What is a congenital
What is a congenital disorder?
What is a congenital disorder? | Pregnancy Birth and Baby beginning of content5-minute read
Listen
What is a congenital disorder?
A congenital disorder is a condition that is present from birth. Congenital disorders can be inherited or caused by environmental factors. Their impact on a child’s health and development isn’t always severe, and sometimes it can be quite mild. However, a child with a congenital disorder may experience a disability or health problems throughout life.
It’s natural to be concerned about congenital disorders if you’re pregnant or planning a pregnancy, especially if your family has a history of a particular disorder. It’s possible to test for some, but not all disorders during pregnancy, and there are also things you can do to reduce the chances of your baby being born with a congenital disorder.
What are the most common congenital disorders?
Some common congenital disorders are:
- cleft lip and cleft palate — usually diagnosed during routine scans in pregnancy
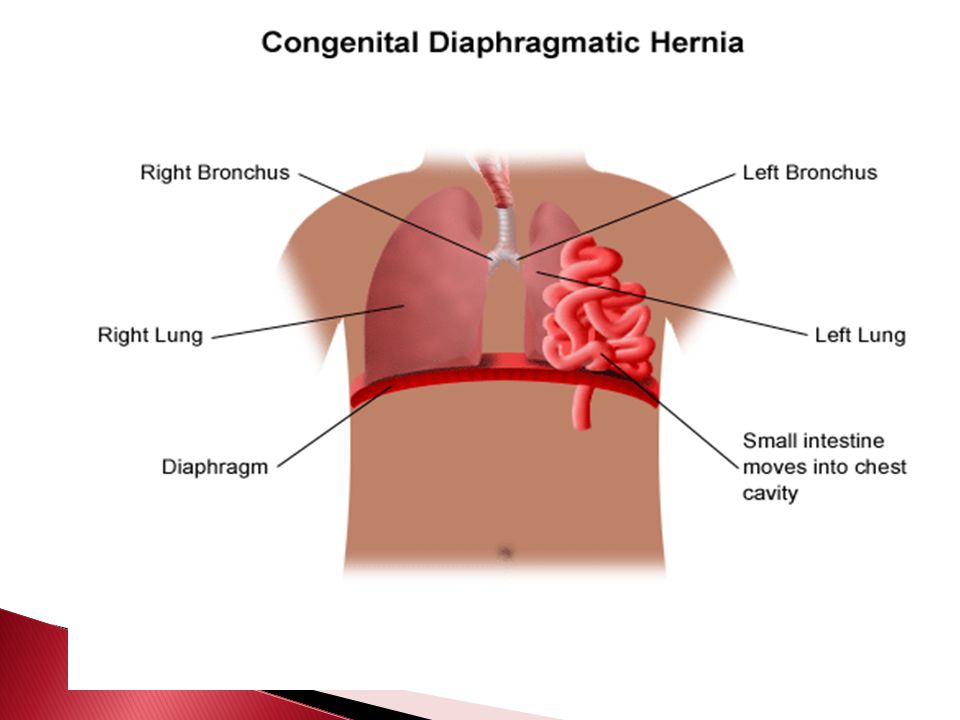
- congenital heart disease — including a hole in the heart, a valve problem or a problem with the blood vessels. These are usually diagnosed during routine scans in pregnancy or during newborn screening.
- cerebral palsy — usually diagnosed in the first few years of life
- Fragile X syndrome — may be diagnosed through genetic testing during pregnancy or in the first few years of life
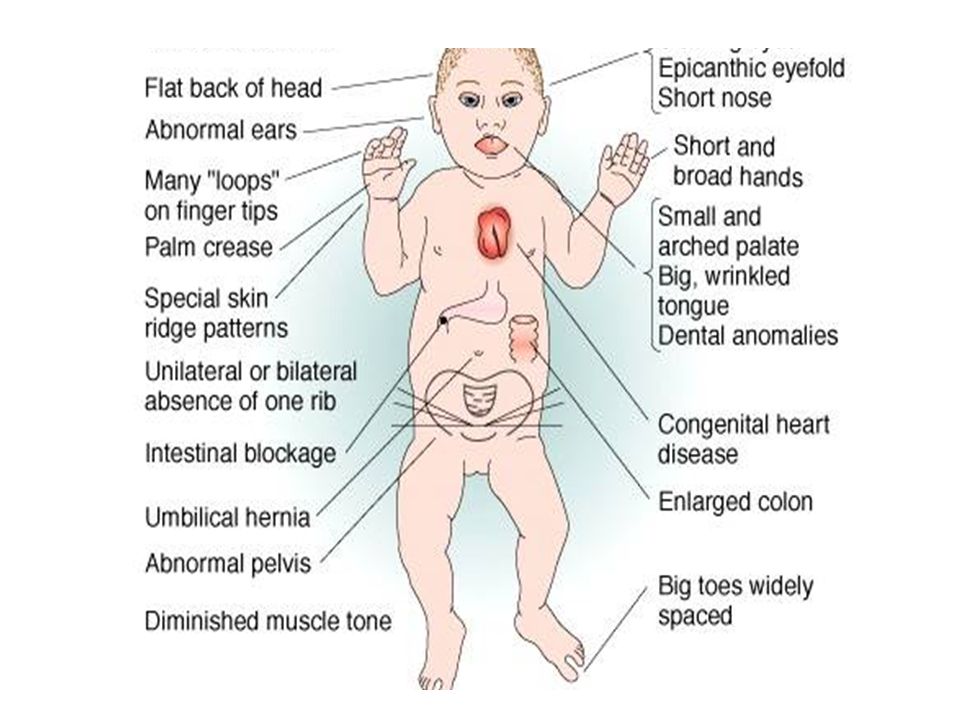
- Down syndrome (Trisomy 21) — usually diagnosed through genetic during pregnancy
- spina bifida — usually diagnosed during routine scans in pregnancy
- cystic fibrosis — usually diagnosed during newborn screening
What tests for congenital disorders are available in pregnancy?
Testing for some congenital disorders, such as Down syndrome, can be performed using a blood test from 10 weeks of pregnancy onwards.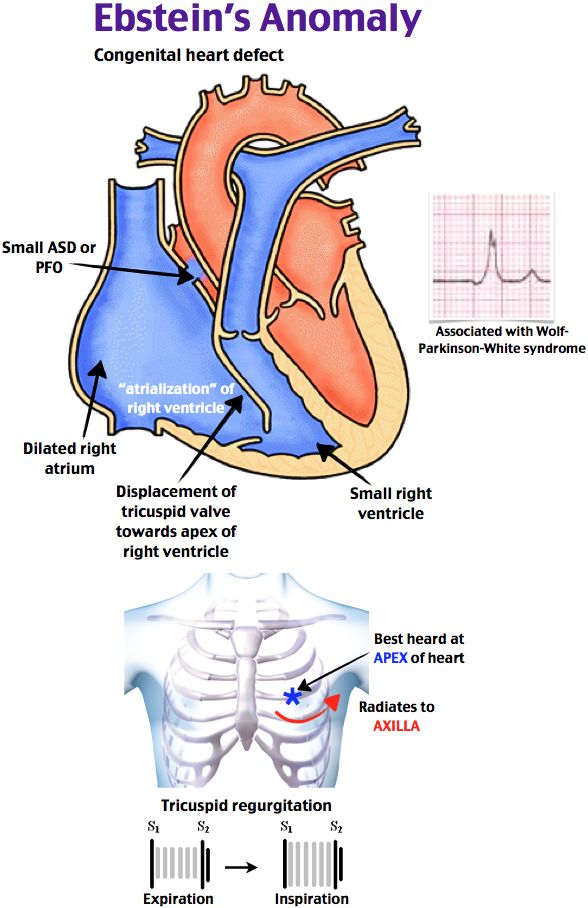 Although many parents choose to have tests during pregnancy, it is not compulsory. Some parents choose not to have tests.
Although many parents choose to have tests during pregnancy, it is not compulsory. Some parents choose not to have tests.
