What is strep b during pregnancy
Group B Strep and Pregnancy (for Parents)
What Is Group B Strep?
Group B Streptococcus (group B strep, GBS) is a type of
bacteriaoften found in the urinary tract, digestive system, and reproductive tracts. The bacteria come and go from our bodies, so most people who have it don't know that they do. GBS usually doesn't cause health problems.
What Problems Can Group B Strep Cause?
Health problems from GBS are not common. But it can cause illness in some people, such as the elderly and those with some medical conditions. GBS can cause infections in such areas of the body as the blood, lungs, skin, or bones.
About 1 out of every 4 women have GBS. In pregnant women, GBS can cause infection of the urinary tract, placenta, womb, and amniotic fluid.
Even if they haven't had any symptoms of infection, pregnant women can pass the infection to their babies during labor and delivery.
How Does Group B Strep Affect Babies?
When women with GBS are treated with antibiotics during labor, most of their babies do not have any problems. But some babies can become very sick from GBS. Premature babies are more likely to be infected with GBS than full-term babies because their bodies and immune systems are less developed.
The two types of GBS disease in babies are:
- Early-onset infections, which happen during the first week of life. Babies often have symptoms within 24 hours of birth.
- Late-onset infections, which develop weeks to months after birth. This type of GBS disease is not well understood.
What Are the Signs & Symptoms of GBS Disease?
Newborns and infants with GBS disease might show these signs:
- a fever
- feeding problems
- breathing problems
- irritability or fussiness
- inactivity or limpness
- trouble keeping a healthy body temperature
Babies with GBS disease can develop serious problems, such as:
- pneumonia
- sepsis
- meningitis (infection of the fluid and lining around the brain).
 Meningitis is more common with late-onset GBS disease and, in some cases, can lead to hearing loss, vision loss, learning disabilities, seizures, and even death.
Meningitis is more common with late-onset GBS disease and, in some cases, can lead to hearing loss, vision loss, learning disabilities, seizures, and even death.
How Is Group B Strep Diagnosed?
Pregnant women are routinely tested for GBS late in the pregnancy, usually between weeks 35 and 37. The test is simple, inexpensive, and painless. Called a culture, it involves using a large cotton swab to collect samples from the vagina and rectum. These samples are tested in a lab to check for GBS. The results are usually available in 1 to 3 days.
If a test finds GBS, the woman is said to be "GBS-positive." This means only that she has the bacteria in her body — not that she or her baby will become sick from it.
GBS infection in babies is diagnosed by testing a sample of blood or spinal fluid. But not all babies born to GBS-positive mothers need testing. Most healthy babies are simply watched to see if they have signs of infection.
How Is Group B Strep Treated?
Doctors will test a pregnant woman to see if she has GBS. If she does, she will get intravenous (IV) antibiotics during labor to kill the bacteria. Doctors usually use penicillin, but can give other medicines if a woman is allergic to it.
If she does, she will get intravenous (IV) antibiotics during labor to kill the bacteria. Doctors usually use penicillin, but can give other medicines if a woman is allergic to it.
It's best for a woman to get antibiotics for at least 4 hours before delivery. This simple step greatly helps to prevent the spread of GBS to the baby.
Doctors also might give antibiotics during labor to a pregnant woman if she:
- goes into labor prematurely, before being tested for GBS
- hasn't been tested for GBS and her water breaks 18 or more hours before delivery
- hasn't been tested for GBS and has a fever during labor
- had a GBS bladder infection during the pregnancy
- had a baby before with GBS disease
Giving antibiotics during labor helps to prevent early-onset GBS disease only. The cause of late-onset disease isn't known, so no method has yet been found to prevent it. Researchers are working to develop a vaccine to prevent GBS infection.
Babies who get GBS disease are treated with antibiotics. These are started as soon as possible to help prevent problems. These babies also may need other treatments, like breathing help and IV fluids.
How Can I Help Prevent Group B Strep Infection?
Because GBS comes and goes from the body, a woman should be tested for it during each pregnancy. Women who are GBS-positive and get antibiotics at the right time during labor do well, and most don't pass the infection to their babies.
If you are GBS-positive and begin to go into labor, go to the hospital rather than laboring at home. By getting IV antibiotics for at least 4 hours before delivery, you can help protect your baby against early-onset GBS disease.
Reviewed by: Thinh Phu Nguyen, MD
Date reviewed: July 2022
What are the risks of group B streptococcus (GBS) infection during pregnancy?
