Water birth pain
How to prepare for a water birth
What is a water birth?
Water birth is the process of giving birth in water using a deep bath or birthing pool. Being in water during labour is shown to help with pain as well as being more relaxing and soothing than being out of water. The water can help to support your weight, making it easier to move around and feel more in control during labour.
Can I have a water birth?
Having a water birth is an option for you if you have had a low risk pregnancy and your midwife or obstetric doctor believes it is safe for you and your baby. You can talk to them about it at any of your antenatal appointments.
You may not be able to have a water birth if:
- your baby is breech
- you are having twins or triplets
- your baby is pre-term (under 37 weeks)
- your baby has passed meconium before or during labour
- you have active Herpes
- you have pre-eclampsia
- you have an infection
- you have a high temperature in labour
- you are bleeding
- your baby needs continuous monitoring via CTG machine
- your waters have been broken for over 24 hours
- you have had a previous caesarean section
- your labour is induced
- you are at high risk of having birth difficulties.
You will probably be advised not to have a water birth if you have any of the risk factors above because it may be difficult to get you out of the pool safely in an emergency. If you have an infection, you may be at risk of passing it onto your baby in the water.
If you are at high risk of bleeding, being in the pool can be dangerous because it is difficult to measure how much blood has been lost in the water.
Ask your midwife if any of the above apply to you.
What are the advantages of water birth?
- The warm water can help to relax, soothe and comfort you.
- The support of the water means you can try different positions and move more freely.
- When upright in the water, gravity will help move the baby down towards the birth canal.
- Being in water can lower your blood pressure and reduce feelings of anxiety, making your body more able to release endorphins, which can help ease pain.
- The water can help to improve back pain and the feeling of pressure, especially when you are fully dilated.

- Being in the pool during labour and birth can be a “cosy” experience, making you feel safe.
- The water can help your perineum stretch gradually as the baby’s head is being born, reducing the risk of injury.
'I was surprised by how warm it was in the water, and so nice and relaxing! They were able to check the baby’s heartbeat while I was inside the pool. I hadn’t eaten so they even made me some toast and my mum had to feed me while I was in the birth pool.' Jade (read her full story)
Are there any disadvantages of having a water birth?
- You will not be able to have some pain-relief options. For example, you cannot have any opiates, such as pethidine, for at least six hours before you get into the pool, and you cannot have an epidural.
- You will be unable to use a Tens machine.
- Your contractions may slow down or get weaker, especially if you go in the pool too soon.
- If the pool water is too cool at birth, your baby is at risk of hypothermia.
 But your midwife will check the water temperature regularly. If your baby’s temperature is low, skin to skin contact with you and warm towels will help.
But your midwife will check the water temperature regularly. If your baby’s temperature is low, skin to skin contact with you and warm towels will help. - You might need to leave the pool if there is a complication.
'When I had my water birth, I was in the pool from about 12.30pm until 3pm but unfortunately my contractions slowed down a bit, so I had to get out of the pool and finish off labour on the bed.'Jade (read her full story)
Can my baby drown if I give birth in water?
Many women wonder whether there is a risk of their baby drowning if they give birth in water but it is very unlikely to happen.
Babies do not need to breathe when they are in the womb because they get oxygen from the blood that comes from their mum through the placenta. When they are born in water, their body behaves as if they are still in the womb until they take their first breath of air, at which point their lungs open up. As a baby comes from water (in the womb) into water (in the birth pool), the lungs are not open and no water can enter.
After your baby is born in the water, you and your midwife will bring them to the surface slowly. Your baby will only be under water for a short time and won’t take a breath until they are out of the water.
Your baby is only at risk:
- if their head is brought above the water and brought down again
- if their oxygen supply from the placenta is affected
- if their temperature changes suddenly.
Your midwife will be careful to make sure this does not happen.
Where can I have a water birth?
- At home, with a hired birthing pool
- In a birth centre
- On the labour ward.
Find out more about where you can give birth.
What should I wear for my water birth?
You can wear what feels comfortable for you, keeping in mind that you will be in what is essentially a large bath. Many women choose to wear a bikini or tankini. Others choose to just wear a bra. You can wear a t-shirt or vest top if you want to be a little more covered. It can be twisted up and tucked into the neck if it’s very long. Some women prefer to be naked.
