Antibodies in the blood during pregnancy
The Rh Factor: How It Can Affect Your Pregnancy
Amniocentesis: A procedure in which amniotic fluid and cells are taken from the uterus for testing. The procedure uses a needle to withdraw fluid and cells from the sac that holds the fetus.
Anemia: Abnormally low levels of red blood cells in the bloodstream. Most cases are caused by iron deficiency (lack of iron).
Antibodies: Proteins in the blood that the body makes in reaction to foreign substances, such as bacteria and viruses.
Breech Presentation: A position in which the feet or buttocks of the fetus would appear first during birth.
Cells: The smallest units of a structure in the body. Cells are the building blocks for all parts of the body.
Chorionic Villus Sampling (CVS): A procedure in which a small sample of cells is taken from the placenta and tested.
Ectopic Pregnancy: A pregnancy in a place other than the uterus, usually in one of the fallopian tubes.
Fetus: The stage of human development beyond 8 completed weeks after fertilization.
Genes: Segments of DNA that contain instructions for the development of a person's physical traits and control of the processes in the body. They are the basic units of heredity and can be passed from parent to child.
Induced Abortion: An intervention to end a pregnancy so that it does not result in a live birth.
Jaundice: A buildup of bilirubin (a brownish yellow substance formed from the breakdown of red cells in the blood) that causes the skin to have a yellowish appearance.
Miscarriage: Loss of a pregnancy that is in the uterus.
Obstetrician–Gynecologist (Ob-Gyn): A doctor with special training and education in women's health.
Oxygen: An element that we breathe in to sustain life.
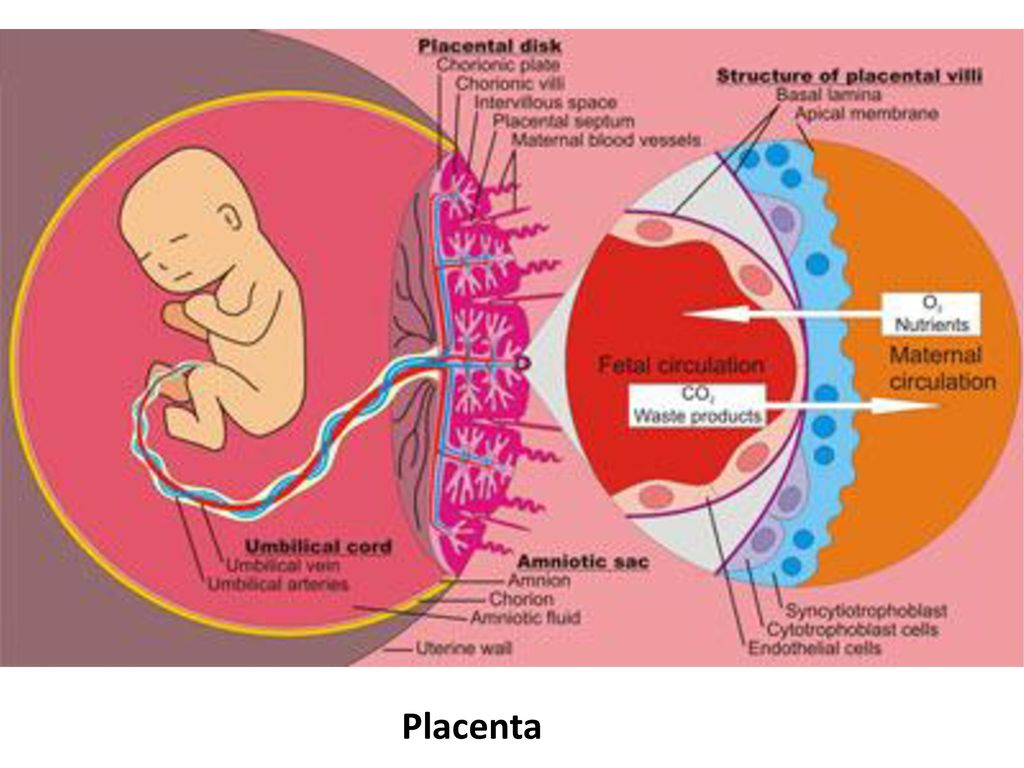
Placenta: An organ that provides nutrients to and takes waste away from the fetus.
