also in Spanish
- ClinicalTrials.
 gov: Anencephaly (National Institutes of Health)
gov: Anencephaly (National Institutes of Health) - ClinicalTrials.gov: Arnold-Chiari Malformation (National Institutes of Health)
- ClinicalTrials.
 gov: Neural Tube Defects (National Institutes of Health)
gov: Neural Tube Defects (National Institutes of Health)
- Article: Prenatal assessment and pregnancy outcomes of foetal low-lying conus medullaris using.
 ..
.. - Article: Aetiology and diagnostics of paediatric hydrocephalus across Africa: a systematic review...
- Article: Analysis of DNMT1 gene variants in progression of neural tube defects-an.
 ..
.. - Neural Tube Defects -- see more articles
- Eunice Kennedy Shriver National Institute of Child Health and Human Development Also in Spanish
- Find a Genetic Counselor (National Society of Genetic Counselors)
- Find a Pediatrician or Pediatric Specialist (American Academy of Pediatrics) Also in Spanish
- March of Dimes Birth Defects Foundation Also in Spanish
- National Institute of Neurological Disorders and Stroke Also in Spanish
What They Are, Causes & Prevention
Overview
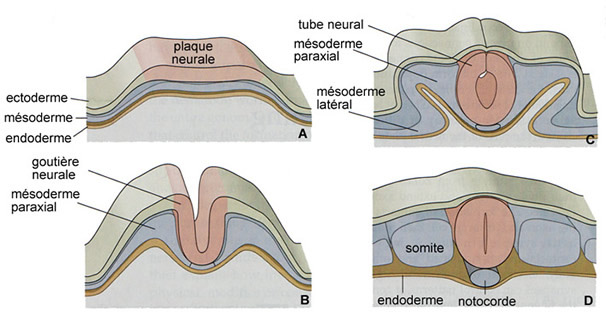
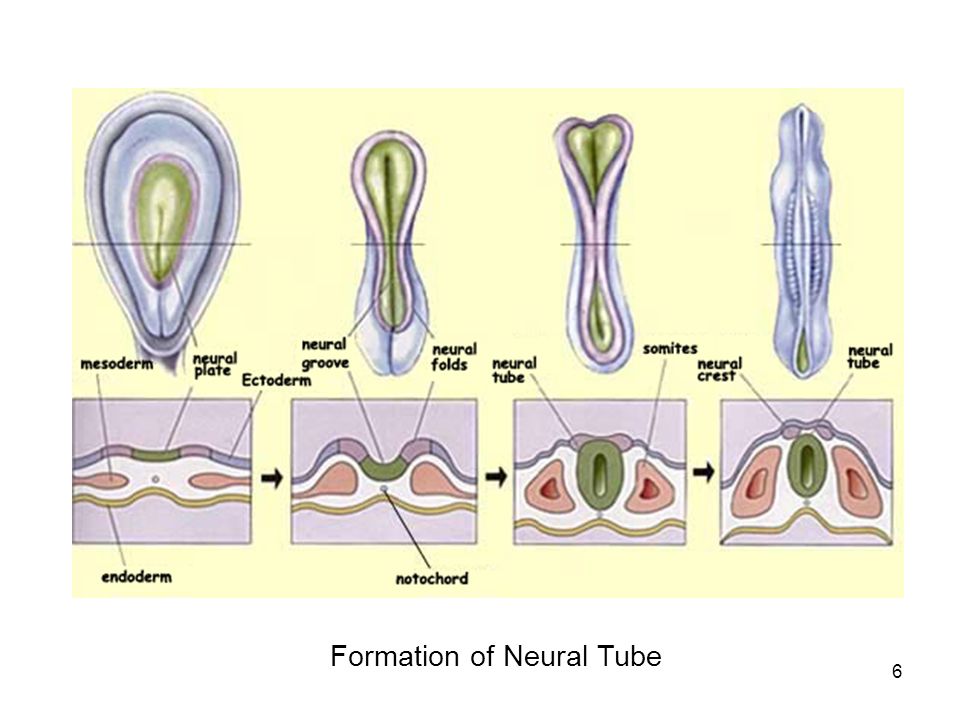
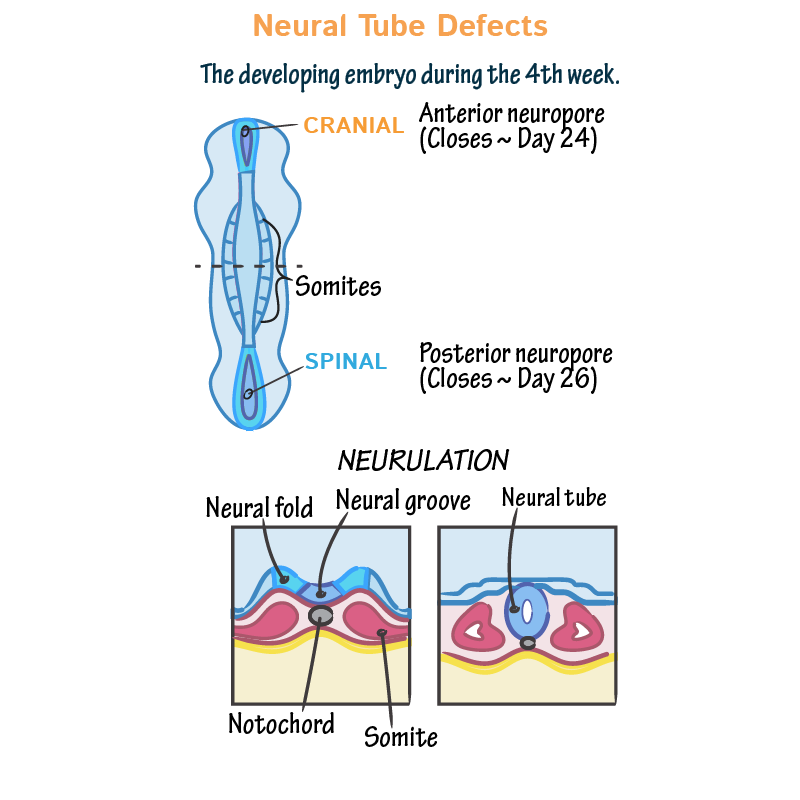
Neural tube defects (NTDs) happen to developing fetuses within the first month of pregnancy.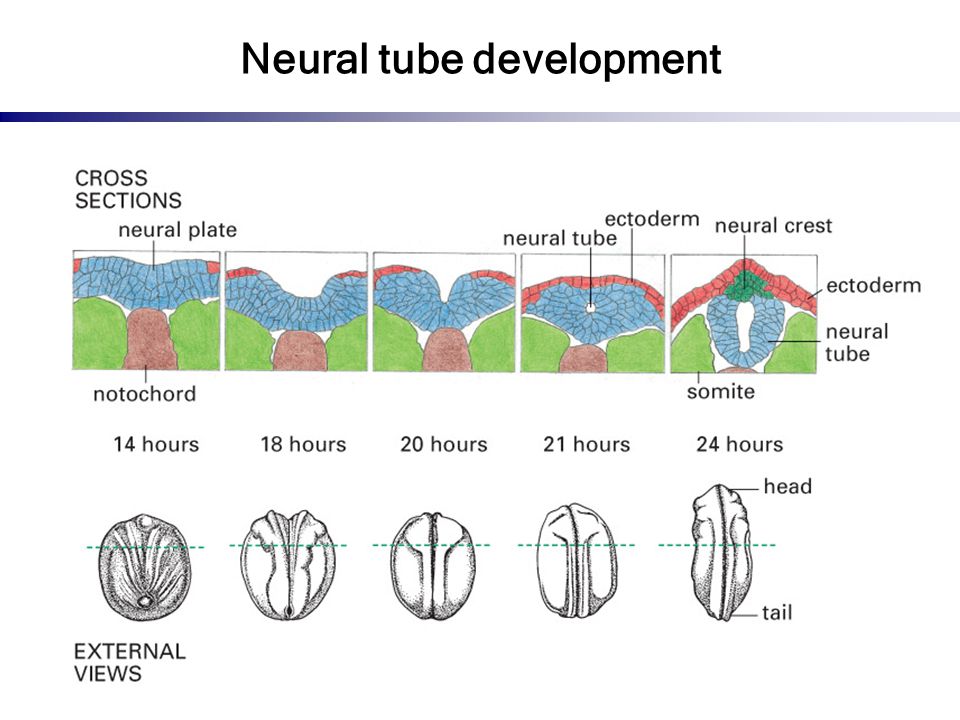 An NTD happens when the neural tube doesn’t close completely somewhere along its length.
An NTD happens when the neural tube doesn’t close completely somewhere along its length.What is a neural tube defect?
Neural tube defects (NTDs) are birth defects (congenital conditions) of the brain, spine or spinal cord. They happen to developing fetuses within the first month of pregnancy — often before you even know you’re pregnant. The two most common neural tube defects are spina bifida and anencephaly.
