What is german measles
Rubella (German Measles) (for Parents)
What Is Rubella?
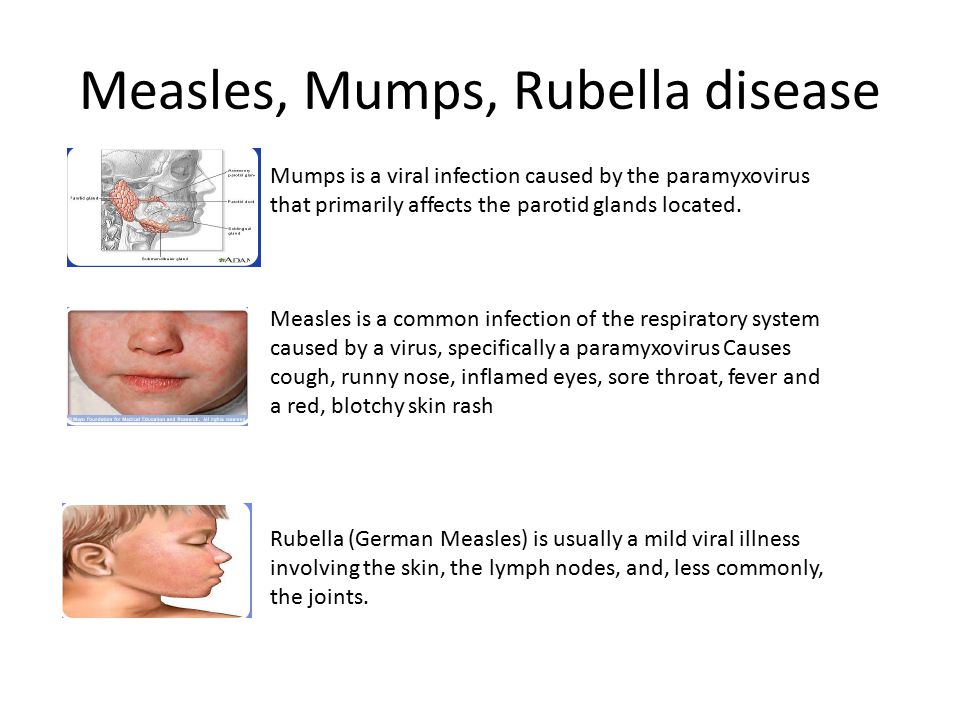
Rubella is an infection that mostly affects the skin and lymph nodes. In kids, rubella — commonly called German measles or 3-day measles — is usually a mild illness. But the infection is dangerous for pregnant women because it can cause serious health problems in their babies.
Rubella is caused by the rubella (roo-BELL-uh) virus (not the same virus that causes measles). It spreads when people breathe in virus-infected fluid.
Before the rubella vaccine, epidemics happened every 6-9 years, usually among kids 5 to 9 years old, along with many cases of congenital rubella. Thanks to immunization, there are far fewer cases of rubella and congenital rubella.
What Are the Signs & Symptoms of Rubella?
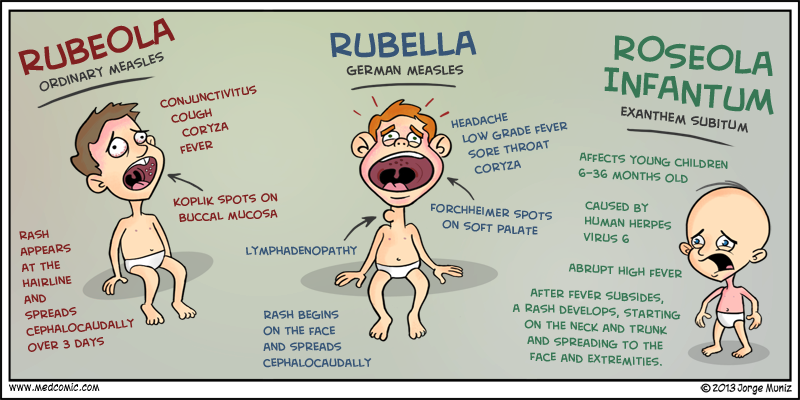
Rubella infection may begin with 1–2 days of mild fever (99°–100°F, 37.2°–37.8°C) and swollen, tender lymph nodes, usually in the back of the neck or behind the ears. A rash then begins on the face and spreads downward. As it spreads, it usually clears on the face.
The rubella rash is often the first sign of illness that a parent notices. It can look like many other viral rashes, appearing as either pink or light red spots, which may merge to form evenly colored patches. The rash can itch and lasts up to 3 days. As the rash clears, the affected skin might shed in very fine flakes.
Other symptoms of rubella, which are more common in teens and adults, can include headache, loss of appetite, mild conjunctivitis (inflammation of the lining of the eyelids and eyeballs), a stuffy or runny nose, swollen
lymph nodesin other parts of the body, and pain and swollen joints. Many people with rubella have few or no symptoms.
The rubella rash usually lasts 3 days. Lymph nodes may be swollen for a week or more, and joint pain can last for more than 2 weeks. Children who have rubella usually recover within 1 week, but adults may take longer.
Is Rubella Contagious?