Screening tests are designed to identify babies who may be at increased risk of a congenital disorder. If a screening test does not rule out your baby having a congenital disorder, the next step is to have a diagnostic test.
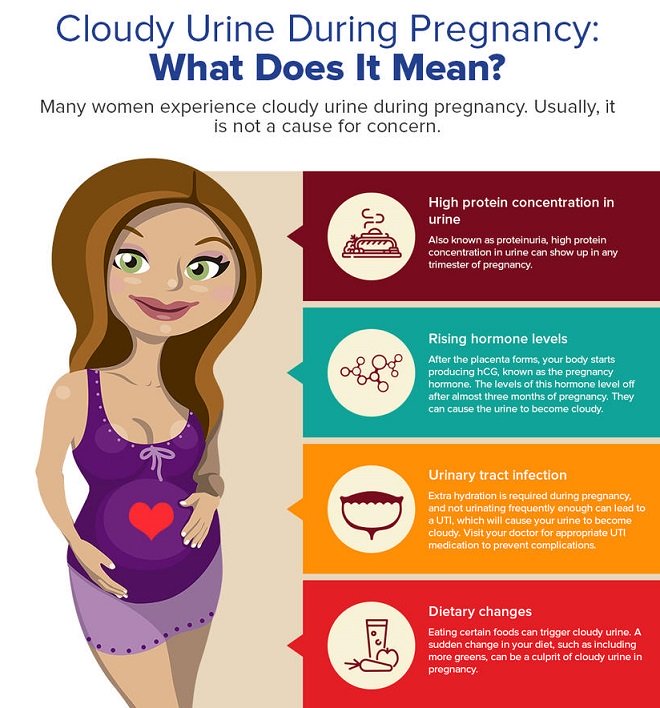
Diagnostic tests, such as ultrasound scans, blood tests and sometimes urine tests, aim to identify babies who have a congenital disorder and to find out what that disorder is.
However, it is not possible to test for all congenital disorders during pregnancy, and testing is not perfect.
Chorionic villus sampling (CVS)
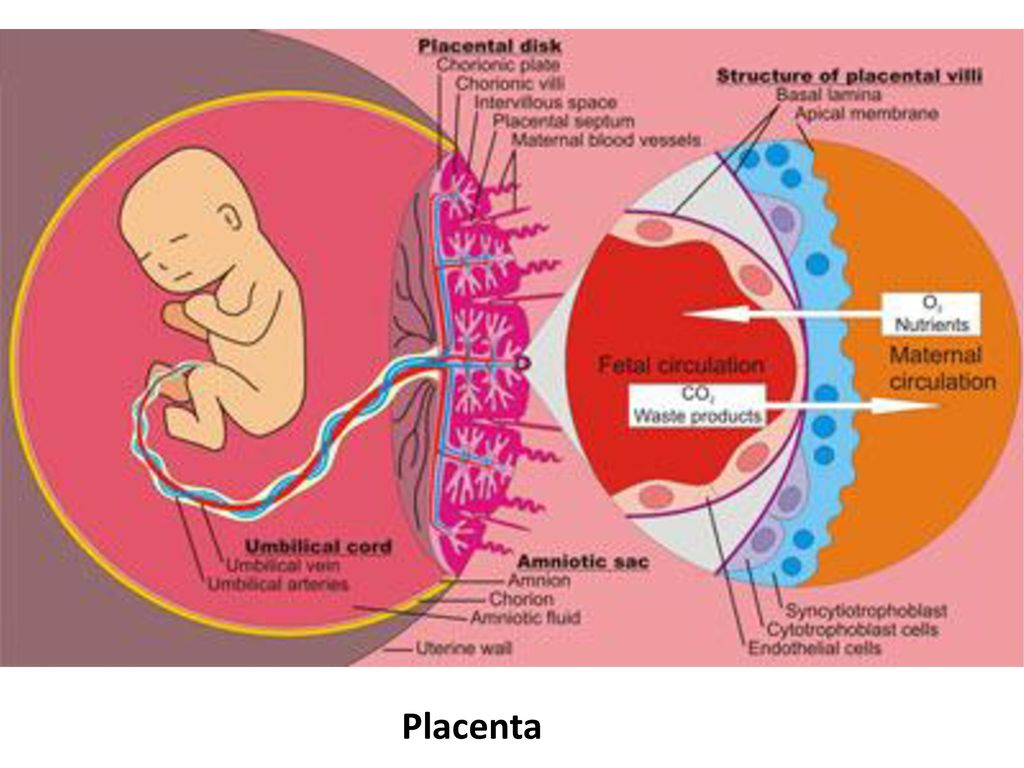
Chorionic villus sampling, or CVS, is usually performed between 10 and 13 weeks of pregnancy if screening tests show your baby may have a congenital disorder. CVS can be used to diagnose babies with Down syndrome or other genetic conditions. You would be given a local anaesthetic and a doctor would use a needle to collect a small sample of cells from your placenta, which is then sent for testing.
Amniocentesis
This test is done after 15 weeks of pregnancy and may be done instead of, or as well as CVS. It can provide a definite answer as to whether your baby has Down syndrome or another congenital disorder.
Amniocentesis involves taking a small amount of fluid from around your baby, using a needle and after a local anaesthetic, which is then sent for testing.
There is a very small risk of miscarriage with both CVS and amniocentesis.
Can congenital disorders be prevented?
If you have a personal or family history of certain congenital disorders, you can have genetic tests before you become pregnant. You may wish to meet with a genetic counsellor to discuss your family history, the likelihood your baby will have any congenital disorders, and possibly to arrange to have genetic testing.
If you are having in vitro fertilisation (IVF) treatment, your embryo can be tested at 2 to 4 days old, before it is implanted into your uterus.
Other things you can do to try to prevent congenital disorders include:
- eating a healthy diet with enough vitamins and minerals, in particular folic acid, during the reproductive years
- taking folic acid supplements before you become pregnant and for the first trimester of pregnancy
- avoiding alcohol, smoking and other drugs because these can harm the fetus
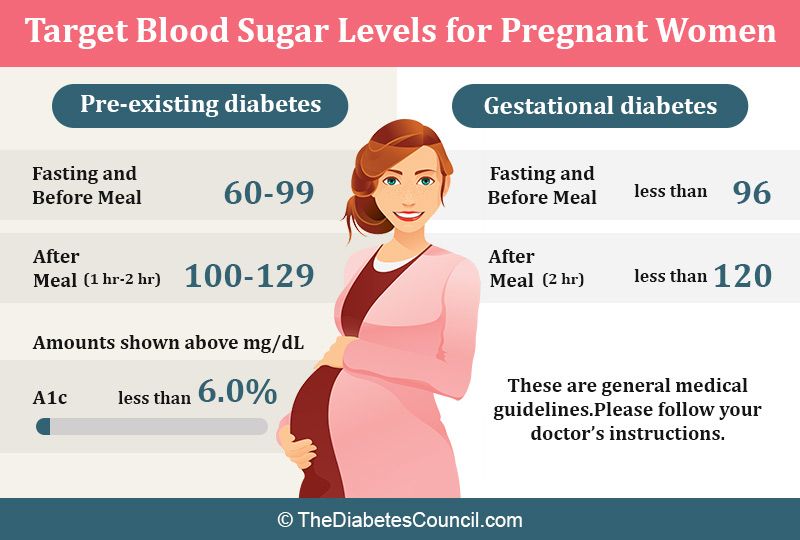
- controlling diabetes and gestational diabetes
- avoiding exposure to chemicals in your environment, such as pesticides or lead
- being vaccinated, especially against rubella
Newborn testing and assessment
A paediatrician and other health professionals examine your baby in the first few days of life to check for hearing problems, heart conditions, and blood, metabolism and hormone disorders. This is called newborn screening. Early detection of such problems can often prevent them from becoming more serious physical, intellectual, visual or hearing disabilities.
This is called newborn screening. Early detection of such problems can often prevent them from becoming more serious physical, intellectual, visual or hearing disabilities.
