Weak legs pregnancy
Aching, Painful, Or Heavy Legs During Pregnancy
Having aching legs during pregnancy is the icing on the cake of all of your physical ailments. But contrary to cake, heavy or aching legs are not something to be desired. While things like morning sickness and fatigue can be expected, when leg pain hits, it might catch you off guard.
To help make your leg troubles a little more bearable, we’ll give you some basic information and help you identify the signs, causes, and treatments for your aching and heavy legs.
Blood Circulation And Heavy Or Aching Legs During Pregnancy
Pregnancy is a period during which the risk of circulatory disruptions becomes particularly high. These disruptions are the consequence of the related increase in body weight and hormonal changes, as seen below:
- As early as the first trimester, the increase in hormones creates circumstances in which the blood in the veins can easily stagnate, weakening vein walls and the firmness of blood vessels.
Estrogen levels can lead to inflammation (edema), and progesterone modifies the vein walls and vessel dilation.
- Throughout pregnancy, the increased volume of the uterus leads to increased pressure on the main vein responsible for returning blood to the heart.
- Finally, an increase in blood weight and volume (of 20% to 30%) contributes to increased pressure on the leg veins, which is doubled or tripled. The valves are separated further from each other by distension of the veins and no longer play their role of impeding blood return.
Blood circulation in the leg veins can be considerably disrupted. The symptoms vary significantly from woman to woman and pregnancy to pregnancy, ranging from simple discomfort to disabling pain.
After delivery, these impairments most often go away on their own within a few weeks.
The Role Of Veins And Vascular Insufficiency
In their normal state, arteries supply the body’s tissues and organs with essential substances for their healthy functioning, such as oxygen.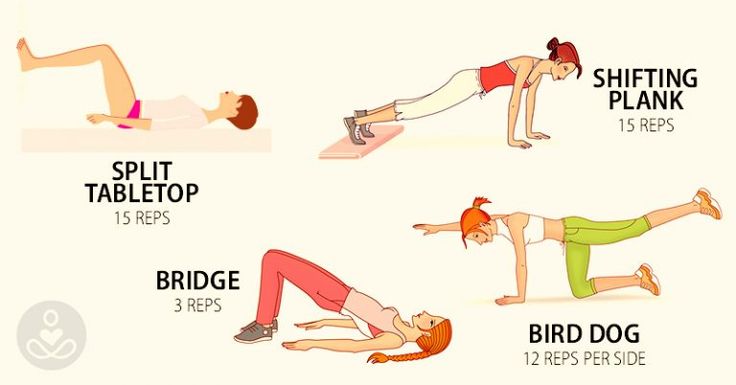 Veins, on the other hand, return blood to the heart.
Veins, on the other hand, return blood to the heart.
Blood pressure and the firmness of vein walls allow blood to flow from the lower to the upper portion of the legs. This blood flow through the veins and back up to the heart is called venous return.
Valves, acting as small flaps, are positioned every 2 to 5 centimeters (0.8 to 2 inches) in the veins. These valves ensure that blood always flows in the same direction without ever “falling” back down the other way.
The calf muscles and compression of the instep also play a role in blood flow, particularly when walking.
Contributing Factors
Several factors can increase the risk of vascular insufficiency during pregnancy:
- Heredity: If your mom has had circulatory issues, you run a higher risk of experiencing them yourself.
- Working in a standing position and shuffling. Prolonged sitting can also disrupt venous return.
- A sedentary lifestyle and lack of physical exercise.
- Excess body weight prior to pregnancy, or significant weight gain during pregnancy.

- Previous pregnancies: The risk of venous insufficiency increases with the number of previous pregnancies carried to term — 23 percent for the first pregnancy and 31 percent for the fourth.
Healthy Habits
To avoid circulatory impairments during pregnancy, prevention is essential. If you need to, try to lose weight before getting pregnant and then limit your weight gain during pregnancy.
Here are some other healthy habits to help you avoid vascular insufficiency:
- Take walks or do light exercise, which boosts blood flow
- Wear shoes with a small heel that is neither too high nor too flat (3 to 4 cm or 1 to 1.5 inches)
- Avoid tight-fitting clothes and constricting socks
- If you suffer from any plantar arch problems, wear corrective insoles
- In certain cases, wearing compression stockings and taking venotonics may be recommended during pregnancy, starting in the second month
If you experience the sensation of heavy legs despite these measures, try some of these tips to help ease the discomfort:
- Raise your feet from the foot of your bed
- At the end of each shower, spray cold water over your legs in an upward motion from the ankles to the thighs
- Avoid sources of heat (prolonged exposure to the sun, high-temperature baths, underfloor heating, etc.
 )
) - Massage your legs every day, from the ankles to the knees, using a specific treatment cream to increase blood return and stimulate blood flow
Signs Of Heavy Or Aching Legs
Aching or heavy legs first appear as a sensation of discomfort, fatigue, and heaviness in the legs. These sensations can be the first sign of an actual circulation impairment alongside other characteristics, such as having pain:
- In the interior and posterior area of the calf that radiates up the leg toward the inside of the knee
- Most often felt towards the end of the day
- If you remain standing for a long time or if you are in contact with heat (summer temperatures, hot baths, hot-wax treatments, etc.)
- Increase as the pregnancy progresses
- Relieved by cold temperatures, winter climates, rest, elevation of the legs, and walking
- Accompanied by cramps at night, restlessness of the legs (painful discomfort that requires that one move one’s legs for relief), inflammation (edema of the ankles), varicosities, and even varicose veins
If you are experiencing any of these symptoms, talk about it with your doctor at your next visit. Your doctor may be able to prescribe a suitable treatment for you.
Your doctor may be able to prescribe a suitable treatment for you.
Causes Of Aching Or Heavy Legs
Like most expecting moms, you’re probably wondering what’s causing your aching or heavy legs. The sensation of heavy or aching legs is related to a loss of firmness and elasticity of the vein walls, which causes a slowing of blood circulation in the veins. Because of this, the veins dilate and blood pressure increases.
Valves — the small flaps that normally keep blood from flowing back down the leg veins — have difficulty maintaining this pressure and progressively become deficient.
