When is the first scan in pregnancy
What Every Mom-To-Be Needs to Know
Moms-to-be typically look forward to ultrasounds during pregnancy more than any other prenatal appointment. It’s easy to see why! It’s fun to get a sneak peek of your bundle of joy while your OBGYN looks for specific growth and development markers. Many women look forward to learning their baby’s sex as soon as possible and wait impatiently for their 20-week ultrasound. Others want to be surprised. Whether or not you intend to learn about your baby’s sex ASAP, it’s important to keep all your ultrasound appointments.
An ultrasound, also known as a sonogram, is typically performed by an ultrasound technician or sometimes by an OBGYN. It uses sound waves to create an image of the organs inside your body. (These sound waves are not harmful to you or your baby.) Ultrasounds during pregnancy help doctors diagnose many diseases and conditions, even those not related to pregnancy.
This article will cover why and how ultrasounds are used during your pregnancy, how many ultrasounds to expect while you’re pregnant, and what your OBGYN may be looking for at each ultrasound.
Most pregnant women typically only get two ultrasounds, one at the beginning of pregnancy and one about halfway through. Other women may have three or more ultrasounds done depending on a number of factors.
Your First Ultrasound
Your first ultrasound is called the “dating” or “viability” ultrasound. It’s typically done between 7 and 8 weeks to verify your due date, to look for a fetal heartbeat, and to measure the length of the baby from “crown to rump.” At this ultrasound, you’ll also learn whether you’re having one baby, pregnant with twins, or more! You may even get to see or hear your baby’s heartbeat during this appointment.
If you have irregular periods, or didn’t have a period after coming off birth control, this ultrasound will be especially helpful in determining a more accurate due date. Your due date is important because it helps your doctor know whether your baby’s development is on track each month.
We’ll perform this ultrasound at our Madison Women’s Health clinic.
What to Expect at Your First Ultrasound
When you’re just 7 or 8 weeks pregnant, your fetus is only about two centimeters long. In order to get a close enough view of your uterus and fetus, the dating ultrasound is done transvaginally. This means the ultrasound is done internally, literally “through the vagina.” A transvaginal ultrasound can be a little uncomfortable, but it is not painful. Most would say it feels less invasive than a gynecological exam that uses a speculum.
To perform this ultrasound, your OBGYN or ultrasound tech will gently insert a narrow ultrasound wand just inside your vagina. The transvaginal ultrasound wand is also called a transducer. It’s about three centimeters around, a little larger than a tampon. It will be covered by a condom and lubricant. The wand will not reach your cervix and is safe for your baby.
You may be asked to arrive at your first ultrasound with a full bladder. Having a fuller bladder helps to put your uterus in a better position for the ultrasound.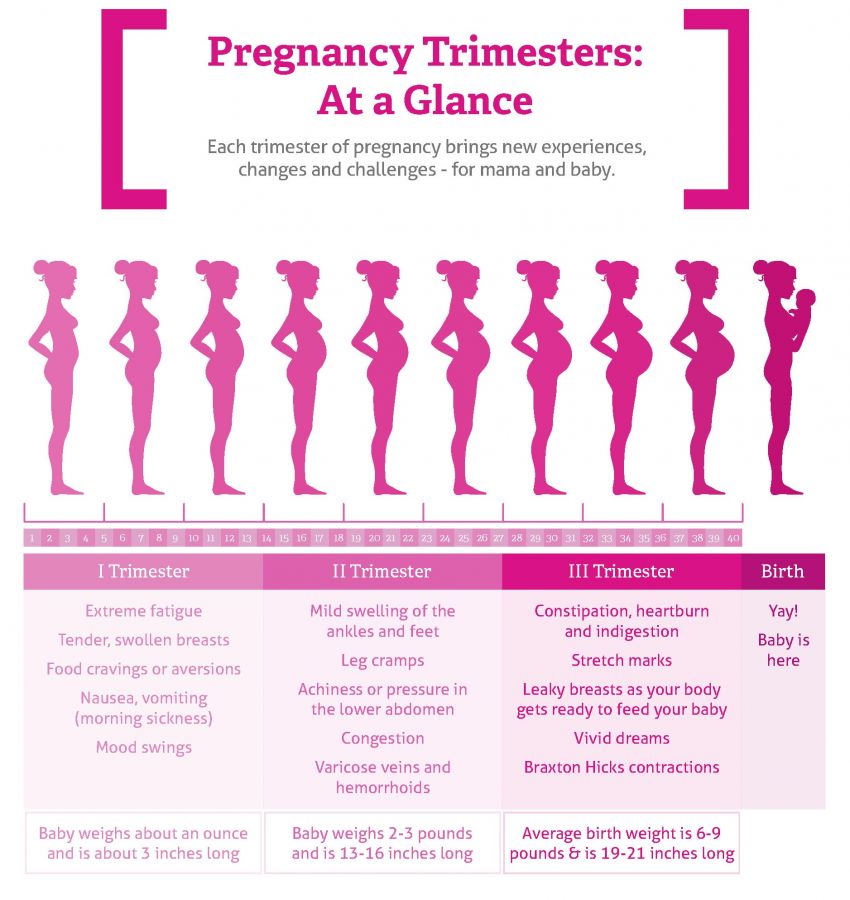
What Your Doctor is Looking for at Your First Ultrasound
- Viability of pregnancy
- Fetal heartbeat
- Fetal size
- Single or multiple pregnancy
Genetic Screening Ultrasound
If you choose to have prenatal genetic testing done, you’ll have your next ultrasound at 12 to 13 weeks gestation. This ultrasound is also called nuchal translucency screening. It’s offered to everyone and is covered by most insurance plans. This genetic screening ultrasound is optional.
During this ultrasound, your doctor will look for indicators of chromosomal disorders. Chromosomal disorders mean that the baby received an extra chromosome at conception and could have moderate to extreme physical or mental challenges. These disorders include:
- Trisomy 21, known as Down Syndrome
- Trisomy 13
- Trisomy 18
Read more about carrier screening and prenatal genetic testing. Also check out the article about at-home genetic testing kits.
Also check out the article about at-home genetic testing kits.
What Your Doctor is Looking for at the Genetic Screening Ultrasound
This ultrasound will be an anatomical scan. Your doctor will look to see if all four limbs are present. They will also look for basic structures in the brain, the stomach, the bladder, the nasal bone, and last but not least, something called nuchal translucency. Nuchal translucency is a fluid sack at the back of the baby’s neck that is filled with lymphatic fluid. There are correlations between the size of that sack of fluid and the likelihood that the fetus could be affected by a major chromosomal disorder.
After the ultrasound has been performed, your OBGYN will interpret the results and share the information with you. You may also meet with a genetic counselor who could recommend having additional tests done to verify the ultrasound results.
Keep in mind that ultrasound screenings for other genetic disorders or anatomic abnormalities become more accurate further into the pregnancy.
We’ll perform this ultrasound at the Madison Women’s Health clinic.
Should you Get a Genetic Screening Ultrasound?
There’s no right or wrong answer to this question. Ultimately, the decision is up to you. Here are some good questions to ask yourself as you decide whether to have the genetic screening:
- Is there a family history of these genetic birth disorders?
- Would I terminate my pregnancy if there was a risk of Downs Syndrome, Trisomy 13, Trisomy 18, or other genetic disorder?
- Would knowing about my pregnancy’s risk of genetic defect make it easier to emotionally or physically prepare for a baby with a birth defect?
- Would it be easier for me to cope with and enjoy pregnancy if I focus on the more likely positive outcome rather than the chance of birth defects?