Prenatal Care: A program of care for a pregnant woman before the birth of her baby.
Rh Factor: A protein that can be found on the surface of red blood cells.
Rh Immunoglobulin (RhIg): A substance given to prevent an Rh-negative person's antibody response to Rh-positive blood cells.
Trimester: A 3-month time in pregnancy. It can be first, second, or third.
Ultrasound Exams: Tests in which sound waves are used to examine inner parts of the body. During pregnancy, ultrasound can be used to check the fetus.
Umbilical Cord: A cord-like structure containing blood vessels. It connects the fetus to the placenta.
Uterus: A muscular organ in the female pelvis. During pregnancy, this organ contains and nourishes the fetus.
Prenatal Antibody Screening: Purpose, Procedure, and Results
Written by Linda Rath
When you're a mom-to-be, one of the prenatal tests you may get is an antibody test or antibody screening.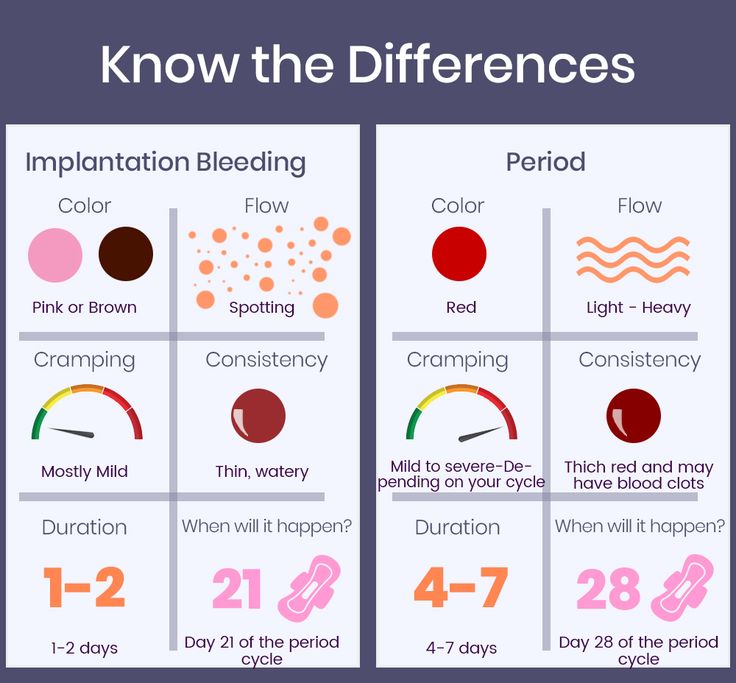 It looks for certain antibodies, special proteins made by your immune system, in your blood.
It looks for certain antibodies, special proteins made by your immune system, in your blood.
You might have these antibodies if you've gotten blood from a donor or given birth before. There's also a chance your body could make them when your and your baby's blood types don't match.
Some of these antibodies can be passed from you into your baby's bloodstream, where they could do harm. Antibody testing lets you and your doctor know if you have them so you can take steps to protect your growing baby.
Why You Get Tested
Your immune system makes antibodies to fight things it sees as "not you." Most of the time, that's great because antibodies usually target germs. And when you're pregnant, your immune system takes care of your baby, too. But if your red blood cells are different from your baby's, that may cause problems.