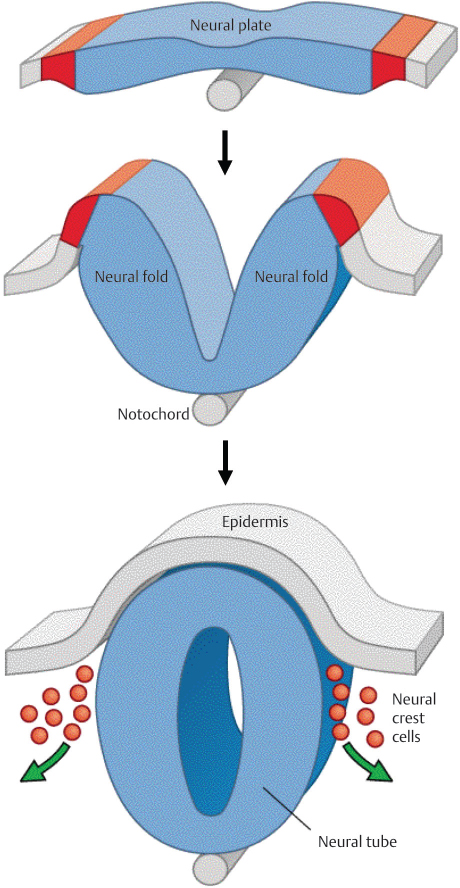
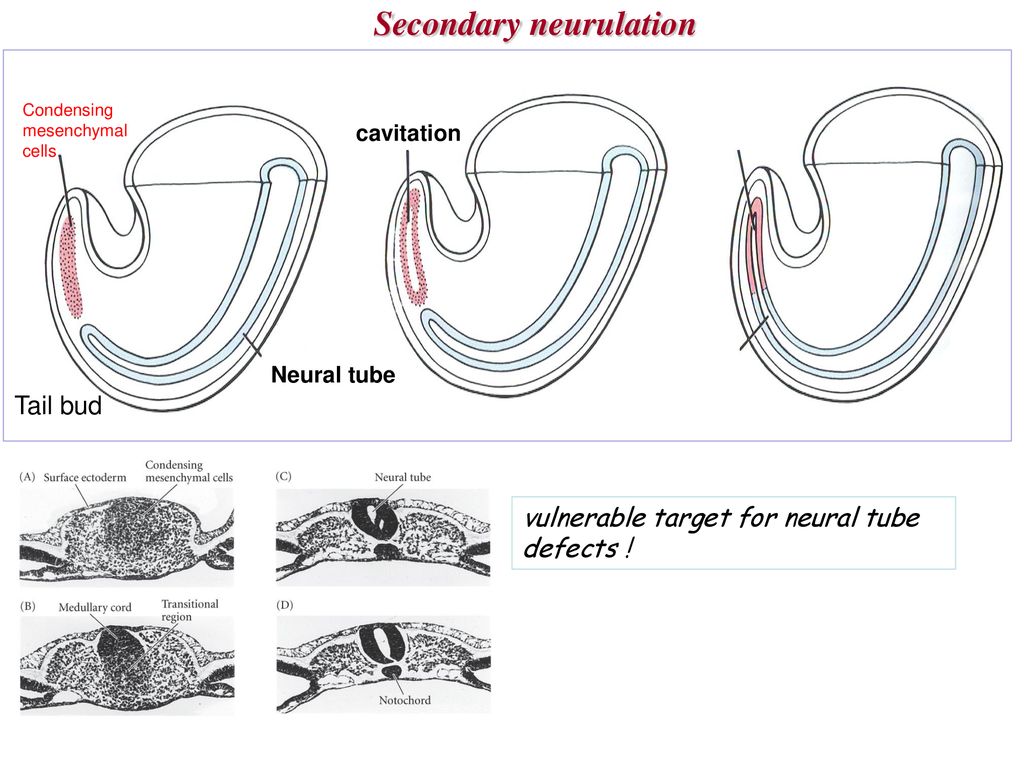
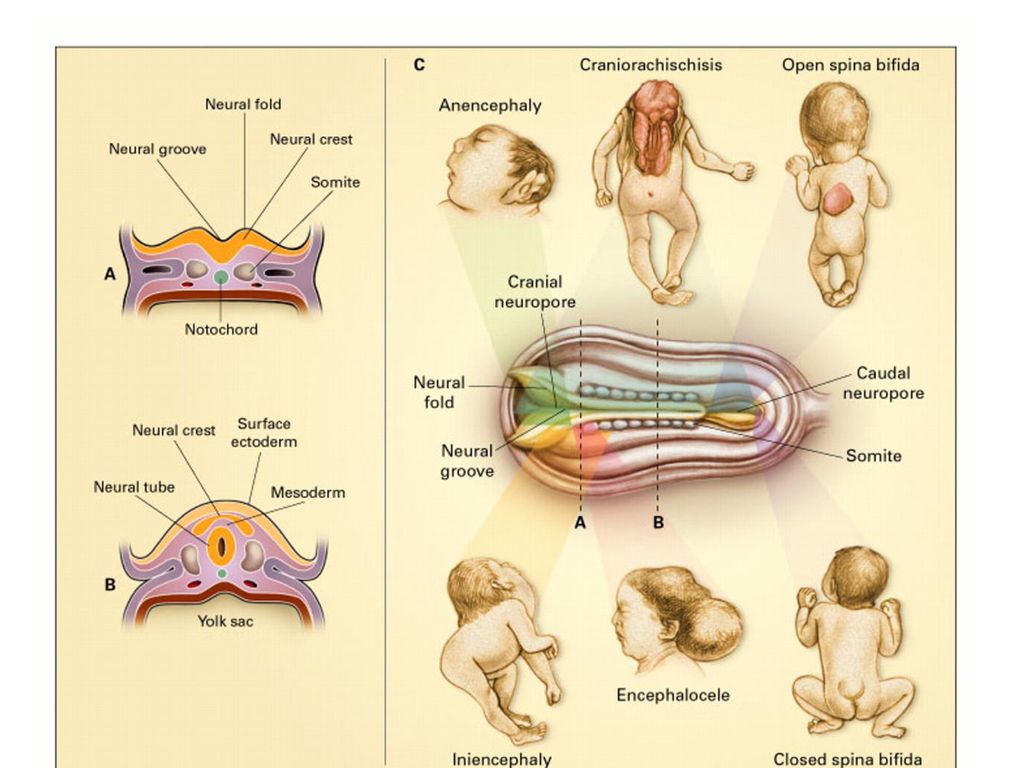
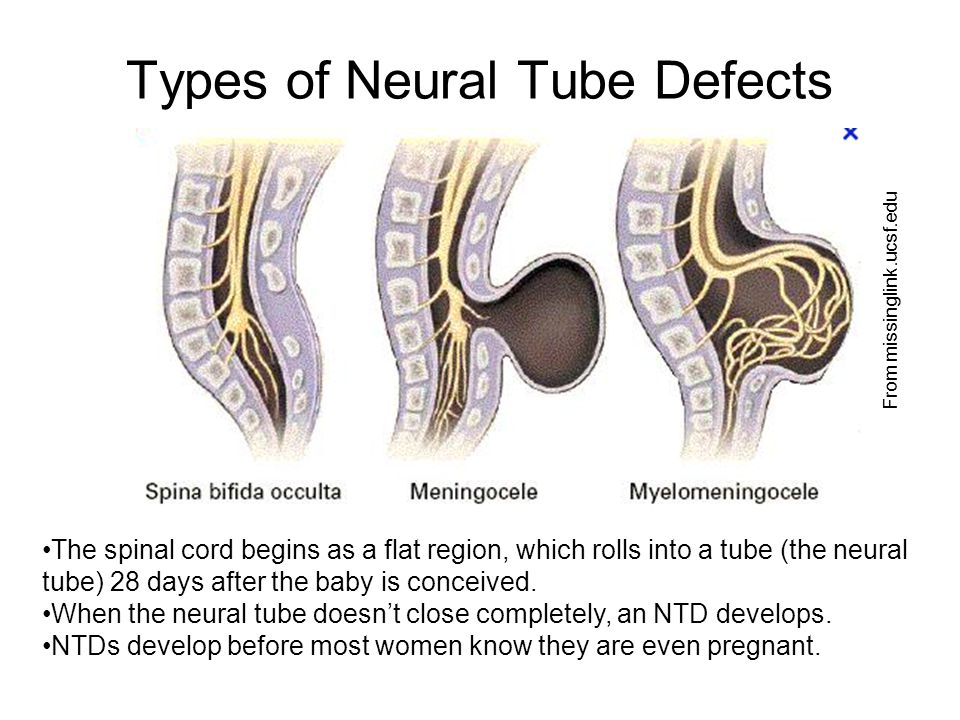
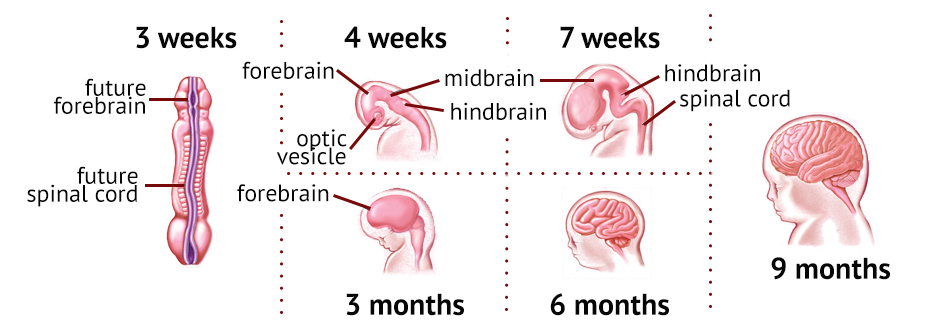
Normally, during your first month of pregnancy, the two sides of the fetus's spine (backbone) join together to cover and protect the spinal cord, spinal nerves and meninges (the tissues covering the spinal cord). At this point, the developing brain and spine are called the neural tube.
As development progresses, the top of the neural tube becomes the brain, and the rest of the tube becomes the spinal cord. An NTD happens when this tube doesn’t close completely somewhere along its length.
What are the types of neural tube defects (NTDs)?
There are several types of neural tube defects, including:
- Spina bifida.
- Anencephaly.
- Encephalocele.
- Iniencephaly.
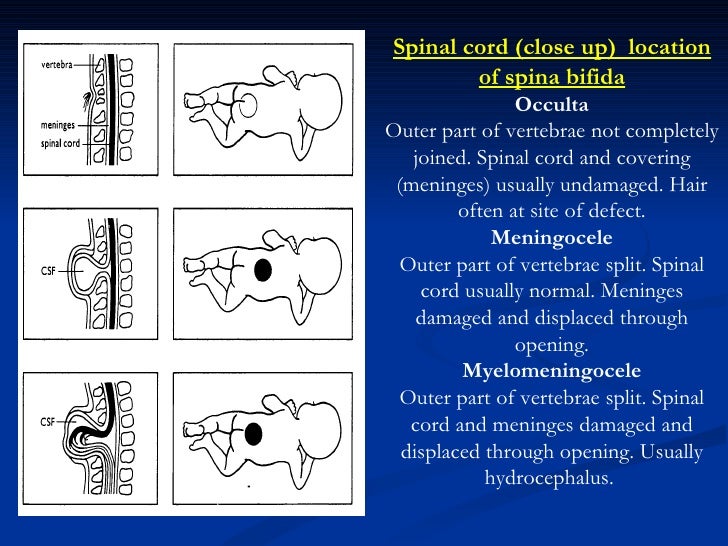
Spina bifida
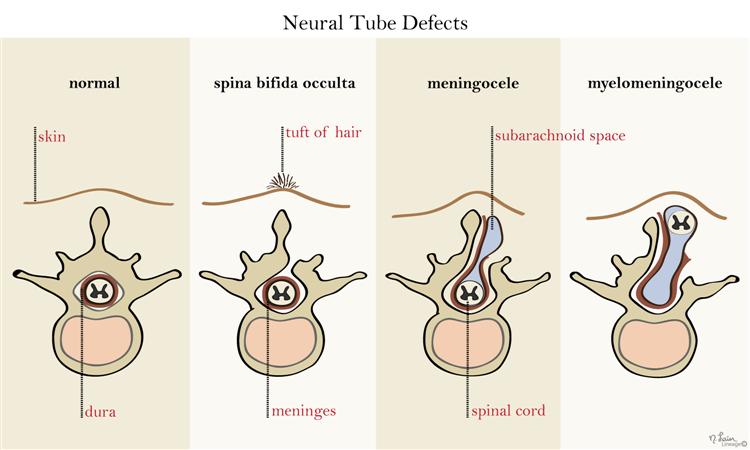
Spina bifida is the most common type of neural tube defect (NTD). It happens when the neural tube doesn’t close completely somewhere along the spine during fetal development.