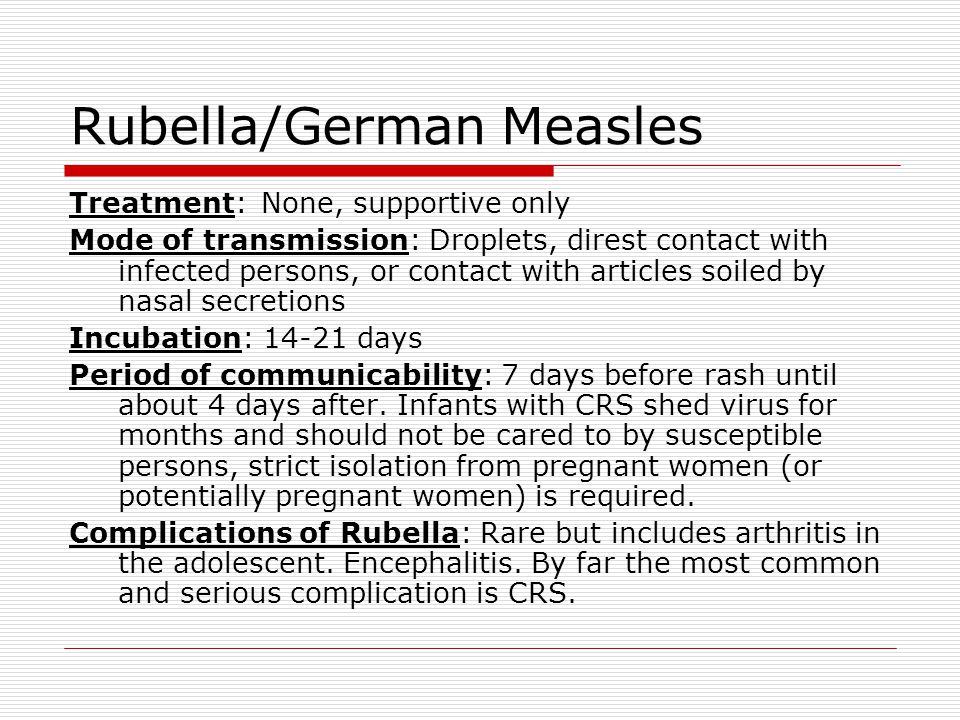
Rubella is contagious, and passes from person to person through tiny drops of fluid from the nose and throat through sneezing and coughing.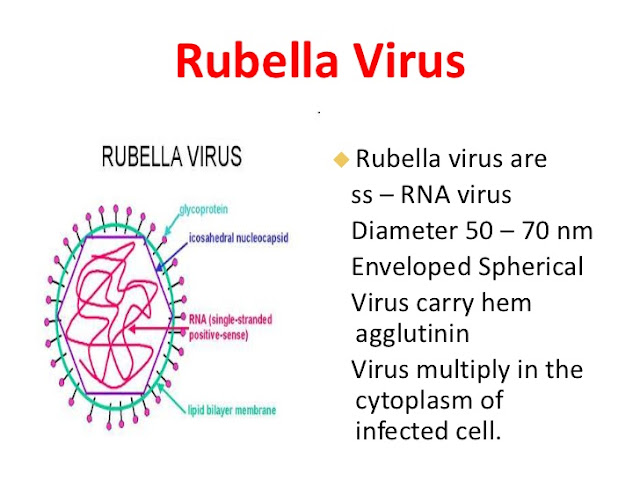 Someone also can get it by sharing food or drink with a person who's infected. People who have rubella are most contagious from 1 week before to 1 week after the rash appears. Someone who is infected but has no symptoms can still spread the virus.
Someone also can get it by sharing food or drink with a person who's infected. People who have rubella are most contagious from 1 week before to 1 week after the rash appears. Someone who is infected but has no symptoms can still spread the virus.
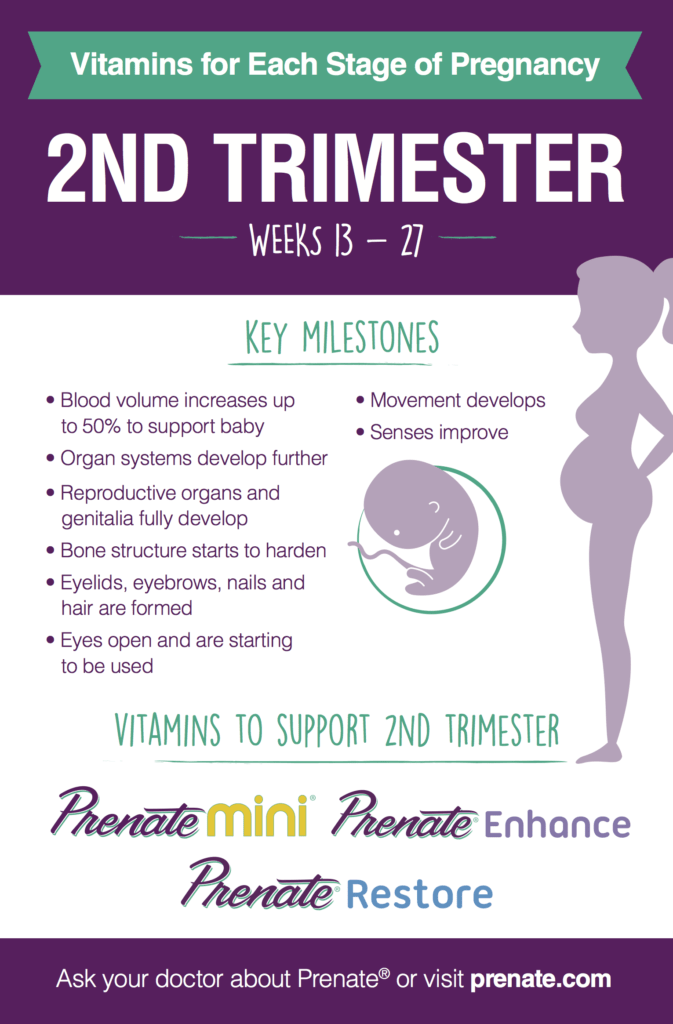
The virus also can pass through a pregnant woman's bloodstream to infect her unborn child. Babies born with congenital rubella syndrome are at risk for serious problems with their growth, thinking, heart and eyes, hearing, and liver, spleen, and bone marrow. They also can shed the virus in their urine (pee) and fluid from their nose and throat for a year or more, so can pass the virus to people who aren't immunized against it.
Can Rubella Be Prevented?
The rubella vaccine protects people from the disease. Widespread immunization is the key to preventing the spread of the virus and protecting babies from the serious health problems of congenital rubella syndrome.
Most rubella infections today are in young, non-immunized adults rather than in kids.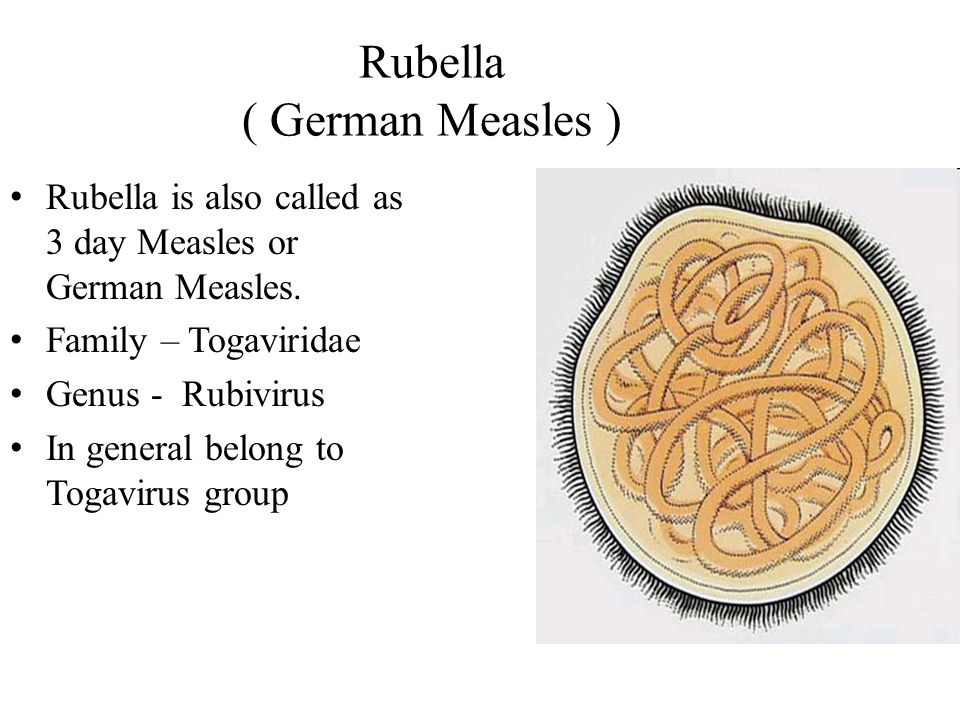 In fact, experts say that about 10% of young adults are not vaccinated against rubella, which could be dangerous for any children they might have someday.