Resistance to leaks weakens and blood stagnates in the lower portion of the veins, which further impairs vein walls. A vicious cycle takes hold.
On top of this, other factors could be causing your aching legs, such as:
- Nerve pressure: When your uterus expands, it puts pressure on certain nerves, which can trigger spasms and cause pain in your legs.
- Dehydration: If your body doesn’t get the right amount of hydration during your pregnancy — and it needs a lot! — it can really suffer.
 Whether you’re dealing with morning sickness, stress, or cramps, drinking water can be the easy answer to all your pregnancy woes. When in doubt, take the water route!
Whether you’re dealing with morning sickness, stress, or cramps, drinking water can be the easy answer to all your pregnancy woes. When in doubt, take the water route! - Increase in your weight: Your legs are carrying around more weight than they’re used to. They’re having to work a little harder each day, so at the end of the day, they’re tired just like you.
- Swelling: Swelling is no stranger to pregnancy, especially in the heat. When your ankles and feet start to swell in the heat, as we’ve mentioned above, circulation gets restricted. This is when your legs start to ache and get heavy. (Note: If you notice consistent swelling in your legs and feet, or your leg starts to feel warm, reach out to your obstetrician right away.)
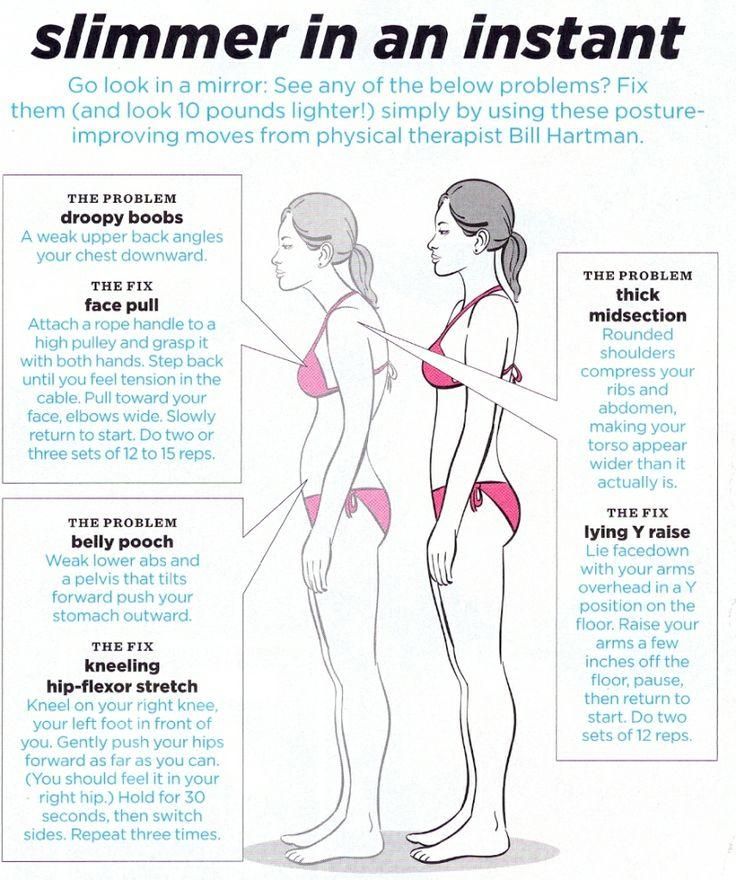
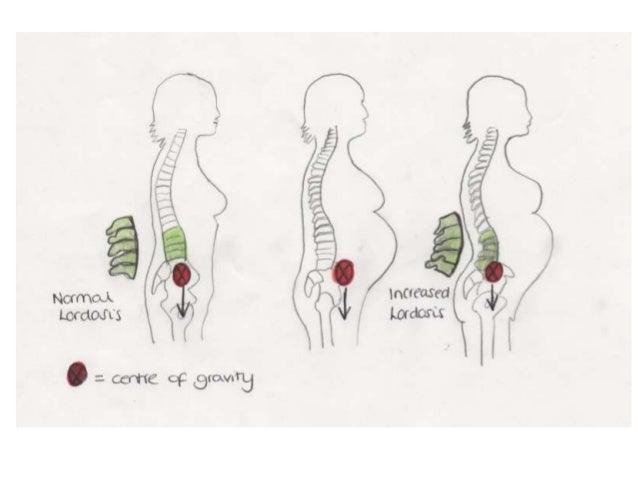
- Changes in your posture as your baby grows: Throughout stages of your pregnancy, your baby has taken different positions inside your uterus. This can take a toll on your body, especially your back.
 Your posture starts to change throughout your pregnancy without you even noticing at times, but your legs are sure to take notice of the change. Your legs have to support you throughout these different stages, and it can impact them.
Your posture starts to change throughout your pregnancy without you even noticing at times, but your legs are sure to take notice of the change. Your legs have to support you throughout these different stages, and it can impact them. - Fluid retention: Your growing uterus puts pressure on the veins that carry blood back from your lower body, which partially blocks blood flow. As a result, fluid remains in your legs and feet.
- Joint laxity: As we’ve discussed, when you’re carrying the extra weight from your precious baby, it’s a lot for your legs — but it’s also a lot for your joints. Your joints can easily become stressed from the added pressure. Your joints may seem a little loose and you might even waddle when you walk!
At-Home Treatment
Most often, your leg aches can be relieved at home. That’s something to shout about because we know leg aches can really be a Debby Downer as you wrap up your day!
Here are a few ideas to relieve your leg aches and heavy legs at the end of the day:
- Stretch your calf muscles by flexing and releasing each foot a few times
- Take short walks throughout the day to boost blood flow
- Avoid standing or sitting with your legs crossed for long periods
- Take a warm bath before bed (After getting out of a relaxing bath, don’t forget to apply Stretch Marks Oil to help limit the appearance of stretch marks! It leaves your skin restored, refreshed, and noticeably smoother.
 )
) - Massage your legs throughout the day and especially before bed (Try using our Body Firming Gel to give your legs a little massage. It hydrates your skin, giving it a firmer look and overall feel.)