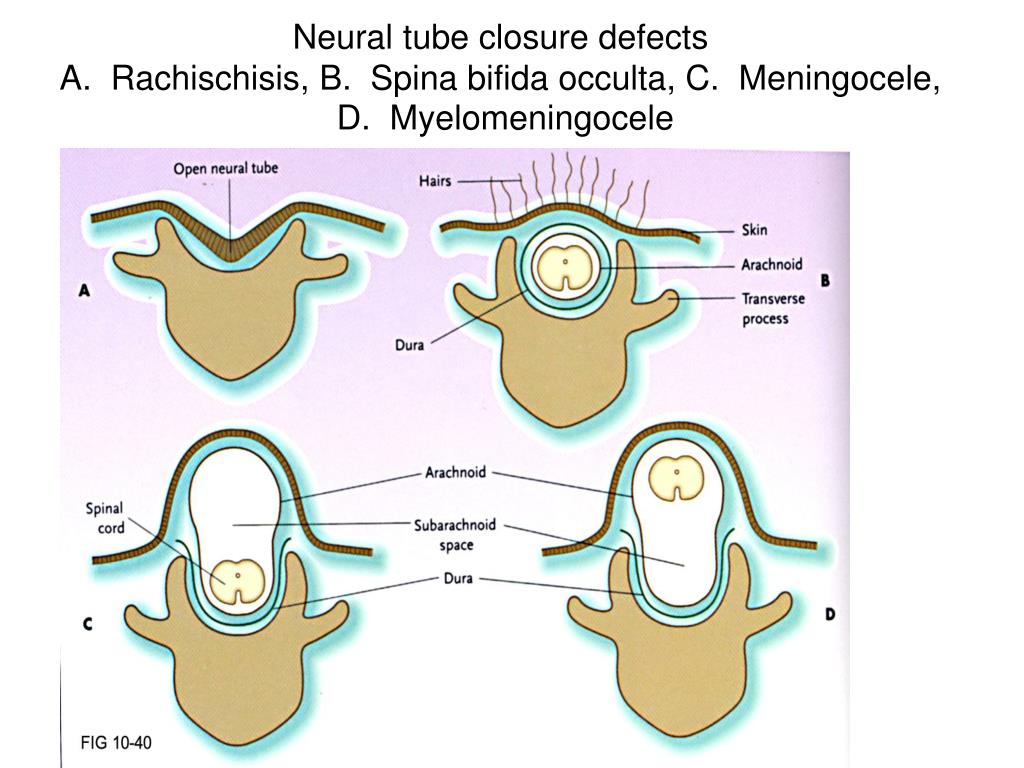
There are a few different types of spina bifida, including:
- Myelomeningocele (open spina bifida): This NTD is characterized by incomplete neural tube closure and a fluid-filled sac that protrudes (sticks out) from your baby’s back. The sac contains part of their spinal cord, meninges, nerves and cerebrospinal fluid (CSF). Myelomeningocele is the most severe and the most common form of spina bifida.
- Meningocele: This NTD is characterized by a sac of fluid that protrudes through an opening in your baby’s back, but their spinal cord is not involved or damaged.
- Spina bifida occulta: This NTD is characterized by a small gap in your baby’s spine, but there isn’t an opening or sac on their back.
 Their nerves and spinal cord aren’t damaged, and the condition usually doesn’t cause any disability. This is the mildest form of spina bifida.
Their nerves and spinal cord aren’t damaged, and the condition usually doesn’t cause any disability. This is the mildest form of spina bifida.
Anencephaly
Anencephaly happens when the fetus's neural tube doesn’t close at the top during fetal development. This causes the skull, scalp and brain not to develop properly, and portions of the brain and skull are missing. The brain tissue that does form is usually exposed because there isn’t enough skin and bone to cover it. Infants with anencephaly are either stillborn or die soon after birth.
Encephalocele
Encephalocele happens when the neural tube doesn’t close near the brain, and there’s an opening in the skull. The fetus's brain and the membranes that cover it can protrude through the skull, forming a sac-like bulge. In some cases, there’s only a small opening in the nasal cavity or forehead area that’s not noticeable.
Iniencephaly
Iniencephaly happens when the spine is severely malformed (misshapen).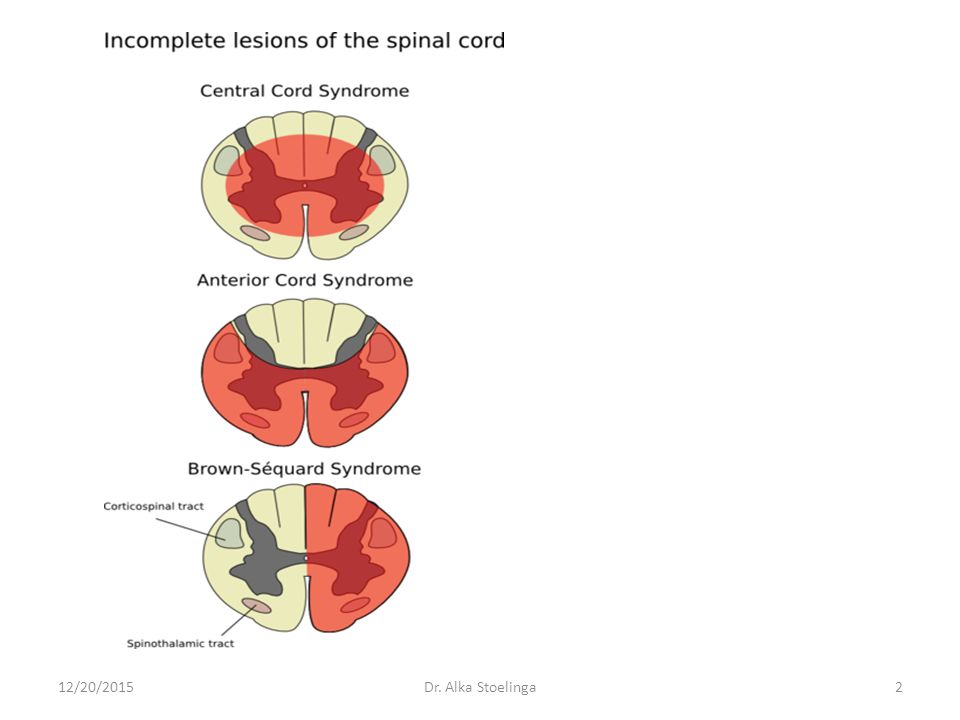 It often causes a lack of a neck, and your baby’s head is bent severely backward. The skin of your baby’s face is connected to their chest, and their scalp is connected to their back. Babies with iniencephaly are usually stillborn.
It often causes a lack of a neck, and your baby’s head is bent severely backward. The skin of your baby’s face is connected to their chest, and their scalp is connected to their back. Babies with iniencephaly are usually stillborn.
Who do neural tube defects affect?
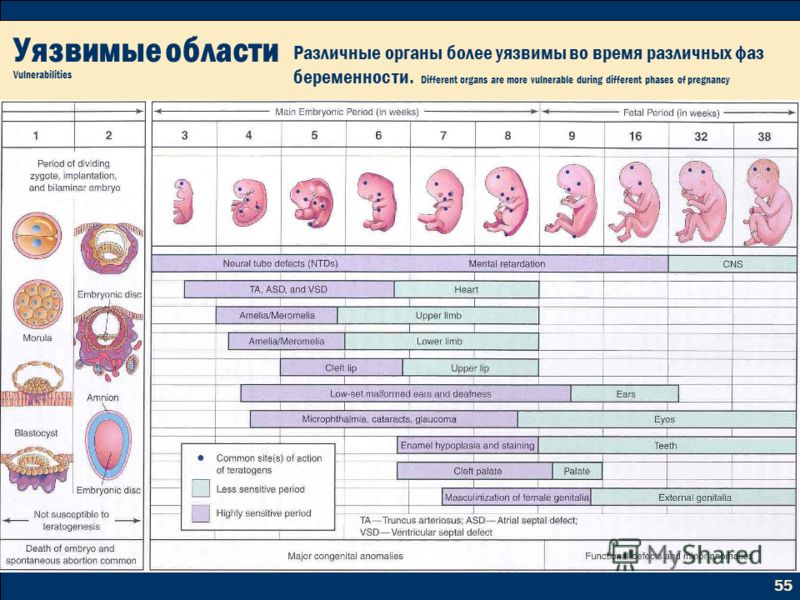
Neural tube defects (NTDs) are birth defects (congenital conditions), so they develop in fetuses. NTDs develop within the first month of pregnancy.
How common are neural tube defects?
Neural tube defects (NTDs) occur in about 3,000 pregnancies each year in the United States. To put that into perspective, there were approximately 3,605,000 births in the U.S. in 2020.
The two most common NTDs are spina bifida and anencephaly. Spina bifida affects about 1,500 babies a year in the U.S., with myelomeningocele being the most common form. Anencephaly affects about 1,000 babies each year in the U.S.
Encephalocele and iniencephaly are both rare NTDs.
Symptoms and Causes
What causes neural tube defects (NTDs)?
Healthcare providers and scientists don’t yet know the exact cause of neural tube defects (NTDs), but they believe it’s a complex combination of genetic, nutritional and environmental factors.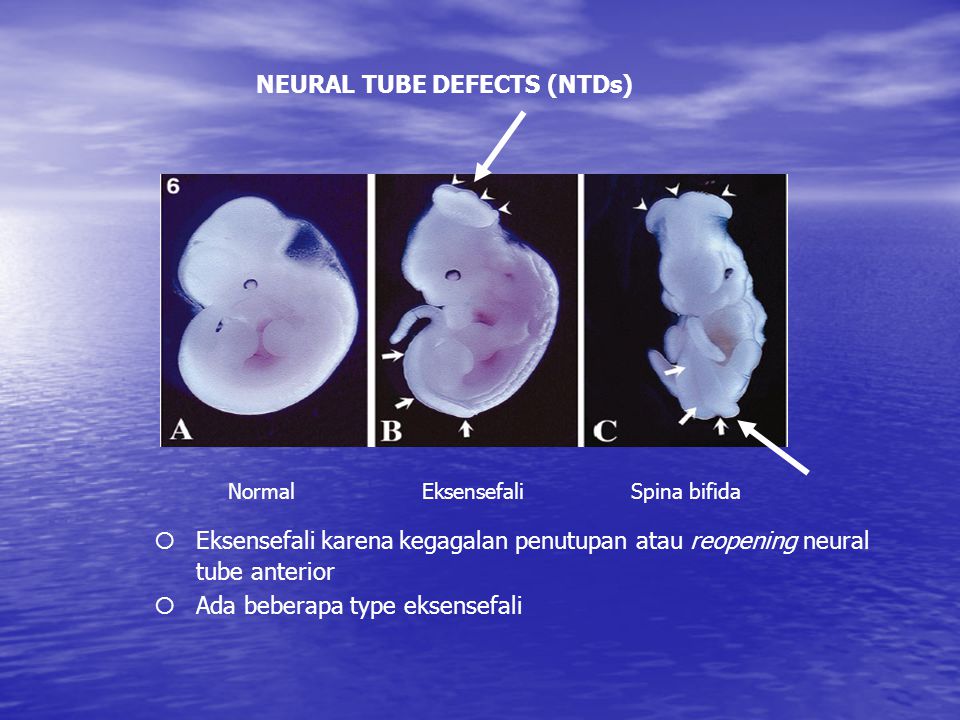
In particular, low levels of folic acid in a person’s body before and during early pregnancy appear to play a part in this type of congenital condition. Folic acid (or folate) is important for the fetal development of the brain and spinal cord.
