Yellow stuff from eyes
Eye - Pus or Discharge
Is this your child's symptom?
- Yellow or green discharge (pus) in the eye
- The eyelids are stuck (matted) together with pus after sleep
- After being wiped away, the pus comes back during the day
- Often caused by a bacterial eye infection
Causes of Eye with Pus
- Bacterial Conjunctivitis. This is a bacterial infection of the eye. The main symptom is eyelids stuck together with pus after sleep. Can be present in 1 or both eyes. A few viruses can cause pus in the eyes, but most don't.
- Viral Conjunctivitis. This is a viral infection of the eyes. Main symptom is pinkness of the white parts of the eyes. The eyes are also watery. Most often, there is no pus. Usually on both sides.
- Normal Discharge. A small amount of dried mucus only in the corner of the eye. It may not even be pus. A collection of mucus can be cream colored. Often due to an irritant that got in the eye from dirty hands.
Needs no treatment except wiping it away with warm water.
- Blocked Tear Duct. Present in 10% of newborns. Main symptom is a constant watery eye. Tears fill the eye and run down the face. This happens even when not crying. The eye is not red and the eyelid is not swollen. The wet eye may get secondary infections. This will cause the eyelids to become matted with pus.
- Foreign Object in Eye (Serious). Small particles such as sand, dirt or sawdust can be blown into the eyes. The grit often gets stuck under the upper eyelid. If not removed, the eye reacts by producing pus. The main clue is an eye infection that does not respond to antibiotic eyedrops. Older children complain of feeling something in the eye.
- Eyelid Cellulitis (Serious). This is a deep infection of the eyelid and tissues around it. The main symptom is a red, swollen, very tender eyelid. The eye can be swollen shut. Usually only on one side. This can be a problem caused by bacterial conjunctivitis.
 The eye infection spreads inward. More commonly this is caused by an ethmoid sinus infection. That type occurs without any pus in the eye.
The eye infection spreads inward. More commonly this is caused by an ethmoid sinus infection. That type occurs without any pus in the eye.
Symptoms of Bacterial Eye Infection
- Yellow or green discharge or pus in the eye
- Dried pus on the eyelids and eyelashes
- The eyelashes are more likely to be stuck together after sleep
- The whites of the eye may or may not be red or pink
- The eyelids are often puffy
When to Call for Eye - Pus or Discharge
Call Doctor or Seek Care Now
- Eyelid is very red or very swollen
- Vision is blurred
- Eye pain or discomfort is more than mild
- Fever over 104° F (40° C)
- Fever in baby less than 12 weeks old. Caution: do NOT give your baby any fever medicine before being seen.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- Pus in the eye, but none of the symptoms above.
 Reason: you may need antibiotic eyedrops to treat it.
Reason: you may need antibiotic eyedrops to treat it. - Using antibiotic eye drops more than 3 days and pus is still there
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Pus In the Eye
- What You Should Know About Bacterial Eye Infections:
- Bacterial eye infections are common with colds.
- They respond to home treatment with antibiotic eye drops which need a prescription.
- They are not harmful to vision.
- Until you get some antibiotic eye drops, here is some advice that should help.
- Bacterial eye infections are common with colds.
- Remove Pus:
- Remove all the dried and liquid pus from the eyelids. Use warm water and wet cotton balls to do this.
- Do this whenever pus is seen on the eyelids.
- Also, remove the pus before the antibiotic eye drops are put in. Reason: they will not work if you don't.
- The pus can spread infection to others. So, dispose of it carefully.
- Wash your hands well after any contact with the pus.
- Antibiotic Eye Drops: How to Use
- For a cooperative child, gently pull down on the lower lid. Put 1 drop inside the lower lid. Then ask your child to close the eye for 2 minutes. Reason: so the medicine will get into the tissues.
- For a child who won't open his eye, have him lie down.
 Put 1 drop over the inner corner of the eye. If your child opens the eye or blinks, the eye drop will flow in. If he doesn't open the eye, the drop will slowly seep into the eye.
Put 1 drop over the inner corner of the eye. If your child opens the eye or blinks, the eye drop will flow in. If he doesn't open the eye, the drop will slowly seep into the eye.