- Take a calcium supplement (with the go-ahead from your doctor)
- Drink a glass of milk before bed
- Prop your legs up on a pillow (make sure your legs are elevated above your heart)
- Wear compression leggings or socks
- Increase your potassium intake
Medical Treatment
If your legs are painful and you see no improvement after trying the recommended measures outlined in the previous section, do not hesitate to see a doctor. They can prescribe suitable treatment for your condition.
Various methods — from medicinal to physical to surgical — may be considered, depending on the severity of your circulatory impairments:
- Compression via pantyhose, stockings, or socks is the basic treatment for anyone experiencing venous insufficiency.
 Different models are available depending on the strength of compression necessary. Significant progress has been made in improving the esthetics of these garments. The cost of some of these compression methods may be eligible for Social Security reimbursement.
Different models are available depending on the strength of compression necessary. Significant progress has been made in improving the esthetics of these garments. The cost of some of these compression methods may be eligible for Social Security reimbursement. - Venotonics have anti-inflammatory properties, stimulating muscle tone and protecting the elasticity of the vein walls. They must be taken for an extended period of time in order to be effective.
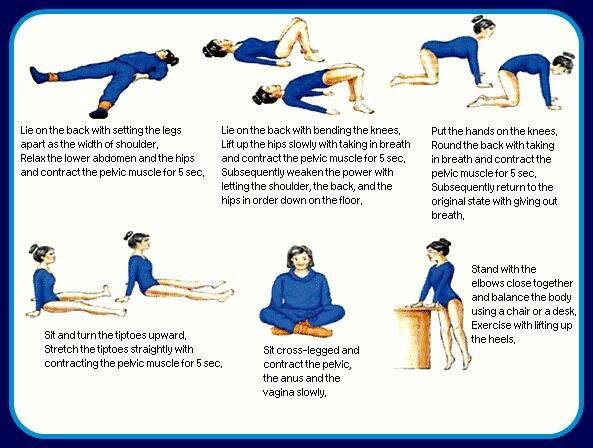
- Kinesitherapy and exercises to build up the leg muscle also have a role to play. Walking, swimming and biking are the best types of activity. Spa treatments, massages, and manual lymphatic drainage can also provide valuable relief.
- If varicose veins developed during your pregnancy and are still present after delivery, vein sclerotherapy or surgery may be considered. These techniques can be performed under local anesthesia, requiring neither an epidural nor general anesthesia, and the patient can go home the same day as treatment, or the following day.
A Comfortable Pregnancy
Aching and heavy legs can be caused by a variety of factors, as we listed above. Although these unpleasant sensations usually disappear on their own after delivery, they should not be taken lightly.
Heavy legs can turn into vascular pathologies that can sometimes be disabling. Monitor your heavy legs closely and give them the appropriate care from the very first signs to limit the risk of complications.
But keep in mind that most often, it’s not a cause for concern or harmful to your baby. Use at-home treatments to ease your leg aches and heavy legs. You may have to try a few before you find what works for you.
And while you’re at it, continue taking care of yourself during your pregnancy by treating your skin. Using the right products that have been clinically proven to effectively help expecting mothers, like our Stretch Marks Cream, will make for one comfortable pregnancy!
Tired pregnancy legs | Pregnancy health
Half of us suffer from aching, tired, crampy legs during pregnancy, usually in our last trimester and, often – infuriatingly – at night.
The aches happen because, obviously, your legs are having to support a whole lot more of you than usual, as well as adjust to ferrying around a body that's carrying more of its weight out front.
Your growing uterus is also putting pressure on the veins whose job it is to carry blood back from your lower body – and this pressure partially blocks the blood flow, keeping fluid in your legs and feet and making them feel swollen and tired.
Swelling in your legs is not generally, by itself, a cause for concern but do see your midwife or GP if you notice your face is swollen and puffy, too, or you're also getting headaches.
Click through to the next pages for clever ways to relieve those mid to late-pregnancy leg aches and pains...
Sleep on your left
Sleep with your legs raised by 10-15 cms. You can do this by putting a couple of cushions under your ankles or buying a block of foam from an upholstery or mattress shop. You’re also advised to sleep on your left side when you’re pregnant. This is to help improve blood flow to your baby and to help your kidneys get rid of waste products. All this helps to cut down on swollen pregnancy ankles and the uncomfortable feeling in your legs. You might find wedging a cushion between your knees helps as your pregnancy progress.
This is to help improve blood flow to your baby and to help your kidneys get rid of waste products. All this helps to cut down on swollen pregnancy ankles and the uncomfortable feeling in your legs. You might find wedging a cushion between your knees helps as your pregnancy progress.
Watch your posture
You want to avoid any kind of behaviour that’s going to stop your blood circulating around your body. The easiest way to do this? Stop crossing your legs! Yes, we know it’s hard when you’ve sat like that for the whole of your life, but it really will help with tired and heavy legs. Unfortunately, like most habits, it’s hard to break. To stop you doing it at work trying sticking a post-it to your screen that says ‘Don’t cross your legs). At home maybe put a piece of sticking plaster on the remote control with the same message written on it. Once you’ve curbed the urge for a few weeks the bad habit will be a thing of the past.
Take a walk
Exercise is one of the best things to get your circulation going and stop those tired legs from aching. But you don’t need to do anything manic. Just walking for half an hour every day should be enough to make them feel better. Of course, make sure you’re in comfy shoes and remember to breathe properly. And don’t overdo it. If you start to feel lightheaded stop and have a sit down.
But you don’t need to do anything manic. Just walking for half an hour every day should be enough to make them feel better. Of course, make sure you’re in comfy shoes and remember to breathe properly. And don’t overdo it. If you start to feel lightheaded stop and have a sit down.
More like this
Don’t get too tight
Pre-pregnancy it’s possible skin tight jeans were your wardrobe staple, but now you have a bump and baby on board, you might want to reconsider. Avoid any clothes that are likely to hinder your circulation – like jeans or socks that are too tight.
