What is a haemorrhage
Causes, Emergency Symptoms, First Aid & More
Bleeding, also called hemorrhage, is the name used to describe blood loss. It can refer to blood loss inside the body, called internal bleeding, or to blood loss outside of the body, called external bleeding.
Blood loss can occur in almost any area of the body. Internal bleeding occurs when blood leaks out through a damaged blood vessel or organ. External bleeding happens when blood exits through a break in the skin.
Blood loss from bleeding tissue can also be apparent when blood exits through a natural opening in the body, such as the:
- mouth
- vagina
- rectum
- nose
Bleeding is a common symptom. A variety of incidents or conditions can cause bleeding. Possible causes include:
Traumatic bleeding
An injury can cause traumatic bleeding. Traumatic injuries vary in their severity.
Common types of traumatic injury include:
- abrasions (scrapes) that don’t penetrate too far below the skin
- hematoma or bruises
- lacerations (cuts)
- puncture wounds from items like needles, nails, or knives
- crushing injuries
- gunshot wounds
Medical conditions
There are also some medical conditions that can cause bleeding. Bleeding due to a medical condition is less common than traumatic bleeding.
Conditions that can cause bleeding include:
- hemophilia
- leukemia
- liver disease
- menorrhagia, heavy or prolonged menstrual bleeding, like what’s sometimes seen in endometriosis
- thrombocytopenia, low blood platelet count
- von Willebrand disease
- vitamin K deficiency
- brain trauma
- colon diverticulosis
- lung cancer
- acute bronchitis
Medicines
Some medicines and certain treatments can increase your chances of bleeding, or even cause bleeding. Your doctor will warn you about this when they first prescribe the therapy. And they’ll tell you what to do if bleeding occurs.
Medications that may be responsible for bleeding include:
- blood thinners
- antibiotics, when used on a long-term basis
- radiation therapy
- aspirin and other NSAIDs
If bleeding is severe, seek help immediately.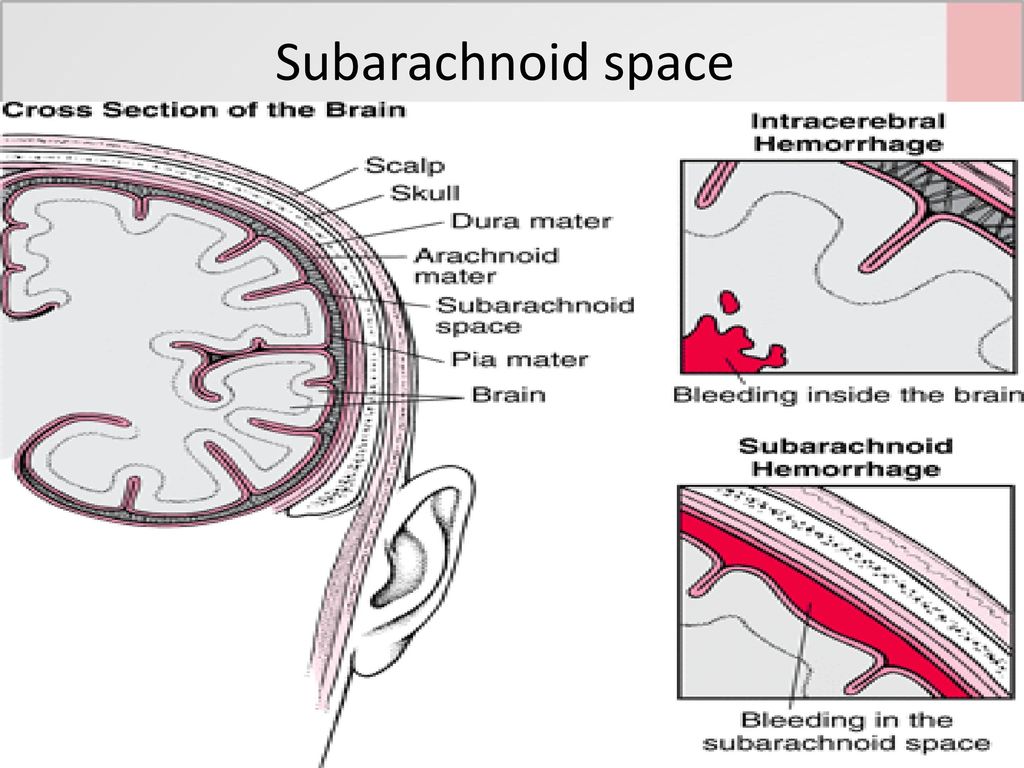 You should seek emergency help if you suspect internal bleeding. This can become life-threatening.
You should seek emergency help if you suspect internal bleeding. This can become life-threatening.
People who have bleeding disorders or take blood thinners should also seek emergency help to stop bleeding.
Seek medical help if:
- the person has gone into shock or has a fever
- the bleeding cannot be controlled using pressure
- the wound requires a tourniquet
- the bleeding was caused by a serious injury
- the wound may need stitches to stop bleeding
- foreign objects are stuck inside the wound
- the wound appears to be infected, such as swelling or leaking a whitish-yellow or brown pus, or has redness
- the injury occurred due to a bite from an animal or human
When you call for help, emergency services will tell you what to do and when they’ll arrive.
In most cases, emergency services will tell you to continue to put pressure on the wound and keep reassuring the person who’s bleeding. You may also be told to lay the person down to reduce their risk of fainting.
A person can bleed to death in 5 minutes. Bystanders may be able to save a life before emergency personnel can arrive.
There is a national campaign called Stop the Bleed to teach anyone how to stop bleeding. People in mass casualty events have died from blood loss even when their wounds shouldn’t have been fatal.
First aid for traumatic bleeding
It’s possible to treat external traumatic bleeding. Seek emergency help if the person is having any of the emergency signs listed above and if you need help to stop the bleeding.
The person who’s bleeding should try to remain calm to keep their heart rate and blood pressure controlled. Either heart rate or blood pressure being too high will increase the speed of bleeding.
Lay the person down as soon as possible to reduce the risk of fainting, and try to elevate the area that’s bleeding.