- Contact Lenses:
- Children who wear contact lenses need to switch to glasses until the infection is gone.
- Reason: to prevent damage to the cornea.
- Disinfect the contacts before wearing them again.
- Discard them if they are disposable.
- Return to School:
- Your child can return to school when the pus is a small amount.
- Antibiotic eye drops should be used for 24 hours before going back.
- What to Expect:
- With treatment, the pus discharge should clear up in 3 days.
- The red eyes may last up to a week.
- Call Your Doctor If:
- Eyelid gets red or swollen
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.

Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 12/06/2022
Last Revised: 01/13/2022
Copyright 2000-2022. Schmitt Pediatric Guidelines LLC.
Eye Discharge: Causes, Types and Treatment
By Aimee Rodrigues; reviewed by Pamela Miller, OD, FAAO, JD, FNAP
Find Eye Doctor
What is eye discharge?
Eye discharge, or "sleep" in your eyes, is a combination of mucus, oil, skin cells and other debris that accumulates in the corner of your eye while you sleep. It can be wet and sticky or dry and crusty, depending on how much of the liquid in the discharge has evaporated.
Other slang terms used to describe eye discharge include eye mattering, eye boogers, eye gunk, eye pus and goopy eyes.
Sometimes called "rheum," eye discharge has a protective function, removing waste products and potentially harmful debris from the tear film and the front surface of your eyes.
Your eyes produce mucus throughout the day, but a continuous thin film of tears bathes your eyes when you blink, flushing out the rheum before it hardens in your eyes.
When you're asleep — and not blinking — eye discharge collects and crusts in the corners of your eyes and sometimes along the lash line, hence the term "sleep" in your eyes.
Some sleep in your eyes upon waking is normal, but excessive eye discharge, especially if it's green or yellow in color and accompanied by blurry vision, light sensitivity or eye pain, can indicate a serious eye infection or eye disease and should be promptly examined by your eye doctor.
Where does eye mucus come from?
Eye discharge (rheum) is a function of your tear film and a necessary component of good eye health. It primarily consists of thin, watery mucus produced by the conjunctiva (called mucin), and meibum — an oily substance secreted by the meibomian glands which helps keep your eyes lubricated between blinks.
Causes of eye discharge
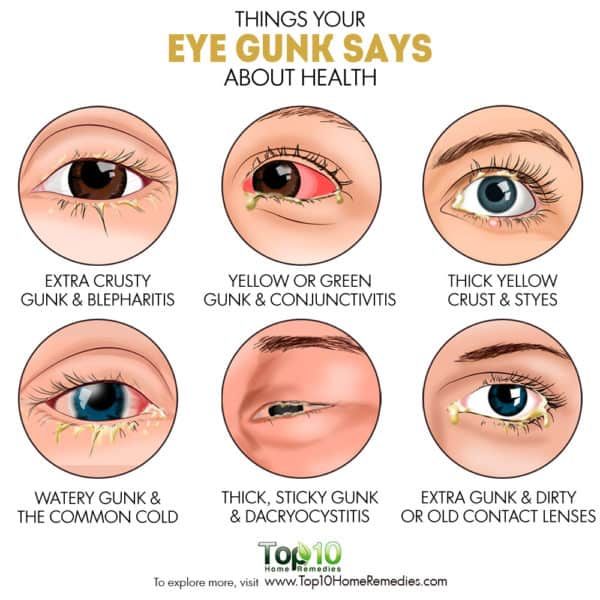
Sleep in your eyes usually isn't cause for alarm, but if you notice a difference in consistency, color and quantity of eye gunk, it could indicate an eye infection or disease.
Common eye conditions associated with abnormal eye discharge include:
Conjunctivitis
Eye discharge is a common symptom of conjunctivitis (pink eye), an inflammation of the conjunctiva — the thin membrane that lines the "white" of the eye (sclera) and the inner surface of the eyelids.
Thick, yellow eye discharge can be caused by an eye infection.
In addition to itchy, gritty, irritated and red eyes, conjunctivitis typically is accompanied by white, yellow or green eye mucus which can form a crust along the lash line while you sleep.
