What is cephalic position in pregnancy
Understanding Your Baby's Presentation at Birth
You know your busy bean is exploring their digs because sometimes you can feel those little feet kick you in the ribs (ouch!) to help propel them along. Just think of them as a little astronaut attached to you — the mother ship — with their oxygen (umbilical) cord.
Your baby may start moving around before you’re barely 14 weeks pregnant. However, you probably won’t feel anything until about the 20th week of pregnancy.
If your baby is bouncing around or turning in your womb, it’s a good sign. A moving baby is a healthy baby. There are even cute names for when you first feel your baby moving, like “fluttering” and “quickening.” Your baby’s movement is most important in the third trimester.
By this time, your growing baby may not be moving that much because the womb isn’t as roomy as it used to be. But your baby can probably still do acrobatic flips and turn himself upside down. Your doctor will closely monitor where your baby’s head is as your due date nears.
Your baby’s position inside you can make all the difference in how you give birth. Most babies automatically get into the head-first cephalic position just before they are born.
If you’re getting closer to your exciting due date, you might have heard your doctor or midwife mention the term cephalic position or cephalic presentation. This is the medical way of saying that baby is bottom and feet up with their head down near the exit, or birth canal.
It’s difficult to know which way is up when you’re floating in a warm bubble, but most babies (up to 96 percent) are ready to go in the head-first position before birth. The safest delivery for you and your baby is for them to squeeze through the birth canal and into the world headfirst.
Your doctor will start checking your baby’s position at week 34 to 36 of your pregnancy. If your baby is not head down by week 36, your doctor might try to gently nudge them into position.
Keep in mind, though, that positions can continue to change, and your baby’s position really doesn’t come into play until you’re ready to deliver.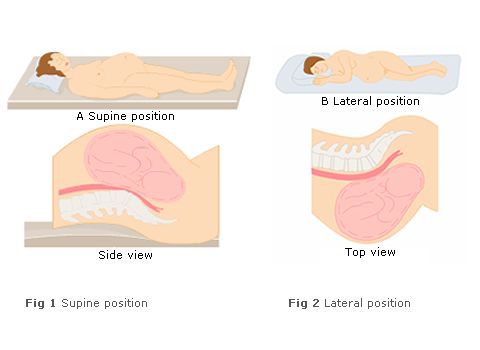
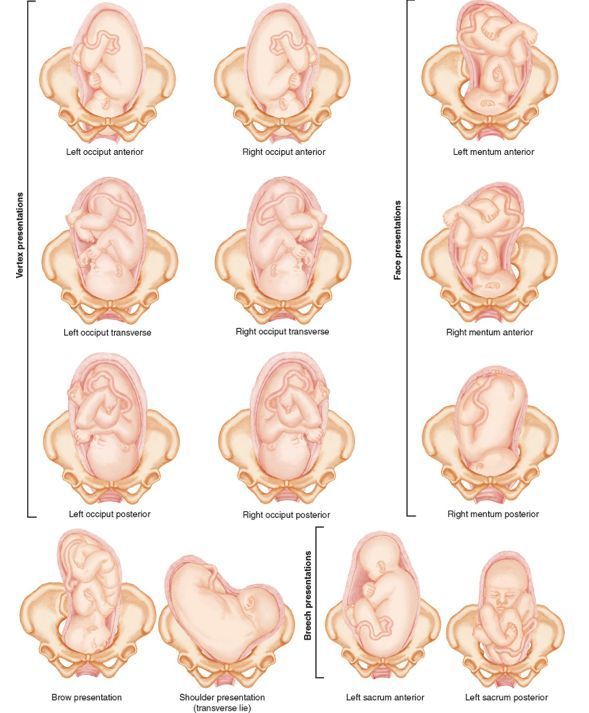
There are two kinds of cephalic (head-down) positions that your little one might assume:
- Cephalic occiput anterior. Your baby is head down and facing your back. Almost 95 percent of babies in the head-first position face this way. This position is considered to be the best for delivery because its easiest for the head to “crown” or come out smoothly as you give birth.
- Cephalic occiput posterior. Your baby is head down with their face turned toward your belly. This can make delivery a bit harder because the head is wider this way and more likely to get stuck. Only about 5 percent of cephalic babies face this way. This position is sometimes called a “sunny side up baby.”
Some babies in the head-first cephalic position might even have their heads tilted back so they move through the birth canal and enter the world face first. But this is very rare and most common in preterm (early) deliveries.
Your baby might settle into a breech (bottom-down) position or even a transverse (sideways) position.
Breech
A breech baby can cause complications for both mom and baby. This is because the birth canal has to open wider if your baby decides to come out bottom first. It’s also easier for their legs or arms to get tangled up a bit as they slide out. However, only about four percent of babies are in the bottom-first position when it’s time for delivery.
There are also different kinds of breech positions your baby could be in:
- Frank breech. This is when your baby’s bottom is down and their legs are straight up (like a pretzel) so their feet are close to their face. Babies are definitely flexible!
- Complete breech. This is when your baby is settled into an almost legs crossed position with their bottom down.
- Incomplete breech. If one of your baby’s legs are bent (like sitting cross-legged) while the other one is trying to kick toward their head or another direction, they’re in an incomplete breech position.
- Footling breech. Just like it sounds, this is one when or both of baby’s feet are down in the birth canal so they would exit foot first.
Transverse
A sideways position where your baby is lying horizontally across your stomach is also called a transverse lie. Some babies start like this close to your due date but then decide to shift all the way into the head-first cephalic position.
So if your baby is settled across your stomach like they’re swinging in a hammock, they may just be tired and taking a break from all the moving before another shift.
In rare cases, a baby can get wedged sideways in the womb (and not because the poor thing didn’t try moving). In these cases, your doctor might recommend a cesarean section (C-section) for your delivery.
Your doctor can find out exactly where your baby is by:
- A physical exam: feeling and pressing over your belly to get an outline of your baby
- An ultrasound scan: provides an exact image of your baby and even which way they’re facing
- Listening to your baby’s heartbeat: honing in on the heart gives your doctor a good estimate of where your baby is settled inside your womb
If you’re already in labor and your baby is not turning into a cephalic presentation — or suddenly decides to acrobat into a different position — your doctor might be concerned about your delivery.
Other things that your doctor has to check include where the placenta and umbilical cord are inside your womb. A moving baby can sometimes get their foot or hand caught in their umbilical cord. Your doctor might have to decide on the spot whether a C-section is better for you and your baby.
You might be able to tell what position your baby is in by where you feel their little feet practice their soccer kick. If your baby is in a breech (bottom-first) position, you might feel kicking in your lower stomach or groin area. If your baby is in the cephalic (head-down) position, they might score a goal in your ribs or upper stomach.
If you rub your belly, you might be able to feel your baby well enough to figure out what position they’re in. A long smooth area is likely your little one’s back, a round hard area is their head, while bumpy parts are legs and arms. Other curved areas are probably a shoulder, hand, or foot. You might even see the impression of a heel or hand against the inside of your belly!
What is lightening?
Your baby will likely naturally drop into a cephalic (head-down) position sometime between weeks 37 to 40 of your pregnancy. This strategic positional change by your brilliant little one is called “lightening.” You might feel a heavy or full sense in your lower stomach — that’s baby’s head!
This strategic positional change by your brilliant little one is called “lightening.” You might feel a heavy or full sense in your lower stomach — that’s baby’s head!
You might also notice that your belly button is now more of an “outie” than an “innie.” That’s also your baby’s head and upper body pushing against your stomach.
As your baby gets into cephalic position, you might suddenly notice that you can breathe more deeply because they’re not pushing up any longer. However, you might have to pee even more often because your baby is pushing against your bladder.
Stroking your belly helps you feel your baby, and your baby feels you right back. Sometimes stroking or tapping your stomach over the baby will get them to move. There are also some at-home methods for turning a baby, like inversions or yoga positions.