It can be twisted up and tucked into the neck if it’s very long. Some women prefer to be naked.
Whatever you feel comfortable with wearing on your top half is fine.
It is best to take your bottom half off so that the midwife can see what is happening as you approach birth. However, if you wish to leave your pants on until that stage, that is fine too.
What other pain relief can I have in the water?
Water is sometimes referred to as ‘nature’s epidural’ or ‘aquadural’, because of the support and pressure it gives you. However, if you need a little extra, it is common to use gas and air (Entonox) while you are in the birth pool. The Entonox tubing is waterproof so this can be used in the pool too.
Find out more about pain relief during labour.
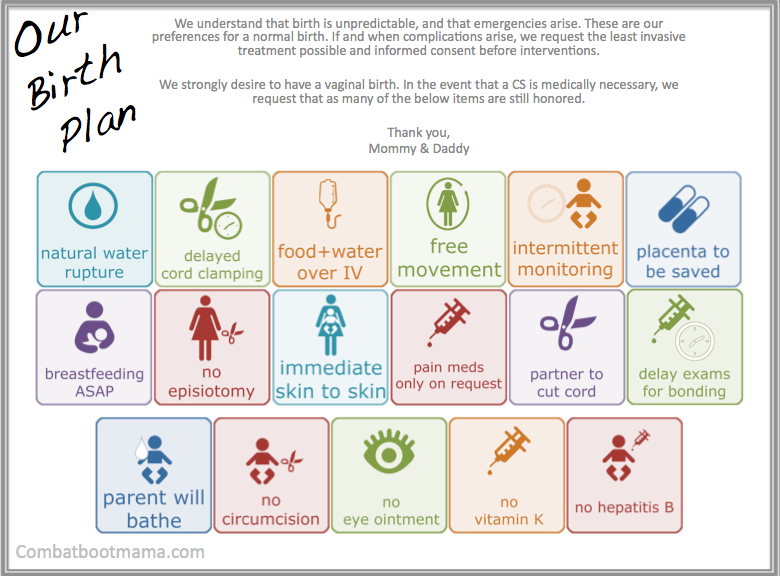
Can I have optimal / delayed cord clamping if I give birth in the water?
Delayed cord clamping (DCC) has become very normal. Most birth centres, labour wards and home birth teams will try to do DDC for every birth. This is because holding off from cutting the cord until the blood from the placenta has stopped going into your baby can increase your baby’s iron levels and the amount of stem cells they have, which will help with their growth and immune system. Although many centres practise DCC as normal, you can add this to your birth plan just in case your hospital does not.
This is because holding off from cutting the cord until the blood from the placenta has stopped going into your baby can increase your baby’s iron levels and the amount of stem cells they have, which will help with their growth and immune system. Although many centres practise DCC as normal, you can add this to your birth plan just in case your hospital does not.
The only reason DCC would not happen is if you or your baby are suddenly unwell just after birth. If the baby is slow to breathe, or you are bleeding more heavily than normal, the midwife may need to cut the cord earlier than usual.
Your and your baby’s safety during and after a water birth is very important and this will always take priority.
Find out more about delayed cord clamping.
How do I deliver the placenta if I have a water birth?
Your midwife is likely to ask you to get out of the pool to deliver the placenta because gravity can be helpful in the third stage of labour. It also makes it easier to help you in case of an emergency, as some new mums can feel faint after birth, or during the third stage of labour. If you do suddenly feel lightheaded, it may be difficult to get you out of the pool quickly and safely.
If you do suddenly feel lightheaded, it may be difficult to get you out of the pool quickly and safely.
Most hospitals, birth centres and home birth teams have a policy on how the placenta should delivered, and most of these are on a bed, toilet, birth stool or floor mat for your safety. Please ask your midwife about this policy.
Find out more about the third stage of labour.
Can I have the injection to deliver the placenta more quickly?
You can be given an oxytocin injection to speed up the delivery of the placenta in the pool. Your thigh or bottom will need to be slightly raised out of the water for this to happen. You will then need to leave the pool within a few minutes to deliver the placenta.
