What causes hcg
Human Chorionic Gonadotropin - StatPearls
Introduction
Human chorionic gonadotropin (hCG) is a chemical created by trophoblast tissue, tissue typically found in early embryos and which will eventually be part of the placenta. Measuring hCG levels can be helpful in identifying a normal pregnancy, pathologic pregnancy, and can also be useful following an aborted pregnancy. There is also a benefit in measuring hCG in a variety of cancers including choriocarcinoma and extra-uterine malignancies.
Etiology and Epidemiology
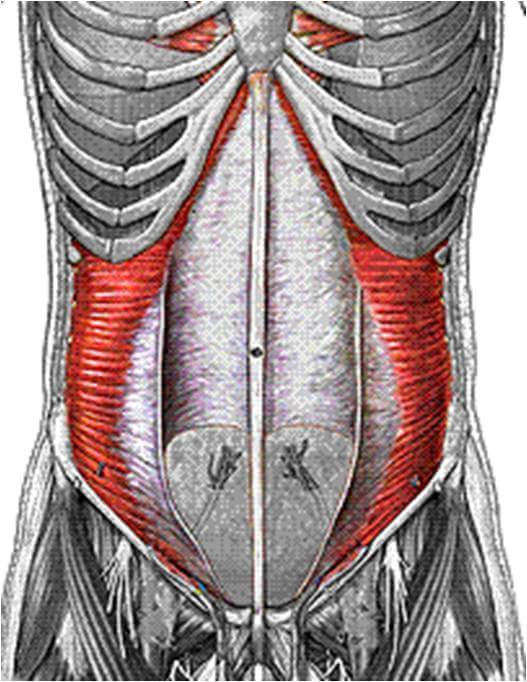
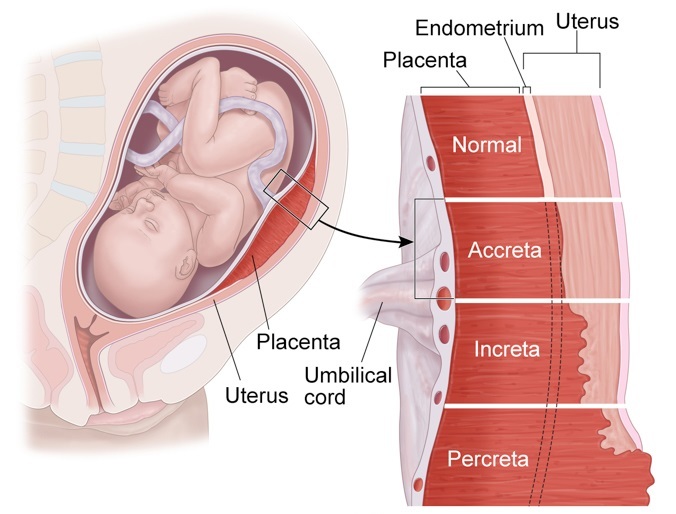
Human chorionic gonadotropin is a hormone produced primarily by syncytiotrophoblastic cells of the placenta during pregnancy. The hormone stimulates the corpus luteum to produce progesterone to maintain the pregnancy. Smaller amounts of hCG are also produced in the pituitary gland, the liver, and the colon.[1] As previously mentioned, certain malignancies can also produce either hCG or hCG-related hormone. Trophoblastic cancers (hydatidiform mole, choriocarcinoma, and germ cell tumors) are associated with high serum levels of hCG-related molecules.
The hormone itself is a glycoprotein composed of two subunits, the alpha and beta subunits.[1] There are multiple forms found in the serum and urine during pregnancy including the intact hormone and each of the free subunits. HCG is primarily catabolized by the liver, although about 20% is excreted in the urine. The beta subunit is degraded in the kidney to make a core fragment which is measured by urine hCG tests.
Specimen Requirements and Procedure
Urine Testing
Urine should not be collected after the patient has been drinking a large amount of fluid, as a dilute specimen may result in a falsely negative test.[2]
Blood in the urine may cause a false positive test result.
Serum Testing
Diagnostic Tests
Serum tests for hCG are immunometric assays. This means that they use 2two antibodies that bind to the hCG molecule, a fixed antibody and a radiolabeled antibody which adhere to different sites on the molecule, sandwiching and immobilize the molecule to make it detectable.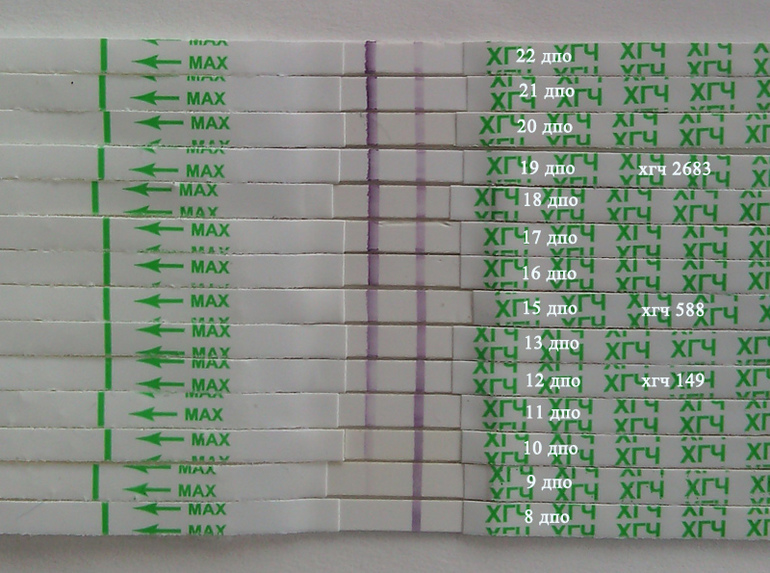 [3] Assays involve washing away the excess serum components and measuring the amount of remaining labeled hCG to give a quantitative result. There are more than 100 different assays commercially available which results in significant variability in reported values.
[3] Assays involve washing away the excess serum components and measuring the amount of remaining labeled hCG to give a quantitative result. There are more than 100 different assays commercially available which results in significant variability in reported values.
Urine assays are similar, although many detect total hCG levels greater than 20 mIU/mL.[4] Many over-the-counter urine pregnancy tests do not detect hyperglycosylated hCG, which accounts for most of the hCG in early pregnancy, resulting in a wide range of sensitivities of these tests.
Serum testing is much more sensitive and specific than urine testing. Urine testing, however, is more convenient, affordable, comfortable for patients, has a fast turnaround (5 to 10 minutes), and does not require a medical prescription.
