What causes strep b
Group B strep disease - Symptoms and causes
Overview
Group B strep (streptococcus) is a common bacterium often carried in the intestines or lower genital tract. The bacterium is usually harmless in healthy adults. In newborns, however, it can cause a serious illness known as group B strep disease.
Group B strep can also cause dangerous infections in adults with certain chronic medical conditions, such as diabetes or liver disease. Older adults are at increased risk of illness due to group B strep, too.
If you're a healthy adult, there's nothing you need to do about group B strep. If you're pregnant, get a group B strep screening test during your third trimester. If you have group B strep, antibiotic treatment during labor can protect your baby.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
Infants
Most babies born to women carrying group B strep are healthy. But the few who are infected by group B strep during labor can become critically ill.
In infants, illness caused by group B strep can be within six hours of birth (early onset) — or weeks or months after birth (late onset).
Signs and symptoms might include:
- Fever
- Low body temperature
- Difficulty feeding
- Sluggishness, limpness or weak muscle tone
- Difficulty breathing
- Irritability
- Jitteriness
- Seizures
- Rash
- Jaundice
Adults
Many adults carry group B strep in their bodies — usually in the bowel, vagina, rectum, bladder or throat — and have no signs or symptoms.
In some cases, however, group B strep can cause a urinary tract infection or other more-serious infections. Signs and symptoms of infections that may be caused by group B strep include the following.
Urinary tract infection
- A strong, persistent urge to urinate
- A burning sensation or pain when urinating
- Passing frequent, small amounts of urine
- Urine that appears red, bright pink or cola colored — a sign of blood in the urine
- Pelvic pain
Blood infection (bacteremia)
- Fever
- Chills
- Confusion or lack of alertness
Pneumonia
- Fever
- Chills
- Cough
- Shortness of breath
- Chest pain when you breathe or cough
Skin or soft-tissue infection
- Swelling, warmth or redness in the area of the infection
- Pain in the area of the infection
- Lesions with pus or drainage
Bone or joint infection
- Fever
- Chills
- Swelling, warmth or redness over the area of the infection
- Pain in the area of the infection
- Stiffness or inability to use a limb or joint
When to see a doctor
If you have signs or symptoms of group B strep infection — particularly if you're pregnant, you have a chronic medical condition or you're older than 65 — contact your doctor right away.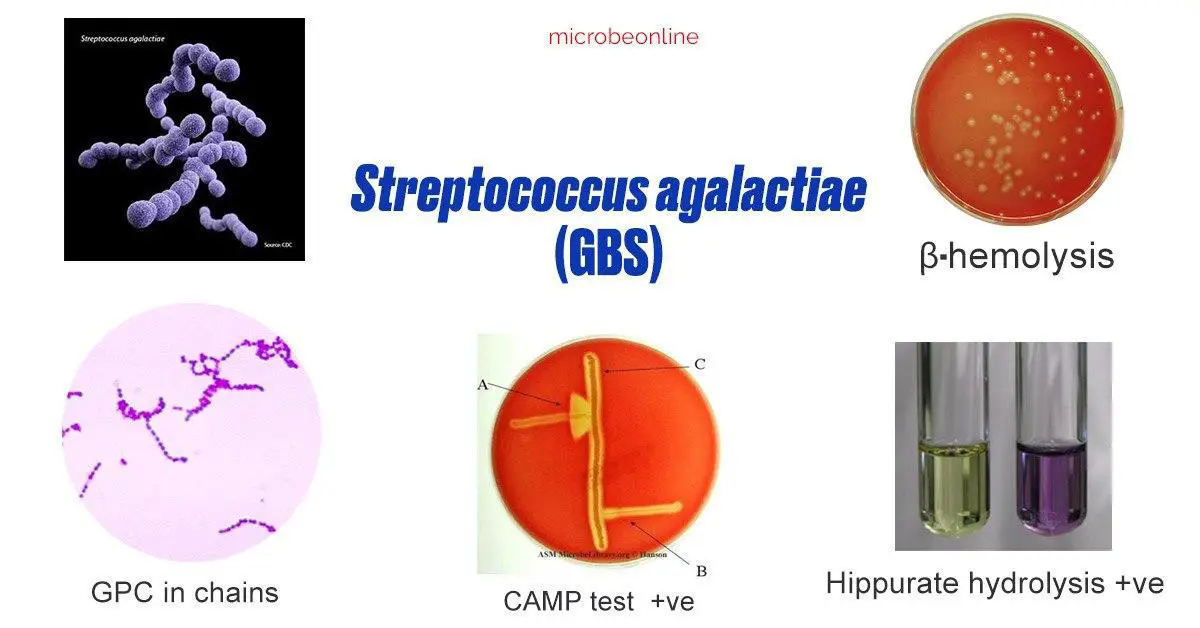
If you notice your infant has signs or symptoms of group B strep disease, contact your baby's doctor immediately.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices.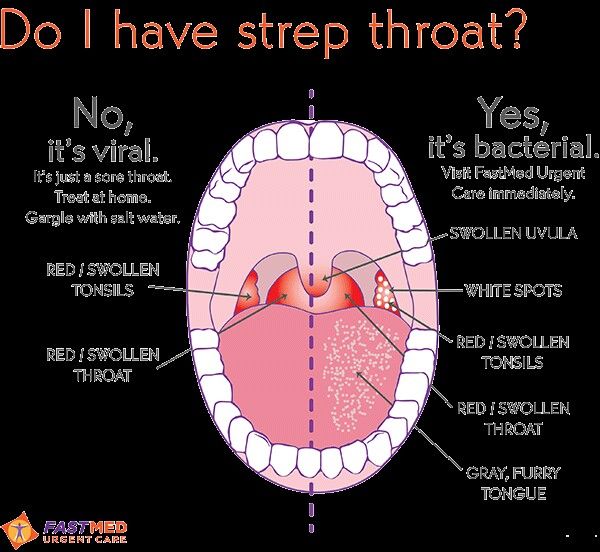 You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
Many healthy people carry group B strep bacteria in their bodies. You might carry the bacteria in your body for a short time — it can come and go — or you might always have it. Group B strep bacteria aren't sexually transmitted, and they're not spread through food or water. How the bacteria are spread to anyone other than newborns isn't known.
