What does fetal distress mean
Fetal distress | Pregnancy Birth and Baby
Fetal distress | Pregnancy Birth and Baby beginning of content7-minute read
Listen
Key facts
- Fetal distress is a sign that your baby is not well.
- Your doctor or midwife will monitor your baby’s heartbeat during pregnancy and labour to assess their wellbeing.
- If your baby shows signs of fetal distress, your midwife or doctor will act quickly to try and treat any underlying cause.
- You may need help to birth your baby quickly with an assisted (instrumental) delivery or caesarean section.
- Fetal distress can increase the risk of birth complications, especially if it isn’t treated quickly.
If you are pregnant and notice a decrease in your baby’s movements, seek urgent medical attention. This may be a sign that your baby is unwell.
What is fetal distress?
Fetal distress is a sign that your baby is not well. It happens when the baby isn’t receiving enough oxygen through the placenta.
Fetal distress can sometimes happen during pregnancy, but it’s more common during labour.
What causes fetal distress?
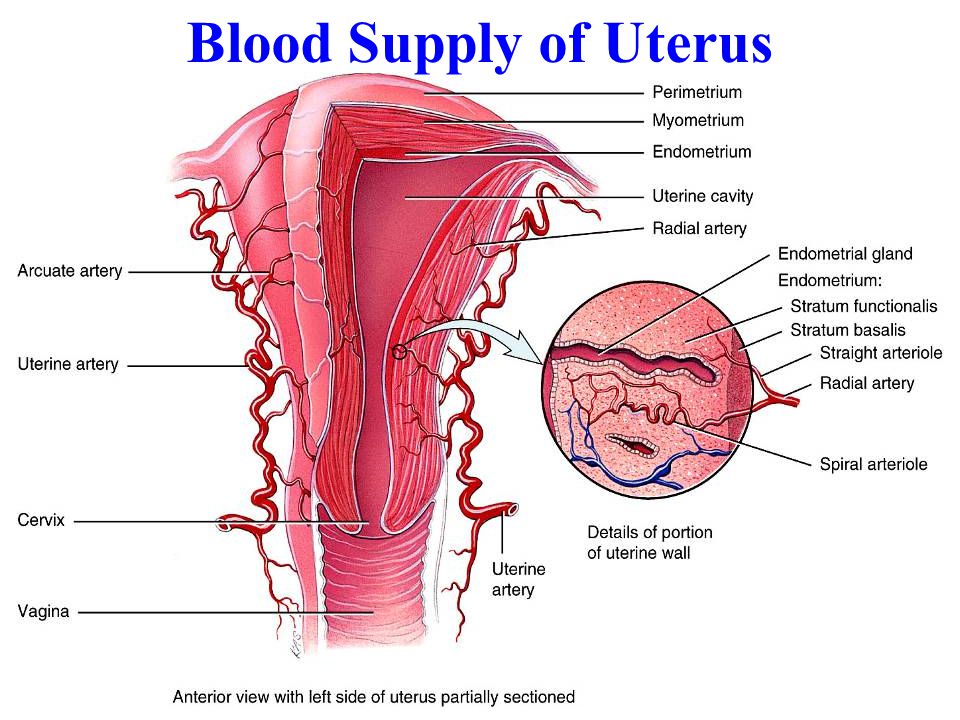
Fetal distress may occur when the baby doesn’t receive enough oxygen because of problems with the placenta (such as placental abruption or placental insufficiency) or problems with the umbilical cord (such as cord prolapse).
It is more common if you are overdue, have pregnancy complications or when there are other complications during labour. Sometimes it happens because the contractions are too strong or too close together.
Your baby is more likely to experience fetal distress if:
- you are obese
- you have high blood pressure in pregnancy or pre-eclampsia
- you have a chronic disease, such as diabetes, kidney disease or cholestasis(a condition that affects the liver in pregnancy)
- you have a multiple pregnancy
- your baby has fetal growth restriction
How is fetal distress diagnosed?
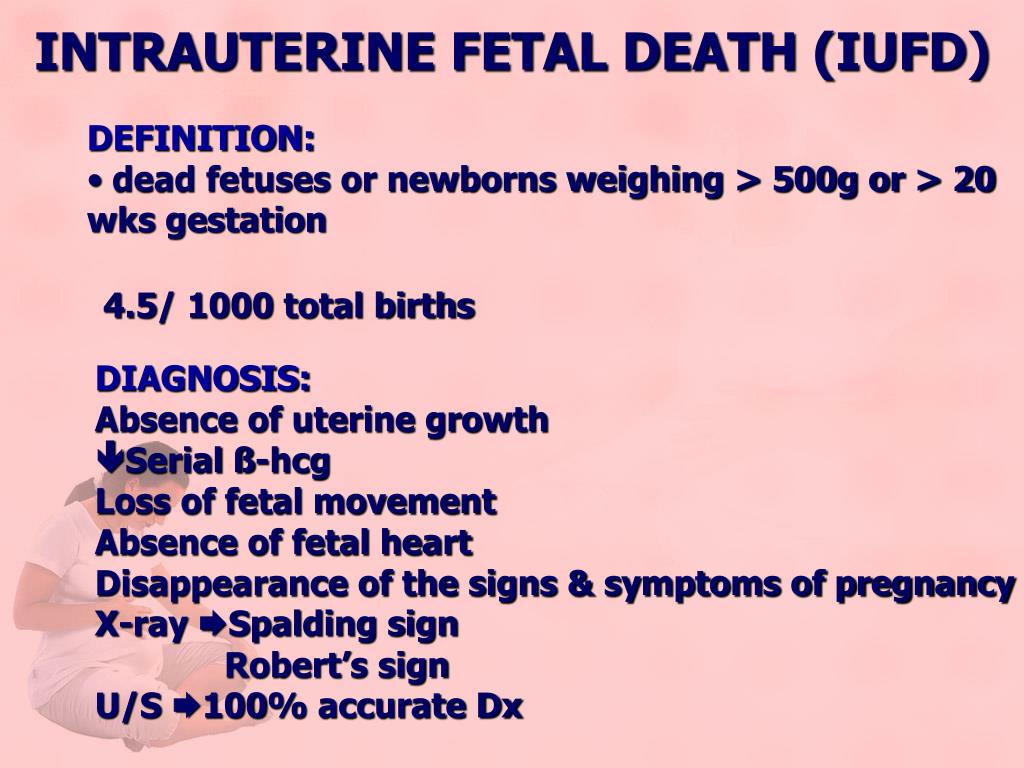
Fetal distress is diagnosed by monitoring the baby’s heart rate.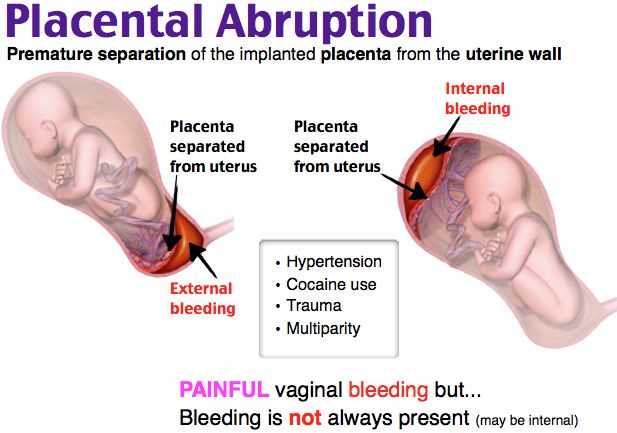 A slow heart rate, or unusual patterns in the heart rate, may signal fetal distress.