When might I need to get out of the pool?
- If the midwife sees meconium (when the baby does a poo whilst still inside).
- If you start to bleed heavily from the vagina.
- Your labour becomes abnormal, changes in your temperature or blood pressure for example.
- If the baby’s heart rate changes.
- To go to the toilet (you can leave and return).
- For your midwife to examine you to check your progress.
- If your labour slows down or if your contractions get weaker.
- To deliver the placenta.
Can I change my mind about having a water birth?
Yes. Even if it is in your birth plan, if you decide you don’t want to get into the pool then you don’t have to.
If you get in the birth pool and don’t like it, you can get out again.
Do not be worried about changing your mind. Midwives are happy to support you as long as you and the baby are safe.
'I’m so glad I went for a water birth and would definitely recommend it! If I have another baby in a few years, which I hope to do, I'm really hoping the birthing pool is available for me to use again!' Jade (read her full story)
Water births and labouring in water: questions answered | Labour & birth articles & support
Giving birth or at least labouring in water is becoming ever more popular and for good reason. It’s a great pain reliever and more. Here we explain all.
It’s a great pain reliever and more. Here we explain all.
Whether or not you’re much of a water baby yourself, labouring or giving birth in water has a whole load of advantages. The great thing is that you should be offered the chance to labour in water, if possible, whether you’ve had children before or are a first-time mother (NICE, 2014).
About 10% of women in the UK give birth in pools but nearly 20% use water for pain relief (CQC, 2018). Water births started gaining in popularity when the Department of Health recommended them for pain relief in 1993 (Winterton, 1992; Cumberledge et al, 1993; Garland, 2000). But it’s not just about the pain…
Why use water in labour or for giving birth?
- Women say they feel more relaxed, involved in decision-making and more in control when using water for labour and birth.
- It is an effective pain reliever – women use less epidural or spinal pain relief when they have access to water.
- It’s safe for you and your baby – there is no increased chance of the baby being admitted to neonatal care after a water birth.

- It might make the first stage of labour shorter and one study said it shortened labour by almost two hours.
- Less or equal blood loss.
(Cluett et al, 2018; Dekker, 2018; RCM, 2018; Ulfsdottir et al, 2018)
Can water births prevent tearing, episiotomy or interventions?
It won’t prevent tearing or episiotomy but it’s possible water births might make them less likely. Yet the evidence is mixed and there has been no research in midwifery-led settings, where there are fewer interventions in any case than in hospitals (Brocklehurst et al, 2011; Cluett et al, 2018).
One study suggests there is less chance of interventions or second-degree tears with water births (Ulfsdottir et al, 2018). While a large review of various studies suggests water has little effect on tearing or interventions in the first stage of labour. That review couldn’t make any conclusions on the rates of tearing for the second stage of labour as the studies did not record them (Cluett et al, 2018).
Another review suggested there is a higher chance of straightforward birth in an upright position with midwife’s ‘hands off’ the perineum with a water birth. They also said that labouring or giving birth in water might make bad tears and episiotomies less likely but may mean minor tears are more likely (Dekker, 2018).
Are water births safe for the baby?
Yes, water births are safe. It makes no difference in how healthy babies are, and they’re no more likely to have difficulty breathing or to die. In fact, some research suggests your baby is less likely to need a transfer to hospital or stay in hospital or to be admitted to neonatal intensive care. Your baby won’t get cold either – there’s no increase in newborn hypothermia with water births (Dekker, 2018).
As for infections, they’re not more likely to get group B Strep infections. Water births also make no difference to babies’ microbiomes (Dekker, 2018).
What are the potential risks of a water birth?
Training has become standardised so that situations like babies inhaling water have not been seen for many years. Even when that has happened in the past, the babies recovered. Midwives are trained to be gentle with the cord too when guiding the baby out of the water, to prevent a (rare) cord snap (Dekker, 2018).
Even when that has happened in the past, the babies recovered. Midwives are trained to be gentle with the cord too when guiding the baby out of the water, to prevent a (rare) cord snap (Dekker, 2018).
There is no increase in the risk of infection in newborns but some isolated cases have been reported. Effective cleaning and pool management protocols have reduced the chance of this happening.