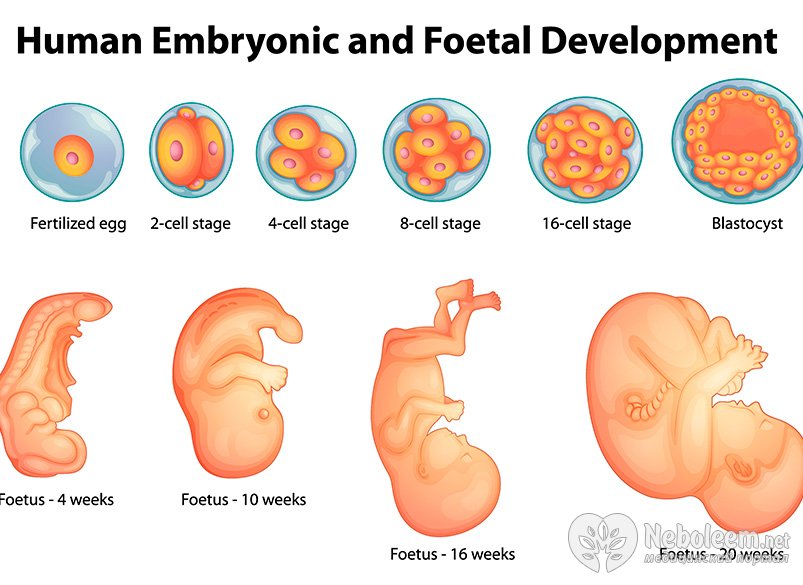
Group B strep can spread to a baby during a vaginal delivery if the baby is exposed to — or swallows — fluids containing group B strep.
Risk factors
Infants
An infant is at increased risk of developing group B strep disease if:
- The mother carries group B strep in her body
- The baby is born prematurely (earlier than 37 weeks)
- The mother's water breaks 18 hours or more before delivery
- The mother has an infection of the placental tissues and amniotic fluid (chorioamnionitis)
- The mother has a urinary tract infection during the pregnancy
- The mother's temperature is greater than 100.
 4 F (38 C) during labor
4 F (38 C) during labor - The mother previously delivered an infant with group B strep disease
Adults
Adults age 65 and older are at increased risk of group B strep. You're also at increased risk of if you have a condition that impairs your immune system or other serious diseases, including the following:
- Diabetes
- HIV infection
- Liver disease
- Heart disease
- Cancer or history of cancer
Complications
Group B strep infection can lead to life-threatening disease in infants, including:
- Pneumonia
- Inflammation of the membranes and fluid surrounding the brain and spinal cord (meningitis)
- Infection in the bloodstream (bacteremia)
If you're pregnant, group B strep can cause the following:
- Urinary tract infection
- Infection of the placenta and amniotic fluid (chorioamnionitis)
- Infection of the membrane lining the uterus (endometritis)
- Bacteremia
If you're an older adult or you have a chronic health condition, group B strep bacteria can lead to any of the following conditions:
- Skin infection
- Bacteremia
- Urinary tract infection
- Pneumonia
- Bone and joint infections
- Infection of the heart valves (endocarditis)
- Meningitis
Prevention
If you're pregnant, the American College of Obstetricians and Gynecologists recommends a group B strep screening during weeks 36 to 37 of pregnancy. Your doctor will take swab samples from your vagina and rectum and send them to a lab for testing.
Your doctor will take swab samples from your vagina and rectum and send them to a lab for testing.
A positive test indicates that you carry group B strep. It doesn't mean that you're ill or that your baby will be affected, but that you're at increased risk of passing the bacteria to your baby.
To prevent group B bacteria from spreading to your baby during labor or delivery, your doctor can give you an IV antibiotic — usually penicillin or a related drug — when labor begins.
If you're allergic to penicillin or related drugs, you might receive clindamycin or vancomycin as an alternative. Because the effectiveness of these alternatives is not well understood, your baby will be monitored for up to 48 hours.
Taking oral antibiotics ahead of time won't help because the bacteria can return before labor begins.
Antibiotic treatment during labor is also recommended if you:
- Have a urinary tract infection
- Delivered a previous baby with group B strep disease
- Develop a fever during labor
- Haven't delivered your baby within 18 hours of your water breaking
- Go into labor before 37 weeks and haven't been tested for group B strep
Vaccine in development
Although it's not available yet, researchers are working on a group B strep vaccine that could help prevent group B strep infections in the future.
By Mayo Clinic Staff
Related
Products & Services
Group B Strep - Affects 25% of Health Pregnant Women
What is group B strep?
Group B streptococcus, or group B strep for short, is a common kind of bacteria (germ). It can live in the intestine, the rectum, or a woman’s vagina. Group B strep doesn’t usually cause problems in healthy adults. Most of the people who get sick from group B strep are newborns who are exposed to the bacteria during birth.