Testing Procedures
Urine Testing
Urine is placed in or on a designated receptacle (most commercially available and medical point of care tests)
An indicator (typically a colored line or symbol), along with a control, will appear if the test is positive
An isolated control line/symbol will be evident if the test is negative
Serum Testing
Serum hCG testing is performed in a laboratory equipped with the proper machinery and uses a peripheral blood sample
If a hook effect/gestational trophoblastic disease is suspected, the lab should perform a dilution prior to testing
Interfering Factors
There are multiple reasons why an hCG test (serum or urine) may have a false report.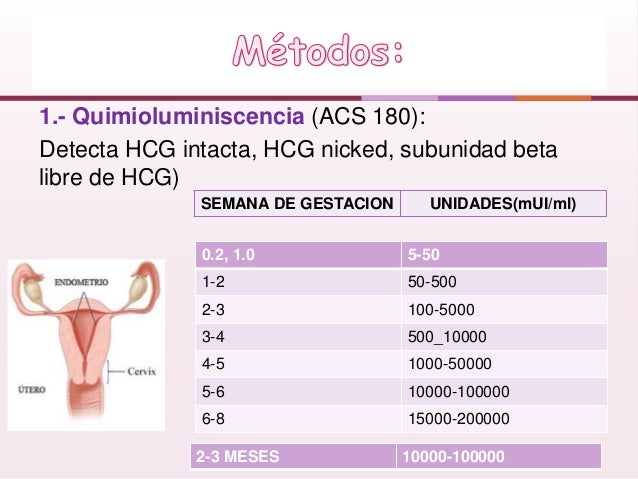 While uncommon, false positive hCG tests can result in unnecessary medical care and/or irreversible surgical procedures. False negatives may be equally concerning and result in a delay in care or diagnostic evaluation. Potential causes of false results are listed and briefly discussed.
While uncommon, false positive hCG tests can result in unnecessary medical care and/or irreversible surgical procedures. False negatives may be equally concerning and result in a delay in care or diagnostic evaluation. Potential causes of false results are listed and briefly discussed.
Serum False Positives (1/1000 to 1/10,000) [5]
Ectopic production of hCG (hydatidiform mole, choriocarcinoma, and germ cell tumors,[6], in addition to multiple myeloma, stomach, liver, lung, bladder, pancreatic, breast, colon, cervical, and endometrial cancers)[7][8][9][10][11]
Heterophile antibodies (autoantibodies and antibodies formed after exposure to animal products that interact with the assay antibodies)[12][13]
Rheumatoid factors (can bind the antibodies in the assay as well)
IgA deficiency[14]
Chronic renal failure or ESRD on hemodialysis (rare)[15]
Red blood cell or plasma transfusion of blood with hCG in it have been reported
Exogenous hCG preparations for weight loss, assisted reproduction, doping[16]
Serum False Negatives
Early measurement after conception
"Hook effect" can occur when hCG levels are about 500,000 mIU/mL.
 [17] This is because there are so many hCG molecules that they saturate both the tracer and the antibodies separately, which doesn't allow for the sandwiching of the tracer-hCG-antibody required for the measurement. This means that all of the complexes are washed away, giving a false-negative result. If gestational trophoblastic disease is suspected, the lab should perform a dilution prior to testing.
[17] This is because there are so many hCG molecules that they saturate both the tracer and the antibodies separately, which doesn't allow for the sandwiching of the tracer-hCG-antibody required for the measurement. This means that all of the complexes are washed away, giving a false-negative result. If gestational trophoblastic disease is suspected, the lab should perform a dilution prior to testing.
Urine False Positives
Blood or protein in the urine
Human error in result interpretation
Ectopic production of hCG
Exogenous hCG
Drugs (aspirin, carbamazepine, methadone, high urinary pH and seminal fluid)[18]
Urine False Negatives
Early measurement after conception
Dilute urine specimen[2]
"Hook effect" as discussed above
Results, Reporting, Critical Findings
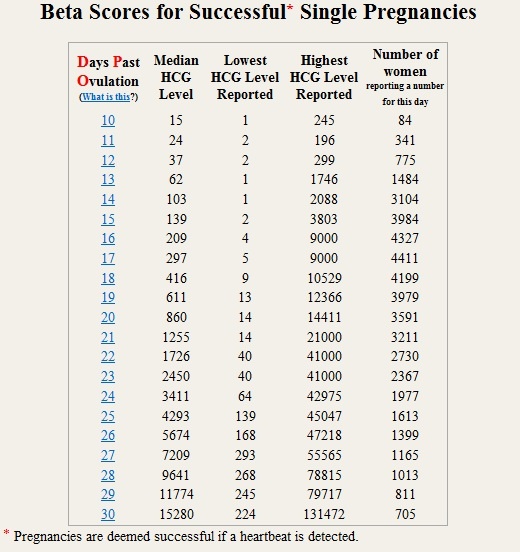
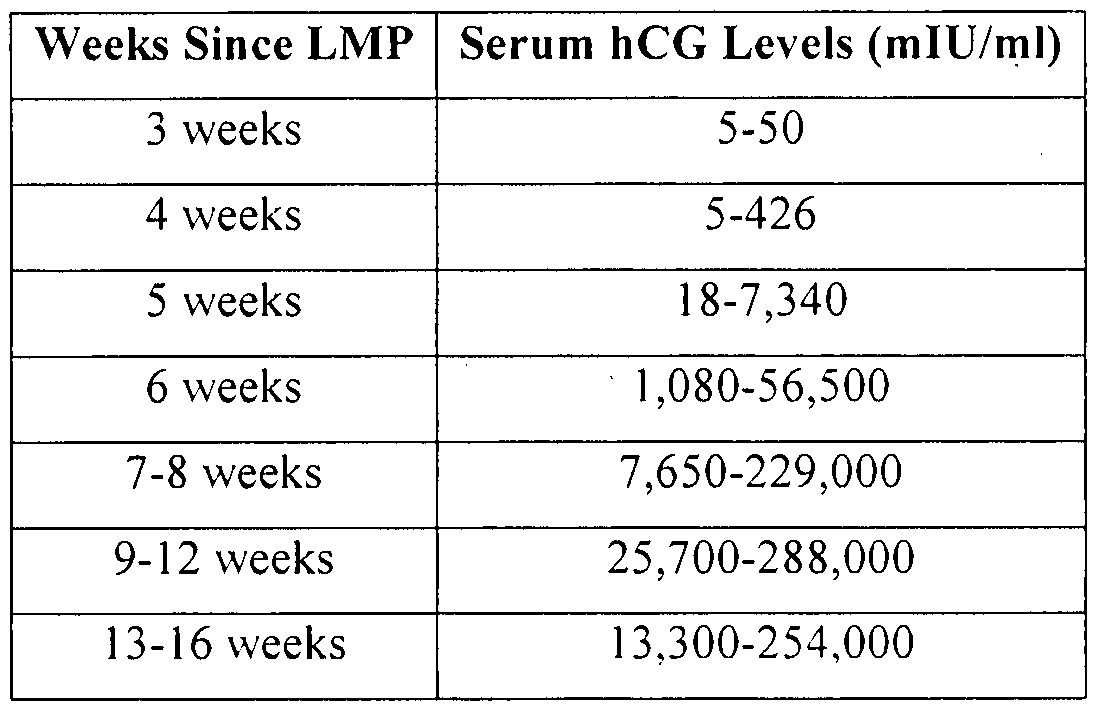
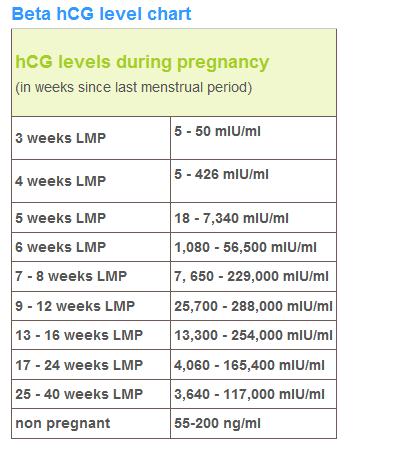
HCG levels are reported in milli-international units of hCG hormone per milliliter of blood, or mIU/mL. International unit per liter (IU/L) may also be used.