By far, the most common one is related to the + or - part of your blood type, called the Rh factor. Many people are Rh-positive, which means they have the Rh protein on their red blood cells.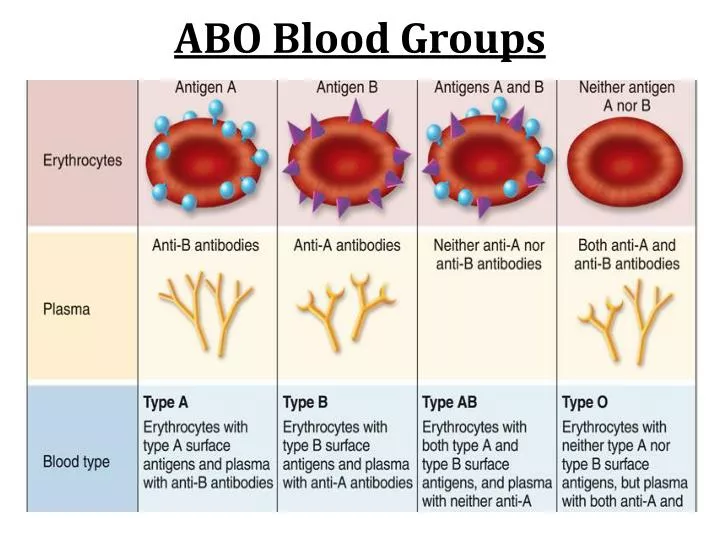 Rh-negative people don't. So they'll make antibodies to attack any Rh-positive blood cells that get into their body.
Rh-negative people don't. So they'll make antibodies to attack any Rh-positive blood cells that get into their body.
If you're Rh-negative and your baby is Rh-positive, your blood might have Rh antibodies that could spread to your baby's blood, where they'd attack and destroy your baby's red blood cells. This can cause a type of anemia that's very serious and could be fatal.
Your body might have made other antibodies that could attack your baby's red blood cells, too.
How It's Done
You should get your blood type checked early in your pregnancy, perhaps at your first prenatal visit. If you're Rh-negative, then you should have the antibody test during the first 3 months that you're pregnant. (If you're Rh-positive, your doctor may still want to do an antibody test in your first trimester.)
A technician uses a needle to take a sample of blood from a vein in your hand or arm. You may feel a small skin prick and have a little bleeding or bruising where the needle goes in.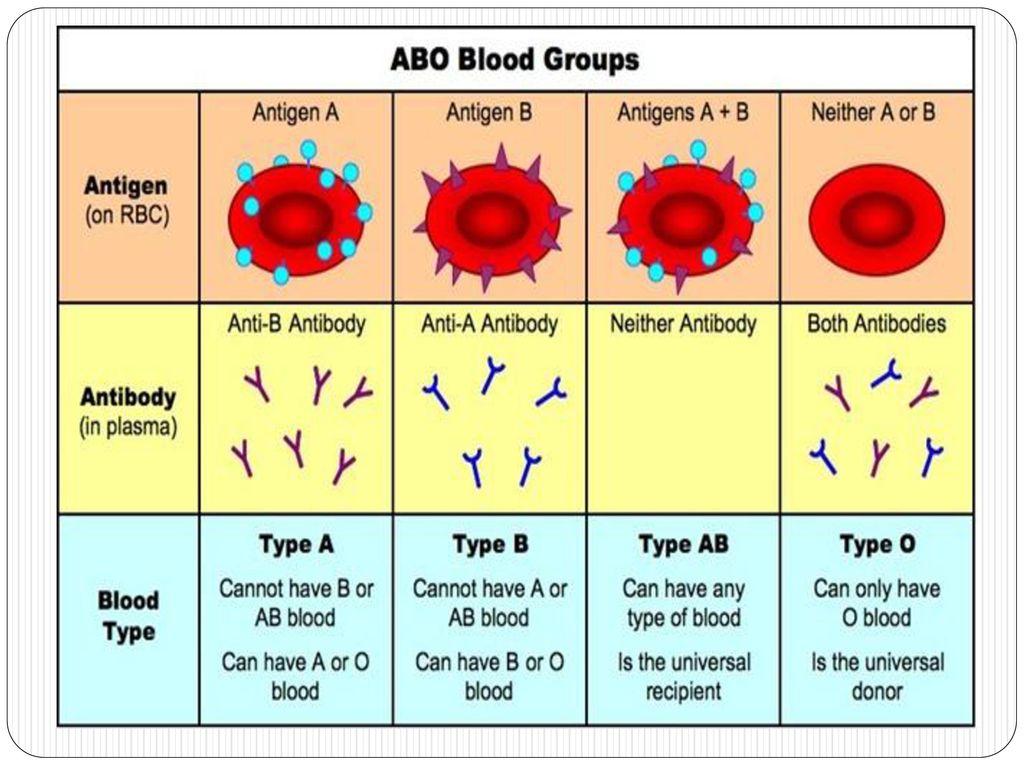
Then they'll send the sample to a lab to run an indirect Coombs test, which checks for red blood cell antibodies.