Most pregnant women who carry group B streptococcus (GBS) bacteria have healthy babies.
But there's a small risk that GBS can pass to the baby during childbirth.
Sometimes GBS infection in newborn babies can cause serious complications that can be life-threatening, but this is not common.
Extremely rarely, GBS infection during pregnancy can also cause miscarriage, early (premature) labour or stillbirth.
What is GBS?
GBS is one of many bacteria that can be present in our bodies. It does not usually cause any harm.
When this happens, it's called carrying GBS, or being colonised with GBS.
It's estimated between 2 and 4 women in every 10 in the UK carries GBS in their digestive system or vagina.
Around the time of labour and birth, many babies come into contact with GBS. Most are unaffected, but a small number can become infected and very unwell.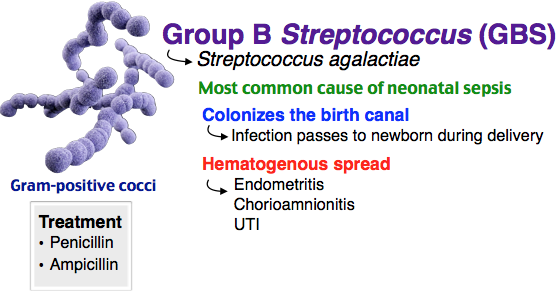
Early-onset GBS infection
If a baby develops GBS infection in the first week after birth, it's known as early-onset GBS infection.
Symptoms include:
- being floppy and unresponsive
- grunting when breathing, or working hard to breathe when you look at their chest or tummy
- a high or low temperature
- very fast or slow heart rate
- very fast or slow breathing
- changes in their skin colour, including blotchy skin
- not feeding well or vomiting milk
- crying and unable to settle
What complications can GBS infection cause?
Most babies who become infected can be treated successfully and will make a full recovery.
But even with the best medical care, the infection can sometimes cause life-threatening complications, such as sepsis or meningitis.
Rarely, GBS can cause infection in the mother. For example, in the womb or urinary tract or, more seriously, sepsis.
Preventing early-onset GBS infection
The Royal College of Obstetricians and Gynaecologists (RCOG) has more information on GBS infection in newborn babies
If you have GBS, or you've had a baby who's been affected by it before, you should be offered antibiotics during labour to reduce the risk of your baby getting ill.
If there's a chance your new baby could have GBS, you might be advised to stay in hospital for at least 12 hours after the birth so they can be checked regularly for signs of infection.
For more information, see Is my baby at risk of early-onset GBS infection?
Late-onset GBS infection
Late-onset GBS infection develops 7 or more days after a baby is born. This is not usually associated with pregnancy.
This is not usually associated with pregnancy.
The baby probably became infected after the birth. For example, they may have caught the infection from someone else.
The symptoms of late-onset GBS are the same as early-onset GBS. Call 999 or take your baby to A&E if they have symptoms of GBS.
GBS infections after 3 months of age are extremely rare.
Breastfeeding does not increase the risk of GBS infection and will protect your baby against other infections.
Further information
- Infections in pregnancy that may affect your baby
- Group B strep
- Group B Strep Support website
Page last reviewed: 3 August 2022
Next review due: 3 August 2025
Infections during pregnancy. Detection of group B streptococcus
05/16/2017
Infections during pregnancy that can be transmitted from mother to fetus deserve great attention, as they carry a potential risk of infection of the fetus or newborn and may lead to undesirable consequences.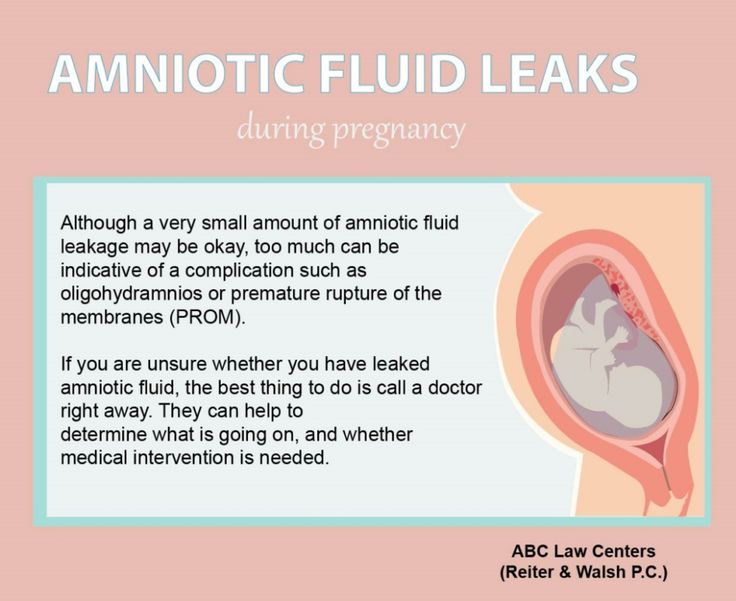 In addition, the diagnosis of infections during pregnancy has certain characteristics due to the asymptomatic course of most maternal infections or non-specific signs and symptoms. nine0003
In addition, the diagnosis of infections during pregnancy has certain characteristics due to the asymptomatic course of most maternal infections or non-specific signs and symptoms. nine0003
Group B Streptococcus (GBS, Streptococcus agalactiae ) - Causes severe neonatal illness and poses a risk to certain patients in other age groups.