In fact, experts say that about 10% of young adults are not vaccinated against rubella, which could be dangerous for any children they might have someday.
Children usually get the vaccine at 12–15 months of age as part of the scheduled measles-mumps-rubella (MMR) immunization or measles-mumps-rubella-varicella vaccine (MMRV). Most get a second dose at 4–6 years of age. As with all immunization schedules, there are important exceptions and special circumstances. For example, a child who will travel outside the United States can get the vaccine as early as 6 months of age. Talk to your doctor to see when your child should get the vaccine.
The rubella vaccine should not be given to pregnant women or to a woman who plans to become pregnant within 1 month of getting it. If you are thinking about becoming pregnant, make sure that you're immune to rubella through a blood test or proof of immunization. If you're not immune, get the vaccine at least 1 month before you become pregnant.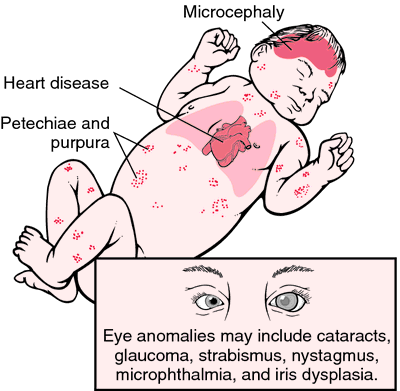
Pregnant women who are not immune should avoid anyone who has the illness, then get the vaccine after their baby is born so they'll be immune during any future pregnancies.
How Is Rubella Treated?
Antibiotics can't treat rubella because they only work against bacteria, not viruses. Unless it causes other problems, rubella will get better on its own. Rubella usually is mild in kids, who often can be cared for at home. Check your child's temperature and call the doctor if the fever climbs too high.
To ease minor discomfort, you can give your child acetaminophen or ibuprofen. Never give aspirin to a child who has a viral illness, as such use is linked to a serious condition called Reye syndrome.
When Should I Call the Doctor?
Call the doctor if your child seems to be getting sicker or has symptoms that don't seem mild.
If a pregnant woman is exposed to rubella, she should contact her doctor right away.
Rubella - Symptoms and causes
Overview
Rubella
Rubella
Rubella results in a fine, pink rash that appears on the face, the trunk (shown in image), and then the arms and legs.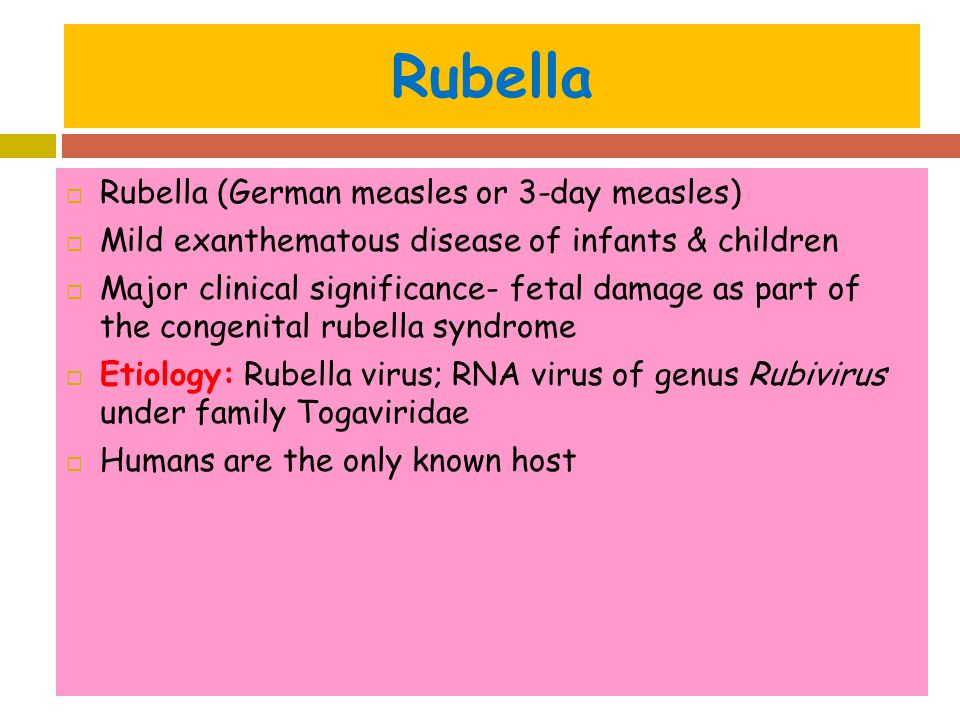
Rubella is a contagious viral infection best known by its distinctive red rash. It's also called German measles or three-day measles. This infection may cause mild or no symptoms in most people. However, it can cause serious problems for unborn babies whose mothers become infected during pregnancy.
Rubella isn't the same as measles, but the two illnesses share some signs and symptoms, such as the red rash. Rubella is caused by a different virus than measles, and rubella isn't as infectious or as severe as measles.
The measles-mumps-rubella (MMR) vaccine is safe and highly effective in preventing rubella. The vaccine provides lifelong protection against rubella.
In many countries, rubella infection is rare or even nonexistent. However, because the vaccine isn't used everywhere, the virus still causes serious problems for babies whose mothers are infected during pregnancy.
Products & Services
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Book: Mayo Clinic Guide to Raising a Healthy Child
Symptoms
The signs and symptoms of rubella are often difficult to notice, especially in children. Signs and symptoms generally appear between two and three weeks after exposure to the virus. They usually last about 1 to 5 days and may include:
Signs and symptoms generally appear between two and three weeks after exposure to the virus. They usually last about 1 to 5 days and may include:
- Mild fever of 102 F (38.9 C) or lower
- Headache
- Stuffy or runny nose
- Red, itchy eyes
- Enlarged, tender lymph nodes at the base of the skull, the back of the neck and behind the ears
- A fine, pink rash that begins on the face and quickly spreads to the trunk and then the arms and legs, before disappearing in the same order
- Aching joints, especially in young women
When to see a doctor
Contact your health care provider if you think you or your child may have been exposed to rubella or if you notice the signs or symptoms that may be rubella.