Indulge in a massage
We never need an excuse for a massage. But now you have a reason for your partner to give you one every day - your aching legs and feet! It’s also a good chance for you and the other half to have a bit of quiet one-on-one time to catch up on any concerns going through your heads now you’re going to become parents.
Diastasis of the rectus abdominis muscles and diastasis of the womb.
 Solvable problems of pregnancy. Interview with Doctor of Medical Sciences, Professor M.A. Chechnevoy
Solvable problems of pregnancy. Interview with Doctor of Medical Sciences, Professor M.A. Chechnevoy — What is muscle diastasis and what is pubic symphysis diastasis?
— Pregnancy is an amazing and wonderful time, but it is also a period of additional loads, which undoubtedly becomes a test of strength for the female body.
The previously existing everyday point of view that pregnancy rejuvenates and gives strength is not confirmed by anything. During the bearing of a child, significant additional loads are placed on the mother's body, which often lead to the manifestation of problems that were invisible before pregnancy.
Diastasis of the rectus abdominis muscles is a divergence of the inner edges of the muscles along the white line of the abdomen (connective tissue structure) at a distance of more than 27 mm. Pubic diastasis is one of the manifestations of pregnancy-associated pelvic girdle pain. This pathology affects the entire pelvic ring, sacroiliac joints and symphysis. And they certainly have common causes for the appearance.
And they certainly have common causes for the appearance.
The formation of such problems is facilitated by a decrease in the strength of connective tissue collagen. One of the reasons is an innate predisposition, the so-called connective tissue dysplasia, when the tissues are very elastic, extensible. During pregnancy, the body of a woman increases the production of the hormone relaxin, which reduces the synthesis of collagen and enhances its breakdown. This is provided by nature to create maximum elasticity of the birth canal. However, other structures, such as the anterior abdominal wall and the pubic symphysis, also fall under the action of relaxin.
— How does diastasis of the muscles and diastasis of the pubis affect pregnancy and childbirth?
- The divergence of the rectus abdominis muscles is observed in about 40% of pregnant women. During pregnancy, it does not give serious complications that threaten the life of the mother or the condition of the fetus.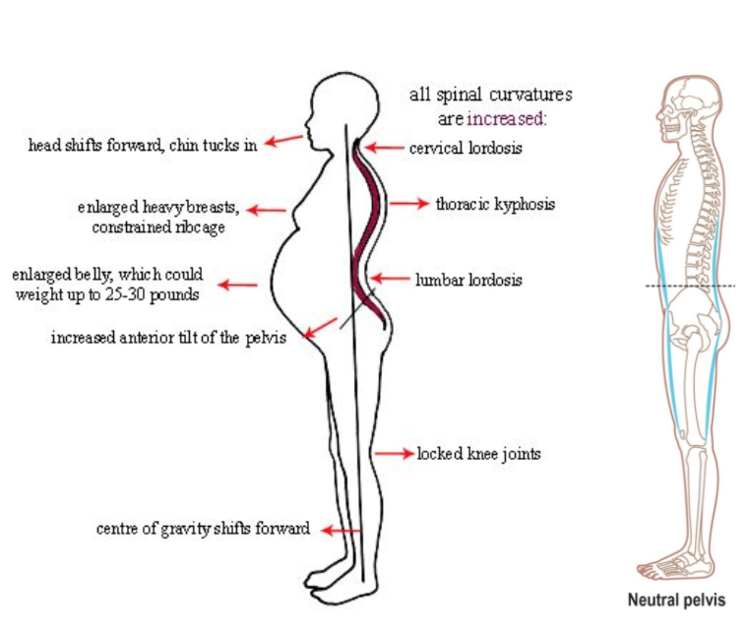 However, the inferiority of the work of the rectus abdominis muscles forces the redistribution of the load on the back muscles, which can lead to lumbar-pelvic pain and, accordingly, discomfort in the back. During childbirth, the abdominal muscles are involved in attempts, and the violation of their anatomy and function can affect the birth act.
However, the inferiority of the work of the rectus abdominis muscles forces the redistribution of the load on the back muscles, which can lead to lumbar-pelvic pain and, accordingly, discomfort in the back. During childbirth, the abdominal muscles are involved in attempts, and the violation of their anatomy and function can affect the birth act.
With diastasis of the pubis, things are more complicated. As already mentioned, this is only one of the manifestations of a violation of the structure and function of the pubic joint (symphysiopathy) during pregnancy. It occurs in about 50% of pregnant women in varying degrees of severity: in 25% of cases it leads to restriction of the mobility of the pregnant woman, in 8% - to severe disorders up to disability.
With symphysiopathy, the ligaments of the pubic articulation and the cartilages that connect the pubic bones are affected. All this leads to severe pain in the pubic joint, pelvic bones, lower back, as well as to a violation of gait and the inability to stand up or lie down without outside help. Women with pelvic girdle pain syndrome experience significant levels of discomfort, disability, and depression, with associated social and economic problems. These include impaired sexual activity during pregnancy, chronic pain syndrome, risk of venous thromboembolism due to prolonged immobility, and even seeking early induction of labor or caesarean section to stop pain.
Women with pelvic girdle pain syndrome experience significant levels of discomfort, disability, and depression, with associated social and economic problems. These include impaired sexual activity during pregnancy, chronic pain syndrome, risk of venous thromboembolism due to prolonged immobility, and even seeking early induction of labor or caesarean section to stop pain.
During childbirth, this patient may experience rupture of the pubic symphysis and may require surgery to repair it.
— How to prevent the development of muscle and pelvic diastasis during pregnancy and childbirth? What factors increase the likelihood of its development?
- There is no recipe that will be one hundred percent. There is a wonderful term in the medical literature called "lifestyle modification". Whatever diseases we study, be it symphysiopathy, diabetes mellitus or preeclampsia, the risk group for pathology is always overweight women. You need to prepare for pregnancy, you need to be in good physical shape. During pregnancy, weight gain should be monitored. The recommendation to "eat for two" is not just wrong, but extremely harmful. Pregnant women should maintain reasonable physical activity. Weak and flabby abdominal muscles, combined with the large size of the fetus, undoubtedly increase the risk of diastasis.