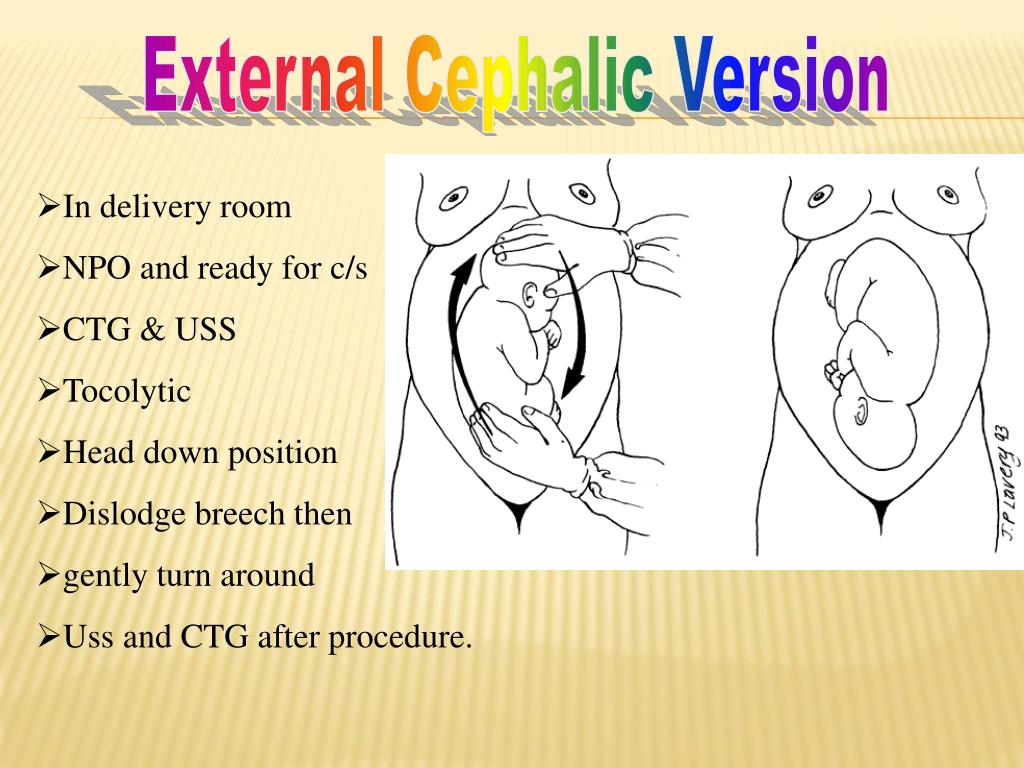
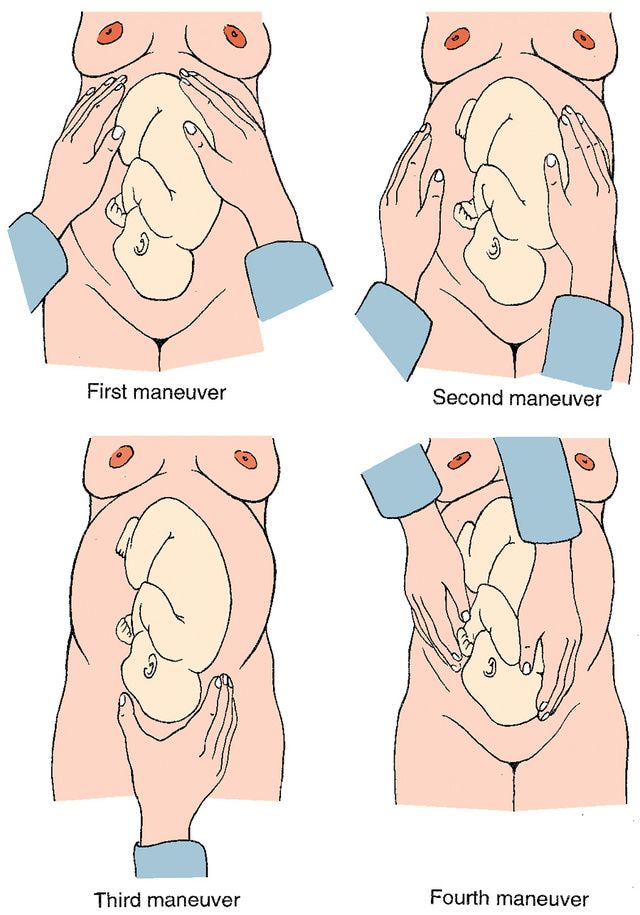
Doctors use a technique called external cephalic version (ECV) to get a breech baby into cephalic position. This involves massaging and pushing on your belly to help nudge your baby in the right direction.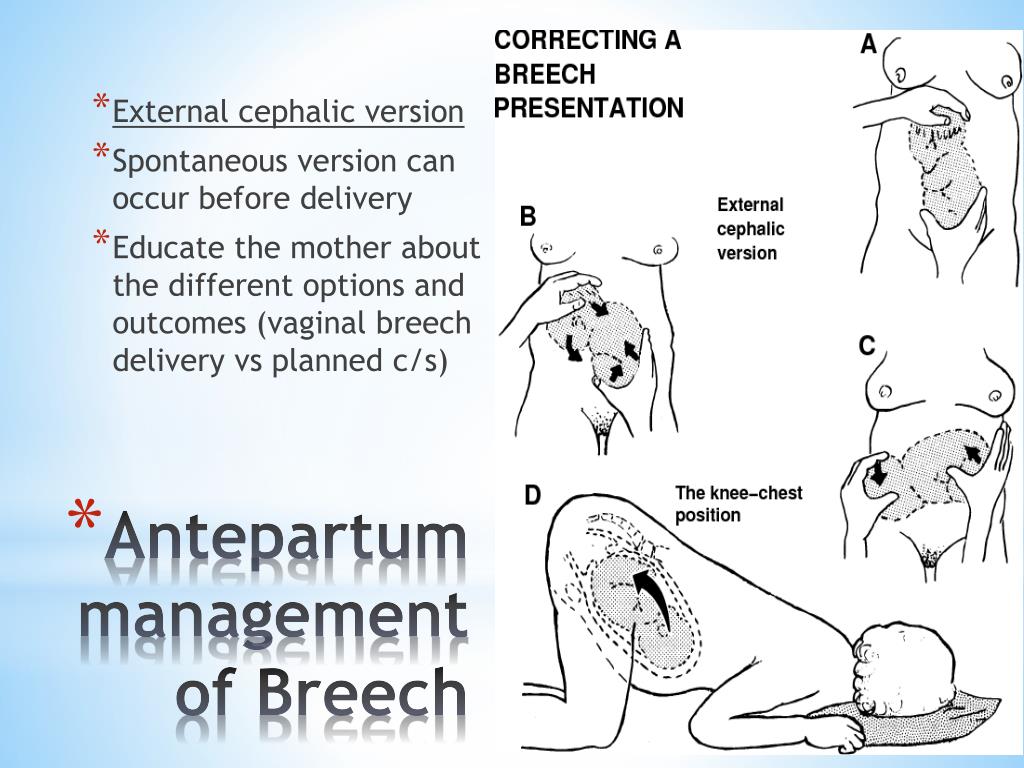 In some cases, medications that help you and your muscles relax can help turn your baby.
In some cases, medications that help you and your muscles relax can help turn your baby.
If your baby is already in cephalic position but not quite facing the right way, a doctor can sometimes reach through the vagina during labor to help gently turn baby the other way.
Of course, turning a baby also depends on how large they are — and how petite you are. And if you’re pregnant with multiples, your babies can be changing positions even during birth as the space in your womb opens up.
About 95 percent of babies drop down into the head-first position a few weeks or days before their due date. This is called the cephalic position, and it’s safest for mom and baby when it comes to giving birth.
There are different kinds of cephalic positions. The most common and safest one is where baby is facing your back. If your little one decides to change positions or refuses to float head down in your womb, your doctor might be able to coax him into the cephalic position.
Other baby positions like breech (bottom first) and transverse (sideways) might mean that you must have a C-section delivery. Your doctor will help you decide what’s best for you and your little one when it’s time for delivery.
Your doctor will help you decide what’s best for you and your little one when it’s time for delivery.
Understanding Your Baby's Presentation at Birth
You know your busy bean is exploring their digs because sometimes you can feel those little feet kick you in the ribs (ouch!) to help propel them along. Just think of them as a little astronaut attached to you — the mother ship — with their oxygen (umbilical) cord.
Your baby may start moving around before you’re barely 14 weeks pregnant. However, you probably won’t feel anything until about the 20th week of pregnancy.
If your baby is bouncing around or turning in your womb, it’s a good sign. A moving baby is a healthy baby. There are even cute names for when you first feel your baby moving, like “fluttering” and “quickening.” Your baby’s movement is most important in the third trimester.
By this time, your growing baby may not be moving that much because the womb isn’t as roomy as it used to be.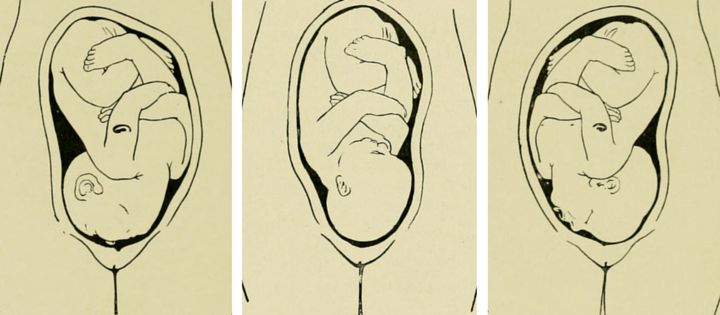 But your baby can probably still do acrobatic flips and turn himself upside down. Your doctor will closely monitor where your baby’s head is as your due date nears.
But your baby can probably still do acrobatic flips and turn himself upside down. Your doctor will closely monitor where your baby’s head is as your due date nears.
Your baby’s position inside you can make all the difference in how you give birth. Most babies automatically get into the head-first cephalic position just before they are born.