Remove loose debris and foreign particles from the wound. Leave large items such as knives, arrows, or weapons where they are.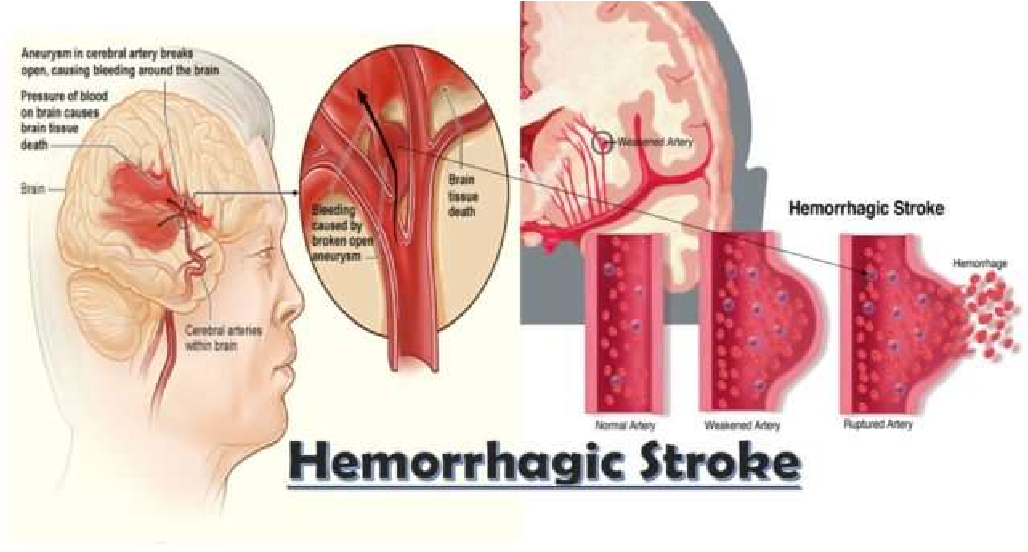 Removing these objects can cause further harm and will likely increase the bleeding. In this case, use bandages and pads to keep the object in place and absorb the bleeding.
Removing these objects can cause further harm and will likely increase the bleeding. In this case, use bandages and pads to keep the object in place and absorb the bleeding.
Use the following to put pressure onto the wound:
- a clean cloth
- bandages
- clothing
- your hands (after applying protective gloves)
Maintain medium pressure until the bleeding has slowed and stops.
Do not:
- remove the cloth when bleeding stops. Use an adhesive tape or clothing to wrap around the dressing and hold it in place. Then place a cold pack over the wound.
- look at the wound to see if bleeding has stopped. This can disturb the wound and cause it to begin bleeding again.
- remove the cloth from the wound, even if blood seeps through the material. Add more material on top, and continue the pressure.
- move anyone with an injury to the head, neck, back, or leg
- apply pressure to an eye injury
Use tourniquets only as a last resort.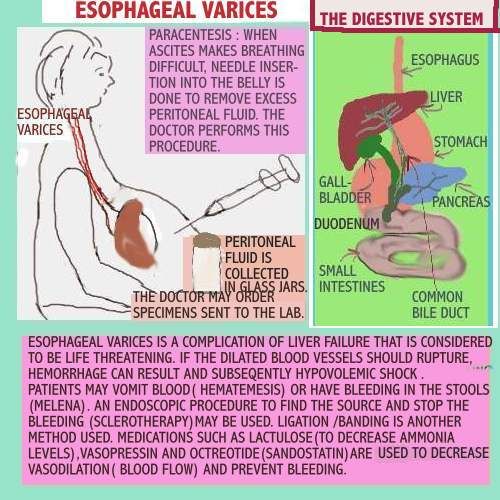 An experienced person should apply the tourniquet. To apply a tourniquet, follow these steps:
An experienced person should apply the tourniquet. To apply a tourniquet, follow these steps:
- Identify where to place the tourniquet. Apply it to a limb between the heart and the bleeding.
- Make the tourniquet using bandages, if possible. Wrap them around the limb and tie a half knot. Ensure there is enough room to tie another knot with the loose ends.
- Place a stick or rod between the two knots.
- Twist the stick to tighten the bandage.
- Secure the tourniquet in place with tape or cloth.
- Check the tourniquet at least every 10 minutes. If the bleeding slows enough to be controlled with pressure, release the tourniquet and apply direct pressure instead.
You will need emergency medical care if:
- bleeding is caused by a serious injury
- bleeding can’t be controlled
- bleeding is internal
Paramedics will attempt to control the bleeding before rushing you to the hospital. In some cases, care might be given at home or while on a stretcher.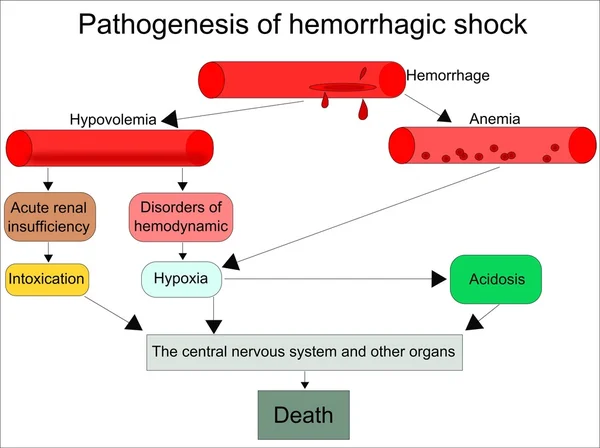 The treatment required will depend on the cause of the bleeding.
The treatment required will depend on the cause of the bleeding.
In rare cases, surgery may be required to stop bleeding.
A medical professional should see anyone who experiences unexplained or uncontrolled bleeding.
Traumatic bleeding
If an injury or accident causes bleeding, it may be stopped with local first aid. If it’s just a minor wound, it may heal without further care.
More significant wounds may require sutures, medicated dressings, or corrective surgery.
Medical bleeding
If a medical condition causes bleeding, and the condition isn’t identified or diagnosed, the bleeding is likely to recur.
Any bleeding that continues without medical treatment could be fatal. For example, if someone has acute bleeding in a short period of time and loses 30 percent or more of their blood volume, they could bleed to death very quickly and would require IV fluid and transfusion of packed red blood cells for resuscitation.