Sources:
Raising Children Network (Tests in pregnancy), Raising Children Network (Newborn screening), Raising Children Network (Antenatal tests: chromosomal abnormalities and other conditions), Raising Children Network (Congenital heart disease), World Health Organization (Congenital anomalies), The Royal Children's Hospital Melbourne (Cleft lip and palate), Cerebral Palsy Alliance (Signs and symptoms of Cerebral Palsy), Fragile X Association of Australia (Testing and screening for Fragile X), NSW Health Centre for Genetics Education (Screening tests during pregnancy), Sydney Children's Hospitals Network (Spina bifida)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: June 2021
Back To Top
Related pages
- What is a childhood disability?
- Your feelings about your child's disability
- Early childhood intervention
- Disability and parenting support
- Disability rights for children
Need more information?
Fragile X syndrome
People with Fragile X syndrome have intellectual disability, behavioural and learning challenges as well as certain physical characteristics.
Read more on Pregnancy, Birth & Baby website
Fragile X syndrome in children | Raising Children Network
Fragile X syndrome causes intellectual disability and other challenges.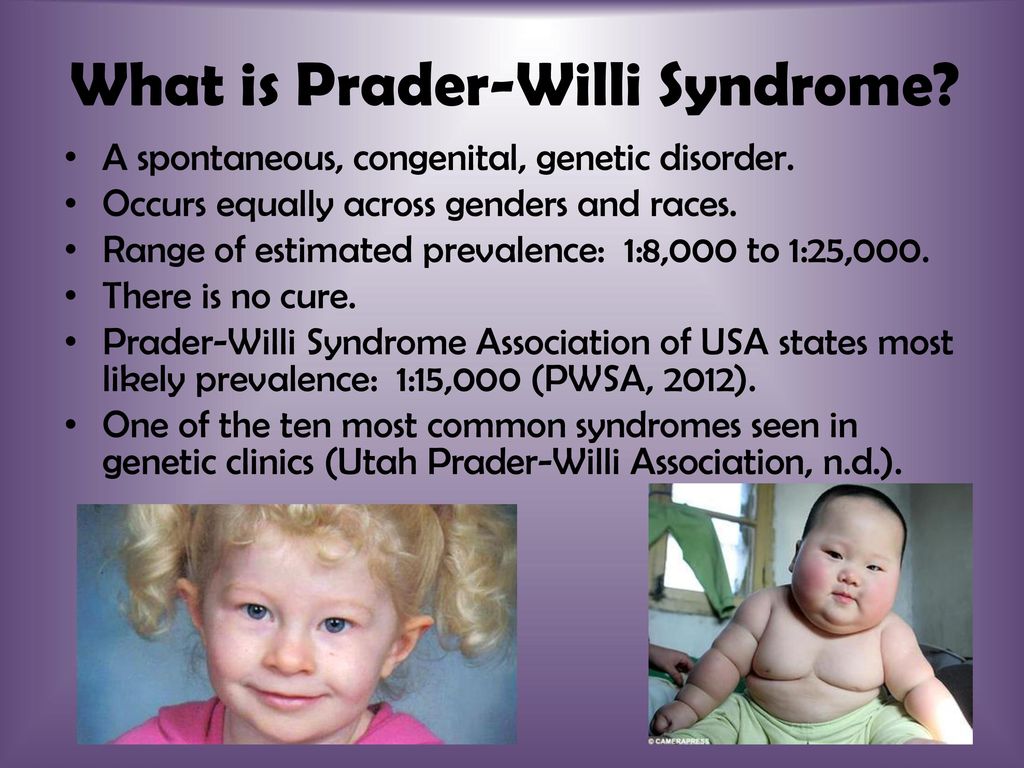 Early intervention and support helps children with Fragile X explore their abilities.
Early intervention and support helps children with Fragile X explore their abilities.
Read more on raisingchildren.net.au website
Fragile X syndrome - Better Health Channel
The facts about fragile X syndrome are complicated, and parents and family members are invited to ask their doctor to refer them to a genetics clinic.
Read more on Better Health Channel website
Congenital heart disease: 0-18 years | Raising Children Network
Children with congenital heart disease are born with heart defects. Many heart defects don’t need treatment, and most children go on to live active, healthy lives.
Read more on raisingchildren.net.au website
Cyanotic Congenital Heart Disease (CCHD) | HeartKids
Cyanotic congenital heart disease (CCHD) refers to birth defects that result in a low blood oxygen level & causes a bluish skin colour.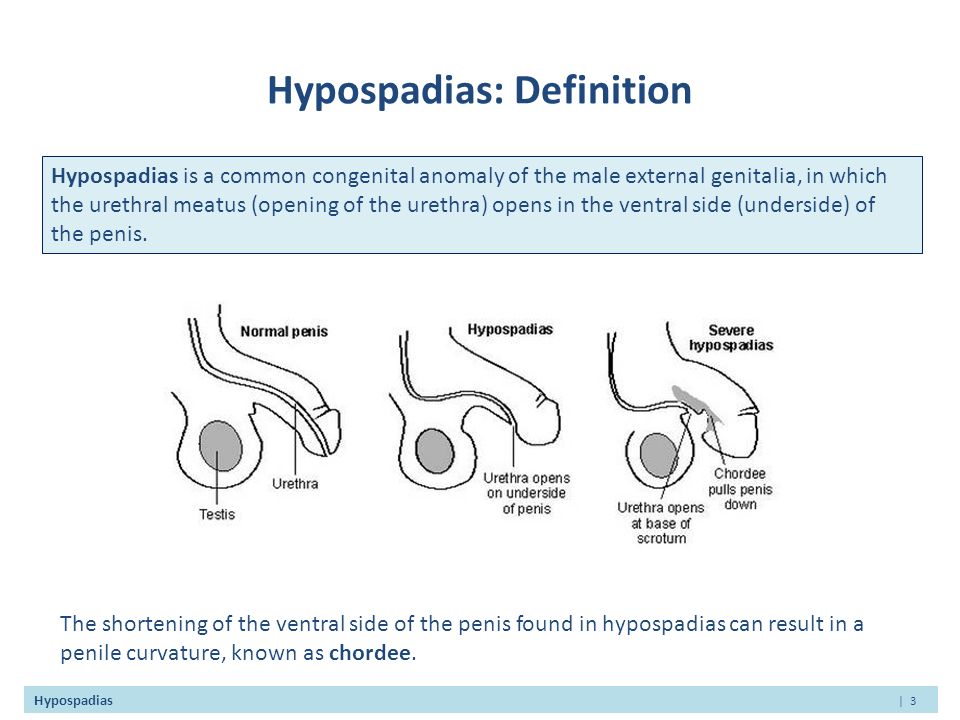 Learn more about it.
Learn more about it.
Read more on HeartKids website
Heart abnormality birth defects - Better Health Channel
Some congenital heart defects are mild and cause no significant disturbance to the way the heart functions.
Read more on Better Health Channel website
What is Down syndrome?
Down syndrome is a genetic disorder characterised by mental and developmental impairments.
Read more on Pregnancy, Birth & Baby website
Caring for a child with Down syndrome
When caring for a child with Down syndrome, you might face some challenges different to other parents.
Read more on Pregnancy, Birth & Baby website
Screening for Down syndrome
Down syndrome is a chromosomal disorder that affects 1 in 1,00 babies.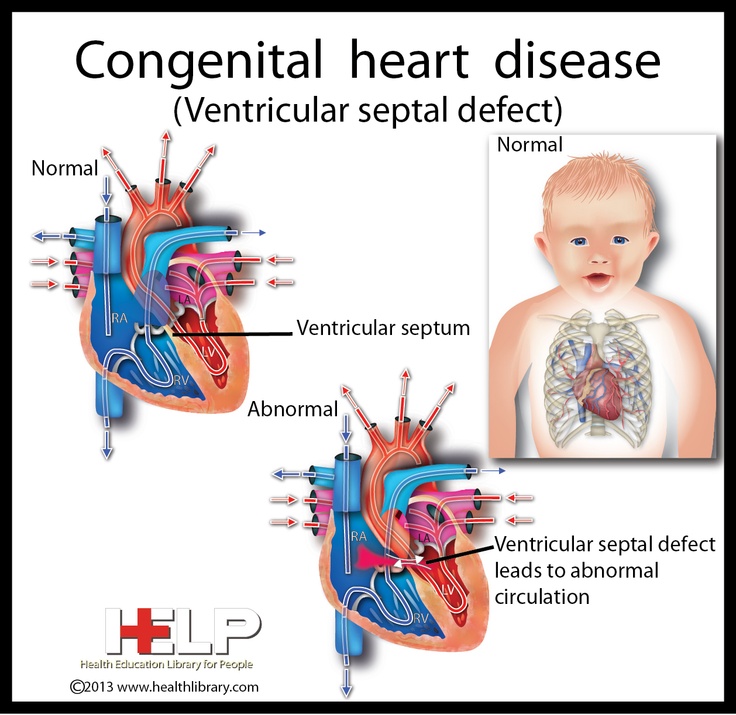 Find out about the screening and diagnostic tests that can detect the condition.