If you’re getting closer to your exciting due date, you might have heard your doctor or midwife mention the term cephalic position or cephalic presentation. This is the medical way of saying that baby is bottom and feet up with their head down near the exit, or birth canal.
It’s difficult to know which way is up when you’re floating in a warm bubble, but most babies (up to 96 percent) are ready to go in the head-first position before birth. The safest delivery for you and your baby is for them to squeeze through the birth canal and into the world headfirst.
Your doctor will start checking your baby’s position at week 34 to 36 of your pregnancy.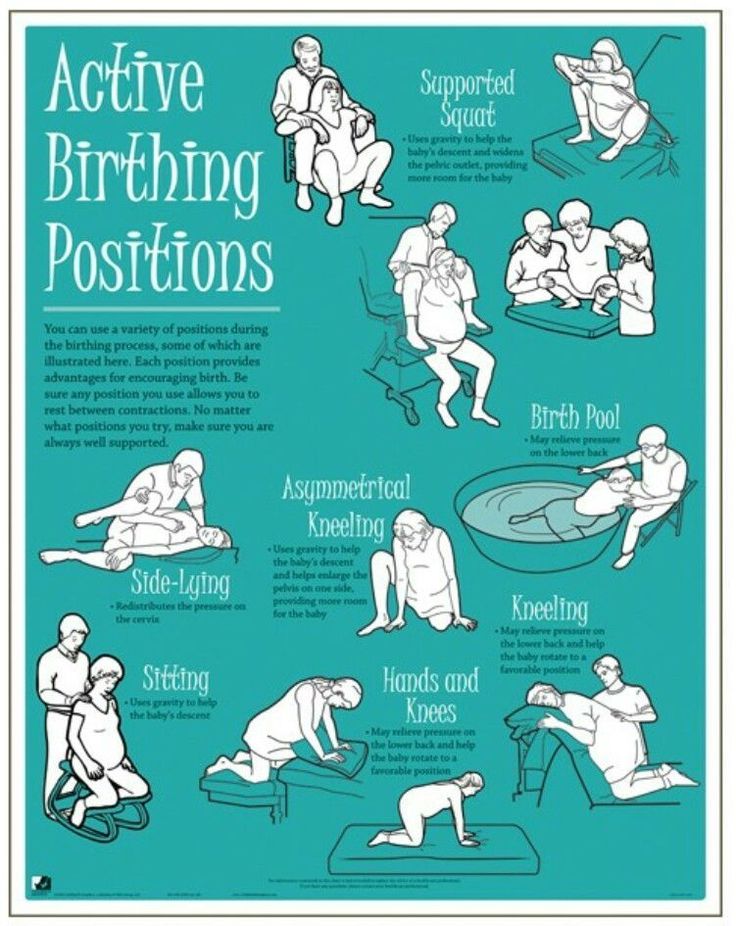 If your baby is not head down by week 36, your doctor might try to gently nudge them into position.
If your baby is not head down by week 36, your doctor might try to gently nudge them into position.
Keep in mind, though, that positions can continue to change, and your baby’s position really doesn’t come into play until you’re ready to deliver.
There are two kinds of cephalic (head-down) positions that your little one might assume:
- Cephalic occiput anterior. Your baby is head down and facing your back. Almost 95 percent of babies in the head-first position face this way. This position is considered to be the best for delivery because its easiest for the head to “crown” or come out smoothly as you give birth.
- Cephalic occiput posterior. Your baby is head down with their face turned toward your belly. This can make delivery a bit harder because the head is wider this way and more likely to get stuck. Only about 5 percent of cephalic babies face this way. This position is sometimes called a “sunny side up baby.”
Some babies in the head-first cephalic position might even have their heads tilted back so they move through the birth canal and enter the world face first.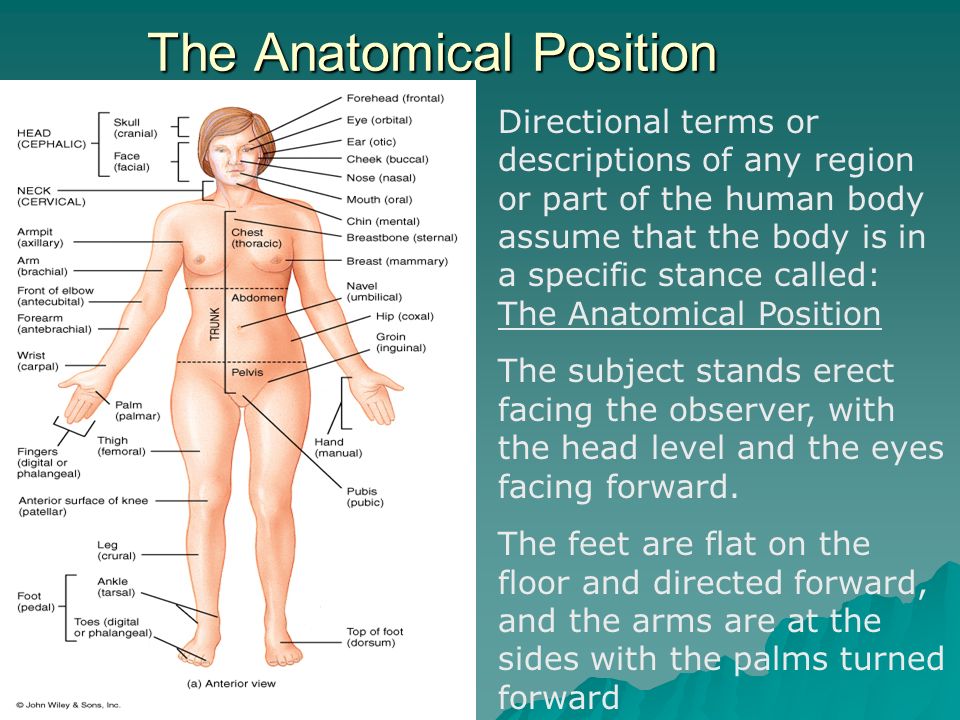 But this is very rare and most common in preterm (early) deliveries.
But this is very rare and most common in preterm (early) deliveries.
Your baby might settle into a breech (bottom-down) position or even a transverse (sideways) position.
Breech
A breech baby can cause complications for both mom and baby. This is because the birth canal has to open wider if your baby decides to come out bottom first. It’s also easier for their legs or arms to get tangled up a bit as they slide out. However, only about four percent of babies are in the bottom-first position when it’s time for delivery.
There are also different kinds of breech positions your baby could be in:
- Frank breech. This is when your baby’s bottom is down and their legs are straight up (like a pretzel) so their feet are close to their face. Babies are definitely flexible!
- Complete breech. This is when your baby is settled into an almost legs crossed position with their bottom down.
- Incomplete breech.
 If one of your baby’s legs are bent (like sitting cross-legged) while the other one is trying to kick toward their head or another direction, they’re in an incomplete breech position.
If one of your baby’s legs are bent (like sitting cross-legged) while the other one is trying to kick toward their head or another direction, they’re in an incomplete breech position. - Footling breech. Just like it sounds, this is one when or both of baby’s feet are down in the birth canal so they would exit foot first.
Transverse
A sideways position where your baby is lying horizontally across your stomach is also called a transverse lie. Some babies start like this close to your due date but then decide to shift all the way into the head-first cephalic position.
So if your baby is settled across your stomach like they’re swinging in a hammock, they may just be tired and taking a break from all the moving before another shift.
In rare cases, a baby can get wedged sideways in the womb (and not because the poor thing didn’t try moving). In these cases, your doctor might recommend a cesarean section (C-section) for your delivery.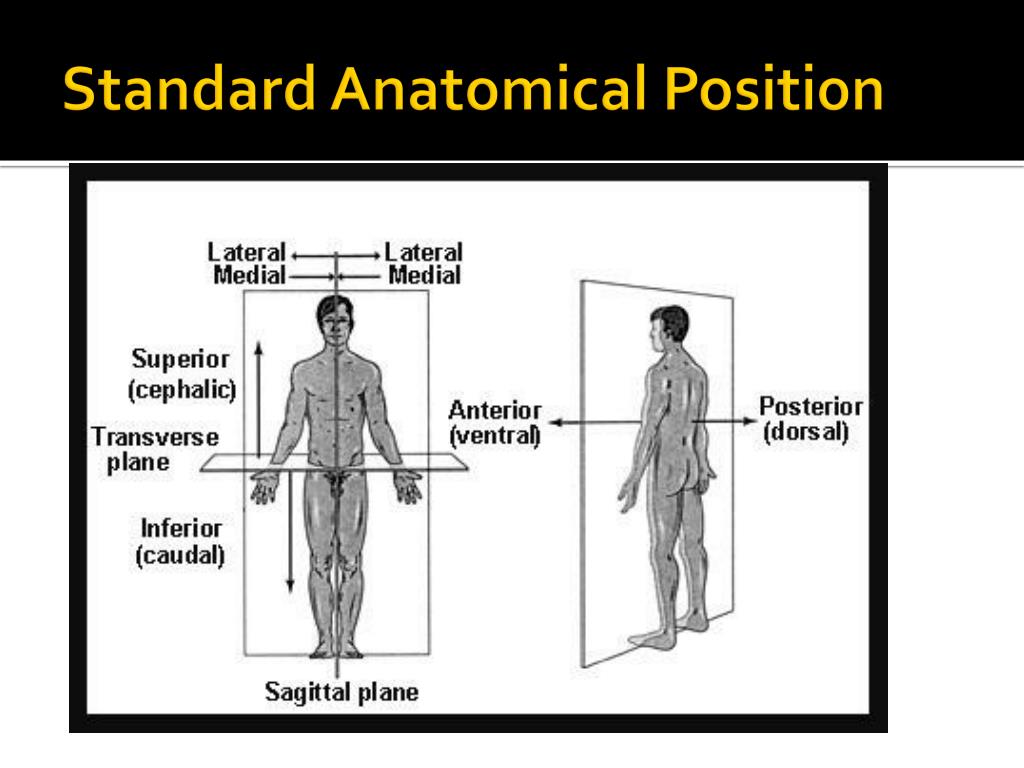
Your doctor can find out exactly where your baby is by:
- A physical exam: feeling and pressing over your belly to get an outline of your baby
- An ultrasound scan: provides an exact image of your baby and even which way they’re facing
- Listening to your baby’s heartbeat: honing in on the heart gives your doctor a good estimate of where your baby is settled inside your womb
If you’re already in labor and your baby is not turning into a cephalic presentation — or suddenly decides to acrobat into a different position — your doctor might be concerned about your delivery.