Whether you choose to have genetic screening done at this time is entirely your decision. Some women prefer to have as much information as possible as early as possible, while other women do not. If you’re still uncertain, you can discuss the pros and cons with your OBGYN.
Some women prefer to have as much information as possible as early as possible, while other women do not. If you’re still uncertain, you can discuss the pros and cons with your OBGYN.
Basic Anatomy Scan Ultrasound
This is the ultrasound that people look forward to the most! The full anatomy ultrasound is typically performed at about 20 weeks, or 5 months. As the name implies, this ultrasound will look at all the baby’s organ systems to make sure they’re present, are a normal size and shape, and are in the right location.
What to Expect at a Full Anatomy Scan Ultrasound
The full anatomy scan is a transabdominal ultrasound. It uses a transducer that looks a lot like a store checkout scanner. The ultrasound technician will put warm ultrasound gel on your stomach and then slide the transducer in the gel around your stomach. The gel helps the sound waves travel through your skin.
Tip: Come to your appointment with a relatively full bladder. This will make it easier for your ultrasound technician to get better images of your baby.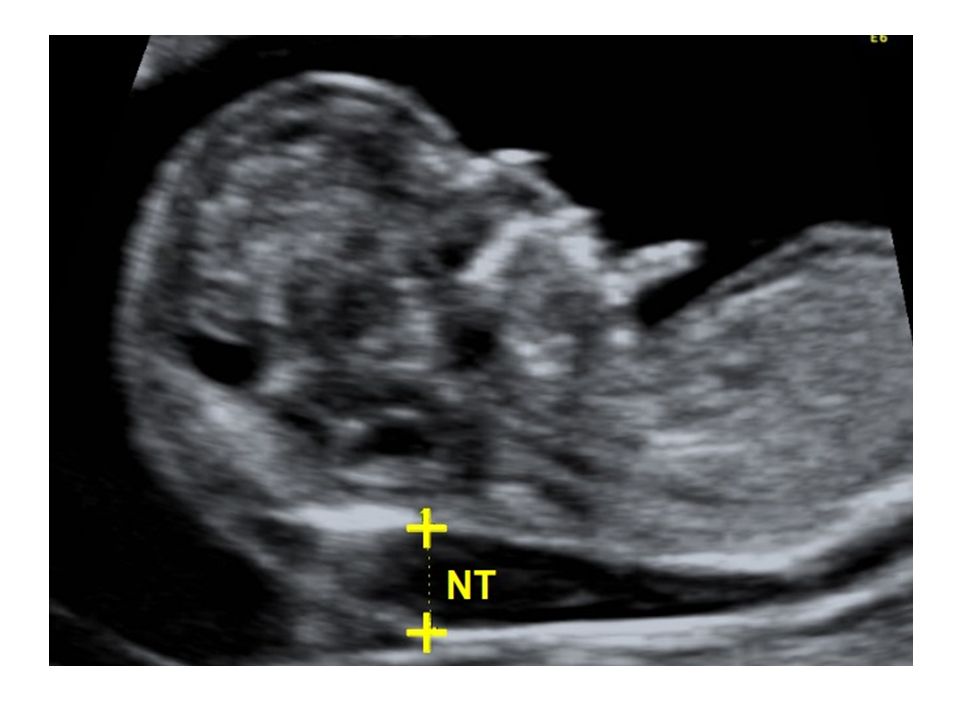
Because there are so many things to look for, this ultrasound will take at least 45 minutes—if your little one cooperates! If you’ve got an extra squirmy baby who is “camera shy,” it could take a few hours to get all the images that we need. Don’t worry, we have a lot of tricks to encourage your baby to change positions—everything from asking you to lay on one side and then the other, emptying your bladder or filling it, maybe even walking around. We’ll do whatever it takes to get the images we need to track your baby’s growth and development.
What Your OBGYN is Looking for at a Full Anatomy Scan
During the full anatomy, 20-week ultrasound, you can find out if your baby is male or female. If you want the sex to be a surprise, be sure to tell your technician know ahead of time so they don’t accidentally let it slip. When the scan is complete, Meriter will even send you a link to view some fun photos of your baby!
Your ultrasound technician will capture a large number images and measurements:
- limbs: arms, legs, feet, hands
- torso: chest, heart, kidneys, stomach, bladder, diaphragm, genitals
- head and face
- spine
- umbilical cord
- amount of amniotic fluid
- location, size, and shape of your placenta
- length of your cervix
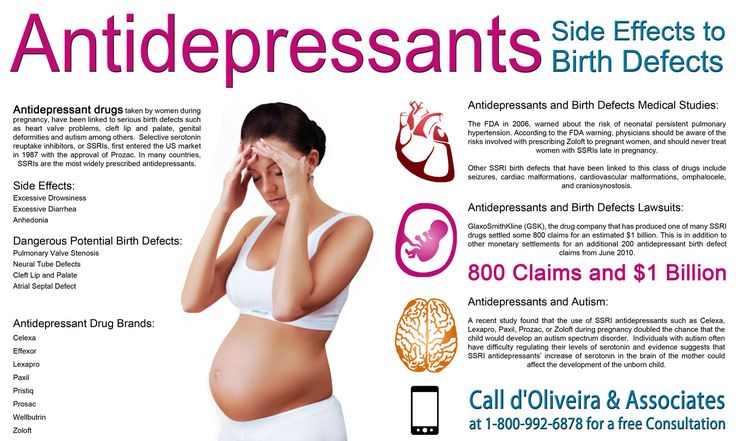
After your ultrasound technician has captured all these images and measurements, your OBGYN will review the pictures and look for abnormalities such as congenital heart defects or cleft lip or palate.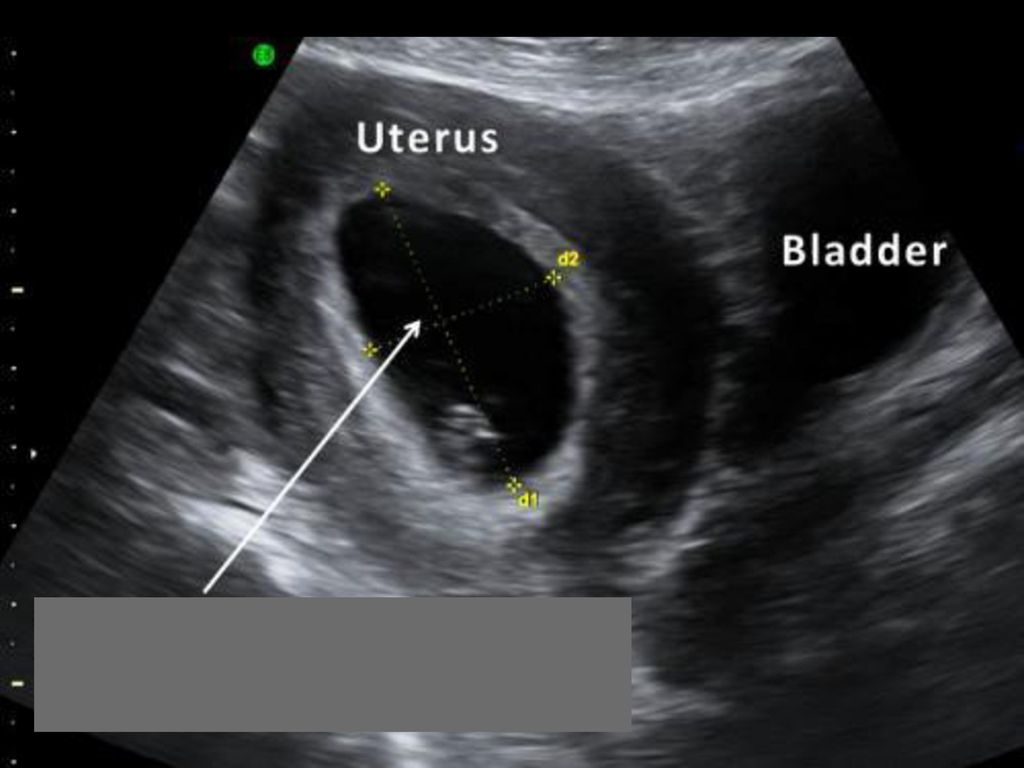 They’ll discuss their findings with you and help you understand what you’re looking at in the different images.
