Parts of pelvic girdle
Anatomy, Abdomen and Pelvis, Bones (Ilium, Ischium, and Pubis) - StatPearls
Introduction
The pelvis is a group of fused bones and may be considered the first step in the linkage of the axial skeleton (bones of the head, neck, and vertebrae) to the lower appendages. The part of the axial skeleton directly communicating with the pelvis is the lumbar spinal column. The femur is the appendicular skeletal bone connected to the pelvis at the acetabulum, a bony ring formed by the fusion of three bones: the ilium, ischium, and pubis. The main function of the pelvis is support for locomotion, as it provides attachment points for muscles, tendons, and ligaments. While stiff joints bind the axial skeleton to the pelvis, the appendicular skeleton is joined via a relatively free-floating ball and socket joint between the femur and the acetabulum to allow maximal mobility of the joint.[1]
In discussing the pelvis, a distinction can be made between the "pelvic spine" and the "pelvic girdle. " The pelvic girdle, also known as the os coxae, Latin for “bone of the hip,” consists of the fused bones identified individually as the ilium, ischium, and pubis. The ring of this girdle is closed in the anterior by the pubic symphysis between the left and right pubic bones, and in the posterior between the left and right ilia and the sacrum at the sacroiliac joints. The pelvic spine consists of the sacrum and coccyx. Together these two parts form the bony pelvis.
Structure and Function
The adage “structure informs function” rings true in the pelvis. The os coxae, or hip bones as they are known colloquially, are attached dorsally to the sacrum by sacroiliac ligaments. In addition to the ligaments of this joint, the interposing areas of the sacrum and the ilium have matching, irregular contours to increase joint strength. The relatively fixed joint between the sacrum and the lumbar spine is ideal for bearing the load of the upper body. At the most ventral area of the pelvis, there is a fibrocartilaginous joint in the pubic symphysis. It is amphiarthrotic, meaning that it is quite firm but allows limited movement similar to the intervertebral joints. This allows the joint to resist shearing forces during movement while still accommodating expansion during labor.
It is amphiarthrotic, meaning that it is quite firm but allows limited movement similar to the intervertebral joints. This allows the joint to resist shearing forces during movement while still accommodating expansion during labor.
Three major ligaments stabilize the femur in the acetabulum, one for each part of the os coxae. The iliofemoral ligament is the most anterior and has a “Y” appearance. It works to prevent hyperextension of the hip. The ischiofemoral ligament is posterior and works to prevent over-abduction along with the pubofemoral ligament located medially. All of these ligaments attach to the acetabular labrum, which is a lip of connective tissue around the acetabulum that deepens the socket of the ball-and-socket joint to increase stability and resist dislocation.
Other ligaments of note in the acetabulum are the transverse acetabular ligament and the ligament of the head of the femur, or ligamentum teres femoris (Latin for round ligament of the femur.) The transverse acetabular ligament is a strong band of connective fibers that traverse the acetabular notch on the inferior aspect of the acetabulum, this creates a foramen for nutrient-supplying blood vessels to enter the hip joint while still maintaining the structural integrity of the joint.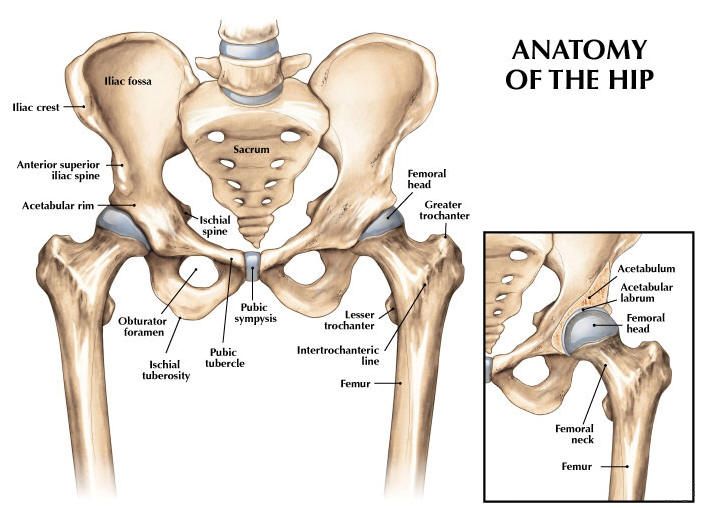 Much as its name implies, the ligament of the head of the femur is connected to the head of the femur at the center of the acetabulum. However, rather than providing support, its main function is to house the artery to the head of the femur, which provides blood to the head of the femur via a branch from the obturator artery. Disruption in perfusion to the femoral head from any cause can result in degradation and even collapse of the femur inside the acetabulum. This disease process is known as avascular necrosis or Legg-Calve-Perthes disease in children.
Much as its name implies, the ligament of the head of the femur is connected to the head of the femur at the center of the acetabulum. However, rather than providing support, its main function is to house the artery to the head of the femur, which provides blood to the head of the femur via a branch from the obturator artery. Disruption in perfusion to the femoral head from any cause can result in degradation and even collapse of the femur inside the acetabulum. This disease process is known as avascular necrosis or Legg-Calve-Perthes disease in children.
There are two notches of note in the bony pelvis: the greater and lesser sciatic notches. The greater notch is on the ileum, whereas the lesser sciatic notch is located inferiorly on the ischium just below the ischial spine. The sacrotuberous ligament runs from the sacrum to the ischial tuberosities and crosses near the greater sciatic notch to form the greater sciatic foramen. Similarly, the sacrospinous ligament runs from the sacrum to the ischial spine to form the lesser sciatic foramen.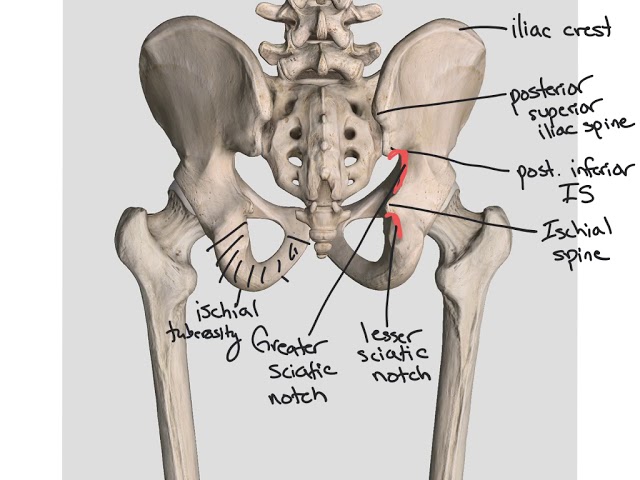 The greater sciatic foramen contains multiple clinically notable structures, such as the sciatic nerve, the superior and inferior gluteal nerves, the pudendal nerve, the nerve to quadratus femoris, nerve to obturator internus, as well as the superior and inferior gluteal vessels and internal pudendal vessels. Finally, the piriformis also passes through this foramen. The lesser sciatic foramen contains the tendon of obturator internus, as well as the pudendal nerve and vessels coming from the greater foramen on their way to the perineum and gonads. Although somewhat controversial, it is considered possible for the piriformis muscle to cause nerve entrapment, known as piriformis syndrome. It presents with symptoms of sciatica and tenderness near the sciatic notch but remains a diagnosis of exclusion.[2]
The greater sciatic foramen contains multiple clinically notable structures, such as the sciatic nerve, the superior and inferior gluteal nerves, the pudendal nerve, the nerve to quadratus femoris, nerve to obturator internus, as well as the superior and inferior gluteal vessels and internal pudendal vessels. Finally, the piriformis also passes through this foramen. The lesser sciatic foramen contains the tendon of obturator internus, as well as the pudendal nerve and vessels coming from the greater foramen on their way to the perineum and gonads. Although somewhat controversial, it is considered possible for the piriformis muscle to cause nerve entrapment, known as piriformis syndrome. It presents with symptoms of sciatica and tenderness near the sciatic notch but remains a diagnosis of exclusion.[2]
Another eye-catching structure in the os coxae is the obturator foramen. The superior and inferior rami of the ischium and pubis bones come together to form this ring-like structure on each side of the pelvis.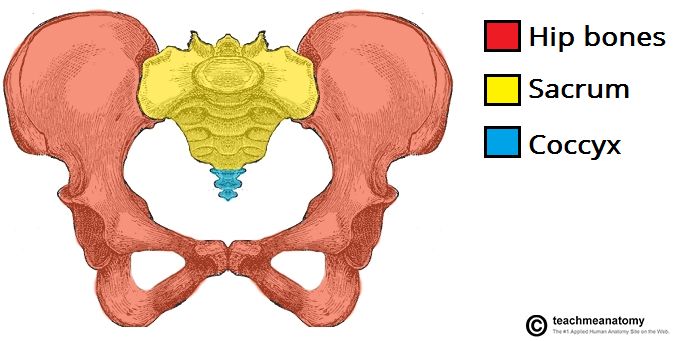 This ring is covered by the obturator membrane, which leaves a small opening known as the obturator canal through which the obturator neurovascular bundle passes. The internal and external sides of the membrane are connected to the respectively named internal and external obturator muscles responsible for external rotation of the hip and stabilization during ambulation.
This ring is covered by the obturator membrane, which leaves a small opening known as the obturator canal through which the obturator neurovascular bundle passes. The internal and external sides of the membrane are connected to the respectively named internal and external obturator muscles responsible for external rotation of the hip and stabilization during ambulation.