Find out about the screening and diagnostic tests that can detect the condition.
Read more on Pregnancy, Birth & Baby website
Maternal screening - Pathology Tests Explained
Why and when to get tested for maternal screening
Read more on Pathology Tests Explained website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.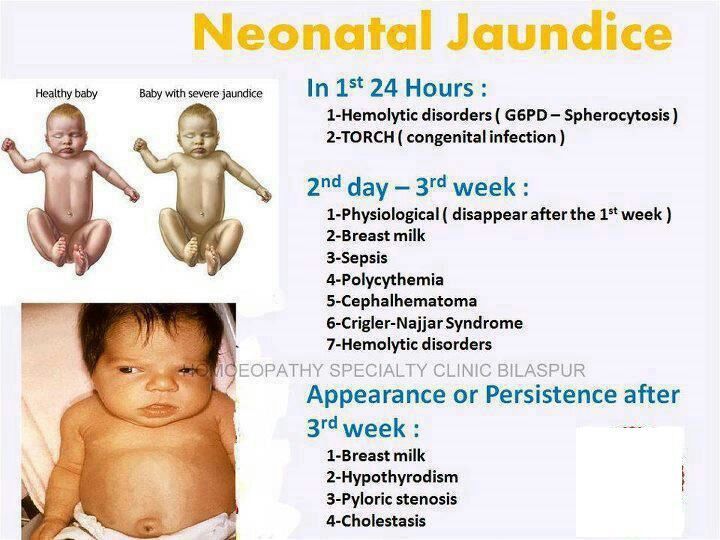
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care.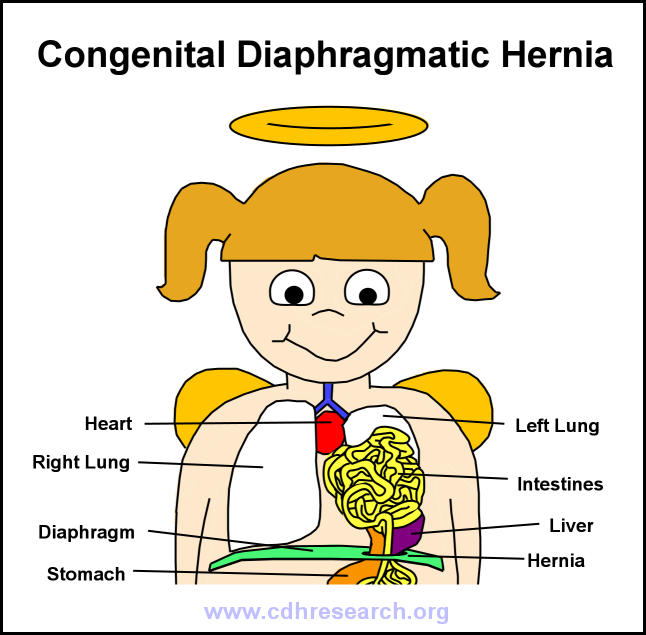 If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Congenital disorders
Congenital disorders- All topics »
- A
- B
- C
- D
- E
- F
- G
- H
- I
- J
- K
- L
- M
- N
- O
- P
- Q
- R
- S
- T
- U
- V
- W
- X
- Y
- Z
- Resources »
- Fact sheets
- Facts in pictures
- Multimedia
- Publications
- Questions & answers
- Tools and toolkits
- Popular »
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Monkeypox
- All countries »
- A
- B
- C
- D
- E
- F
- G
- H
- I
- J
- K
- L
- M
- N
- O
- P
- Q
- R
- S
- T
- U
- V
- W
- X
- Y
- Z
- Regions »
- Africa
- Americas
- South-East Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- WHO in countries »
- Statistics
- Cooperation strategies
- Ukraine emergency
- All news »
- News releases
- Statements
- Campaigns
- Commentaries
- Events
- Feature stories
- Speeches
- Spotlights
- Newsletters
- Photo library
- Media distribution list
- Headlines »
- Focus on »
- Afghanistan crisis
- COVID-19 pandemic
- Northern Ethiopia crisis
- Syria crisis
- Ukraine emergency
- Monkeypox outbreak
- Greater Horn of Africa crisis
- Latest »
- Disease Outbreak News
- Travel advice
- Situation reports
- Weekly Epidemiological Record
- WHO in emergencies »
- Surveillance
- Research
- Funding
- Partners
- Operations
- Independent Oversight and Advisory Committee
- WHO's Health Emergency Appeal 2023
- Data at WHO »
- Global Health Estimates
- Health SDGs
- Mortality Database
- Data collections
- Dashboards »
- COVID-19 Dashboard
- Triple Billion Dashboard
- Health Inequality Monitor
- Highlights »
- Global Health Observatory
- SCORE
- Insights and visualizations
- Data collection tools
- Reports »
- World Health Statistics 2022
- COVID excess deaths
- DDI IN FOCUS: 2022
- About WHO »
- People
- Teams
- Structure
- Partnerships and collaboration
- Collaborating centres
- Networks, committees and advisory groups
- Transformation
- Our Work »
- General Programme of Work
- WHO Academy
- Activities
- Initiatives
- Funding »
- Investment case
- WHO Foundation
- Accountability »
- Audit
- Programme Budget
- Financial statements
- Programme Budget Portal
- Results Report
- Governance »
- World Health Assembly
- Executive Board
- Election of Director-General
- Governing Bodies website
- Member States Portal
- Home/
- Health topics/
- Congenital disorders
UNICEF/Noorani
Newborn baby in Timor-Leste
© Credits
Fact sheets
Questions and answers
Guidelines
Databases and tools
Resolutions and decisions
Technical work
- Newborn Health Unit
- Maternal, Newborn, Child and Adolescent Health and Ageing
- Nutrition and Food Safety
- Sensory Functions, Disability and Rehabilitation
- Sexual and Reproductive Health
Our work
News
All →Publications
All →A wide range of causes of congenital anomalies means that a portfolio of prevention approaches is needed including prevention of sexually transmitted infections,. ..
..
Congenital anomalies, also known as birth defects, are structural or functional abnormalities, including metabolic disorders, that are present from birth....
Survive and thrive: transforming care for every small and sick newborn maps out a pathway towards 2030. It is built upon epidemiology, historical trends,...
Feature stories
Related health topics
Congenital dyskeratosis. What is Dyskeratosis Congenita?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Congenital dyskeratosis is an extremely rare genetic disease, the classic clinical picture of which includes local hyperpigmentation of the skin, degeneration of the nail plates, and leukoplakia.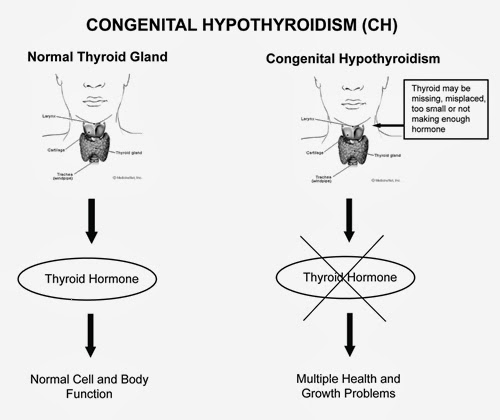 Bone marrow depression also occurs, which is manifested by aplastic anemia, immunodeficiency and bleeding. Often, congenital dyskeratosis is complicated by malignant neoplasms. Diagnosis involves comparing clinical symptoms and identifying karyotype defects using karyotyping or fluorescent hybridization. Treatment consists of restoring normal bone marrow function through bone marrow transplantation or pharmacological stimulation. In parallel, symptomatic therapy is carried out.