In some cases, eyelid crusting can be so severe that it temporarily seals your eye shut.
There are three types of pink eye: viral, bacterial and allergic.
Viral conjunctivitis is highly contagious and is caused by a virus such as the common cold or herpes simplex virus. Eye discharge associated with viral pink eye typically is clear and watery, but may include a white or light yellow mucus component.
Eye discharge associated with viral pink eye typically is clear and watery, but may include a white or light yellow mucus component.
Bacterial conjunctivitis, as the name indicates, is caused by bacterial infection and can be sight-threatening if not treated promptly. Eye discharge is usually thicker and more pus-like (purulent) in consistency than viral pink eye, and is commonly yellow, green or even gray. Often, the sticky mattering will cause your eyelids to feel completely glued shut upon waking in the morning.
Allergic conjunctivitis is triggered by allergens — pollen, dander, dust and other common irritants that cause eye allergies. It also can be caused by an allergic reaction to chemical pollutants, makeup, contact lens solutions, and eye drops. Eye discharge associated with allergic conjunctivitis is typically watery.
Unlike viral and bacterial pink eye, allergic conjunctivitis is not contagious and always affects both eyes.
Other eye infections
In addition to conjunctivitis, there are many eye infections that cause abnormal eye discharge. These include: eye herpes (a recurrent viral eye infection), fungal keratitis (a rare but serious inflammation of the cornea) and Acanthamoeba keratitis (a potentially blinding infection typically caused by poor contact lens hygiene or swimming while wearing contacts).
These include: eye herpes (a recurrent viral eye infection), fungal keratitis (a rare but serious inflammation of the cornea) and Acanthamoeba keratitis (a potentially blinding infection typically caused by poor contact lens hygiene or swimming while wearing contacts).
Discharge from an eye infection varies considerably — it could be clear and watery or thick, green and sticky — so make sure you see your eye doctor promptly for an accurate diagnosis and treatment.
Blepharitis
A chronic disorder of the eyelids, blepharitis describes either inflammation of the eyelash hair follicles or abnormal oil production from the meibomian glands at the inner edge of the eyelids. A related condition called Meibomian gland dysfunction (MGD) can cause foamy eye discharge, eyelid crusting, as well as yellow or green eye pus, among other irritating and often painful symptoms.
Stye
A stye is a clogged meibomian gland at the base of the eyelid, typically caused by an infected eyelash follicle. Also called a hordeolum, it resembles a pimple on the eyelid margin and is commonly accompanied by redness, swollen eyelids and tenderness in the affected area. Yellow pus, eyelid crusting and discomfort while blinking also can occur.
Also called a hordeolum, it resembles a pimple on the eyelid margin and is commonly accompanied by redness, swollen eyelids and tenderness in the affected area. Yellow pus, eyelid crusting and discomfort while blinking also can occur.
An eye stye usually resolves on its own, but there are also some home remedies for styes you can try. It's important to refrain from squeezing the pus from a stye to reduce the risk of the infection spreading to other areas of the eye.
SEE ALSO: Why you should never pop a stye
The tear drainage system keeps the eye moist and protected.
Dry eyes
Insufficient tear production or dysfunction of the meibomian glands can lead to dry eye syndrome — an often chronic condition in which the surface of the eyes is not properly lubricated and becomes irritated and inflamed.
Symptoms of dry eyes include red, bloodshot eyes, a burning sensation, blurry vision and a feeling something is "in" your eye (foreign body sensation). Sometimes, dry eyes also can cause a very watery eye discharge to occur.
Sometimes, dry eyes also can cause a very watery eye discharge to occur.
Contact lenses
If you wear contact lenses, you may find more sleep in your eyes than normal. This can be due to a number of reasons, including a contact lens-related eye infection, contact lens discomfort resulting in dry and irritated eyes, as well as rubbing your eyes more while wearing contacts.
If you experience an increase in eye discharge when wearing contacts, remove your lenses and see your eye doctor to rule out a potentially serious eye condition.
Eye injury
A foreign body in the eye (such as dirt, debris or a chemical substance) or an eye injury can cause your eyes to secrete a watery discharge as a natural protective response.