International unit per liter (IU/L) may also be used.
Urine hCG testing is qualitative, reporting a positive or negative result. The assays detect hCG levels typically starting at 20 to 50 (reportedly as low as 6.3 to 12.5)[19] mIU/mL, corresponding to levels at approximately 4 weeks post-conception.
Serum assays can measure beta-hCG as low as 1 to 2 mIU/mL.
Clinical Significance
Pregnancy
HCG is an important hormone in pregnancy, and its clinical utility is primarily centered around its detection in early pregnancy, along with serial measurement during pregnancy and pregnancy-related complications.
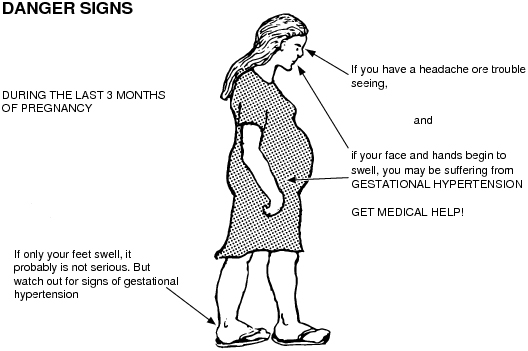
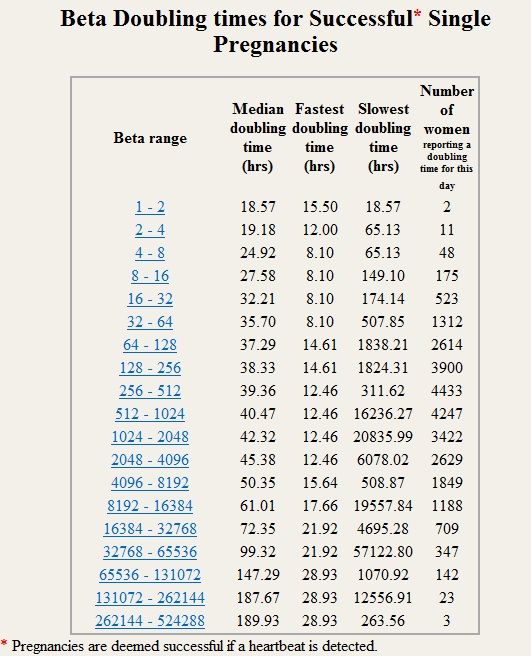
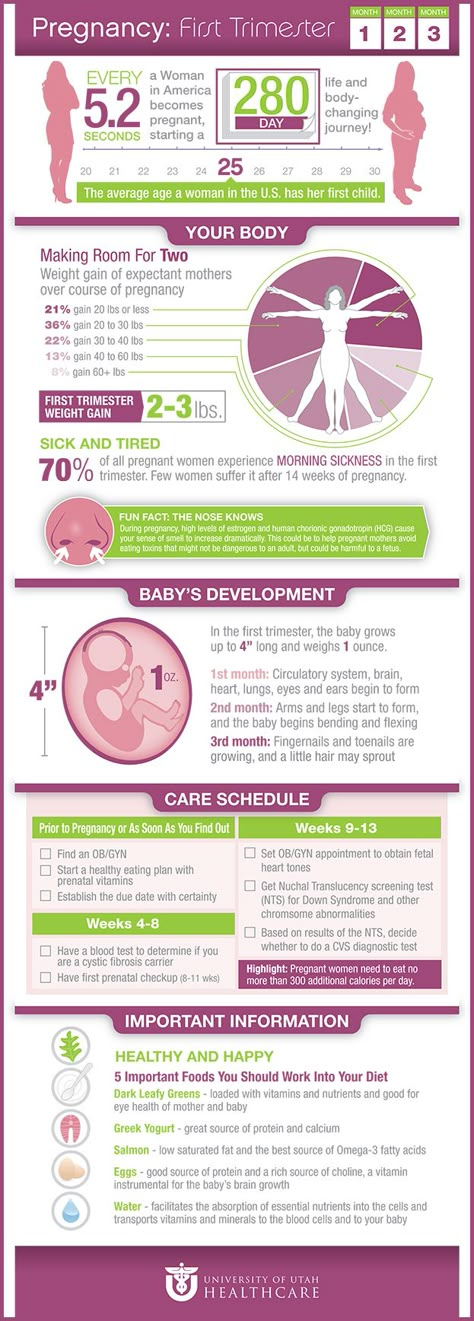
Levels of hCG can vary widely between women with normal pregnancies. Typically, serum and urine concentrations of hCG rise exponentially in the first trimester of pregnancy, doubling about every 24 hours during the first 8 weeks. The peak is usually around 10 weeks of gestation and then levels decrease until about the 16th week of gestation where they remain fairly constant until term. [3]
[3]
Patients who have hCG levels that plateau prior to 8 weeks or that fail to double commonly have a nonviable pregnancy, whether intra-uterine or extra-uterine. Extra-uterine (ectopic) pregnancies usually have a rate-of-rise that is low without the typical doubling. However, given the large range of normal hCG levels and inconsistent rates-of-rise of this hormone, checking serum levels is typically paired with ultrasound evaluation to improve sensitivity and specificity.[20]
Return of hCG to zero following delivery or termination of pregnancy ranges from 7 to 60 days.[21] Trending the fall of hCG levels can be important in termination of molar pregnancies and also following the termination of normal or ectopic pregnancies to be assured that the therapy has been successful.