Bone marrow depression also occurs, which is manifested by aplastic anemia, immunodeficiency and bleeding. Often, congenital dyskeratosis is complicated by malignant neoplasms. Diagnosis involves comparing clinical symptoms and identifying karyotype defects using karyotyping or fluorescent hybridization. Treatment consists of restoring normal bone marrow function through bone marrow transplantation or pharmacological stimulation. In parallel, symptomatic therapy is carried out.
- Causes of congenital dyskeratosis
- Symptoms of dyskeratosis congenita
- Diagnosis of congenital dyskeratosis
- Treatment of dyskeratosis congenita
- Prices for treatment
General
Congenital dyskeratosis is a genetically determined syndrome, manifested by bone marrow failure and a set of specific symptoms. For the first time, the classical triad of the disease was described in 1906 by the German dermatovenereologist Zinsser. At 19In the 30s, Cole and Engman supplemented the description, after which the pathology received a second name - the Zinsser-Cole-Engman syndrome. At the moment, the clinical characteristics of the disease, in addition to the classic triad, include other symptoms and syndromes. Pathology is extremely rare, the prevalence is 1:1000000. Males get sick 4.7 times more often than females. The manifestation of the disease occurs at the age of 5 to 15 years, so the pediatrician is the first to encounter it. Symptoms develop gradually, the most pronounced clinical picture occurs at the age of 25-30 years and older. As a rule, patients die from complications in the form of secondary infections, malignant neoplasms and internal bleeding.
At 19In the 30s, Cole and Engman supplemented the description, after which the pathology received a second name - the Zinsser-Cole-Engman syndrome. At the moment, the clinical characteristics of the disease, in addition to the classic triad, include other symptoms and syndromes. Pathology is extremely rare, the prevalence is 1:1000000. Males get sick 4.7 times more often than females. The manifestation of the disease occurs at the age of 5 to 15 years, so the pediatrician is the first to encounter it. Symptoms develop gradually, the most pronounced clinical picture occurs at the age of 25-30 years and older. As a rule, patients die from complications in the form of secondary infections, malignant neoplasms and internal bleeding.
Congenital dyskeratosis
Causes of congenital dyskeratosis
Dyskeratosis congenita is a hereditary disease that is transmitted by X-linked, autosomal dominant and autosomal recessive types.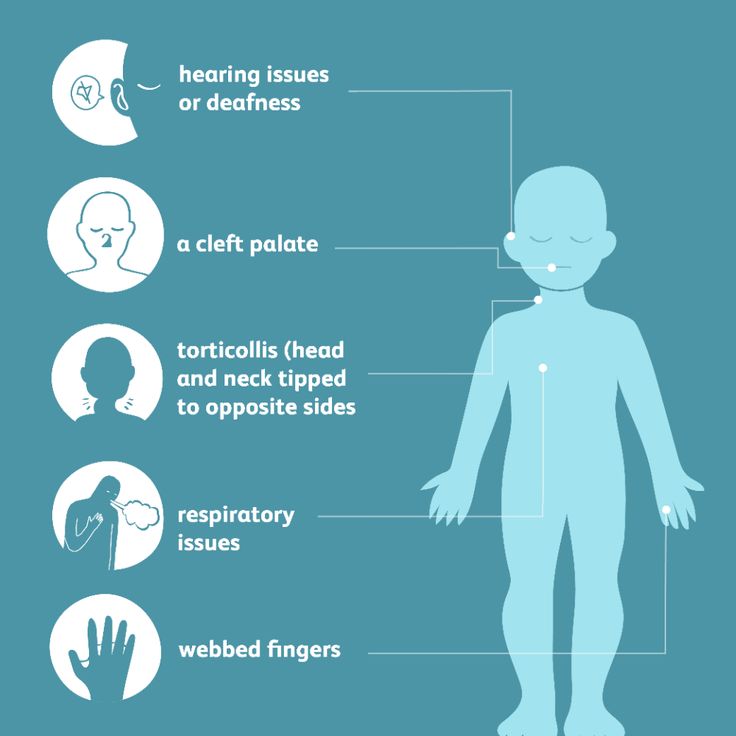 In more than 75% of cases, the transmission is recessive, through the X chromosome, in 25% - by an autosomal dominant mechanism. Localization of the defective gene that causes the development of dyskeratosis - dyskeratin - Xq28, rarely - in 3q14. Chromatid breaks can be observed at the 2q33 and 8q22 loci, mitosis anomalies. The causes and mechanisms of development of the primary karyotype defect are unknown.
In more than 75% of cases, the transmission is recessive, through the X chromosome, in 25% - by an autosomal dominant mechanism. Localization of the defective gene that causes the development of dyskeratosis - dyskeratin - Xq28, rarely - in 3q14. Chromatid breaks can be observed at the 2q33 and 8q22 loci, mitosis anomalies. The causes and mechanisms of development of the primary karyotype defect are unknown.
Symptoms of dyskeratosis congenita
The classic version of congenital dyskeratosis includes a triad of symptoms: dystrophic changes in the nails, hyperpigmentation of the skin and leukoplakia of the mucous membranes. In more than 85% of cases, its course is complicated by other pathological conditions: aplastic anemia, immunodeficiency, anomaly in the development of the cerebellum, mental retardation, fibrous degeneration of the lungs or liver, malignant neoplasm. The disease develops gradually. Up to 5 years, congenital dyskeratosis proceeds latently.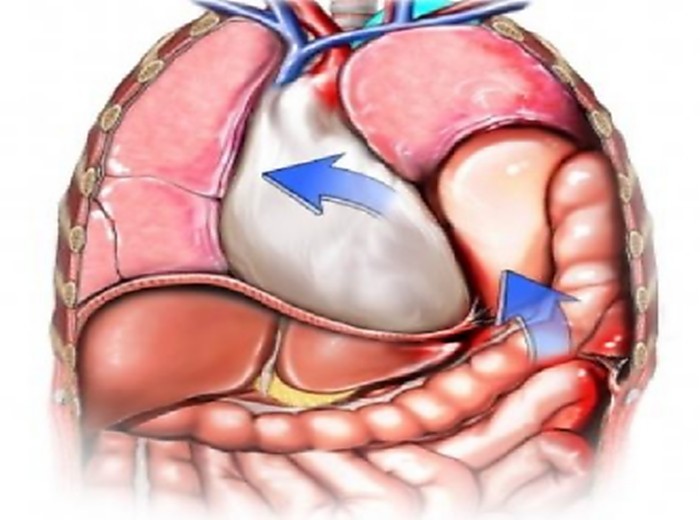 The first manifestations can develop between the ages of 6 and 15, sometimes after 20. With age, all symptoms worsen and complications develop.
The first manifestations can develop between the ages of 6 and 15, sometimes after 20. With age, all symptoms worsen and complications develop.
The primary manifestation of congenital dyskeratosis, as a rule, is dystrophy of the nail plates. The nails become thin and brittle, there is a longitudinal striation. After 2-3 years, these manifestations are joined by reticular hyperpigmentation of the skin with characteristic localization - the face, neck, upper chest surface. The average size of the affected areas is 2-8 mm in diameter. The skin atrophies, acquires a brown tint, and telangiectasias can be observed on it. Often there is hyperhidrosis and hyperkeratosis of the feet and hands, acrocyanosis, alopecia. After some time, the nail plastics can spontaneously fall off, which is most often observed on the little toes of the feet.