It has been estimated that GBS in 30% of pregnant women can be found in the vagina and often in the urethra of their sexual partners. Despite the fact that GBS can occur as part of the normal intestinal microflora of a woman, their colonization of the urogenital tract of a pregnant woman poses a significant risk to the fetus due to the possibility of ascending infection. There is a significant relationship between the carriage of GBS in the vagina, not only with early infection of newborns (sepsis, pneumonia and meningitis), but also with premature birth, premature discharge of amniotic fluid, urinary infection in pregnant women, development of chorioamnionitis during childbirth, endometritis.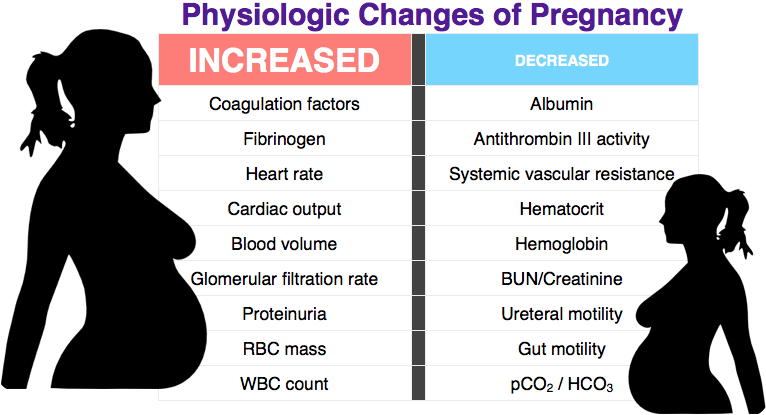 nine0003
nine0003
In the USA, Canada and European countries, regulated National programs for the prevention and treatment of GBS infections have been adopted, which are mandatory for all medical institutions.
From 01.05.17, DILA ML introduces a new study “Identification of group B streptococcus (streptococcus agalactiae) with sensitivity to antibiotics”.
| Prompt identification of pregnant women who are positive for group B streptococcus and who have risk factors for an increased chance of infection in the newborn allows to conduct intravenous antibiotic prophylaxis with the onset of labor and prevent early infection of the newborn with group B streptococcus:
|
Rules for preparation : 24 hours before the use of intravaginal and rectal medications should be excluded, before taking the biomaterial, do not wash the external genital organs.
The biomaterial is taken from two points: the lower third of the vagina and the next - the rectum, the overall result is evaluated. nine0059 Detection of group B streptococcus is carried out by a cultural method with the determination of sensitivity to antibiotics.
Research period: 6 days (Kyiv), 7.5 days (Regions).
Adequate assessment of the risk of infection of the newborn with group B streptococcus will significantly reduce the possibility of complications and ensure a favorable pregnancy outcome.
Literature:
1. Australasian society for infectious diseases, 2014
2. Antibiotic Prevention for Maternal Group B Streptococcal Colonization on Neonatal GBS-Related Adverse Outcomes: A Meta-Analysis, Shunming Li, Jingya Huang, 2017.
3. Early onset Group B Streptococcal disease Queensland clinical guidelines, 2016
4. Effect of group B streptococci colonizing the urogenital tract of pregnant women on the course and outcome of pregnancy / Oganyan K.A., Zatsiorskaya S.L., Arzhanova O.N., Savicheva A.M. – St. Petersburg, 2014
5. Digest of professional medical information. Congenital and perinatal infections: prevention, diagnosis and treatment. / Catherine S. Peckham. - No. 1 (4). – 2008.