About 25% of healthy pregnant women have group B strep in their bodies. A woman who has group B strep is said to be “colonized” with this germ. If you are colonized with group B strep, your baby can become infected with these germs while being born and can get sick. There is less than a 1% chance that this will happen. But because group B strep infection is so dangerous for babies, it’s important to find out if you’re colonized while you’re pregnant.
Symptoms of group B strep
Group B strep doesn’t usually cause symptoms in healthy adults.
Babies who have group B strep may develop symptoms during their first week of life. This is called early-onset disease. Or they may develop symptoms from 1 week to 3 months of life. This is called late-onset disease.
The symptoms of group B strep infection in newborns may include:
- Fever
- Difficulty feeding
- Lethargy (the baby is tired, hard to wake up, limp, or inactive)
- Difficulty breathing (with severe breathing problems, the baby’s skin, lips, or nails may turn blue)
If you notice these symptoms in your newborn, call your doctor right away.
What causes group B strep?
The group B strep bacteria come and go naturally in people’s bodies. If a pregnant woman has the bacteria in her body, she can pass it to her baby during labor and delivery. A group B strep infection happens when a baby is exposed to the bacteria while it’s being born. The bacteria can cause the baby to get sick. The most common illnesses caused by the bacteria in newborns are:
- Pneumonia (infection in the lungs)
- Meningitis (infection of the tissue covering the brain and spinal cord)
- Bacteremia or sepsis (infection in the blood)
There are some factors that increase a pregnant woman’s risk of having a baby who develops group B strep disease. These include:
These include:
- Testing positive for the bacteria late in pregnancy (35-37 weeks)
- Having the bacteria found in your urine anytime during your pregnancy
- Having the baby early (before 37 weeks)
- Developing a fever during labor
- Going a long time between when your water breaks and when you deliver (18 hours or more)
- Having had a baby before who developed group B strep disease
How is group B strep diagnosed?
If you’re pregnant, your doctor can do a test to see if you are “group B strep positive.” This test usually is done when you are 35 to 37 weeks pregnant. To perform the test, your doctor will swab your vagina and your rectum and will send the swabs to a lab to see if the strep bacteria grow.
If you have group B strep, it’s important to understand that you aren’t sick. Also, you probably will not make your baby sick. Knowing that you carry the bacteria just helps you and your doctor make decisions that can protect your baby from infection.
Can group B strep be prevented or avoided?
Pregnant women can’t avoid having group B strep in their bodies. But passing it along to their babies is preventable. The two ways to prevent your baby from getting an early-onset group B strep infection is to:
- Get tested for the bacteria late in pregnancy (35-37 weeks).
- Get antibiotics during labor and delivery if you are at increased risk. This includes women who tested positive for the bacteria.
Currently there is not a way to prevent your baby from getting late-onset group B strep disease.
Group B strep treatment
If you test positive for group B strep or are at increased risk of having it, your doctor will give you antibiotics during labor. These will be given intravenously (through an IV) to kill the germs. Because the bacteria grow quickly, the antibiotics are only effective if they are given during labor. Penicillin is the most common antibiotic that doctors prescribe to treat group B strep.
If you get antibiotics while you’re in labor, the chances are very good that your baby won’t get an early-onset group B strep infection.
What if my baby has group B strep?
If your baby gets group B strep, he or she will be treated with IV antibiotics to kill the bacteria. Your baby will stay in the hospital until your doctor is sure your baby is better.
Living with group B strep
In healthy adults, group B strep doesn’t usually cause any problems. Certain groups are more likely to have complications from group B strep:
- Infants who have group B strep can develop serious or life-threatening infections, such as meningitis, pneumonia, or sepsis.
- Some pregnant women who have group B strep may develop an infection of the urinary tract (also called a UTI), placenta, amniotic fluid, or bloodstream.
- Older adults and people who have a chronic illness or a weak immune system are more likely to develop problems due to group B strep infection.
 These problems may include infections of the skin, bloodstream, urinary tract, lungs, bones and joints, heart valve (called endocarditis), or the fluid around the brain and spinal cord.
These problems may include infections of the skin, bloodstream, urinary tract, lungs, bones and joints, heart valve (called endocarditis), or the fluid around the brain and spinal cord.
Questions to ask your doctor
- Is testing for group B strep infection a standard part of my prenatal care?
- When should I schedule the test?
- What do my test results mean?
- If I have group B strep, how do we keep my baby from getting it too?
- Will I need antibiotics? Are they safe for the baby?
- Will I need a C-section, or can I still deliver my baby vaginally?