The pelvis has both an inlet and an outlet, also known as the superior and inferior apertures, as it forms somewhat of a funnel. The pelvic inlet is marked by the pelvic brim, a bony ring made up of the sacral prominence posteriorly, the arcuate line of the ilium laterally, and the pectineal line of the pubis and pubic symphysis anteriorly. The wings of the ilium extending above this line form the greater, or “false” pelvis, and the area below this line forms the lesser or “true” pelvis. The outlet of the pelvis is marked posteromedially by the coccyx, posterolaterally by the sacrotuberous ligaments connecting the sacrum to the ischial tuberosities, laterally by the ischial bones, and anteriorly by the pubic arch of the pubic bones.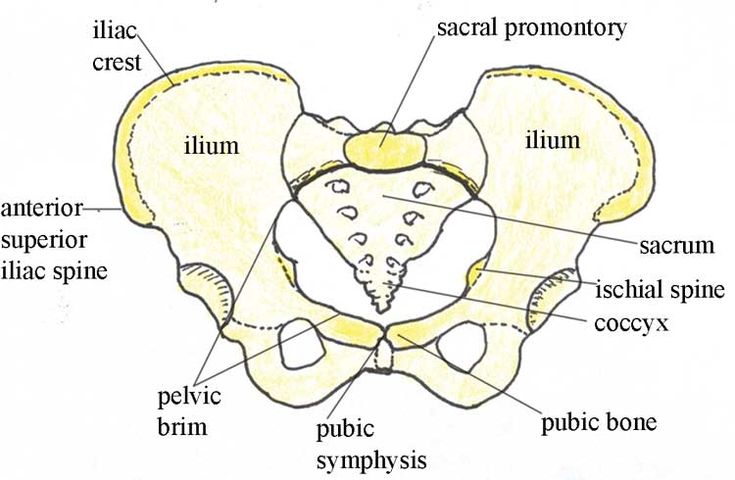
The pelvis has a "floor" at this outlet that serves multiple functions. The first function is to contain the visceral organs in the caudal region of the pelvis and help prevent organ prolapse through the pelvic outlet. The second function is to maintain the continence of the anus and urinary tract through several layers of musculature and ligaments. These pelvic floor muscles are complex and will be described further in the “Muscles” section.
Embryology
The earliest appendicular skeletal elements appear at approximately 28 days, which coincides with the appearance of limb buds. Condensation of mesenchymal tissue in the limb buds become scaffolds for bone formation in the fifth week. These models undergo chondrification to form hyaline cartilage beginning in the sixth week. At this point, imaging can discern a basic skeletal system. By the time the fetus reaches the gestational age of nine weeks (seven weeks after fertilization), chondrification centers in the ilium, ischium, and pubis first appear and grow rapidly. The following week the first ossification center begins to replace cartilage in the iliac crest. At the same time, the fusion of the sacrum and ilium occurs. After the tenth week of gestation, the fusion of all the bones of the pelvic girdle has occurred. Secondary ossification continues postnatally, and complete ossification is not achieved until adulthood. [3]
The following week the first ossification center begins to replace cartilage in the iliac crest. At the same time, the fusion of the sacrum and ilium occurs. After the tenth week of gestation, the fusion of all the bones of the pelvic girdle has occurred. Secondary ossification continues postnatally, and complete ossification is not achieved until adulthood. [3]
Blood Supply and Lymphatics
The aorta bifurcates into the common iliac arteries at the level of the L4 vertebra. At the pelvic brim, the common iliac arteries bifurcate into the internal and external iliac arteries. The external iliac exits the pelvis underneath the inguinal ligament and becomes the femoral artery to supply the lower extremity with blood. The internal iliac artery supplies the pelvic organs, perineal floor, and gluteal muscles with blood. It has 2 major branches, known as the anterior and posterior divisions.
The anterior division supplies the upper part of the bladder via the superior vesicular artery and umbilical artery in the fetus.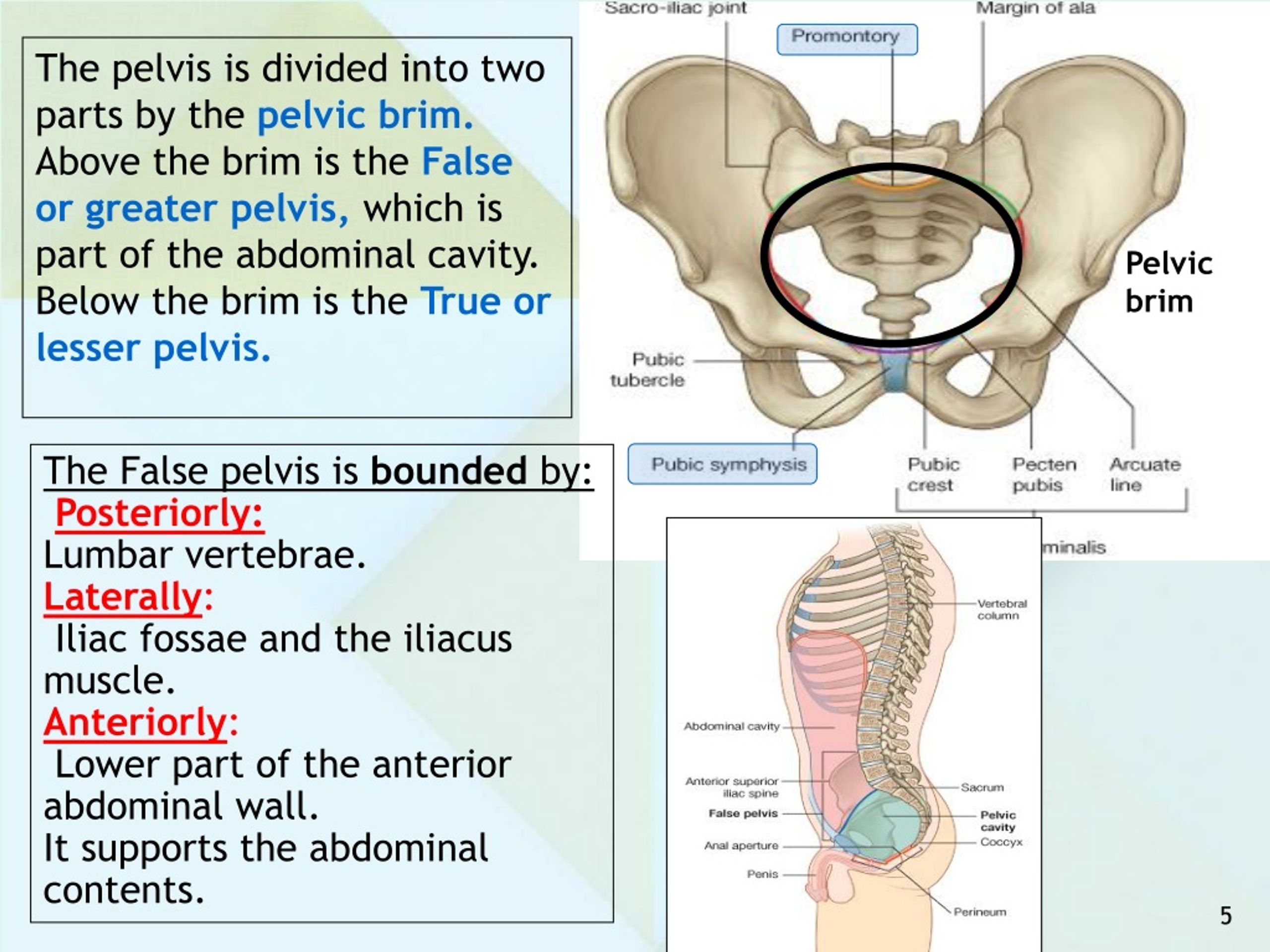 In adults the umbilical artery becomes obliterated and the remnant is known as the medial umbilical ligament. The trigone of the bladder, prostate, and seminal glands are supplied with blood by the inferior vesical artery. The internal pudendal artery supplies the perineal muscles and skin as well as the penis and clitoris. The middle rectal artery supplies the rectum with blood. The obturator artery supplies the pelvic floor, head of the femur, and ilium. The inferior gluteal artery provides circulation to the gluteal region, head of the femur, upper thigh, and sciatic nerve. In women, the uterine artery supplies blood to the uterus, fallopian tube, ovary, cervix, and vagina.
In adults the umbilical artery becomes obliterated and the remnant is known as the medial umbilical ligament. The trigone of the bladder, prostate, and seminal glands are supplied with blood by the inferior vesical artery. The internal pudendal artery supplies the perineal muscles and skin as well as the penis and clitoris. The middle rectal artery supplies the rectum with blood. The obturator artery supplies the pelvic floor, head of the femur, and ilium. The inferior gluteal artery provides circulation to the gluteal region, head of the femur, upper thigh, and sciatic nerve. In women, the uterine artery supplies blood to the uterus, fallopian tube, ovary, cervix, and vagina.
The posterior division includes three main branches. The iliolumbar artery supplies blood to the psoas major, iliacus, and quadratus lumborum muscles. The lateral sacral arteries supply blood to the sacral meninges and skin over the sacrum as well as the coccyx where it anastomoses with the middle sacral artery from the aorta.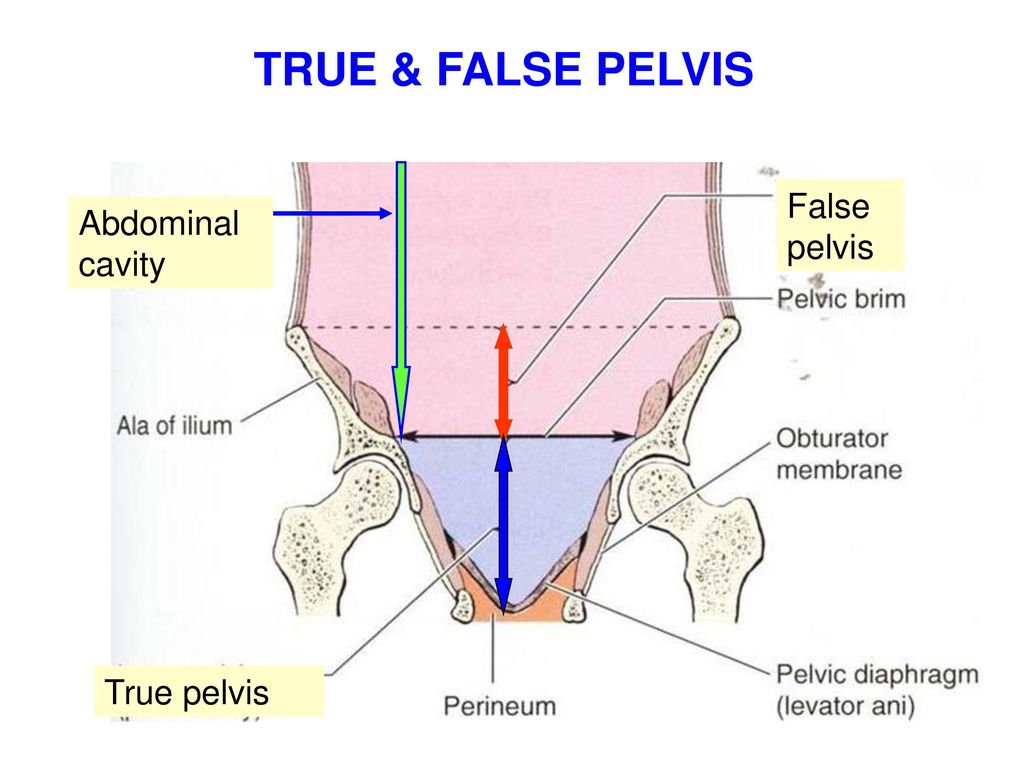 The superior gluteal artery supplies blood to the gluteal muscles and anastomoses around the hip as well as the ASIS.
