What causes large babies
Macrosomia: Symptoms, Causes, and Complications
Macrosomia: Symptoms, Causes, and Complications- Health Conditions
- Featured
- Breast Cancer
- IBD
- Migraine
- Multiple Sclerosis (MS)
- Rheumatoid Arthritis
- Type 2 Diabetes
- Articles
- Acid Reflux
- ADHD
- Allergies
- Alzheimer's & Dementia
- Bipolar Disorder
- Cancer
- Crohn's Disease
- Chronic Pain
- Cold & Flu
- COPD
- Depression
- Fibromyalgia
- Heart Disease
- High Cholesterol
- HIV
- Hypertension
- IPF
- Osteoarthritis
- Psoriasis
- Skin Disorders and Care
- STDs
- Featured
- Discover
- Wellness Topics
- Nutrition
- Fitness
- Skin Care
- Sexual Health
- Women's Health
- Mental Well-Being
- Sleep
- Product Reviews
- Vitamins & Supplements
- Sleep
- Mental Health
- Nutrition
- At-Home Testing
- CBD
- Men’s Health
- Original Series
- Fresh Food Fast
- Diagnosis Diaries
- You’re Not Alone
- Present Tense
- Video Series
- Youth in Focus
- Healthy Harvest
- No More Silence
- Future of Health
- Wellness Topics
- Plan
- Health Challenges
- Mindful Eating
- Sugar Savvy
- Move Your Body
- Gut Health
- Mood Foods
- Align Your Spine
- Find Care
- Primary Care
- Mental Health
- OB-GYN
- Dermatologists
- Neurologists
- Cardiologists
- Orthopedists
- Lifestyle Quizzes
- Weight Management
- Am I Depressed? A Quiz for Teens
- Are You a Workaholic?
- How Well Do You Sleep?
- Tools & Resources
- Health News
- Find a Diet
- Find Healthy Snacks
- Drugs A-Z
- Health A-Z
- Health Challenges
- Connect
- Breast Cancer
- Inflammatory Bowel Disease
- Psoriatic Arthritis
- Migraine
- Multiple Sclerosis
- Psoriasis
Medically reviewed by Karen Gill, M. D. — By Stephanie Watson on October 12, 2017
Overview
Macrosomia is a term that describes a baby who is born much larger than average for their gestational age, which is the number of weeks in the uterus. Babies with macrosomia weigh over 8 pounds, 13 ounces.
On average, babies weigh between 5 pounds, 8 ounces (2,500 grams) and 8 pounds, 13 ounces (4,000 grams). Babies with macrosomia are in the 90th percentile or higher in weight for their gestational age if born at term.
Macrosomia can cause a difficult delivery, and increase the risks for a cesarean delivery (C-section) and injury to the baby during birth. Babies born with macrosomia are also more likely to have health problems such as obesity and diabetes later in life.
Causes and risk factors
About 9 percent of all babies are born with macrosomia.
Causes of this condition include:
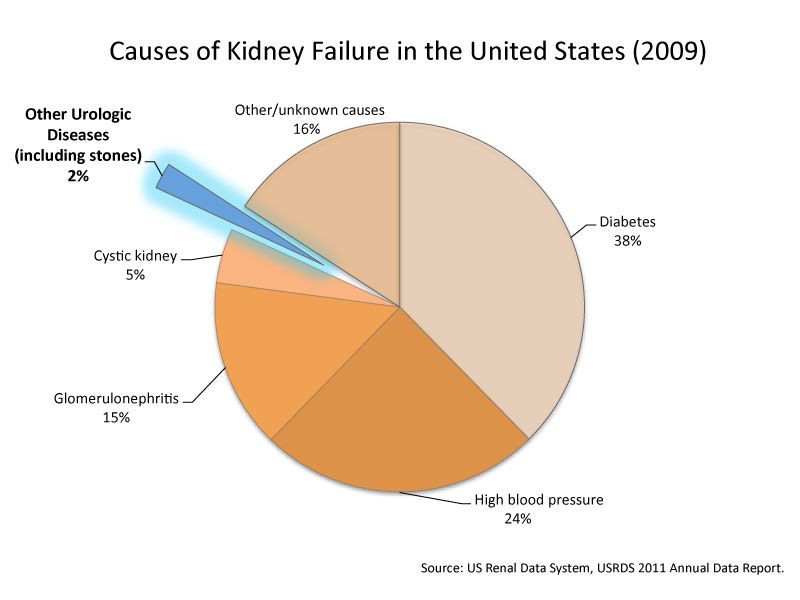
- diabetes in the mother
- obesity in the mother
- genetics
- a medical condition in the baby
You’re more likely to have a baby with macrosomia if you:
- have diabetes before you get pregnant, or develop it during your pregnancy (gestational diabetes)
- start out your pregnancy obese
- gain too much weight while pregnant
- have high blood pressure during pregnancy
- have had a previous baby with macrosomia
- are more than two weeks past your due date
- are over 35 years of age
Symptoms
The main symptom of macrosomia is a birth weight of more than 8 pounds, 13 ounces — regardless of whether the baby was born early, on time, or late.
How is it diagnosed?
Your doctor will ask about your medical history and past pregnancies. They can check your baby’s size during pregnancy, however this measurement isn’t always accurate.
Methods to check the baby’s size include:
- Measuring the height of the fundus. The fundus is the length from the top of the mother’s uterus to her pubic bone. A larger than normal fundal height could be a sign of macrosomia.
- Ultrasound. This test uses sound waves to view an image of the baby in the uterus. Although it’s not completely accurate at predicting the birth weight, it can estimate whether the baby is too large in the womb.