As for the mums, water births carry no increased risk of maternal infections (Dekker, 2018).
Can you have water births with gas and air, TENS, epidurals or pethidine?
It's not possible to have an epidural in water. TENS is electrical stimulation so it’s also incompatible with water births.
As for what you can use in water, you can breathe a bit sigh of relief that entonox (gas and air) is fine for water births. And you can use self-help techniques like breathing, movement, massage, visualisation, distraction, or other complementary therapies to your heart’s content in water.
When it comes to epidurals, a few women labour in water for a while but get out to have an epidural or further assistance. In any case, labouring in water seems to reduce the chance of having an epidural (Cluett et al, 2018). Water also reduces the need for other forms of pain relief, and women are more satisfied with the pain relief water provides (Dekker, 2018).
A woman can use both water and opioids (e.g. pethidine) during labour, but not at the same time. If she has used pethidine she will need to wait for guidance from her midwife that it has passed out of her system before getting in the water, usually a few hours.
When can’t I labour or birth in water?
The NICE guidelines say that all ‘healthy women and babies...between 37 and 42 weeks of gestation’ should be offered the opportunity to labour in water (NICE, 2014). But here’s where it gets complicated – women outside of those criteria are not actually excluded from using water in labour. What it actually means is that this is an opportunity for you and your health professionals to explore each other’s concerns, before you decide.
There might be local guidance too and you can ask for this. You can also ask to talk with a consultant midwife to explore your options. All NHS midwives are trained to support women birthing in water.
The local Maternity Voices Partnership (MVP), or AIMS may also be interested in supporting you if you want, and these contacts can be found on the internet.
When an NHS Trust is not comfortable with supporting a woman in hospital, some women will decide to use a pool at home, with either an NHS or an independent midwife.
Can I have a water birth if I have a high BMI?
Your BMI (body mass index) will be taken into consideration along with your preferences, mobility, and any other conditions (NICE, 2019). You can talk to your health professional about how your BMI might affect things (NICE, 2019). Local guidance may affect whether women with high BMIs have water births (Marshall, 2019).
Can I have a water birth if I have herpes?
If you’re in the third trimester of your pregnancy and it’s the first time you’ve had genital herpes, you’ll be offered a planned caesarean. This is because a caesarean decreases the risk of passing the infection to the baby (NICE, 2011).
This is because a caesarean decreases the risk of passing the infection to the baby (NICE, 2011).
If you have a recurrence of herpes, you won’t be routinely offered a caesarean because of the lack of evidence that a caesarean will reduce the risk of passing on the infection to the (NICE, 2011). It’s best to talk with the health professionals caring for you about how a recurrence of herpes may affect your choice for a water birth.
Can I have a water birth if I’m expecting twins?
Selective (caesarean) birth may be offered early to reduce risk for the babies, while expectant management (watchful waiting) is also possible (NICE, 2011a). Women can discuss options with their carers, and some women will decide to birth in a pool.
Can I have a water birth if I have Group B Strep?
Guidelines say there is no reason you can’t use water during labour and birth as long as you’re offered intrapartum antibiotic prophylaxis (IAP) (RCOG, 2017). Although one report suggested there was insufficient evidence around transmission of Group B Strep, with no increased chance found in the available evidence (Dekker, 2018).
Can I have a water birth if I have gestational diabetes?
The concern here is likely to be the estimated size of the baby and its effect on the progress of labour, i.e. you may be offered an induction. You can discuss this with the health professionals who are caring for you. Some women choose to have a water birth with well-controlled gestational diabetes.
Can I have a water birth if I am due to be induced?
This tends to fall under local practice. Where appropriate facilities exist (i.e. a pool on the obstetric unit) and staff are confident, then women do have water births even when the labour is being induced.
This page was last reviewed in March 2019
Further information
Our support line offers practical and emotional support with feeding your baby and general enquiries for parents, members and volunteers: 0300 330 0700.
We also offer antenatal courses which are a great way to find out more about labour and life with a new baby. There might also be an NCT Waterbirth workshop in your area.
There might also be an NCT Waterbirth workshop in your area.
A Guide to Water Birth, 12-minute video.