If eye pus or blood in the eye (subconjunctival hemorrhage) occurs after an eye injury, see your eye doctor immediately for treatment. All eye injuries should be treated as a medical emergency.
Corneal ulcer
A corneal ulcer is a sight-threatening, abscess-like infection of the cornea, usually caused by trauma to the eye or an untreated eye infection. If not treated promptly, corneal ulcers can lead to complete vision loss. Eye pain, redness, swollen eyelids and thick eye discharge are characteristic of a corneal ulcer. Eye pus can be so severe that it clouds the cornea and impairs vision.
If not treated promptly, corneal ulcers can lead to complete vision loss. Eye pain, redness, swollen eyelids and thick eye discharge are characteristic of a corneal ulcer. Eye pus can be so severe that it clouds the cornea and impairs vision.
Dacryocystitis
When a tear duct is blocked, the lacrimal sac in the tear drainage system leading to the nose can become inflamed and infected, causing a tender and swollen bump to appear under the inner eyelid. In addition to pain and redness, common symptoms of dacryocystitis include watery eyes, a sticky eye discharge and blurred vision.
Eye discharge treatment
A small amount of eye discharge is harmless, but if you notice changes in the color, frequency, consistency and amount, consult your eye doctor.
If an eye infection is the cause of eye mucus, your eye care practitioner may prescribe antibiotic or antiviral eye drops and ointments. If eye allergies are making your eyes watery and irritated, over-the-counter antihistamine eye drops and decongestants may relieve symptoms.
Warm compresses placed over your eyes may help relieve symptoms of itching and general eye discomfort, as well as help remove eye goop.
If your eyelids are stuck together, the best way to "unglue" your lids is to wet a washcloth in warm water and place it over your eyes for a few minutes before gently wiping away the eye gunk.
At-home checklist
Follow these simple tips to avoid or manage eye discharge:
Refrain from touching your eyes to avoid the onset or spread of an eye infection.
Wash your hands frequently, especially if you have contagious pink eye.
If you experience eye discharge when wearing contacts, remove your lenses and see your eye doctor. Sometimes switching to daily disposable contacts or a different contact lens material can reduce the risk of contact lens-related discharge.
If you have an eye infection, discard any potentially contaminated cosmetics such as mascara and eyeliner, as well as current contacts, which may be contaminated.

If allergies are the cause of your watery eyes, investigate your environment and try to remove or minimize your exposure to the irritants. And if you're sensitive to eye drops, try using preservative-free drops.
Note for Parents
Babies and blocked tear ducts
Many babies are born with obstructed tear ducts — the tubes that drain tears from the surface of the eyes to the nasal cavity — causing watery eyes and (sometimes) eye discharge.
Symptoms of a blocked tear duct include a constant pooling of tears in the eye (even when the child isn't crying), which can spill onto the cheek. Sticky eye mucus also may be present, especially collecting on the eyelid margin and causing the eyelashes stick together.
To help relieve symptoms, keep the area clean by regularly wiping your baby's eyes with a clean, moist cloth. Gently massage the inner corner of your infant's eyes to help to open or unblock the tear duct.
While most cases of blocked tear ducts resolve over the first several months of a child's life, at the first signs of a blocked tear duct always see your baby's eye doctor for a comprehensive eye exam to rule out a more serious problem.
If your infant's eyes are producing a thick yellow or green discharge, or there is redness and swelling around the eyes, this could indicate an eye infection that should be evaluated by your eye doctor straightaway.
SEE RELATED: Eye discharge in toddlers and babies
Page published on Monday, March 4, 2019
Medically reviewed on Friday, April 30, 2021
Yellow eyes: a disease or nothing to worry about? Should action be taken?
From All About Vision
Have you noticed that the whites of your eyes have turned yellow? Jaundice, overuse of certain medications, or other medical conditions, sometimes even serious ones, can cause yellow eyes.
This article tells you everything you need to know about yellow eyes and how to deal with them.
What causes yellow eyes?
The sclera (white of the eye) should always look like white . If suddenly it turns red or changes its color, you need to contact an ophthalmologist to identify the cause of the color change.