A slow heart rate, or unusual patterns in the heart rate, may signal fetal distress.
Your doctor or midwife might pick up signs of fetal distress as they listen to your baby’s heart during pregnancy.
Your baby’s movements are a sign that your baby is well. A change in your baby’s movements may be a sign of fetal distress.
If you haven’t felt your baby move, or the pattern of moments has changed, contact your doctor or midwife immediately, as this may be a sign of fetal distress.
Another sign of possible fetal distress is meconium in the amniotic fluid. Let your doctor or midwife know right away if your notice your amniotic fluid is green or brown, since this could signal the presence of meconium (newborn poo, that your baby may pass while still in your uterus if they are distressed).
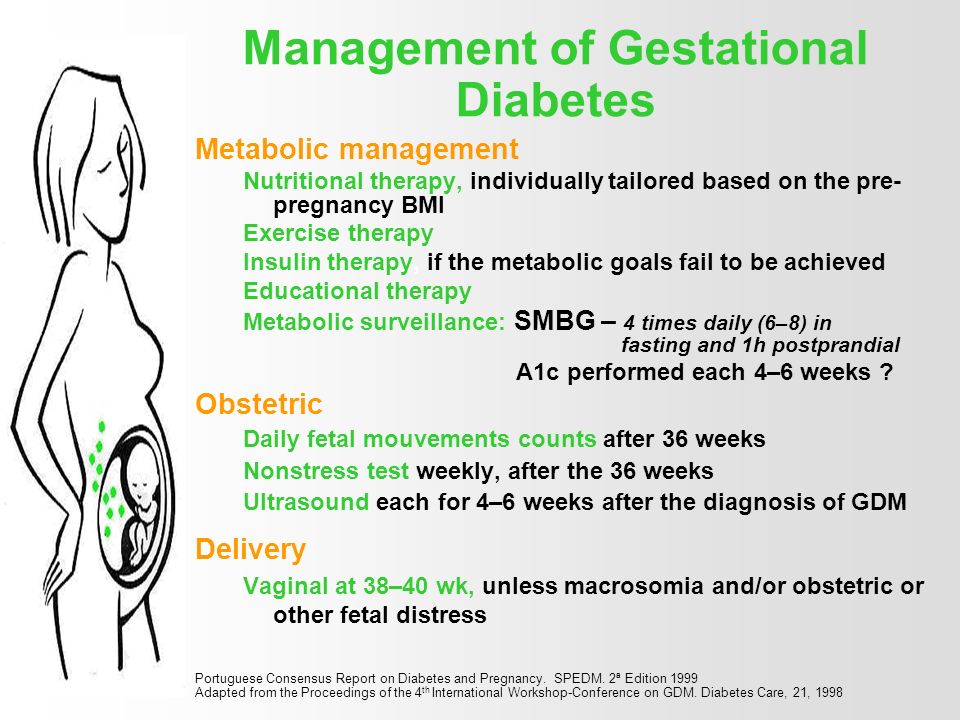
How is fetal distress managed?
There are a few ways that fetal distress may be managed. Your doctor will assess your situation and discuss with you the best management option in your situation.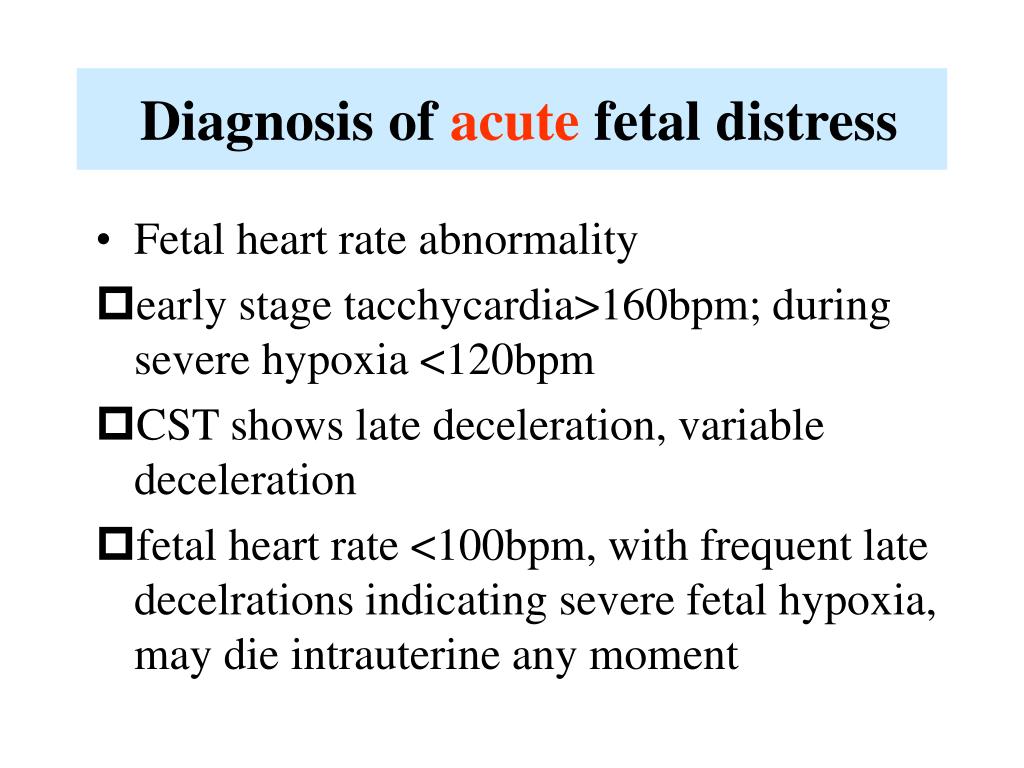
If you are not in labour
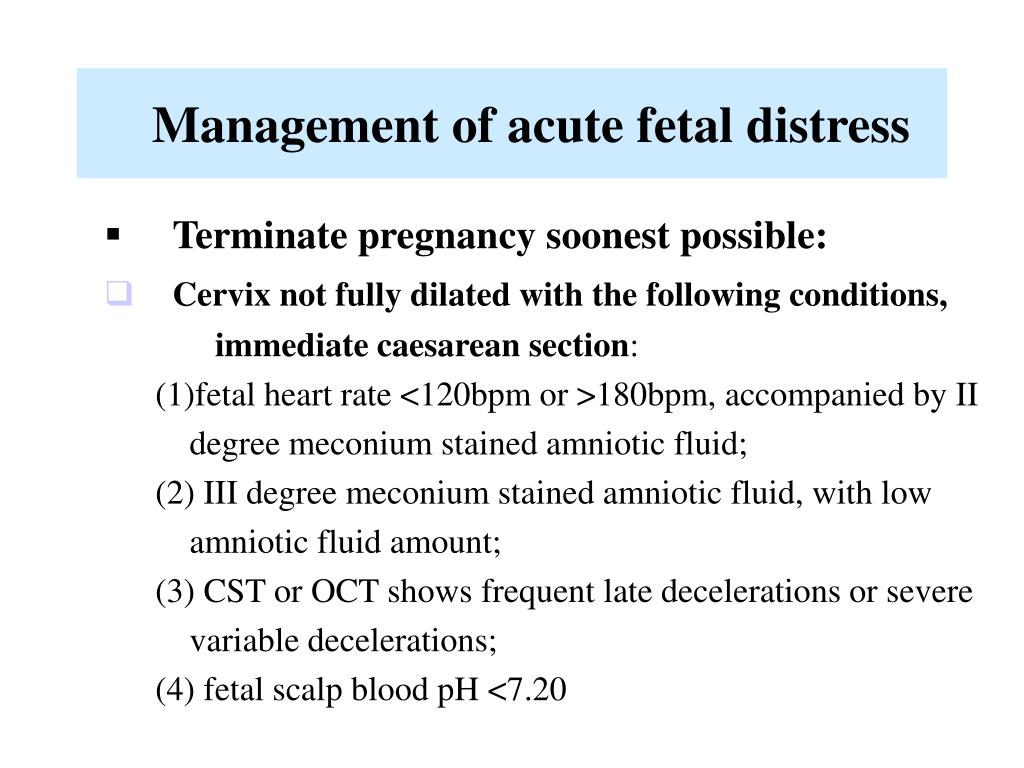
Depending on your situation, your doctor or midwife may recommend interventions such as medicines or intravenous fluids. If these interventions do not help, your doctor may recommend an emergency caesarean section so you birth your baby quickly.