References
Brocklehurst P, Hardy P, Hollowell J, Linsell L, Macfarlane A, McCourt C, Marlow N, Miller A, Newburn M, Petrou S, Puddicombe D, Redshaw M, Rowe R, Sandall J, Silverton L, Stewart M. (2011) Perinatal and maternal outcomes by planned place of birth for healthy women with low risk pregnancies: the Birthplace in England national prospective cohort study. BMJ.343:d7400. Available from: https://www.ncbi.nlm.nih.gov/pubmed/22117057 [Accessed: 13th November 2018]
Cluett ER, Burns E, Cuthbert A. (2018) Immersion in water in labour and birth. Cochrane Database Syst Rev. (5):CD000111. Available from: https://www.cochrane.org/CD000111/PREG_immersion-water-labour-and-birth [Accessed 13th November 2018]
CQC. (2018) 2017 Maternity survey: national tables for England. Available from: https://www.cqc.org.uk/publications/surveys/maternity-services-survey-2017 [Accessed 13th November 2018]
(2018) 2017 Maternity survey: national tables for England. Available from: https://www.cqc.org.uk/publications/surveys/maternity-services-survey-2017 [Accessed 13th November 2018]
Cumberledge J; Expert Maternity Group; Department of Health. (1993) Changing childbirth. Part 1, report of the expert maternity group, London, HMSO. [Accessed 13th November 2018]
Dekker R. (2018) The evidence on: waterbirth. Available from: http://evidencebasedbirth.com/waterbirth/ [Accessed 4th March 2019]
Garland D. (2000) Waterbirth: an Attitude to Care. 2nd edition. Oxford: Books for Midwives Press
Marshall A. (2019) High BMI waterbirth – time for trusts to take the plunge? AIMS Journal. 31(2). Available from: https://www.aims.org.uk/journal/item/waterbirth-high-bmi [Accessed 13th November 2018]
NICE. (2014) CG190 Intrapartum care. Available from: https://www.nice.org.uk/guidance/cg190/chapter/recommendations#timing-of-regional-analgesia [Accessed 13th November 2018]
Public Health England. (2014) Patient safety alert: Legionella and heated birthing pools filled in advance of labour in home settings. Available from: https://www.england.nhs.uk/wp-content/uploads/2014/06/psa-legionella-birth-pool.pdf [Accessed 4th March 2019]
(2014) Patient safety alert: Legionella and heated birthing pools filled in advance of labour in home settings. Available from: https://www.england.nhs.uk/wp-content/uploads/2014/06/psa-legionella-birth-pool.pdf [Accessed 4th March 2019]
RCM. (2018) RCM Midwifery blue top guidance No. 1, London, Royal College of Midwives. Available from: https://www.rcm.org.uk/media/2539/professionals-blue-top-guidance.pdf [Accessed 4th March 2019]
Ulfsdottir H, Saltvedt S, Georgsson S (2018) Waterbirth in Sweden – a comparative study. Acta Obstet Gynecol Scand. 97(3):341-348. Available from: https://www.ncbi.nlm.nih.gov/pubmed/29288489 [Accessed 13th November 2018]
Winterton N. (1992) Maternity Services: Second report of the House of Commons Health Committee (The Winterton Report), London, HMSO.
Further reading
Lewis L, Hauck YL, Crichton C, Barnes C, Poletti C, Overing H, Keyes L, Thomson B. (2018) The perceptions and experiences of women who achieved and did not achieve a waterbirth. BMC Pregnancy and Childbirth. 18(1):23. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5763519/ [Accessed 13th November 2018]
BMC Pregnancy and Childbirth. 18(1):23. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5763519/ [Accessed 13th November 2018]
Redshaw M, Henderson J. (2015) Safely delivered: a national survey of women’s experience of maternity care 2014, Oxford, NPEU. Available from: https://www.npeu.ox.ac.uk/downloads/files/reports/Safely%20delivered%20NMS%202014.pdf [Accessed 13th November 2018]
Water injections can relieve back pain during childbirth | News
Keywords / keywords: Obstetrics, Pain relief, Labor
About a third of women experience severe back pain during childbirth. Injection of a small volume of sterile water intradermally into the lumbar region has been used by some midwives for many years to relieve this pain, but the procedure has been controversial to date.