0 0
Rate satisfaction
DILA for you
Clinical consulting service for clinical support of doctors and patients before visiting a doctor
0-800-600-911
Bacterial infections during pregnancy
Among the inflammatory diseases of bacterial origin that occur during pregnancy, a significant place is occupied by conditions caused by disturbances in the normal microflora of the genitourinary tract. The microflora of the vagina is characterized by a wide variety of bacterial species and is divided into flora characteristic of healthy women (obligate) and pathological. With adverse external influences, in stressful situations, with a decrease in the body's immunological defense, with hormonal disorders, gynecological diseases, qualitative and quantitative changes in the microflora can occur in the genital tract. A decrease in the number of bacteria belonging to the normal microflora in the vagina leads to a decrease in protective barriers in the vagina, and to excessive reproduction of opportunistic microorganisms. Violations of the normal microflora of the birth canal pose a great danger to pregnant women, as they can lead to abortion, premature birth, intrauterine infection of the fetus and postpartum inflammatory complications in puerperas. nine0003
The microflora of the vagina is characterized by a wide variety of bacterial species and is divided into flora characteristic of healthy women (obligate) and pathological. With adverse external influences, in stressful situations, with a decrease in the body's immunological defense, with hormonal disorders, gynecological diseases, qualitative and quantitative changes in the microflora can occur in the genital tract. A decrease in the number of bacteria belonging to the normal microflora in the vagina leads to a decrease in protective barriers in the vagina, and to excessive reproduction of opportunistic microorganisms. Violations of the normal microflora of the birth canal pose a great danger to pregnant women, as they can lead to abortion, premature birth, intrauterine infection of the fetus and postpartum inflammatory complications in puerperas. nine0003
Physiological and biological changes that occur in the genital tract during pregnancy lead to the fact that the vaginal microflora becomes more homogeneous with a predominance of lactic acid bacilli (lactobacilli).
There are a number of factors that control and influence the composition of the normal vaginal microflora. The vaginal environment affects the microflora, providing conditions for the possible presence in certain quantities of various types of microorganisms. In general, the vaginal microflora includes various types of microorganisms. Vaginal discharge normally contains 108-1010 microorganisms per 1 ml, while aerobic bacteria are 105-108, anaerobic 108-109cfu/ml Lactobacilli dominate in the microbial flora of the vagina and cervix. It should be noted that bifidobacteria are more common in pregnant women than lactobacilli, and this fact is regarded as a reaction to the absence or inhibition of lactobacilli. In general, anaerobic organisms prevail over aerobic and facultative anaerobic organisms. Among aerobic bacteria, diphtheroids, staphylococci, streptococci are most often detected, and among anaerobic bacteria - lactobacilli, bifidobacteria, peptostreptococci, prevotella and bacteroids. nine0003
nine0003
streptococcal infection
The family of these microorganisms includes several genera of morphologically similar gram-positive cocci, which are facultative anaerobes. There are serological groups of streptococci A, B, C, D, E, F, G and H. According to the appearance of the colonies and the nature of hemolysis on blood agar, these pathogens are divided into hemolytic, green and non-hemolytic species. Three groups of streptococci can be present in the vagina of healthy women: streptococci of the viridans group (green streptococci), serogroup B streptococci, and serogroup D streptococci (enterococci). The frequency of detection and the number of streptococci belonging to these groups varies significantly and normally does not exceed 104 CFU / ml. During pregnancy, from the point of view of possible infection, pathogens such as Streptococcus pyogenes (group A beta-hemolytic streptococcus) and Streptococcus agalactiae (group B streptococcus, which has recently become the most common cause of infections in both newborns, especially premature ones, so do their mothers). nine0003
nine0003
Diseases caused by Streptococcus pyogenes
About 20% of pregnant women are carriers (nasopharynx, vagina and perianal area). A pregnant woman may experience: tonsillitis, pharyngitis, pyoderma, urinary infection, chorionamnionitis, endometritis, postpartum sepsis. The infection can be transmitted to the child at birth, with subsequent risk of neonatal sepsis increased, especially with prolonged anhydrous interval.
nine0108 The main diagnostic method is a culture method (on blood agar aerobically and anaerobically).