During pregnancy, weight gain should be monitored. The recommendation to "eat for two" is not just wrong, but extremely harmful. Pregnant women should maintain reasonable physical activity. Weak and flabby abdominal muscles, combined with the large size of the fetus, undoubtedly increase the risk of diastasis.
The risk factors for symphysiopathy in numerous studies are hard physical labor and previous injuries of the pelvic bones. Factors such as time elapsed from previous pregnancies, smoking, use of hormonal contraception, epidural anesthesia, mother's ethnicity, number of previous pregnancies, bone density, weight and gestational age of the fetus (post-term fetus) are not associated with an increased risk of symphysiopathy.
— How to diagnose diastasis recti and diastasis pubis?
— In most cases, diastasis rectus abdominis can be diagnosed clinically. It happens that inspection, palpation and simple measurements are enough.
In the standing position, you can see the divergence of the muscles when the woman does not have subcutaneous fat. In this case, diastasis is defined as a vertical defect between the rectus muscles.
In this case, diastasis is defined as a vertical defect between the rectus muscles.
With tension of the abdominal press, a longitudinal protrusion is observed in the diastasis zone. Such a protrusion is especially noticeable if the patient in the supine position is asked to raise her head and legs. If necessary, you can measure the width of the defect simply with a ruler.
Ultrasound may be the most accurate diagnostic method. With ultrasound, the inner edges of the rectus muscles are clearly visible and the distance between them at different levels can be measured.
Computed tomography is used in the diagnosis of diastasis extremely rarely, mainly in scientific research.
For the diagnosis of symphysiopathy and diastasis pubis there is no one test as a "gold standard".
The first place, of course, is the questioning and examination of the patient. We pay attention to the gait of the pregnant woman, to how she sits down, lies down and how she gets up. Symphysiopathy is characterized by a “duck gait”, when a pregnant woman rolls from foot to foot. On palpation in the area of the womb, pain and swelling are noted. The so-called pain provocative tests are used, for example, a mat-test (pulling up an imaginary rug, mat with your foot towards you).
Symphysiopathy is characterized by a “duck gait”, when a pregnant woman rolls from foot to foot. On palpation in the area of the womb, pain and swelling are noted. The so-called pain provocative tests are used, for example, a mat-test (pulling up an imaginary rug, mat with your foot towards you).
The following questionnaires are used to assess quality of life, pain and disability: Health-Related Quality of Life (HRQL), Oswestry Disability Index (ODI), Disability Rating Index (DRI), Edinburgh Postpartum Depression Scale (EPDS), Pregnancy Mobility Index (PMI), and Pelvic Ring Score (PGQ).
Of the instrumental methods, ultrasound is the most widely used, less often computed or magnetic resonance imaging. Ultrasound allows you to assess the condition of the ligaments of the pubic joint and the interpubic disc, the severity of the changes and the risk of natural childbirth.
— What is the treatment for diastasis recti or pubis?
— Primary prevention: when planning and during pregnancy, it is necessary to strengthen all muscle groups of the pelvic girdle, as well as the pelvic diaphragm.
More often, diastasis of the rectus muscles disappears on its own during the first months after childbirth. Special physical exercises to correct the work of muscles, to tone them and restore their basic functions should be performed under the guidance of a competent instructor. There are types of physical exercises that can, on the contrary, worsen the situation with diastasis of the rectus abdominis muscles. In some cases, when there is no effect from physiotherapy exercises, it is necessary to resort to surgical correction of the defect. Currently, both endoscopic and open surgery are practiced. The choice of method depends on the size and localization of the defect.
With symphysiopathy, therapeutic exercises reduce lumbar and pelvic pain. Acupuncture and wearing a pelvic bandage have a positive effect on symphysiopathy.
Initial treatment of pubic symphysis should be conservative even if symptoms are severe. Treatment includes bed rest and the use of a pelvic brace or corset that tightens the pelvis. Early appointment of physiotherapy with dosed therapeutic exercises will help to avoid complications associated with prolonged immobilization. Walking should be done with assistive devices such as walkers.
Early appointment of physiotherapy with dosed therapeutic exercises will help to avoid complications associated with prolonged immobilization. Walking should be done with assistive devices such as walkers.
In most cases (up to 93%), the symptoms of dysfunction of the pelvic ring, including the pubic joint, progressively subside and completely disappear six months after birth. In other cases, it persists, becoming chronic. However, if the diastasis exceeds 40 mm, then surgical treatment may be required. Most studies recommend surgery only after failure of conservative treatment, inadequate enlargement of diastasis, or its recurrence. Several procedures have been described, including external fixation and open reduction of the pubic bones with internal fixation.
The best advice for prevention, diagnosis and treatment: ask a competent doctor all the questions that worry you. Only the joint efforts of the doctor and the patient can overcome all problems and find the best solutions.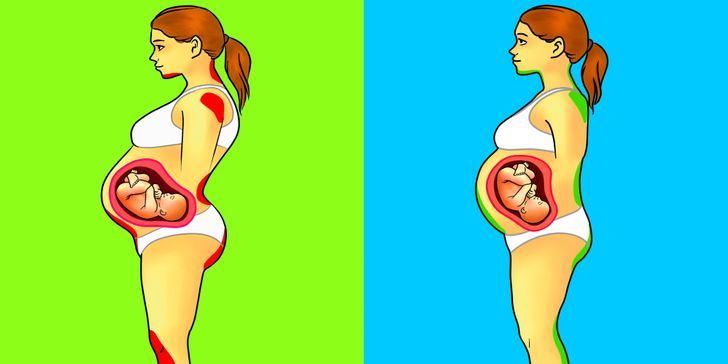
Why does the stomach pull in the early stages of pregnancy?
Why does the stomach pull in early pregnancy? This question often worries expectant mothers, and at times leads to panic. When is discomfort pathology, and when is it normal?
Pregnancy is a special time for a mother and her baby. After all, the connection between them is inextricable, and every negative influence or stress affects both of them.