It notable that there are many different combinations of antibodies used in commercial assays. This results in heterogeneous results with as much as a 50-fold difference in immunoassay results.[3] This is clinically relevant, particularly when comparing results from different laboratories in different facilities/hospitals when examining low values following pregnancy termination or trophoblastic disease.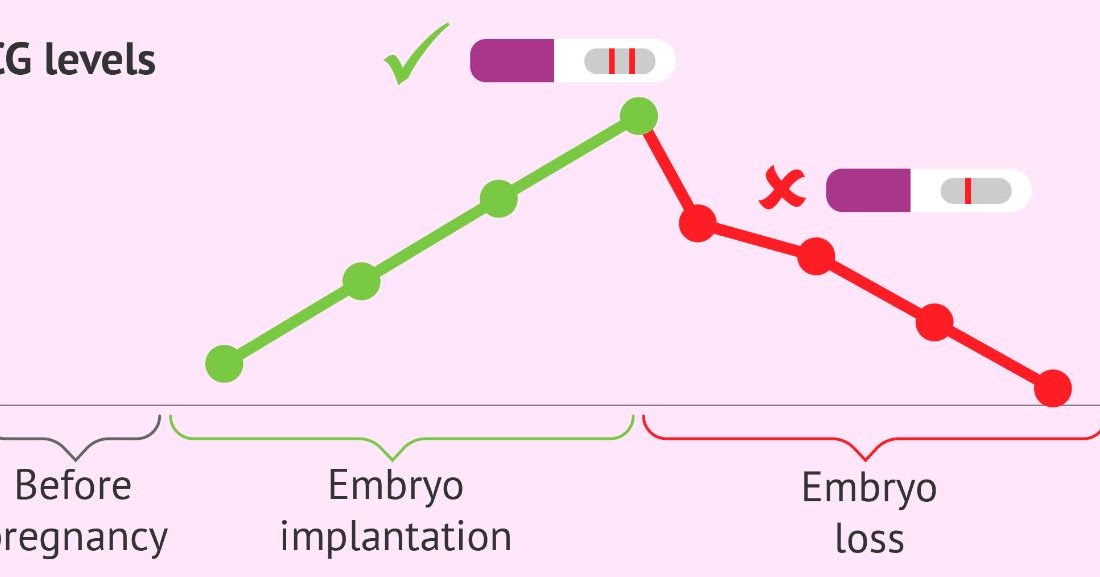
Gestational Trophoblastic Disease
Detection of hCG is also useful in the evaluation of trophoblastic disease, including complete and partial hydatidiform mole, postmolar tumor, gestational choriocarcinoma, testicular choriocarcinoma, and placental site trophoblastic disease. All of these entities produce hCG, varying levels of which are reported on commercial assays. A total hCG level of greater than 100,000 mIU/mL in early pregnancy, for example, is highly suggestive of a complete hydatidiform mole,[22] although many normal pregnancies may reach this level at their peak around weeks 8 to 11 of gestation. Precise hCG measurements are important to assess the tumor mass, the successful treatment of malignancy, and to test for recurrence or persistence of disease.[6]
Non-Pregnant Patients
HCG in the serum increases with age in nonpregnant women. A cut off of 14 mIU/mL has been suggested for use in interpreting results in women over the age of 55. In all nonpregnant patients, testicular cancer, ovarian cancer, bladder cancer, or other malignancy should be evaluated as a source of persistently positive hCG testing.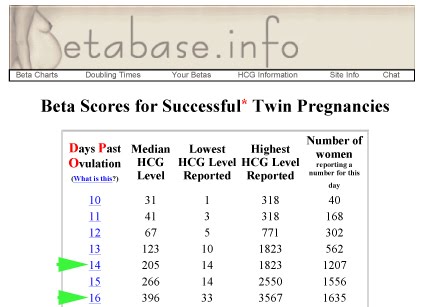
Enhancing Healthcare Team Outcomes
Knowing the utility and variability of different hCG assays is clinically relevant to a wide range of medical providers. False positive and false negative testing has a large impact on patient care. All providers in a patient care team should be aware of common limitations in testing, for example, urine assay false positives with hematuria, false negatives with dilute urine, along with more obscure but still very relevant causes of inaccurate testing. Interpreting results that may be false should be undergone with care to help prevent unnecessary testing and treatment.[23] (Level V) Collaboration, shared decision making, and communication are critical elements in good patient care.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Montagnana M, Trenti T, Aloe R, Cervellin G, Lippi G. Human chorionic gonadotropin in pregnancy diagnostics.
 Clin Chim Acta. 2011 Aug 17;412(17-18):1515-20. [PubMed: 21635878]
Clin Chim Acta. 2011 Aug 17;412(17-18):1515-20. [PubMed: 21635878]- 2.
Ong S, Beebeejaun H. The effect of physiological urine dilution on pregnancy test results in complicated early pregnancies. Br J Obstet Gynaecol. 1999 Jan;106(1):87-8. [PubMed: 10426268]
- 3.
Cole LA. Immunoassay of human chorionic gonadotropin, its free subunits, and metabolites. Clin Chem. 1997 Dec;43(12):2233-43. [PubMed: 9439438]
- 4.
Greene DN, Schmidt RL, Kamer SM, Grenache DG, Hoke C, Lorey TS. Limitations in qualitative point of care hCG tests for detecting early pregnancy. Clin Chim Acta. 2013 Jan 16;415:317-21. [PubMed: 23159297]
- 5.
Braunstein GD. False-positive serum human chorionic gonadotropin results: causes, characteristics, and recognition. Am J Obstet Gynecol. 2002 Jul;187(1):217-24. [PubMed: 12114913]
- 6.