- Check the amniotic fluid level. Too much amniotic fluid is a sign that the baby is producing excess urine. Larger babies produce more urine.
- Nonstress test. This test measures your baby’s heartbeat when he or she moves.
- Biophysical profile.
 This test combines the nonstress test with an ultrasound to check your baby’s movements, breathing, and the level of amniotic fluid.
This test combines the nonstress test with an ultrasound to check your baby’s movements, breathing, and the level of amniotic fluid.
How does it affect delivery?
Macrosomia can cause these problems during delivery:
- the baby’s shoulder may get stuck in the birth canal
- the baby’s clavicle or another bone gets fractured
- labor takes longer than normal
- forceps or vacuum delivery is needed
- cesarean delivery is needed
- the baby doesn’t get enough oxygen
If your doctor thinks your baby’s size could cause complications during a vaginal delivery, you may need to schedule a cesarean delivery.
Complications
Macrosomia can cause complications to both the mother and baby.
Problems with the mother include:
- Injury to the vagina. As the baby is delivered, he or she can tear the mother’s vagina or the muscles between the vagina and anus, the perineal muscles.
- Bleeding after delivery. A large baby can prevent the muscles of the uterus from contracting like they should after delivery. This can lead to excess bleeding.
- Uterine rupture. If you’ve had a past cesarean delivery or uterine surgery, the uterus can tear during delivery. This complication could be life-threatening.
Problems with the baby that may arise include:
- Obesity. Babies born at a heavier weight are more likely to be obese in childhood.
- Abnormal blood sugar. Some babies are born with lower than normal blood sugar. Less often, blood sugar is high.
Babies born large are at risk for these complications in adulthood:
- diabetes
- high blood pressure
- obesity
They’re also at risk of developing metabolic syndrome. This cluster of conditions includes high blood pressure, high blood sugar, excess fat around the waist, and abnormal cholesterol levels. As the child gets older, metabolic syndrome can increase their risk for conditions like diabetes and heart disease.
As the child gets older, metabolic syndrome can increase their risk for conditions like diabetes and heart disease.
Important questions to ask your doctor
If tests during your pregnancy show that your baby is larger than normal, here are a few questions to ask your doctor:
- What can I do to stay healthy during my pregnancy?
- Will I need to make any changes to my diet or activity level?
- How might macrosomia affect my delivery? How could it affect my baby’s health?
- Will I need to have a cesarean delivery?
- What special care will my baby need after birth?
Outlook
Your doctor may recommend a cesarean delivery as necessary to ensure a healthy delivery. Inducing labor early so that the baby is delivered before its due date, hasn’t been shown to make a difference in the outcome.
Babies born large should be monitored for health conditions like obesity and diabetes as they grow. By managing preexisting conditions and your health during pregnancy, as well as monitoring the health of your baby into adulthood, you may be able to help prevent complications that can arise from macrosomia.
Last medically reviewed on October 12, 2017
- Parenthood
- Baby
- 06 Months
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Gibson E, et al. (2015). Large-for-gestational-age (LGA) infant.
merckmanuals.com/en-pr/professional/pediatrics/perinatal-problems/large-for-gestational-age-lga-infant - Low birthweight. (n.d.).
stanfordchildrens.org/en/topic/default?id=low-birthweight-90-P02382 - Macrosomia. (2016).
winchesterhospital.org/health-library/article?id=223413 - Mayo Clinic Staff. (2015). Fetal macrosomia.
mayoclinic.org/diseases-conditions/fetal-macrosomia/basics/causes/con-20035423 - Mohammadbeigi A, et al.
 (2013). Fetal macrosomia: Risk factors, maternal, and perinatal outcome. DOI:
(2013). Fetal macrosomia: Risk factors, maternal, and perinatal outcome. DOI:
10.4103/2141-9248.122098 - Zamorski MA, et al. (2001). Management of suspected fetal macrosomia.
aafp.org/afp/2001/0115/p302.html
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Oct 12, 2017
Written By
Stephanie Watson
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Karen Richardson Gill, MD
Share this article
Medically reviewed by Karen Gill, M.D. — By Stephanie Watson on October 12, 2017
related stories
Your Baby Was How Big?! Why Your Supersized Baby Is Perfectly Normal (and Beautiful)
C-Section (Cesarean Section)
Pregnancy Complications
High Blood Pressure During Pregnancy
Pregnancy Doctors and Birthing Options
Read this next
Your Baby Was How Big?! Why Your Supersized Baby Is Perfectly Normal (and Beautiful)
Medically reviewed by Karen Gill, M.
 D.
D.Next time someone gawks at your large baby, remind them it's not nice to stare.
READ MORE
C-Section (Cesarean Section)
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
A cesarean section — or C-section — is the surgical delivery of a baby. It involves one incision in the mother’s abdomen and another in the uterus. A…
READ MORE
Pregnancy Complications
Medically reviewed by Michael Weber, MD
Sometimes a pregnant woman’s existing health conditions can contribute to problems, and other times new conditions arise because of body and hormonal…
READ MORE
High Blood Pressure During Pregnancy
Medically reviewed by Holly Ernst, PA-C
High blood pressure is common during pregnancy, but can also be a serious concern to monitor.
 High blood pressure during pregnancy can occur due to…
High blood pressure during pregnancy can occur due to…READ MORE
Pregnancy Doctors and Birthing Options
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
When deciding on a birthing plan, it’s important to be aware of your options and to create a plan that fits your needs. Here we’ll explain the roles…
READ MORE
What Are the Symptoms of Hyperovulation?