If you are in labour
You will usually be given you oxygen and fluids. Sometimes changing position, such as turning onto your side, can reduce the baby’s distress.
You may be given medicine to slow down the contractions. If you had medicines to speed up labour, these may be stopped if there are signs of fetal distress.
Sometimes, a baby in fetal distress needs to be born quickly. Your doctor may recommend an assisted (or instrumental) birth or you might need to have an emergency caesarean.
Most of the time, there will be time to discuss your options with your doctor and/or midwife. However, in some emergency situations, your doctor or midwife will need to act quickly. If there are any medical interventions you object to, such as receiving a blood donation, it’s a good idea to make sure that your doctor and/or midwife are aware of this when you arrive at the hospital.
Does fetal distress have any lasting effects?
Babies who experience fetal distress are at greater risk of complications after birth. Prolonged lack of oxygen during pregnancy and birth can lead to serious complications for the baby, if it is not noticed and managed early. Complications may include brain injury, cerebral palsy and even stillbirth.
Fetal distress may require an assisted birth or caesarean section. While these interventions are safe, they are associated with their own set of risks and complications. Having fetal distress in one pregnancy doesn’t mean you will necessarily experience fetal distress in your next pregnancy. Every pregnancy is different. If you’re worried about future pregnancies, it can help to talk to your doctor or midwife so they can explain what happened before and during the birth.
Where can I find resources and support?
If your labour didn’t go to plan, you may experience difficult feelings about their birth experience.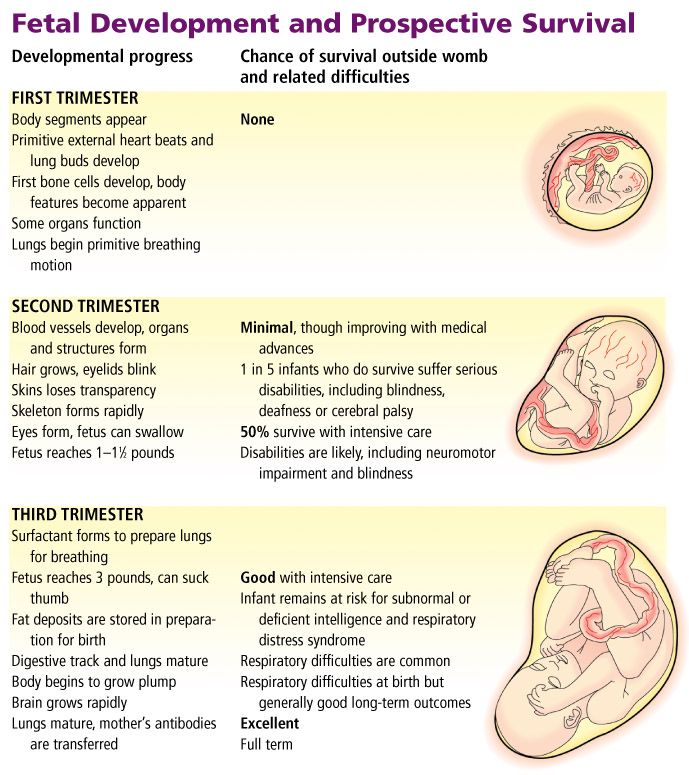
If you feel sad, disappointed or traumatised about what happened, it is important to talk to someone. There are lots of people and organisations who can help, including:
- your doctor
- PANDAon 1300 726 306
- Australasian Birth Trauma Association
- Beyond Blueon 1300 22 4636
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Australasian Birth Trauma Association (What is birth trauma?), King Edward Memorial Hospital (Fetal compromise (acute): Management if suspected), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Labour and birth), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Intrapartum fetal Surveillance Clinical Guideline)Learn more here about the development and quality assurance of healthdirect content.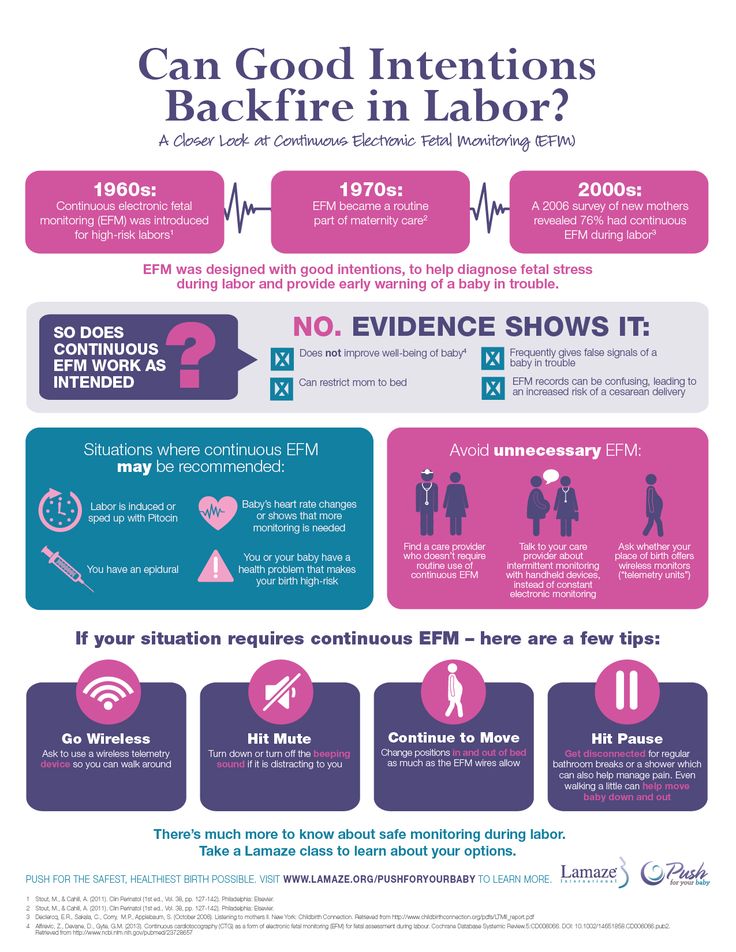
Last reviewed: July 2022
Back To Top
Related pages
- Labour complications
- Interventions during labour
- Induced labour
- Giving birth - stages of labour
- Fetal heart rate monitoring
- Baby movements during pregnancy
Need more information?