Cole LA, Shahabi S, Butler SA, Mitchell H, Newlands ES, Behrman HR, Verrill HL. Utility of commonly used commercial human chorionic gonadotropin immunoassays in the diagnosis and management of trophoblastic diseases.
 Clin Chem. 2001 Feb;47(2):308-15. [PubMed: 11159780]
Clin Chem. 2001 Feb;47(2):308-15. [PubMed: 11159780]- 7.
Marcillac I, Troalen F, Bidart JM, Ghillani P, Ribrag V, Escudier B, Malassagne B, Droz JP, Lhommé C, Rougier P. Free human chorionic gonadotropin beta subunit in gonadal and nongonadal neoplasms. Cancer Res. 1992 Jul 15;52(14):3901-7. [PubMed: 1377600]
- 8.
Alfthan H, Haglund C, Roberts P, Stenman UH. Elevation of free beta subunit of human choriogonadotropin and core beta fragment of human choriogonadotropin in the serum and urine of patients with malignant pancreatic and biliary disease. Cancer Res. 1992 Sep 01;52(17):4628-33. [PubMed: 1324787]
- 9.
Sheaff MT, Martin JE, Badenoch DF, Baithun SI. beta hCG as a prognostic marker in adenocarcinoma of the prostate. J Clin Pathol. 1996 Apr;49(4):329-32. [PMC free article: PMC500461] [PubMed: 8655711]
- 10.
Lundin M, Nordling S, Carpelan-Holmstrom M, Louhimo J, Alfthan H, Stenman UH, Haglund C. A comparison of serum and tissue hCG beta as prognostic markers in colorectal cancer.
 Anticancer Res. 2000 Nov-Dec;20(6D):4949-51. [PubMed: 11326644]
Anticancer Res. 2000 Nov-Dec;20(6D):4949-51. [PubMed: 11326644]- 11.
Reisenbichler ES, Krontiras H, Hameed O. Beta-human chorionic gonadotropin production associated with phyllodes tumor of the breast: an unusual paraneoplastic phenomenon. Breast J. 2009 Sep-Oct;15(5):527-30. [PubMed: 19624411]
- 12.
Kricka LJ. Human anti-animal antibody interferences in immunological assays. Clin Chem. 1999 Jul;45(7):942-56. [PubMed: 10388468]
- 13.
Check JH, Nowroozi K, Chase JS, Lauer C, Elkins B, Wu CH. False-positive human chorionic gonadotropin levels caused by a heterophile antibody with the immunoradiometric assay. Am J Obstet Gynecol. 1988 Jan;158(1):99-100. [PubMed: 2447778]
- 14.
Knight AK, Bingemann T, Cole L, Cunningham-Rundles C. Frequent false positive beta human chorionic gonadotropin tests in immunoglobulin A deficiency. Clin Exp Immunol. 2005 Aug;141(2):333-7. [PMC free article: PMC1809437] [PubMed: 15996198]
- 15.
Fahy BG, Gouzd VA, Atallah JN. Pregnancy tests with end-stage renal disease. J Clin Anesth. 2008 Dec;20(8):609-13. [PubMed: 19100935]
- 16.
Delbeke FT, Van Eenoo P, De Backer P. Detection of human chorionic gonadotrophin misuse in sports. Int J Sports Med. 1998 May;19(4):287-90. [PubMed: 9657371]
- 17.
Griffey RT, Trent CJ, Bavolek RA, Keeperman JB, Sampson C, Poirier RF. "Hook-like effect" causes false-negative point-of-care urine pregnancy testing in emergency patients. J Emerg Med. 2013 Jan;44(1):155-60. [PubMed: 21835572]
- 18.
Chard T. Pregnancy tests: a review. Hum Reprod. 1992 May;7(5):701-10. [PubMed: 1639991]
- 19.
Cervinski MA, Lockwood CM, Ferguson AM, Odem RR, Stenman UH, Alfthan H, Grenache DG, Gronowski AM. Qualitative point-of-care and over-the-counter urine hCG devices differentially detect the hCG variants of early pregnancy. Clin Chim Acta. 2009 Aug;406(1-2):81-5. [PubMed: 19477170]
- 20.

Davies S, Byrn F, Cole LA. Human chorionic gonadotropin testing for early pregnancy viability and complications. Clin Lab Med. 2003 Jun;23(2):257-64, vii. [PubMed: 12848444]
- 21.
Butts SF, Guo W, Cary MS, Chung K, Takacs P, Sammel MD, Barnhart KT. Predicting the decline in human chorionic gonadotropin in a resolving pregnancy of unknown location. Obstet Gynecol. 2013 Aug;122(2 Pt 1):337-343. [PMC free article: PMC3752097] [PubMed: 23969803]
- 22.
Menczer J, Modan M, Serr DM. Prospective follow-up of patients with hydatidiform mole. Obstet Gynecol. 1980 Mar;55(3):346-9. [PubMed: 7360433]
- 23.
Cole LA. Phantom hCG and phantom choriocarcinoma. Gynecol Oncol. 1998 Nov;71(2):325-9. [PubMed: 9826481]
Low hCG Levels: Causes, Treatments, and Symptoms
Low hCG Levels: Causes, Treatments, and Symptoms- Health Conditions
- Featured
- Breast Cancer
- IBD
- Migraine
- Multiple Sclerosis (MS)
- Rheumatoid Arthritis
- Type 2 Diabetes
- Articles
- Acid Reflux
- ADHD
- Allergies
- Alzheimer's & Dementia
- Bipolar Disorder
- Cancer
- Crohn's Disease
- Chronic Pain
- Cold & Flu
- COPD
- Depression
- Fibromyalgia
- Heart Disease
- High Cholesterol
- HIV
- Hypertension
- IPF
- Osteoarthritis
- Psoriasis
- Skin Disorders and Care
- STDs
- Featured
- Discover
- Wellness Topics
- Nutrition
- Fitness
- Skin Care
- Sexual Health
- Women's Health
- Mental Well-Being
- Sleep
- Product Reviews
- Vitamins & Supplements
- Sleep
- Mental Health
- Nutrition
- At-Home Testing
- CBD
- Men’s Health
- Original Series
- Fresh Food Fast
- Diagnosis Diaries
- You’re Not Alone
- Present Tense
- Video Series
- Youth in Focus
- Healthy Harvest
- No More Silence
- Future of Health
- Wellness Topics
- Plan
- Health Challenges
- Mindful Eating
- Sugar Savvy
- Move Your Body
- Gut Health
- Mood Foods
- Align Your Spine
- Find Care
- Primary Care
- Mental Health
- OB-GYN
- Dermatologists
- Neurologists
- Cardiologists
- Orthopedists
- Lifestyle Quizzes
- Weight Management
- Am I Depressed? A Quiz for Teens
- Are You a Workaholic?