A new study from the University of Queensland has shown that the administration of sterile water can be a safe and effective way to reduce back pain during childbirth.
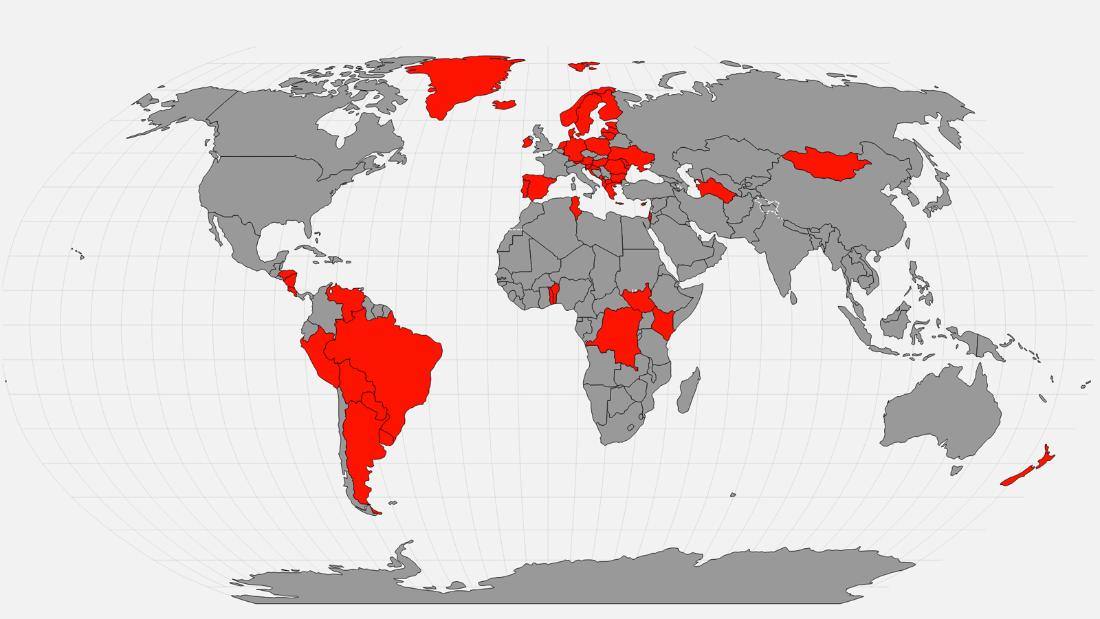
The researchers evaluated the analgesic effects of sterile water injections and their effect on birth outcomes. A multicentre, double-blind study was conducted between December 2012 and December 2017 in one UK and 15 Australian maternity hospitals.
Women who experienced severe back pain during childbirth were given injections of either sterile water or saline (placebo). A total of 1166 women were selected for the study, 580 of whom received injections of sterile water and 567 received placebo. The women in labor and the medical workers who performed the procedure were not aware that they were receiving and administering from the two solutions, respectively.
The primary outcome of the study was the caesarean section rate. The main secondary outcomes included a reduction in pain of at least 30% or 50% at 30, 60, and 90 minutes after injection, as assessed by women in labor.
The caesarean section rate was 17.1% (82 of 580 people) in the sterile water injection group and 14. 8% (82 of 567 people) in the placebo group (p = 0.293).
8% (82 of 567 people) in the placebo group (p = 0.293).
At 30 minutes post-treatment, 60.8% (330 of 543 women) in the sterile water injection group reported a 30% reduction in pain compared to 31.4% of the placebo group (163 of 520 women, p<0, 001).
Further, 43.3% (235 of 534 women) in the sterile water injection group reported a 50% reduction in pain compared to 18.1% of the placebo group (94 of 520 women, p<0.001).
The analgesic effect of sterile water, compared with placebo, remained significant also 90 minutes after injection.
There were no significant differences between groups of women in other maternal and newborn health outcomes.
The study was published in The Lancet EClinical Medicine.
Thus, compared with placebo, injections of sterile water did not reduce caesarean section rates, however, the intervention resulted in a significant increase in the number of women reporting at least 30% and 50% pain reduction within 90 minutes.