Fetal heart rate monitoring
During pregnancy and labour, your baby's heart rate is monitored to check for any signs of distress.
Read more on Pregnancy, Birth & Baby website
Monitoring the Baby’s Heart Rate in Labour
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website
Pregnant women not to trust smartphone heart rate apps
Pregnant women are being urged not to rely on smartphone apps that claim to listen to your baby's heartbeat.
Read more on Pregnancy, Birth & Baby website
Baby movements during pregnancy
Every baby is unique and it is important for you to get to know your baby’s movement patterns.
Read more on Pregnancy, Birth & Baby website
Heart abnormality birth defects - Better Health Channel
Some congenital heart defects are mild and cause no significant disturbance to the way the heart functions.
Read more on Better Health Channel website
Congenital heart defects - MyDr.com.au
Congenital heart defects are problems with the structure of the heart that are present from birth. The defects develop during pregnancy.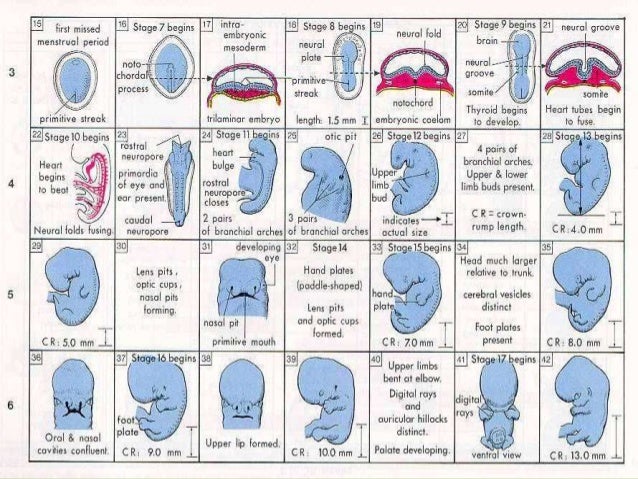 In Australia, as many as one baby in 100 is born with a heart defect.
In Australia, as many as one baby in 100 is born with a heart defect.
Read more on myDr website
Ultrasound scans during pregnancy
Ultrasound scans will help you and your doctors monitor your baby’s health throughout your pregnancy. Find out more, including about why you might need one.
Read more on Pregnancy, Birth & Baby website
External cephalic version (ECV)
ECV is a procedure to try to move your baby if they are in a breech position to the head-down position.
Read more on Pregnancy, Birth & Baby website
Preterm labour - MyDr.com.au
Going into labour before your 37th week of pregnancy is called preterm labour, or premature labour. Find out what it means for you and your baby.
Find out what it means for you and your baby.
Read more on myDr website
Having a small baby
It's normal for parents to worry about their baby's birth weight and growth. Here’s what you need to know if you have been told your baby is likely to be small (less than 2.5kg at birth).
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.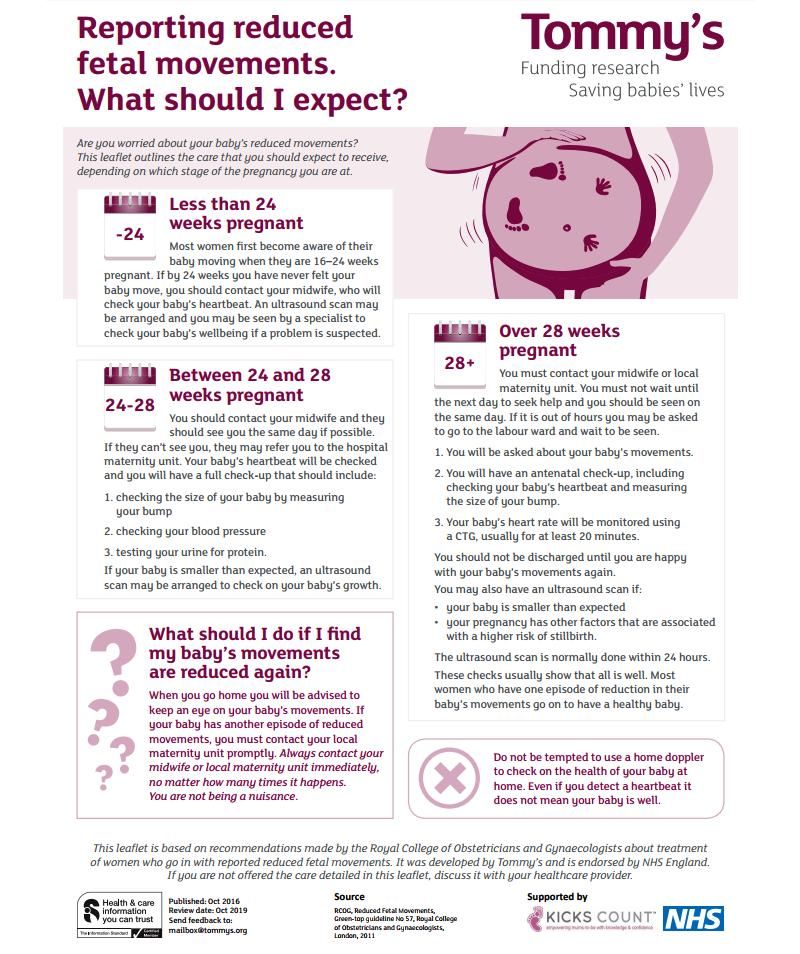
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.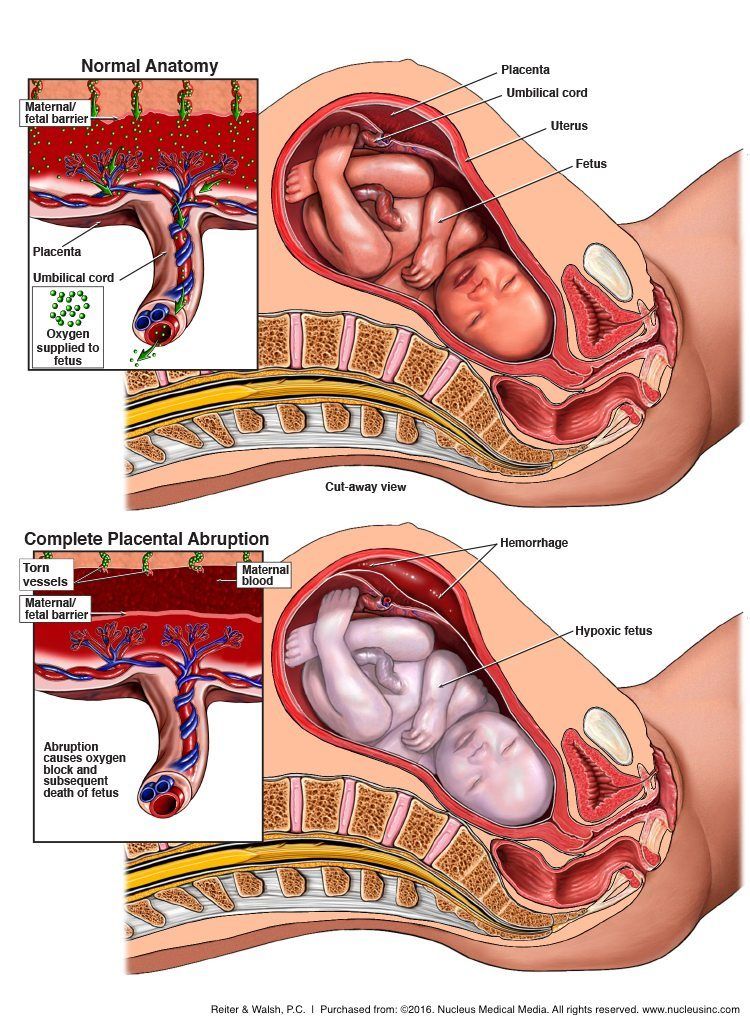
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Fetal Distress - American Pregnancy Association
Historically, the term fetal distress has been used to describe when the fetus does not receive adequate amounts of oxygen during pregnancy or labor. It is oftentimes detected through an abnormal fetal heart rate. However, while the term fetal distress is commonly used, it is not well defined. This makes it more difficult to make an accurate diagnosis and provide proper treatment. Because of the term’s ambiguity, its use has the potential to lead to improper treatment.