The superior gluteal artery supplies blood to the gluteal muscles and anastomoses around the hip as well as the ASIS.
The ovarian artery branches from the aorta and travels within the suspensory ligament of the ovary to supply blood to the ovaries. The testicular arteries also originate from the aorta and pass through the inguinal canal to supply the testes.
There are several groups of lymph nodes in the pelvis. Some surround vasculature like the external, internal, and common iliac nodes. There are also sacral, pararectal, lumber, and inguinal nodes. These nodes are important in staging the spread of cancers in the pelvic area and can even be used to localize malignancies based on nodal involvement. For example, the testes, ovaries, and uterus drain to para-aortic nodes, while the lower rectum, bladder, vagina, cervix, and prostate drain into the internal iliac nodes. Lastly, the anal canal, scrotum, vulva, and most of the skin below the umbilicus drain into the superficial inguinal nodes.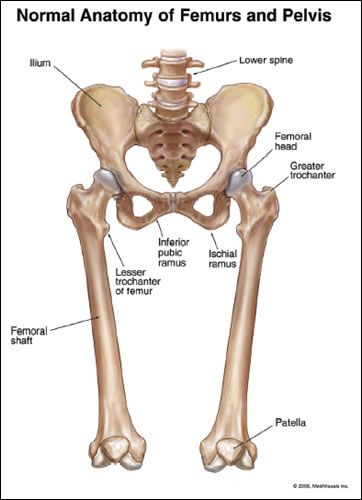
Nerves
There are multiple plexuses of nerves that provide motor and sensory innervation to the pelvis. [4]
The sacral plexus arises from L4-S4 spinal nerves. It includes the largest nerve in the body, the sciatic nerve, which contains nerves from spinal levels L4-S3. The sciatic nerve innervates most of the skin of the leg as well as many muscles of the thigh and leg. It is composed of two bundles of nerve tracts, called the tibial and fibular division, which split at the level of the knee into the tibial and fibular nerves. The pudendal nerve (S2-S4) innervates the skin and muscles of the perineum. The superior gluteal nerve (L4-S1) and the inferior gluteal nerve (L5-S2) innervate the gluteal muscles. The nerve to the quadratus femoris (L4-S1) innervates the quadratus femoris and gemellus inferior muscles of the hip. The nerve to the obturator internus muscle (L5-S2) innervates said muscle. The nerve to the piriformis (S1-S2) similarly innervates its eponymous muscle. The perforating cutaneous nerve (S2-S3) innervates the medial and lower part of the buttock. The posterior femoral cutaneous nerve (S2-S3) innervates the skin on the posterior thigh/leg and the perineum. The pelvic splanchnic nerves (S2-S4) provide parasympathetic innervation to pelvic organs.
The perforating cutaneous nerve (S2-S3) innervates the medial and lower part of the buttock. The posterior femoral cutaneous nerve (S2-S3) innervates the skin on the posterior thigh/leg and the perineum. The pelvic splanchnic nerves (S2-S4) provide parasympathetic innervation to pelvic organs.
The coccygeal plexus (S4-S5) and coccygeal nerves innervate the coccygeus and levator ani muscles, as well as the skin immediately dorsal to the anus.
The lumbar plexus (L2-L4) gives rise to the obturator nerve that innervates the skin of the medial aspect of the thigh and the hip adductor muscles.
The superior hypogastric plexus provides sympathetic innervation to the pelvis, while the inferior hypogastric plexus contains both parasympathetic and sympathetic fibers. The pelvic splanchnic nerves (S2-S4) provide parasympathetic innervation to pelvic organs. Parasympathetic output causes gastrointestinal peristalsis and contracts muscles for defecation and urination. It is also involved in the engorgement of erectile tissue.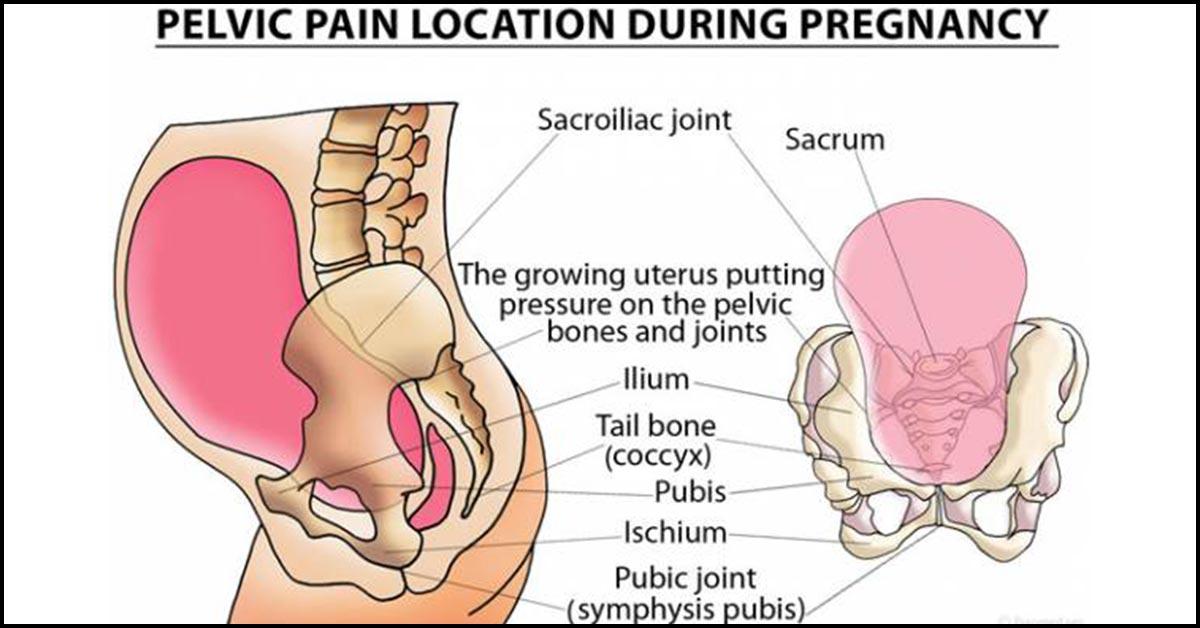 Sympathetic output acts antagonistically to the parasympathetic output and is involved in muscle contraction during orgasm.
Sympathetic output acts antagonistically to the parasympathetic output and is involved in muscle contraction during orgasm.
Muscles
The muscles of the pelvis can be divided into 3 groups. Some muscles attach to the trunk and provide postural support. Other muscles attach to the hip and thigh and allow for movement. Finally, the muscles of the pelvic floor and perineum are involved in support of the pelvic floor as well as urogenital and gastrointestinal functions. [5][6]
The iliopsoas muscle attaches the spine to the pelvis at the iliac fossa and the spine to the femur at the lesser trochanter. It flexes the hip, which is the action performed during a “sit-up.” The gluteus maximus muscle is the primary hip extensor and composes most of the mass of the buttocks. It originates at the ilium and sacrum and attaches to the gluteal tuberosity of the femur as well as the iliotibial band. The iliotibial band is a band of connective tissue on the lateral thigh running from the iliac crest to the proximal anterolateral tibia.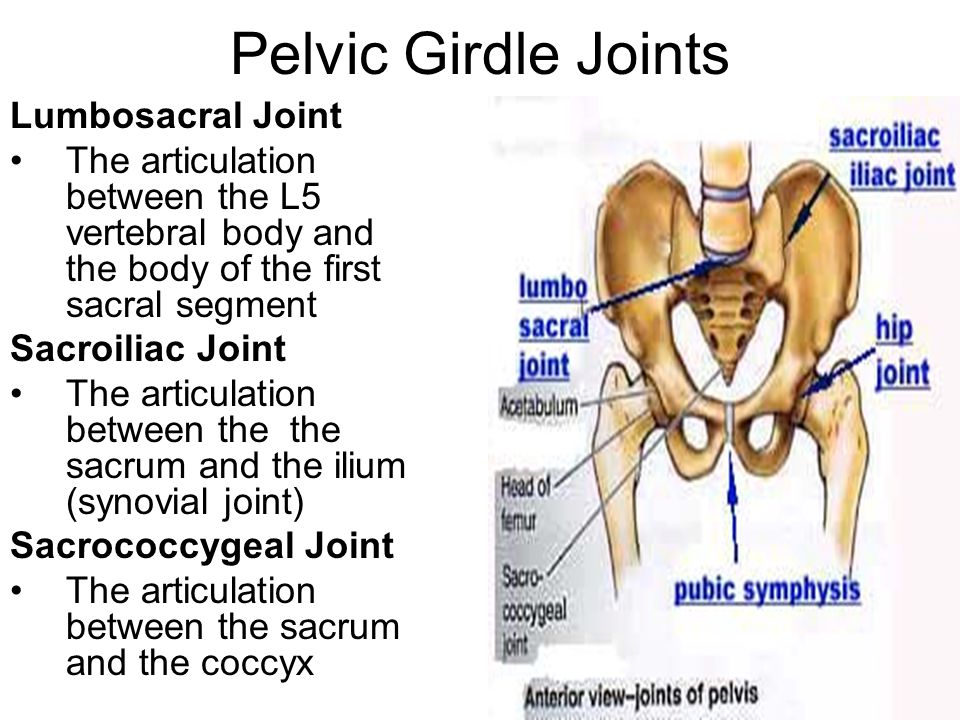 The gluteus medius, located deep to the gluteus maximus, runs from the ilium to the greater trochanter of the femur. It serves to externally rotate and abduct the hip as well as balance the pelvis during ambulation. Weakness of this muscle, as can be found with superior gluteal nerve injuries, will result in a Trendelenburg gait, where the contralateral hip drops while walking. Like the gluteus maximus, it also attaches to the iliotibial band. The superior portion of the iliotibial band blends with the muscle fibers of the tensor fascia lata, which aids with stabilization and hip abduction. This “IT” band can be a source of discomfort for runners, known as iliotibial band syndrome.[7] The gluteus minimus is located just inferior to the gluteus medius. It also runs from the ilium to the greater trochanter of the femur and assists the gluteus medius to abduct the hip.