Possible causes of pain
Every woman dreams of an easy pregnancy and no cause for alarm. However, a very common complaint among pregnant women is pain in the lower abdomen of a pulling or aching nature.
Complaints are so common that it is necessary to clearly understand when pulling sensations during pregnancy are pathological and require immediate medical attention, and when they are completely physiological and require only general recommendations.
Of course, pain in the lower abdomen can appear at any stage of pregnancy, however, most often women notice their appearance in the early stages of pregnancy.
Painful sensations in the abdomen during pregnancy are very diverse both in subjective sensations and in their localization, in intensity of occurrence. Pain can appear both at rest and after any physical activity. Unpleasant sensations can manifest themselves in one place, or radiate to other areas.
Unpleasant sensations in the lower abdomen are rarely avoided during pregnancy. These sensations can occur not only in pathology. During pregnancy, the uterus increases in size, there is a tension in its ligaments and muscles. In addition, there is a displacement of the pelvic organs. All this leads to the appearance of pulling or aching sensations in the abdomen. All these phenomena are manifestations of physiological changes that occur to a woman during pregnancy.
Of course, this state of fear does not cause and does not require any intervention on the part of the doctor. However, pulling pains in the lower abdomen are not always a physiological process. It happens that this indicates that the pregnancy proceeds with pathology and requires medical adjustment.
It happens that this indicates that the pregnancy proceeds with pathology and requires medical adjustment.
That is why, if there are pulling or aching pains in the lower abdomen, it is necessary to contact an obstetrician-gynecologist in order to accurately determine the cause of the pain.
Never self-medicate. Remember that you are responsible not only for yourself, but also for the little man that you carry under your heart.
Abdominal pain during pregnancy may be:
- "obstetric";
- "non-obstetric".
Pain associated with pregnancy may be developmental:
- physiological changes during pregnancy;
- threatened miscarriage;
- miscarriage;
- ectopic pregnancy.
Pain not associated with pregnancy may occur with:
- inflammatory processes;
- pathologies of the digestive system;
- surgical diseases;
- diseases of other organs or systems.

Pain in the lower abdomen during pregnancy as a variant of the norm
Not all pain in the lower abdomen during pregnancy is a manifestation of pathology. Sometimes they can occur during the normal course of pregnancy.
As a physiological process, pain in the lower abdomen can occur in the following situations:
- sign of pregnancy;
- displacement of the pelvic organs by the growing uterus;
- stretching of the ligaments and muscles associated with the growth of the uterus.
Abdominal pain is a sign of pregnancy
Finding out that you are pregnant is now not a big deal, because there are pregnancy tests. In addition, a delay in menstruation can serve as evidence of pregnancy.
All this is good when menstruation is regular and delayed by at least 14 days. In this case, the pregnancy test may be positive. However, do not forget that not all tests are highly accurate, so it can show two cherished strips much later than we would like.
Therefore, it is necessary to pay close attention to the sensations of your body, because it signals the onset of pregnancy long before the manifestation of a delay in menstruation.
If you assume that pregnancy is possible, then listen carefully to your body: it can send you a signal in the form of pulling pains in the lower abdomen. At the same time, the pains will differ in their intensity: one woman will say that the pains are unbearable, the other will not notice them at all. Each woman is individual.
If each menstruation is preceded by unpleasant pain in the lower abdomen or lower back, you may not understand that once again they are associated with the onset of pregnancy.
Pain in the lower abdomen during pregnancy may be associated with the implantation process. To do this, you need to remember the process of fertilization of the egg by the sperm. After their fusion in the fallopian tubes, the fertilized egg enters the uterus under the action of the movement of cilia in the fallopian tubes.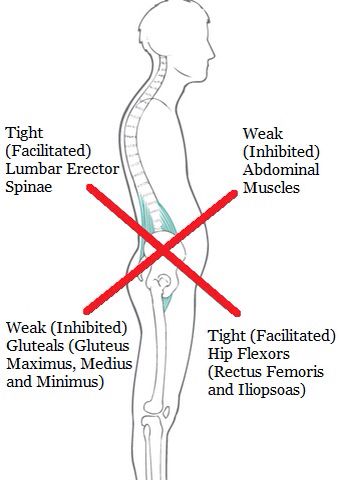 The uterine endometrium is a loose mass where a fertilized egg is implanted.
The uterine endometrium is a loose mass where a fertilized egg is implanted.
The process of implantation is the introduction of a fertilized egg into the endometrium of the uterus. At this time, there is a violation of the integrity of the endometrium, which may be accompanied by unpleasant sensations in the lower abdomen. In addition, sometimes slight dark bloody discharge may appear from the genital tract, which can be perceived as the beginning of another menstruation.
Threatened miscarriage
A fairly common cause of pain in the lower abdomen is a threatened miscarriage. This condition is individual and does not depend on physical exertion or complete rest, but on the condition of the woman and her unborn child.
Causes that may cause miscarriage include:
- heavy physical exertion;
- sexual contact;
- malnutrition of the ovum;
- genetic disorders and other causes.
Of course, this is not evidence that a miscarriage will not occur with complete rest. Miscarriage can occur due to genetic abnormalities, and due to stress. No woman is immune from the threat of pregnancy loss.
Miscarriage can occur due to genetic abnormalities, and due to stress. No woman is immune from the threat of pregnancy loss.
That is why attention and sensitivity to the state of your body is so necessary, which will in every possible way send signals that the pregnancy is not going the way you want.
Threatened miscarriage is accompanied by:
- aching or pulling pains in the lower abdomen;
- aching or drawing pains in the small of the back or sacrum.
- bloody discharge from the genital tract.
If you experience pain in the lower abdomen, you should consult a doctor, as a threatened miscarriage, if not provided with medical assistance, can turn into an abortion that has begun, the treatment of which is much more difficult, if not completely useless.
An ambulance should be called if:
- pain in the lower abdomen gets worse;
- pains begin to radiate to other areas;
- painful sensations do not go away for a long time;
- bloody discharge from the genital tract appeared.

Increased pain
If the pulling pains in the lower abdomen are weak, do not increase and do not radiate to other areas, then you can come to the antenatal clinic in the daytime on your own. This will not threaten serious complications of your condition.