In the treatment prescribed antibiotics from the group of penicillins and cephalosporins for at least 10 days. In postpartum sepsis, high doses of parenteral benzylpenicillin or ampicillin are prescribed. Newborns with streptococcal infections are also given high doses of benzylpenicillin, ampicillin, or cephalosporins. nine0003
Due to the fact that Streptococcus pyogenes is transmitted by contact, prevention is to comply with the rules of asepsis during childbirth.
Diseases caused by Streptococcus agalactiae
This type of streptococcus is part of the vaginal microflora in 20% of pregnant women. With a disease in a pregnant woman, asymptomatic bacterial colonization of the vagina and perianal area, urinary tract infection, chorionamnionitis, endometritis can be observed. nine0003
The main diagnostic method is a cultural method. The more intense the infection of the pregnant woman, the more likely the infection of the child. With delivery through the natural birth canal, the frequency of transmission of infection to the child is 50-60%. The risk of disease in a full-term baby is 1-2%, and in a premature baby - 15--20%, with a period of less than 28 weeks of pregnancy - 100%. If a child is infected during childbirth, sepsis, pneumonia, meningitis, and severe neurological complications may develop. In severe cases, the disease begins immediately after birth and progresses rapidly. The risk for the child increases with premature rupture of the membranes, premature birth, symptoms of chorionamnionitis in the mother. nine0003
nine0003
When prescribing treatment it should be taken into account that group B streptococci are sensitive to all beta-lactam antibiotics, cephalosporins. If streptococci are detected in a pregnant woman, even without clinical symptoms, penicillin therapy is necessary for 10 days, cephalosporins and macrolides may be used.
Prevention. According to some studies, the appointment of ampicillin to a woman in labor prevents infection with Streptococcus agalactiae. The disadvantages of prophylactic administration of ampicillin include the need for a preliminary bacteriological study. It is advisable to screen all pregnant women in the third trimester for the presence of group B streptococci using gynecological culture. nine0003
Bacterial vaginosis
Among bacterial diseases in pregnant women, a large proportion are pathological conditions associated with violations of the normal microflora of the genital tract. Bacterial vaginosis is a clinical syndrome caused by a pathological change in the structure of the microbial environment of the vagina. In patients with bacterial vaginosis, concentrations of facultative and anaerobic bacteria predominate to a large extent, which displace lactic acid bacilli, which leads to significant changes in the vaginal microflora. The main feature of the violation of the composition of the normal vaginal microflora in bacterial vaginosis is a significant decrease in the number of lactic acid bacilli and a pronounced colonization of the vagina by anaerobic bacteria (Prevotella/Porphyromonas spp., Peptostreptococcus spp., Fusobacteium spp., Mobiluncus spp.) and Gardnerella vaginalis. nine0003
In patients with bacterial vaginosis, concentrations of facultative and anaerobic bacteria predominate to a large extent, which displace lactic acid bacilli, which leads to significant changes in the vaginal microflora. The main feature of the violation of the composition of the normal vaginal microflora in bacterial vaginosis is a significant decrease in the number of lactic acid bacilli and a pronounced colonization of the vagina by anaerobic bacteria (Prevotella/Porphyromonas spp., Peptostreptococcus spp., Fusobacteium spp., Mobiluncus spp.) and Gardnerella vaginalis. nine0003
During pregnancy, the reasons for the violation of the normal composition of the microflora of the vagina may be the corresponding hormonal changes, the use of antibiotics, etc. More than half of all women with bacterial vaginosis have some kind of subjective complaints and pathological secretions from the genital tract (leucorrhoea) are absent, along with the available positive laboratory signs. Inflammatory reaction of the vaginal epithelium is not a characteristic sign bacterial vaginosis .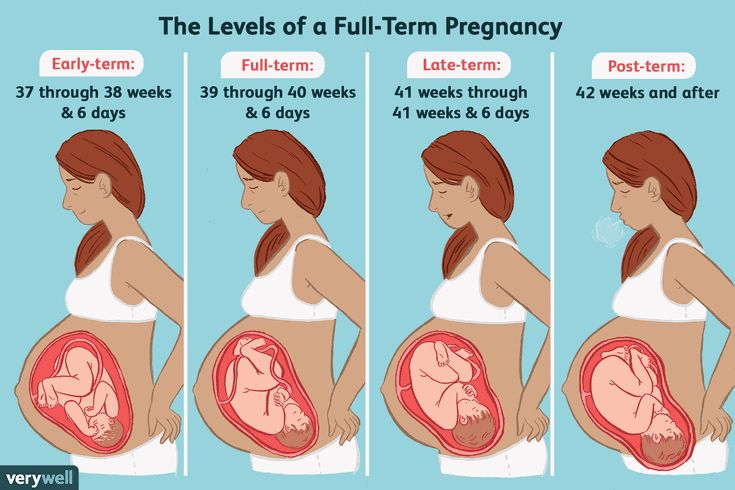 In the clinical variant of the course of bacterial vaginosis with severe symptoms, prolonged abundant, liquid, milky or grayish-white homogeneous discharge (leucorrhoea), mainly with an unpleasant fishy odor, is noted. nine0003