Hyperovulation has few symptoms, if any. It's typically diagnosed after an individual develops multiple pregnancies at once.
READ MORE
Pregnancy Friendly Recipe: Creamy White Chicken Chili with Greek Yogurt
This pregnancy-friendly spin on traditional chili is packed with the nutrients your body needs when you're expecting.
READ MORE
What You Should Know About Consuming Turmeric During Pregnancy
Consuming turmeric in pregnancy is a debated subject.
 We'll tell you if it's safe.
We'll tell you if it's safe.READ MORE
Pregnancy-Friendly Recipe: Herby Gruyère Frittata with Asparagus and Sweet Potatoes
Medically reviewed by Kathy W. Warwick, R.D., CDE
So easy and delicious. This frittata is high in protein and rich in essential nutrients your body needs to support a growing baby. Bonus: You can…
READ MORE
The Best Stretch Mark Creams and Belly Oils for Pregnancy in 2023
Stretch marks are easier to prevent than erase. If you're seeking a preventive, we've gathered a few of the best stretch mark creams for pregnancy.
READ MORE
Fetal Macrosomia (Large Baby) Birth Injuries
According to a Study Released by the National Institutes of Health (NIH), babies born with the birth weight of more than 8.8 pounds (large babies) “have increased risk of cerebral palsy associated with neonatal encephalopathy (Enc-CP). ”
”
Newborns that are macrosomic (large for their gestational age) are often the result of gestational diabetes, maternal obesity or another untreated health condition of the mother. Macrosomia (LGA – large for gestational age) can be prevented with appropriate maternal health screening and routine monitoring of the mother’s health during pregnancy.
It is crucial that doctors diagnose macrosomia prenatally and monitor changes using various tools including ultrasounds the estimate fetal weight, amniotic fluid tests, fundal height measurements and Leopold maneuvers (a systematic process for determining fetal position in the mother’s uterus.
A failure to diagnose macrosomia and treat the mother accordingly might be considered a deviation from the standards of care and pose a significant health risk to both the baby and the mother.
Birth Weight Is a Primary Cause of Fetal Macrosomia
The American College of Obstetricians and Gynecologists (ACOG) acknowledges there is a significant risk to maternal and newborn morbidity and children delivered with the birth weight of 4000 g (8. 188 pounds). This is on the upper end of the range of average birth weight.
188 pounds). This is on the upper end of the range of average birth weight.
Large babies are typically the result of a high-risk pregnancy that results in birth injuries including cerebral palsy, Erb’s palsy, traumatic brain injuries, brain bleeding, and HIE (hypoxic-ischemic encephalopathy).
Typically, doctors would perform a cesarean delivery when there is suspected fetal macrosomia. They would monitor the estimated fetal weight and act when there are potential maternal complications.
If your child was considered to be 'large' at birth and developed complications, such as cerebral palsy, contact Rosenfeld Injury Lawyers LLC for a free review of your legal rights and options for a financial recovery. Our firm handles birth injury lawsuits on a contingency fee basis where there is never a legal fee charged unless there is a recovery for you.
Risk Factors for Fetal Macrosomia
Macrosomia typically develops in the womb when the fetus receives an abundance of nutrients that might be caused by the mother’s obesity or diabetic condition, especially a gestational diabetic condition. In rare cases, the fetus might be suffering from a genetic medical condition, which accelerates fetal growth.
In rare cases, the fetus might be suffering from a genetic medical condition, which accelerates fetal growth.
Many factors can increase the potential risk of the newborn suffering from macrosomia.
The leading factors include:
- Mother’s Diabetes Mellitus Condition– The fetus can grow inside the womb at an accelerated rate if the mother suffers from type II diabetes (diabetes mellitus). The increase in fetal body weight is often the result of the mother’s elevated insulin and blood sugar levels that overly stimulate the baby’s growth.
- Mother’s Obesity– Macrosomia can develop during pregnancy if the mother gains an excessive amount of weight was obese before becoming pregnant.
- Previous Pregnancies– Pregnant women who have had an earlier pregnancy have an increased risk of experiencing fetal macrosomia. It is a common occurrence that the 2nd to 5th child born to the same mother will have an increased body weight of up to hundred 20 g (4 ounces).
- Multiple Births– Pregnancies involving multiple gestations (twins, triplets, quadruplets, etc.) have an increased potential risk of macrosomia events.
- Post-term Pregnancies – Overdue pregnancies, or any pregnancy that takes longer than 40 weeks, increases the potential risk of macrosomia incidents.
- Older Pregnancy Age– Pregnant mothers 35 years or older have an increased risk of having a baby diagnosed with an LGA condition.
- Male Babies– In the womb and at birth, boys tend to weigh significantly more (10 pounds and higher) than girls.
- Genetics– There are certain genetic factors involved in birthing a macrosomia baby including taller and heavier biological parents.
- Antibiotic Use While Pregnant– Studies have shown that pregnant mothers taking antibiotic medications including pivampicillin and amoxicillin increases the chance of birthing a macrosomic baby.
- Congenital Anomaly– The increased potential risk of developing macrosomia is elevated if the fetus suffers from a cardiac malformation like transposition of the great vessels.