What the Results Mean
A negative antibody test tells you that you don't have harmful antibodies in your blood. If you're also Rh-positive, you can safely carry a baby with either a + or - blood type. Relax and enjoy being pregnant!
If the test was negative and you're Rh-negative -- but there's a chance your baby is Rh-positive (because the father is) -- you'll need another test about 28 weeks into your pregnancy. If it's negative again, your doctor will probably give you a shot of medicine called Rho(D) immune globulin (RhoGAM, RhIG, WinRho) to stop your immune system from making Rh antibodies.
These antibodies might not cause trouble for your first baby, but the shot will also help prevent trouble if you get pregnant again.
A positive test means you already have antibodies in your blood. If they're Rh antibodies, the shot won't help. Your doctor will watch you and your baby closely. If there are problems while you're pregnant, your baby may need to be born early or get a blood transfusion through the umbilical cord.
If there are problems while you're pregnant, your baby may need to be born early or get a blood transfusion through the umbilical cord.
Pregnancy in women with Rh-negative blood
The issue of Rhesus conflict during pregnancy is one of the few in medicine, in which all the i's are dotted and not only diagnostic and treatment methods have been developed, but, most importantly, effective prevention.
The history of immunoprophylaxis of Rhesus conflict is a rare example of unconditional success in medicine. Indeed, after the introduction of a set of preventive measures, infant mortality from complications of the Rhesus conflict decreased from 46 to 1.6 per 100 thousand children - that is, almost 30 times.
What is Rh conflict, why does it occur and what can be done to minimize the risk of its occurrence?
The entire population of the planet, depending on the presence or absence on erythrocytes (red blood cells) of the protein, denoted by the letter "D", is divided respectively into Rh-positive and Rh-negative people.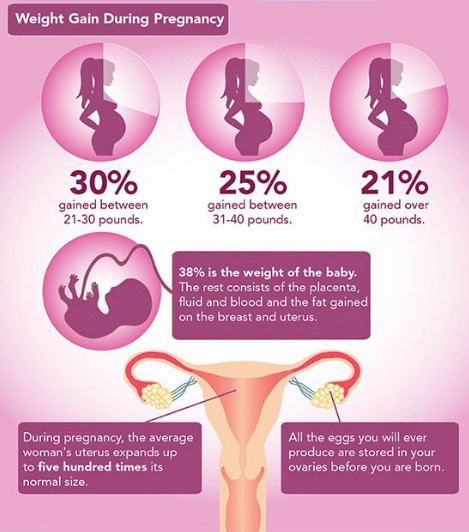 According to approximate data, about 15% of Europeans are Rh-negative. When pregnancy occurs in an Rh-negative woman from an Rh-positive man, the probability of having an Rh-positive child is 60%.
According to approximate data, about 15% of Europeans are Rh-negative. When pregnancy occurs in an Rh-negative woman from an Rh-positive man, the probability of having an Rh-positive child is 60%.
In this case, when fetal erythrocytes enter the mother's bloodstream, an immune reaction occurs, as a result of which fetal erythrocytes are damaged, anemia and a number of other serious complications occur.
During physiological pregnancy, fetal erythrocytes cross the placenta in the first trimester in 3% of women, in the second - in 15%, in the third - in 48%. In addition, massive casting occurs in childbirth, after termination of pregnancy (abortion, miscarriage, ectopic pregnancy, hydatidiform mole), invasive procedures (chorionic villus biopsy, amniocentesis), prenatal bleeding with a threat of termination of pregnancy.
The total risk of developing an Rh conflict in Rh-negative women pregnant with an Rh-positive fetus in the absence of prophylaxis is about 16%. In women who have undergone prophylaxis, this risk is reduced to 0.2%.
In women who have undergone prophylaxis, this risk is reduced to 0.2%.