The gluteus medius, located deep to the gluteus maximus, runs from the ilium to the greater trochanter of the femur. It serves to externally rotate and abduct the hip as well as balance the pelvis during ambulation. Weakness of this muscle, as can be found with superior gluteal nerve injuries, will result in a Trendelenburg gait, where the contralateral hip drops while walking. Like the gluteus maximus, it also attaches to the iliotibial band. The superior portion of the iliotibial band blends with the muscle fibers of the tensor fascia lata, which aids with stabilization and hip abduction. This “IT” band can be a source of discomfort for runners, known as iliotibial band syndrome.[7] The gluteus minimus is located just inferior to the gluteus medius. It also runs from the ilium to the greater trochanter of the femur and assists the gluteus medius to abduct the hip.
Another group of six muscles works to externally rotate the hip: the piriformis, gemellus superior, gemellus inferior, obturator internus, obturator externus, and quadratus femoris.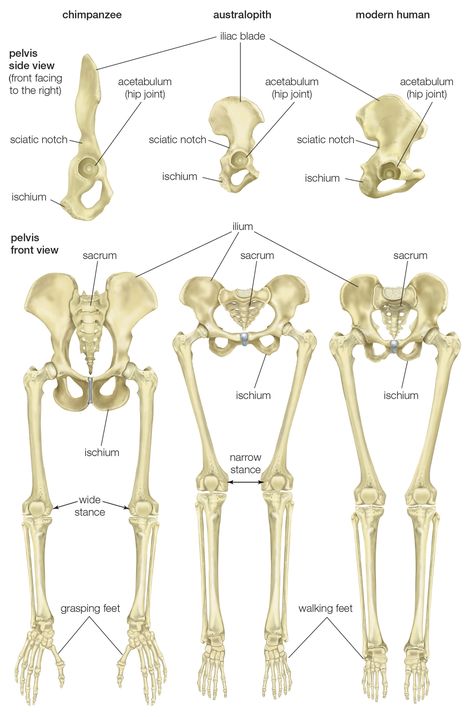 Due to their shared function, this group of muscles is known as the lateral rotator group. The piriformis originates on the sacrum and inserts on the greater trochanter. The gemellus (Latin for “twin”) superior and inferior muscles originate on the ischium and insert indirectly onto the greater trochanter by blending with the tendon of the obturator internus originating from the obturator membrane. The obturator externus also functions as a hip adductor and originates on the ischiopubic ramus and inserts into the trochanteric fossa. Finally, the quadratus femoris originates on the ischium and inserts on the intertrochanteric crest.
Due to their shared function, this group of muscles is known as the lateral rotator group. The piriformis originates on the sacrum and inserts on the greater trochanter. The gemellus (Latin for “twin”) superior and inferior muscles originate on the ischium and insert indirectly onto the greater trochanter by blending with the tendon of the obturator internus originating from the obturator membrane. The obturator externus also functions as a hip adductor and originates on the ischiopubic ramus and inserts into the trochanteric fossa. Finally, the quadratus femoris originates on the ischium and inserts on the intertrochanteric crest.
Other muscles assisting with external rotation outside of these include the lower fibers of the gluteus maximus, the gluteus medius, and gluteus minimus when the hip is extended (if flexed they internally rotate the hip,) the psoas, and sartorius muscles. The sartorius originates on the anterior superior iliac spine and inserts on the pes anserinus in the tibia.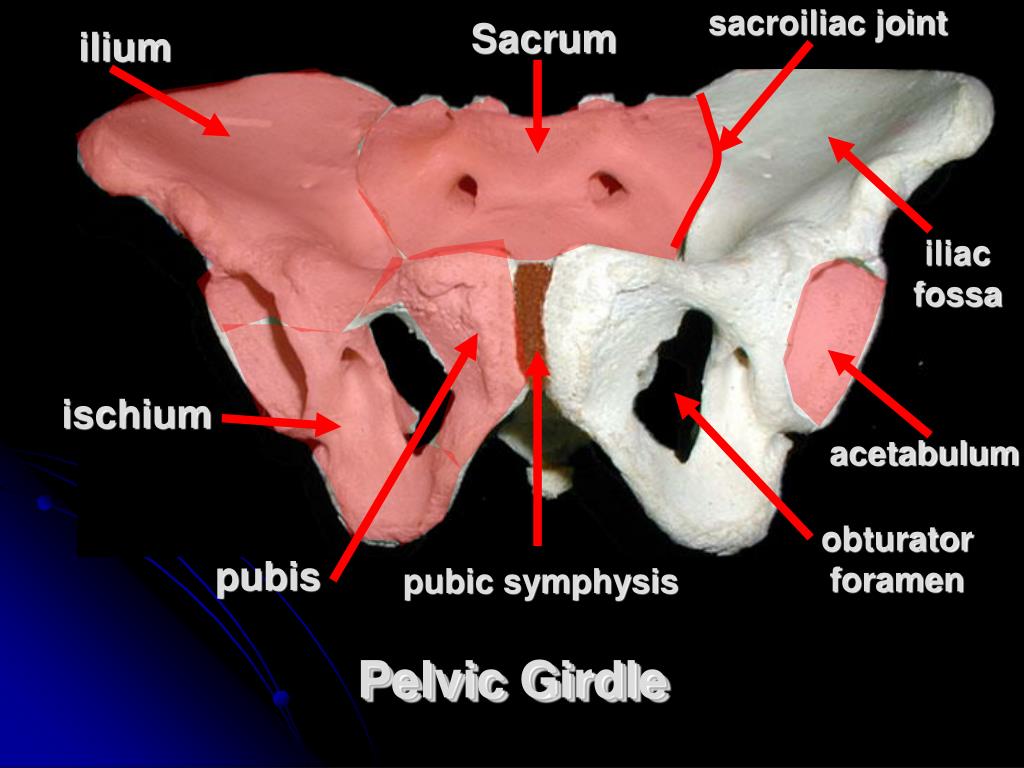 It has four functions: flexion, abduction, and lateral rotation of the hip as well as flexion of the knee. The name comes from the Latin word for tailor, and all four actions can be performed to look at the sole of one’s shoe.
It has four functions: flexion, abduction, and lateral rotation of the hip as well as flexion of the knee. The name comes from the Latin word for tailor, and all four actions can be performed to look at the sole of one’s shoe.
The hip adductors are large muscles on the medial thigh that adduct the leg and share a common innervation in the obturator nerve. They include the adductor longus, adductor brevis, adductor magnus, gracilis, pectineus, and obturator externus muscles. The adductor longus, brevis, and magnus muscles originate on the pubic bone and insert on the linea aspera of the femur. The adductor magnus also has some fibers originating on the ischial tuberosity and additional insertions on the adductor tubercle, as well as some innervation from the tibial nerve. The gracilis originates on the pubic bone and inserts on the pes anserinus of the tibia along with the sartorius. The pectineus originates on the pectineal line of the pubic bone and inserts on the pectineal line of the femur. While it has occasional innervation from the obturator nerve, it commonly is innervated by the femoral nerve.
The hamstrings are a group of muscles on the posterior aspect of the thigh that flexes the leg composed of the semitendinosus, semimembranosus, and biceps femoris. They originate on the ischial tuberosity and insert around the knee on the tibia and fibula. They are innervated by the tibial branch of the sciatic nerve. Occasionally, the adductor magnus is considered a hamstring as it shares many of these characteristics.
There are 3 layers of the pelvic floor musculature. From caudal (superficial) to cephalad (deep), they are the urogenital triangle, the urogenital diaphragm, and the pelvic diaphragm.
The urogenital triangle consists of several muscles. The superficial transverse perineal muscle originates at the ischial tuberosity and extends to the central tendinous perineal body, which lies immediately ventral to the anus. It is involved primarily with the support of the pelvic floor. The ischiocavernosus muscle extends from the ischial tuberosity to the ischiopubic rami and is involved in supporting the erect male penis, the female vagina, as well as flexing the anus. The bulbocavernosus (bulbospongiosus in men) muscle is located in the midline of the pelvis and describes a dorsal to ventral path starting at the tendinous body and coursing to the ischiocavernosus and contributes to erections. In females, the fibers are divided and course laterally around the vaginal introitus. The final muscle in the urogenital triangle is the anal sphincter. It is attached to the dorsal central tendinous end of the perineal body and its fibers spread to the levator ani posteriorly. This muscle regulates defecation.
Deeper (more cephalad) into the pelvis is the urogenital diaphragm. It is a triangular ligament with a strong muscular component that stretches from the pubic symphysis to the ischial tuberosities. It occupies the ventral side of the pelvic outlet and is composed of several muscles. The urethral sphincter is an autonomic smooth muscle internal sphincter located at the urethro-vesicular junction. In males, the external sphincter is located just caudal to the prostate, and in females, it is located just caudal to the internal sphincter. The external sphincter is skeletal muscle and is under voluntary control. Both the internal and external sphincters are involved in regulating urination. The deep transverse perineal muscle extends from the inferior rami of the ischium and inserts into the tendinous median plane and aids in the support of the pelvis. The caudal and cephalad borders of this muscular-tendinous plane are embedded in a layer of fascia. The caudal layer of fascia is known as the perineal membrane.