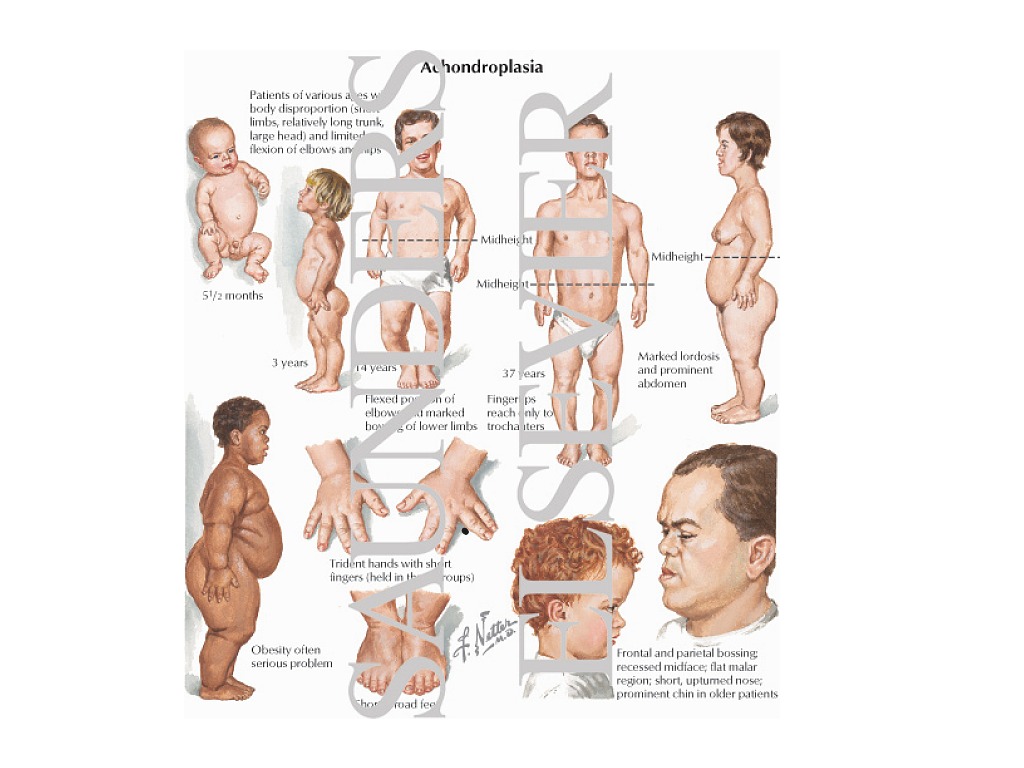
- Overgrowth Genetic Disorder– There are certain genetic disorders including Sotos syndrome (overgrowth during childhood, distinctive facial characteristics, delay development, restricted movement, and learning disabilities during the first few years of life) that often presents itself as macrosomia during pregnancy or at birth.
Gestational Diabetes as a Cause of Fetal Macrosomia
Nearly all macrosomia cases involve material weight gain, obesity or maternal diabetes. Unfortunately, the larger size of the baby can lead to other birthing problems including shoulder dystocia involving delivery problems when the mother’s pelvis blocks the baby shoulders in the birth canal.
What causes fetal macrosomia in a mother’s pregnancy is an important factor to consider to ensure the child’s health and an adverse perinatal outcome. Pregnant women with known risk factors should talk to their doctor about macrosomia being a concern.
Pregnant women with known risk factors should talk to their doctor about macrosomia being a concern.
The obstetrician can provide different medical options to reduce the potential risk to the child and the mother including controlling weight gain, planning a cesarean section and more.
Pregnancy Weight Gain as a Cause of Fetal Macrosomia
Pregnancy weight gain is a major risk factor for fetal macrosomia. When the mother progresses beyond a healthy weight, they can harm both their health and that of the baby. The excess weight could increase the mother's risk of heart disease.
The more weight the mother gains, the more weight the child will usually gain.
Gestational Age as a Cause of Fetal Macrosomia
When the baby has prolonged gestation, they may gain too much weight, and the risk of fetal macrosomia increases. The doctor will continuously monitor the child's height and weight during the pregnancy. When a baby approaches a certain size, the doctor should consider both the health of the child and mother and perform a cesarean section delivery.
What Are the Indicators of Fetal Macrosomia?
There are two signs associated with macrosomia for gynecologists providing neonatal care. These indicators include:
- Polyhydramnios (Too Much Amniotic Fluid)– During pregnancy, the buildup of excessive levels of amniotic fluid that protects and surrounds the fetus could be an indicator of a large-size baby. The fluid might be the buildup of excessive urine output by the fetus because larger babies tend to produce more urine.
- Larger Fundal Height– Obstetricians can monitor the mother’s fundal height (McDonald’s rule) by measuring the size of the uterus to determine fetal growth and take appropriate measures to treat any conditions that could increase risk factors including maternal obesity or diabetes.
Managing Macrosomia
To prevent fetal macrosomia, it is crucial that the neonatal physician identifies the underlying cause of the condition before the baby comes to full-term. In many pregnancies involving macrosomia, vaginal delivery is still an option.
In many pregnancies involving macrosomia, vaginal delivery is still an option.
However, some newborns are at risk of suffering grave injury if the obstetrician must use tools including forceps and vacuum extractors during the birthing process when the baby has trouble progressing past the pubic bone.
In some cases, these instruments can cause traumatic head injuries. Because of that, doctors often recommend a cesarean section (see section) delivery to ensure a successful macrosomic delivery. Many doctors will evaluate amniotic fluid levels after the 39th week to identify any problems that might arise including underdeveloped lungs or other conditions.
Maternal and Neonatal Complications
Common complications associated with pregnancies involving macrosomia can include:
- Uterine Rupture– Serious emergencies can occur during labor and delivery if the mother’s uterus ruptures during the birthing process. In some cases, the uterus will tear open on a scar from an earlier surgery or cesarean section and redirect the fetus out of the mother’s birth canal and into the abdomen.