What are the symptoms of neural tube defects (NTDs)?
Each type of neural tube defect (NTD) has different symptoms.
Some babies with NTDs have no symptoms, while others experience serious disabilities. Babies with iniencephaly and anencephaly are typically stillborn or die shortly after birth due to complications from the defect.
General symptoms of NTDs can include:
- Physical problems, such as paralysis and urinary and bowel control issues.
- Blindness.
- Deafness.
- Intellectual disability.
- Lack of consciousness and, in some cases, death.
If your healthcare provider suspects that the fetus you're carrying has a neural tube defect, your medical team will be able to provide more information about what to expect.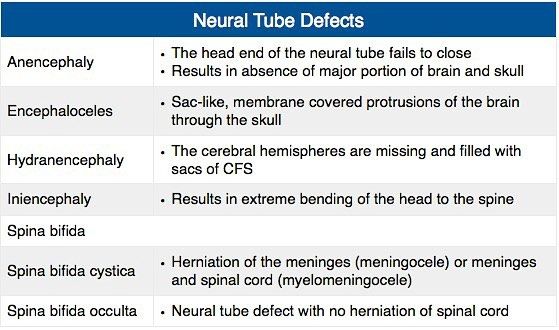 NTDs affect each baby differently.
NTDs affect each baby differently.
What are the signs of neural tube defects (NTDs) during pregnancy?
If you’re pregnant with a fetus that has a neural tube defect (NTD), you won’t experience any symptoms directly related to it.
When you undergo a fetal ultrasound, your healthcare provider will look for certain signs of the fetus's health and development depending on its fetal age, including looking for signs of NTDs in the spine and head. Healthcare providers can usually diagnose NTDs with an ultrasound.
Diagnosis and Tests
How are neural tube defects (NTDs) diagnosed?
Healthcare providers typically diagnose neural tube defects (NTDs) during pregnancy through prenatal tests, such as ultrasound.
What tests will be done to diagnose neural tube defects (NTDs)?
Healthcare providers use the following tests to help diagnose neural tube defects (NTDs) before birth:
- Blood test: Your healthcare provider will order a screening test that measures the amount of alpha-fetoprotein (AFP) in your blood during the 16th to 18th week of pregnancy.
 The amount is higher than normal in about 75% to 80% of pregnant people who are carrying a fetus with an NTD. If your level is elevated, your healthcare provider will order other tests, such as an ultrasound, to better evaluate the growing fetus.
The amount is higher than normal in about 75% to 80% of pregnant people who are carrying a fetus with an NTD. If your level is elevated, your healthcare provider will order other tests, such as an ultrasound, to better evaluate the growing fetus. - Fetal (prenatal) ultrasound: An ultrasound during pregnancy is the most accurate method to diagnose several NTDs. Healthcare providers typically recommend ultrasounds during the first trimester (11 to 14 weeks of pregnancy) and second trimester (18 to 22 weeks of pregnancy).
- Amniocentesis: Healthcare providers use this test to check for NTDs and other birth defects. During amniocentesis, they use a needle to remove a sample of fluid from the amniotic sac that surrounds te fetus. You can get this test at 15 to 20 weeks of pregnancy. This test carries certain risks. Be sure to talk to your healthcare provider about the process.
Healthcare providers also use imaging tests, such as an MRI (magnetic resonance imaging) or CT (computed tomography) scan, to diagnose some NTDs after birth.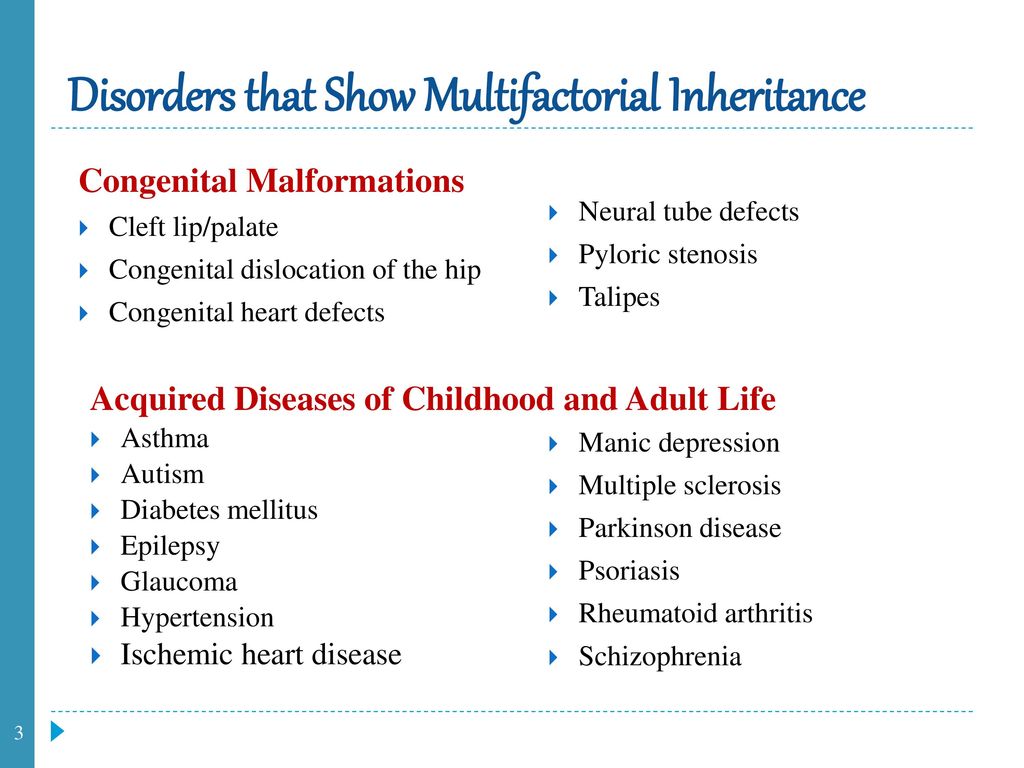
Management and Treatment
How are neural tube defects (NTDs) treated?
There are several treatment options for spina bifida and encephalocele depending on the severity of the condition.
There isn’t a treatment for anencephaly or iniencephaly. Infants with these conditions are typically stillborn or die shortly after birth.
Treatment for spina bifida and encephalocele
Treatment for both spina bifida and encephalocele depends on the severity of the condition and if your baby has other complications. Surgery is a common option for both conditions.
Healthcare providers typically treat encephalocele with surgery to place the protruding part of your baby’s brain and the membranes covering it back into their skull. They then close the opening in your baby’s skull.
Treatment for myelomeningocele, the most common form of spina bifida, typically involves surgery to repair the opening in your baby’s spine. Healthcare providers can perform surgery before birth (fetal surgery) or shortly after birth (postnatal surgery).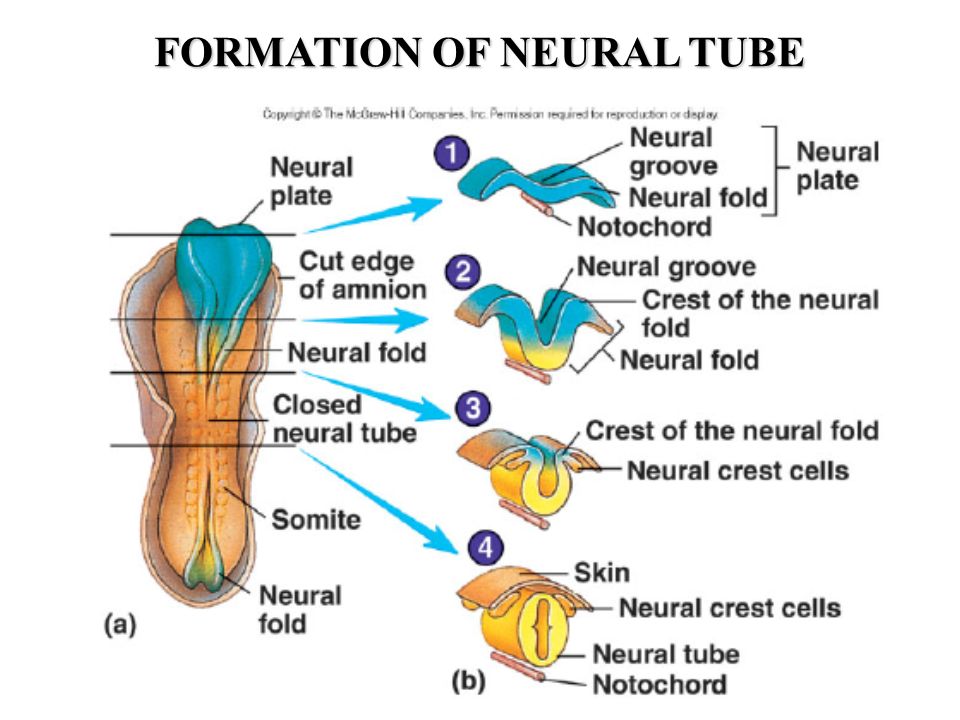
Long-term treatment for both conditions depends on your child’s condition. They may need multiple surgeries over time and other treatments related to complications, such as a shunt to treat hydrocephalus (excess fluid surrounding their brain).
Prevention
What are the risk factors for developing a neural tube defect (NTD)?
Any person can have a baby with a neural tube defect (NTD). But certain factors make you more likely to have a baby with an NTD, including:
- Folate (folic acid) deficiency: Folate, the natural form of vitamin B-9, is important for healthy fetal development. A folate deficiency before and during pregnancy increases the risk of having a baby with spina bifida and other NTDs. If you’re pregnant or thinking of becoming pregnant, it’s important to take prenatal vitamins to ensure you’re getting enough folate (folic acid) and other nutrients to support a healthy pregnancy. The Centers for Disease Control and Prevention (CDC) recommends all people who can become pregnant take 400 micrograms (mcg) of folic acid every day, in addition to eating food with folate, to help prevent NTDs.
- Family history of neural tube defects: People who’ve had one baby with an NTD have a 2% to 3% increased risk of having a second baby with an NTD. To learn more about your risk of having a baby with an NTD, consider seeing a genetic counselor.
- Certain antiseizure medications: These medications are linked to neural tube defects when taken during pregnancy. If you take medicine to prevent seizures, talk to your healthcare provider before you get pregnant about how the medicine may affect your pregnancy.
- Diabetes: People with poorly managed diabetes who are pregnant have a higher risk of having a baby with an NTD.
- Obesity: People who have obesity before pregnancy have an increased risk of having a baby with an NTD.
- Increased body temperature in early pregnancy: Increases in core body temperature (hyperthermia) in the early weeks of pregnancy due to a prolonged fever or use of a sauna or hot tub have been associated with a slightly increased risk of NTDs.
- Opioid use in early pregnancy: Opioids are a class of very powerful and highly addictive drugs that reduce pain. People who are pregnant and who’ve taken opioids in the first two months of pregnancy have an increased chance of having a baby with an NTD, in addition to other complications. If you’re pregnant and taking any drugs or medications that may be an opioid, tell your healthcare provider right away.