And now the most interesting - what is this very prevention and what needs to be done to keep the situation under control.
All women who applied to a medical institution for pregnancy registration, as well as those who applied to terminate an unwanted pregnancy, are assigned an analysis to determine the blood type and Rh factor. Sexual partners of women who have a negative Rh are also recommended to undergo an examination to establish Rh-affiliation. If, by a happy coincidence, a man also has a negative Rh factor, then there is no risk of an Rh conflict and there is no point in conducting immunoprophylaxis.
Women with Rh-negative blood and Rh-positive partner's blood who wish to terminate an unwanted pregnancy are advised to give an injection of anti-Rh immunoglobulin within 72 hours after the termination. The mechanism of action of this drug is based on the fact that the injected antibodies bind the fetal erythrocytes that have entered the maternal bloodstream and prevent the development of an immune response.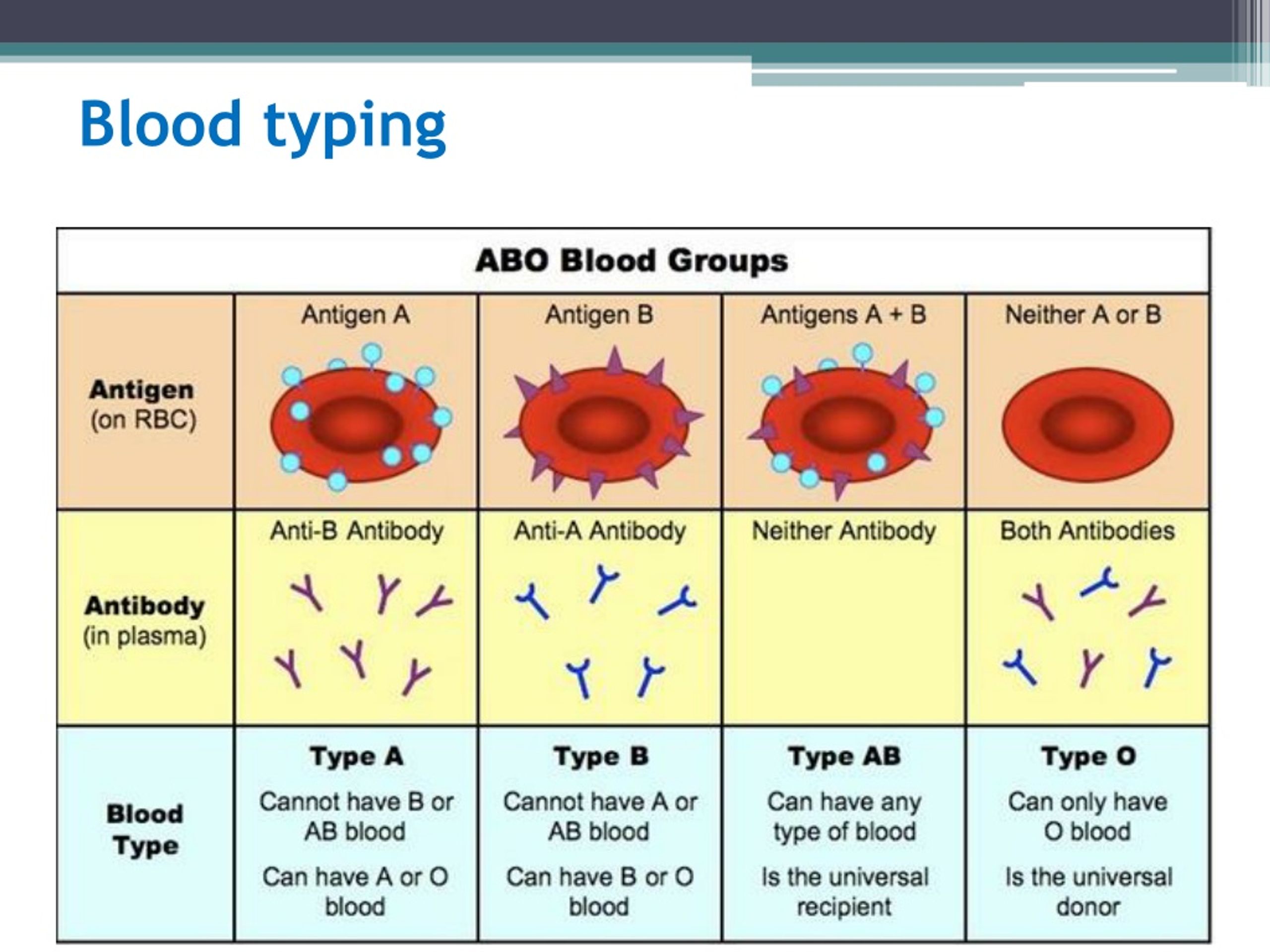
Rh-negative women registered for pregnancy are prescribed a monthly blood test for anti-Rh antibodies. Thus, it is determined whether there was contact between the blood of the mother and the fetus, and whether the woman's immune system reacted to a foreign protein.