 In some cases, excessive pressure or force during the delivery process caused by the excessive baby’s large size can increase the potential risk of a uterine rupture. Many maternal and fetal deaths are the result of a uterine rupture or the newborn suffering fetal asphyxia (hypoxic-ischemic encephalopathy). Typically, the doctor must perform an emergency cesarean section to minimize complications or prevent life-threatening problems.
In some cases, excessive pressure or force during the delivery process caused by the excessive baby’s large size can increase the potential risk of a uterine rupture. Many maternal and fetal deaths are the result of a uterine rupture or the newborn suffering fetal asphyxia (hypoxic-ischemic encephalopathy). Typically, the doctor must perform an emergency cesarean section to minimize complications or prevent life-threatening problems. - HIE (Hypoxic-Ischemic Encephalopathy)– Fetal asphyxia can be a serious complication in macrosomic pregnancies where the baby’s brain is deprived of much-needed oxygen. HIE often results in permanent injuries including learning disabilities, seizures, Erb’s palsy and cerebral palsy when brain cells die from a lack of oxygen. This condition often develops when the baby is too large to travel through the mother’s birth canal and instead becomes stuck causing the restriction of essential flow of oxygenated blood to the baby’s body and brain.

- Brachial Plexus Injury– Babies can develop Erb’s palsy when caught in the birth canal when experiencing a neck tear that damages the brachial plexus nerve in the baby’s upper arm, caused by downward traction. Typically, a brachial plexus injury occurs because of a force compressing the umbilical cord during the delivery process that restricts oxygen flow and causes a permanent injury like HIE (hypoxic-ischemic encephalopathy).
- Cesarean Section– Birthing a large baby increases the potential risk of complications associated with delivery if the newborn becomes stuck in the birth canal that can only be remedied with an emergency cesarean section. If the C-section takes too long perform, it could cause oxygen deprivation to the baby and cause lifelong health issues including cerebral palsy.
- Vacuum Extractors and Forceps-Associated Injuries– Delivery instruments are sometimes used during the birthing process to assist a macrosomic baby who has become more might become stuck in the birth canal.
 However, when doctors use vacuum extractors and forceps incorrectly, the baby’s head may experience extreme forces that can cause a blood clot or intracranial hemorrhage that leads to brain cell damage, stroke, brachial plexus injury, ischemia, or cerebral palsy. The extreme force can result in skull fractures; I have leads (retinal hemorrhage), brain damage including seizures and cerebral palsy, and brain bleeds involving subgaleal hemorrhages.
However, when doctors use vacuum extractors and forceps incorrectly, the baby’s head may experience extreme forces that can cause a blood clot or intracranial hemorrhage that leads to brain cell damage, stroke, brachial plexus injury, ischemia, or cerebral palsy. The extreme force can result in skull fractures; I have leads (retinal hemorrhage), brain damage including seizures and cerebral palsy, and brain bleeds involving subgaleal hemorrhages. - Post-delivery Bleeding– Mothers can suffer severe uterine atony after giving birth if the uterus failed to contract after the birthing process that could lead to postpartum hemorrhage where the excessive bleeding causes a life-threatening condition to the mother.
- Post-delivery Child’s Complications– Even if the child survives their macrosomic delivery, there are certain complications that could develop in the days, months and years after their birth. Some of these complications include:
- Cerebral Palsy and Erb’s Palsy
- Elevated Blood Sugar Levels
- Obesity
- Developing Metabolic Syndrome
Medical Malpractice Involving Macrosomia & Injuries to the Child
The neonatal physician and obstetrician must monitor the baby and the mother during pregnancy, labor, and delivery to identify macrosomia-related risk factors.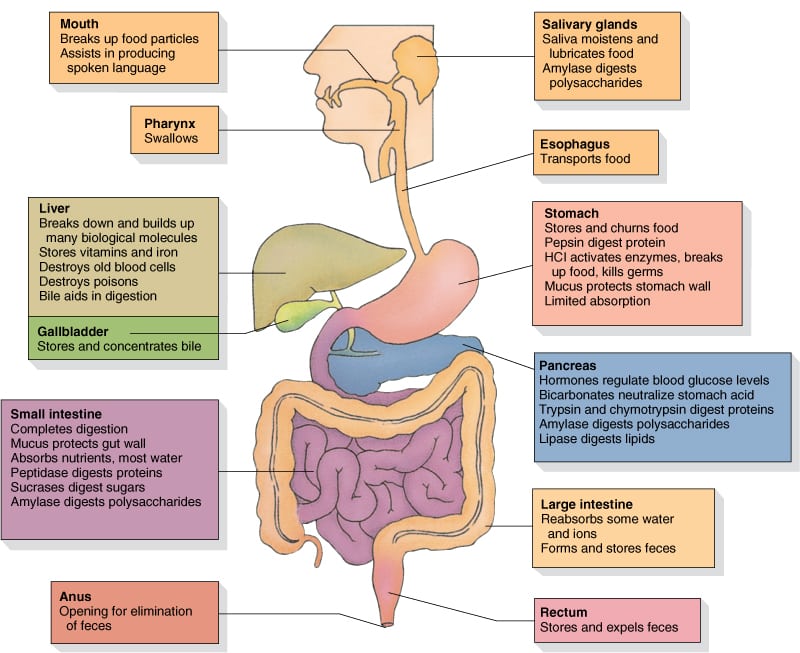 Doctors must act to facilitate a healthy pregnancy and practice proper maternal fetal medicine.
Doctors must act to facilitate a healthy pregnancy and practice proper maternal fetal medicine.