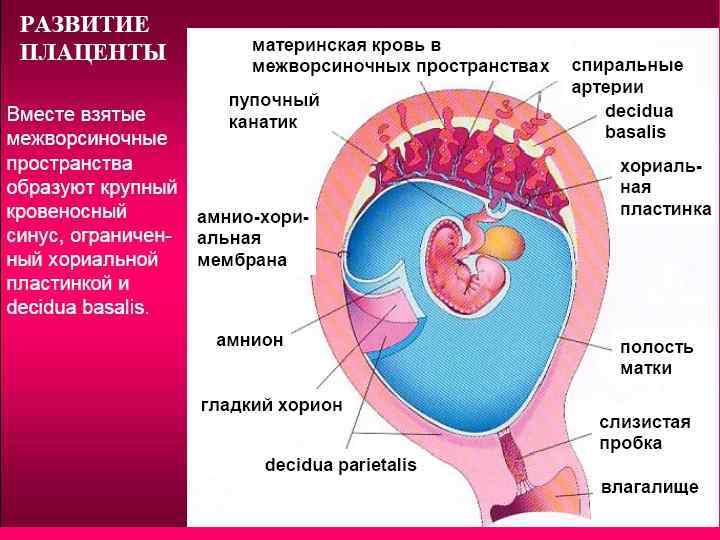
Other things that your doctor has to check include where the placenta and umbilical cord are inside your womb. A moving baby can sometimes get their foot or hand caught in their umbilical cord. Your doctor might have to decide on the spot whether a C-section is better for you and your baby.
You might be able to tell what position your baby is in by where you feel their little feet practice their soccer kick. If your baby is in a breech (bottom-first) position, you might feel kicking in your lower stomach or groin area. If your baby is in the cephalic (head-down) position, they might score a goal in your ribs or upper stomach.
If your baby is in a breech (bottom-first) position, you might feel kicking in your lower stomach or groin area. If your baby is in the cephalic (head-down) position, they might score a goal in your ribs or upper stomach.
If you rub your belly, you might be able to feel your baby well enough to figure out what position they’re in. A long smooth area is likely your little one’s back, a round hard area is their head, while bumpy parts are legs and arms. Other curved areas are probably a shoulder, hand, or foot. You might even see the impression of a heel or hand against the inside of your belly!
What is lightening?
Your baby will likely naturally drop into a cephalic (head-down) position sometime between weeks 37 to 40 of your pregnancy. This strategic positional change by your brilliant little one is called “lightening.” You might feel a heavy or full sense in your lower stomach — that’s baby’s head!
You might also notice that your belly button is now more of an “outie” than an “innie.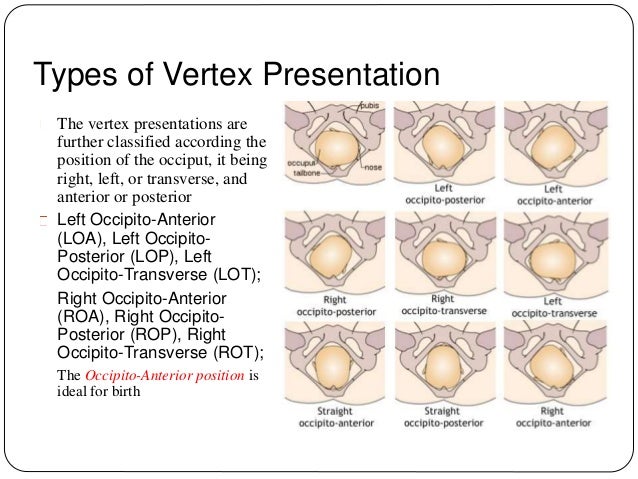 ” That’s also your baby’s head and upper body pushing against your stomach.
” That’s also your baby’s head and upper body pushing against your stomach.
As your baby gets into cephalic position, you might suddenly notice that you can breathe more deeply because they’re not pushing up any longer. However, you might have to pee even more often because your baby is pushing against your bladder.
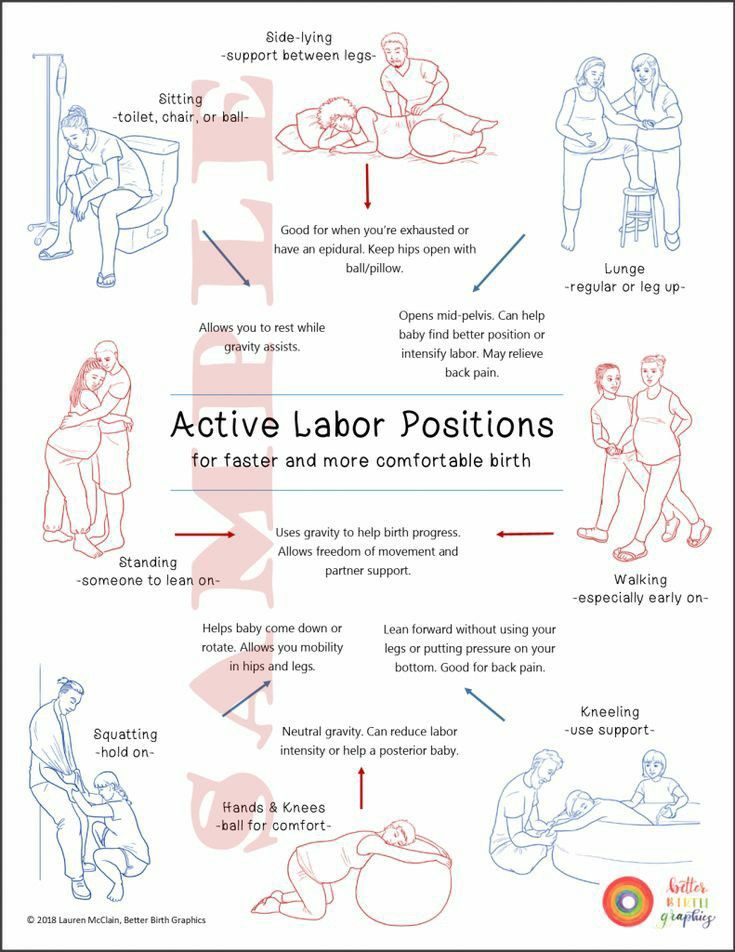
Stroking your belly helps you feel your baby, and your baby feels you right back. Sometimes stroking or tapping your stomach over the baby will get them to move. There are also some at-home methods for turning a baby, like inversions or yoga positions.
Doctors use a technique called external cephalic version (ECV) to get a breech baby into cephalic position. This involves massaging and pushing on your belly to help nudge your baby in the right direction. In some cases, medications that help you and your muscles relax can help turn your baby.
If your baby is already in cephalic position but not quite facing the right way, a doctor can sometimes reach through the vagina during labor to help gently turn baby the other way.
Of course, turning a baby also depends on how large they are — and how petite you are. And if you’re pregnant with multiples, your babies can be changing positions even during birth as the space in your womb opens up.
About 95 percent of babies drop down into the head-first position a few weeks or days before their due date. This is called the cephalic position, and it’s safest for mom and baby when it comes to giving birth.
There are different kinds of cephalic positions. The most common and safest one is where baby is facing your back. If your little one decides to change positions or refuses to float head down in your womb, your doctor might be able to coax him into the cephalic position.
Other baby positions like breech (bottom first) and transverse (sideways) might mean that you must have a C-section delivery. Your doctor will help you decide what’s best for you and your little one when it’s time for delivery.