Even medical conditions that cause slow blood loss over time can add up and cause major organ injury, possibly leading to death.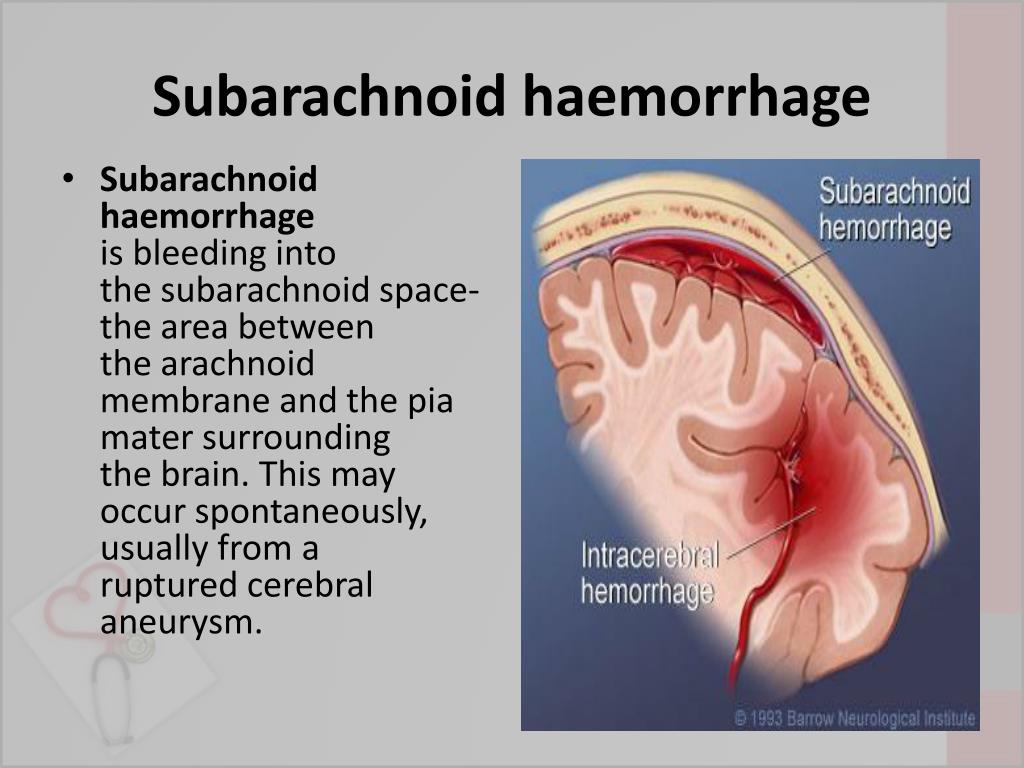
Exsanguination, which is severe bleeding or bleeding to death, can occur without any visible external bleeding. Catastrophic internal hemorrhages can cause a great deal of blood loss, such as ruptured blood vessel aneurysms.
From Cuts, Wounds, and More
First aid
Injuries and certain medical conditions can result in bleeding. This can trigger anxiety and fear, but bleeding has a healing purpose. Still, you need to understand how to treat common bleeding incidents such as cuts and bloody noses, as well as when to seek medical help.
Before you begin to treat an injury, you should identify its severity as best you can. There are some situations in which you shouldn’t try to administer any kind of first aid at all. If you suspect that there’s internal bleeding or if there’s an embedded object surrounding the site of the injury, immediately call 911 or your local emergency services.
Also seek immediate medical care for a cut or wound if:
- it’s jagged, deep, or a puncture wound
- it’s on the face
- it’s the result of an animal bite
- there’s dirt that won’t come out after washing
- the bleeding will not stop after 15 to 20 minutes of first aid
If a person is bleeding profusely, be on the lookout for symptoms of shock. Cold, clammy skin, a weakened pulse, and loss of consciousness can all indicate that a person is about to go into shock from blood loss, according to the Mayo Clinic. Even in cases of moderate blood loss, the bleeding person may feel lightheaded or nauseous.
Cold, clammy skin, a weakened pulse, and loss of consciousness can all indicate that a person is about to go into shock from blood loss, according to the Mayo Clinic. Even in cases of moderate blood loss, the bleeding person may feel lightheaded or nauseous.
If possible, have the injured person lie down on the floor while you wait for medical care to arrive. If they are able, have them elevate their legs above their heart. This should help circulation to the vital organs while you wait for help. Hold continuous direct pressure on the wound until help arrives.
When your skin is cut or scraped, you begin to bleed. This is because blood vessels in the area are damaged. Bleeding serves a useful purpose because it helps to clean out a wound. However, too much bleeding can cause your body to go into shock.
You can’t always judge the seriousness of a cut or wound by the amount it bleeds. Some serious injuries bleed very little. On the other hand, cuts on the head, face, and mouth may bleed a lot because those areas contain a lot of blood vessels.
Abdominal and chest wounds can be quite serious because internal organs may be damaged, which can cause internal bleeding as well as shock. Abdominal and chest wounds are considered an emergency, and you should call for immediate medical help. This is especially important if there are symptoms of shock, which may include:
- dizziness
- weakness
- pale and clammy skin
- shortness of breath
- increased heart rate
A first aid kit that’s properly stocked can make all the difference in stopping heavy bleeding. You should keep the following items around for situations where you may need to close a wound:
- sterilized medical gloves
- sterile gauze dressings
- small scissors
- medical grade tape
Saline wash can also be helpful to have on hand in order to clear out debris or dirt from a wound without touching it. An antiseptic spray, applied at the site of the cut, can help staunch blood flow and also reduce the risk of a cut becoming infected later on.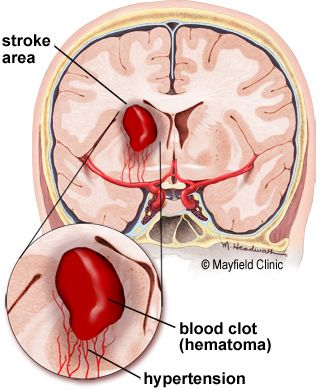
In the days following an injury, be on the lookout to ensure that a wound is healing correctly. If the initial scab covering the wound grows bigger or becomes surrounded by redness, there may be an infection. A cloudy fluid or pus draining from the wound is also a sign of possible infection. If the person develops a fever or begins to have pain again at the sign of the cut, seek medical attention immediately.