When macrosomic conditions are found, the doctor must be prepared for the worst-case scenario that could occur during delivery. Saving the lives of the mother and baby might require delivering the newborn early or performing an emergency cesarean section.
It is the doctor’s responsibility to inform the pregnant mother of the potentially serious complications involved in the delivery and all the options she has to ensure delivering a safe and healthy baby.
In some cases, the physician might be held legally liable for medical malpractice if they were negligent in their actions by:
- Not ordering a cesarean section;
- Failure to act when there is excessive weight gain during pregnancy
- Inappropriately using delivery instruments like vacuum extractors and forceps;
- Forcing the mother to have a vaginal birth that led to a birth injury;
- Improperly using oxytocin/Pitocin during labor and delivery;
- Not acting promptly during an emergent situation that necessitated an immediate cesarean section to avoid the child experiencing asphyxia;
- Not providing the patient adequate information to make an informed consent and how to deal with the risks associated with a macrosomic birth and delivery alternatives.
Medical Malpractice for Fetal Macrosomia
If the doctor has failed to uphold their standard of care, you can hold them legally responsible in a lawsuit. You would have to show that the doctor did not act as a reasonable doctor would under the circumstances. First, you would contact a birth injury lawyer who would review your child's medical records and consult with expert witnesses to establish where the doctor made a medical mistake.
Attorneys for Fetal Macrosomia Cases
Handling these cases in court often involves complex legal issues. An attorney working on behalf of the family can review the mother and child’s medical records and identify any negligence that might have played a role that resulted in a birthing injury.
However, time is of the essence. All the necessary paperwork must be filed in the proper county courthouse before the state statute of limitations expires.
Contact the birth injury attorneys at Rosenfeld Injury Lawyers today and let us evaluate if your child's condition is related to a large birth weight.
LARGE FETUS - Article I Clinic of evidence-based medicine NEPLACEBO
Site search Begovaya, 2/3
Personal account
Navigation
For the patient
Personal account
Site search
Kolyadina Anna Alexandrovna
06/30/2021
Surely you have heard how after giving birth a large baby is called a “hero”? In fact, very often (although not always) the birth of a child over 4500 g indicates problems during pregnancy and / or carries risks directly during and after childbirth.
⠀
Gynecologist Anna Kolyadina about a fetus that is too large for her gestational age and, accordingly, a large newborn.
⠀
So, the diagnosis of fetal macrosomia is made if, during a full-term pregnancy, the child was born more than 4000-4500 g (in different countries, different upper limits), or more than 90-95 percentile for a given period.
⠀
Why is fetal macrosomia dangerous?
⠀
For the mother:
🔸Long labor
🔸Increased likelihood of operative vaginal delivery (vacuum extractor) or caesarean section
🔸Ruptures of the vagina, perineum of varying degrees
🔸Risk of postpartum hemorrhage
🔸In rare cases, uterine rupture
⠀
During childbirth for the fetus: manipulations).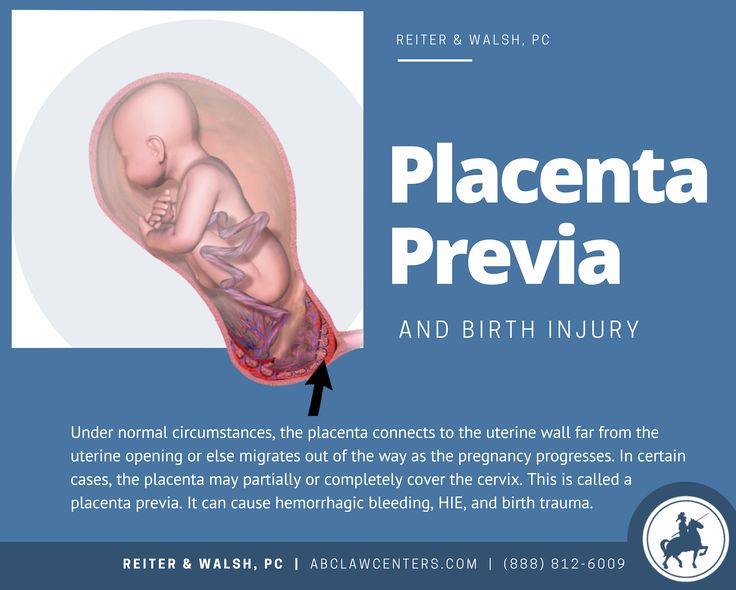 This situation increases the likelihood of trauma to the baby and mother during childbirth
This situation increases the likelihood of trauma to the baby and mother during childbirth
⠀
For newborns:
🔺 Hypoglycemia (low glucose levels)
🔺 Polycythemia (elevated hematocrit and hemoglobin, which can lead to increased blood viscosity)
🔺 Respiratory problems, risk of perinatal asphyxia
⠀
delayed consequences for children:
a child over 4000 g in a previous pregnancy
✔ Mother's own birth weight over 4000 g
✔ Rarely - some hereditary syndromes
✔ Postterm pregnancy
✔ Maternal obesity
✔ Excessive weight gain during pregnancy (with a normal BMI and weight gain of more than 16 kg, the risk of having a fetus with macrosomia increases by 2.5 times) : many women who have given birth to large children do not have three main factors (obesity, diabetes and overweight)! Probably, the role of genetic and epigenetic factors is also great.
⠀
❓Why the fetus weighs more than it should
It is believed that the main mechanism for the development of fetal macrosomia is an increased glucose level in a pregnant woman, which, in turn, leads to its increased level in the fetus. As a result, the level of insulin, IGF and growth hormone begins to “storage” fat by the fetus.