If you're considering getting pregnant, check your vaccination record to make sure you've received your MMR vaccine. If you're pregnant and you develop rubella, especially during the first trimester, the virus can cause death or serious birth defects in the developing fetus.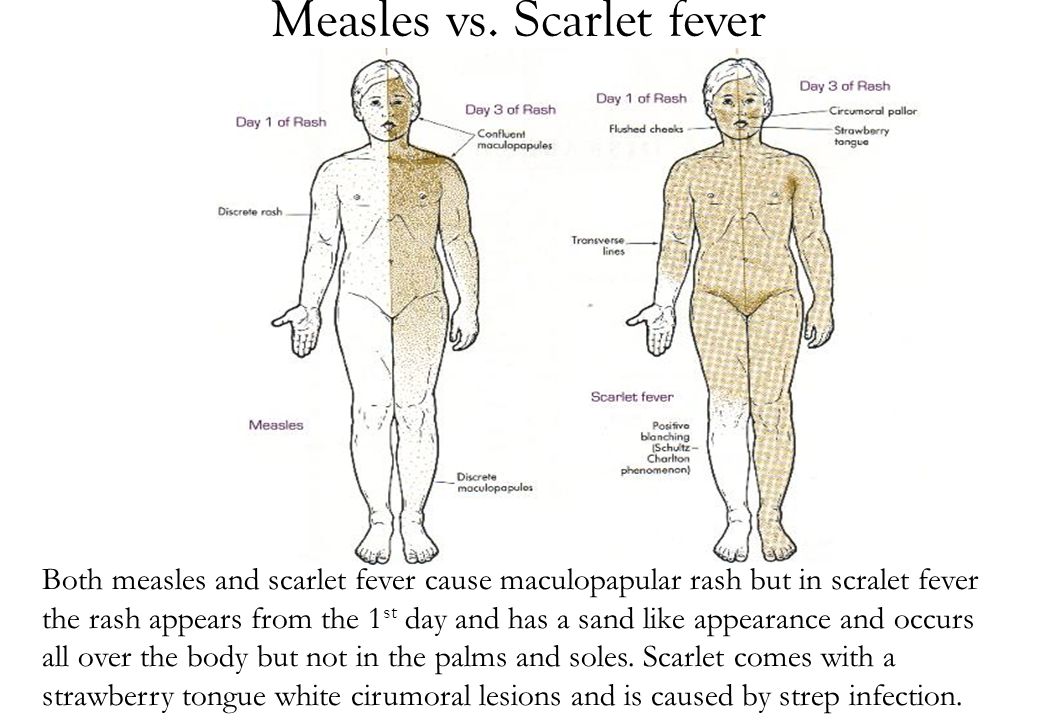 Rubella during pregnancy is the most common cause of congenital deafness. It's best to be protected against rubella before pregnancy.
Rubella during pregnancy is the most common cause of congenital deafness. It's best to be protected against rubella before pregnancy.
If you're pregnant, you'll likely undergo a routine screening for immunity to rubella. But if you've never received the vaccine and you think you might have been exposed to rubella, contact your health care provider immediately. A blood test might confirm that you're already immune.
Request an Appointment at Mayo Clinic
Causes
Rubella is caused by a virus that's passed from person to person. It can spread when an infected person coughs or sneezes. It can also spread by direct contact with infected mucus from the nose and throat. It can also be passed on from pregnant women to their unborn children through the bloodstream.
A person who has been infected with the virus that causes rubella is contagious for about one week before the onset of the rash until about one week after the rash disappears. An infected person can spread the illness before the person realizes he or she has it.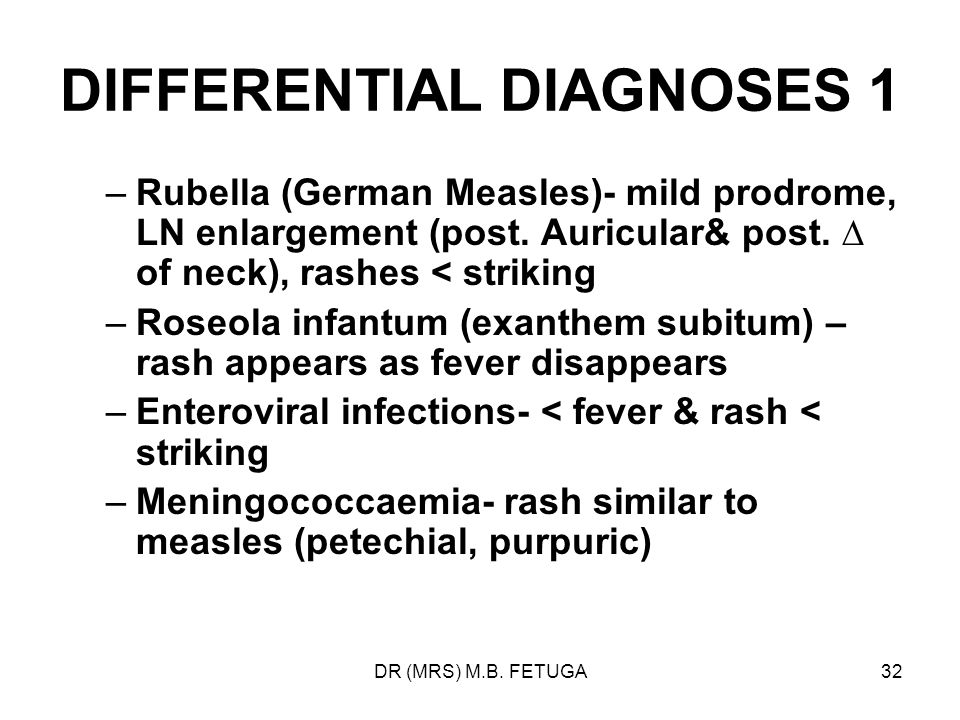
Rubella is rare in many countries because most children are vaccinated against the infection at an early age. In some parts of the world, the virus is still active. This is something to consider before going abroad, especially if you're pregnant.
Once you've had the disease, you're usually permanently immune.
Complications
Rubella is a mild infection. Some women who have had rubella experience arthritis in the fingers, wrists and knees, which generally lasts for about one month. In rare cases, rubella can cause an ear infection or inflammation of the brain.
However, if you're pregnant when you get rubella, the effect on your unborn child may be severe, and in some cases, fatal. Up to 90% of infants born to mothers who had rubella during the first 12 weeks of pregnancy develop congenital rubella syndrome. This syndrome can cause one or more problems, including:
- Growth delays
- Cataracts
- Deafness
- Problems with the development of the heart (congenital heart defects)
- Problems with the development of other organs
- Problems with mental development and learning
The highest risk to the fetus is during the first trimester, but exposure later in pregnancy also is dangerous.