First aid do’s
- Help the person to remain calm. If the cut is large or bleeding heavily, have them lie down. If the wound is on an arm or leg, raise the limb above the heart to slow bleeding.
- Remove obvious debris from the wound, such as sticks or grass.
- If the cut is small, wash it out with soap and water.
- After putting on clean latex gloves, apply firm pressure to the wound with a folded cloth or bandage for about 10 minutes. If blood soaks through, add another cloth or bandage and continue putting pressure on the cut for an additional 10 minutes.
- When bleeding has stopped, tape a clean bandage over the cut.
First aid don’ts
- Don’t remove an object if it’s embedded in the body.
- Don’t attempt to clean a large wound.
- When first applying the bandage, don’t remove it to look at the wound during this time. It may begin bleeding again.
Sometimes injuries that aren’t traumatic or painful can bleed a great deal. Nicks from shaving, scrapes from falling off of a bike, and even pricking a finger with a sewing needle can result in excessive bleeding. For minor injuries such as these, you’ll still want to stop the injury from bleeding. A sterilized bandage or Band-Aid, antiseptic spray, and a healing agent such as Neosporin can all be helpful in treating these injuries and preventing future infection.
Even with a minor cut, it’s possible to have nicked an artery or blood vessel. If bleeding is still occurring after 20 minutes, medical attention is needed. Don’t ignore a wound that won’t stop bleeding just because it looks small or isn’t painful.
A bloody nose is common in both children and adults. Most nosebleeds are not serious, especially in children. Yet, adults can have nosebleeds related to high blood pressure or hardening of the arteries, and it may be more difficult to stop them.
Having tissues in your first aid kit, along with a topical nasal spray that is designed to go in the nasal passage (such as Sinex or Afrin), will help you administer first aid for a nosebleed.
First aid for a nosebleed
- Have the person sit down and lean their head forward. This will reduce pressure in the nasal veins and slow the bleeding. It will also keep blood from flowing down into the stomach, which can cause nausea.
- If you’d like, use a nasal spray in the bleeding nostril while the person holds their head still. Have them push the bleeding nostril firmly against the septum (the dividing wall in the nose). If the person is unable to do this, put on latex gloves and hold the nose for them for five to 10 minutes.
- Once the nose stops bleeding, instruct the person not to blow their nose for several days. This could dislodge the clot and cause bleeding to begin again.
Seek professional help for a nosebleed if bleeding does not stop after about 20 minutes, or if the nosebleed is related to a fall or injury. The nose may have been broken during an injury. Recurring nosebleeds could be a symptom of something more serious, so tell a doctor if you’re having regular nosebleeds.
Any situation that involves heavy bleeding can create fear and stress. Most people don’t want to see their own blood, let alone someone else’s! But staying calm and being prepared with a well-established first aid kit can make a difficult and painful experience a lot less traumatic. Remember that emergency help is only a phone call away, and take any incident of heavy bleeding seriously.
Cerebral hemorrhage -
Postoperative examination of a glial brain tumor
Cerebral hemorrhage
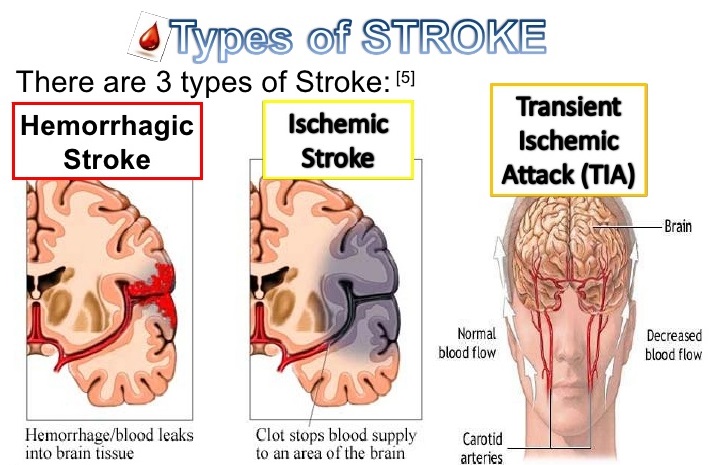
Cerebral hemorrhage is expressed by bleeding with blood entering the brain tissue (intracerebral hemorrhage) or into the space between the outer meninges and the skull (subarachnoid, subdural epidural hemorrhages). All these bleedings can occur both as a result of traumatic brain injuries, and due to any other causes associated with diseases such as systemic hypertension and other systemic diseases of the body.
All these bleedings can occur both as a result of traumatic brain injuries, and due to any other causes associated with diseases such as systemic hypertension and other systemic diseases of the body.
Intracerebral hemorrhage
Intracerebral hemorrhage occurs as a result of rupture of the walls of small blood vessels supplying the brain, especially in certain areas of the brain, in connection with which the blood from the burst vessels enters the brain and destroys brain tissue. Every year, intracerebral hemorrhage occurs in approximately 12-15 patients out of 100,000 people. Moreover, this figure is significantly higher in patients over the age of 40 years. The ratio of men and women who have intracerebral hemorrhage is 1:1.67.
Risk factors include hypertension, amyloid angiopathy, trauma, alcohol use, and smoking. In addition, intracerebral effusion can also be caused by the use of drugs such as aspirin, non-steroidal anti-inflammatory drugs and thrombolytic drugs.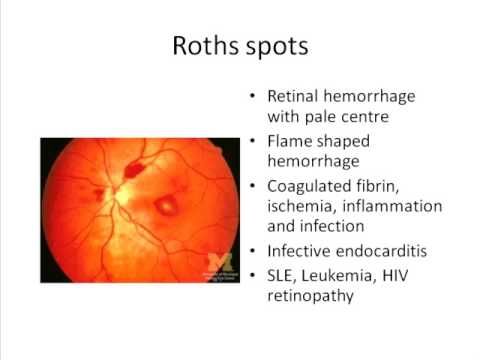 With age, the vessels of the brain are subject to wear and tear and lose their elastic properties. As a result, the walls of such vessels lose their elasticity. Loss of elasticity and wear of the walls of blood vessels caused by diseases such as amyloid angiopathy and hypertension contribute to rupture of blood vessels and leakage of blood into the brain tissue. This creates a buildup and formation of blood clots that damage the brain tissue. At the same time, such a manifestation, due to the formation and accumulation of such blood clots, disrupting the circulatory system, contributes to the development of ischemia in the brain.