In the clinical variant of the course of bacterial vaginosis with severe symptoms, prolonged abundant, liquid, milky or grayish-white homogeneous discharge (leucorrhoea), mainly with an unpleasant fishy odor, is noted. nine0003
Bacterial vaginosis occurs in 15 - 20% of pregnant women, and is a serious risk factor for the development of infectious complications. A pronounced relationship of bacterial vaginosis with premature termination of pregnancy and untimely rupture of the amniotic membranes was noted. The risk of developing these complications compared with healthy pregnant women in patients with bacterial vaginosis increases by 2.6 times. Approximately 10% of preterm women give birth to gardnerella and other microorganisms from the amniotic fluid, while normally the amniotic fluid is sterile. It was noted that in women who gave birth before 37 weeks. there is a high probability of having bacterial vaginosis. nine0003
Chorioamnionitis, detected in 1% of pregnant women, is a severe complication that threatens the life of the mother and fetus. The development of chorionamnionitis associated with bacterial vaginosis in the mother can subsequently lead to premature abortion or premature rupture of amniotic fluid. The presence of chorionamnionitis in patients with bacterial vaginosis is histologically confirmed by the identification of relevant pathogenic microorganisms in the placental tissue, which can also be the cause. premature birth . nine0003
The development of chorionamnionitis associated with bacterial vaginosis in the mother can subsequently lead to premature abortion or premature rupture of amniotic fluid. The presence of chorionamnionitis in patients with bacterial vaginosis is histologically confirmed by the identification of relevant pathogenic microorganisms in the placental tissue, which can also be the cause. premature birth . nine0003
There is also a relationship between the presence of bacterial vaginosis and the development of postpartum endometritis including after caesarean section. The risk of developing postpartum endometritis in pregnant women with bacterial vaginosis is 10 times higher than in healthy women. The microbial flora detected in the endometrium in patients with endometritis is often similar to that in bacterial vaginosis. This is especially true for anaerobic microorganisms. Mixed microflora in bacterial vaginosis can lead to the development of other inflammatory complications, such as breast abscess, inflammation of the umbilical wound, etc. nine0003
nine0003
Thus, patients with bacterial vaginosis are at increased risk for the development of inflammatory diseases of the pelvic organs, premature termination of pregnancy, untimely rupture of amniotic fluid, the occurrence of chorionamnionitis, postpartum and postoperative endometritis. The high concentration of virulent microorganisms in the vagina of patients suffering from bacterial vaginosis is a risk factor for the penetration of bacteria into the higher parts of the genitourinary system. nine0003
Diagnostics - the complex includes four diagnostic tests
- during an external gynecological examination of the patient in the area of the vestibule of the vagina, leucorrhoea typical of bacterial vaginosis is noted. If the discharge is too profuse, it may also drain to the perineum. In this case, usually the external genital organs are not hyperemic and not edematous. However, in the presence of concomitant infection, edema and hyperemia of the vaginal mucosa are observed; nine0042
- PH value of vaginal discharge in patients with bacterial vaginosis is usually 5.
 0 - 6.0;
0 - 6.0; - a positive amine test, which is accompanied by the appearance of an unpleasant fishy odor when exposed to a 10% potassium hydroxide solution on a sample of the contents from the middle third of the vagina;
- detection by microscopy in the discharge from the vagina of "key cells", which are mature cells of the vaginal epithelium with microorganisms adhered to them in large numbers, which are located mostly chaotically. nine0042
Microscopic analysis of vaginal secretions is the method of final diagnosis, including Gram-stained smears.