Ictericity (icterus) of the conjunctiva
One of the causes of changes in eye color may be icterus of the conjunctiva. This is the medical term used for yellowing of the eyes. (Sometimes the term "icteric sclera" is also used to describe yellowing of the eyes.)
Jaundice
In most cases, yellow eyes are a symptom of jaundice: due to an increase in the level of the pigment bilirubin, the skin and eyes change their color. Although jaundice is not a disease in itself, it is an indication that the liver, gallbladder, and bile ducts are not functioning properly.
Jaundice is most common in newborns. According to the US Centers for Disease Control and Prevention (CDC), approximately 60% of all newborns have jaundice. Premature babies are at increased risk because their livers have not yet developed enough to clear bilirubin.
Jaundice is much less common in older children or adults. If this happens, then a more serious disease requiring treatment is usually suspected. As in the case of newborns, first of all, attention should be paid to the liver.
As in the case of newborns, first of all, attention should be paid to the liver.
Mild cases of neonatal jaundice usually go away on their own. Only 1 in 20 children may need specialized treatment. The standard treatment for moderate jaundice is light (phototherapy), which reduces bilirubin levels and the child usually recovers very quickly.
The change in eye color with jaundice does not affect vision.
Diseases associated with yellow eyes
The most common diseases that can cause yellow eyes are:
-
Acute pancreatitis, or infection of the pancreas
-
Certain types of cancer, including cancer of the liver, pancreas, or gallbladder.
-
Hemolytic anemia (a congenital blood disease) characterized by a lack of red blood cells as a result of their premature breakdown.
-
Malaria (an infectious disease of the blood) transmitted by mosquito bites.
-
Certain blood disorders that affect the production and life cycle of red blood cells, such as sickle cell anemia.

-
Rare genetic disorders that affect the ability of the liver to clear bilirubin.
Other diseases and drugs that can cause yellow eyes:
-
Autoimmune diseases that affect the human immune system. Hepatitis A, B, and C viruses infect liver cells, causing acute (short-term) or chronic (long-term) hepatitis and yellowing of the eyes.
-
Obstructive jaundice can occur when one or more of the ducts that carry bile from the liver to the gallbladder is blocked by gallstones. As a result of violation of the outflow of bile is absorbed into the blood.
-
Cirrhosis, the end stage of chronic liver disease where scarring occurs, reduces the ability of the liver to filter out bilirubin. Cirrhosis results from various forms of liver disease, including hepatitis, non-alcoholic steatohepatitis, and chronic alcoholism. All these diseases cause yellowing of the eyes.
-
Certain drugs, such as over-the-counter acetaminophen (when overused) or prescription drugs such as penicillin, oral contraceptives, chlorpromazine, and anabolic steroids, can also cause yellow eyes.
Pinguecula: Not quite yellow eyes, but...
Another condition that causes yellow eyes is pinguecula.
A pinguecula is a yellow deposit that appears on the surface of the sclera, causing that part of the eye to turn yellow.
The eye does not turn yellow completely, but only in the place where the pinguecula has grown.
These formations can be caused by excessive exposure to UV rays from prolonged exposure to the sun. If the pinguecula grows and causes discomfort, surgery is indicated.
OTHER RELATED MATERIALS: Pinguecula (yellow growth on the eye): definition, causes and treatment
Yellow eye treatment
Yellow eye treatment depends on the underlying cause of yellow eyes.
Yellowing of the eyes is a visible sign of certain medical conditions. At the same time, it is important to determine the accompanying symptoms in order to find out the nature of the health problem.
Associated symptoms may include itchy skin, bloating, fatigue, fever, light-colored stools, dark-colored urine, loss of appetite, nausea, and rapid weight loss.
In order to prescribe the correct and effective treatment, it is necessary to carry out examinations, including checking the level of bilirubin in the blood, a comprehensive blood count and a liver test.
Examination results, symptom analysis, history, physical examination of the patient, and possibly imaging studies will help to make a correct diagnosis.
If the underlying cause of yellow eyes is an infectious disease, such as hepatitis C or malaria, antibiotics, as well as antifungal and antiviral drugs, may be treated.