If by the 28th week there are no anti-Rh antibodies in the woman's blood, she is sent for prophylactic administration of anti-Rh immunoglobulin. This prophylaxis is carried out from 28 to 30 weeks of pregnancy. After that, the determination of anti-Rhesus antibodies in the mother's blood is not carried out.
If, according to the results of the examination, anti-Rhesus antibodies are detected in a woman before 28 weeks of pregnancy, she is sent for an in-depth examination to determine the severity of the Rh conflict, timely treatment and, if necessary, emergency delivery.
After the birth of an Rh-negative woman, the Rh factor is determined. And, if the baby is Rh-positive, within 72 hours after birth, the woman is also injected with anti-Rh immunoglobulin.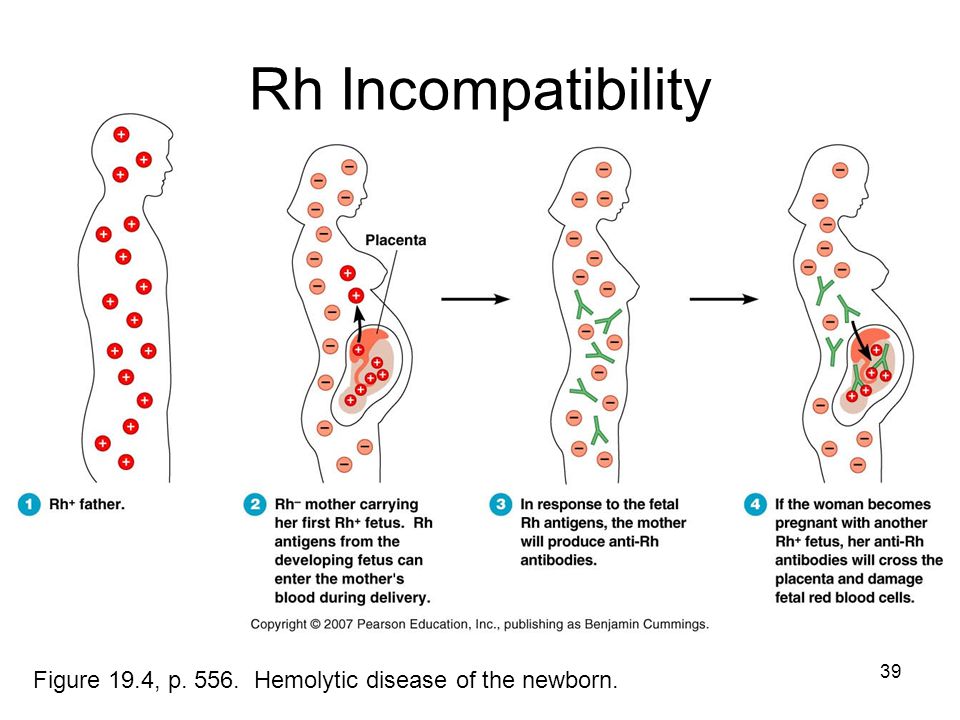
Other situations requiring prophylactic administration of anti-Rhesus immunoglobulin:
- miscarriage or non-progressive pregnancy;
- ectopic pregnancy;
- hydatidiform mole;
- prenatal bleeding with threatened miscarriage;
- invasive intrauterine interventions during pregnancy.