This makes it more difficult to make an accurate diagnosis and provide proper treatment. Because of the term’s ambiguity, its use has the potential to lead to improper treatment.
Fetal distress is commonly confused with the term birth asphyxia. Birth asphyxia occurs when the baby does not have adequate amounts of oxygen before, during, or after labor. This may have multiple causes, some of which include low oxygen levels in the mother’s blood or reduced blood flow due to compression of the umbilical cord.
As many have incorrectly used fetal distress and birth asphyxia as interchangeable terms, the Committee on Obstetric Practice of the American Congress of Obstetricians and Gynecologists (ACOG) has expressed concern regarding the use of the two terms. ACOG recommends that the term fetal distress be replaced with “non-reassuring fetal status.”
Along with this new term, ACOG further recommends physicians add to the diagnosis a list of additional findings such as fetal tachycardia, bradycardia, repetitive variable decelerations, low biophysical profile, and late decelerations. ACOG’s Committee on Obstetric Practice has also stated that the term birth asphyxia should no longer be used as it is too vague of diagnosis for medical use.
ACOG’s Committee on Obstetric Practice has also stated that the term birth asphyxia should no longer be used as it is too vague of diagnosis for medical use.
Fetal Distress Diagnosis
It is important for physicians to monitor the fetus throughout pregnancy to detect any potential complications. One of the more widely used methods of monitoring is electronic fetal heart rate (FHR) monitoring.
Benefits of FHR monitoring include:
- The ability to recognize the development of hypoxia (when the fetus does not receive adequate amounts of oxygen) by analyzing patterns in the fetal heart rate
- The ability to monitor the mother’s contractions
- The ability to monitor the response of the fetus to hypoxia
- A more positive outcome for high-risk deliveries
Nonetheless, FHR monitoring does come with risks as well, including an increased likelihood of having a cesarean section due to misinterpretation of FHR monitoring results.
Conditions Behind Fetal Distress
Potential precursors to fetal distress or non-reassuring fetal status may include:
- Anemia (the most prevalent obstetric condition seen behind non-reassuring fetal status)
- Oligohydraminos (a condition in which there is a lower level of amniotic fluid around the fetus)
- Pregnancy Induced Hypertension (PIH)
- Post-term pregnancies (42 weeks or more)
- Intrauterine Growth Retardation (IUGR)
- Meconium-stained amniotic fluid (a condition in which meconium, a baby’s first stool, is present in the amniotic fluid which can block fetal airways)
Treatment
The primary treatment used for non-reassuring fetal status is intrauterine resuscitation. This will help prevent any unnecessary procedures.
Some means of intrauterine resuscitation include:
- Changing the mother’s position
- Ensuring the mother is well-hydrated
- Ensuring the mother has adequate oxygen
- Amnioinfusion (the insertion of fluid into the amniotic cavity to alleviate compression of the umbilical cord)
- Tocolysis (a therapy used to delay preterm labor by temporarily stopping contractions)
- Intravenous hypertonic dextrose
Nonetheless, there are cases in which an emergency cesarean section is necessary.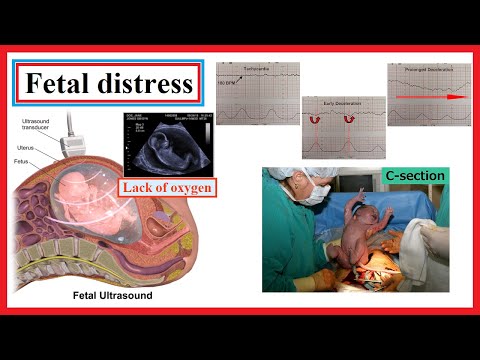 However, due to the over-diagnosis of fetal distress and potential misinterpretation of the fetal heart rate, it is recommended to confirm a potential fetal distress diagnosis with a fetal blood acid-base study. Overall, this condition points to the importance of prenatal care and proper monitoring of the mother and fetus throughout pregnancy.
However, due to the over-diagnosis of fetal distress and potential misinterpretation of the fetal heart rate, it is recommended to confirm a potential fetal distress diagnosis with a fetal blood acid-base study. Overall, this condition points to the importance of prenatal care and proper monitoring of the mother and fetus throughout pregnancy.
Want to Know More?
- Most Common Pregnancy Complications
- What is a High-Risk Pregnancy?
Compiled from the following References:
ACOG Committee on Obstetric Practice. (2005). Inappropriate use of the terms of fetal distress and birth asphyxia. Committee Opinion, 326.
Beckmann, C. R. B., Ling, F. W., Barzansky, B. M., Herbert, W. N. P., Laube, D. W., & Smith, R. P. (2010). Obstetrics and gynecology (6th ed.). Philadelphia, PA: Lippincott Williams & Wilkins.