Prevention
The rubella vaccine is usually given as a combined measles-mumps-rubella (MMR) vaccine. This vaccine may also include the chickenpox (varicella) vaccine ⸺ MMRV vaccine. Health care providers recommend that children receive the MMR vaccine between 12 and 15 months of age, and again between 4 and 6 years of age — before entering school.
The MMR vaccine prevents rubella and protects against it for life. Getting the vaccine can prevent rubella during future pregnancies.
Babies born to women who have received the vaccine or who are already immune are usually protected from rubella for 6 to 8 months after birth. If a child requires protection from rubella before 12 months of age — for example, for certain foreign travel — the vaccine can be given as early as 6 months of age. But children who are vaccinated early still need to be vaccinated at the recommended ages later.
Providing the MMR vaccine as a combination of recommended vaccines can prevent delays in protection against measle, mumps and rubella ⸺ and with fewer shots.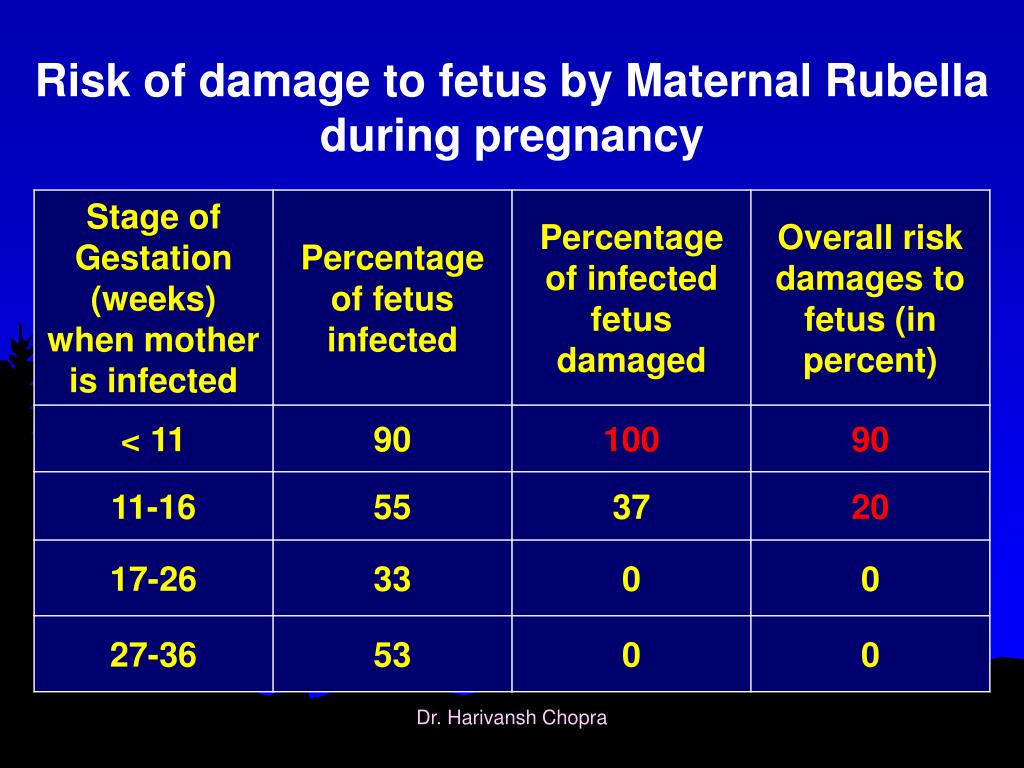 The combination vaccine is as safe and effective as the vaccines given separately.
The combination vaccine is as safe and effective as the vaccines given separately.
No proven link between the MMR vaccine and autism
Widespread concerns have been raised about a possible link between the MMR vaccine and autism. However, extensive reports from the American Academy of Pediatrics, the National Academy of Medicine, and the Centers for Disease Control and Prevention conclude that there is no scientifically proven link between the MMR vaccine and autism.
These organizations note that autism is often identified in toddlers between the ages of 18 and 30 months, which is about the time children are given their first MMR vaccine. But this coincidence in timing shouldn't be mistaken for a cause-and-effect relationship.
Do you need the MMR vaccine?
You don't need a vaccine if you:
- Had two doses of the MMR vaccine after 12 months of age.

- Have blood tests that show you're immune to measles, mumps and rubella.
- Were born before 1957. People born before 1957 are likely to have had measles, mumps and rubella during childhood and are immune. However, without a blood test that shows immunity, the MMR vaccine is recommended.
Get a vaccine if you have not had two doses of the MMR vaccine after age 12 months or a blood test to show that you're immune to measles, mumps and rubella.
Ensuring immunity is especially important if you:
- Are a nonpregnant woman of childbearing age
- Attend college, trade school or postsecondary school
- Work in a hospital, medical facility, child-care center or school
- Plan to travel overseas or take a cruise
The vaccine is not recommended for:
- Pregnant women or women who plan to get pregnant within the next four weeks
- People who have had a life-threatening allergic reaction to gelatin, the antibiotic neomycin or a previous dose of MMR vaccine
If you have cancer, a blood disorder or another disease, or you take medication that affects your immune system, talk to your health care provider before getting an MMR vaccine.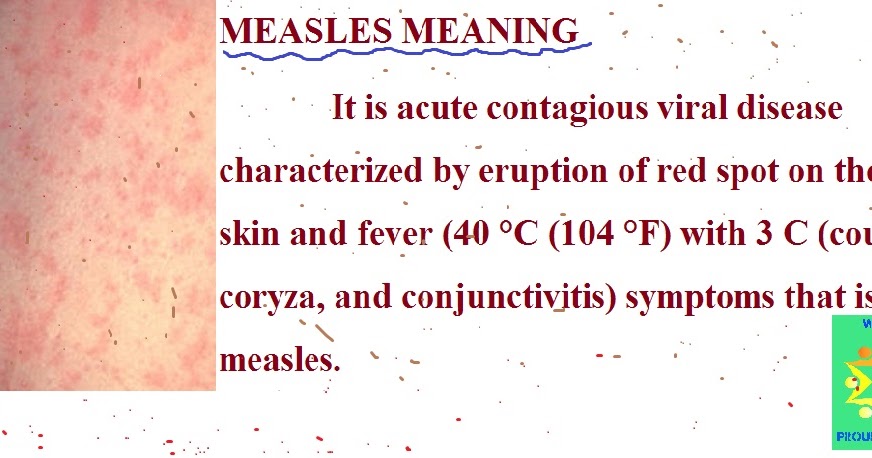
Side effects of the vaccine
Most people experience no side effects from the vaccine.