The only controversial issue at the moment is the determination of the Rh factor of the fetus during pregnancy. To do this, starting from the 10th week of pregnancy, a woman’s blood is taken, the genetic material of the fetus is isolated from it, and on the basis of a genetic study, the Rh affiliation of the unborn child is determined.
On the one hand, this study would allow 40% of Rh-negative women carrying an Rh-negative fetus to avoid monthly testing of anti-Rh antibodies and the introduction of anti-Rh immunoglobulin.
On the other hand, this research does not appear in the official order of the Ministry of Health, is not included in the CHI system and is carried out only on a paid basis.
Thus, at the moment, a clear algorithm has been developed for the management of pregnant women with Rh-negative blood. And following this simple algorithm will allow a woman to give birth to one, two or more healthy babies.
Obstetrician-gynecologist
antenatal clinic No. 14
Khivrich E.B.
Antibody testing during pregnancy in Moscow
| Additional tests | |
|---|---|
| CIA (dermatologist, smear, blood test for RW) | 700 |
| HIV testing | 300 |
| Staphylococcus aureus test | 540 |
| Brucellosis test | 300 |
| Bacterial analysis for intestinal group (typhoid, salmanella, shigella) | 460 |
| Enterobiasis test, worm eggs | 220 |
| Fluorography | 300 |
| ATT (attestation) | 1260 |
| ADsM (diphtheria) vaccination | 200 |
| ZHV vaccination (measles) | 200 |
| Hepatitis B vaccination | 500 |
| Hepatitis A vaccination | 200 |
| Dysentery | 200 |
| Therapist's report | 300 |
| ENT conclusion | 300 |
| Dental opinion | 300 |
| Narcologist's conclusion | 300 |
| Psychiatric report | 300 |
| Test for HBsAg, HCV (hepatitis B and C) | 400 |
| Conclusions of an otolaryngologist, dentist, analysis for Saphylococcus aureus | 540 |
| Diagnosis of Swine Flu A(h2N1) | 1300 |
If you are expecting a baby, you should understand that pregnancy is not only a wonderful time, but also frequent trips to the doctor for control and for the purpose of passing urine and blood tests.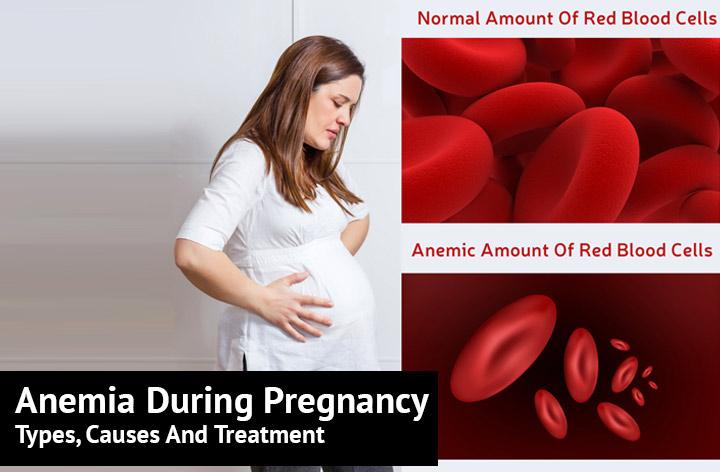 Do not think that this is a waste of time: such studies make it possible to understand whether everything is in order with the health and well-being of the expectant mother, whether the development of the fetus is normal. And blood is the main indicator of malfunctions in our body, it signals problems even when it cannot be determined visually and by sensations.
Do not think that this is a waste of time: such studies make it possible to understand whether everything is in order with the health and well-being of the expectant mother, whether the development of the fetus is normal. And blood is the main indicator of malfunctions in our body, it signals problems even when it cannot be determined visually and by sensations.
One of the most important examinations is the test for antibodies in the blood. An antibody is a special type of protein produced by the cells of our immune system. If such a compound is absent in the body, a person becomes susceptible to a certain disease. If it is, the disease will proceed much easier or even bypass you. Since susceptibility to various infections increases greatly during pregnancy, analysis becomes the only possible way to prevent potential danger.