If the pain becomes more intense, does not go away at rest, you should not self-medicate, take drugs without a doctor's prescription.
Do not put anything on the stomach. Both hot and cold application can contribute to the onset of a miscarriage. In addition, with the threat of termination of pregnancy, this manipulation will not remove the pain.
Localized pain
When a threatened miscarriage occurs, pain of a pulling or aching nature disturbs the pregnant woman in the lower abdomen.
If the pains have a clear localization in a certain place, most often on the right or left, then a mandatory consultation with a specialist is necessary, since an ectopic pregnancy or surgical pathology, such as appendicitis, may develop.
Bloody discharge from the genital tract
If bloody discharge from the genital tract has joined the pulling pain in the lower abdomen, urgent medical attention is needed. This phenomenon may indicate a miscarriage that has begun.
The discharge may be scanty, spotting or copious, dark or bright. In any case, you can not do without consulting an obstetrician-gynecologist.
There are situations when there is no pain, but there is bloody discharge from the genital tract. This case also requires specialist advice.
Any bloody discharge from the genital tract may indicate a miscarriage. Only timely treatment can contribute to the preservation and prolongation of pregnancy.
In some cases, the appearance of bloody discharge from the genital tract may be a manifestation of a miscarriage, which requires immediate medical attention.
Missing pregnancy
A fertilized egg does not always develop correctly. In some cases, there is a cessation of its division and death.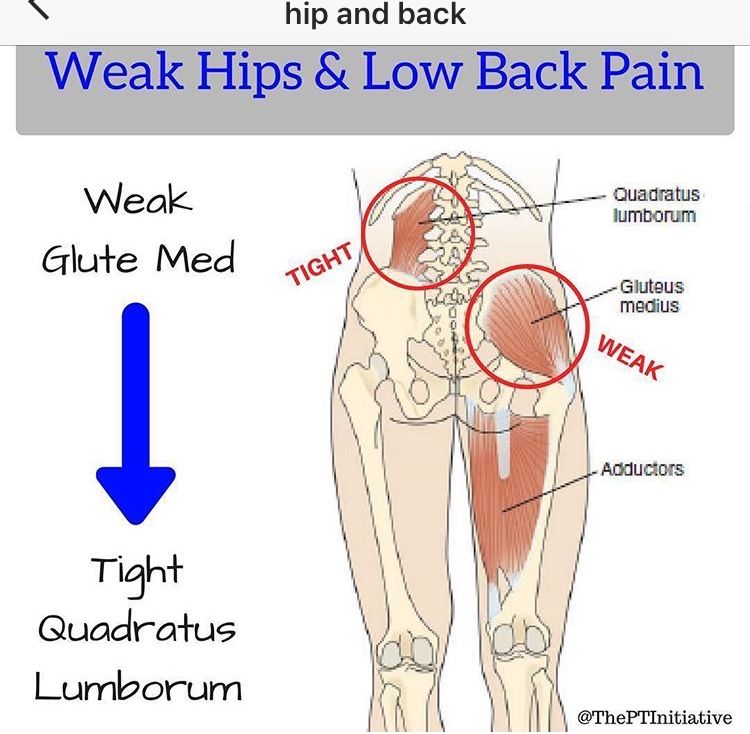 Most often, missed pregnancy occurs due to any mutations. At the same time, the woman does not suspect that the pregnancy has stopped.
Most often, missed pregnancy occurs due to any mutations. At the same time, the woman does not suspect that the pregnancy has stopped.
However, the dead fetal egg begins to be rejected on its own. At the same time, there are pulling pains in the lower abdomen, which are soon joined by bloody discharge from the genital tract.
When a miscarriage is diagnosed, curettage of the uterine cavity may be indicated. Conservative management is also possible, but this can only be determined by a specialist after consultation.
Ectopic pregnancy
Ectopic pregnancy most often occurs as a tubal pregnancy, when the fertilized egg does not reach the uterus, and the implantation process occurs in the fallopian tube. At the same time, the development of the fetal egg can continue for a long time without any manifestations, up to 12 weeks of pregnancy. However, most often such a pregnancy is interrupted at 6 to 8 weeks.
The fertilized egg develops and grows, which causes pain in the right or left side of the lower abdomen.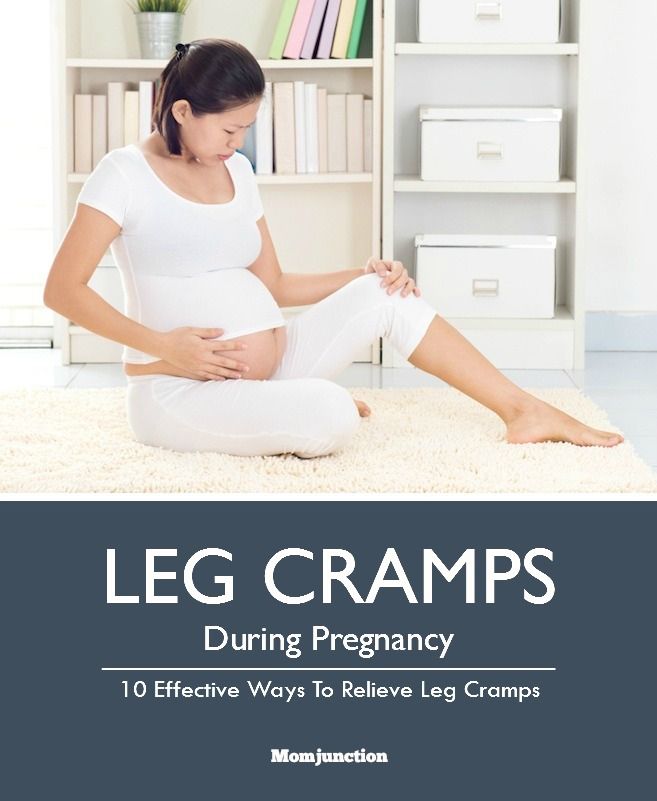 The pains are unilateral, are obsessive, tend to increase.