Resources
Centers for Disease Control and Prevention, Group B Strep (GBS)
diagnosis and treatment - symptoms and prevention for adults and children
Each infectious disease has pathogens - pathogenic or opportunistic microorganisms. The former invade the body from the outside, the latter belong to a small part of the natural microflora and are activated only under favorable conditions for reproduction.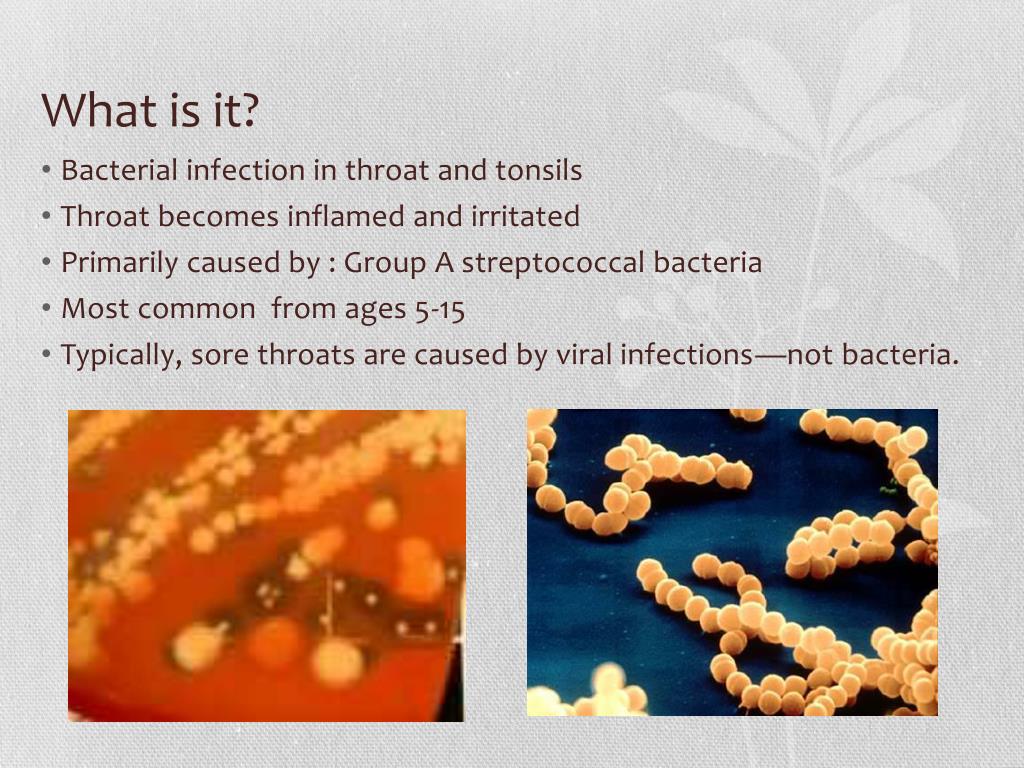
The etiology of infection is determined by its belonging to the group - viruses, bacteria, protozoan microorganisms, fungi, worms or protozoan parasites. Among a large number of bacteria, streptococci are especially dangerous. They provoke severe pathologies - up to toxic shock with a high probability of death. We will talk about the features of streptococcal infection, methods of treatment and prevention in the article. nine0003
Streptococcal infections
The source of infection is an infected child or adult. Ways of transmission of streptococcus:
- aerogenic - during close contact with a sick person, including asymptomatic carriage of the infection;
- food - through contaminated food - dairy, sour-milk products;
- contact-household - through objects contaminated with bacteria;
- intranatal - if the woman's reproductive system is affected by a streptococcal infection. nine0014
Due to the high contagiousness of pathogens, there is a risk of an epidemic among socially organized children.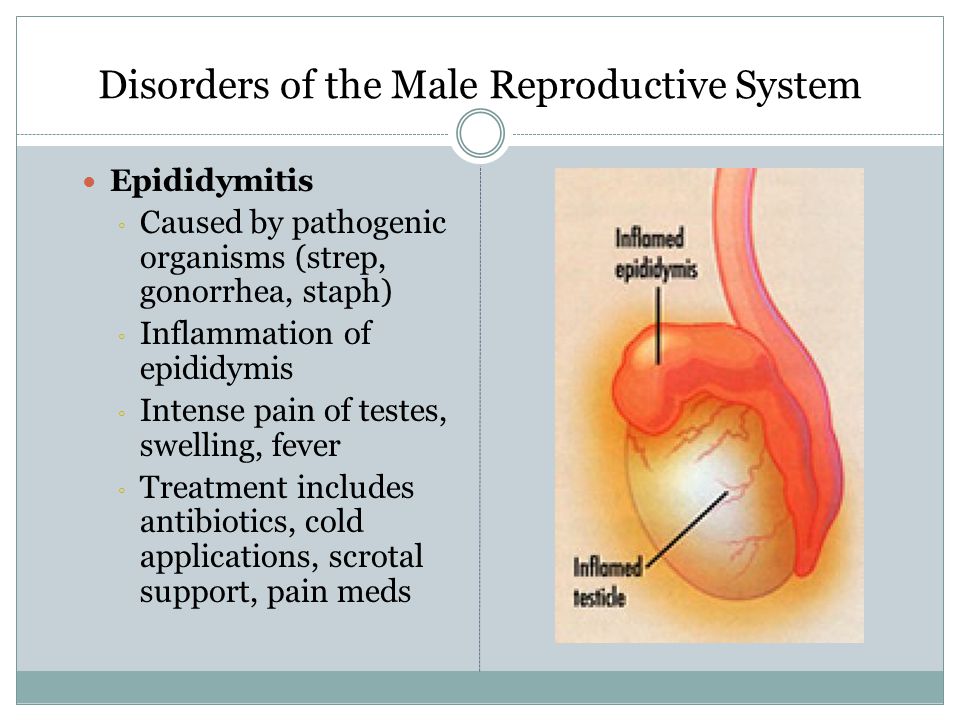
Classification of streptococci
Streptococcus is a gram-positive bacterium of a facultative aerobic species. In a meager amount, they live on the skin, in the gastrointestinal tract, on the mucous membranes of the mouth and organs of the genitourinary system. The bacterial family has 83 representatives. Cause-significant are:
- A-hemolytic Streptococcus - causes purulent infections, inflammatory pathologies of the heart, pneumococcal pneumonia. nine0014
- B-hemolytic Streptococcus - includes five groups of dangerous pathogens (A, B, C, D, F, G). Group A Streptococcus pyogenes is considered the most active, provoking diseases of the ENT organs, the respiratory system, acute inflammation of the heart, kidneys, and hard-to-treat skin lesions.