More than half of patients under the age of 8-10 years develop hypoplastic anemia, which in pediatrics is often regarded as Fanconi's anemia. The first clinical manifestations are frequent nosebleeds. Soon there is a decrease in immunity. Rarely, anemia and immunodeficiency are the primary signs of dyskeratosis congenita. At the age of 25-30 years, there is a lesion of the mucous membranes of the mouth. They may develop vesicles or papules, turning into erosion; papillomas, atrophy of the papillae of the tongue, gingivitis, leukoplakia. There is a loss of teeth. Often there is eye damage - conjunctivitis, blepharitis, ectropion, cataracts and glaucoma. Gradually, leukoplakia also affects other mucous membranes - the urethra, intestines, and genital organs. A third of patients have mental retardation.
The first clinical manifestations are frequent nosebleeds. Soon there is a decrease in immunity. Rarely, anemia and immunodeficiency are the primary signs of dyskeratosis congenita. At the age of 25-30 years, there is a lesion of the mucous membranes of the mouth. They may develop vesicles or papules, turning into erosion; papillomas, atrophy of the papillae of the tongue, gingivitis, leukoplakia. There is a loss of teeth. Often there is eye damage - conjunctivitis, blepharitis, ectropion, cataracts and glaucoma. Gradually, leukoplakia also affects other mucous membranes - the urethra, intestines, and genital organs. A third of patients have mental retardation.
Diagnosis of congenital dyskeratosis
Diagnosis of congenital dyskeratosis is difficult. The disease is extremely rare and has a large number of clinical manifestations. The diagnosis is made on the basis of all available symptoms and syndromes, laboratory data and histological examination of the skin biopsy.
General clinical analyzes make it possible to establish the presence of individual syndromes. In the KLA in the early stages, leukocytosis, neutropenia, and an increase in ESR are possible. Further, pancytopenia, aplastic anemia develops, macrocytosis and an increase in the concentration of fetal hemoglobin are possible. Sternal puncture in the later stages reveals depression of the bone marrow. Histological examination of the affected areas of the skin reveals atrophy of the epidermis, mild hyperkeratosis, increased pigmentation of the basal layer, in the dermis - an increase in the number of melanophages in the papillary and reticular layers, dilation of the vessels of the microvasculature. Possible violation of the structure of collagen, homogenization and fragmentation of its fibers. Specific diagnostics is aimed at identifying karyotype defects. Karyotyping or fluorescent hybridization is carried out, in which it is possible to establish a gene mutation in the Xq28 region, rarely in 3q14.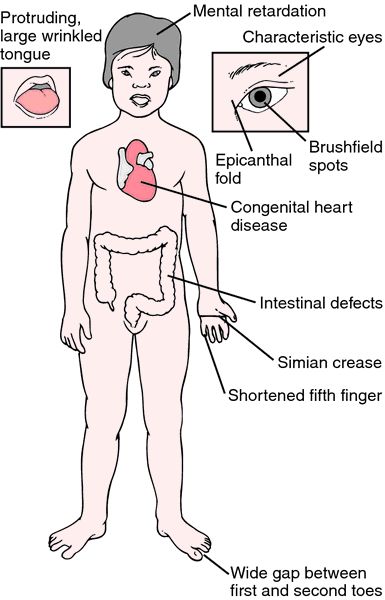
Differential diagnosis of congenital dyskeratosis is carried out with xeroderma pigmentosum, anhydrotic ectodermal dysplasia, poikiloderma, epidermolysis bullosa, Fanconi anemia.
Treatment of dyskeratosis congenita
Treatment of congenital dyskeratosis is ineffective. The main goal is to combat the suppression of bone marrow function. The method of choice is bone marrow transplantation from a brother or sister who does not suffer from this disease. Even against the background of transplantation, most patients experience a graft-versus-host reaction. If it is impossible to carry out transplantation, the use of anabolic hormonal agents (oxymetholone), colony-stimulating factors, erythropoietins is indicated. Treatment of malignant neoplasms in such patients is carried out using proton therapy. Leukoplakia is treated with retinoids and P-carotene.
The prognosis for congenital dyskeratosis is unfavorable.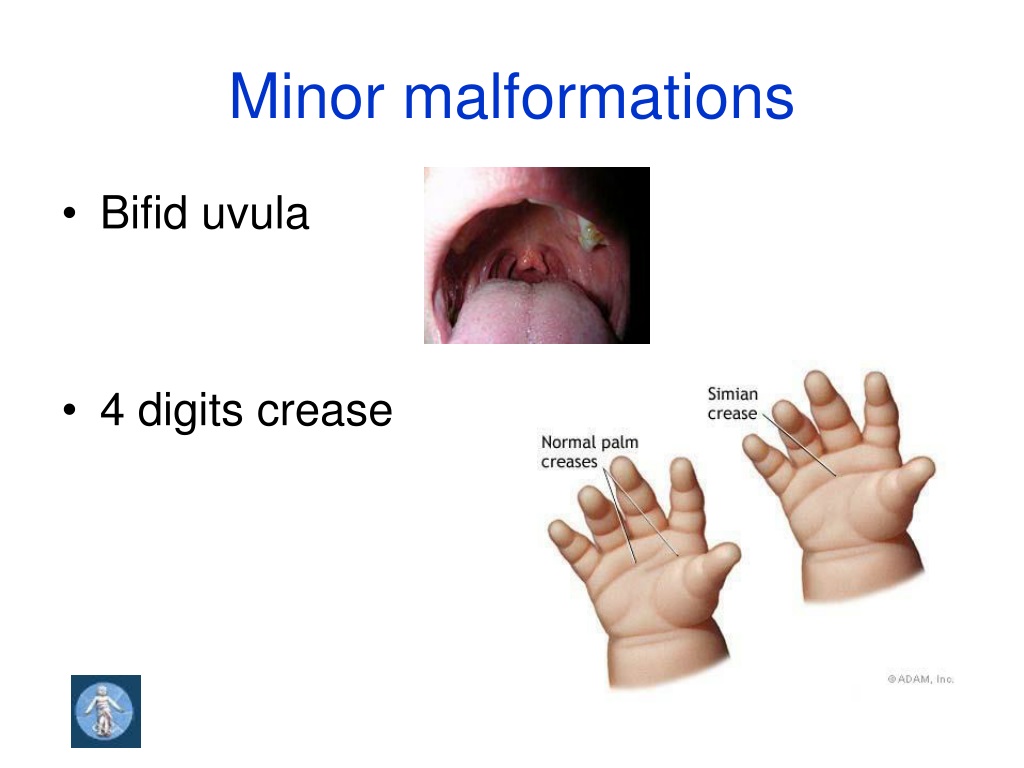 The disease is almost always fatal. Death is caused by malignant neoplasms, the addition of a secondary infection (mainly pneumonia), gastrointestinal or other internal bleeding. Most often, patients die from squamous cell cancer of the oral cavity, laryngopharynx, genital organs, urethra and gastrointestinal tract, less often - pancreatic adenocarcinoma, Hodgkin's lymphoma.
The disease is almost always fatal. Death is caused by malignant neoplasms, the addition of a secondary infection (mainly pneumonia), gastrointestinal or other internal bleeding. Most often, patients die from squamous cell cancer of the oral cavity, laryngopharynx, genital organs, urethra and gastrointestinal tract, less often - pancreatic adenocarcinoma, Hodgkin's lymphoma.