Outlook / Prognosis
Can a baby live with a neural tube defect?
Yes, your baby can live with certain neural tube defects, including spina bifida and encephalocele.
Babies with anencephaly and iniencephaly are typically stillborn or die shortly after birth, however.
What is the prognosis (outlook) for neural tube defects (NTDs)?
For babies with spina bifida, especially myelomeningocele, or encephalocele, there’s a high likelihood of nerve damage, which can cause paralysis and other issues. The nerve damage and loss of function that are present at birth are usually permanent.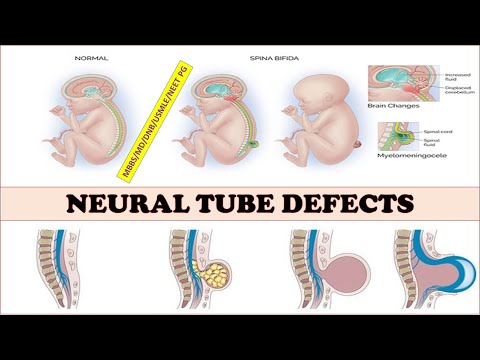 But there are a number of treatments that can sometimes prevent further damage and help with complications.
But there are a number of treatments that can sometimes prevent further damage and help with complications.
Some babies with spina bifida have no or minimal complications.
Living With
How do I take care of my baby with a neural tube defect?
It’s important to remember that no two people with a neural tube defect (NTD), especially spina bifida and encephalocele, are affected in the same way. It’s impossible to predict how your baby will be affected. The best way you can prepare is to talk to healthcare providers who specialize in researching and treating your baby’s condition.
As they grow, your child may benefit from a team of healthcare providers who can care for their needs. It’s important to advocate for your child and to arrange the best medical care possible.
When should I see my healthcare provider about neural tube defects (NTDs)?
If your child was born with a neural tube defect (NTD), they’ll likely need to see their healthcare provider — or team of healthcare providers — regularly throughout their life.
If you take antiseizure medication or opioids, it’s important to talk to your healthcare provider before becoming pregnant about how these medications could affect your pregnancy and the likelihood of having a child with an NTD.
A note from Cleveland Clinic
Learning that the fetus you're carrying has a neural tube defect (NTD) is scary and overwhelming. But know that you’re not alone — many resources are available to help you and your family. It’s important that you speak with a healthcare provider who’s very familiar with neural tube defects so you can learn more about how your baby will be affected and how to prepare.
Fomina Clinic - a network of multidisciplinary clinics
We have already found out that when planning a pregnancy, the lifestyle of the expectant mother plays an important role, namely the rejection of bad habits, proper nutrition, hygiene and sports. Vitamins play an important role in this, namely folic acid, which is advised to start taking 1-3 months before the expected pregnancy. It is its use that prevents possible malformations that can lead to the death of the child. nine0003
It is its use that prevents possible malformations that can lead to the death of the child. nine0003
This is a B vitamin that prevents fetal neural tube defects. Moreover, it is important to understand that such an effect is possible only if folic acid begins to enter the mother's body before pregnancy and continues to be taken during pregnancy. Thus, from the first days after conception, the child begins to develop in the right conditions, because by this time folic acid has time to get into your bloodstream in sufficient quantities.
Unfortunately not. The fact is that violations of the laying of the neural tube usually occur on the 18th - 30th day after conception, when a woman may still not know about her pregnancy. nine0003
Let's start with the statistics: neural tube defects (yes, there are several!) are found in about 7 out of 10,000 newborns, and it is believed that in half of these cases they are caused by a lack of folic acid in the mother's diet.
The two most common neural tube defects are:
- Spina bifida damages the spinal cord: with this defect, most children survive and reach adulthood, but they may be accompanied by central nervous system disorders throughout life, such as paralysis or inability to control urination and defecation; nine0020
- with anencephaly, the entire brain or a significant part of it is missing, in which case most children die shortly after birth.
Recommended foods include: Green vegetables, legumes (beans, peas, lentils), lettuce, berries, citrus fruits (fruits and juices), breakfast cereal, whole grain bread/bread.
This, of course, is not enough, because in most of these products the content of folic acid is less than 20% (or even 10%) of the recommended daily amount by doctors. The only exception is lentils, one glass of which contains 90%. Therefore, additionally every day when planning pregnancy and throughout its duration, you need to take vitamins that contain 400 mcg of folic acid.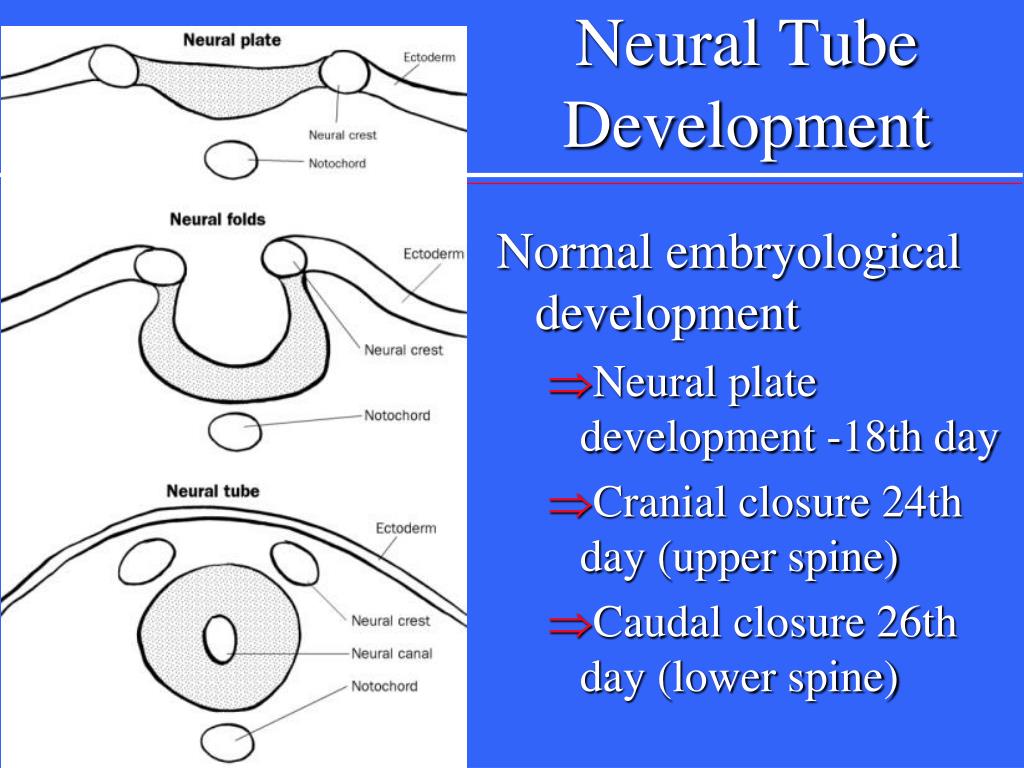
Healthy women with normal pregnancy really need such a small dose, but there are preparations containing from 1 to 5 mg of folic acid. There are several "risk groups" to which they are prescribed:
- women who had a child with a neural tube defect from a previous pregnancy; nine0020
- diabetic women;
- women with elevated levels of homocysteine in the blood;
- women taking antiepileptic drugs.
If you recognize yourself in one of these groups, be sure to check with your doctor to discuss the need for higher doses of folic acid. But remember that more is not always better, and in this case, this common truth works.
Follow us
Malformations
Malformations- Healthcare issues »
- A
- B
- in
- g
- D
- Ф
- and
- L
- L
- L
- L
- L
- L
- L
- L
- L
- L
- L
- L
- L O
- P
- R
- S
- T
- U
- F
- X
- C
- W
- S
- S
- S
- E
- S
- S
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- Newsletter
- The facts are clear
- Publications
- Find a country »
- A
- B
- in
- g
- D
- E
- Ф
- С
- and
- I
- to
- L
- N
- From
- t
- in
- f
- x
- c
- h
-
- s
- E
- I
- WHO in countries » nine0018
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A nine0020
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Highlights " nine0020
- About WHO »
- General director
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center/
- Newsletters/
- Read more/ nine0019 Malformations
\n
- \n
- development and strengthening of registration and surveillance systems; \n
- experience and capacity building; \n
- strengthening research and scientific work in the field of etiology, diagnosis and prevention; \n
- strengthening international cooperation.
 \n
\n
\n
Definition
\n
\nCongenital malformations are also referred to as congenital malformations, congenital disorders, or congenital deformities. Congenital malformations can be defined as structural or functional abnormalities (eg, metabolic disorders) that appear in utero and may be identified before birth, during birth, or later in life. nine0003
\n
Causes and risk factors
\n
\nApproximately 50% of all malformations cannot be attributed to any specific cause, but some causes or risk factors are known.
\n
Socio-economic factors
\n
\nAlthough low income may be an indirect determinant, malformations are more likely to occur in families and countries with insufficient resources. It is estimated that approximately 94% of severe malformations occur in middle- and low-income countries, where women often do not have access to sufficient and good enough food and may be exposed to some agent or factor, such as infection or alcohol, that provokes or enhances deviations from the norm in prenatal development.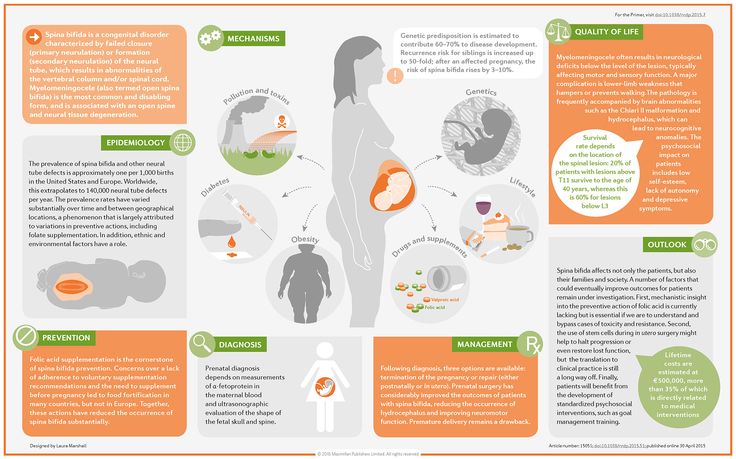 Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations. nine0003
Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations. nine0003
\n
Genetic factors
\n
\nIncest (consanguinity) increases the incidence of rare genetic birth defects and almost doubles the risk of neonatal and infant mortality, mental retardation and severe birth defects in children born to first cousins . Some ethnic groups, such as Ashkenazi Jews and Finns, have a relatively high prevalence of rare genetic mutations that lead to an increased risk of malformations.\n
\n
Infections
\n
\nMaternal infections such as syphilis or measles are a common cause of birth defects in low- and middle-income countries.