Bacteria are quite resistant to environmental factors. They withstand temperatures up to 60 ℃, within a quarter of an hour they are able to withstand antiseptics, sanitizers. In dried sputum, pus remains viable for several months.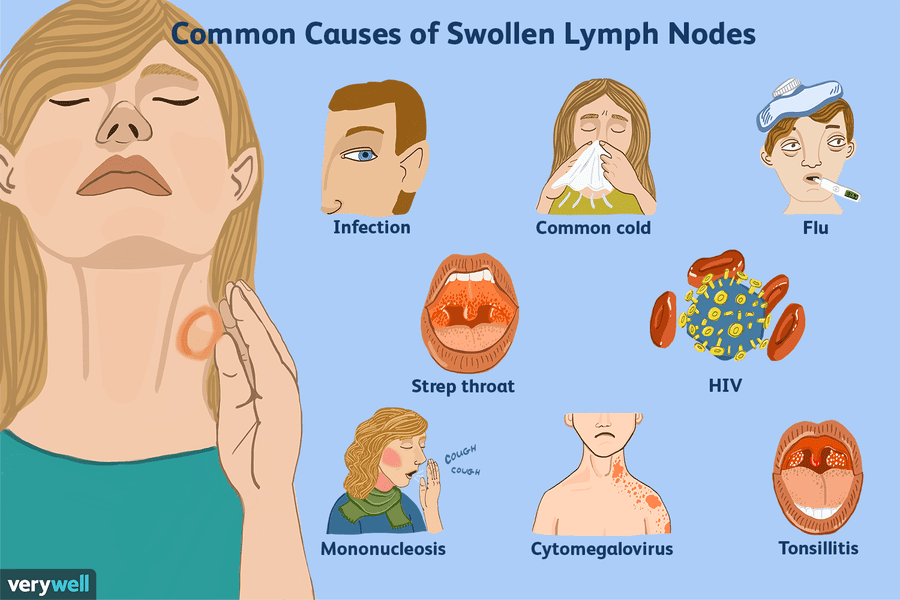 nine0003
nine0003
Virulence factors
Streptococci are characterized by high virulence - the ability to quickly capture and destroy the attacked organism. The main factors are the ability of microorganisms to:
- promptly colonize and disseminate;
- bypass immune defenses;
- instantly bind to specific receptors for entry into the cells of the body.
Pathogens produce substances that destroy tissues, as well as exotoxins, which provoke the development of a cytokine storm. This is the main cause of toxic shock and death. Penetrating through the mucous membranes of the oropharynx or lesions on the skin, the pathogen forms a bacterial-active focus, which includes conditionally pathogenic microflora. Streptococci secrete toxic substances into the blood, causing a systemic immune response - the release of cytokines, histamine, the synthesis of immunoglobulins. With a significant bacterial load, weakened immunity, the body cannot give the pathogen a worthy rebuff.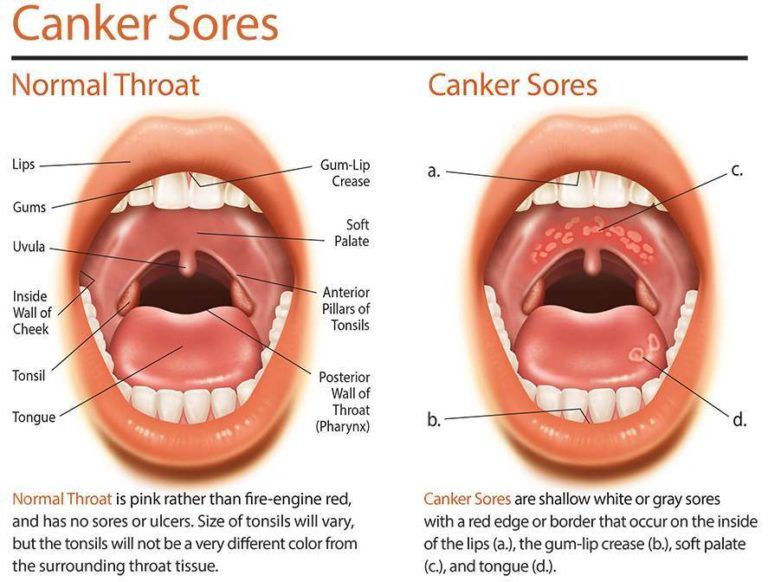 The course of the disease can be extremely severe, treatment can be lengthy, and the risk of post-infection complications is high. nine0003
The course of the disease can be extremely severe, treatment can be lengthy, and the risk of post-infection complications is high. nine0003
Diseases caused by streptococci
Active β-hemolytic group A Streptococcus causes disease with variable symptoms and course. The clinical picture of streptococcal infection depends on the location of the inflammatory focus, the bacterial load, and the patient's premorbid background. Because of the "survivability" it is quite difficult to find an effective cure for an infectious disease.