They’ll discuss their findings with you and help you understand what you’re looking at in the different images.
If everything looks normal and there are no other issues during your pregnancy, the next time you’ll see your baby is when he or she is in your arms! In the meantime, you can enjoy those 2D or 3D photos of your baby!
This ultrasound will be performed at UnityPoint Health – Meriter Hospital Center for Perinatal Care.
“Extra” Ultrasounds
Sometimes, women need additional ultrasounds during pregnancy. Your OBGYN may ask you to come in for additional ultrasounds to check your:
- Cervical length: if your cervix is shorter than expected, you may need to have your cervix checked regularly to be sure it stays closed so that you can maintain your pregnancy. If the cervix continues to shorten or thin, you may need a cerclage to help strengthen it until it’s time to deliver your baby. Cervical length ultrasounds occur at 16, 18, 20 and 22 weeks and are done transvaginally.
- Placental location and size: if your placenta is too small, if it is in an abnormal location or if it is an abnormal shape, then we will need to monitor it and the growth of your baby with regular ultrasounds. Your placenta is responsible for passing blood and nutrients to your baby, so it’s important thrat it is growing correctly.
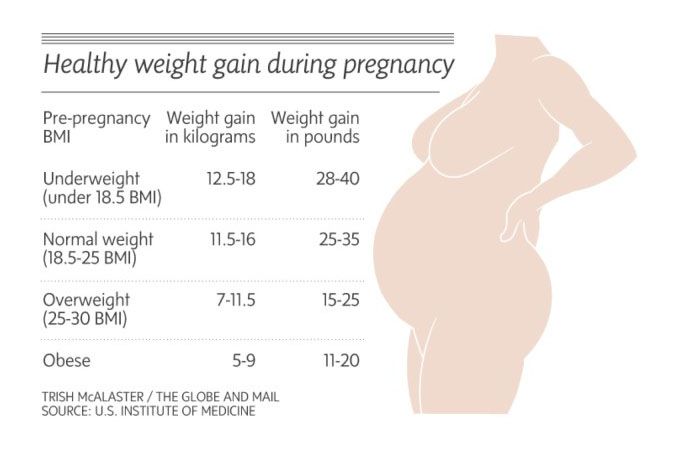
You may need growth ultrasounds if you have:
- hypertension
- diabetes
- high BMI (body mass index) going into pregnancy
- preeclampsia
- indicators that your placenta or uterus is not growing appropriately
Sometimes, growth ultrasounds are needed to check that your baby’s growth is continuing along the growth curve. They’re done at 28, 32, and 36 weeks. One way doctors estimate whether your baby is growing as expected is by measuring your fundal height. Fundal height is the number of centimeters from your pubic bone to the top of your uterus. This measurement typically increases about 1 cm each week. If your uterus has not grown appropriately in the last month, your OBGYN will surmise that your baby is also not growing and will want to perform monthly growth ultrasounds.
This measurement typically increases about 1 cm each week. If your uterus has not grown appropriately in the last month, your OBGYN will surmise that your baby is also not growing and will want to perform monthly growth ultrasounds.
What to Expect at a Growth Ultrasound
These ultrasounds take less time than the full basic anatomy ultrasound because there are fewer measurements required. The ultrasound technician will measure the baby’s head circumference, bi-parietal diameter, abdominal circumference, and femur length.
What Your OBGYN is Looking for at Growth Ultrasounds
Your OBGYN is looking to see if your baby is staying on its growth curve. We will also use the measurements to estimate your baby’s weight. A large or extra large baby isn’t typically concerning. An extra-small baby or a baby who does not grow according to their growth curve could mean that the baby is not getting enough nourishment through the placenta and may need to be delivered early.
2D, 3D, and 4D Ultrasounds
2D ultrasounds are the black and white images that you’re probably used to seeing. To an untrained eye, they can look pretty fuzzy or obscure. However, they give the best definition of the structures of your growing peanut and are considered the “gold standard” of diagnostic imaging.
To an untrained eye, they can look pretty fuzzy or obscure. However, they give the best definition of the structures of your growing peanut and are considered the “gold standard” of diagnostic imaging.
3D images are especially popular among parents-to-be who want to enjoy those cute baby pictures even before the baby is born! These pictures show facial features and look much more baby-like than the kind of obscure 2D images. 3D ultrasounds have usefulness beyond the cuteness factor, however! In the case of abnormalities of the spine or palate, 3D ultrasounds can help your OBGYN get a better idea of the severity.
4D images are like a 3D image, but show the baby moving around. They’re like getting to see a live action video of your little one. These are less commonly done because they don’t actually help with diagnoses. Depending on which perinatal center you go to, you might receive a link to view your ultrasound images or videos online.
While there are some stand-alone ultrasound centers offering to tell you your baby’s sex early on or to give you keepsake 3D or 4D images, these aren’t necessary and are rarely covered by insurance. You’ll find out everything you need to know during your appointments at the perinatal center — and those appointments will be covered by your insurance.
You’ll find out everything you need to know during your appointments at the perinatal center — and those appointments will be covered by your insurance.
The best place to have an ultrasound performed is always at a clinic, where you will have access to a physician who has been trained in interpreting the images. At Madison Women’s Health, we’re happy to print off pictures for you to put in your baby’s scrapbook — or anywhere else you’d like to display those “coming soon” photos.
Final Thoughts
Ultrasounds during pregnancy are a fascinating way to get a glimpse of your developing baby. Don’t be afraid to ask your OBGYN for more details about genetic screening as you determine whether that is something you want done. And make sure you’ve set aside a good amount of time for your ultrasounds — especially the all-important full anatomy scan!