The pains are unilateral, are obsessive, tend to increase.
In addition to pain in the lower abdomen, bloody discharge from the genital tract appears, and the pain begins to radiate to the leg from the side of the pain. There may be unpleasant sensations of pressure on the rectum. Medical surgery is the only way to save a woman's life. Preservation of pregnancy is impossible.
"Non-obstetric" causes of pain in the lower abdomen
Inflammatory processes
Among the "non-obstetric" causes of pain in the lower abdomen, the most common are inflammatory processes of the pelvic organs. If earlier it was believed that there could be no inflammation in pregnant women, now it has been proven that a decrease in the immunity of a pregnant woman awakens all pathological processes in her body.
Pain in inflammatory processes of the pelvic organs differ in their intensity. At the same time, they occur in the lower abdomen and most often have a pulling or aching character.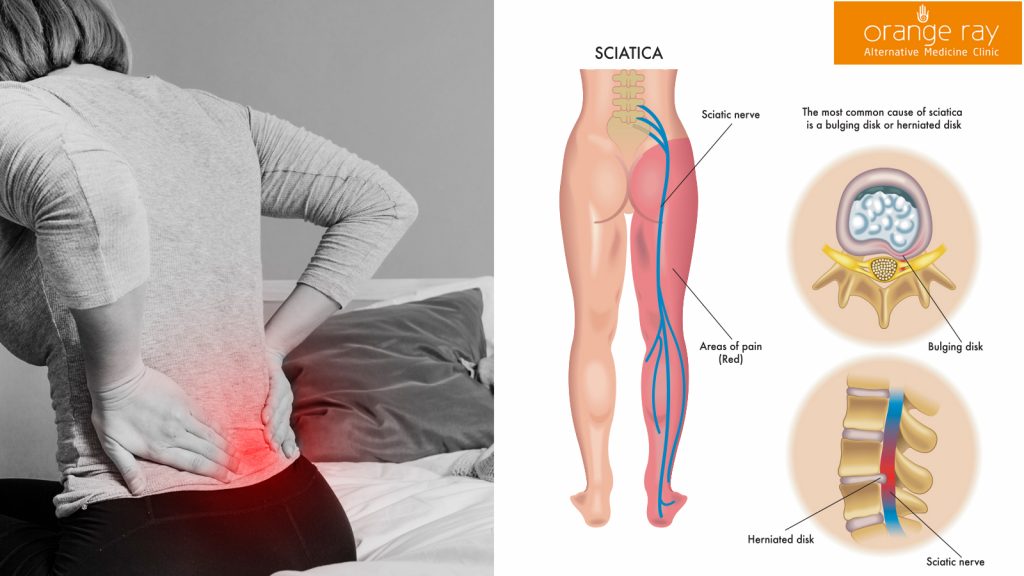
Pathology of the digestive system
Very often, pulling pains in the lower abdomen can occur in a pregnant woman due to problems with the digestive tract. During pregnancy, there is a decrease in intestinal contractility. In addition, there are significant changes in the hormonal background of a woman. Therefore, very often pregnancy is accompanied by constipation and bloating. To normalize digestion, a change in diet is recommended and mild laxatives can be taken.
Surgical pathology
Of the surgical pathologies that may be accompanied by pulling pains in the lower abdomen during pregnancy, acute appendicitis is the most common.
In the early stages of pregnancy, it is obligatory to differentiate obstetric and gynecological diseases from appendicitis, since it has similar symptoms. There are pains in the lower abdomen, which most often occur in the navel or stomach, and then descend to the right iliac region. Nausea, vomiting, fever joins. The only treatment is surgery.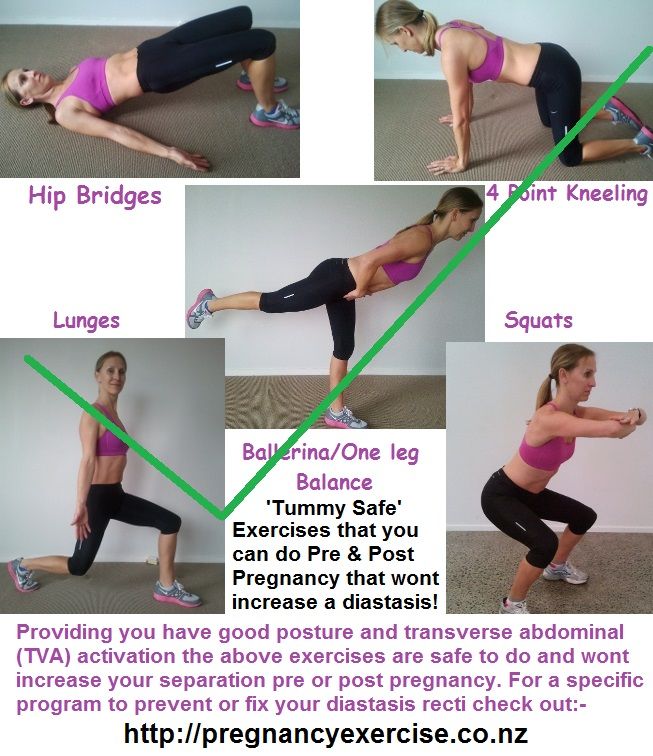 In this case, the pregnancy is preserved.
In this case, the pregnancy is preserved.
Diseases of other organs or systems
In addition to obstetric and surgical causes, which can cause pulling pains in the lower abdomen in early pregnancy, other body systems may also be involved in the pathological process. The most common lesion is the urinary tract.
Cystitis
Cystitis due to the anatomical features of a woman can occur at any time and in any condition, so pregnant women are just as susceptible to it as non-pregnant women.
The bladder, located in the lower third of the abdomen, may give false symptoms of threatened miscarriage.
Cystitis, in addition to pulling or aching pains in the lower abdomen, is accompanied by pain during urination, pain at the end of the act of urination. In addition, with cystitis, the urine may be stained with blood, and it is difficult to distinguish this from bloody discharge during a miscarriage.
In any case, it is necessary to consult an obstetrician-gynecologist, pass a general urine test, and then consult a urologist and treat the infection.