How to sleep during pregnancy
It is difficult to overestimate the role of sleep in the life of every person.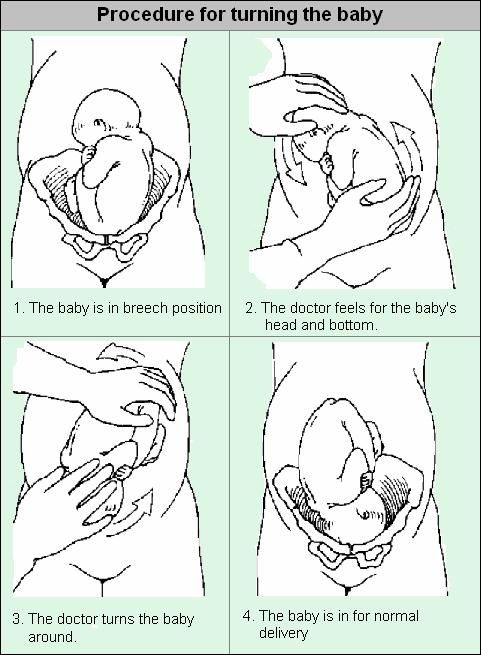 A complete healthy rest allows you to fully restore the functioning of the nervous system, relieve stress, improve performance and increase activity. Chronic sleep deprivation is the cause of many diseases. What can we say about a woman who is at the stage of bearing a baby. During this period, more than ever, she needs a healthy, long and full sleep. However, unfortunately, it is during this period that one can only dream of a restful sleep.
A complete healthy rest allows you to fully restore the functioning of the nervous system, relieve stress, improve performance and increase activity. Chronic sleep deprivation is the cause of many diseases. What can we say about a woman who is at the stage of bearing a baby. During this period, more than ever, she needs a healthy, long and full sleep. However, unfortunately, it is during this period that one can only dream of a restful sleep.
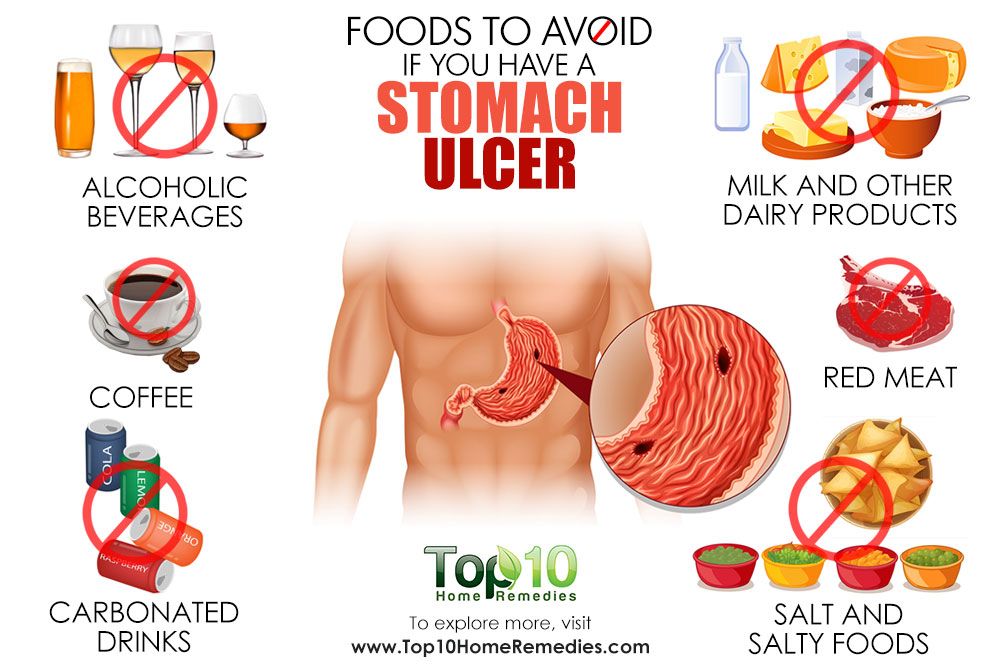
As soon as a woman finds out about her new position, she has to give up a lot for the sake of the health of her unborn baby. And you need to give up not only bad habits: alcohol, cigarettes, coffee, but also from a comfortable sleep.
The cause of insomnia can be :
- Anxiety;
- Frequent urination;
- Fears and phobias before a new stage of one's life;
- Nervousness and irritability;
- Digestive disorder;
- Toxicosis;
- Physical indisposition;
- Uncomfortable posture.
During the period of bearing a child, the female body experiences an extraordinary load, especially in the last trimester. The need for more sleep increases, because the body expends much more energy. Therefore, healthy sleep and pregnancy are inextricably linked.
As soon as a woman finds out about her new position, she has to give up a lot for the sake of the health of her unborn baby. And you need to give up not only bad habits: alcohol, cigarettes, coffee, but also from a comfortable sleep.
Let's try to figure out how to sleep during pregnancy, so as not only not to harm the health of your unborn baby, but to sleep well.
Looking for a comfortable sleeping position
Each person has his own favorite position, in which it is easy to fall asleep and sleep. Many do not imagine a comfortable rest on their backs, accustomed to sleeping on their stomachs. This habit will have to be sacrificed, as it is unsafe for the normal development of the fetus.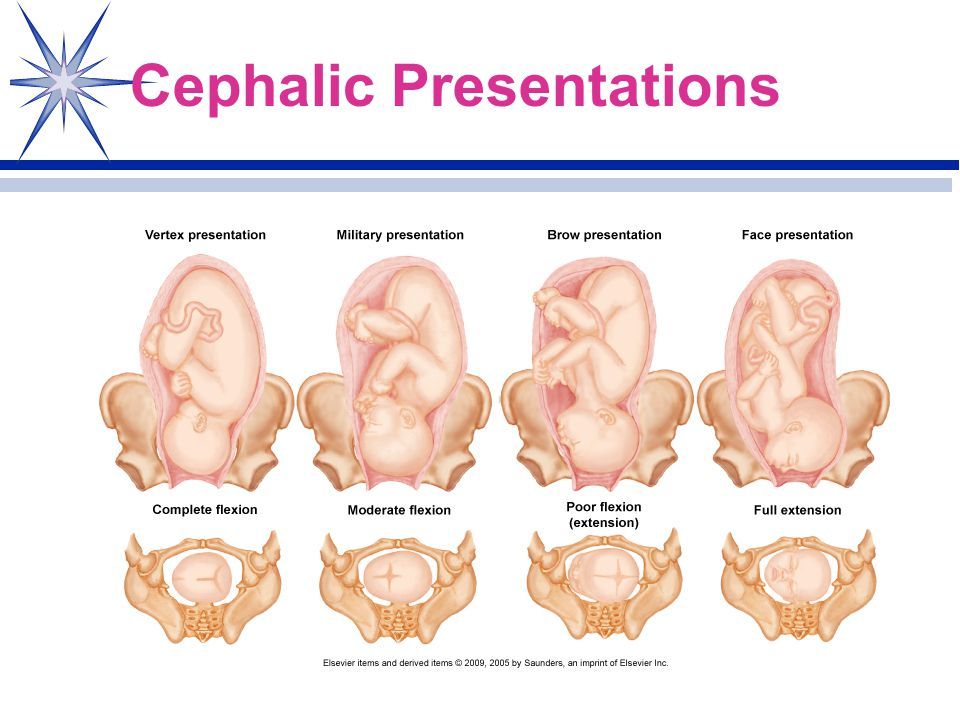 If in the first three months of pregnancy a woman can still sleep in the position in which she is used to and feels comfortable, then after the first trimester the growing belly will not allow her to lie safely in this position. Despite the natural protection of the baby in the form of amniotic fluid, there is a high probability of injuring the baby in a dream, squeezing it. But what is the right way to sleep during pregnancy?
If in the first three months of pregnancy a woman can still sleep in the position in which she is used to and feels comfortable, then after the first trimester the growing belly will not allow her to lie safely in this position. Despite the natural protection of the baby in the form of amniotic fluid, there is a high probability of injuring the baby in a dream, squeezing it. But what is the right way to sleep during pregnancy?
Back position
Even if you are used to sleeping in a Spartan position, on your back, with your arms spread wide, from the 28th week you will have to radically change your lifestyle. The fact is that as the fetus grows, the load on the intestines and vena cava will increase significantly, blocking the access of oxygen to the baby.