- How Well Do You Sleep?
- Tools & Resources
- Health News
- Find a Diet
- Find Healthy Snacks
- Drugs A-Z
- Health A-Z
- Health Challenges
- Connect
- Breast Cancer
- Inflammatory Bowel Disease
- Psoriatic Arthritis
- Migraine
- Multiple Sclerosis
- Psoriasis
Medically reviewed by Karen Gill, M.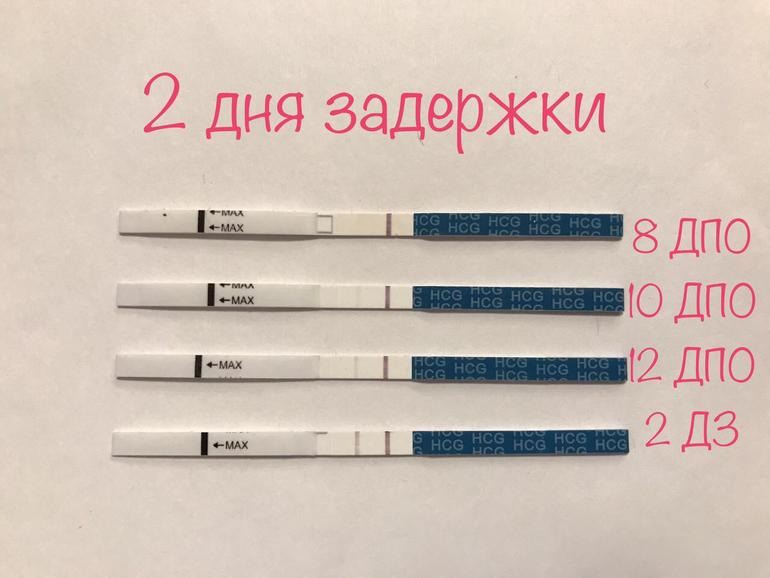 D. — By Becky Young on November 3, 2017
D. — By Becky Young on November 3, 2017
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Read more about our vetting process.What is an hCG test?
Human chorionic gonadotropin (hCG) is a hormone produced by your placenta once an embryo implants in the uterus.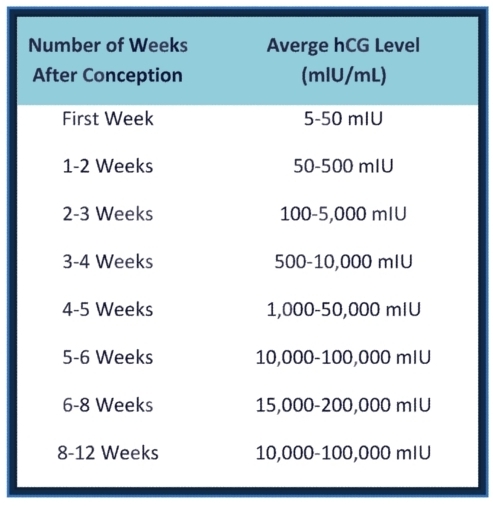
The purpose of the hormone is to tell your body to continue to produce progesterone, which prevents menstruation from occurring. This protects the endometrial uterine lining and your pregnancy.
A pregnancy test can detect hCG in your urine if your levels are high enough. This is how the test identifies that you are pregnant. But only a blood test can give you a precise numerical hCG reading.
Purchase pregnancy tests here.
Standard hCG levels
Standard hCG levels vary quite massively from woman to woman. This is because hCG levels really depend on what is normal for you, how your body responds to pregnancy, as well as how many embryos you are carrying. The way a woman’s body reacts to pregnancy is entirely unique.
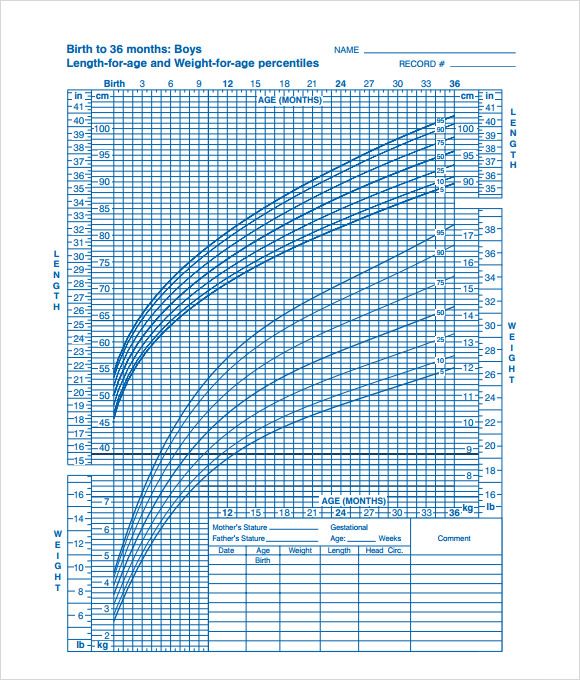
The table below gives you a guideline as to the normal wide range of hCG levels in each week of pregnancy. hCG levels are measured in milli-international units of hCG hormone per milliliter of blood (mIU/mL).
hCG levels usually consistently rise until around week 10–12 of your pregnancy, when the levels plateau or even decrease. This is the reason why pregnancy symptoms can be greater in the first trimester and ease off after this time for many women.
This is the reason why pregnancy symptoms can be greater in the first trimester and ease off after this time for many women.
In early pregnancy, hCG levels usually double every two to three days. Interestingly, when the measurements start off high they don’t expand at the same rate. If they start off more slowly, the increase ends up happening much quicker.
If your hCG levels fall below the normal range, your doctor may want you to have a blood test every two to three days to ensure the levels are increasing. A single measurement of your hCG level is not useful. To give an accurate indication, a series of hCG blood tests needs to be taken a couple of days apart and the readings compared. There is often variation with a rapid increase in numbers, especially in the first few weeks of pregnancy.
Causes of low hCG levels
If your hCG levels fall below the normal range, it’s not necessarily a cause for concern. Many women have gone on to have healthy pregnancies and babies with low hCG levels. Most women don’t ever have cause to find out what their hCG levels are specifically.
However, sometimes low hCG levels can be caused by an underlying problem.