—
Dr. Beth Wiedel has been providing healthcare to women in Madison since 2002 and is a founding partner of Madison Women’s Health.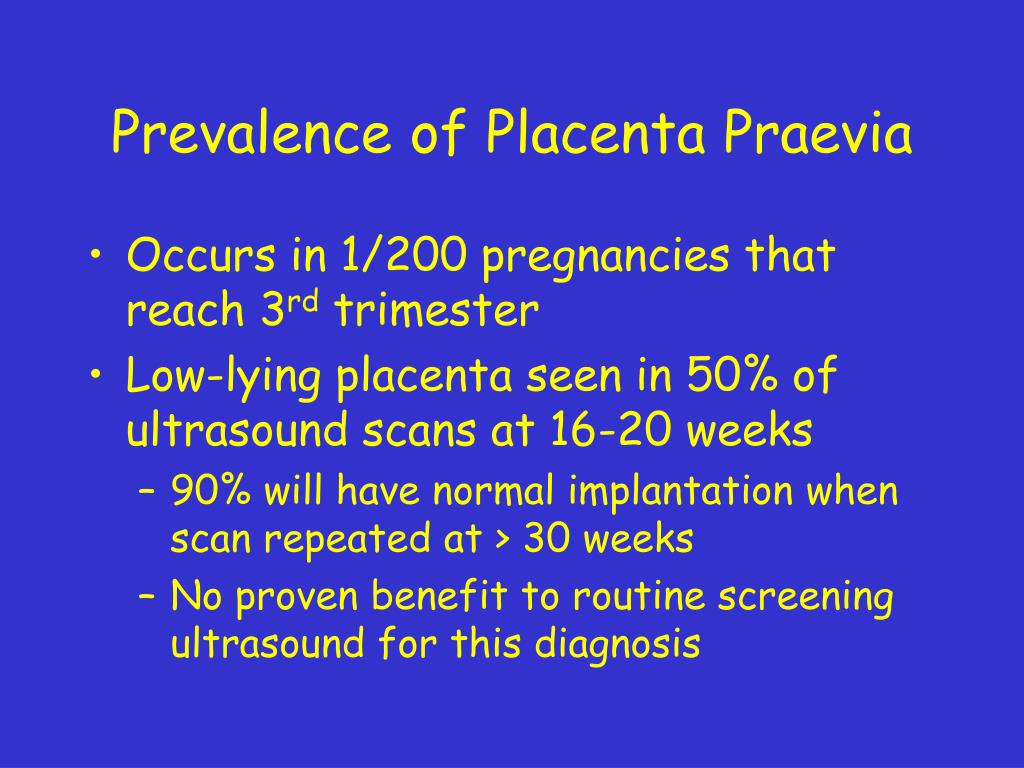 She shares the vision of all the partners of being a strong healthcare advocate for her patients, emphasizing compassion and communication throughout her practice.
She shares the vision of all the partners of being a strong healthcare advocate for her patients, emphasizing compassion and communication throughout her practice.
12-week scan - NHS
If you're pregnant in England you'll be offered an ultrasound scan at around 10 to 14 weeks of pregnancy. This is called the dating scan. It's used to see how far along in your pregnancy you are and check your baby's development. The scan may also be part of a screening test for Down's syndrome.
Your midwife or doctor will book you a dating scan appointment. It will usually take place at your local hospital ultrasound department. Most scans are carried out by sonographers.
You may need to have a full bladder for this scan, as this makes the ultrasound image clearer. You can ask your midwife or doctor before the scan if this is the case. The dating scan usually takes about 20 minutes.
Find out more about what happens during a pregnancy ultrasound scan
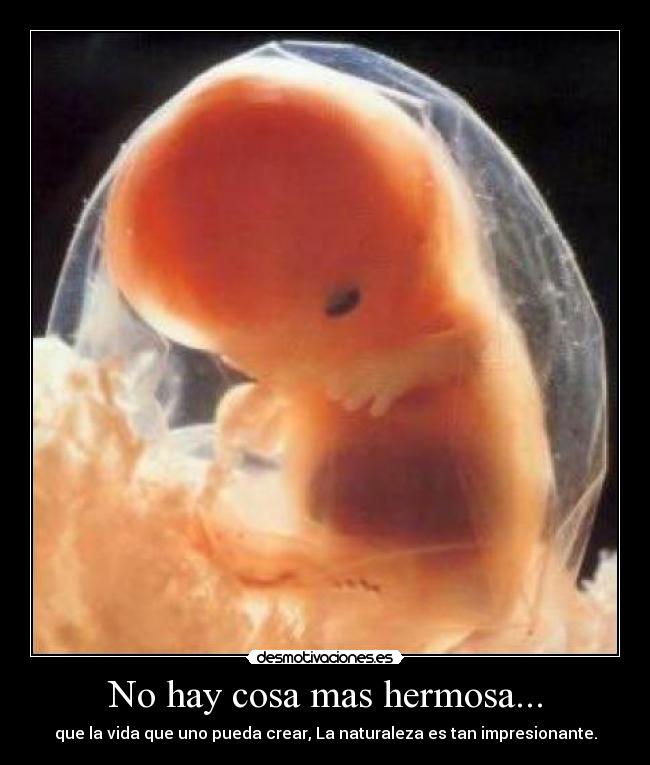
Dating scan imageCredit:
Nic Cleave / Alamy Stock Photo https://www. alamy.com/stock-photo-12-twelve-week-ultrasound-scan-antenatal-photo-of-unborn-foetus-baby-18962836.html?pv=1&stamp=2&imageid=E0A8E3FE-D4B6-4EF5-9687-24C92C3FEA0F&p=74035&n=0&orientation=0&pn=1&searchtype=0&IsFromSearch=1&srch=foo%3dbar%26st%3d0%26pn%3d1%26ps%3d100%26sortby%3d2%26resultview%3dsortbyPopular%26npgs%3d0%26qt%3dB2RR84%26qt_raw%3dB2RR84%26lic%3d3%26mr%3d0%26pr%3d0%26ot%3d0%26creative%3d%26ag%3d0%26hc%3d0%26pc%3d%26blackwhite%3d%26cutout%3d%26tbar%3d1%26et%3d0x000000000000000000000%26vp%3d0%26loc%3d0%26imgt%3d0%26dtfr%3d%26dtto%3d%26size%3d0xFF%26archive%3d1%26groupid%3d%26pseudoid%3d788068%26a%3d%26cdid%3d%26cdsrt%3d%26name%3d%26qn%3d%26apalib%3d%26apalic%3d%26lightbox%3d%26gname%3d%26gtype%3d%26xstx%3d0%26simid%3d%26saveQry%3d%26editorial%3d1%26nu%3d%26t%3d%26edoptin%3d%26customgeoip%3d%26cap%3d1%26cbstore%3d1%26vd%3d0%26lb%3d%26fi%3d2%26edrf%3d0%26ispremium%3d1%26flip%3d0%26pl%3d
alamy.com/stock-photo-12-twelve-week-ultrasound-scan-antenatal-photo-of-unborn-foetus-baby-18962836.html?pv=1&stamp=2&imageid=E0A8E3FE-D4B6-4EF5-9687-24C92C3FEA0F&p=74035&n=0&orientation=0&pn=1&searchtype=0&IsFromSearch=1&srch=foo%3dbar%26st%3d0%26pn%3d1%26ps%3d100%26sortby%3d2%26resultview%3dsortbyPopular%26npgs%3d0%26qt%3dB2RR84%26qt_raw%3dB2RR84%26lic%3d3%26mr%3d0%26pr%3d0%26ot%3d0%26creative%3d%26ag%3d0%26hc%3d0%26pc%3d%26blackwhite%3d%26cutout%3d%26tbar%3d1%26et%3d0x000000000000000000000%26vp%3d0%26loc%3d0%26imgt%3d0%26dtfr%3d%26dtto%3d%26size%3d0xFF%26archive%3d1%26groupid%3d%26pseudoid%3d788068%26a%3d%26cdid%3d%26cdsrt%3d%26name%3d%26qn%3d%26apalib%3d%26apalic%3d%26lightbox%3d%26gname%3d%26gtype%3d%26xstx%3d0%26simid%3d%26saveQry%3d%26editorial%3d1%26nu%3d%26t%3d%26edoptin%3d%26customgeoip%3d%26cap%3d1%26cbstore%3d1%26vd%3d0%26lb%3d%26fi%3d2%26edrf%3d0%26ispremium%3d1%26flip%3d0%26pl%3d
What is the purpose of the dating scan?