The third, most cephalad (deep) layer is the pelvic diaphragm, a thin and muscular layer that extends from the pubic ramus to the coccyx and inserts laterally into the arcus tendinous fascia, a condensation of the membrane of the obturator internus muscle. It is a funnel-shaped sling and represents the inferior (caudal) border of the internal pelvic cavity. The diaphragm is composed of several muscles and endopelvic fascia, the largest of which is the levator ani muscle. This muscle is composed of 3 parts: the puborectalis muscle, pubococcygeus muscle, and the iliococcygeus muscle. The levator ani's ventral border is the posterior surface of the superior pubic rami. It courses bilaterally around the pelvis and inserts at the arcus tendinous fascia. Between the left and right levator pass the urethra, anal canal, and vagina in females.
Physiologic Variants
The most significant physiologic variants of the pelvis are relevant to child-bearing. There are 4 recognized variants of the pelvis as classified by the "Caldwell-Moloy" system. [8]
Gynecoid
This is the classic female pelvis found in roughly half of women. The inlet is ovoid to almost circular. The pubic arch and pelvic outlet are wide. The sacrum is deeply curved, and the ischial spines are relatively blunt. Overall, the internal dimensions of this pelvic type are the largest and most conducive to childbirth.
Android
This is the classical male pelvis, although it is present in approximately 20% of women. The inlet is heart-shaped, and the sidewalls are convergent. The sacral curve is shallow. Overall, internal dimensions are smaller than those of the gynecoid pelvis, and childbirth can be complicated due to this shape.
Anthropoid
Common in men and present in approximately 25% of women. It has an ovoid inlet and is greater in dimension from front to rear than side to side. The pubic angle is somewhat less than the gynecoid but greater than the android pelvis. This pelvis is generally considered suitable for childbirth.
Platypelloid
A very wide and shallow inlet is the hallmark of this pelvis. It is present in approximately 5% of women. This pelvis is commonly associated with a high transverse arrest of labor due to the inability of the fetal head to navigate the inlet secondary to insufficient space in the anterior to posterior dimension. Uncomplicated vaginal birth is very uncommon with this pelvis.
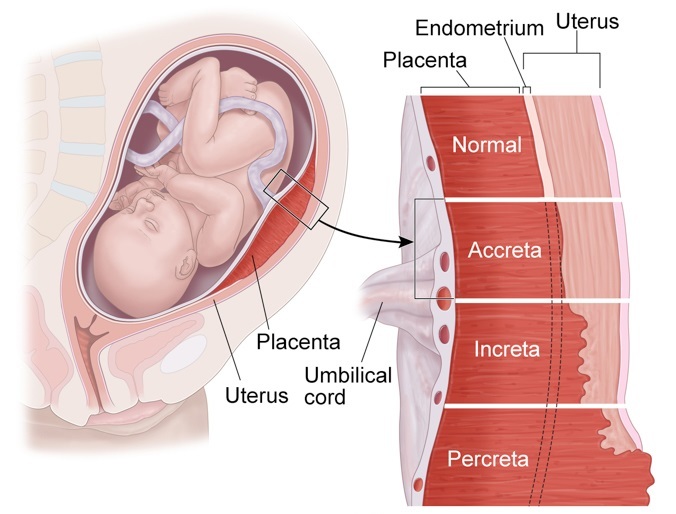
The body assists childbirth with any type of pelvis through the hormone relaxin, which is released by the placenta and causes the ligaments that bind the pubic bones to become more pliable. This allows the pelvis to enlarge by facilitating motion at the pubic symphysis. This increased laxity can be a source of pain in late pregnancy.
Surgical Considerations
Trauma to the pelvis has a high mortality rate, as bleeding both from associated vessels, such as the pre-sacral venous plexus, and the pelvis itself commonly leads to acute hemorrhagic shock. For this reason, the initial assessment in trauma bays often involves examining the integrity of the pelvis through compression and digital rectal exam, followed by an AP pelvic x-ray. “Open book” fractures occur when sufficient trauma breaks the pelvic ring in two or more locations.[9]
Acetabular fractures can involve the anterior column, posterior column, or both, and the specific classification of fracture is assessed with Judet views on x-ray. [10] The anterior column is also known as the iliopubic column, as it is comprised primarily of these bones along with the anterior wall of the acetabulum. The posterior column involves the ischium, sciatic notches, and posterior wall of the acetabulum. The posterior wall is most likely to be injured in high energy trauma due to force being transmitted up the femur in situations like motor vehicle accidents. Acetabular fractures can present with hip dislocation, especially posterior wall fractures with posterior dislocation following a “dashboard” injury when the flexed hip is struck at the knee against the dashboard of a vehicle in a collision. Posterior dislocations resulting from these injuries present with limb length discrepancy, adduction, internal rotation, and flexion. Conversely, anterior hip dislocations are much less common and present in extension and external rotation.
The ureters enter the pelvic brim over the bifurcation of the common iliac arteries into the internal and external branches. The course of the ureter may be identified by watching for the peristaltic motion and tracing it down to the lower pelvis, where it passes under the uterine artery in females. This relationship can be remembered by the mnemonic “water under the bridge,” where the ureter is water and the uterine artery is the bridge. This way, a surgeon may ensure that he or she is working safely away from it during pelvic surgery. Additionally, the ureters course approximately 2 cm from the cervix at the level of the uterine artery. One study showed that in 15% of women, that distance is less than 5 mm. This may explain the observed incidence of ureteral ligation during hysterectomy. [11]
Clinical Significance
Many pelvic landmarks are easily palpable on physical exam including the iliac crest, the anterior superior iliac spine (ASIS), and the posterior superior iliac spine (PSIS.) As such, these landmarks have become instrumental in physical examinations by allowing practitioners to quickly and simply identify internal anatomy based on its relation to superficial anatomy for both diagnostic and therapeutic measures.
The iliac crest is the most superior part of the pelvis located near what is commonly referred to as the waist. This level corresponds to around L3-L4 lumbar vertebrae and can be used to safely place a lumbar puncture needle by minimizing the potential for spinal cord damage while still accessing cerebrospinal fluid, as the cord itself ends around the L1 vertebral level.
The ASIS is the most anterior portion of the iliac crest and is the attachment point for the sartorius muscle as well as the inguinal ligament which connects to the pubic tubercle. This point finds its use in the evaluation of appendicitis, as McBurney’s point of the appendix is defined as one-third the distance from the ASIS to the umbilicus. The ASIS also becomes helpful in identifying leg length discrepancies, as pelvic rotation often accommodates these differences while standing and walking. Therefore, leg length is measured from the ASIS to the medial malleolus.[12]
The PSIS marks the posterior edge of the iliac crest and manifests in some individuals as dimples on the lower back, colloquially called “dimples of Venus. ” This landmark is useful for identifying the sacroiliac joint, and tenderness over this joint can be a symptom of sacroiliitis, a condition present in some inflammatory spondyloarthropathies.
In developmental dysplasia of the hip, the acetabulum is not properly formed to hold the head of the femur. This condition is associated with breech presentation in labor. To assess for this disorder there are two physical exam maneuvers: Ortolani and Barlow. With the Barlow maneuver pressure is applied posteriorly with an adducted and flexed hip to assess for dislocation, while the Ortolani maneuver involves relocation with hip abduction and anterior force.[13]
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
Figure
Pelvis, Female, Pubic Arch, Brim of lesser Pelvis,. Contributed by Gray's Anatomy
References
- 1.
Wei JT, De Lancey JO. Functional anatomy of the pelvic floor and lower urinary tract.
Clin Obstet Gynecol. 2004 Mar;47(1):3-17. [PubMed: 15024268]
- 2.
Hopayian K, Song F, Riera R, Sambandan S. The clinical features of the piriformis syndrome: a systematic review. Eur Spine J. 2010 Dec;19(12):2095-109. [PMC free article: PMC2997212] [PubMed: 20596735]
- 3.
Verbruggen SW, Nowlan NC. Ontogeny of the Human Pelvis. Anat Rec (Hoboken). 2017 Apr;300(4):643-652. [PubMed: 28297183]
- 4.
Percy JP, Neill ME, Swash M, Parks AG. Electrophysiological study of motor nerve supply of pelvic floor. Lancet. 1981 Jan 03;1(8210):16-7. [PubMed: 6109050]
- 5.
DeLancey JO. What's new in the functional anatomy of pelvic organ prolapse? Curr Opin Obstet Gynecol. 2016 Oct;28(5):420-9. [PMC free article: PMC5347042] [PubMed: 27517338]
- 6.
Lawson JO. Pelvic anatomy. I. Pelvic floor muscles. Ann R Coll Surg Engl. 1974 May;54(5):244-52. [PMC free article: PMC2388375] [PubMed: 4829749]
- 7.
Baker RL, Fredericson M. Iliotibial Band Syndrome in Runners: Biomechanical Implications and Exercise Interventions. Phys Med Rehabil Clin N Am. 2016 Feb;27(1):53-77. [PubMed: 26616177]
- 8.
SWENSON PC. Anatomical variations in the female pelvis; the Caldwell-Moloy classification. Radiology. 1947 May;48(5):527. [PubMed: 20240130]
- 9.
Coccolini F, Stahel PF, Montori G, Biffl W, Horer TM, Catena F, Kluger Y, Moore EE, Peitzman AB, Ivatury R, Coimbra R, Fraga GP, Pereira B, Rizoli S, Kirkpatrick A, Leppaniemi A, Manfredi R, Magnone S, Chiara O, Solaini L, Ceresoli M, Allievi N, Arvieux C, Velmahos G, Balogh Z, Naidoo N, Weber D, Abu-Zidan F, Sartelli M, Ansaloni L. Pelvic trauma: WSES classification and guidelines. World J Emerg Surg. 2017;12:5. [PMC free article: PMC5241998] [PubMed: 28115984]
- 10.