Gestational age miscalculated
Typically, the gestational age of your baby is calculated by the date of your last menstruation. This can be easily miscalculated, particularly if you have a history of irregular periods or are unsure of your dates.
When low hCG levels are detected, it’s often because a pregnancy that was thought to be between 6 and 12 weeks is actually not that far along. An ultrasound and further hCG tests can be used to calculate the gestational age correctly. This is usually the first step when low hCG levels are detected.
Miscarriage
A miscarriage is a pregnancy loss that occurs before 20 weeks of gestation. Sometimes low hCG levels can indicate that you have had or will have a miscarriage. If the pregnancy fails to develop a placenta, then the levels may be normal initially but fail to rise. Common signs that you are experiencing a miscarriage are:
- vaginal bleeding
- abdominal cramps
- passing tissue or clots
- cessation of pregnancy symptoms
- discharge of white/pink mucus
Blighted ovum
This is when an egg is fertilized and attaches to the wall of your womb, but does not continue to develop. When the gestational sac develops, hCG hormone can be released, but the level does not rise since the egg doesn’t develop.
This occurs very early in pregnancy. Most women won’t even know that it’s taken place. Usually you’ll experience your normal menstruation symptoms and assume it’s your usual period. However, if you’re trying to conceive, you may do an early pregnancy test that could pick up the presence of hCG.
Ectopic pregnancy
An ectopic pregnancy is when the fertilized egg remains in the fallopian tube and continues to develop. It’s a dangerous and life-threatening condition, as it may cause the fallopian tube to rupture and bleed excessively. Low hCG levels can help to indicate an ectopic pregnancy. At first the symptoms of an ectopic pregnancy can be similar to those of a normal pregnancy, but as it progresses you can experience the following:
- abdominal or pelvic pain that worsens with straining or movement (this can happen strongly on one side initially and then spread)
- heavy vaginal bleeding
- shoulder pain caused by internal bleeding (the bleeding aggravates the diaphragm and presents as pain at the tip of the shoulder)
- pain during intercourse
- pain during a pelvic examination
- dizziness or fainting due to internal bleeding
- symptoms of shock
How is it treated?
Unfortunately, there is nothing that can be done to treat low hCG levels, though low levels alone are not always a cause for concern.
If your low hCG levels have been caused by a miscarriage, it’s possible that you may need treatment if any pregnancy tissue is left inside your womb. If there’s no tissue retained, then you won’t require any treatment at all. If there is, then there are three treatment options available:
- You can wait for the tissue to pass naturally.
- You can take medication to help you to pass the tissue.
- You can have it surgically removed.
Your doctor will discuss with you what the best course of action is.
The treatments for an ectopic pregnancy are similar. Medications are given to prevent the pregnancy from continuing to grow. If surgery is required, it’s standard for the doctors to remove the affected fallopian tube as well as the pregnancy.
What’s the outlook?
Low hCG levels alone are not necessarily a reason to be worried. There are many factors that affect the levels, and the normal range varies hugely between individual women. Your doctor will be able to monitor your hCG levels for you if you have concerns. Even if they remain low, there is nothing that you can do. It’s also important to remember that low hCG isn’t caused by anything you’ve done.
If your low hCG levels are due to a pregnancy loss, this doesn’t necessarily mean that you won’t be able to get pregnant and carry to term in the future. If you lose a fallopian tube due to an ectopic pregnancy, your fertility shouldn’t change significantly as long as your other tube is functioning. Even if it isn’t, reproductive technologies like in vitro fertilization can help lead to successful pregnancy.
Last medically reviewed on November 3, 2017
- Parenthood
- Pregnancy
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Fan J, et al. (2017). Advances in human chorionic gonadotropin detection technologies: A review.
ncbi.nlm.nih.gov/pubmed/29056064
- Human chorionic gonadotropin (HCG): The pregnancy hormone. (2017).
americanpregnancy.org/while-pregnant/hcg-levels/ - Lawrenz B, et al. (2017). Luteal phase serum progesterone levels after GnRH-agonist trigger – how low is still high enough for an ongoing pregnancy?
ncbi.nlm.nih.gov/pubmed/29037085 - Matson PL, et al. (1990). Measurement of human chorionic gonadotropin during early pregnancy: A comparison of two immunoradiometric assays.
link.springer.com/article/10.1007/BF01135683 - Schumacher A. (2017). Human chorionic gonadotropin as a pivotal endocrine immune regulator initiating and preserving fetal tolerance.
ncbi.nlm.nih.gov/pubmed/29039764
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Nov 3, 2017
Written By
Becky Young
Edited By
Phil Riches
Medically Reviewed By
Karen Richardson Gill, MD
Share this article
Medically reviewed by Karen Gill, M. D. — By Becky Young on November 3, 2017
Read this next
Human Chorionic Gonadotropin (hCG) Blood Test
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
Get the facts on the human chorionic gonadotropin (hCG) blood test. Although it's often used to detect pregnancy, it has other uses such as detecting…
READ MORE
Can Taking Prometrium Vaginally Prevent Miscarriage?
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
Progesterone is known as the “pregnancy hormone.” Without enough progesterone, a woman’s body can’t continue to grow a fertilized egg. If you’ve…
READ MORE
How Many Eggs Are Women Born With? And Other Questions About Egg Supply
Medically reviewed by Amanda Kallen, MD
If you're looking to get pregnant, you may wonder how many eggs you have at various points in life.
The short answer: It goes from millions to none.
READ MORE
How Does Clomid Work for Fertility?
Medically reviewed by Amanda Kallen, MD
Clomid is also known as clomiphene citrate. It’s an oral medication that is often used to treat certain types of female infertility.
READ MORE
Your Guide to the Egg Donation Process
Medically reviewed by Fernando Mariz, MD
There are many reasons you might consider donating your eggs. Learn more about the egg donation process, including possible risks, legal…
READ MORE
What’s the Connection Between Your Biological Clock and Fertility?
Medically reviewed by Amanda Kallen, MD
The biological clock describes the pressure people may feel to get pregnant while at the peak of their reproductive years, before fertility declines.
READ MORE
How Polycystic Ovary Syndrome (PCOS) Affects Fertility and What to Do
Medically reviewed by Amanda Kallen, MD
Polycystic ovary syndrome is a common cause of infertility. We'll discuss why and what you can do.