As soon as a woman finds out about her new position, she has to give up a lot for the sake of the health of her unborn baby. And you need to give up not only bad habits: alcohol, cigarettes, coffee, but also from a comfortable sleep.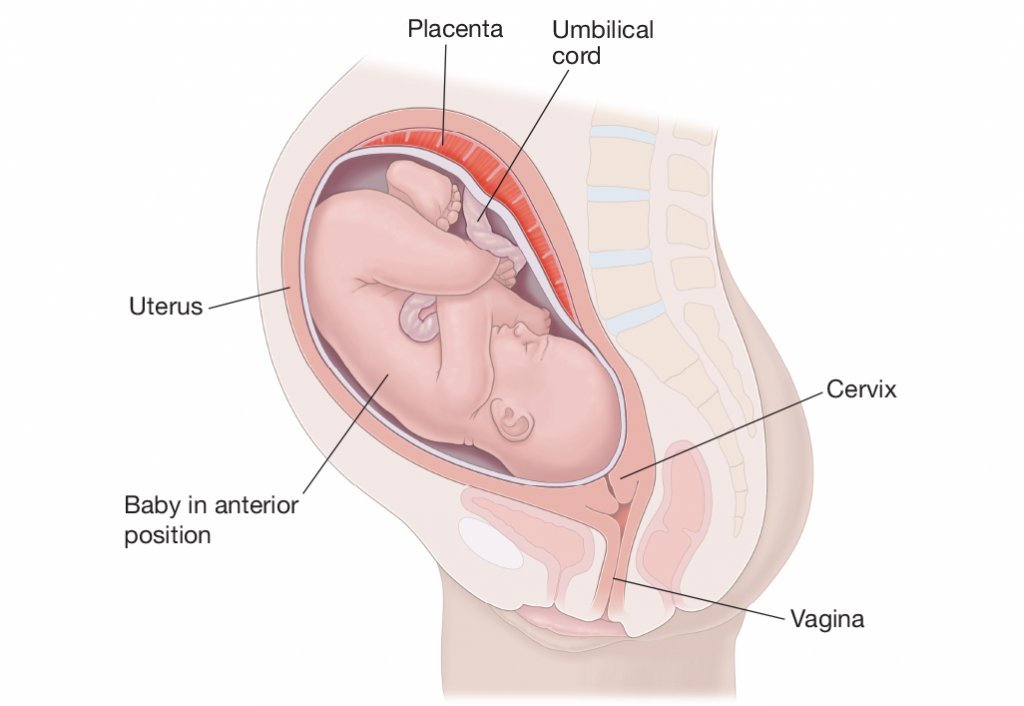
If you sleep on your back during pregnancy, you may experience the following problems:
- Dizziness;
- Nausea;
- Convulsions;
- Numb limbs;
- Pressure reduction;
- Hemorrhoids;
- Heaviness of breathing.
If you feel these symptoms or the baby gives persistent signals, you need to urgently change your position, so squeezing the vena cava is fraught not only with poor health for the mother, but also with a lack of oxygen supply to the fetus.
Stomach position
One of the most beloved positions for many people, which allows you to quickly fall asleep while hugging a pillow. Many women, as soon as they find out about the change in their lives, are interested in the question, is it possible to sleep on your stomach during pregnancy? Doctors recommend abandoning this position already in the first weeks, even before the enlarged belly makes it impossible to fall asleep peacefully.
If you are afraid during sleep, without controlling your movements, to arbitrarily roll over on your stomach, you can put a large pillow that does not allow you to change position.
Side position
In order to normalize your sleep and not harm the health of the baby, experts recommend sleeping on your side during pregnancy. And if at first this option seems unacceptable to many, after the second trimester, lying on your side is the only possible one. But here the question arises, on which side to sleep in order to ensure the safety of the fetus?
Sleeping on the right side can cause squeezing of the kidney, which can have dire consequences. The ideal posture is lying on the left side. Thus, you not only do not injure the unborn baby, but also improve blood flow along with oxygen to the placenta.
But one should not ignore the individual characteristics of each organism and the position of the fetus in the uterus. When the baby is in a transverse position, choose the side where the baby's head is. And with a breech presentation, doctors recommend changing the position several times a night.
If you still cannot improve your sleep, you feel unwell and you are tormented by insomnia, then it is better to consult a specialist.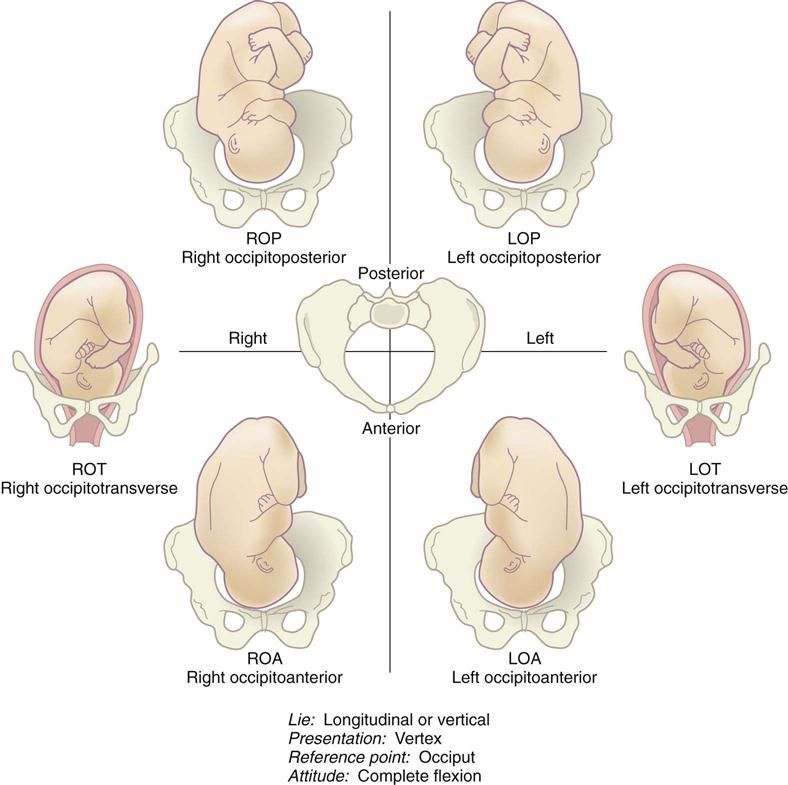 A good gynecologist will analyze the situation and help solve the problem. If necessary, he will prescribe a safe sedative that stabilizes the emotional state and helps to fall asleep calmly, resting and restoring the nervous system in a dream.
A good gynecologist will analyze the situation and help solve the problem. If necessary, he will prescribe a safe sedative that stabilizes the emotional state and helps to fall asleep calmly, resting and restoring the nervous system in a dream.
Help pillow
Fortunately, now modern manufacturers help women survive the pregnancy period with great comfort by offering special pillows. They are made taking into account the physiological characteristics of a woman in this period and allow you to find a comfortable position for relaxation.
You can buy two pillows and put one under your stomach and the other under your knees, looking for your best option. And you can buy a long banana-shaped pillow, which allows you to throw your leg on it while sleeping, which improves well-being and relieves the main load from the lower back and abdomen. Already in the last weeks of pregnancy, when the growing belly does not allow you to breathe normally, the pillow will allow you to take a comfortable half-sitting position.
Remember that pregnancy is your opportunity to gain strength and fully relax before the most crucial period in your life. Childbirth and the first weeks of caring for your baby will require a lot of energy from you, so good luck and sound sleep!
Dizziness during pregnancy - a dangerous symptom or the norm, why dizziness in early pregnancy
{{if type === 'partner-stocks'}}
{{/if}}
{{/if}} {{each list}}${this} {{if isGorzdrav}}
Delete
{{/if}}
{{/each}} {{/if}} Search by drug, disease, substance: DERMAKOSMETIKA, SOLGAR, R.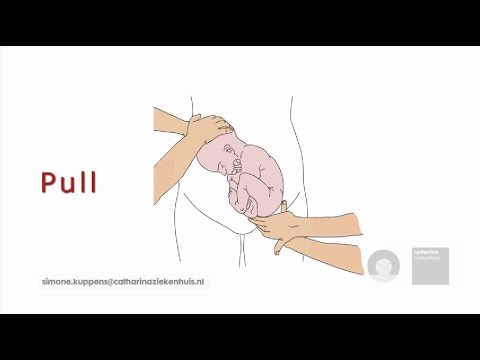 O.C.S., Bifiform,
O.C.S., Bifiform, Home
Articles
Dizziness during pregnancy - a dangerous symptom or a norm
Dizziness (vertigo) is the second most common neurological symptom after headache. It affects up to 5% of the world's population. During pregnancy, any deviations that affect the physical and emotional state of the expectant mother are undesirable. It is difficult for women in the position and without feeling the precariousness of space or the appearance of symptoms of near loss of consciousness. Therefore, dizziness during pregnancy is monitored and blocked as soon as possible. In this case, it is important to remember that vertigo is not a disease, but a symptom provoked by a physical condition, body structure, or exacerbated pathologies.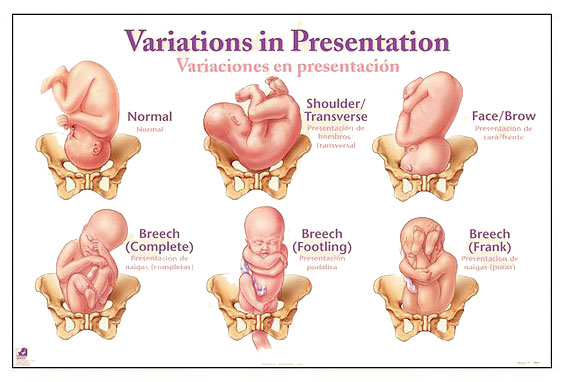 The way to deal with dizziness also depends on the provocateur of the disorder.