The same analysis allows you to find out the Rh factor of the mother and father, as well as determine whether there is a Rh conflict. If the answer is yes, the pregnant woman is observed up to 32 weeks of gestation.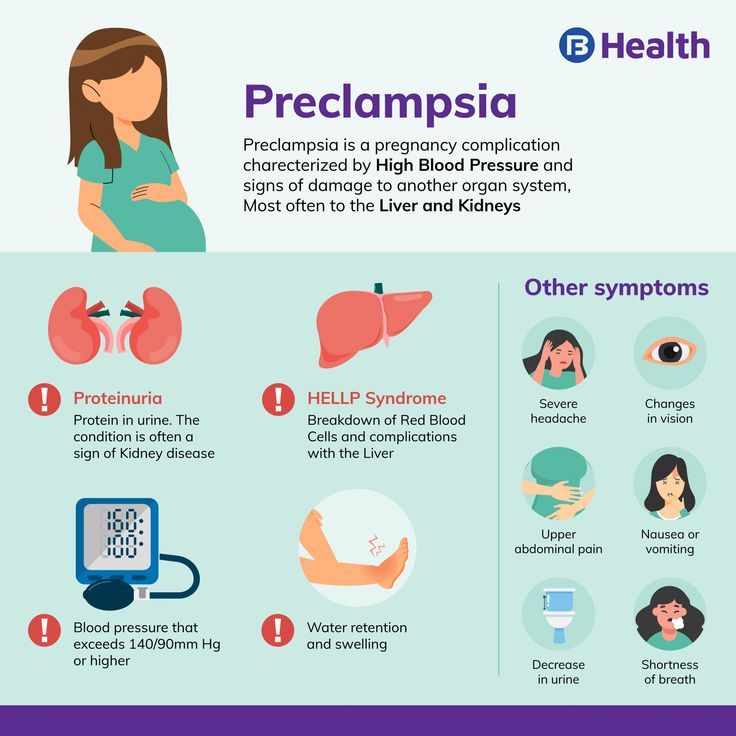 If this is not done, then the life of the unborn child is endangered, since an instantaneous development of jaundice, anemia, cerebral edema, hemolytic disease, and so on is possible.
If this is not done, then the life of the unborn child is endangered, since an instantaneous development of jaundice, anemia, cerebral edema, hemolytic disease, and so on is possible.
Preparation for the procedure
In order to successfully pass a blood test for group antibodies, you must first prepare. To do this, you will need to follow a diet, which is not at all difficult even during pregnancy, because women are “in an interesting position” and so limit themselves in many ways. For example, 2-3 days before the procedure, you will have to limit the consumption of fatty, spicy and fried foods, do not drink coffee and soda, and if you are taking any medications, then either refuse them or inform your doctor about taking medications .
By the way, many women resort to this examination even when planning a pregnancy, and not when it has already begun. This allows you to draw up a plan of further actions in advance and follow it calmly if it turns out that there is a Rhesus conflict. But even if you did not attend to the issue ahead of time, there is nothing wrong with that. Most of these situations, if their development is closely monitored, are resolved safely for both the mother and the fetus.
But even if you did not attend to the issue ahead of time, there is nothing wrong with that. Most of these situations, if their development is closely monitored, are resolved safely for both the mother and the fetus.
Promotions are constantly held in our clinic
How is blood drawn?
On the day of the procedure, you come to the blood collection room - eating before this (approximately 2 hours) is prohibited. For analysis, venous blood is required, which is taken from the cubital vein, after applying a tourniquet to the arm. The process lasts for several minutes, and discomfort is minimized and can be directly related to the moment of puncture.
Call us
+7 (495) 106-06-20
Where to donate blood for analysis?
To get a blood test for anti-Rhesus antibodies, please contact the medical center OOO "Medicina" located in Moscow and offering the services of its own modern clinical laboratory. In our clinic, highly qualified experienced doctors practice an individual, very attentive approach to patients and adhere to modern methods of diagnosis and treatment.