READ MORE
Human chorionic gonadotropin (hCG)
Human chorionic gonadotropin (hCG) is a special hormone protein that is produced by the membranes of the developing embryo during the entire period of pregnancy. HCG supports the normal development of pregnancy. Thanks to this hormone, the processes that cause menstruation are blocked in the body of a pregnant woman and the production of hormones necessary to maintain pregnancy increases. An increase in the concentration of hCG in the blood and urine of a pregnant woman is one of the earliest signs of pregnancy. HCG consists of two units - alpha and beta hCG. The alpha component of hCG has a similar structure to the units of the hormones TSH, FSH and LH, and the beta hCG is unique. Therefore, in the diagnosis, laboratory analysis of b-hCG is of decisive importance. Small amounts of hCG are produced by the human pituitary gland even in the absence of pregnancy. This explains the fact that in some cases very low concentrations of this hormone are determined in the blood of non-pregnant women (including women during menopause) and even in the blood of men.
Study preparation
The study is carried out in the morning, on an empty stomach. At least 8 hours must have elapsed since the last meal.
It is recommended to conduct a study no earlier than 3-6 days late menstruation in order to avoid false negative results. In case of doubtful results, the test should be carried out twice with an interval of 2-3 days. When determining the completeness of the removal of an ectopic pregnancy or abortion, an hCG test is performed 1-2 days after the operation, to exclude a false positive result.
Indications for examination
- Amenorrhea
- Early diagnosis of pregnancy
- Suspicion of ectopic pregnancy
- Evaluation of the completeness of operative termination of pregnancy
- Dynamic monitoring of pregnancy
- Suspicion of threatened miscarriage and not developing pregnancy
- Diagnosis of trophoblastic diseases (chorioepithelioma, hydatidiform mole)
- Monitoring the effectiveness of the treatment of trophoblastic diseases
- Dynamic follow-up after trophoblastic disease
- Prenatal diagnosis (part of the triple test together with AFP and free estriol)
Interpretation
Reference values: unit MME/ml.
| Norm | Norm |
| General norm for women | <5.3 |
| General norm for men | <5.3 |
| Pregnancy: 3-4 weeks | 0. |
| Pregnancy: 4-5 weeks | 101-4870 |
| Pregnancy: 5-6 weeks | 1110-31500 |
| Pregnancy: 6-7 weeks | 2560-82300 |
| Pregnancy: 7-8 weeks | 23100-151000 |
| Pregnancy: 8-9 weeks | 27300-233000 |
| Pregnancy: 9-13 weeks | 20900-291000 |
| Pregnancy: 13-18 weeks | 6140-103000 |
| Pregnancy: 18-23 weeks | 4720-80100 |
| Pregnancy: 23-41 weeks | 2700-78100 |
There are no strict standards for the content of hCG in the blood of pregnant women. HCG levels at the same gestational age can vary significantly from woman to woman. In this regard, single measurements of hCG levels are not very informative. To assess the development of pregnancy, the dynamics of changes in the concentration of hCG in the blood is important. With the normal development of pregnancy, hCG is determined in the blood of pregnant women from about 8-11-14 days after conception. The level of hCG rises rapidly and, starting from the 3rd week of pregnancy, doubles approximately every 2-3 days. The increase in the concentration of hCG in the blood of a pregnant woman continues until about 11-12 weeks of pregnancy. Between 12 and 22 weeks of pregnancy, the concentration of hCG decreases slightly. From 22 weeks until delivery, the concentration of hCG in the blood of a pregnant woman begins to increase again, but more slowly than at the beginning of pregnancy.
Increased performance
HCG in the blood of men and non-pregnant women can indicate the presence of oncological diseases of the intestines, lungs, kidneys, uterus or testicles and other organs. In addition, a high level of human chorionic gonadotropin is fixed within 4-5 days after an abortion and due to the intake of drugs containing hCG. In pregnant women, the level of hCG rises noticeably as a result of:
- multiple pregnancy;
- diabetes mellitus;
- early toxicosis, preeclampsia;
- prolonged pregnancy;
- fetal chromosomal abnormalities;
- taking synthetic gestagens - drugs that replenish the level of the main female hormone - progesterone in the body.
Low levels of hCG in pregnant women require careful consideration and immediate referral to specialists. A decrease in the level by more than 50% of the norm may be evidence of an ectopic or non-developing pregnancy, a threatened miscarriage, placental insufficiency, a true overcarriage of pregnancy, and intrauterine fetal death in the later stages.
Results may be affected
When diagnosing pregnancy, taking the test too early - when less than 5 days have passed since conception - can lead to a false negative result.
Assigned in combination with
Alpha-fetoprotein (alpha-FP)
Estriol free >
Pregnancy - prenatal screening for trisomies of the first trimester of pregnancy (Down's syndrome)
Pregnancy-associated plasma protein-A (PAPP-A)
hcg. What does this hormone show? Indications, preparation, interpretation
One of the main tests during pregnancy is the study of the level of the pregnancy hormone hCG or human chorionic gonadotropin.
hCG is a protein with hormonal activity, which begins to be produced by the tissue after implantation of the embryo as early as 6-8 days after fertilization of the egg and is one of the most important indicators of the presence and successful development of pregnancy.
HCG is necessary for the development and maintenance of pregnancy, it blocks the menstrual cycle and activates the production of other hormones necessary to maintain pregnancy - estrogen and progesterone.
In the future, monitoring of hCG is necessary for doctors to detect certain pathologies in the development of the fetus. The level of hCG rises not only during normal pregnancy, but also during ectopic, as well as within a few days after an abortion, and with some hormonally active tumors.
HCG in oncology is an indicator of a number of tumors (trophoblastic and testicular).
Main indications for use:
Screening of pregnant women in order to detect chromosomal abnormalities in the fetus in the first trimester (trisomy 21 chromosome - Down syndrome, trisomy 18 chromosome), diagnosis of malignant tumors, as in women (hormepitemoma). Same for men (testicular tumors)
The main functions of hCG in the body of a woman and fetus during pregnancy include: growth of the corpus luteum in which progesterone and estradiol are produced, necessary for the normal development of the fetus in the early stages of pregnancy
3-hCG causes the production of testosterone in the testes of the male fetus, before the birth of the child, which is necessary for the normal formation of male sexual characteristics
HCG is one of the earliest markers of pregnancy. Its concentration increases until the end of the first trimester, and then decreases
When preparing for donating blood for hCG, no restrictions on diet and diet are required
The main distorting factor is hemolysis. And the factors that increase the result are menotropins (Pergonal, drugs with FSH)
Indications for the study:
fetus)
- diagnosis of trophoblast tumors (hydatidiform mole, choriocarcinoma), as well as other tumors that secrete hCG.