The purpose of the dating scan is to check:
- how many weeks pregnant you are and work out your due date (the estimated date of delivery, or EDD)
- whether you're expecting more than 1 baby
- that the baby is growing in the right place
- your baby's development
This scan can detect some health conditions, such as spina bifida.
Does screening for Down's syndrome happen at the dating scan?
This depends on whether you have agreed to have the screening and when the scan takes place. Screening for Down's syndrome will happen at the dating scan if:
- you have agreed to have screening for the condition
- the scan takes place between 10 and 14 weeks of pregnancy
The screening test for Down's syndrome used at this stage of pregnancy is called the combined test. It involves a blood test and measuring the fluid at the back of the baby's neck (nuchal translucency) with an ultrasound scan. This is sometimes called a nuchal translucency scan.
The nuchal translucency measurement can be taken during the dating scan. If you have agreed to have screening for Down's syndrome, the dating scan and the screening will usually happen at the same time.
Find out more about the screening for Down's syndrome, Edwards' syndrome and Patau's syndrome
You will not be offered the combined screening test if your dating scan happens after 14 weeks. Instead, you'll be offered another blood test between 14 and 20 weeks of pregnancy to screen for your chance of having a baby with Down's syndrome. This test is not quite as accurate as the combined test.
Find out more about:
- the 20-week scan
- ultrasound scans in pregnancy
- GOV.UK: screening tests for you and your baby
Page last reviewed: 18 December 2020
Next review due: 18 December 2023
When to do the first ultrasound during pregnancy - "happy days" for screening of the 1st trimester
The world of a modern woman is always full of important events, meetings and an endless series of pre-planned things.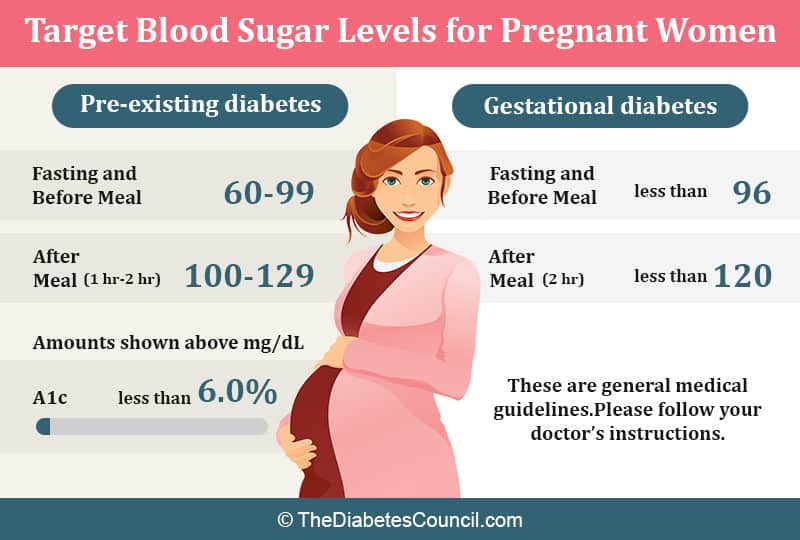 When pregnancy occurs, many planned events can be moved from “expected” to “impossible” or simply postponed indefinitely. It is quite difficult to worry in advance and reschedule an important event at the most appropriate time, because planning events against the backdrop of pregnancy is a very difficult science. nine0003
When pregnancy occurs, many planned events can be moved from “expected” to “impossible” or simply postponed indefinitely. It is quite difficult to worry in advance and reschedule an important event at the most appropriate time, because planning events against the backdrop of pregnancy is a very difficult science. nine0003
Therefore, when pregnancy occurs, it is advisable to draw up at least an approximate “life plan for 9 months”. For example, it is known that maternity leave is most often preceded by unspent regular leave, and registration for pregnancy is preceded by the fact that a pregnancy has occurred and is developing normally.
Many events will now depend on how the new life develops. So, when a multiple pregnancy is diagnosed, not only the estimated due date will change, but maternity leave will come 14 days earlier, and the beginning of unspent leave will move with it. Therefore, one of the first steps in the event of a desired pregnancy is the passage of an ultrasound examination (ultrasound). Scientific and technological progress is rapidly changing the whole world, including the state of the prenatal ultrasound diagnostic service. Opportunities are changing, and with them the timing of the passage of research, which I would like to dwell on in more detail. nine0003
Scientific and technological progress is rapidly changing the whole world, including the state of the prenatal ultrasound diagnostic service. Opportunities are changing, and with them the timing of the passage of research, which I would like to dwell on in more detail. nine0003
When to do an ultrasound scan during pregnancy
In 2012, the regulation “Decree of the Health Committee of the Government of St. Petersburg No. 39-r”1 came into force in St. Petersburg. Based on the above document, for a full-fledged ultrasound screening, it is desirable to undergo a study in “... the first trimester: 11 + 0-13 + 6 weeks; 18+0-20+6 weeks; and 32+0-34+6 weeks of pregnancy.” However, these terms apply only to uncomplicated singleton pregnancies. At the same time, early registration is limited to up to 12 weeks of pregnancy with the ensuing consequences (payment of a lump-sum allowance to women registered in medical institutions in the early stages of pregnancy, clause 2-c of Decree of the Government of the Russian Federation of October 15, 2001 N 727 (as amended on 04. 09.2012).
09.2012).
Therefore, at 11 weeks, a pregnant woman can be registered when establishing the fact of a developing pregnancy , for which ultrasound "... in the first trimester" is recommended. Most doctors recommend doing it at terms 7-8 weeks of pregnancy , because it is at this time that the heartbeat of a developing embryo is always determined as a sign of the physiological development of pregnancy.
The next obligatory steps in the ultrasound are screening. The entire pregnancy is divided into three periods (trimesters) and ultrasound plays an important role in each. nine0003
What is the diagnostic window for ultrasound during pregnancy
The first screening study is carried out from 11 weeks 0 days of pregnancy to 13 weeks 6 days of pregnancy. These limits are adopted for the timely detection of pathological conditions that determine the prognosis for the health of the fetus. Theoretically, any pregnant woman can apply for an ultrasound both at the beginning of the eleventh and at the end of the thirteenth week - the entire period is screening. However, among doctors who have dedicated their lives to prenatal ultrasound diagnostics, there is an opinion about the most preferable period in each screening period - the so-called " diagnostic window" or "happy days" .
However, among doctors who have dedicated their lives to prenatal ultrasound diagnostics, there is an opinion about the most preferable period in each screening period - the so-called " diagnostic window" or "happy days" .
Terms of fetal ultrasound examination
| Legally regulated period (order KZ SPb No. 39-r dated 02/01/12) | Optimal timing/happy days |
| - | 7-8 |
| 11 weeks 0 days – 13 weeks 6 days | 12 weeks 2 days - 12 weeks 4 days |
| 18 weeks 0 days – 20 weeks 6 days | 20 weeks 0 days - 20 weeks 6 days |
| 32 weeks 0 days – 34 weeks 6 days | 32 weeks 0 days - 33 weeks 3 days |
Diagnostic window in the 1st trimester of pregnancy
For the first screening study, these days include the interval from 12 weeks to 12 weeks. 2 days to 12 weeks 4 days . It is in this interval that the fetus has already grown enough to evaluate the smallest organs (eye lenses, heart), and the probability of ascertaining the most important morphological changes is significantly higher than at 11 weeks 0 days. On the other hand, each day lived by the baby increases not only the height and weight of the body, but the quality of the picture on the ultrasound machine.