With age, the vessels of the brain are subject to wear and tear and lose their elastic properties. As a result, the walls of such vessels lose their elasticity. Loss of elasticity and wear of the walls of blood vessels caused by diseases such as amyloid angiopathy and hypertension contribute to rupture of blood vessels and leakage of blood into the brain tissue. This creates a buildup and formation of blood clots that damage the brain tissue. At the same time, such a manifestation, due to the formation and accumulation of such blood clots, disrupting the circulatory system, contributes to the development of ischemia in the brain.
Clinical symptoms are most often manifested as unilateral weakening of muscle tone, headache and changes in consciousness. In addition, slurred speech, convulsions, nausea and vomiting may occur.
In order to establish a preliminary diagnosis, it is necessary to obtain detailed information regarding the patient's medical history. When making a diagnosis, it is necessary to analyze radiological results and imaging images obtained during computed tomography and magnetic resonance imaging. When choosing a diagnostic method, preference is given to computed tomography because of the possibility of an accurate diagnosis in a short time.
When choosing a diagnostic method, preference is given to computed tomography because of the possibility of an accurate diagnosis in a short time.
In order to protect the vital functions of the patient in the treatment of intracerebral hemorrhage, it is first necessary to provide support for the respiratory and cardiovascular systems. After analyzing and determining the amount of bleeding and its localization in the brain, a general assessment of the patient's neurological picture is performed. A decision is then made as to which treatment should be given to the patient: surgery or medication. During surgery, the blood mass accumulated in the brain tissue is removed, as well as bleeding stops. With drug treatment, the patient is prescribed drugs to reduce intracranial pressure and reduce swelling in the area of bleeding. In addition, antiepileptic drugs may be prescribed to the patient to prevent the possible occurrence of seizures.
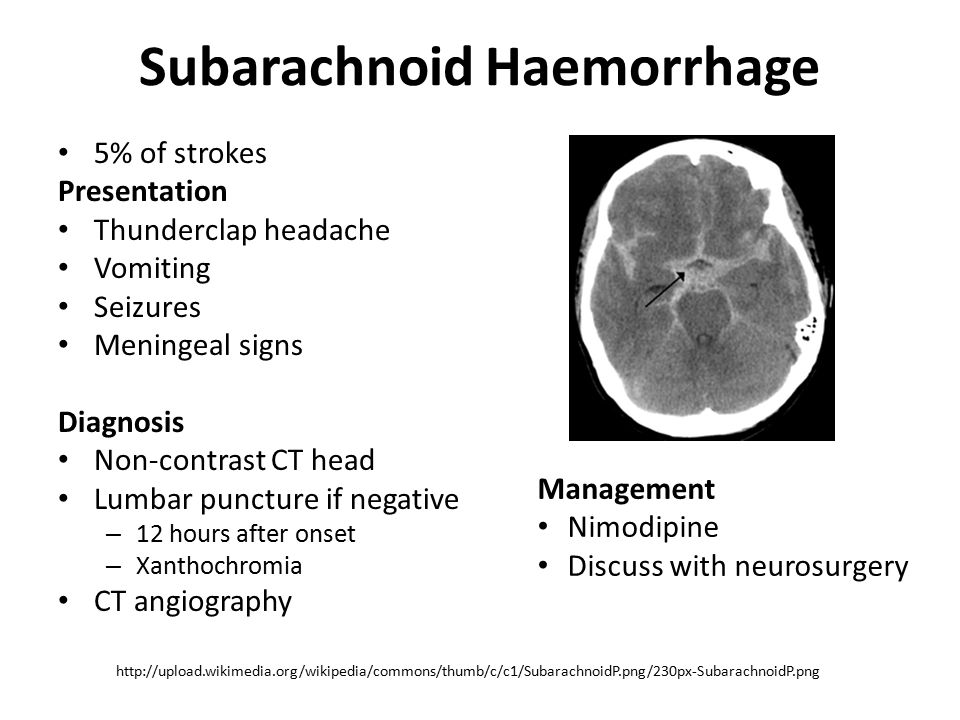
Subarachnoid hemorrhage
Subarachnoid hemorrhage is a hemorrhage into the subarachnoid space or cavity, which is located between the arachnoid and pia mater.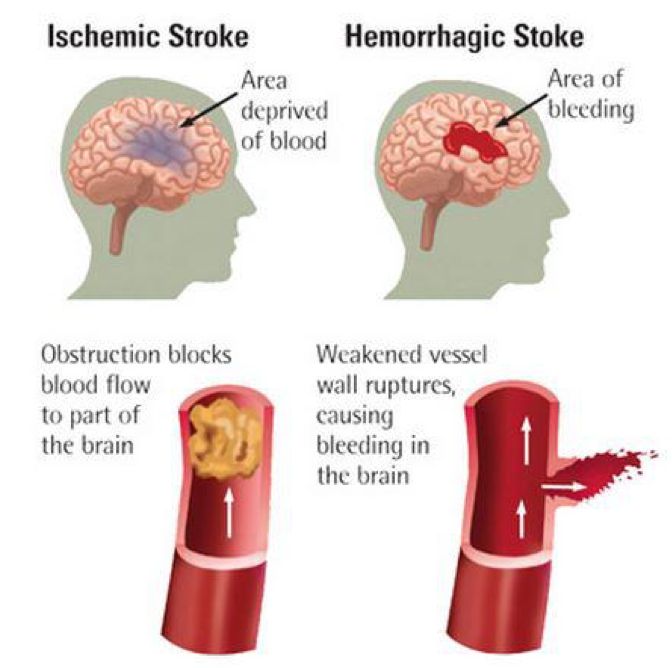 It occurs in 10-16 people per 100,000 people. Risk factors include hereditary diseases, smoking, alcohol use, hypertension, and the use of drugs such as oral contraceptives, cocaine, and amphetamines. Subarachnoid hemorrhage can occur spontaneously, usually due to rupture of an arterial aneurysm, or as a result of traumatic brain injury, hypertension, atherosclerosis, arteriovenous malformations, brain tumors, bleeding disorders, encephalitis, meningitis, meningoencephalitis, and also due to complications associated with anticoagulant therapy or as a result of any other unknown causes.