\n
Maternal nutrition
\n
\nDeficiencies in iodine, folate, obesity, or conditions such as diabetes mellitus are associated with some malformations.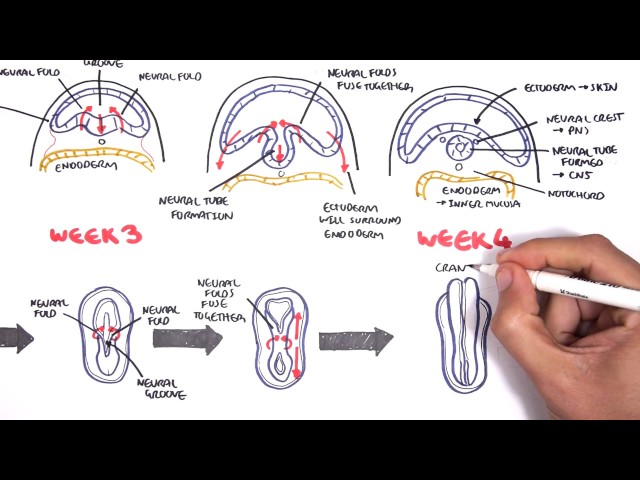 For example, folic acid deficiency increases the risk of having a baby with a neural tube defect. In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus. nine0003
For example, folic acid deficiency increases the risk of having a baby with a neural tube defect. In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus. nine0003
\n
Environmental factors
\n
\nMaternal exposure to certain pesticides and other chemicals, as well as certain drugs, alcohol, tobacco, psychoactive substances, or radiation during pregnancy may increase the risk of developing the fetus or a newborn baby with birth defects. Working or living near or close to landfills, smelters, or mines can also be a risk factor, especially if the mother is exposed to other environmental risk factors or malnutrition. nine0003
\n
Prevention
\n
\nPregnancy and conception preventive health care, and prenatal care, reduce the incidence of some birth defects. Primary prevention of malformations includes the following measures:
\n
- \n
- Improving the nutrition of women during the reproductive period by ensuring adequate intake of vitamins and minerals, especially folic acid, as a result of daily oral supplementation or fortification of staple foods, such as wheat or corn flour.
 nine0020 \n
nine0020 \n - See to it that the pregnant woman does not consume or consumes in limited quantities unhealthy foods, especially alcohol. \n
- Pre-pregnancy and pregnancy prevention of diabetes through counseling, weight management, proper nutrition, and, if necessary, insulin administration. \n
- Prevention of exposure to environmental hazardous substances (eg, heavy metals, pesticides, certain drugs) during pregnancy. nine0020 \n
- Ensuring that any exposure of a pregnant woman to drugs or medical exposure (such as X-rays) is justified and based on a careful analysis of the health risks and benefits. \n
- Increase vaccination coverage for women and children, especially against rubella. This disease can be prevented by vaccinating children. Rubella vaccine may also be given at least one month before pregnancy to women who did not receive the vaccine or who did not have rubella in childhood. nine0020 \n
- Increase vaccination coverage for women and children, especially against rubella virus.
 This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy. \n
This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy. \n - Scaling up and strengthening training for health professionals and other staff involved in strengthening malformation prevention. \n
\n
Identification
\n
\nPre-conception (pre-conception) and near conception (peri-conception) care includes basic reproductive health care as well as medical genetic screening and counseling. Screening can be carried out during the three periods listed below.
\n
- \n
- Pre-pregnancy screening is designed to identify people who are at risk of developing certain health conditions or at risk of passing on any health conditions to their children. Screening includes family medical history and vector screening. Screening is especially important in countries where incestuous marriages are common.
 nine0020 \n
nine0020 \n - Preconception screening: maternal characteristics may increase risk, and screening results should be used to provide appropriate care based on risk. During this period, screening of young and mature mothers, as well as screening for the use of alcohol, tobacco and other psychoactive substances, can be carried out. Ultrasound can be used to detect Down's syndrome during the first trimester of pregnancy and severe fetal malformations during the second trimester. Additional tests and amniocentesis help detect neural tube defects and chromosomal abnormalities during the first and second trimesters of pregnancy. nine0020 \n
- Newborn screening includes a clinical examination, as well as screening for hematological, metabolic, and hormonal disorders. Screening for deafness and heart disease, and early detection of birth defects, can facilitate life-saving treatment and prevent progression of the defect, which could lead to some form of physical, mental, or visual or hearing disability.
 In some countries, all newborns are screened for thyroid and adrenal abnormalities before being discharged from the maternity ward. nine0020 \n
In some countries, all newborns are screened for thyroid and adrenal abnormalities before being discharged from the maternity ward. nine0020 \n
\n
Treatment and care
\n
\nIn countries with adequate health services, structural congenital malformations can be corrected with pediatric surgery and children with functional problems such as thalassemia (inherited by recessive blood disease), sickle cell disorders, and congenital hypothyroidism.
\n
WHO activities
\n
\nIn 2010, the World Health Assembly published a report on birth defects. The report outlines the main components of establishing national programs for the prevention and care of birth defects before and after birth. The report also recommends priority actions for the international community to help establish and strengthen such national programs.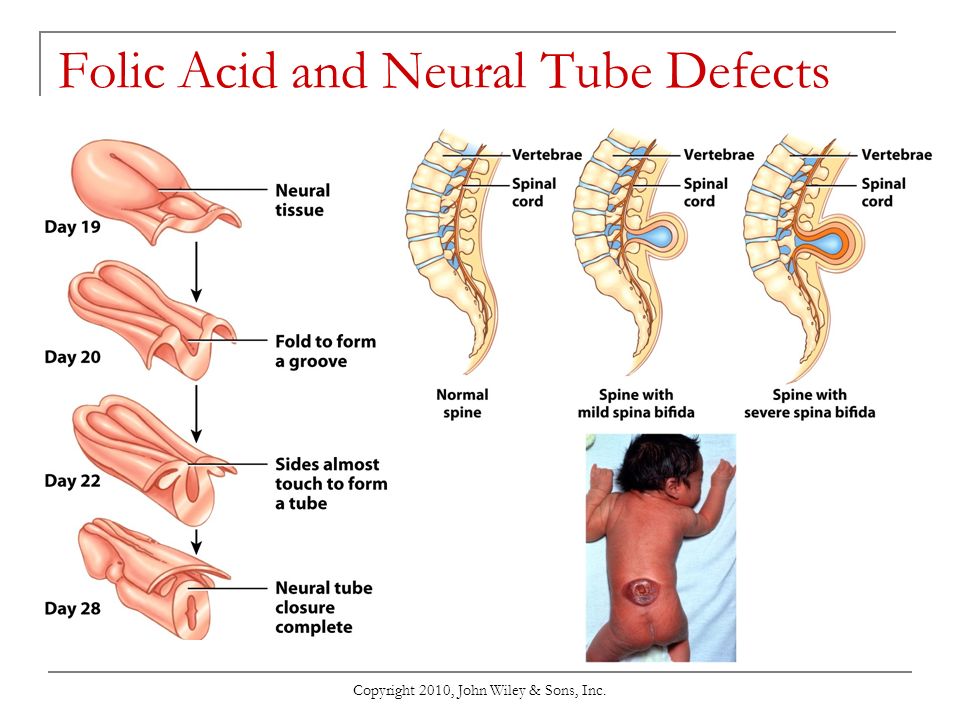
\n
\nThe global strategy for women's and children's health, announced in September 2010 by the United Nations in collaboration with government leaders and other organizations such as WHO and UNICEF, plays a critical role in implementing efficient and cost-effective action to promote newborn and child health.\n
\n
\nWHO is also working with the National Center for Birth and Developmental Disorders, part of the US Centers for Disease Control and Prevention (CDC), and other partners to develop a global policy for salt fortification in foods folic acid at the country level. In addition, WHO is working with partners to provide the necessary technical expertise to conduct surveillance of neural tube defects, monitor efforts to fortify foods with folic acid salts, and strengthen laboratory capacity to assess risks for birth defects prevented by folic acid salts. nine0003
\n
\nThe International Clearing House for Surveillance and Research on Birth Defects is a voluntary, non-profit, international organization in official relations with WHO.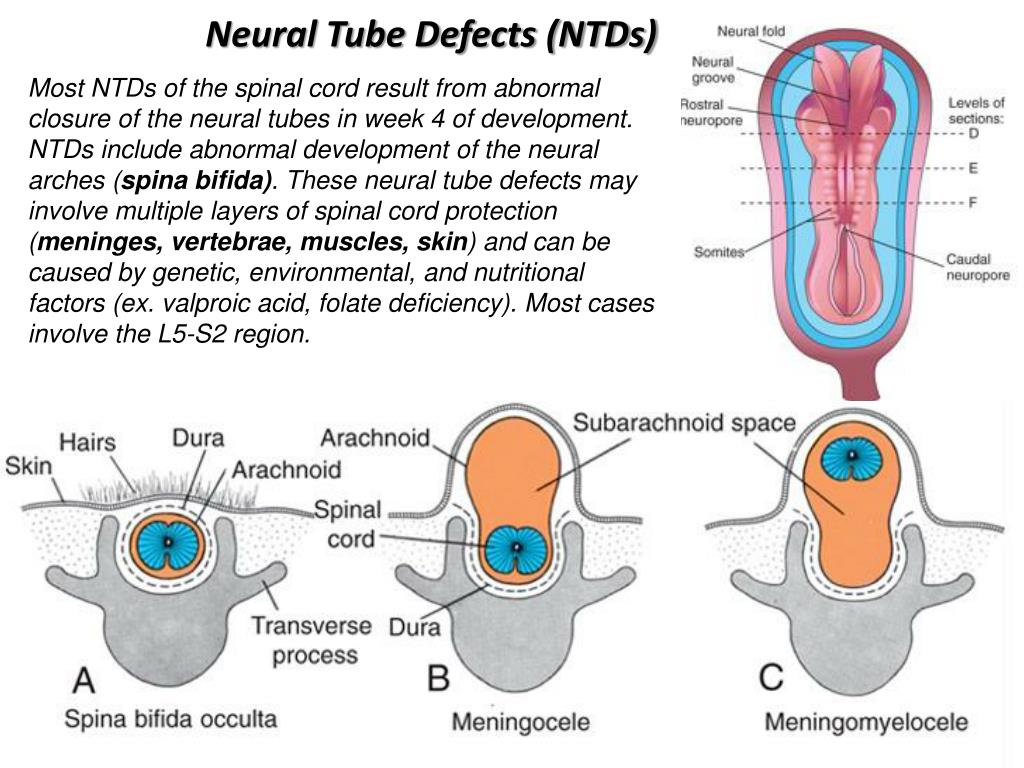 This organization collects surveillance data on birth defects and research programs around the world to study and prevent birth defects and mitigate their effects.
This organization collects surveillance data on birth defects and research programs around the world to study and prevent birth defects and mitigate their effects.