For some people, minor side effects may appear about two weeks after vaccination, but usually occur less often after the second shot. These can include:
- Sore arm at the injection site
- Fever
- Mild rash or redness at the injection site
Very few people experience:
- Temporary joint pain or stiffness, especially in teens and adult women who weren't previously immune to rubella
- Swelling of the glands in the cheeks or neck
- Seizures that occur with a fever
- Low level of cells in the blood that help with clotting (platelets), which can cause unusual bleeding or bruising
- Rash all over the body
- Serious allergic reaction, very rarely
After a diagnosis
If you've been exposed to the virus and get rubella, you can help keep friends, family and co-workers safe by telling them about your diagnosis.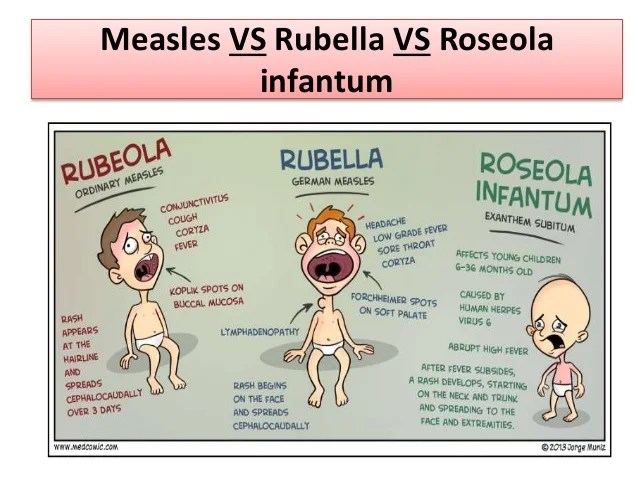 If your child has rubella, let the school or child-care provider know.
If your child has rubella, let the school or child-care provider know.
By Mayo Clinic Staff
Related
Products & Services
Rubella
Rubella- Healthcare issues »
- A
- B
- B
- G
- D
- E
- and
- 9000 About
- P
- P
- With
- T
- in
- F
- x
- 9 h
- K.
- S
- B
- E
- S
- I
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- Newsletter
- The facts are clear
- Publications
- Find country »
- A
- B
- C
- g
- D
- E
- and
- th
- K
- L
- 9000 N
- 9000
- in
- Ф
- x
- C hours
- Sh
- Sh.

- K
- E 9000 WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A nine0005
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Highlights " nine0005
- About WHO »
- General director
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/ nine0004 Rubella
","datePublished":"2019-10-04T07:00:00. 0000000+00:00","image":"https://cdn.who.int/media/images/default- source/imported/rwanda-measles-rubella-vaccine.jpg?sfvrsn=a7078766_0","publisher":{"@type":"Organization","name":"World Health Organization: WHO","logo":{ "@type":"ImageObject","url":"https://www.who.int/Images/SchemaOrg/schemaOrgLogo.jpg","width":250,"height":60}},"dateModified" :"2019-10-04T07:00:00.0000000+00:00","mainEntityOfPage":"https://www.who.int/ru/news-room/fact-sheets/detail/rubella","@context ":"http://schema.org","@type":"Article"}; nine0285
0000000+00:00","image":"https://cdn.who.int/media/images/default- source/imported/rwanda-measles-rubella-vaccine.jpg?sfvrsn=a7078766_0","publisher":{"@type":"Organization","name":"World Health Organization: WHO","logo":{ "@type":"ImageObject","url":"https://www.who.int/Images/SchemaOrg/schemaOrgLogo.jpg","width":250,"height":60}},"dateModified" :"2019-10-04T07:00:00.0000000+00:00","mainEntityOfPage":"https://www.who.int/ru/news-room/fact-sheets/detail/rubella","@context ":"http://schema.org","@type":"Article"}; nine0285
Basic Facts
- Rubella is a contagious viral infection most commonly found in children and young adults.
- Rubella is the leading cause of birth defects among vaccine-preventable causes. Rubella in pregnant women can lead to fetal death or congenital malformations such as congenital rubella syndrome.
- There is no specific treatment for rubella, but the disease can be prevented by vaccination. nine0005
Rubella is an acute, contagious viral infection. While the rubella virus usually causes mild fever and rash in children and adults, infection in a woman during pregnancy, especially in the first trimester, can lead to miscarriage, fetal death, stillbirth, or a congenital malformation in the infant known as congenital rubella syndrome (CRS). ).
While the rubella virus usually causes mild fever and rash in children and adults, infection in a woman during pregnancy, especially in the first trimester, can lead to miscarriage, fetal death, stillbirth, or a congenital malformation in the infant known as congenital rubella syndrome (CRS). ).
The rubella virus is spread through the air when an infected person sneezes or coughs. Humans are the only known carrier of the rubella virus. nine0285
Symptoms
In children, the disease is usually mild, with symptoms including rash, mild fever (<39°C), vomiting, and mild conjunctivitis. The rash, which appears in 50-80% of cases, usually first appears on the face and neck, then goes down the body and lasts 1-3 days. Swollen lymph nodes behind the ears and in the neck are the most common clinical sign. Infected adults, more often women, may develop arthritis with joint pain, which usually lasts 3-10 days. nine0285
After infection, the virus spreads in the human body within 5-7 days. Symptoms usually appear 2-3 weeks after exposure. The most infectious period usually occurs 1-5 days after the onset of the rash.
Symptoms usually appear 2-3 weeks after exposure. The most infectious period usually occurs 1-5 days after the onset of the rash.
If a woman becomes infected with rubella early in her pregnancy, she has a 90% chance of transmitting the virus to her fetus. This can cause fetal death or congenital rubella syndrome (CRS). Infants with CRS may shed the virus for a year or more after birth. Children with CRS may shed the virus for a year or more after birth. nine0285
Congenital rubella syndrome
Children with CRS can suffer from hearing loss, eye defects, heart defects, and other lifelong disabilities, including autism, diabetes, and thyroid dysfunction. Many of these disorders require expensive therapy, surgery, and other expensive medical care.