As a result, the level of insulin, IGF and growth hormone begins to “storage” fat by the fetus.
Other parameters associated with the risk of macrosomia include elevated triglycerides (⬆️risk) and HDL (⬇️risk) in the mother.
⠀
DIAGNOSIS
⠀
During pregnancy, the large size of the fetus and large weight can be determined using ultrasound (the closer the ultrasound date to childbirth, the more accurate the weight forecast for the newborn)
⠀
During routine visits to the gynecologist, suspicion of a large the fetus can occur when it is palpated and measuring the height of the fundus of the uterus. But this method is quite subjective and imprecise.
⠀
PREVENTION
⠀
All of the above was not intended to scare the expectant mother, but to convey an important message: most macrosomia risk factors can be corrected!
⠀
In case of diabetes or gestational diabetes mellitus, the prevention of fetal macrosomia is GLUCOSE CONTROL and maintenance of its target values.
⠀
In case of obesity, it is worth doing WEIGHT REDUCTION before pregnancy
⠀
In case of normal weight and absence of diabetes, it is worth taking control of WEIGHT GAIN during pregnancy, avoiding going beyond the upper limit of the norm. Adequate regular physical activity will contribute to the favorable course of pregnancy and reduce risks.
⠀
You may be interested in
Sore throat
Every person has experienced sore throat at least once. More often …
Runny nose
“I don’t have a runny nose, just a stuffy nose”, so often …
Nutrition for children
Understanding how much a child’s health depends on the fact that he …
Remember: JavaScript is required for this content .
Open chat
A real hero: what are the causes of a large fetus, and what is the danger of childbirth - Parents.ru
ChildbirthPregnancyHealth
- Photo
- Don Bayley/Getty Images/E+
obstetrician-gynecologist
Predicting the birth of a large child, doctors are guided by its weight, since height is not a determining criterion. Normal weight of newborns ranges on average from 3000 g to 3800 g. As a rule, girls are more often born with a weight of 3200-3400 g, and boys - 3400-3500 g. However, the figures may differ from the norm. With cephalic presentation, a baby whose weight exceeds 4 kg is considered large, with pelvic presentation - 3600 g. If the fetus weighs more than 5 kg, doctors call it giant.
Normal weight of newborns ranges on average from 3000 g to 3800 g. As a rule, girls are more often born with a weight of 3200-3400 g, and boys - 3400-3500 g. However, the figures may differ from the norm. With cephalic presentation, a baby whose weight exceeds 4 kg is considered large, with pelvic presentation - 3600 g. If the fetus weighs more than 5 kg, doctors call it giant.
Risk group
There are certain prerequisites for the birth of overweight babies. First of all, genetic: it has been established that large children are more often born from tall parents of a strong physique. The second risk factor is endocrine metabolic disorders in the mother (diabetes mellitus, obesity). With these diseases, carbohydrate metabolism is disturbed, and an increased amount of glucose, nutrients and enzymes enters the baby through the blood. Its metabolism is activated, which leads to obesity. Such newborns have a standard height with excessive weight.
In 1955, a baby weighing 10. 2 kg was born in Italy. He was immediately recorded in the Guinness Book of Records. In 2009, a boy was born in Indonesia, who weighed about 9 kg. At the same time, the height of the “hero” was a little more than 60 cm. The next reason is post-term pregnancy (more than 41 weeks), which most often occurs with violations of the central nervous system and endocrine diseases. But if the expectant mother suffered severe psycho-emotional shocks during pregnancy or did not move much, such a “protracted” scenario is also real. It is important that with each subsequent birth with a normal pregnancy, the weight of the child increases. The walls of the uterus stretch more easily, the uteroplacental circulation improves, and more nutrients are supplied to the baby, due to which its size increases. There is evidence that the risk of having a large baby may be due to certain drugs that are prescribed to improve uteroplacental circulation and maintain pregnancy.
2 kg was born in Italy. He was immediately recorded in the Guinness Book of Records. In 2009, a boy was born in Indonesia, who weighed about 9 kg. At the same time, the height of the “hero” was a little more than 60 cm. The next reason is post-term pregnancy (more than 41 weeks), which most often occurs with violations of the central nervous system and endocrine diseases. But if the expectant mother suffered severe psycho-emotional shocks during pregnancy or did not move much, such a “protracted” scenario is also real. It is important that with each subsequent birth with a normal pregnancy, the weight of the child increases. The walls of the uterus stretch more easily, the uteroplacental circulation improves, and more nutrients are supplied to the baby, due to which its size increases. There is evidence that the risk of having a large baby may be due to certain drugs that are prescribed to improve uteroplacental circulation and maintain pregnancy.
Control rules
An obstetric examination helps to recognize a large baby. From the second half of the term, at each visit to the doctor, the height of the fundus of the uterus (VDM) is measured for a woman - the distance between the upper edge of the pubic joint and the fundus of the uterus - and the circumference of the abdomen (OC). If the coolant is more than 100 cm at the end of pregnancy, it can be assumed that the child is large. The approximate weight of the child can be calculated by multiplying the VMD by the coolant. But this formula only works if the woman is not obese. More accurate information is provided by ultrasound, and already in the middle of the third trimester, at 32–34 weeks. The doctor measures the circumference of the head, abdomen, the length of the femur and humerus of the baby - these data allow you to calculate his estimated body weight.