\n
\nThe WHO Departments of Reproductive Health and Research and Nutrition for Health and Development, in collaboration with the International Clearing House for Surveillance and Research in Birth Defects and the CDC National Center for Birth Defects and Development, organize annual seminars on surveillance and prevention of birth defects and preterm birth. The WHO Department of HIV/AIDS is collaborating with these partners to strengthen surveillance for malformations among women receiving antiretroviral drugs during pregnancy as an integral part of the monitoring and evaluation of national HIV programs. nine0003
\n
\nThe GAVI Alliance, partnered with WHO, is helping developing countries to increase the control and elimination of rubella and congenital rubella syndrome through immunization.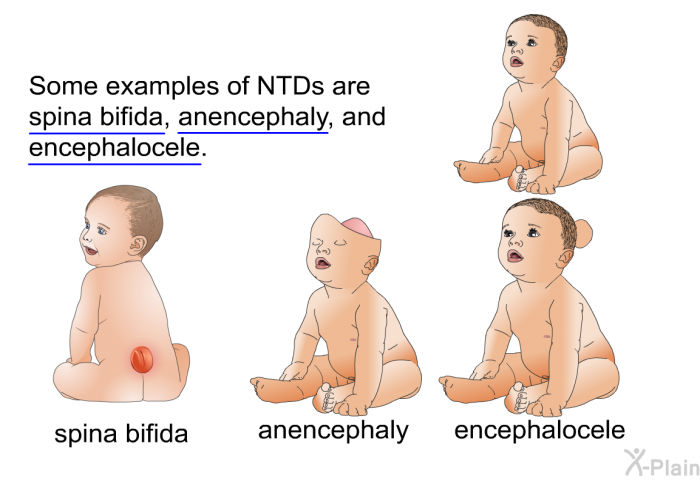
\n
\nWHO is developing normative tools, including guidelines and a global plan of action to strengthen health care and rehabilitation services in support of the implementation of the Convention on the Rights of Persons with Disabilities. Similarly, WHO is helping countries integrate health care and rehabilitation services into general primary health care, supporting the development of community-based rehabilitation programs and strengthening specialized rehabilitation centers and their links with community-based rehabilitation centers. nine0003
\n
United Nations Convention on the Rights of Persons with Disabilities
\n
\nThe WHO Department of Public Health and Environment works across a range of activities and develops interventions to address the environmental and social determinants of child development. These include: child-only vulnerability to indoor and outdoor air pollution, water pollution, lack of basic hygiene, toxic compounds, heavy metals, waste components and radiation exposure; mixed impact of factors related to the social environment, professional activities and nutrition, as well as the living conditions of children (home, school).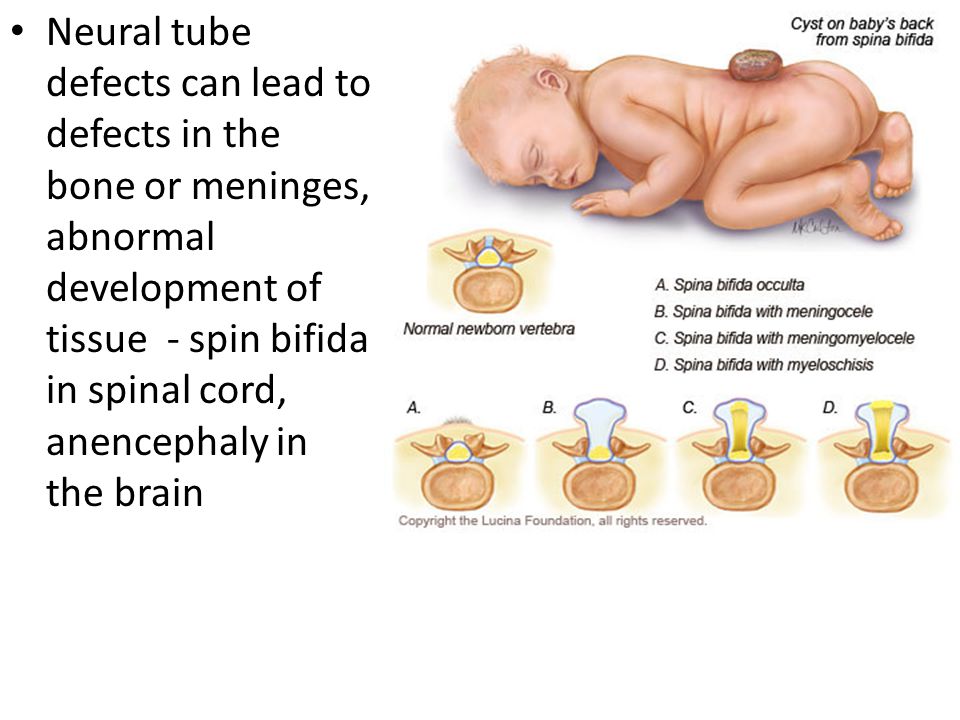 nine0003
nine0003
\n
","datePublished":"2022-02-28T22:52:00.0000000+00:00","image":"https://cdn.who.int/media/images/default -source/imported/preterm-birth-mother-jpg.jpg?sfvrsn=c5c1adf1_0","publisher":{"@type":"Organization","name":"World Health Organization: WHO","logo": {"@type":"ImageObject","url":"https://www.who.int/Images/SchemaOrg/schemaOrgLogo.jpg","width":250,"height":60}},"dateModified ":"2022-02-28T22:52:00.0000000+00:00","mainEntityOfPage":"https://www.who.int/ru/news-room/fact-sheets/detail/congenital-anomalies", "@context":"http://schema.org","@type":"Article"}; nine0003
Key Facts
- An estimated 303,000 children die each year from malformations in the first 4 weeks of life.
- Developmental disabilities can lead to long-term disability, which has a significant impact on individuals, their families, health systems and society.
- The most severe malformations include heart defects, neural tube defects, and Down syndrome.
- Although malformations may be genetic, infectious, or environmental in origin, the exact cause is often difficult to establish. nine0020
- Some birth defects can be prevented. The main elements of prevention are, inter alia, vaccination, adequate intake of folic acid or iodine through fortification of staple foods or provision of nutritional supplements, and proper prenatal care.
Malformations and preterm birth are major causes of childhood death, chronic disease and disability in many countries. In 2010, the World Health Assembly adopted a resolution calling on all Member States to promote primary prevention and health promotion for children with developmental disabilities through:
- development and strengthening of registration and surveillance systems;
- experience and capacity building;
- strengthening research and scientific work in the field of etiology, diagnosis and prevention;
- strengthening international cooperation.
Definition
Congenital malformations are also referred to as congenital malformations, congenital disorders or congenital deformities. Congenital malformations can be defined as structural or functional abnormalities (eg, metabolic disorders) that appear in utero and may be identified before birth, during birth, or later in life. nine0003
Causes and risk factors
Approximately 50% of all malformations cannot be attributed to any specific cause, but some causes or risk factors are known.
Socio-economic factors
While low income may be an indirect determinant, malformations are more likely to occur in under-resourced families and countries. It is estimated that approximately 94% of severe malformations occur in middle- and low-income countries, where women often do not have access to sufficient and good enough food and may be exposed to some agent or factor, such as infection or alcohol, that provokes or enhances deviations from the norm in prenatal development.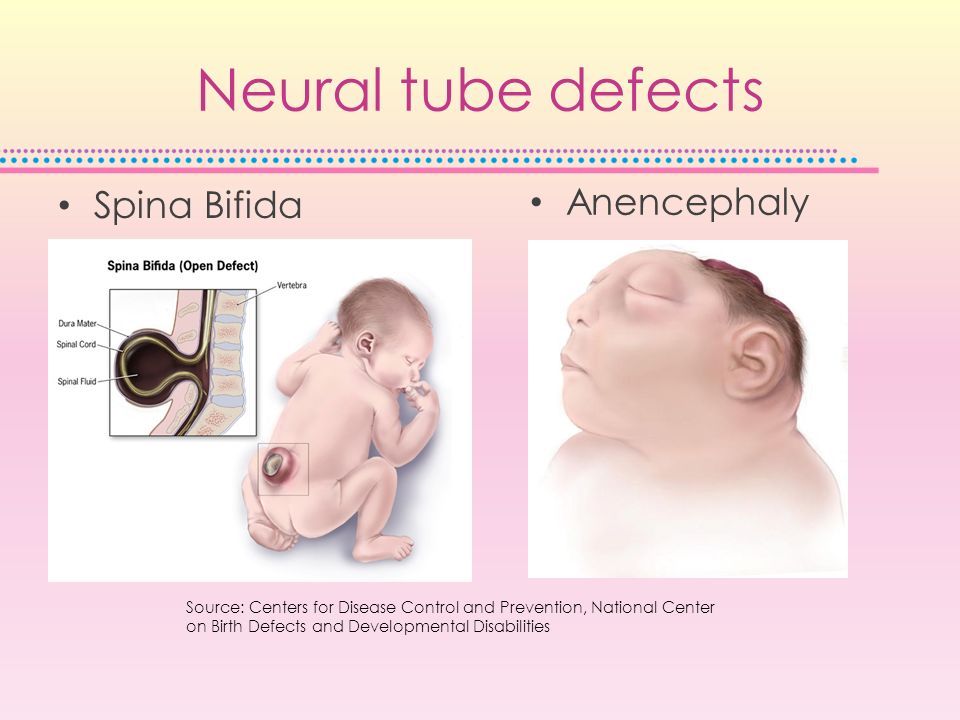 Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations. nine0003
Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations. nine0003
Genetic factors
Incest (consanguinity) increases the prevalence of rare genetic birth defects and almost doubles the risk of neonatal and infant mortality, mental retardation and severe birth defects in children born to first cousins. Some ethnic groups, such as Ashkenazi Jews and Finns, have a relatively high prevalence of rare genetic mutations that lead to an increased risk of malformations. nine0003
Infections
Maternal infections such as syphilis or measles are a common cause of birth defects in low- and middle-income countries.