Mauffrey C, Stacey S, York PJ, Ziran BH, Archdeacon MT. Radiographic Evaluation of Acetabular Fractures: Review and Update on Methodology.
J Am Acad Orthop Surg. 2018 Feb 01;26(3):83-93. [PubMed: 29266045]
- 11.
Hurd WW, Chee SS, Gallagher KL, Ohl DA, Hurteau JA. Location of the ureters in relation to the uterine cervix by computed tomography. Am J Obstet Gynecol. 2001 Feb;184(3):336-9. [PubMed: 11228483]
- 12.
Hubbard EW, Liu RW, Iobst CA. Understanding Skeletal Growth and Predicting Limb-Length Inequality in Pediatric Patients. J Am Acad Orthop Surg. 2019 May 01;27(9):312-319. [PubMed: 31026239]
- 13.
Yang S, Zusman N, Lieberman E, Goldstein RY. Developmental Dysplasia of the Hip. Pediatrics. 2019 Jan;143(1) [PubMed: 30587534]
The Pelvic Girdle - Structure - Function - Assessment
The pelvic girdle is a ring-like bony structure, located in the lower part of the trunk. It connects the axial skeleton to the lower limbs.
In this article, we shall look at the anatomy of the pelvic girdle – its bony landmarks, functions, and its clinical relevance.
The bony pelvis consists of the two hip bones (also known as innominate or pelvic bones), the sacrum and the coccyx.
There are four articulations within the pelvis:
- Sacroiliac joints (x2) – between the ilium of the hip bones, and the sacrum
- Sacrococcygeal symphysis – between the sacrum and the coccyx.
- Pubic symphysis – between the pubis bodies of the two hip bones.
Ligaments attach the lateral border of the sacrum to various bony landmarks on the bony pelvis to aid stability.
By TeachMeSeries Ltd (2023)
Fig 1 – The pelvic girdle is formed by the hip bones, sacrum and coccyx.
Functions of the PelvisThe strong and rigid pelvis is adapted to serve a number of roles in the human body. The main functions being:
- Transfer of weight from the upper axial skeleton to the lower appendicular components of the skeleton, especially during movement.
- Provides attachment for a number of muscles and ligaments used in locomotion.
- Contains and protects the abdominopelvic and pelvic viscera.
The osteology of the pelvic girdle allows the pelvic region to be divided into two:
- Greater pelvis (false pelvis) – located superiorly, it provides support of the lower abdominal viscera (such as the ileum and sigmoid colon). It has little obstetric relevance.
- Lesser pelvis (true pelvis) – located inferiorly. Within the lesser pelvis reside the pelvic cavity and pelvic viscera.
The junction between the greater and lesser pelvis is known as the pelvic inlet. The outer bony edges of the pelvic inlet are called the pelvic brim.
By TeachMeSeries Ltd (2023)
Fig 2 – The greater and lesser pelvis. The lesser pelvis is the ‘true’ pelvis and contains the pelvic cavity.
The pelvic inlet marks the boundary between the greater pelvis and lesser pelvis. Its size is defined by its edge, the pelvic brim.
The borders of the pelvic inlet:
- Posterior – sacral promontory (the superior portion of the sacrum) and sacral wings (ala).
- Lateral – arcuate line on the inner surface of the ilium, and the pectineal line on the superior pubic ramus.
- Anterior – pubic symphysis.
The pelvic inlet determines the size and shape of the birth canal, with the prominent ridges a key site for attachment of muscle and ligaments.
Some alternative descriptive terminology can be used in describing the pelvic inlet:
- Linea terminalis – the combined pectineal line, arcuate line and sacral promontory.
- Iliopectineal line – the combined arcuate and pectineal lines. This represents the lateral border of the pelvic inlet.
By TeachMeSeries Ltd (2023)
Fig 3 – Looking down onto the pelvis, the borders of the pelvic brim.
Pelvic OutletThe pelvic outlet is located at the end of the lesser pelvis, and the beginning of the pelvic wall.
Its borders are:
- Posterior: The tip of the coccyx
- Lateral: The ischial tuberosities and the inferior margin of the sacrotuberous ligament
- Anterior: The pubic arch (the inferior border of the ischiopubic rami).
The angle beneath the pubic arch is known as the sub-pubic angle and is of a greater size in women.
By TeachMeSeries Ltd (2023)
Fig 4 – The borders of the pelvic outlet.
Adaptation for ChildbirthThe majority of women have a gynaecoid pelvis, as opposed to the male android pelvis. The slight differences in their structures creates a greater pelvic outlet, adapted to aid the process of childbirth. When comparing the two, the gynaecoid pelvis has:
- A wider and broader structure yet it is lighter in weight
- An oval-shaped inlet compared with the heart-shaped android pelvis.
- Less prominent ischial spines, allowing for a greater bispinous diameter
- A greater angled sub-pubic arch, more than 80-90 degrees.
- A sacrum which is shorter, more curved and with a less pronounced sacral promontory.
In addition to the bony adaptations, the sacrotuberous and sacrospinous ligaments can stretch under the influence of progesterone and increase the size of the outlet further.
By TeachMeSeries Ltd (2023)
Fig 5 – Gynaecoid pelvis vs the android pelvis.
Clinical Relevance: Assessment of the Female Bony Pelvis
The lesser pelvis is the bony canal through which the fetus has to pass during childbirth. It is therefore of great importance to determine the diameter of this canal and therefore the childbearing capacity of the mother.
The diameter can be determined by a pelvic examination or radiographically. There are two measurements that are of importance:
Obstetric ConjugateIn order to determine the narrowest fixed distance that the fetus would have to negotiate, the minimum antero-posterior diameter of the pelvic inlet is measured.
This distance is between the sacral promontory and the midpoint of the pubic symphysis (where the pubic bone is thickest) and is known as the obstetric conjugate (or true conjugate). However, this measurement cannot be assessed clinically, due to the presence of the bladder.
Diagonal Conjugate
The diagonal conjugate is the alternative, measuring from the inferior border of the pubic symphysis to the sacral promontory and can be measured manually via the vagina.
(To do this you use the tip of your middle finger to measure the sacral promontory and then using the other hand to mark the level of the inferior margin of the pubic symphysis on the examining hand. You then use the distance between the index finger and the pubic symphysis to measure the diagonal conjugate, ideally 11cm or greater)
In addition to measuring the diagonal conjugate, a mid-pelvis check is carried out. Here, the clinician is testing for straight side walls and measuring the bispinous diameter which is narrowest part of the pelvic canal. The width of the subpubic angle at the pelvic outlet can be determined by the distance between the ischial tuberosities.
By TeachMeSeries Ltd (2023)
Fig 6 – Assessment of the female pelvis, via the diagonal conjugate
printPrint this Article
Encyclopedia - Pelvic Girdle
The pelvic girdle bears the weight of the entire upper body, and the lower limbs rest against it. This part of the body experiences a lot of pressure from both sides - from below and from above, it promotes the movements of the lower limbs and protects important internal organs. The most important function of the pelvis is locomotor, contributing to the movement of the body in space.
Differences between the human pelvis and the pelvis of other mammals are related
with an upright body position. Only in humans transverse dimensions
the pelvis is more straight (anterior-posterior). Even the pelvis of the great apes
already more elongated. In the human fetus, the pelvis has the same shape,
as the pelvis of four-legged mammals. Pelvis transformations begin
under the influence of mechanical loads: gravity of the body, pressure in the hip
joint during movements, etc. Active formation of sex differences
in the structure of the pelvis occurs during puberty under the action of
hormones. Characteristically, with reduced ovarian function (female
gonads) slows down the formation of female
features - the pelvis remains relatively narrow.
Pelvic bones
The pelvic girdle, or pelvis, is a strong bone ring that is located in the lower part of the skeleton of the human torso. It is formed from almost immovably connected bones: unpaired - the sacrum and two massive, flat - right and left pelvic bones. A sacrum is wedged between the pelvic bones, to which is attached a small bone - the coccyx - a rudimentary remnant of the caudal skeleton.
In children under 16, each pelvic bone consists of 3 separate bones: the ilium, ischium and pubis, interconnected by layers of cartilage. After 16 years they grow together. In this place there is a deep fossa - the acetabulum. It includes the head of the femur, forming the hip joint.
Structure of the ischium
The ischial bone has a powerful ischial tuberosity on which the human body rests when sitting. If a person is standing, the ischial tuberosity is hidden by a thick layer of gluteal muscles and fatty tissue.
Structure of the pubic bone
The pubic bone has 2 branches connected to each other at an angle. These branches, together with the branch of the ischium, limit a large obturator opening on the pelvic bone, covered with a dense membrane. The pubic bones on the right and left are interconnected by means of cartilage - thus, a pubic symphysis (half-joint), one of the joints of the pelvic girdle, is formed. The elevation of the skin above the site of the symphysis is called the pubis.
The value of the pubic symphysis is especially great for the female body. By the time of childbirth, the cartilaginous layer between the pubic bones softens, and the gap inside it allows the bones to move apart and thereby somewhat expand the birth canal.
Structure of the ilium
The ilium consists of a body and a thin wing, which expands upward and ends in a long crest. The crest serves as an attachment site for the broad abdominal muscles. The deepening of the inner surface of the wing forms the iliac fossa. It is in this hole on the right that the caecum with the appendix (appendix) is located.
Behind the ilium there is an articular surface, shaped like an auricle. It connects tightly with exactly the same surface on the sacrum, forming a flat sacroiliac joint. This joint is strengthened on all sides by bundles of ligaments, which, by their strength, are considered the most powerful in the human body.
Pelvic angle
The pelvic bones are the attachment point for the muscles of the abdomen, back and lower extremities. In the vertical position of a person, the pelvis is tilted forward at an angle of 45-60 degrees relative to the horizontal plane. The value of the angle depends on the posture, in women it is greater than in men.
Large and small pelvis
There are large and small pelvis. The boundary line separating them runs along the inner surface of the pelvic bones from the protrusion on the spine - the cape (the junction of the last lumbar vertebra with the sacrum) to the upper edge of the pubic symphysis.