Sources
- This article was prepared based on the site: https://www.krasotaimedicina.ru/
IMPORTANT
Information from this section cannot be used for self-diagnosis and self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
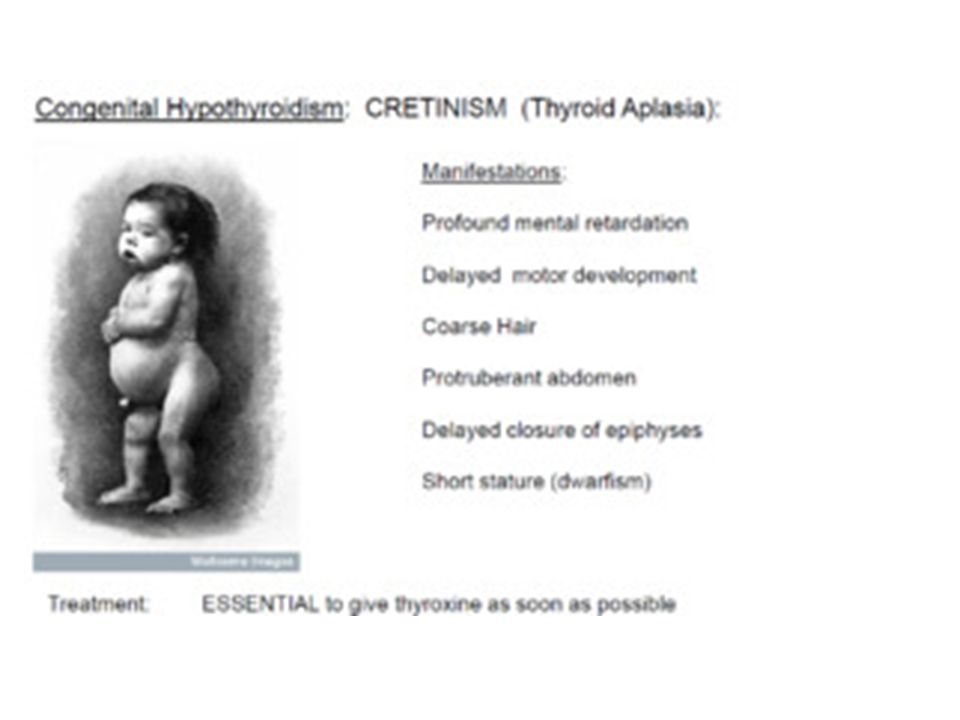
Congenital hypothyroidism. What is Congenital Hypothyroidism?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Congenital hypothyroidism is a complex of clinical and laboratory manifestations that occur in a child from birth with a deficiency of thyroid hormones or resistance of tropic organs to them. Symptoms include a lag in psychophysical development, myxedema, trophic disorders of the skin and its appendages, depression of the heart, and a decrease in basal metabolism. Diagnosis is based on a characteristic clinic, X-ray diagnostic data, ultrasound of the thyroid gland, ECG, laboratory tests, including measurements of thyroid-stimulating hormone and thyroxine in blood plasma. Treatment involves lifelong replacement therapy with artificial analogues of thyroid hormones.
- Causes
- Classification of congenital hypothyroidism
- Symptoms of congenital hypothyroidism
- Diagnostics
- Treatment of congenital hypothyroidism
- Prices for treatment
General
Congenital hypothyroidism is a polyetiological disease characterized by clinical manifestations of thyroid insufficiency.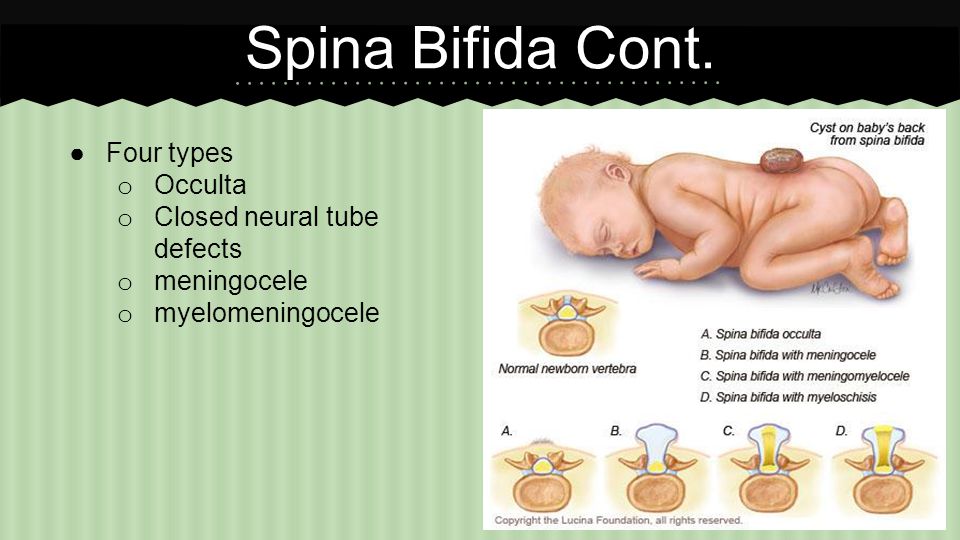 It is the most common endocrine pathology in pediatrics. Most often, the disease occurs against the background of changes directly in the thyroid gland, less often it is the result of a pathology of the hypothalamic-pituitary system or a defective structure of the receptor apparatus of tropic organs. AT 90% of cases are sporadic. The incidence is 1:3.7-4 thousand newborns in Europe and the USA, in Japan - 1:6-7 thousand. The female sex is sick 2-2.5 times more often than the male. The first screening tests for congenital hypothyroidism were performed in 1973 by Canadians J. Dussault, C. Laberge. At the moment, neonatal screening is carried out in order to make the diagnosis as quickly as possible and, if necessary, to conduct timely treatment.
It is the most common endocrine pathology in pediatrics. Most often, the disease occurs against the background of changes directly in the thyroid gland, less often it is the result of a pathology of the hypothalamic-pituitary system or a defective structure of the receptor apparatus of tropic organs. AT 90% of cases are sporadic. The incidence is 1:3.7-4 thousand newborns in Europe and the USA, in Japan - 1:6-7 thousand. The female sex is sick 2-2.5 times more often than the male. The first screening tests for congenital hypothyroidism were performed in 1973 by Canadians J. Dussault, C. Laberge. At the moment, neonatal screening is carried out in order to make the diagnosis as quickly as possible and, if necessary, to conduct timely treatment.
congenital hypothyroidism
Reasons
In 80-90% of cases, a primary form of congenital hypothyroidism occurs. Causes - anomalies in the development of the thyroid gland, most often - dystopia in the retrosternal or sublingual space, less often - hypoplasia, athyreosis. Risk factors can be autoimmune and infectious diseases of the mother, the toxic effects of medicines, chemicals, radiation exposure, iodine deficiency during pregnancy. About 2% of cases of malformations of the gland are hereditary forms. Their main cause is mutations in the TITF1, TITF2, FOXE1, PAX8 genes. As a rule, genetically determined forms accompany other developmental anomalies: congenital heart defects, "cleft palate", etc.
Risk factors can be autoimmune and infectious diseases of the mother, the toxic effects of medicines, chemicals, radiation exposure, iodine deficiency during pregnancy. About 2% of cases of malformations of the gland are hereditary forms. Their main cause is mutations in the TITF1, TITF2, FOXE1, PAX8 genes. As a rule, genetically determined forms accompany other developmental anomalies: congenital heart defects, "cleft palate", etc.
From 5 to 10% of children with congenital hypothyroidism have disorders in the synthesis, secretion or interaction of the thyroid hormones themselves. Transmission usually occurs in an autosomal recessive manner. The most common variants are defects in the organization of iodine and thyroid hormones (frequency - 1:40,000), Pendred's syndrome (1:50,000). Other forms are extremely rare.
Approximately 5% of all cases of congenital hypothyroidism are central (secondary or tertiary) forms. The most common variant is a combined deficiency of adenohypophysis hormones, including TSH. Isolated deficiency is rare. Causes of damage to the hypothalamic-pituitary system - anomalies in the development of the brain, cysts, malignant and benign tumors, birth trauma of newborns, asphyxia during childbirth, rarely - aplasia of the pituitary gland.
Isolated deficiency is rare. Causes of damage to the hypothalamic-pituitary system - anomalies in the development of the brain, cysts, malignant and benign tumors, birth trauma of newborns, asphyxia during childbirth, rarely - aplasia of the pituitary gland.
The cause of the development of clinical symptoms of hypothyroidism may be an anomaly in the structure of receptors in target organs caused by gene mutations. The impossibility of interaction of a sufficient amount of hormones with receptors of tropic tissues provokes the development of the so-called "resistance syndrome". As a rule, this is a hereditary pathology transmitted in an autosomal dominant manner. With it, the level of TSH in the blood plasma is normal, T3 and T4 are within the normal range or moderately elevated.