Bucklin, B. A., Gambling, D. R., & Wlody, D. J. (2009). A practical approach to obstetric anesthesia.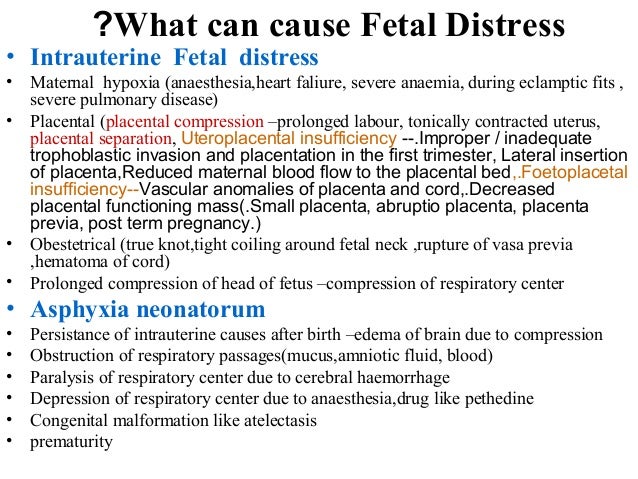 Gravlee, G. P. (Ed.). Philadelphia, PA: Lippincott Williams & Wilkins.
Gravlee, G. P. (Ed.). Philadelphia, PA: Lippincott Williams & Wilkins.
Kaur, J., & Kaur, K. (2012). Conditions behind fetal distress. Annals of Biological Research, 3(10). Retrieved from https://scholarsresearchlibrary.com/ABR-vol3-iss10/ABR-2012-3-10-4845-4851.pdf
Mayo Clinic. (2012). Biophysical profile: Why it’s done.
Merck Manuals. (n.d.) Fetal distress.
The American Congress of Obstetricians and Gynecologists (ACOG). (2013, October 22). Ob-gyns redefine the meaning of “term pregnancy.”
University of California San Francisco Benioff Children’s Hospital. (n.d.). Birth asphyxia. Retrieved from https://www.ucsfbenioffchildrens.org/conditions/birth_asphyxia/
Fetal distress - all you need to know about fetal distress
Sometimes at the last moment of pregnancy, unpleasant things happen that can be very sad. Fetal distress is one such complication that, if not addressed, can lead to problems for both the mother and the baby.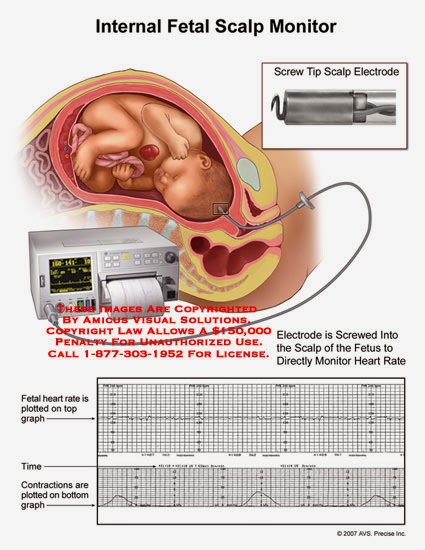
Fetal distress
Fetal distress is subdivided into intrauterine and birth distress. Distress is usually determined by monitoring the child's heart rate. The presence of meconium (the baby's first stool) may also indicate that the fetus is unwell in the womb. nine0003
Often referred to as hypoxia or threatened asphyxia, fetal distress occurs when an infant does not receive enough oxygen in the womb or during labor.
What causes fetal distress?
The reason why your unborn baby faces the problem of lack of oxygen can be different. These could be umbilical cord problems, fetal abnormalities, the stress of childbirth, or reactions to certain medications. This can happen due to abnormal fetal development, problems with the placenta, or even multiple births. nine0003
Fetal monitoring during labor
When a pregnant woman gives birth, the baby is constantly monitored.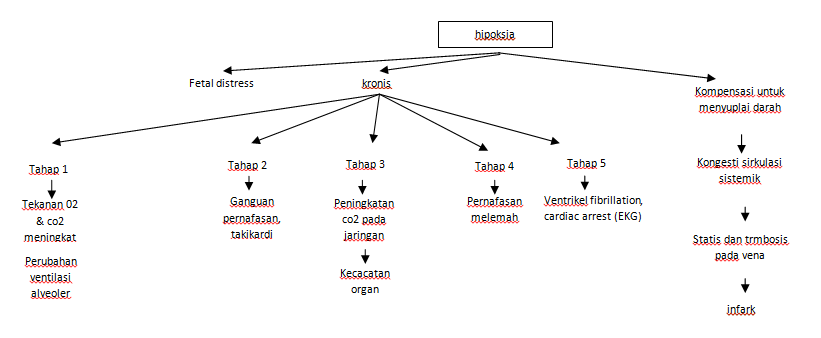 One of the most common methods for monitoring a baby is the use of an electronic fetal monitor (EFM). In this technique, two straps are wrapped around the abdomen, one measures the baby's heart rate, and the other assesses contractions or uterine activity. Monitors are also used to determine if the baby is having problems with each contraction. nine0003
One of the most common methods for monitoring a baby is the use of an electronic fetal monitor (EFM). In this technique, two straps are wrapped around the abdomen, one measures the baby's heart rate, and the other assesses contractions or uterine activity. Monitors are also used to determine if the baby is having problems with each contraction. nine0003
For monitoring, doctors may also use a device that is applied to the baby's scalp.
What should be the ideal fetal heart rate?
The results of the electronic fetal monitor are shown on the monitor in diagrammatic form. The doctor and nurses constantly monitor the numbers on the graphs and check if the heart rate is within adequate parameters. The ideal range should be between 110 and 160 beats per minute. nine0003
A temperature that is too high may indicate that the child is unwell or has a fever. While too low a temperature "speaks" of a lack of oxygen. Monitoring divides indications into 2 categories: accelerated heartbeat and slow heartbeat.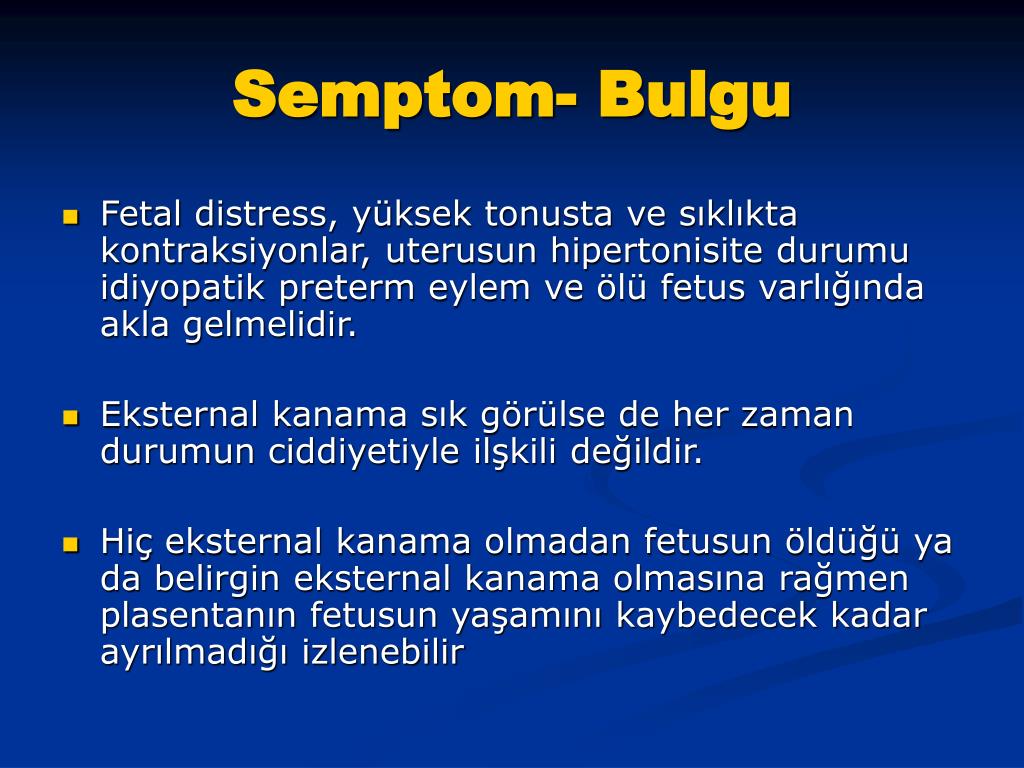