It occurs in 10-16 people per 100,000 people. Risk factors include hereditary diseases, smoking, alcohol use, hypertension, and the use of drugs such as oral contraceptives, cocaine, and amphetamines. Subarachnoid hemorrhage can occur spontaneously, usually due to rupture of an arterial aneurysm, or as a result of traumatic brain injury, hypertension, atherosclerosis, arteriovenous malformations, brain tumors, bleeding disorders, encephalitis, meningitis, meningoencephalitis, and also due to complications associated with anticoagulant therapy or as a result of any other unknown causes.
The most common symptoms most often manifest as a very intense headache and stiff neck are. In addition, patients may experience nausea, vomiting, dizziness, double vision, convulsions, clouding of consciousness, which accompany the symptoms that occur with intracerebral hemorrhage. The diagnosis is made after an examination using computed tomography, due to which the presence of hemorrhage in the brain tissue is detected in the fastest way. Once bleeding is determined, angiography is required to visualize cerebral vessels.
Once bleeding is determined, angiography is required to visualize cerebral vessels.
If an aneurysm is detected during angiography, then, depending on the area of its localization and its characteristic properties, it must be removed using surgical or endovascular methods, while the walls of the vessel are strengthened with a special material. Despite all the developments in modern medicine, 25-30% of patients with subarachnoid hemorrhage die before they are admitted to the hospital, while 30-50% of the remaining patients are completely cured.
Epidural hematoma
Epidural hematoma is an accumulation of blood that occurs between the inner surface of the skull and the dura mater as a result of traumatic injury to the bones of the skull. The cause of such a hematoma is rupture and damage to the blood vessels of the dura mater, which, as a rule, are the result of trauma or fracture of the bones of the skull. Epidural hematoma accounts for 0.2-0.6% of all cases of brain injury. Clinically, epidural hematoma manifests itself in three ways: first of all, it is a lucid interval - a temporary improvement in the patient's condition after a traumatic brain injury, followed by a sharp deterioration. In the second case, consciousness is completely closed and there is no improvement in the state, in the third case, clouding of consciousness occurs. An accurate diagnosis is confirmed by computed tomography, while magnetic resonance imaging can also be used for diagnosis. But due to the fact that computed tomography makes it possible to obtain results that are of vital importance in a faster way, and it is more preferable in the diagnosis of this type of hematoma.
Clinically, epidural hematoma manifests itself in three ways: first of all, it is a lucid interval - a temporary improvement in the patient's condition after a traumatic brain injury, followed by a sharp deterioration. In the second case, consciousness is completely closed and there is no improvement in the state, in the third case, clouding of consciousness occurs. An accurate diagnosis is confirmed by computed tomography, while magnetic resonance imaging can also be used for diagnosis. But due to the fact that computed tomography makes it possible to obtain results that are of vital importance in a faster way, and it is more preferable in the diagnosis of this type of hematoma.
Treatment of an epidural hematoma involves monitoring the amount of blood accumulated in the area between the inner surface of the skull and the dura mater and the amount of pressure it exerts on the brain tissue, followed by surgery. If there is a small amount of accumulated blood, the patient is monitored very carefully and his health condition is constantly monitored.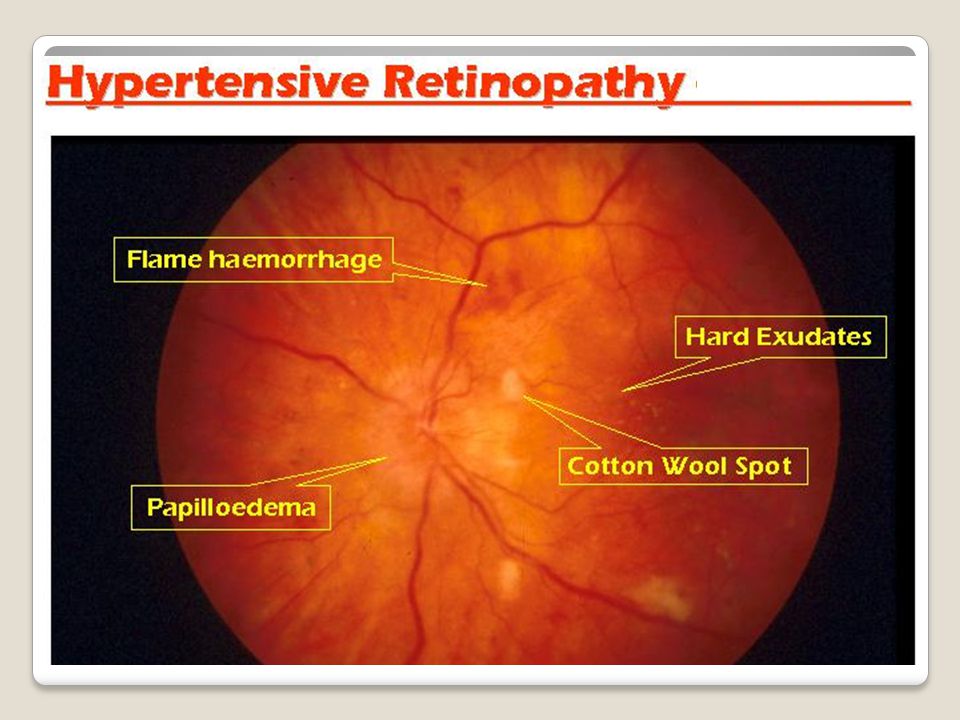 If, however, a decision is made on the need for surgical intervention, it should be implemented as soon as possible. During a surgical intervention, the blood accumulated in the brain tissue is drained and, by determining the source of occurrence, stop the bleeding. The outcome of surgical intervention brings quite brilliant results. Good results are achieved at 55-89% after surgical treatment, while the mortality rate ranges from 5-29%.
If, however, a decision is made on the need for surgical intervention, it should be implemented as soon as possible. During a surgical intervention, the blood accumulated in the brain tissue is drained and, by determining the source of occurrence, stop the bleeding. The outcome of surgical intervention brings quite brilliant results. Good results are achieved at 55-89% after surgical treatment, while the mortality rate ranges from 5-29%.