The way to deal with dizziness also depends on the provocateur of the disorder.
Symptoms of the disorder - how vertigo manifests itself in pregnant women
Women "in position" complain of the following signs of an attack of vertigo:
- Pulsation of blood in the temporal region is the first symptom that precedes an attack.
- Ringing in the ears - it is superimposed on the pulsation in the temporal region and indicates an increase in symptoms. At this stage, you should be alert and find a quiet place where you can wait until your head stops spinning.
- Loss of focus - this sign indicates the onset of dizziness, and most women complain of background darkening and white or black "midges" floating before their eyes.
- Feeling of weakness, profuse sweating, nausea, numbness of the fingers and toes - these signs of oxygen deficiency in the blood do not leave the pregnant woman until the end of the attack.
Non-pregnant women who experience spontaneous dizziness also complain of similar symptoms. Pregnant women feel dizzy much more often, and literally from the first trimester. And not all women experience this disorder painlessly. In some patients, dizziness comes to vomiting and loss of consciousness. After all, the severity of the attack is determined by the cause of the problem.
What can make you dizzy
According to WHO, dizziness and loss of stability in women are due to the following reasons:
- A sudden change in the position of the head or body - your vestibular apparatus does not have time to orient in space, against which neurological symptoms worsen. For the same reason, the patient may have a headache or neck pain.
- Oxygen starvation of the brain - stale air in the room, a large number of people in the neighborhood, closeness, all this ends in fainting even without a history of pregnancy.
- Decrease in blood pressure - against the background of hypotension, oxygen starvation of the brain develops, provoking dizziness and fainting.
 In this case, the head will hurt in the forehead and temples.
In this case, the head will hurt in the forehead and temples. - Hyperventilation of the lungs - an excess of oxygen and a fall below the norm of carbon dioxide leads to metabolic disorders, vertigo and fainting.
- Anemia and glucose deficiency - a drop in hemoglobin levels during pregnancy is observed in most patients, and iron deficiency reduces the oxygen content in the blood. Against this background, the head begins to hurt, and fainting occurs.
Vertigo is one of the symptoms indicating viral diseases, tumors and brain anomalies, diseases of the cardiovascular system, osteochondrosis, vegetative dystonia. And this condition can also be provoked by a sharp change in weather due to a jump in atmospheric pressure. Therefore, pregnant women and their relatives should not panic when stability is lost.
Most serious illnesses are detected during pregnancy monitoring. Therefore, in a healthy woman, depending on the trimester, the most likely cause of vertigo is increased blood supply to the uterus, fetal pressure on internal organs, and other “profile” problems.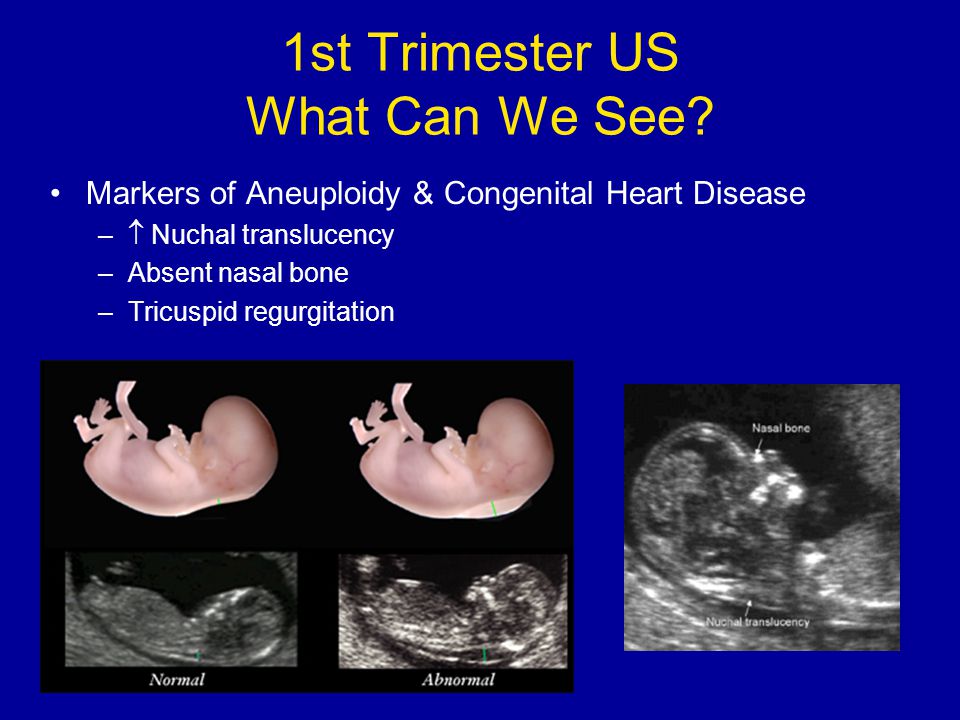
Vertigo in the first trimester — causes and consequences
During the first weeks of pregnancy, all systems of the future mother's body are restructured. A woman's hormonal background changes, immunity is suppressed, blood supply to the uterus increases. The pregnant woman will feel sick from toxicosis throughout the first trimester, in addition, in the early stages she will face severe attacks of vertigo. Moreover, during the starting toxicosis, the head is spinning especially strongly.
In addition to hormonal changes, the causes of vertigo in the early stages include the careless behavior of the patient. After confirming the status of a future mother, women continue to live without taking into account the peculiarities of their condition. But nature prioritizes from the first days of gestation. Systems and internal organs are still designed to serve one person. Therefore, even with slight overwork or frequent lack of sleep, the vestibular apparatus breaks down literally on the go. The body is filled with heaviness, the sense of balance disappears in an unknown direction (you will be rocked, stagger and feel sick in any transport), severe shortness of breath appears.
The body is filled with heaviness, the sense of balance disappears in an unknown direction (you will be rocked, stagger and feel sick in any transport), severe shortness of breath appears.
How to deal with vertigo in the early stages? In this case, you need to reconsider your regimen. Give up night shifts, hard physical work. And be sure to sign up for a consultation - obstetricians will explain to you again why a woman in position should go to bed no later than 23:00 and sleep at least 9-10 hours a day.
Dizziness during the second trimester - a danger or a norm?
The hormonal storm will shake the body during the entire first trimester, but by the beginning of the second third, the restructuring of the immune system will be over. The fetus will finish forming organs, the blood flow will be adjusted to the needs of two people, and the expectant mother will find a long-awaited peace. At this time, vertigo does not bother patients very much. But no doctor can rule out this problem.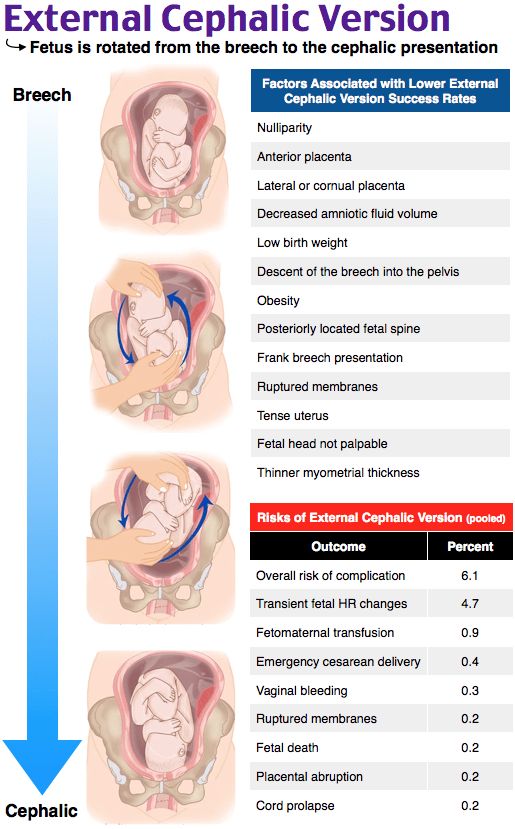 After all, a woman's body reacts to external stimuli in slowdown mode, and the growing uterus absorbs up to 60% of the blood flow.
After all, a woman's body reacts to external stimuli in slowdown mode, and the growing uterus absorbs up to 60% of the blood flow.
As a result, provocateurs of dizziness in the second trimester are:
- Prolonged immobility, followed by a sudden attempt to stand up or sit down — after such a shake, the head is spinning especially strongly.
- Oxygen starvation provoked by anemia, stuffiness or heart problems - under the weight of these problems, the patient begins to stagger even in a sitting position.
- Hypotension provoked by the weather or health condition - in this case, not only vertigo is observed, but also fainting.