Rapid heartbeat
This means a short-term increase in heart rate, say 15 beats per minute, which can last 15 seconds or more. Accelerated, quite normal, it indicates an abundance of oxygen. For most babies, the heartbeat can speed up several times during the entire birth process. nine0003
If the doctor has any suspicions that the fetus is deteriorating, he may cause an increase in the fetal heart rate. Suspicion may arise from:
- Gently touching the mother's abdomen
- As a result of pressing the child's head, with a finger, through the cervix
Slow heart rate
Slow refers to temporary drops in heart rate. It can be divided into three types:
1. Early Deceleration
This is usually normal and nothing to worry about. Early deceleration occurs when the baby's head contracts. It mostly happens in the later stages of labor as the baby descends through the birth canal.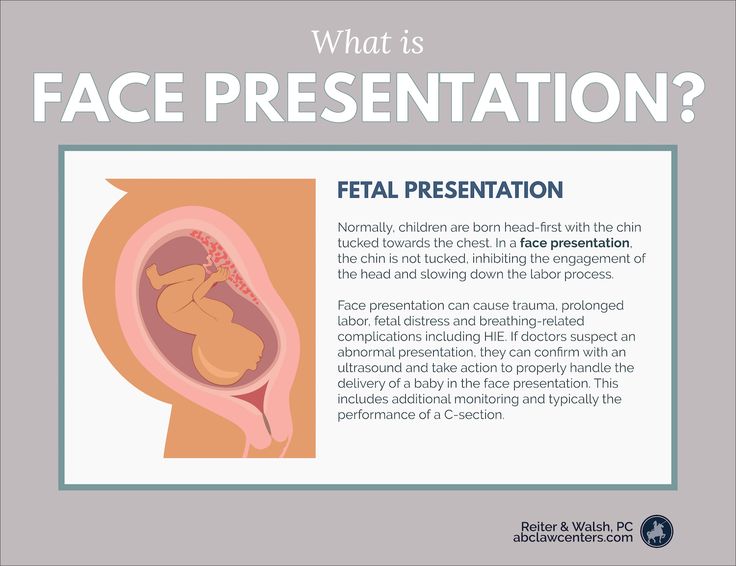 Sometimes this happens during childbirth when the baby is premature or in a state of breech presentation.
Sometimes this happens during childbirth when the baby is premature or in a state of breech presentation.
2. Late Deceleration
They only happen when contractions are at their peak. Typically, late slows are smooth and shallow dips in heart rate that reflect the contraction that causes them. As long as the baby's heart rate shows an accelerated rhythm, late slowdowns are not a cause for concern. Late decelerations can also be a sign that the baby is not getting the amount of oxygen it needs.
3. Variable Deceleration
Variable decelerations are sudden dips in the fetal heart rate that can lead to serious consequences. These slowdowns mostly occur during childbirth when the umbilical cord temporarily contracts, indicating a decrease in blood flow. Such variable changes in heart rate can be unsafe.
What to expect from a medical team?
In principle, the procedure for monitoring a child's heart rate is often painless.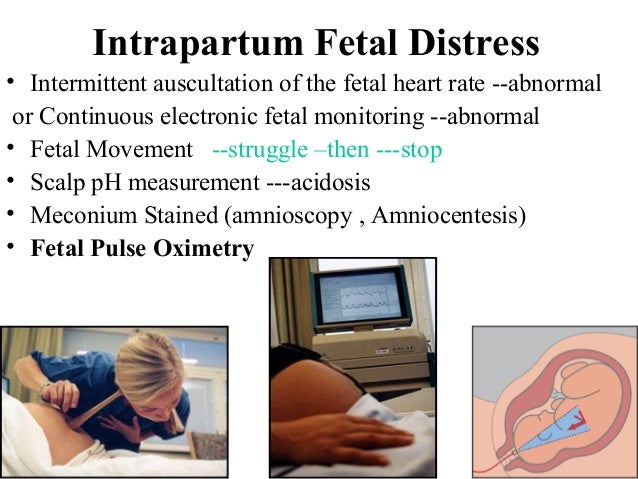 However, there are several risks associated with difficult birth situations that result in the medical team doing the following:
However, there are several risks associated with difficult birth situations that result in the medical team doing the following:
- Oxygen supply to mother
- Instillation of fluid into the amniotic sac to thicken the meconium (Amnioinfusion is the infusion of Ringer's solution or normal saline into the amniotic sac using a catheter.)
- Instrumentation (forceps/vacuum)
- Caesarean section
Before giving birth, be sure to consult with your doctor, ask him all the necessary and interesting questions. Get your medical card. And go to birth!!! nine0003
And remember, vigilance is the Key to a successful birth of your baby!!!
Distress of the fetus during childbirth: acute, respiratory, prevention
Complain
Updated 3
Content:
Disadvantage of oxygen in the fetus during the fetal
Distress Dytraz during birth
9 9Causes of fetal distress and management of labor
Consequences
Video
Fetal distress can occur both during pregnancy and during childbirth.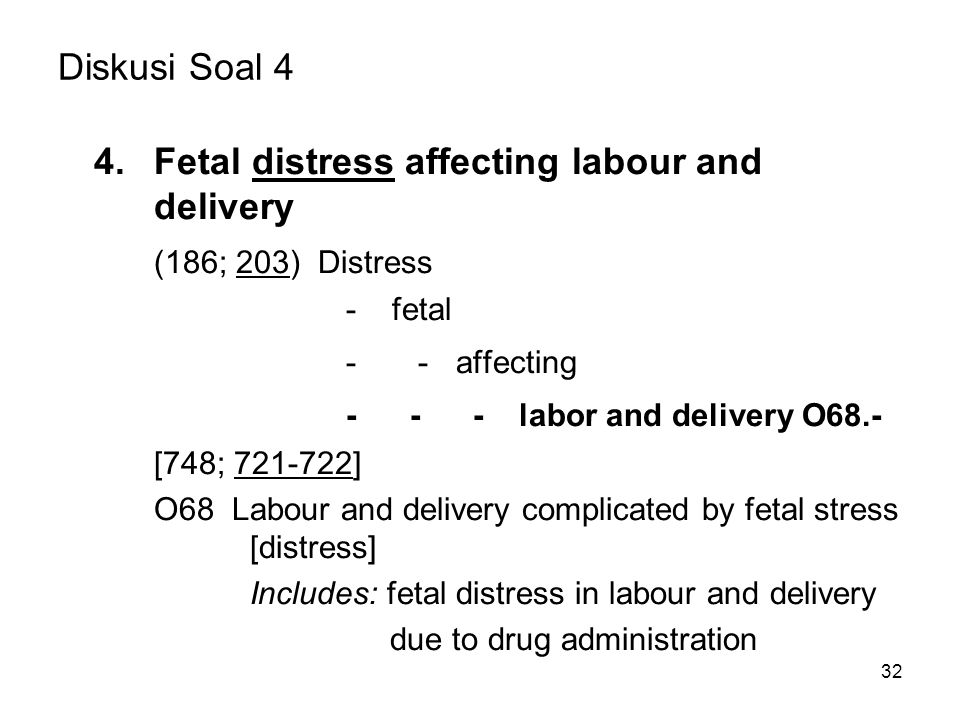 This general term refers to violations of the functional state of the fetus during pregnancy and / or childbirth. Separately, respiratory (respiratory) distress of the fetus associated with a lack of oxygen is isolated.