Large basin
The large pelvis is the upper part of the pelvis, formed by the deployed wings of the ilium. It is the lower wall of the abdominal cavity and serves as a support for the internal organs.
Pelvis
The small pelvis is located below the large one and is bounded behind by the sacrum and coccyx, in front and from the sides - by the ischial and pubic bones. It distinguishes between the entrance, exit and cavity. The pelvic cavity contains the bladder, rectum and internal genital organs (ovaries, fallopian tubes, uterus and vagina, prostate, seminal vesicles and vas deferens). The entrance to the small pelvis is open to the abdominal cavity and corresponds to the boundary line with the large pelvis. The exit from the pelvic cavity is closed by the muscles that form the pelvic diaphragm, the urethra and rectum pass through it in men, the urethra, rectum and vagina in women. Outside, this area of the body stands out as the perineum.
The pelvic organs differ from the abdominal organs in that they can
significantly change its volume: periodically filled
and the bladder and rectum are emptied, enlarged
and the uterus moves during pregnancy. It affects
on the work of other organs and blood supply.
Pelvis female and male
In no part of the skeleton are sex differences as pronounced as in the pelvis. Sex differences in the pelvis begin to appear in children between the ages of 8 and 10 years. The average size of the male pelvis is about 2 cm smaller than the average size of the female pelvis. The female pelvis is wider and shorter than the male, the wings of the ilium are deployed more strongly. The angle between the lower branches of the pubic bones is rounded in the form of a pubic arch, the cape almost does not protrude into the pelvic cavity, and due to the wide, short and flat sacrum, the pelvic cavity has the shape of a cylinder.
Male pelvic structure
In men, the pelvis is already higher: the wings of the ilium are located almost vertically, the sacrum is strongly concave, and the promontory clearly protrudes into the cavity of the small pelvis, the subpubic angle is sharp. As a result, both the entrance and exit from the male pelvis are greatly narrowed, and its cavity itself has a conical shape.
The structure of the pelvis in women
The fetus moves through the small pelvis in women during childbirth, so its shape and size are of great importance for a normal birth act. The dimensions of the small pelvis are determined by indirect measurements of the large pelvis with obstetric compasses. The internal dimensions are determined during a vaginal examination and with the help of ultrasound.
For example, the distance between protruding tubercles on the iliac crest (the so-called superior anterior iliac spines) in women is normally 25–27 cm, and the distance between the most distant points of the crest on the right and left is 28–30 cm. The size of the entrance and exit from the small pelvis, which, both in direct and transverse dimensions, are about 11–13 cm in women. 1.5–2 cm due to the deviation of the tip of the coccyx posteriorly.
With violations in the development of the girl, due to rickets, spondylitis, coxitis and other diseases and poor nutrition, neglect of physical education or too much physical activity, deviations in the normal development of the pelvis are possible - a narrow pelvis. With a small degree of narrowing, childbirth is possible, but they are long and difficult. With a greater narrowing, there are obstacles to the passage of the fetus through the birth canal.
Author: Olga Gurova, Candidate of Biological Sciences, Senior Researcher, Associate Professor, Department of Human Anatomy, Peoples' Friendship University of Russia
The material uses photographs owned by shutterstock.com
Lower limb belt | it's... What is the Lower Limb Belt?
InterpretationTranslation
- Lower limb belt
-
In the skeleton of the pelvic girdle, the right and left pelvic bones are joined together (through pubic fusion) and each of the pelvic bones and the sacrum to form the sacroiliac joint.
The bone pelvis formed as a result of these connections ensures the distribution and transfer of body weight to the bones of the lower limb and protection of the pelvic organs.
The pelvic bone is generally irregular in shape; on its outer surface there is an acetabulum (acetabulum) (Fig. 40, 43) - a spherical depression that serves to connect with the pelvic bone of the femoral head and is limited by the lunate articular surface (fasies lunata) (Fig. 40). In the formation of the acetabulum, both the pubic and iliac, and the ischium are involved. Their relative position relative to the acetabulum helps to highlight these bones on the body of the pelvic bone.
In the structure of the pubic bone (Fig. 39), located in front-below of the acetabulum, the body (corpus ossis pubis) (Fig. 41), the upper branch (r. superior ossis pubis) (Fig. 40, 41) and the lower branch (r. inferior ossis pubis) (Fig.
40, 41) of the pubic bone. The body of the pubic bone is involved in the formation of the acetabulum. On the upper edge of the superior branch of the pubic bone are the pubic crest (crista pubica) (Fig. 40, 41) and the pubic tubercle (tuberculum pubicum) (Fig. 40, 42), on the lower edge - the obturator ridge (crista obturatoria) (Fig. 41), in the posterior part of which there is an anterior obturator tubercle (tuberculum obturatorium anterius) (Fig. 41). On the inner side of each of the pubic bones, at the point of transition of its upper branch to the lower one, there is a rough (symphysial) surface (facies symphysialis) (Fig. 41) of an oval shape. The latter serves to connect with another pubic bone with the formation of pubic fusion (simphisis ossium pubis) .
The ilium is located above and behind the acetabulum, in the formation of which it also participates. In the structure of the ilium, a short and massive body of the ilium (corpus ossis ilii) (Fig.
40, 41) and a wing (ala ossis ilii) (Fig. 40, 41) are distinguished, under which an arcuate line passes on the inner surface (linea arcuata) (Fig. 41). Upper edge of wing - iliac crest (crista iliaca) (Fig. 41, 42) - has two protrusions on its anterior and posterior margins. These protrusions are called, respectively, the upper anterior (spina iliaca anterior superior) (Fig. 40, 41, 42) and the lower anterior (spina iliaca anterior inferior) (Fig. 40, 41, 42) iliac spines and the upper posterior ( spina iliaca posterior superior) (Fig. 40, 41) and lower posterior iliac spines (spina iliaca posterior inferior) (Fig. 40, 41). The inner surface of the wing forms an extensive iliac fossa (fossa iliaca) (Fig. 41, 42) with a smooth, gently sloping surface. The gluteal surface of the wing has an anterior (linea glutea anterior) (Fig. 40), a posterior (linea glutea posterior) (Fig. 40) and a lower (linea glutea inferior) (Fig.
40) gluteal lines serving as places muscle attachments. On the sacro-pelvic surface of the wing there is an ear-shaped surface (facies auricularis) (Fig. 41), through which the ilium articulates with the iliac tuberosity (tuberositas iliaca) (Fig. 41) and sacrum. With the sacrum, the ilium forms a semi-joint (articulatio sacroiliaca) .
The ischium is located posterior to the acetabulum. In the structure of the ischium, there is also a body (corpus ossis ischii) (Fig. 40, 41), which is involved in the formation of the acetabulum, and a branch (r. ossis ischii) (Fig. 40, 41). At the junction of the body and the branch of the ischium, there is a massive thickening - the ischial tuberosity (tuber ischiadicum) (Fig. 40), above which is the ischial spine (spina ischiadica) (Fig. 41, 42). On both sides of the ischial spine there are large (incisura ischadica major) (Fig. 40, 41) and small (incisura ischadica minor) (Fig.
40) ischial notches. The bodies and branches of the ischial and pubic bones, closing, form the boundaries of the obturator foramen (foramen obturatum) (Fig. 40, 41, 43).
Coccyx, sacrum and pelvic bones connected to each other make up bone pelvis (pelvis) . It contains the organs of the digestive and genitourinary systems, large vessels and nerves. This bone skeleton of the pelvis is divided into upper and lower sections - the large and small pelvis.
Large pelvis (pelvis major) (Fig. 43) has an open front wall, from the sides it is limited by the wings of the ilium, and from behind - by the base of the sacrum and lower lumbar vertebrae. The border line 9 runs along the crest of the pubic bone and the arcuate line of the ilium.0027 (linea terminalis) (Fig. 43), which is the lower border of the large pelvis. Below the boundary line is the small pelvis (pelvis minor) (Fig. 43), which is a cylindrical cavity.
The lateral walls of the small pelvis are formed by the lower part of the bodies of the iliac bones, ischial bones, the anterior walls - by the pubic bones, and the posterior - by the sacral and coccygeal. Connecting at an angle, the pubic bones form a subpubic angle in men (angulus subpubicus) (Fig. 43), and in women, the pubic arch (arcus pubis) (Fig. 43). The middle of the straight diameters of the entrance and exit of the small pelvis are connected by the axis of the pelvis (axis pelvis) .
In the place where the large pelvis passes into the small one, the upper opening of the pelvis is formed (apertura pelvis superior) . The lower opening of the pelvis (apertura pelvis inferior) from the sides ischium tubercles, in front - the pubic fusion and the lower branches of the pubic bones, and behind - the coccygeal bone.
In the structure of the bone base of the pelvis, sexual dimorphism is especially noticeable. This is explained by the fact that in women, the device and method of connecting the pelvic bones are designed, in addition to purely mechanical tasks, to ensure the successful passage of childbirth.
In particular, during pregnancy, the internal cavity of the small pelvis can increase due to loosening of the cartilaginous interpubic disc and, accordingly, expansion of the symphysis.
The female pelvis is wider and lower, with wings of the iliac bones deployed to the sides. The lower branches of the pubic bones converge in a wide arc, and the small pelvis has the shape of a wide cylinder. The upper aperture of the small pelvis is close to oval in shape, the symphysis is wider and lower located than in the male pelvis.
The male pelvis is taller and narrower than the female pelvis, with less developed iliac wings. The lower branches of the pubic bones converge at an acute angle, the cavity of the small pelvis noticeably narrows from below, the opposite ischial tubercles and spines are located closer to each other. The upper and lower apertures of the male small pelvis differ significantly in size and shape from the corresponding apertures of the female one due to the more prominent promontory of the sacral bone, as well as due to the coccyx, which protrudes more sharply into the lumen of the exit from the small pelvis.