From the second half of the term, at each visit to the doctor, the height of the fundus of the uterus (VDM) is measured for a woman - the distance between the upper edge of the pubic joint and the fundus of the uterus - and the circumference of the abdomen (OC). If the coolant is more than 100 cm at the end of pregnancy, it can be assumed that the child is large. The approximate weight of the child can be calculated by multiplying the VMD by the coolant. But this formula only works if the woman is not obese. More accurate information is provided by ultrasound, and already in the middle of the third trimester, at 32–34 weeks. The doctor measures the circumference of the head, abdomen, the length of the femur and humerus of the baby - these data allow you to calculate his estimated body weight.
To reduce the chances of having a large baby, expectant mothers should carefully monitor their weight. By the time of childbirth, thin women are allowed to recover no more than 15 kg, owners of an average physique - 10-12 kg, puffy young ladies - a maximum of 7-8 kg.
- Photo
- Getty Images/Science Photo Library RF
Difficulties along the way
Due to the fact that the uterus is overdistended, women who are expecting a large baby often develop weakness in labor. In this case, doctors, as a rule, resort to stimulating contractions with the help of special drugs. Another high risk is birth canal ruptures. It is for this reason that such expectant mothers almost always undergo an episiotomy - a perineal incision. Problems can arise even after the baby is born. Due to the fact that the uterus was greatly overstretched, it will contract more slowly, which is fraught with bleeding and the occurrence of postpartum infection. Droppers with oxytocin again help to correct the situation.
During a post-term pregnancy, the baby's skull bones grow together, which means that it becomes more difficult for him to pass through the birth canal, and if he does not succeed in this, a diagnosis of "clinically narrow pelvis" is made and an emergency caesarean section is performed.
Another thing
A large baby can also be born due to prolonged pregnancy, which occurs with a long menstrual cycle. It usually lasts one to two weeks longer than usual. But unlike a post-term pregnancy, with a prolonged baby, the fontanelles do not grow together, so the risk of injury when passing through the birth canal is much less.
An informed decision
Many mothers, fearing the above complications, ask doctors to perform a caesarean section. But obstetricians never make concessions out of pity, because any operation requires strong evidence. Despite the fact that such births are almost always delayed and the list of possible complications is really large, now the expectant tactics are most often used. This means that in the vast majority of cases, a woman who is expecting a large child begins to give birth herself. With normal labor activity and the absence of associated health problems, the natural scenario will certainly be optimal. If complications arise during childbirth, doctors perform an emergency caesarean section.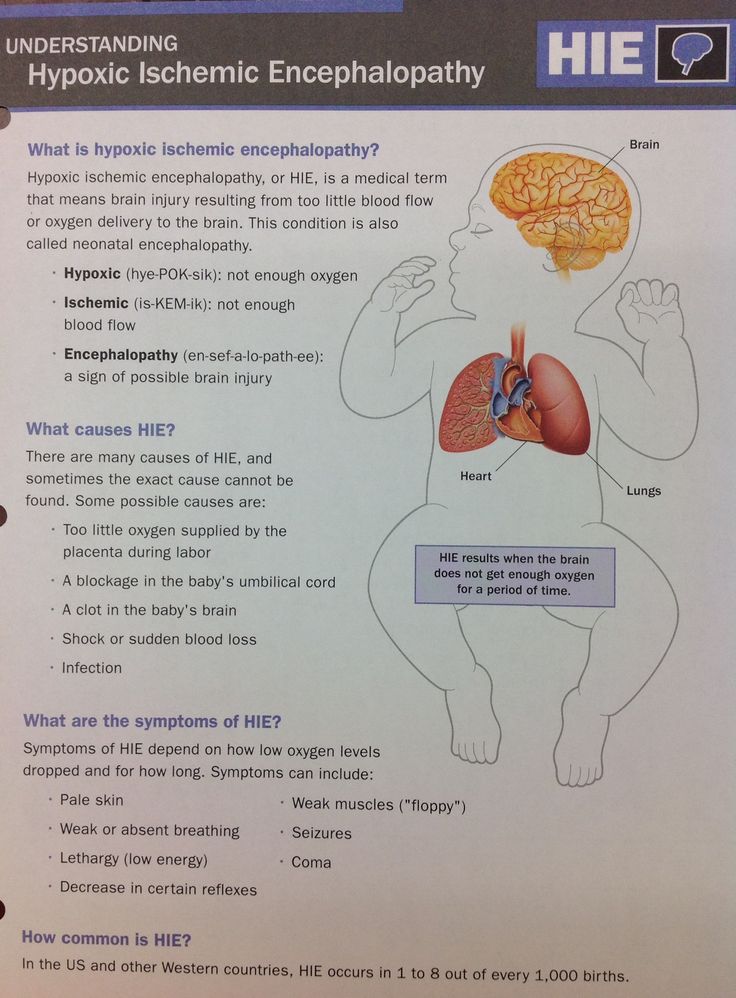 Most often, the operation is done when there is a weakness of labor or a clinically narrow pelvis. And, of course, doctors wait until the last moment for a reason.
Most often, the operation is done when there is a weakness of labor or a clinically narrow pelvis. And, of course, doctors wait until the last moment for a reason.
-
First of all, it is impossible to predict the exact development of events in advance, moreover, surgical intervention is not always required. So it makes no sense to get ahead of events.
-
Secondly, despite the fact that a planned caesarean is less likely to cause complications than an emergency one, in the latter case there is still one plus: since labor begins on its own, after the operation, the uterus will contract better under the influence of its own hormones.
In some cases (for example, with progressive gestosis, diabetes mellitus, edematous form of hemolytic disease, etc.), doctors recommend early delivery, that is, artificial premature birth through the natural birth canal. This measure is usually resorted to at the 36th week (not earlier), which avoids possible complications, because at this time the weight of the child will be lower than at 38–40 weeks.