This general term refers to violations of the functional state of the fetus during pregnancy and / or childbirth. Separately, respiratory (respiratory) distress of the fetus associated with a lack of oxygen is isolated.
Fetal oxygen deficiency during pregnancy
Location of the fetus during pregnancyFetal distress is often synonymous with fetal hypoxia.
The mechanism of development of such a respiratory pathology is as follows:
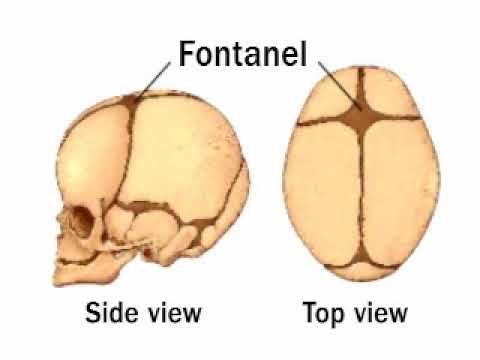
- The production of surfactant (a fluid that lubricates the alveoli) in the fetus begins after 20 weeks, and the respiratory system is fully mature almost before the birth itself.
- In case of pathologies in the mother or problems during pregnancy, there may be a deficiency in the production of surfactant or its insufficient activity. nine0061
- Problems with surfactant lead to edema, decreased lung capacity in the child, and breathing problems.
The condition is diagnosed in several ways:
- Listening to cardiac activity.
 Manipulation is carried out starting from the 20th week of pregnancy, when the gynecologist can listen to the fetal heartbeat through the mother's stomach during regular examinations. The normal heart rate is considered to be 110-170 beats per minute. Deviation in the direction of increasing or decreasing the number of strokes may be a sign of oxygen deficiency. nine0061
Manipulation is carried out starting from the 20th week of pregnancy, when the gynecologist can listen to the fetal heartbeat through the mother's stomach during regular examinations. The normal heart rate is considered to be 110-170 beats per minute. Deviation in the direction of increasing or decreasing the number of strokes may be a sign of oxygen deficiency. nine0061 - Biophysical profile assessment. The procedure is carried out from the 30th week of pregnancy and includes the evaluation of several indicators, each of which is estimated from 0 to 2 points. The resulting total value gives an understanding of the degree of development of the fetus and allows you to suspect violations in time. The following parameters are taken for evaluation: physical activity, respiration, cardiac activity, volume of amniotic fluid. An oxygen deprivation syndrome can be suspected with a score below 7 points. nine0061
- Doppler. Evaluation of blood flow makes it possible to evaluate the work of the placenta.
Pathological is a condition with slow blood flow, zero or reverse.
Fetal distress during birth
The process of childbirth is physically very difficult for both mother and baby. During the entire birth process, starting from admission to the hospital, doctors constantly monitor the condition of the child. To do this, they evaluate the heart rate and other parameters. It is very important to carefully and regularly monitor the child's condition in order to suspect hypoxia in a timely manner and take measures to save the baby's life. nine0003
Signs of oxygen deprivation during childbirth may include:
- heartbeat above 170 and below 110 beats per minute, except for the moment of uterine contraction;
- pathological color of amniotic fluid.
When in doubt, examinations are carried out in more detail, for which the heartbeat is heard with the help of auscultation, as well as cardiotocography. A significant deviation from the norm and diagnosed fetal hypoxia are an indication for emergency delivery. If the problem is discovered in the second stage of labor, a caesarean section becomes impossible, but the process of having a baby is accelerated. For this, a vacuum extraction of the fetus or the use of obstetric forceps is performed. nine0003
A significant deviation from the norm and diagnosed fetal hypoxia are an indication for emergency delivery. If the problem is discovered in the second stage of labor, a caesarean section becomes impossible, but the process of having a baby is accelerated. For this, a vacuum extraction of the fetus or the use of obstetric forceps is performed. nine0003
Such methods are quite risky and can have unpredictable consequences, so it is important to detect hypoxia in time and prevent its occurrence.
Causes of fetal distress and management of labor
Intrauterine hypoxia cannot be visually identified, so the condition is assessed by clinical signs. Emergency measures must be taken if the child's condition is dangerous for the development of persistent pathologies or can lead to death. nine0003
Oxygen deficiency can be triggered by the following intranatal factors:
- induction of labor if deemed necessary by the physician;
- preeclampsia
- prolonged delivery;
- meconium admixture;
- oligohydramnios.
Other precipitating factors may be:
- maternal endocrine disorders; nine0061
- multiple pregnancy;
- presence of infection;
- Rhesus conflict.
If there is an abnormal heartbeat, the gynecologist may puncture the amniotic sac to assess the condition and color of the amniotic fluid. If they are stained with meconium, an emergency cesarean is performed.
If the mother's heartbeat is normal, but the fetus is elevated in the absence of a contraction, this is a sure sign of hypoxia. To eliminate hypoxia, the following preventive measures can be used:
- stop oxytocin administration;
- put the woman on her left side;
- use an oxygen mask.
Extra fluid may also be given intravenously.
Consequences
Intranatal distress even in utero causes oxygen deficiency, metabolic acidosis and adversely affects the respiratory and nervous system of the child. After birth, these children have:
After birth, these children have:
- acute respiratory syndrome with respiratory failure;
- retraction of the chest on inspiration;
- cyanosis of the skin and mucous membranes, their blanching;
- crepitus.
To avoid serious consequences, doctors begin treatment immediately after the baby is born. Measures taken in the first hour can reduce the severity of manifestations, prevent disability and improve the quality of life of the baby. nine0003
Prophylaxis, if at risk, should be carried out throughout pregnancy. To do this, a woman may be prescribed drugs that improve oxygenation. It is important to visit the doctor in charge of the pregnancy in a timely manner and carefully follow his appointments.
videos
Read the following article: Vacuum Fetal Extraction
* The information provided cannot be used for self-diagnosis, treatment determination and does not replace a visit to a doctor!
RubricExaminations, analyzes
HCG during a missed pregnancy - does the hormone level change
The size of the uterus in women is normal
Optimism is a magnet of happiness.