Fig. 39. Pelvic bone and skeleton of the free part of the lower limb:
1 - sacrum; 2 - pelvic bone; 3 - tibia; 4 - patella;
5 - fibula; 6 - tibia; 7 - foot bones
Fig. 40. Pelvic bone (outside view):
1 — wing of the ilium; 2 - anterior gluteal line; 3 - back gluteal line; 4 - superior anterior iliac spine;
5 - superior posterior iliac spine; 6 - lower posterior iliac spine; 7 - large sciatic notch;
8 - lower gluteal tenderloin; 9 - lower anterior iliac spine; 10 - the body of the ilium;
11 - lunar surface; 12 - acetabulum; 13 - small sciatic notch;
14 - body of the ischium; 15 - the upper branch of the pubic bone; 16 - pubic tubercle;
17 - obturator foramen; 18 - the lower branch of the pubic bone; 19 - ischial tubercle;
20 ischial ramus
Fig. 41. Pelvic bone (inside view):
1 - iliac crest; 2 - iliac fossa; 3 - iliac tuberosity; 4 - wing of the ilium;
5 - superior posterior iliac spine; 6 - upper anterior iliac spine; 7 - ear-shaped surface;
8 - lower posterior iliac spine; 9 - lower anterior iliac spine; 10 - arcuate line;
11 - large sciatic notch; 12 - the body of the ilium; 13 - the body of the ischium;
14 - body of the pubic bone; 15 - ischial spine; 16 - pubic crest; 17 - obturator crest;
18 - anterior obturator tubercle; 19 - the upper branch of the pubic bone; 20 - branch of the ischium;
21 - rough surface; 22 - obturator opening; 23 - lower branch of the pubic bone
Fig.
A - male; B - female:
1 - iliac fossa; 2 - the base of the sacrum; 3 - iliac crest; 4 - superior anterior iliac spine;
5 - ischial spine; 6 - lower anterior iliac spine; 7 - coccyx; 8 - pubic crest; 9 - pubic tubercle
Fig. 43. Pelvis (front view):
A - male; B - female:
1 - large pelvis; 2 - sacrum; 3 - border line; 4 - small pelvis;
5 - acetabulum; 6 - obturator opening; 7 - subpubic angle; 8 - pubic arch
* * *
See also: Skeleton of the lower limbJoints of the bones of the girdle of the lower limb
Skeleton of the free part of the lower limb
Joints of the free part of the lower limb formation of the sacroiliac joint. The bone pelvis formed as a result of these connections ensures the distribution and transfer of body weight to the bones of the lower limb and protection of the pelvic organs.
The pelvic bone is generally irregular in shape; on its outer surface there is an acetabulum (acetabulum) (Fig. 40, 43) - a spherical depression that serves to connect with the pelvic bone of the femoral head and is limited by the lunate articular surface (fasies lunata) (Fig. 40). In the formation of the acetabulum, both the pubic and iliac, and the ischium are involved. Their relative position relative to the acetabulum helps to highlight these bones on the body of the pelvic bone.
In the structure of the pubic bone (Fig. 39), located in front-below of the acetabulum, the body (corpus ossis pubis) (Fig. 41), the superior branch (r. superior ossis pubis) (Fig. 40, 41) and the lower branch (r. inferior ossis pubis) (Fig. 40, 41) of the pubic bone. The body of the pubic bone is involved in the formation of the acetabulum. On the upper edge of the upper branch of the pubic bone there is a pubic crest (crista pubica) (Fig. 40, 41) and a pubic tubercle (tuberculum pubicum) (Fig. 40, 42), on the lower edge - the obturator crest (crista obturatoria) (Fig. 41 ), in the posterior part of which there is an anterior obturator tubercle (tuberculum obturatorium anterius) (Fig. 41). On the inner side of each of the pubic bones, at the point of transition of its upper branch to the lower one, there is a rough (symphysial) surface (facies symphysialis) (Fig. 41) of an oval shape. The latter serves to connect with another pubic bone to form a pubic fusion (simphisis ossium pubis).
The ilium is located above and behind the acetabulum, in the formation of which it also participates. In the structure of the ilium, a short and massive body of the ilium (corpus ossis ilii) (Fig. 40, 41) and a wing (ala ossis ilii) (Fig. 40, 41) are distinguished, under which an arcuate line passes on the inner surface (linea arcuata) (Fig. 41). The upper edge of the wing - the iliac crest (crista iliaca) (Fig. 41, 42) - has two protrusions on its anterior and posterior margins. These protrusions are called, respectively, the upper anterior (spina iliaca anterior superior) (Fig. 40, 41, 42) and the lower anterior (spina iliaca anterior inferior) (Fig. 40, 41, 42) iliac spines and the upper posterior (spina iliaca posterior superior) (Fig. 40, 41) and the lower posterior iliac spine (spina iliaca posterior inferior) (Fig. 40, 41). The inner surface of the wing forms an extensive iliac fossa (fossa iliaca) (Fig. 41, 42) with a smooth, gently sloping surface. The gluteal surface of the wing has an anterior (linea glutea anterior) (Fig. 40), a posterior (linea glutea posterior) (Fig. 40) and a lower (linea glutea inferior) (Fig. 40) gluteal lines that serve as attachment points for muscles. On the sacro-pelvic surface of the wing there is an ear-shaped surface (facies auricularis) (Fig. 41), through which the ilium articulates with the iliac tuberosity (tuberositas iliaca) (Fig. 41) and the sacrum. With the sacrum, the ilium forms a semi-joint (articulatio sacroiliaca).
| external view 1 — wing of the ilium; 2 - anterior gluteal line; 3 - posterior gluteal line; 4 - superior anterior iliac spine; 5 - superior posterior iliac spine; 6 - lower posterior iliac spine; 7 - large sciatic notch; 8 - lower gluteal notch; 9 - lower anterior iliac spine; 10 - body of the ilium; 11 - lunar surface; 12 - acetabulum; 13 - small ischial notch; 14 - body of the ischium; 15 - superior branch of the pubic bone; 16 - pubic tubercle; 17 - obturator foramen; 18 - lower branch of the pubic bone; 19 - ischial tuberosity; 20 ischial ramus |
|
| inside view 1 — iliac crest; 2 - iliac fossa; 3 - iliac tuberosity; 4 - wing of the ilium; 5 - superior posterior iliac spine; 6 - superior anterior iliac spine; 7 - ear-shaped surface; 8 - lower posterior iliac spine; 9 - lower anterior iliac spine; 10 - arcuate line; 11 - large sciatic notch; 12 - body of the ilium; 13 - body of the ischium; 14 - body of the pubic bone; 15 - ischial spine; 16 - pubic ridge; 17 - obturator ridge; 18 - anterior obturator tubercle; 19 - superior branch of the pubic bone; 20 - branch of the ischium; 21 - rough surface; 22 - obturator foramen; 23 - inferior ramus of pubis |
|
The ischium is located from below-behind relative to the acetabulum. In the structure of the ischium, a body (corpus ossis ischii) (Fig. 40, 41), which is involved in the formation of the acetabulum, and a branch (r. ossis ischii) (Fig. 40, 41) are also distinguished. At the junction of the body and the branch of the ischial bone, there is a massive thickening - the ischial tubercle (tuber ischiadicum) (Fig. 40), above which is the ischial spine (spina ischiadica) (Fig. 41, 42). On both sides of the ischial spine are large (incisura ischadica major) (Fig. 40, 41) and small (incisura ischadica minor) (Fig. 40) ischial notches. The bodies and branches of the ischial and pubic bones, closing, form the boundaries of the obturator foramen (foramen obturatum) (Fig. 40, 41, 43).
The coccyx, sacrum and pelvic bones connected to each other constitute the actual bone pelvis (pelvis). It contains the organs of the digestive and genitourinary systems, large vessels and nerves. This bone skeleton of the pelvis is divided into upper and lower sections - the large and small pelvis.
| Fig. 42. Entrance to the cavity of the small pelvis A - male; B - female: 1 - iliac fossa; 2 - the base of the sacrum; 3 - iliac crest; 4 - superior anterior iliac spine; 5 - ischial spine; 6 - lower anterior iliac spine; 7 - coccyx; 8 - pubic ridge; 9 - pubic tubercle | |
| front view A - male; B - female: 1 - large pelvis; 2 - sacrum; 3 - frontier line; 4 - small pelvis; 5 - acetabulum; 6 - obturator opening; 7 - subpubic angle; 8 - pubic arch | |
The large pelvis (pelvis major) (Fig. 43) has an open front wall, from the sides it is limited by the wings of the ilium, and from behind by the base of the sacrum and the lower lumbar vertebrae. The border line (linea terminalis) (Fig. 43), which is the lower border of the large pelvis, passes along the crest of the pubic bone and the arcuate line of the ilium. Below the boundary line is the small pelvis (pelvis minor) (Fig. 43), which is a cylindrical cavity. The lateral walls of the small pelvis are formed by the lower part of the bodies of the iliac bones, ischial bones, the anterior walls - by the pubic bones, and the posterior - by the sacral and coccygeal. Connecting at an angle, the pubic bones form a subpubic angle (angulus subpubicus) in men (Fig. 43), and in women a pubic arch (arcus pubis) (Fig. 43). The middle of the straight diameters of the entrance and exit of the small pelvis are connected by the axis of the pelvis (axis pelvis).
In the place where the large pelvis passes into the small one, the upper opening of the pelvis (apertura pelvis superior) is formed. The lower opening of the pelvis (apertura pelvis inferior) from the sides ischium tubercles, in front - the pubic fusion and the lower branches of the pubic bones, and behind - the coccygeal bone.
In the structure of the bone base of the pelvis, sexual dimorphism is especially noticeable. This is explained by the fact that in women, the device and method of connecting the pelvic bones are designed, in addition to purely mechanical tasks, to ensure the successful passage of childbirth. In particular, during pregnancy, the internal cavity of the small pelvis can increase due to loosening of the cartilaginous interpubic disc and, accordingly, expansion of the symphysis.
The female pelvis is wider and lower, with wings of the iliac bones deployed to the sides. The lower branches of the pubic bones converge in a wide arc, and the small pelvis has the shape of a wide cylinder. The upper aperture of the small pelvis is close to oval in shape, the symphysis is wider and lower located than in the male pelvis.