Classification of congenital hypothyroidism
Congenital hypothyroidism has several classifications based on the localization of the disorder, the severity of symptoms and the level of thyroxine, compensation during treatment, and the duration of the disease. According to the origin of the disease, the following forms of hypothyroidism are distinguished:
According to the origin of the disease, the following forms of hypothyroidism are distinguished:
According to the severity of clinical symptoms and the level of T4 in plasma, hypothyroidism can be latent, manifest and complicated. Latent or subclinical hypothyroidism is characterized by a normal T4 level against the background of an increase in TSH.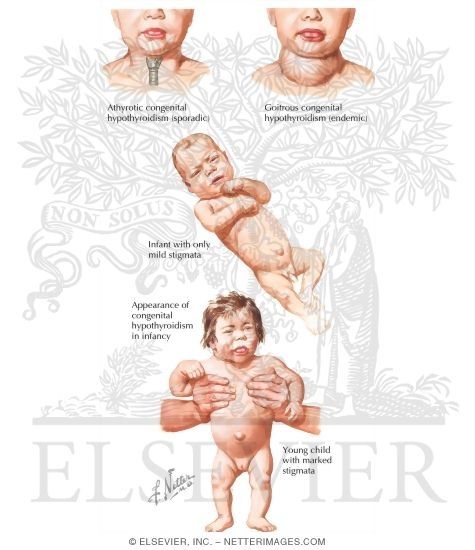 Clinical manifestations do not occur or they are nonspecific and hardly noticeable. With a manifest form, against the background of a high concentration of TSH, the level of T4 is somewhat reduced. The classic clinical picture of hypothyroidism develops. Complicated hypothyroidism occurs with a high level of TSH, a sharp deficiency of T4. In addition to the severe degree of hypothyroidism, there are violations of other organs and systems: heart failure, polyserositis, cretinism, coma, and rarely - pituitary adenoma.
Clinical manifestations do not occur or they are nonspecific and hardly noticeable. With a manifest form, against the background of a high concentration of TSH, the level of T4 is somewhat reduced. The classic clinical picture of hypothyroidism develops. Complicated hypothyroidism occurs with a high level of TSH, a sharp deficiency of T4. In addition to the severe degree of hypothyroidism, there are violations of other organs and systems: heart failure, polyserositis, cretinism, coma, and rarely - pituitary adenoma.
Depending on the effectiveness of treatment, congenital hypothyroidism is distinguished:
- compensated - against the background of the treatment, the phenomena of hypothyroidism disappear, the concentration of TSH, T3, T4 in the blood plasma is within the normal range;
- decompensated - even against the background of adequate treatment, there are clinical and laboratory manifestations of hypothyroidism.
By duration, congenital hypothyroidism is divided into:
- transient - the disease develops against the background of exposure to maternal antibodies to the child's TSH.
 Duration - from 7 days to 1 month.
Duration - from 7 days to 1 month. - permanent - requires lifelong replacement therapy.
Symptoms of congenital hypothyroidism
Depending on the form and severity of disorders, the first signs of primary congenital hypothyroidism can manifest at different ages. Sharp hypoplasia or aplasia of the gland manifests itself in the first 7 days of a child's life. Dystopia or mild hypoplasia may cause clinical manifestations between the ages of 2 and 6 years.
Primary signs indicating congenital hypothyroidism: birth weight of the child over 4 kg; immaturity with full-term or post-term (more than 40 weeks) pregnancy; delayed discharge of meconium masses; prolonged jaundice in newborns; dyspeptic phenomena; slow weight gain; lethargy; macroglossia; flatulence and constipation; muscle weakness; hyporeflexia; cyanosis and episodes of apnea during feeding. The skin of the child is cold, swelling of the extremities and genitals occurs. Often there are enlarged fontanelles, nonunion of the sutures of the bones of the skull, dysplasia of the hip joints. Breastfeeding can reduce the severity of clinical manifestations of hypothyroidism.
Often there are enlarged fontanelles, nonunion of the sutures of the bones of the skull, dysplasia of the hip joints. Breastfeeding can reduce the severity of clinical manifestations of hypothyroidism.
Primary congenital hypothyroidism develops in stages. A pronounced clinic is observed at the age of 3-6 months. There is myxedema. The skin is compacted, icteric-gray, dry. Sweating is drastically reduced. Atrophy of the nail plates and hair develops. The child's voice is low, hoarse and rough. There is a lag in psychomotor and physical development, teeth erupt and are replaced with a delay. With further development, mental retardation is observed. This is manifested by the scarcity of vocabulary and a decrease in intelligence, which is prone to progression up to oligophrenia.
Central congenital hypothyroidism has an indistinct clinical picture. It is often combined with anomalies of the facial skull ("cleft lip", "cleft palate") and insufficiency of other pituitary hormones (somatotropic, luteinizing and follicle-stimulating) with characteristic symptoms.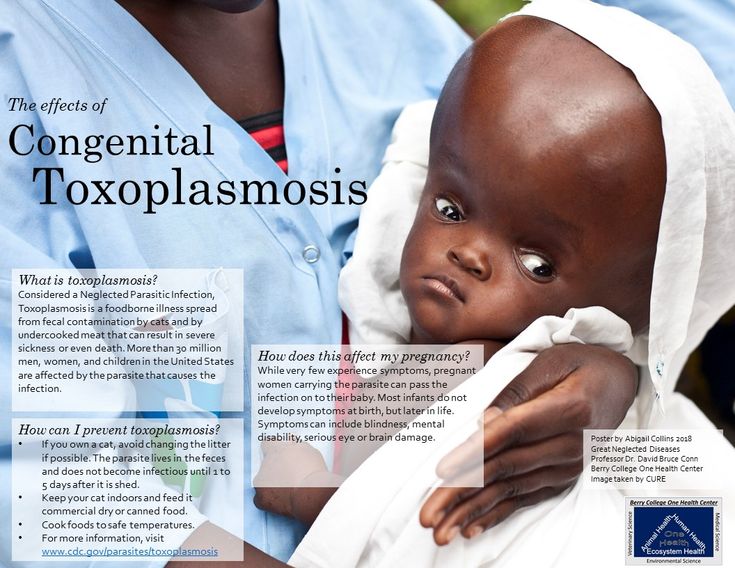
Diagnosis
Diagnosis of congenital hypothyroidism includes the collection of anamnestic data, an objective examination of the child by a pediatrician or neonatologist, instrumental studies, general and specific laboratory tests. In the anamnesis, predisposing factors can be identified - aggravated heredity, maternal diseases during pregnancy, malnutrition, the use of obstetric benefits during childbirth, etc. A physical examination of the child reveals a decrease in heart rate, blood pressure, moderate hypothermia, hyporeflexia, developmental delay.
On the radiograph of the extremities, a delay and a violation of the sequence of formation of ossification nuclei, their asymmetry and a specific sign - epiphyseal dysgenesis are determined. On the ECG - sinus bradycardia, a decrease in the amplitude of the teeth, the expansion of the QRS complex. Ultrasound of the thyroid gland reveals dystopia, hypoplasia or the absence of this organ.
In the KLA - normochromic anemia. In a biochemical blood test, an increase in lipoproteins and cholesterol is detected. If a central origin of hypothyroidism is suspected, CT and MRI of the pituitary gland are performed. Specific laboratory tests - measurement of T4 and TSH levels in blood plasma. These tests are used as neonatal screening. Depending on the form of hypothyroidism, the concentrations of these hormones in the blood can be increased or decreased. Rarely, molecular genetic testing is used to identify gene mutations.
Treatment of congenital hypothyroidism
Treatment for congenital hypothyroidism begins immediately upon diagnosis and continues for life. The drug of choice is L-thyroxine. This tool is a synthetic analogue of thyroid hormones and is used as a replacement therapy. The dosage is selected individually. If necessary, the drug can be mixed with breast milk. The effectiveness of the treatment is assessed by the level of TSH and T4 in the blood, the disappearance of symptoms of hypothyroidism.