The risk of CRS is highest in countries where women of childbearing age do not have immunity to the disease (either through vaccination or previous rubella). Prior to the introduction of the vaccine, up to 4 children per 1000 live births were born with CRS.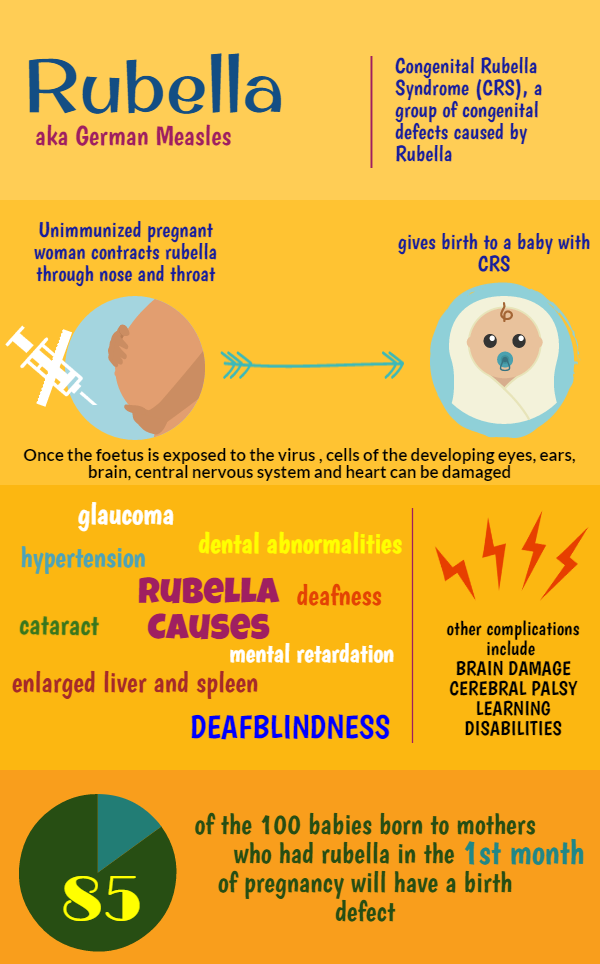 nine0285
nine0285
Vaccination
A single dose of live attenuated rubella vaccine provides more than 95% long-term immunity, similar to that produced by natural infection.
Rubella vaccines are either monovalent (a vaccine that targets only one pathogen) or, most often, combined with other vaccines such as measles (MR), measles and mumps (MM) or measles, mumps and varicella vaccines. smallpox (KSKB). nine0285
Adverse reactions to vaccination are usually mild. These may include pain and redness at the injection site, mild fever, rash, and muscle pain. During mass immunization campaigns in the Region of the Americas, reaching more than 250 million adolescents and adults, there were no serious adverse reactions associated with this vaccine.
WHO activities
WHO recommends that all countries that have not yet introduced rubella vaccine should consider introducing it as part of existing sustainable measles immunization programmes. To date, the goal of eliminating this preventable cause of malformations has been set in four WHO regions.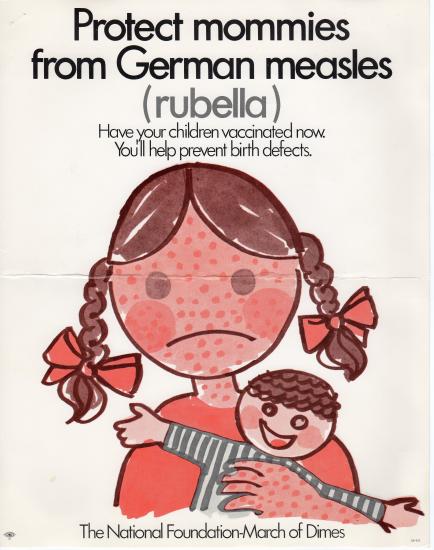 In 2015, the WHO Region of the Americas became the first region in the world to be declared free from endemic rubella transmission. nine0285
In 2015, the WHO Region of the Americas became the first region in the world to be declared free from endemic rubella transmission. nine0285
The number of countries using rubella vaccines as part of their national immunization programs is steadily increasing. As of December 2018, rubella vaccination had been introduced in 168 out of 194 countries, and the average rubella coverage rate worldwide was estimated to be 69%. The number of reported cases of rubella decreased by 97% from 670 894 cases in 102 countries in 2000 to 14 621 cases in 151 countries in 2018. Among WHO regions, the prevalence of CRS is highest in the African Region and the South-East Asia Region, where vaccine coverage is at its lowest. nine0285
In April 2012, the Measles Initiative—now known as the Measles and Rubella Initiative—launched the Global Measles and Rubella Strategic Plan, which sets out a set of global targets in this area for the period until 2020
By the end of 2020
- Complete measles and rubella elimination in at least 5 WHO regions.
The 2018 Global Vaccine Action Plan (GVAP) Progress Report prepared by the WHO Strategic Advisory Group of Experts (SAGE) on Immunization indicates that rubella control is not well underway. For example, 42 countries have not yet implemented rubella vaccination, and two regions (the African Region and the Eastern Mediterranean Region) have not yet set rubella elimination or control targets. nine0285
In order to further control the disease, SAGE recommends that rubella vaccination be included in immunization programs as soon as possible. As a founding member of the Measles and Rubella Initiative, WHO provides technical support to governments and communities to improve routine immunization programs and targeted vaccination campaigns. In addition, the WHO Global Measles and Rubella Laboratory Network provides support for diagnosing rubella and CRS cases and tracking the spread of rubella viruses. nine0285
- Child Health Thematic Review
Rubella: symptoms, diagnosis and treatment
General practitioner
Ablyazov
Irshat Ravilevich
Experience 23 years
District therapist of the highest category.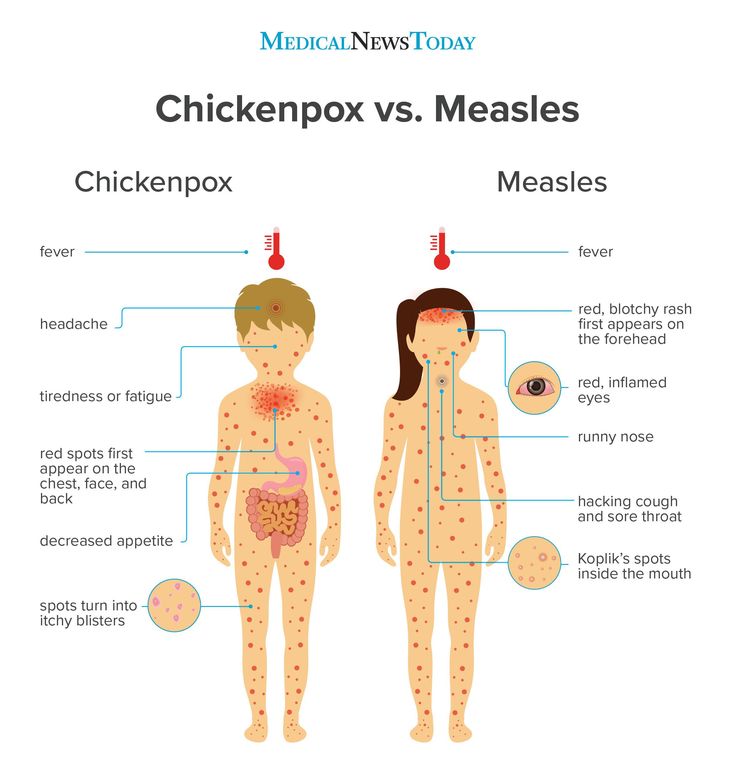 Member of the Russian Scientific Medical Society of Therapists.