Subdural hematoma
In patients who have suffered a head injury, in 8-57% of cases there is a subdural hematoma. It is an accumulation of blood that occurs between the inner surface of the skull and the dura mater as a result of traumatic injury to the bones of the skull. In 50% of cases, subdural hematoma is accompanied by various other pathologies of the brain. In general, patients present with severe neurological disorders and in 50% of cases these patients are unconscious. The best ways to diagnose epidural hematoma are computed tomography and magnetic resonance imaging.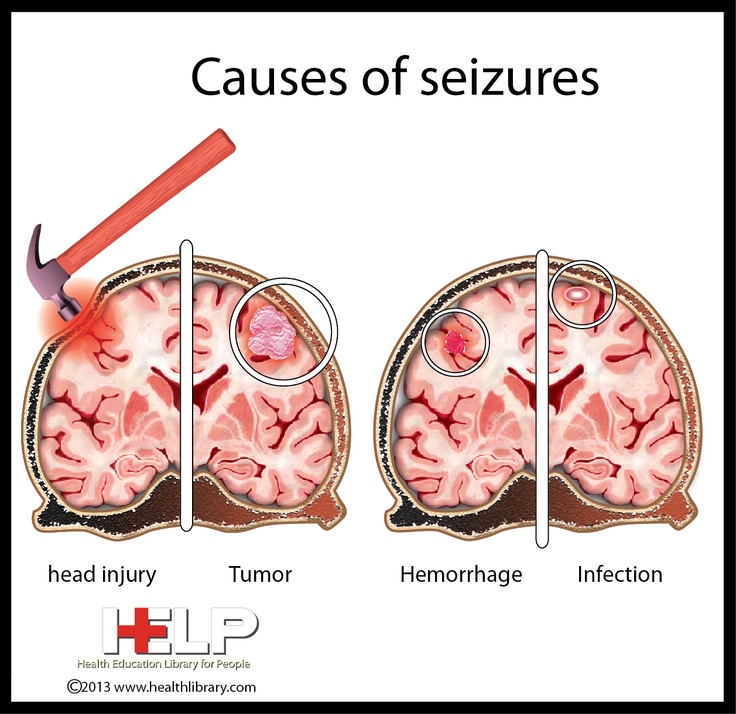
Surgery is used to treat hematomas that cause neurological damage and put pressure on surrounding tissues. During surgical intervention, the blood accumulated in the brain tissue is removed and the source of the occurrence is determined, and the bleeding is stopped. The mortality rate ranges from 42-90%, while this figure is significantly higher than with epidural hematoma.
Cerebral hemorrhage ▷ Symptoms, therapy and rehabilitation
What is a cerebral hemorrhage?
"Cerebral hemorrhage" is a medically colloquial term for bleeding inside the skull (intracranial), in an area of the brain (intracerebral), and also in the area of the meninges (extracerebral). As a rule, they talk about cerebral hemorrhage when an intracerebral hemorrhage occurs in the brain. Every year in Germany, intracerebral hemorrhage occurs in about 10-12 people out of every 100,000. Subarachnoid hemorrhage, epidural and subdural hematoma as an intracranial extracerebral form of hemorrhage should be distinguished from intracerebral hemorrhage.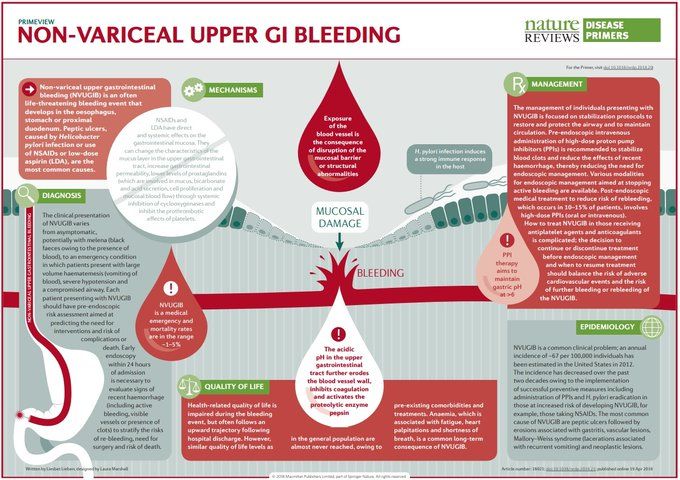 In ischemic stroke, which causes symptoms similar to intracerebral hemorrhage, ischemic damage (lack of oxygen supply) leads to destruction of brain tissue. In an intracerebral hemorrhage ("hemorrhagic stroke"), brain tissue is damaged as a result of the hemorrhage. 10-17% of strokes are caused by intracerebral hemorrhage.
In ischemic stroke, which causes symptoms similar to intracerebral hemorrhage, ischemic damage (lack of oxygen supply) leads to destruction of brain tissue. In an intracerebral hemorrhage ("hemorrhagic stroke"), brain tissue is damaged as a result of the hemorrhage. 10-17% of strokes are caused by intracerebral hemorrhage.
Because the brain is inside the cranial bone, it cannot expand further as volume increases. With bleeding in the brain, its volume increases, and with it the pressure on the brain tissue. The increased pressure on the nerve cells in the brain damages and destroys them.
What causes a brain hemorrhage?
Long-term high blood pressure, obesity, dyslipidemia and tobacco use lead to certain vascular changes (atherosclerosis) in the long term. Both aneurysms and thrombi can form at the altered sites, which plays a crucial role in the pathophysiology of strokes and other cardiovascular diseases. Other causes of stroke are tumors, bleeding disorders, or amyloid angiopathy (abnormal deposits of protein in blood vessels in the brain).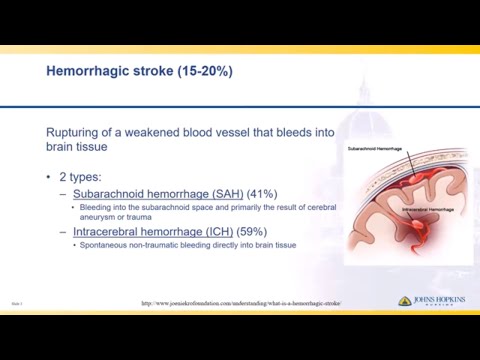 Hemorrhagic (bloody) strokes also occur as a result of severe traumatic brain injury. Currently, more and more patients, especially the elderly, are taking anticoagulant drugs, which can play an important role in the development of cerebral hemorrhage, so they should be prescribed after a rigorous study of the indications and a careful consideration of the risk-benefit ratio.