At this time, vertigo is rare, so with frequent dizziness, a pregnant woman should see a doctor. He must figure out why you are dizzy in order to eliminate the causes and consequences of the disorder. The latter are extremely unpleasant, up to the threat of miscarriage and fetal arrest due to oxygen starvation.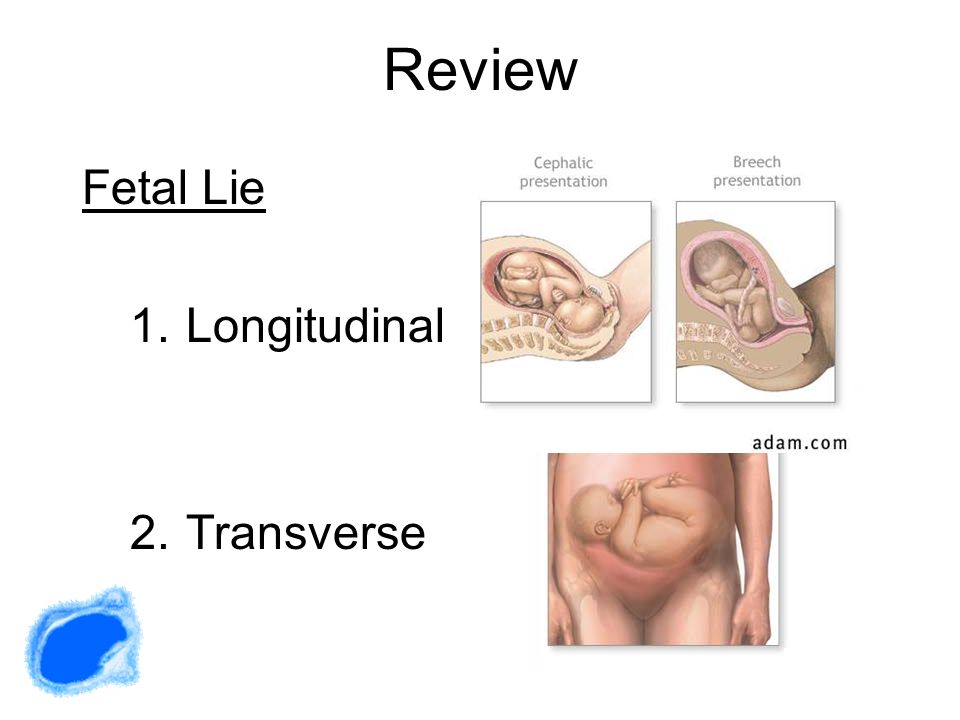
Why can I feel dizzy in the third trimester?
In the later stages, vertigo is a normal, almost natural phenomenon. In the third trimester, a woman feels weak and dizzy for an obvious reason - the uterus, ready for childbirth, consumes most of the blood flow, provoking oxygen starvation of the brain. Because of this, the patient has a strong attack of vertigo, but without nausea and fainting. If you begin to feel sick during this period, contact your doctor immediately.
In addition, by the third trimester, the uterus grows so much that it begins to press down on the vena cava, slowing down the intensity of blood flow. Therefore, in the later stages, one can observe a relatively strong, but completely safe attack of dizziness, which disturbs a woman even in a supine position.
The main danger of the last trimester is severe nausea, and with mild vertigo you will have to live until the very birth. However, the true cause of a strong or weak attack of vertigo can only be established through laboratory and hardware diagnostics.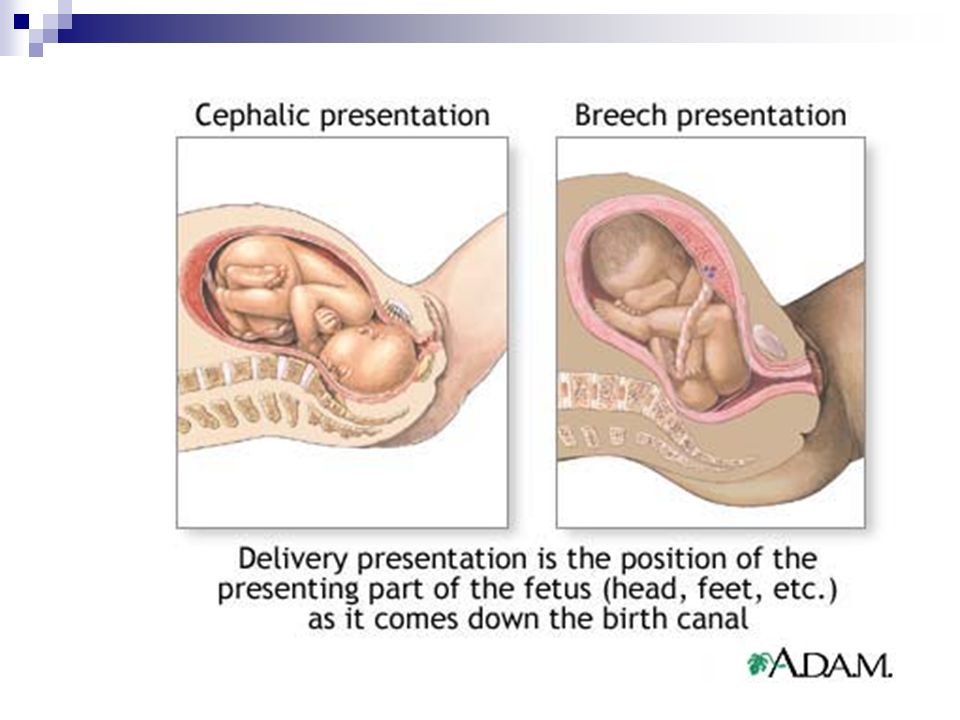
How to identify the causes of dizziness in a pregnant woman
Early and late vertigo is an almost natural condition of the expectant mother. And some women in labor complained of seizures from the first to the last week. But this does not mean that nothing needs to be done with patients experiencing frequent attacks of vertigo - in this case, at least monitoring of the health of the woman and the fetus is necessary.
If the seizures appear too often or disturb the pregnant woman constantly, especially in the second trimester, the obstetrician will write a referral to a neuropathologist and psychoneurologist. These doctors must decide what to do with such a patient. After all, constantly disturbing attacks of vertigo indicate the onset of serious problems with the cardiovascular, immune and neurological systems.
To confirm or refute the fears of neuropathologists and psychoneurologists, the patient is sent for hardware and laboratory diagnostics.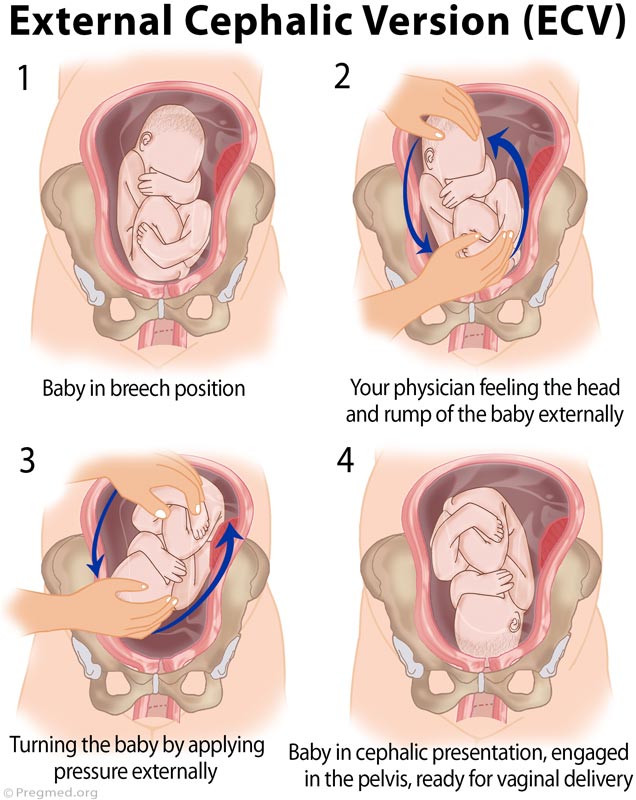 In these circumstances, it is customary to do an MRI, radiography of the cervical vertebrae, a urine test and blood biochemistry. Based on the results of these tests, a conclusion is prepared on the condition of the pregnant woman and symptomatic or deep therapy for vertigo is prescribed.
In these circumstances, it is customary to do an MRI, radiography of the cervical vertebrae, a urine test and blood biochemistry. Based on the results of these tests, a conclusion is prepared on the condition of the pregnant woman and symptomatic or deep therapy for vertigo is prescribed.
Treatment of dizziness in pregnancy
The treatment of serious pathologies, the symptoms of which are weakness and dizziness, requires considerable effort and expense. The treatment regimen for neurological, cardiovascular and oncological diseases is prescribed by specialized doctors. Fortunately, every year among pregnant women there is a very insignificant percentage of such patients.
Most women suffer from vertigo due to natural causes - due to changes in the uterine blood supply and hormonal storm. Only childbirth can cure these problems. During gestation, doctors can relieve the symptoms of vertigo by prescribing the following drugs to the patient suffering from dizziness:
- sedative drugs - they will relieve stress;
- antiemetics - they make life easier during the first trimester;
- erythrocyte stimulants - this drug enhances blood oxygen saturation;
- vitamin B12 and folic acid - they increase hemoglobin;
- caffeine - it increases blood pressure.