If the patient has a history of excessive alcohol or drug use, treatment should begin with stopping the use of these substances.
Diet can also play a significant role. The liver processes and metabolizes most of the nutrients that enter the body. But hard-to-digest substances make it difficult to work. It is refined sugar, salt and fat with a high content of saturated fatty acids.
Patients with jaundice are advised to maintain a drinking regimen and eat foods that are good for the liver - fruits and vegetables, whole grains, healthy proteins, nuts and legumes.
As the liver recovers after treatment, jaundice and yellowing of the eyes also resolve.
In some cases, surgery may be needed to correct concomitant factors such as blockage of the bile ducts.
Yellowing of the eyes? See an ophthalmologist
If you think your eyes are turning yellow, see an ophthalmologist immediately.
After a thorough eye examination and if an illness is suspected, an optometrist or ophthalmologist may refer you to a specialist or another doctor.
Do not underestimate the yellowing of the eyes. If liver disease or another disease is the underlying cause, prompt diagnosis and effective treatment can prevent a serious complication that can result in damage to internal organs.
Page published on Monday, November 16, 2020
causes, diseases, treatment methods
Yellow whites of the eyes: causes
Yellowed sclera (whites) of the eyes cannot go unnoticed. This is not an independent disease, but the result of pathology, i. e. another illness. With yellow whites of the eyes, the Patient does not experience pain and other discomfort, except for aesthetic. For this reason, people rarely seek medical help, waiting for more severe symptoms to appear.
e. another illness. With yellow whites of the eyes, the Patient does not experience pain and other discomfort, except for aesthetic. For this reason, people rarely seek medical help, waiting for more severe symptoms to appear.
The yellow color of the sclera may be a congenital feature, and in some cases the mucous membrane changes color abruptly and may retain it for a long time. This is a signal of a serious violation in the body.
The main reason is the high level of bilirubin, a bile component that causes pigmentation of the skin and mucous membranes. This condition may indicate the presence of a serious liver disease, such as hepatitis or an infection in the body.
Diseases associated with yellow whites of the eyes
Yellowness of the sclera can appear with blood diseases, poisoning, malignant neoplasms of the conjunctiva.
The reason for the change in the color of the sclera can be bad habits, for example, smoking abuse, as well as:
- Liver disease (liver cirrhosis, hepatitis, cancer).
 With liver damage, the concentration of bilirubin increases
With liver damage, the concentration of bilirubin increases - Violation of metabolic processes in the body (Gilbert's disease (pigmented hepatosis, characterized by a moderate intermittent increase in the content of free bilirubin in the blood), Wilson-Konovalov's disease (congenital disorder of copper metabolism, leading to severe hereditary diseases of the central nervous system and internal organs, amyloidosis ( a systemic disease in which amyloid (a protein-polysaccharide substance) is deposited in organs and tissues, which leads to a violation of their functions))
- Blood disease eg enzymopathy, babesiosis, hemoglobinopathies, malaria. With these diseases, red blood cells are destroyed, and the concentration of hemoglobin increases
- Diseases of the eye , e.g. benign and malignant conjunctivitis, melanoma, pinguecula, pterygium, in which isolated spots appear on the mucous membrane of the eyes
- Diseases of the pancreas .
 The appearance of yellowness on the whites of the eyes is associated with a violation of the outflow of bile from the liver into the duodenum
The appearance of yellowness on the whites of the eyes is associated with a violation of the outflow of bile from the liver into the duodenum - Poisoning of the body with helminths eg echinococcosis, amoebiasis.
Methods of diagnosis and treatment
Treatment is prescribed after a comprehensive ophthalmological examination and includes medication, hardware, surgical and other methods of treatment. Sometimes, in order to get rid of the yellowness of the sclera, it is enough for the Patient to change the diet and lifestyle. Since yellowness of the sclera is a symptom, the main treatment is carried out by a specialized specialist (therapist, infectious disease specialist, etc.).
Consultation with an ophthalmologist is recommended in case of the appearance of individual yellow spots or complete "yellowing" of the mucous membrane of the eye. Even if there are no other symptoms, we recommend that you contact your doctor to find out the causes and prescribe timely treatment for the underlying disease.