Member of the Russian Scientific Medical Society of Therapists.
Make an appointment
Rubella is an acute infection of a viral nature, which manifests itself in the form of characteristic rashes all over the body except for the palms and feet, as well as general intoxication of the body of a moderate degree against the background of a concomitant increase in lymph nodes and blood reaction. The rubella virus is transmitted by airborne droplets and enters the body through the upper respiratory tract. The incubation period lasts from 10 to 25 days. Rubella-specific rashes initially appear on the face, then quickly spread throughout the body. nine0285
Symptoms and signs
Signs of rubella in adults usually begin with catarrhal manifestations:
- fever;
- general weakness and malaise;
- headache;
- lacrimation and photophobia;
- slight coryza;
- sore throat and dry coryza;
- mild inflammation of the throat and mucous membranes.
Rubella symptoms of the initial stage are enlarged lymph nodes in the occipital and mid-cervical region. The main symptom of rubella is a specific rash that appears from the first days of the disease, spreads throughout the body in just a day. The rash begins to spread from the neck, behind the ears, under the hair and on the face, leaving the palms and soles intact. The rash is small red or pink spots of a rounded shape, having smooth edges and not rising above the skin. nine0285
Routes of infection and risk factors
The rubella virus is practically unstable to the external environment, easily decomposes under the influence of ultraviolet radiation, heat and disinfectants. At the same time, it easily tolerates freezing and lives for several hours at room temperature. Rubella is transmitted to the fetus through the placenta during pregnancy. At the same time, congenital rubella is observed in children.
Women of childbearing age are the most susceptible to the virus. The spread and multiplication of the virus in the blood provokes the work of the immune system, under the influence of which antibodies to rubella are produced, which have a persistent lifelong effect. Rubella can occur in a passive form, in which case a blood reaction is observed in women - rubella igg positive. To date, the only risk factor for infection with viruses is close contact with a patient with an acute or erased form of the disease. nine0285
The spread and multiplication of the virus in the blood provokes the work of the immune system, under the influence of which antibodies to rubella are produced, which have a persistent lifelong effect. Rubella can occur in a passive form, in which case a blood reaction is observed in women - rubella igg positive. To date, the only risk factor for infection with viruses is close contact with a patient with an acute or erased form of the disease. nine0285
Complications
Complications after rubella are rare and are caused by a concomitant bacterial infection. The greatest danger is rubella during pregnancy, as it has a negative effect on the normal development of the fetus and can even cause intrauterine death.
Among bacterial infectious diseases, pneumonia, encephalitis, tonsillitis, otitis media, arthritis and others can be distinguished.
Diagnostics
Diagnosis of rubella in adults is carried out comprehensively, includes the following activities:
- patient interview and external examination - at this stage it is established whether the rubella vaccination was carried out, when the last rubella vaccination was received, and a detailed collection of the clinical picture and all manifestations during the passive time of the incubation period is carried out.
At the time of manifestation of rashes, it becomes relevant to conduct laboratory tests to detect antibodies to rubella. Here the most informative are the following methods: nine0285
- serodiagnosis - based on a blood test to detect M and G antibody titers. This test is also carried out for pregnant women to identify a predisposition to the disease, while rubella has a positive reaction in the case of a previous illness;
- virological research is aimed at identifying the virus itself in the human body. The study is carried out from any swabs - blood, saliva, urine, feces, etc. This method is most informative in the period from 7 to 14 days of the incubation period; nine0005
- polymerase chain reaction or PCR is the most informative method for detecting positive rubella titer and is based on the synthesis of the two previous methods.
The final diagnosis is made taking into account all the studies. A non-specific study is a complete blood count, showing an increase in lymphocytes and high ESR values.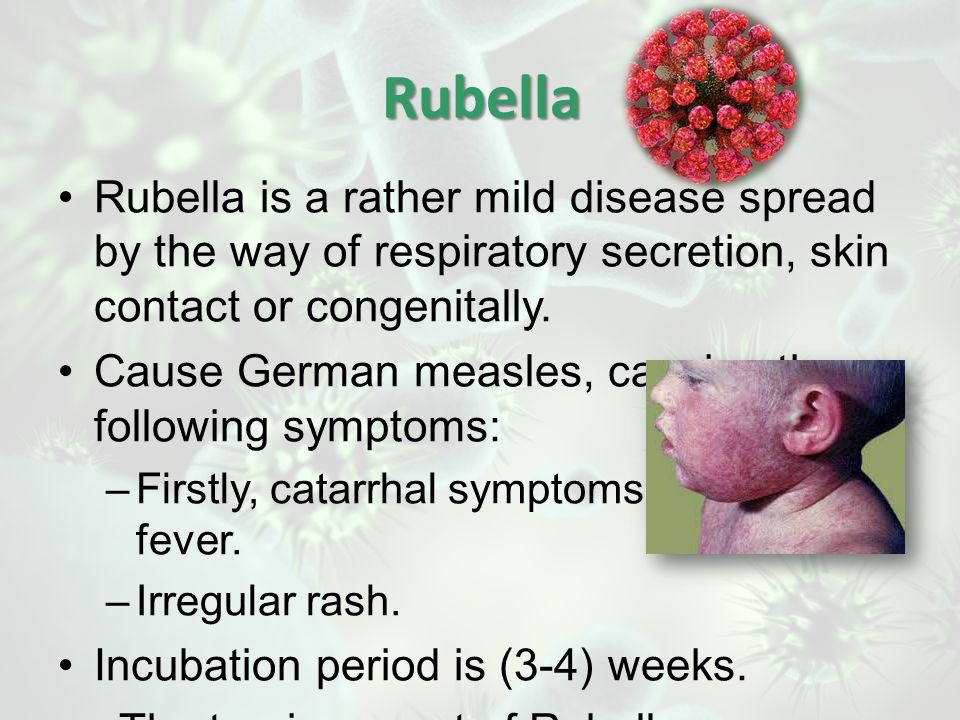
Treatment
The treatment of the disease consists in creating a sparing regimen, since recovery occurs by itself at the time of the formation of an immune response to the invading virus. How long does rubella last? It depends on the strength of the body's immune system, but on average, the period of the acute stage of the disease takes 5-7 days, while the incubation period is 10-25 days. nine0285
In case of a severe course of the disease, symptomatic treatment is prescribed:
- antipyretics;
- sedatives;
- taking antihistamines;
- funds aimed at detoxification of the body.
Prevention
Prevention of the spread of the virus lies in the timeliness of vaccinations against rubella.
The rubella vaccine is administered twice - the first time at 12-16 months, the second - at the age of 6 years. Adolescent girls and young women should be revaccinated. In case of contact with a sick person, an emergency administration of rubella immunoglobulin is possible.