The researchers concluded that injections of sterile water into the lumbar region do not affect birth outcomes, although they may be effective in alleviating labor back pain.
However, more research is needed before the introduction of this method into clinical guidelines in Australia, the US and other countries.
In Russia, this method is also not included in the clinical guidelines and is not approved for reducing back pain during childbirth.
doi.org/10.1016/j.eclinm.2020.100447
field required field
mandatory
field required
SpecializationObstetrician-gynecologistAllergologistGastroenterologistHematologistHepatologistDermato-venereologistCardiologistNeurologistNeurosurgeonInfectionistOncologistOtolaryngologistOphthalmologistPediatricianPsychiatristPulmonologistProctologistRheumatologistRadiologist and RadiologistTherapist and General PractitionerUrologistPhthisiatricianSurgeonEndocrinologistOther 9002 field mandatory
By clicking on the Subscribe button, you consent to the processing of personal data
- Premium
- Allergology
- Bronchopulmonology
- Vaccination
- Gastroenterology
- Hepatology
- Gynecology
- Dermatovenereology
- Immunology
- infections
- Cardiology
- ENT pathology
- Medical equipment
- Urgent care
- Nutriciology
- Oncology
- Pediatrics
- Psychoneurology
- Rheumatology
- seasonal allergies
- Therapy
- Uronephrology
- Pharmacology
- Endocrinology
- IT in healthcare
Buy Subscribe Number archive
-
19
OctScientific-practical conference "Interdisciplinary approach to the treatment of patients with diabetes mellitus" end date: 19 October 2022 Venue: Moscow, st.
 New Arbat, 36, building of the Government of Moscow
New Arbat, 36, building of the Government of Moscow -
19
OctWebinar FGBOU DPO RMANPO “Autism Spectrum Disorders. Approaches to therapy, comorbid conditions» end date: 19 October 2022 Venue: Online
-
20
OctAll-Russian scientific-practical conference "Surgery in modern times" end date: 21 October 2022 Venue: Vladikavkaz, st. Pushkinskaya, 40, North Ossetian State Medical Academy of the Ministry of Health and Social Development of the Russian Federation
-
20
OctIII Online Cancer Marathon "Online Autumn - 2022" end date: 21 October 2022 Venue: Online
-
20
OctCongress “Seasons.
 Women's health - from young to silver and golden age " end date: 21 October 2022 Venue: Online on the educational medical portal MEDTOUCH.ORG
Women's health - from young to silver and golden age " end date: 21 October 2022 Venue: Online on the educational medical portal MEDTOUCH.ORG
Why the memory of the pain we experienced does not leave us
- Claudia Hammond
- BBC Future
will help you understand the events.
Image copyright Thinkstock
If people weren't able to forget the pain they once experienced, women would never decide to have a second child. At least that's what the popular myth says. However, in reality, as the correspondent found out BBC Future , painful memories don't always fade.
Talk to any woman who has just given birth to a child, and she will almost certainly say, describing the pain experienced during childbirth: "Again? Never in my life!" A friend of mine begged me to dissuade her from such a step if she even hinted at a second child in the future. And what? It's only been a few years, and here you are: it's time for her to give birth...
And what? It's only been a few years, and here you are: it's time for her to give birth...
The usual explanation is that women simply forget the pain they experienced during childbirth, as the brain edits memories. From an evolutionary point of view, it would be wise to forget the pain of childbearing if the memory of it would hold back the desire of people to reproduce. Unfortunately, things are not so simple.
With regard to childbirth in particular, a review of studies up to 2000 suggests that women do not completely forget the pain of labor pains, nor the intensity of the pain they experienced. However, this is a difficult topic to study. There is a scale that allows people to assess the severity of pain, but since labor can last for many hours, it is not very clear at what stage of contractions or labor itself the study participants concentrated their attention. Even the pain of each uterine contraction can vary in severity, so assessing the pain experienced during the entire process is unlikely to ever be an easy task.
(Similar articles in the Journal section)
However, there are some things that can be done, such as examining whether a particular woman's memories of pain have changed over time. Swedish experts conducted a survey of 2428 women and compared their memories of pain experienced two months and one year after childbirth.