Maternal nutrition
Deficiency of iodine, folic acid salts, obesity, or conditions such as diabetes mellitus are associated with some malformations. For example, folic acid deficiency increases the risk of having a baby with a neural tube defect.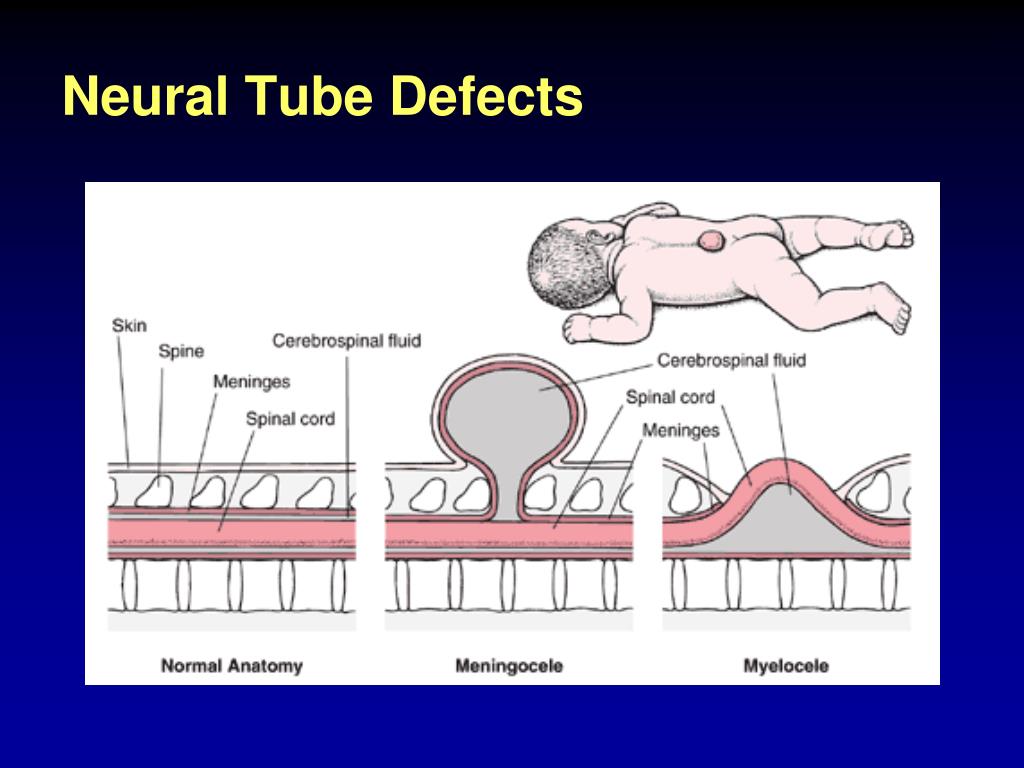 In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus. nine0003
In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus. nine0003
Environmental factors
Maternal exposure to certain pesticides and other chemicals, as well as certain drugs, alcohol, tobacco, psychoactive substances, or radiation during pregnancy may increase the risk of birth defects in the fetus or newborn. Working or living near or close to landfills, smelters, or mines can also be a risk factor, especially if the mother is exposed to other environmental risk factors or malnutrition. nine0003
Prevention
Preventive health care during pregnancy and conception, as well as antenatal care, reduce the incidence of some birth defects. Primary prevention of malformations includes the following measures:
- Improving the nutrition of women during the reproductive period by ensuring adequate intake of vitamins and minerals, especially folic acid, through daily oral supplementation or fortification of staple foods such as wheat or corn flour .
 nine0020
nine0020 - Supervise that a pregnant woman does not consume or consume in a limited amount unhealthy foods, especially alcohol.
- Prevention of diabetes in pregnancy and during pregnancy through counseling, weight management, proper nutrition and, if necessary, insulin administration.
- Prevention during pregnancy of exposure to hazardous environmental substances (eg, heavy metals, pesticides, certain drugs). nine0020
- Ensuring that any exposure of a pregnant woman to drugs or radiation for medical purposes (such as x-rays) is justified and based on a careful analysis of health risks and benefits.
- Increase vaccination coverage for women and children, especially against rubella virus. This disease can be prevented by vaccinating children. Rubella vaccine may also be given at least one month before pregnancy to women who did not receive the vaccine or who did not have rubella in childhood. nine0020
- Increase vaccination coverage for women and children, especially against rubella virus.
 This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy.
This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy. - Scaling up and strengthening training for health professionals and other staff involved in strengthening malformation prevention.
Revealing
Medical care before conception (in the preconception period) and around the time of conception (in the periconceptional period) includes basic reproductive health care, as well as medical genetic screening and counseling. Screening can be carried out during the three periods listed below.
- Pre-pregnancy screening is designed to identify people who are at risk of developing certain health conditions or passing on any health conditions to their children. Screening includes family medical history and vector screening. Screening is especially important in countries where incestuous marriages are common. nine0020
- Preconception screening: maternal characteristics may increase risk, and screening results should be used to provide appropriate care based on risk.
 During this period, screening of young and mature mothers, as well as screening for the use of alcohol, tobacco and other psychoactive substances, can be carried out. Ultrasound can be used to detect Down's syndrome during the first trimester of pregnancy and severe fetal malformations during the second trimester. Additional tests and amniocentesis help detect neural tube defects and chromosomal abnormalities during the first and second trimesters of pregnancy. nine0020
During this period, screening of young and mature mothers, as well as screening for the use of alcohol, tobacco and other psychoactive substances, can be carried out. Ultrasound can be used to detect Down's syndrome during the first trimester of pregnancy and severe fetal malformations during the second trimester. Additional tests and amniocentesis help detect neural tube defects and chromosomal abnormalities during the first and second trimesters of pregnancy. nine0020 - Newborn screening includes a clinical examination, as well as screening for hematological, metabolic and hormonal disorders. Screening for deafness and heart disease, and early detection of birth defects, can facilitate life-saving treatment and prevent progression of the defect, which could lead to some form of physical, mental, or visual or hearing disability. In some countries, all newborns are screened for thyroid and adrenal abnormalities before being discharged from the maternity ward. nine0020
Treatment and medical care
In countries with adequate health services, structural birth defects can be corrected with pediatric surgery and timely treatment can be provided for children with functional problems such as thalassemia (a recessive blood disorder), sickle cell disorders, and congenital hypothyroidism.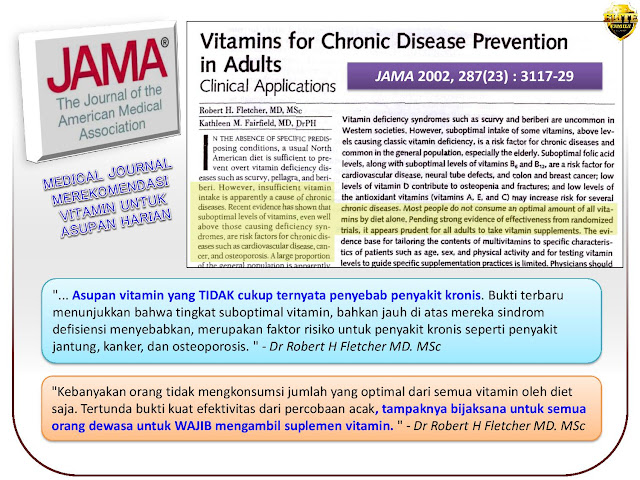
WHO activities
In 2010, the World Health Assembly published a report on birth defects. The report outlines the main components of establishing national programs for the prevention and care of birth defects before and after birth. The report also recommends priority actions for the international community to help establish and strengthen such national programs. nine0003
The Global Strategy for Women's and Children's Health, launched in September 2010 by the United Nations in collaboration with government leaders and other organizations such as WHO and UNICEF, plays a critical role in achieving effective and cost-effective action to improve newborn health and children.
WHO is also working with the National Center for Birth and Developmental Disorders, part of the US Centers for Disease Control and Prevention (CDC), and other partners to develop a global policy for folic acid fortification at the country level. In addition, WHO is working with partners to provide the necessary technical expertise to conduct surveillance of neural tube defects, monitor efforts to fortify foods with folic acid salts, and strengthen laboratory capacity to assess risks for birth defects prevented by folic acid salts.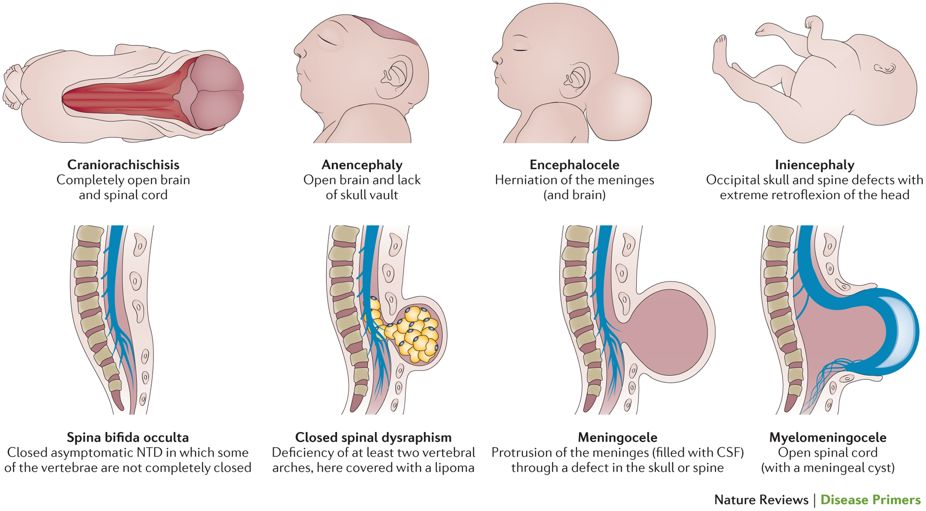 nine0003
nine0003
The International Clearing House for Surveillance and Research on Birth Defects is a voluntary, non-profit international organization in official relations with WHO. This organization collects surveillance data on birth defects and research programs around the world to study and prevent birth defects and mitigate their effects.
The WHO Departments of Reproductive Health and Research and Nutrition for Health and Development, in collaboration with the International Clearing House for Surveillance and Research on Birth Defects and the CDC National Center for Birth Defects and Development, organize annual workshops on surveillance and prevention of birth defects and premature birth. The WHO Department of HIV/AIDS is collaborating with these partners to strengthen surveillance for malformations among women receiving antiretroviral drugs during pregnancy as an integral part of the monitoring and evaluation of national HIV programs. nine0003
The GAVI Alliance, with WHO among its partners, is helping developing countries to accelerate the control and elimination of rubella and congenital rubella syndrome through immunization.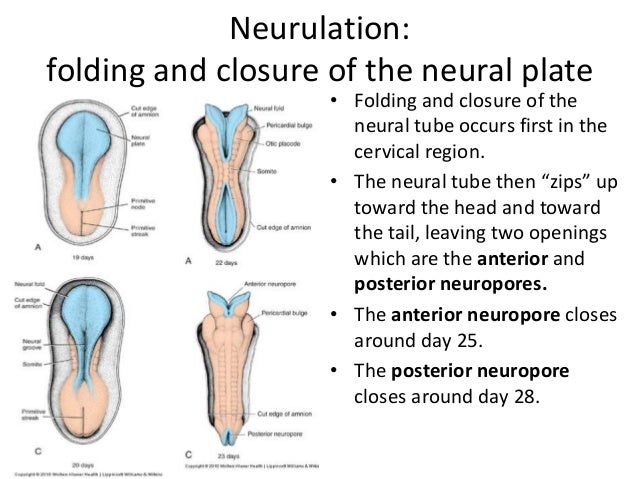
WHO is developing normative tools, including guidelines and a global action plan to strengthen health care and rehabilitation services in support of the implementation of the Convention on the Rights of Persons with Disabilities. Similarly, WHO is helping countries integrate health care and rehabilitation services into general primary health care, supporting the development of community-based rehabilitation programs and strengthening specialized rehabilitation centers and their links with community-based rehabilitation centers. nine0003
UN Convention on the Rights of Persons with Disabilities
The WHO Department of Public Health and Environment works across a range of activities and develops interventions to address the environmental and social determinants of child development. These include: child-only vulnerability to indoor and outdoor air pollution, water pollution, lack of basic hygiene, toxic compounds, heavy metals, waste components and radiation exposure; mixed impact of factors related to the social environment, professional activities and nutrition, as well as the living conditions of children (home, school).