Streptococcal pharyngitis
Inflammation is localized on the back wall of the pharynx - in the mucous membrane. The incubation period lasts 2-3 days, then acute symptoms appear - pain when swallowing saliva, enlargement and soreness of the cervical lymph nodes, hyperthermia. In about 20% of patients, the lymphadenoid tissue of the tonsils is involved in the infectious process, and pharyngotonsillitis develops. The disease is characterized by high fever, the formation of serous-purulent plugs on the mucous membrane of the tonsils, unbearable sore throat.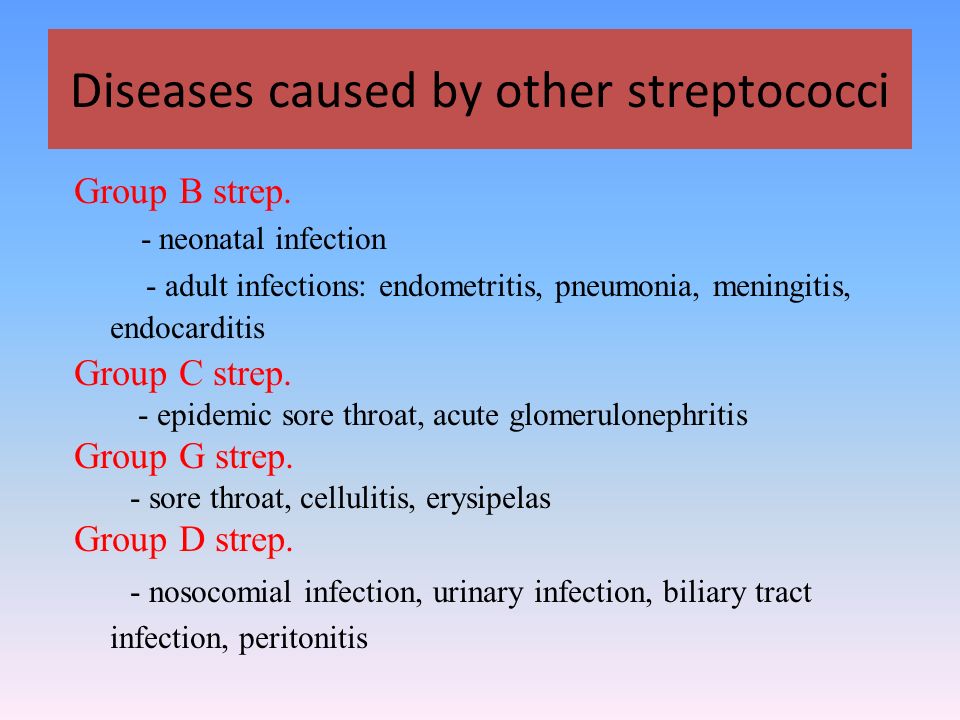 Peritonsillar abscess can become a complication. nine0003
Peritonsillar abscess can become a complication. nine0003
Scarlet fever
Acute inflammation of the oropharynx is often diagnosed in preschool children. Scarlet fever debuts with a high temperature, signs of intoxication of the body. Characteristic symptoms are a swollen bright crimson tongue, small punctate papular rashes, localized mainly on the face and upper body. For mild forms of the disease, outpatient treatment is allowed. Young children are hospitalized due to the risk of purulent-inflammatory complications.
Skin infections
Streptoderma is common in children, erysipelas or streptococcal phlegmon in adults. The first signs of streptoderma are skin conflicts filled with serous fluid. They transform into purulent vesicles, after which dense crusts form on the skin. Children often scratch itchy rashes, transferring streptococcus to healthy areas of the skin, which makes treatment more difficult. Forced opening of conflicts with subsequent treatment of the skin with Fukortsin and antibacterial ointments helps to speed up recovery. nine0003
nine0003
Erysipelas is a superficial inflammation of the skin, phlegmon is a deep inflammatory lesion that spreads to the subcutaneous fat. Diseases are associated with headache, fever, insomnia, regional lymphadenitis.
Necrotizing fasciitis
Purulent inflammation of the connective tissue associated with the death of skin cells and subcutaneous fat layer in the affected area. It is characterized by a high rate of development, severity of the course, frequent complications, and risks of mortality. The pathogenesis is closely related to vascular thrombosis, due to which there is a lack of oxygen supplied to the soft tissues. nine0003
Toxic shock syndrome (TSS)
Most cases of TSS are associated with the use of superabsorbent tampons during menstruation. An extremely severe somatic condition is caused by hypercytokinemia - an overproduction of cytokines in response to damage to the body by streptococcal toxins. This leads to a break in the information links between T-lymphocytes, as a result of which they attack the cells of their own body.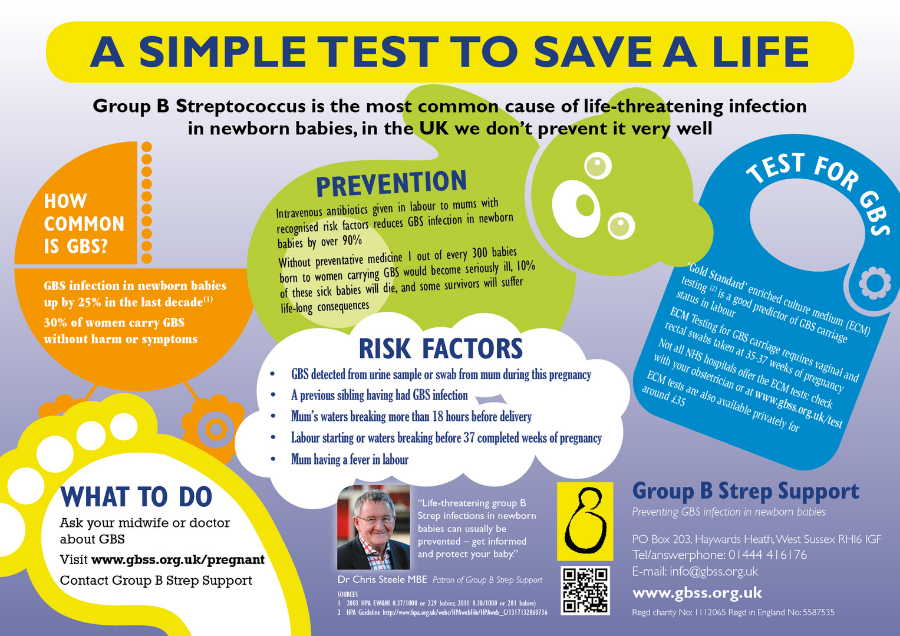 Vascular permeability increases sharply, pressure drops, the intercellular space is filled with plasma, and multiple organ failure develops. The lungs, the heart suffer, then the kidneys and liver fail. nine0003
Vascular permeability increases sharply, pressure drops, the intercellular space is filled with plasma, and multiple organ failure develops. The lungs, the heart suffer, then the kidneys and liver fail. nine0003
Late complications
The mechanism of development of late complications has not been studied. The main pathologies include glomerulonephritis, sepsis, necrotizing myositis, rheumatic fever.