2 days to 12 weeks 4 days . It is in this interval that the fetus has already grown enough to evaluate the smallest organs (eye lenses, heart), and the probability of ascertaining the most important morphological changes is significantly higher than at 11 weeks 0 days. On the other hand, each day lived by the baby increases not only the height and weight of the body, but the quality of the picture on the ultrasound machine.
According to various authors, the frequency of congenital pathology reaches 5%, and for patients in this group it is especially important to identify the problem at an early stage. In such special cases, it may be necessary to expand the range of diagnostic procedures, including prenatal karyotyping (obtaining samples of fetal tissue or amniotic structures in order to determine its karyotype). It takes time to carry out these procedures, from preparing the necessary tests for a pregnant woman, ending with directly invasive diagnostics and obtaining results about the health of the fetus. nine0003
nine0003
In some cases, the established disease of the fetus raises the question of the impossibility of prolonging the pregnancy. According to the current legislation of the Russian Federation, the procedure of medical termination of pregnancy by the decision of the woman can be performed "... no later than the end of the twelfth week of pregnancy", but "... not earlier than 48 hours from the moment the woman applied to the medical organization for artificial termination of pregnancy" (clause 3.1, clause 3-b of article 56. Federal Law No. 323 of November 21, 2012)2. In other words, if a patient goes for an ultrasound scan at 12 weeks 5 days, if a serious pathology is detected, she is no longer sent for an artificial medical abortion, but for an abortion, which is a more complex and traumatic procedure. Therefore, when asked about the best rock for the first screening, almost any practitioner will answer: "up to 12 weeks 4 days" .
Diagnostic window in the 2nd trimester of pregnancy
The second screening period occurs at 18 weeks. 0 days and ends at 20 weeks 6 days pregnant . "Lucky days" is considered the entire twentieth week: 20 weeks. 0 days - 20 weeks 6 days . Not all the subtleties of the architectonics of the main organs can be considered so successfully, especially in pregnant women with increased body weight at 18 weeks of pregnancy. If so-called "markers of chromosomal problems" are detected, it may be necessary to perform prenatal karyotyping (obtaining fetal blood or amniotic fluid), which may take some time. nine0003
0 days and ends at 20 weeks 6 days pregnant . "Lucky days" is considered the entire twentieth week: 20 weeks. 0 days - 20 weeks 6 days . Not all the subtleties of the architectonics of the main organs can be considered so successfully, especially in pregnant women with increased body weight at 18 weeks of pregnancy. If so-called "markers of chromosomal problems" are detected, it may be necessary to perform prenatal karyotyping (obtaining fetal blood or amniotic fluid), which may take some time. nine0003
The collection of the material itself takes several minutes, but the preparation of the pregnant woman (examination, obtaining the results of blood and urine tests, etc.), transporting the material to the laboratory, examination and obtaining the results can take several days. If serious deviations in the state of health of the fetus are detected, in order to resolve the issue of further management tactics, the pregnant woman is sent to undergo a prenatal consultation consisting of an ultrasound doctor, a specialist in the field to which the identified disease belongs (for example, a surgeon, neurosurgeon, cardiologist, etc. ) . nine0003
) . nine0003
Prior to the new regulation, the second screening period ranged from 18-22 weeks, even earlier than 18-24 weeks of pregnancy. According to WHO recommendations, the fetus becomes viable from the 22nd week of pregnancy, therefore, before this period it is very important to obtain all possible information about its condition and form a prognosis for health and later life. That is why now there is a restriction regulated by law, so that if serious problems with the health of the fetus are detected, all additional diagnostic procedures should be carried out in a timely manner and, if necessary, terminate the pregnancy without violating the Legislation of the Russian Federation2. nine0003
Diagnostic window in the 3rd trimester of pregnancy
The third screening period (32 weeks 0 days - 34 weeks 6 days of pregnancy) has two main objectives: the exclusion of congenital malformations with late manifestation and assessment of the fetal condition. Issuance of a referral for the passage of the third ultrasound along with maternity leave of 30 weeks. 0 days of pregnancy potentiates untimely early appeal of pregnant women for the third screening ultrasound before the period of 32 weeks 0 days, which in turn may require a second planned ultrasound in the "scheduled time". A later turnout (after 34 weeks) reduces the quality of the ultrasound picture obtained by changing the relationship between the amount of amniotic fluid and the volume of the fetal body towards the latter. Therefore " happy days" the third trimester can be considered the period 32 weeks 0 days - 33 weeks 3 days of pregnancy .
Issuance of a referral for the passage of the third ultrasound along with maternity leave of 30 weeks. 0 days of pregnancy potentiates untimely early appeal of pregnant women for the third screening ultrasound before the period of 32 weeks 0 days, which in turn may require a second planned ultrasound in the "scheduled time". A later turnout (after 34 weeks) reduces the quality of the ultrasound picture obtained by changing the relationship between the amount of amniotic fluid and the volume of the fetal body towards the latter. Therefore " happy days" the third trimester can be considered the period 32 weeks 0 days - 33 weeks 3 days of pregnancy .
Unscheduled ultrasound at any stage is required, as a rule, only in case of complicated pregnancy, therefore, it is prescribed only according to indications and is performed regardless of the gestational age.
Notes: 1 - Order of the Health Committee of the Government of St. Petersburg dated February 1, 2012 N 39-r "On measures to reduce hereditary and congenital diseases in children in St. Petersburg".
Petersburg dated February 1, 2012 N 39-r "On measures to reduce hereditary and congenital diseases in children in St. Petersburg".
2- Article 56 "Artificial termination of pregnancy". Federal Law of the Russian Federation of November 21, 2011 N 323-FZ "On the basics of protecting the health of citizens in the Russian Federation", entered into force: November 22, 2011, published on November 23, 2011 in "RG" - Federal issue No. 5639
timing and when is the first, second and third screening done?
Pregnancy screening is a whole range of studies that allows parents and doctors to get the most complete information about the health of an unborn baby. Screening reveals many congenital diseases and physical characteristics. How and when is pregnancy screening done, why is it needed and what examinations does it include? nine0102
Pregnancy screening is a complex of examinations, which includes ultrasound and biochemical analysis of venous blood for hormones. As a rule, screening is carried out three times - in the first, second and third trimester.
As a rule, screening is carried out three times - in the first, second and third trimester.
In our country, according to the order of the Ministry of Health of the Russian Federation No. 572n dated November 1, 2012, only a planned three-time ultrasound is mandatory during pregnancy [1] . Full screening is considered an additional study, which is usually carried out at the request of the expectant mother. However, in some cases, the doctor strongly recommends it. If you were given a referral for a full screening, do not panic - this does not mean at all that the doctor suspects some kind of pathology. It's just that in some situations the risk of their development is statistically higher, and the doctor needs to be aware of the possible dangers for the proper management of pregnancy. Screening during pregnancy is usually prescribed:
- pregnant women over 35 years of age and if the father's age is over 40 years;
- in the presence of genetic pathologies in family members;
- if you have had a miscarriage, miscarriage or premature birth in the past;
- pregnant women who had any infectious disease in the first trimester;
- women who are forced to take drugs that may be dangerous to the fetus and affect the development of pregnancy;
- women working in hazardous industries and / or those who have bad habits.
 nine0158
nine0158
Early detection of pathologies is very important. This makes it possible to start treating genetic diseases as early as possible and, if not completely cure them, then at least stop the symptoms as much as possible. If the doctor notices any abnormalities during the examination, the pregnancy is monitored especially carefully, which makes it possible to prevent the development of complications or premature birth. If the detected pathologies turn out to be too severe and incompatible with life, the doctor will refer the patient to terminate the pregnancy for medical reasons. nine0003
Pregnancy screening is safe for both mother and baby. This is a fairly accurate study, although it should be clearly understood that it does not give a 100% guarantee. The accuracy of screening depends on many factors - the professionalism of the researchers, the woman's compliance with the rules for preparing for the examination, and so on.