Treatment of bacterial vaginosis
In the first trimester of pregnancy, for the treatment of bacterial vaginosis, it is possible to prescribe clindamycin 2% in the form of a vaginal cream of 5.0 g for 3-7 days or povidone-iodine 1 vaginal suppository per day for 14 days or from the 10th week Terzhinan 1 vaginal tablet 10 days. nine0003
In II trimester of pregnancy the arsenal of drugs for the treatment of bacterial vaginosis can be supplemented with Clotrimazole 1 vaginal tablet for 10 days, as well as oral administration of Clindamycin 300 mg 2 times - 7 days.
In the III trimester, in addition to the listed drugs, Ornidazole 500 mg 2 times - 5 days, or Metronidazole 500 mg 2 times - 7 days, as well as Viferon-2 Suppositories or KIP-feron 1 suppository 2 times 10 days rectally can be used. nine0003
Gonorrhea
The causative agent of the disease is Neisseria gonorrhoeae - Gram-negative bacteria sensitive to light, cold and dryness. Outside the human body, these pathogens are not able to live long. The infection is transmitted by sexual infection. When infected, gonococci are detected in the urethra, the large gland of the vestibule, the cervix, tubes and peritoneum. The infection can spread through the mucous membranes of the endometrium and pelvic organs. nine0003
In 80% of women, gonorrhea is asymptomatic, with cervical lesions observed in more than 50% of cases, rectum - more than 85%, pharynx - more than 90%. The presence of gonorrhea in a pregnant woman is a significant risk factor for adverse outcomes for both mother and fetus. In women who contract gonorrhea after 20 weeks of pregnancy or after childbirth increases the risk of developing gonococcal arthritis. In acute gonorrhea, there is an increased risk of premature rupture of amniotic fluid, spontaneous abortion, and preterm birth. Chronic gonorrhea may worsen immediately after childbirth, with an increased risk of gonococcal sepsis. nine0003
In women who contract gonorrhea after 20 weeks of pregnancy or after childbirth increases the risk of developing gonococcal arthritis. In acute gonorrhea, there is an increased risk of premature rupture of amniotic fluid, spontaneous abortion, and preterm birth. Chronic gonorrhea may worsen immediately after childbirth, with an increased risk of gonococcal sepsis. nine0003
Infection of the fetus occurs in utero or during childbirth. intrauterine infection manifested by gonococcal sepsis in the newborn and chorionamnionitis. Infection during childbirth can lead to gonococcal conjunctivitis, otitis externa, and vulvovaginitis.
If gonorrhea is suspected, a study is made of discharge from the vagina and cervix. An indicative diagnosis is established when pathogens of gonorrhea are detected in a smear. To confirm the diagnosis, sowing of the discharge on a special medium is used. Also use the PCR method. nine0003
Treatment of gonorrhea in pregnant women
Treatment of pregnant women at any gestational age should be carried out in a hospital. Treatment of disseminated gonorrhea should be carried out with the involvement of specialists of the appropriate profile. In the treatment of the disease, pregnant women with gonococcal urethritis, endocervicitis, proctitis or pharyngitis are prescribed ceftriaxone 250 mg intramuscularly or spectinomycin (trobicin) 2.0 g intramuscularly once. With gonococcal sepsis, ceftriaxone is prescribed 1 g intravenously or intramuscularly 1 time per day for 7-10 days. 7 days after the end of treatment, repeated crops are carried out. With ophthalmic rhea of newborns, ceftriaxone is used at a dose of 25-50 mg / kg intravenously or intramuscularly once and frequent washing of the conjunctiva with isotonic sodium chloride solution. nine0003
Treatment of disseminated gonorrhea should be carried out with the involvement of specialists of the appropriate profile. In the treatment of the disease, pregnant women with gonococcal urethritis, endocervicitis, proctitis or pharyngitis are prescribed ceftriaxone 250 mg intramuscularly or spectinomycin (trobicin) 2.0 g intramuscularly once. With gonococcal sepsis, ceftriaxone is prescribed 1 g intravenously or intramuscularly 1 time per day for 7-10 days. 7 days after the end of treatment, repeated crops are carried out. With ophthalmic rhea of newborns, ceftriaxone is used at a dose of 25-50 mg / kg intravenously or intramuscularly once and frequent washing of the conjunctiva with isotonic sodium chloride solution. nine0003
As a control for treatment, sowing is carried out after the end of treatment after 7 days and after 4 weeks.
As a preventive measure during the initial examination of a pregnant woman, it is necessary to sow the discharge from the cervix for gonorrhea.