Hemorrhagic (bloody) strokes also occur as a result of severe traumatic brain injury. Currently, more and more patients, especially the elderly, are taking anticoagulant drugs, which can play an important role in the development of cerebral hemorrhage, so they should be prescribed after a rigorous study of the indications and a careful consideration of the risk-benefit ratio.
What are the symptoms of a cerebral hemorrhage?
Intra- and extracerebral hemorrhages often have similar symptoms. Patients suddenly develop speech and movement disorders, often with an emphasis on one side, and clouding of consciousness up to coma can also be observed. Most patients also complain of nausea, vomiting and headaches.
Intracerebral hemorrhage: chances of survival and treatment
An intracerebral hemorrhage is a life-threatening emergency that requires prompt action. Since bleeding every minute causes further damage to the brain due to increasing pressure, quick action is needed to transport the victim to the hospital as quickly as possible.
Neurosurgical intervention may be required to reduce the pressure on the brain caused by bleeding and stop the bleeding.
Since the symptoms of intracerebral hemorrhage cannot be distinguished from those of ischemic stroke, and the treatments are nevertheless opposite, performing an imaging procedure ( CT or MRI ) is crucial for an accurate and, above all, fast diagnosis. As a rule, computed tomography (CT) is performed due to the speed of obtaining results.
Depending on the specific case, emergency therapy includes both non-operative and neurosurgical methods of treatment. The non-surgical method of treatment mainly involves precise control of blood pressure. Surgical, neurosurgical intervention to reduce intracranial pressure is necessary, first of all, in violation of consciousness or an increase in the degree of hemorrhage. After an intracerebral hemorrhage, the risk of epileptic seizures increases due to brain damage.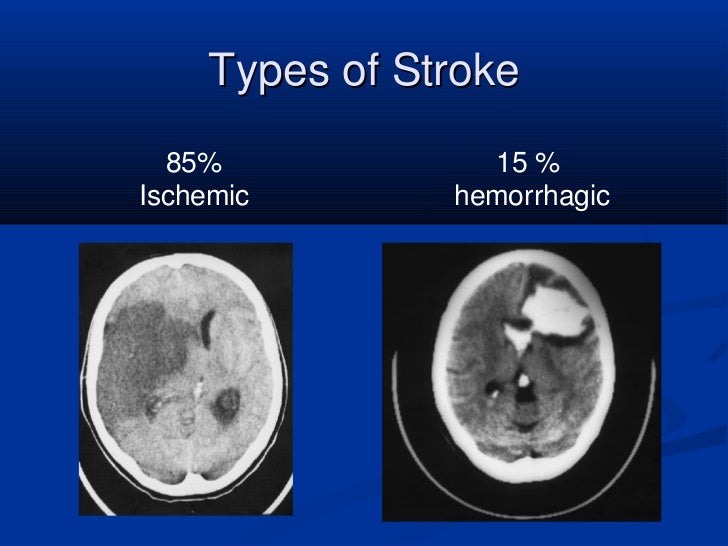 One of the main complications after a cerebral hemorrhage is postoperative bleeding, which occurs in almost 40% of victims in the first 24 hours after a hemorrhage.
One of the main complications after a cerebral hemorrhage is postoperative bleeding, which occurs in almost 40% of victims in the first 24 hours after a hemorrhage.
Survival of intracerebral hemorrhage depends mainly on the size and location of the injury. So, with a hemorrhage of more than 60 ml of blood in the case of deep-seated hemorrhages, about 93% of patients die, while with a hemorrhage of less than 30 ml of blood in a comparable place, only 23% die. In general, studies show that 35-52% of patients die within the first month after a cerebral hemorrhage and only 20% of patients no longer need outside help 6 months after a hemorrhage. Most patients experience long-term damage during the course of their illness, such as motor, language, or cognitive impairment.
What will happen next? - Rehabilitation after cerebral hemorrhage
If the condition of the patients has stabilized, then immediately after the acute phase of the disease, rehabilitation measures begin, often carried out in parallel with intensive medical therapy.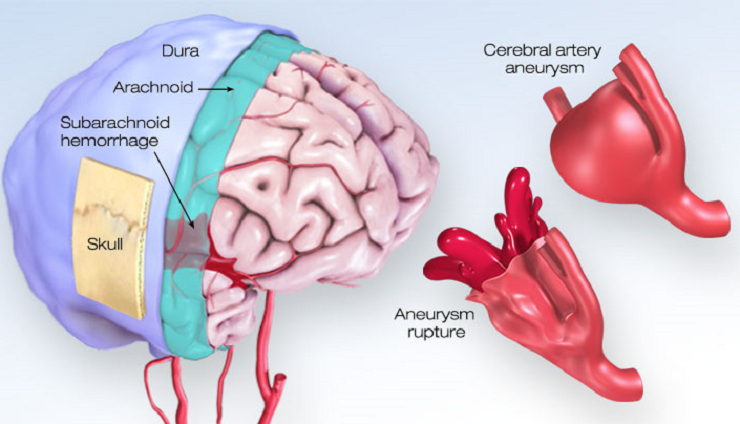 Since the human brain is able to restore lost functions and compensate for damage to brain structures with healthy nerve cells, careful and early care by experienced neurologists is important.
Since the human brain is able to restore lost functions and compensate for damage to brain structures with healthy nerve cells, careful and early care by experienced neurologists is important.
What is done during rehabilitation after a brain hemorrhage?
During the course neurological rehabilitation patients receive support in the fight against motor and speech, as well as cognitive and other disorders. As a rule, treating therapists (doctors, physiotherapists, occupational therapists, speech therapists, psychotherapists, etc.) work in close cooperation as part of an interdisciplinary team in order to achieve the best result in working with patients. Since the limitations of patients after intracerebral hemorrhage can be quite different, the treatment plan is always developed taking into account the individual characteristics of the patient.
Depending on the degree of neurological limitations, rehabilitation care may vary in duration.