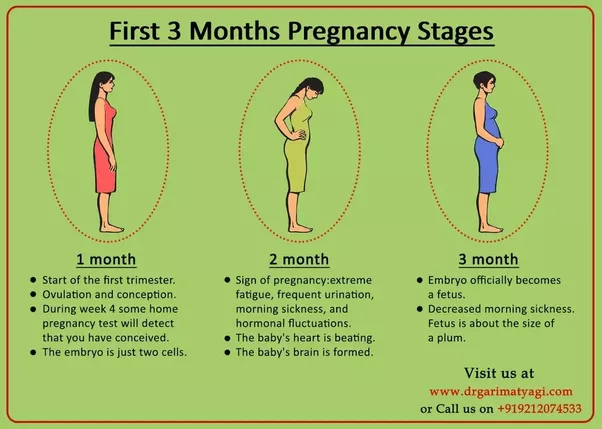
First Pregnancy Screening
First Pregnancy Screening between 11 and 13 weeks.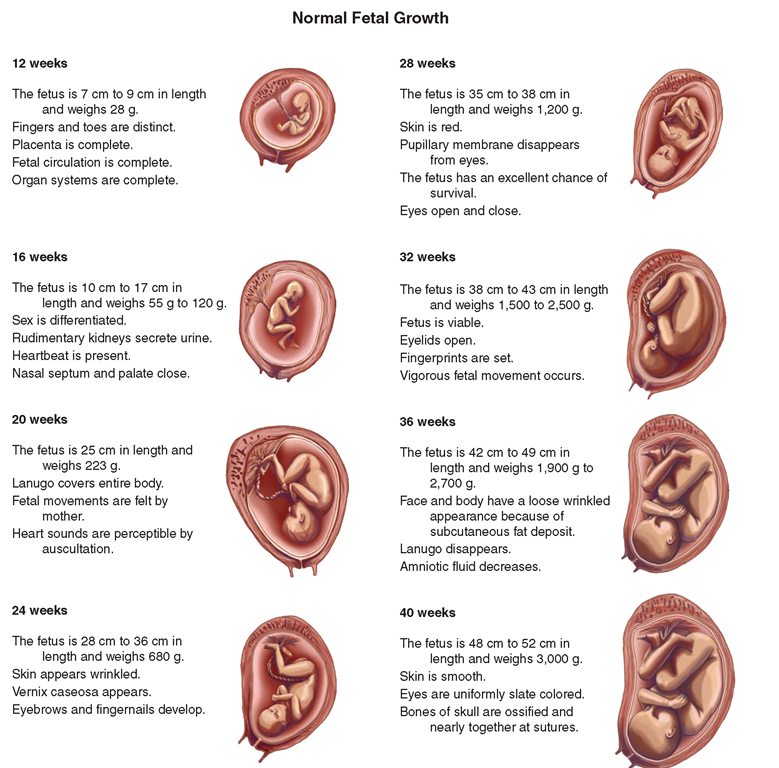 It makes no sense to undergo this examination earlier: before the 11th week of pregnancy, many indicators are practically indeterminate. nine0003
It makes no sense to undergo this examination earlier: before the 11th week of pregnancy, many indicators are practically indeterminate. nine0003
The test includes two medical tests, an ultrasound and a blood test.
Ultrasound
With the help of ultrasound, the doctor determines the exact gestational age, evaluates the baby’s physique, size (head circumference, limb length, height), heart muscle function, brain symmetry, amniotic fluid volume, structure and size of the placenta , as well as the condition and tone of the uterus. For each of these parameters there are indicators of the norm, with which the doctor will compare the results. For 11-13 weeks pregnant, these rates are:
- KTR (coccygeal-parietal size, that is, the length of the fetus from the top of the head to the tailbone) - 43–84 mm. If this figure is more than normal, then the child will be large. A downward deviation indicates slow development (the cause of this state of affairs is often a hormonal imbalance or infectious diseases suffered by the expectant mother), genetic pathologies or fetal death (in this case, the heart will not be auscultated).
 However, this may be due to a banal error in determining the timing of pregnancy. nine0158
However, this may be due to a banal error in determining the timing of pregnancy. nine0158 - BDP (biparietal size, that is, the distance from temple to temple) - 17–24 mm. A high BDP means a large fetus, but only on the condition that all other indicators say the same. Otherwise, we can talk about a herniated brain or hydrocephalus. Low BDP indicates slow brain development.
- TVP (collar space thickness) - 1.6–1.7 mm (depending on the gestational age). Deviation from this norm (TVP above 3 mm) is considered a sign of some severe chromosomal pathologies - Down syndrome, Edwards syndrome, and so on. However, one should not panic ahead of time: no one will make such a serious diagnosis only on the basis of TVP. To confirm, you need to take a blood test for hormones and take a biopsy of the outer dense shell of the embryo for further research. nine0158
- The length of the nose bone is 2–4.
 2 mm. Too small a nose bone can indicate pathology or simply that the baby's nose will be snub-nosed.
2 mm. Too small a nose bone can indicate pathology or simply that the baby's nose will be snub-nosed. - Heart rate (heart rate) - 140-160 beats per minute. A small (up to 40 beats per minute) deviation in one direction or another is considered a variant of the norm.
- Size of chorion, amnion and yolk sac.
- Chorion is the outer shell of the fetus, which will eventually become the placenta. If it is located on the lower wall of the uterus, they speak of chorion presentation. This is a potentially dangerous situation, fraught with miscarriage, and in this case, bed rest is recommended for the pregnant woman.
- Amnion is the inner membrane that holds the amniotic fluid. The normal volume of amniotic fluid for a period of 11–13 weeks is 50–100 ml.
- The yolk sac is a germinal organ, which in the first weeks of life of the fetus acts as some of the internal organs that will be formed later.
 By the time of the first screening, the yolk sac should have practically disappeared (then the examination form will indicate “not visualized”). If its size is about 6 mm, then the fetus may have certain pathologies. nine0158
By the time of the first screening, the yolk sac should have practically disappeared (then the examination form will indicate “not visualized”). If its size is about 6 mm, then the fetus may have certain pathologies. nine0158
- Cervix. It is normally 35–40 mm long by the time of the first screening. A shorter cervix means a risk of preterm labor.
Ultrasound is performed in two ways: transabdominal, in which the probe of the ultrasound machine is placed on the abdomen, and transvaginal, in which it is inserted into the vagina. Transvaginal ultrasound provides more complete and accurate information, but it is usually performed only in the first trimester. This method is usually used when examining overweight women, since the fat layer in the abdomen does not allow a detailed view of the fetus and uterus. nine0003
Preparing for the ultrasound should be done accordingly. Before a transabdominal ultrasound, it is advised to drink about a liter of water so that the bladder is full at the time of the examination - then the uterus will shift slightly towards the abdomen, and the picture will be clearer.
The degree of fullness of the bladder does not matter for transvaginal ultrasound. The amniotic fluid is a good acoustic window for imaging, but before the examination it is better to go to the toilet - this will be more comfortable. Before the study, you need to take a shower or “refresh” with wet wipes. nine0003
The accumulation of gases can distort the results of ultrasound, no matter what method it is performed. Therefore, expectant mothers suffering from flatulence are advised to take appropriate remedies the day before the examination and not eat anything that produces gas.