The data obtained showed that most women do not forget their feelings: memories of the experience of childbirth in 60% of women remained the same, both after two and after 12 months. In fact, only a third of mothers at 12 months had forgotten how painful it was for them to remember childbirth two months after birth. With 18% of the women surveyed, something exactly the opposite happened - they not only did not forget the intensity of the pain experienced, but, on the contrary, in their memory, childbirth became more painful 12 months later.
Rewrite the past
Skip the Podcast and continue reading.
Podcast
What was that?
We quickly, simply and clearly explain what happened, why it's important and what's next.
episodes
The End of the Story Podcast
Five years have passed and the scientists again surveyed the same group of women. By this time, indeed, the memory of pain in some of them had become dull. About half said the pain was less severe than they thought two months after giving birth. However, those who most negatively assessed the experienced experience of childbirth two months after the event, memories of pain did not leave. However, this is not necessarily a bad thing. In the course of some studies, it turned out that women who remember the pain experienced during childbirth perceive this event as their own achievement that remains with them forever. "If I can handle the pain during contractions, I can handle anything. "
"
At the same time, the very fact that the memory of pain does not change over time may be surprising. As the results of several decades of psychological research show, whenever we remember something, we reconstruct the events of the past in a slightly different way.
Image copyright, Thinkstock
Image caption,The pain experienced by a woman during childbirth is hard to measure
Our memory is not a collection of digital discs of videotapes that will play back the events of the past every time we see them exactly as they were in reality. Instead, the context of the original memory is changed. We talk about this or that event, each time reproducing it from memory in a slightly different way than before.
The pain of childbirth has a purpose. If the birth went well, this positive outcome in itself should dull the memory of suffering. But something else is also clear: for some mothers, even the happy event of having a baby does not alleviate the painful memories of the childbearing process.
So, if the intensity of this kind of "positive" pain is not necessarily forgotten, what about negative experiences?
Sometimes it is important that we experience pain and remember what caused it. Such a memory ensures our safety and avoids the repetition of painful troubles. If you cut yourself painfully while opening a tin, you'll be more careful the next time you cook dinner. Or if, like me, you decide to test whether the metal rim around the hearth really gets very hot, and touch it with four fingers, you probably won't repeat this experiment. Alas, I was 30 years old, not five. Not surprisingly, people who suffer from disorders that prevent them from feeling pain often get burned or otherwise injure themselves. So forget about the pain is not necessary.
It can still be useful to forget about pain, although chronic pain is often associated with diseases such as diabetes. The key to regulating this kind of pain and getting rid of it at the molecular level is provided by some new discoveries.
Even when you just walk through the gate where you once cut your leg, or open the door where you once pinched your finger, you will close your eyes at the memory of these incidents. In 2006, researchers at the Arizona State University College of Medicine made the claim that this was due to the function of the PKM-zeta (PKM-ζ) molecule. This molecule (also called the memory molecule in the popular science literature) strengthens the connections between neurons in the brain when we learn something new. It also creates physical sensitivity after experienced pain.
Image copyright Thinkstock
Image captionEven if memories of pain can be erased, what will it do?
Experiments on mice have shown that if you block a certain molecule in the spine of experimental animals, you can thereby erase their additional susceptibility to pain. However, later other scientists called the results of the described experiment into question and proved that mice born with the PCM-zeta molecule could still feel pain.
What about uncomfortable or traumatic pain associated with certain medical procedures? For example, when colonoscopy (bowel probing) is performed using conscious sedation, patients are sometimes given a drug called medazolam, which reduces the urge to defecate and contributes to the inability to form memories after the onset of the disease. Patients may wince or writhe in discomfort during this procedure, but it is hoped that at the end of the colonoscopy they will not feel pain and discomfort.
Underlying sensations
Some people question the ethics of this approach, as well as its consequences. In an article published last year, Andrew Davidson, an anesthetist at the Royal Victorian Children's Hospital in Australia, warns that while drugs like midazolam make it harder to form conscious memories, they can't affect implicit, unconscious memories. These memories affect us, although we cannot consciously recall them. Just like we automatically button up our shirts or arrive at the bus stop in a familiar way, without thinking about when and how we formed the memories of these actions.