Diagnosis
It is possible to identify the causative agent of the active form of the disease or to identify the carrier of the infection using laboratory tests of the biomaterial (skin scraping, throat swab). Bacteriological culture is used for diagnosis. If streptococcus colonies are detected, an antibiogram is additionally performed - determination of resistance to various types of antibiotics. nine0003
Treatment
Preparations for etiotropic therapy for children and adults are selected according to the results of laboratory diagnostics.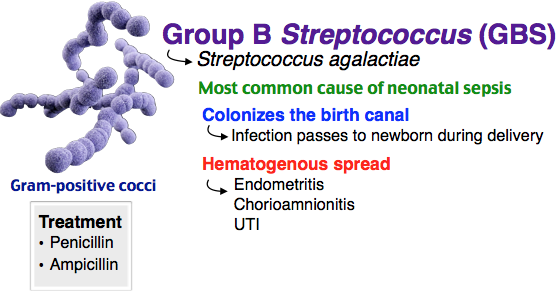 Many bacteria of hemolytic streptococcus are sensitive to antibiotics of the penicillin group. If treatment is ineffective, penicillins are replaced by macrolides - Sumamed, Azithromycin, Clarithromycin. To prevent an imbalance of microflora, probiotics and prebiotics are prescribed in parallel. Additionally, symptoms are treated based on the clinical picture of the disease. Of modern drugs, it is recommended to use Streptococcal Bacteriophage - a solution for irrigation of mucous membranes, applications, enemas, douching. nine0003
Many bacteria of hemolytic streptococcus are sensitive to antibiotics of the penicillin group. If treatment is ineffective, penicillins are replaced by macrolides - Sumamed, Azithromycin, Clarithromycin. To prevent an imbalance of microflora, probiotics and prebiotics are prescribed in parallel. Additionally, symptoms are treated based on the clinical picture of the disease. Of modern drugs, it is recommended to use Streptococcal Bacteriophage - a solution for irrigation of mucous membranes, applications, enemas, douching. nine0003
Streptococcal infection: Causes of streptococcal infection, Symptoms, Treatment of diseases caused by streptococcal infection
Streptococcal infection is a group of infectious diseases caused by different types of streptococcal flora. The infection affects the upper skin, mainly the skin of the face, hands, neck, as well as the respiratory organs. Streptococcal infection causes diseases such as streptoderma, pneumonia, glomerulonephritis, vasculitis, tonsillitis, rheumatism, erysipelas, scarlet fever, etc.
Attention!
Here you can choose a doctor who treats Streptococcal Infection If you are not sure about the diagnosis, make an appointment with a general practitioner or general practitioner to clarify the diagnosis.
Causes of streptococcal infection
Symptoms
Diagnostics
Treatment of diseases caused by streptococcal infection
Streptococcus - a kind of bacterial organisms, which is present in the human body. There are more than 15 subtypes of bacteria, but the most common are: alpha, beta and gamma. With an acceptable value of alpha and gamma, streptococci are part of the normal microflora of the gastrointestinal tract, oral cavity, larynx and respiratory system of a person, they do not carry harm to the body. Beta streptococci are dangerous to human health, and they cause a wide range of human diseases. nine0003
Hemolytic streptococcus (group A) is a common bacterium found in the body. The predominant number of infections develops precisely due to group A streptococcus. In this regard, a person has a high susceptibility to streptococcus and, accordingly, under favorable conditions for the bacterium, it actively multiplies in the human body. Group A bacteria most often cause:
The predominant number of infections develops precisely due to group A streptococcus. In this regard, a person has a high susceptibility to streptococcus and, accordingly, under favorable conditions for the bacterium, it actively multiplies in the human body. Group A bacteria most often cause:
- angina;
- pharyngitis;
- impetigo; nine0013 face;
- scarlet fever;
- pneumonia;
- glomerulonephritis;
- vasculitis;
- rheumatism;
- bronchitis;
- periodontitis.
Group B streptococcus mainly affects the genitourinary system, since this type of bacteria is found in the urethra in men and in the vagina in women.
Causes of streptococcal infection
A pathogenic bacterium is transmitted in three ways:
- airborne - the spread of infection with saliva and mucus when sneezing, crying, coughing; nine0014
- household contact - direct contact with the carrier of the infection, even if he does not show symptoms of diseases, contact with household items in the house and public places;
- sexual - through unprotected intercourse.

The fastest way to spread streptococcus is by airborne droplets, so children who are in a large group (school, kindergarten, various classes) very often succumb to infection.
Streptococcal infection in children develops most often in the cold season (end of autumn, winter). Due to the fact that children do not always observe hand hygiene, they can become infected in almost any environmental condition. nine0003
Often streptococcal infection occurs in newborns, this is due to the ability of streptococcus to penetrate into tissues and organs. At the time of childbirth, infection can occur through the amniotic fluid. The infection develops in the first few hours of life and leads to pneumonia, sepsis, and meningitis. The mortality rate with this development of infection is more than 50%.