Note
There is an opinion that ultrasound "stuns" the unborn child. This, of course, is a myth that arose due to ignorance of the basic laws of physics. Ultrasound is a high frequency vibration that neither adults nor children can hear. Ultrasound is one of the most accurate, inexpensive and safe studies. nine0102
Blood test
A biochemical screening, also called a dual test, is done to measure the levels of two hormones (hence the name), free b-hCG and PAPP-A.
b-hCG (human chorionic gonadotropin) begins to be produced from the first days of pregnancy. Its amount gradually increases until about the 9th week, and then begins to gradually decrease. On average, for a period of 11–13 weeks, 50,000–55,000 mIU / ml is considered the norm. To determine the risk of pregnancy, MoM is used - a coefficient showing the degree of deviation of specific parameters from the norm for a given period. At this stage, the norm is from 0.5 to 2.5 MoM. An elevated level of hCG may indicate a multiple pregnancy, or, in the worst case, genetic pathologies of the fetus, or the presence of diabetes in the mother. Reduced hCG is typical of miscarriage, ectopic pregnancy, fetal death, or certain malformations (Patau syndrome and Edwards syndrome). nine0003
PAPP-A - A-plasma protein. The content rate for a period of 11–13 weeks is 0.79–6.01 mU / l (from 0.5 to 2.5 MoM). Low PAPP-A is a sign of such chromosomal pathologies as Down syndrome and Edwards syndrome, fetal death and miscarriage, fetal malnutrition (underweight) and preeclampsia.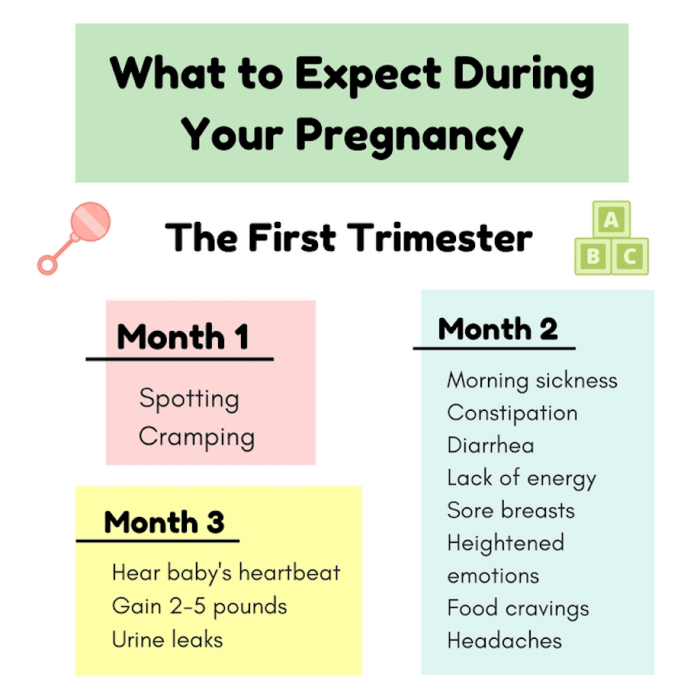 High PAPP-A is a sign of multiple pregnancy, large fetus or low placenta.
High PAPP-A is a sign of multiple pregnancy, large fetus or low placenta.
For the most accurate blood test, take it on an empty stomach, at least eight hours after your last meal. Two to three days before the analysis, you should refrain from fried, fatty, spicy, smoked foods, chocolate, nuts, seafood. It is also recommended not to have sexual intercourse. All this is not so significant, but it can affect the result in one way or another. nine0003
Second pregnancy screening
Second pregnancy screening at 18-20 weeks. It includes the same two stages - an ultrasound and a blood test, but the latter is only given if the woman did not do the first screening.
Ultrasound
This time the doctor determines not only the size, but also the position of the fetus, its bone structure, the condition of the internal organs, the place of attachment of the umbilical cord, and the volume of amniotic fluid. Here are the approximate main indicators of the norm for a period of 16-20 weeks:
- BPR - 26–56 mm.

- DBK (femur length) - 13–38 mm.
- DPC (humerus length) - 13–36 mm.
- exhaust (head circumference) - 112-186 mm.
- IAI (amniotic fluid index, that is, the volume of amniotic fluid) - 73–230 mm. Oligohydramnios can negatively affect the state of the child's bone structure and the development of his nervous system. nine0158
- Localization of the placenta. There is some risk only when the placenta is located on the lower part of the uterine cavity - with such localization, detachment of the placenta is possible.
- Umbilical cord. One of the most important parameters is the place of attachment of the umbilical cord. Edge, split or sheath attachment is fraught with fetal hypoxia and difficulties during childbirth, often it becomes an indication for caesarean section.
 The umbilical cord is fed through two arteries and one vein, but sometimes only one artery is available. This can cause fetal hypoxia, heart disease, disturbances in the work of the child's cardiovascular system, and cause low body weight of the baby. However, if all other tests and examinations do not show deviations from the norm, you should not worry. nine0158
The umbilical cord is fed through two arteries and one vein, but sometimes only one artery is available. This can cause fetal hypoxia, heart disease, disturbances in the work of the child's cardiovascular system, and cause low body weight of the baby. However, if all other tests and examinations do not show deviations from the norm, you should not worry. nine0158 - Cervix. The length of the cervix at this time should be 40-45 mm. A short cervix means a threatened miscarriage.
- Visualization. Unsatisfactory visualization can be caused both by the peculiarities of the position of the fetus or the excess weight of the expectant mother, and by edema or hypertonicity of the uterus.
Blood test
As already mentioned, if the first screening was not carried out, then during the second screening, a blood test for b-hCG is taken, the level of free estriol and AFP is also checked. Here are the norms for their content at the 16–20th week of pregnancy:
Here are the norms for their content at the 16–20th week of pregnancy:
- b-hCG - 4720-80 100 mIU/ml.
- Free estriol is a hormone whose level can be used to judge the state of the placenta. The norm is 1.17–3.8 ng / ml. Elevated estriol is characteristic of multiple pregnancy or a large fetus. Reduced - may be with the threat of miscarriage, placental insufficiency, anencephaly and Down's syndrome.
- AFP is a protein produced in the gastrointestinal tract of the fetus. Norm - 15-27 U / ml. A slightly lower AFP may mean that the gestational age was determined incorrectly (slightly underestimated). If AFP is very low, the cause may be the threat of miscarriage or fetal death, as well as the development of pathologies, such as Edwards or Down syndrome. High AFP is characteristic of neural tube pathologies, esophageal atresia, Meckel's syndrome. High AFP is also possible in women who have had an infectious disease during pregnancy.
 nine0158
nine0158
Third pregnancy screening
Third pregnancy screening at 30-34 - weeks. Based on the results of this screening, the doctor decides whether a caesarean section is necessary or if a natural birth is possible. The basis of the third screening is the same ultrasound. Dopplerography is sometimes prescribed - a study of the work of blood vessels. Here are the approximate norms of ultrasound for a given gestational age:
- BDP - 67–91 mm.
- DBK - 47–71 mm.
- WPC - 44-63 mm.
- exhaust - 238-336 mm.
- IAZH - 82–278 mm.
- Placental thickness - 23.9-40.8 mm.
Too thin placenta is not a particularly dangerous abnormality. The reason may be the miniature physique of a woman, her infectious diseases, hypertension.