In children aged 2 to 8 years, streptococcus often causes pneumonia as a complication of a previous infection: whooping cough, influenza, measles, chicken pox. Immunocompromised children who have suffered severe hypothermia are also susceptible to this disease.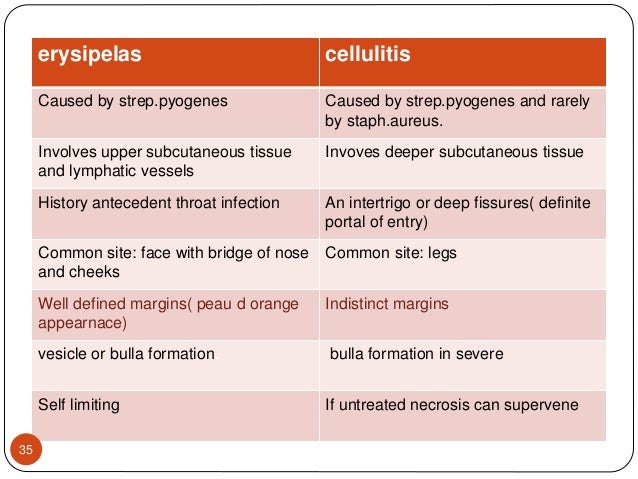 nine0003
nine0003
Symptoms
In medical practice, in diseases, streptococcal infection is manifested by a variety of symptoms. It depends on the specific disease that this type of pathogenic bacterium caused.
For the group of diseases of the respiratory tract, these are:
- sore throat;
- fever;
- plaque formation with pus on tonsils;
- swollen lymph nodes.
Streptococcal skin infection is usually accompanied by: inflammatory processes on the skin; nine0003
- itching;
- redness;
- the appearance of vesicles, plaques on the skin;
- fever;
- chills;
- weakness.
Diseases of the genitourinary system caused by hemolytic streptococcus are most often asymptomatic. However, there may also be symptoms similar to those of diseases in this area:
- itching;
- selection;
- soreness in the organs of the genitourinary system.
 nine0014
nine0014
Diagnosis
To identify the bacteria of the genus Streptococcus, a series of studies are carried out that allow you to determine the specific causative agent of the infection, its type and sensitivity to medicines. Traditionally, doctors (whose specialty depends on the affected area or organ) conduct a comprehensive diagnosis:
- bacteriological examination (inoculation of biological material) - a swab from the tonsils, lesions on the skin, sputum examination on the lungs; nine0014
- general analysis of urine, blood;
- microbiological examination for the level of sensitivity to antibiotics;
- examination of the affected organs by a narrow specialist.
Treatment of diseases caused by streptococcal infection
Treatment of streptococcal infection requires an initial correct diagnosis of the underlying disease, its differentiation from similar diseases.
When diagnosing the pathogenic bacterium streptococcus, treatment should be carried out by a narrow specialist depending on the affected organ: pulmonologist, dermatologist, gynecologist, urologist, etc.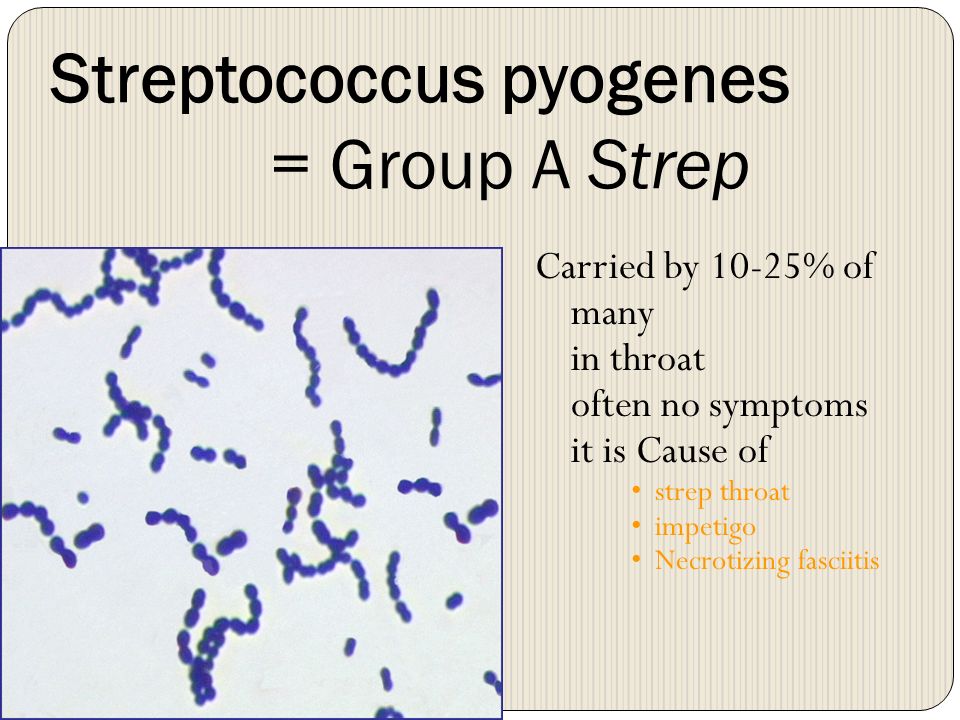




:max_bytes(150000):strip_icc()/hemorrhage-in-miscarriage-meaning-2371523-FINAL-f2ab04cab1cc491e964a45e682f93da5.png)