Very swollen feet
Swollen ankles, feet and legs (oedema)
Swelling in the ankles, feet or legs often goes away on its own. See a GP if it does not get better in a few days.
Common causes of swollen ankles, feet and legs
Swelling in the ankles, feet and legs is often caused by a build-up of fluid in these areas, called oedema.
Oedema is usually caused by:
- standing or sitting in the same position for too long
- eating too much salty food
- being overweight
- being pregnant
- taking certain medicines – such as some blood pressure medicines, contraceptive pills, hormone therapy, antidepressants or steroids
Oedema can also be caused by:
- an injury – such as a strain or sprain
- an insect bite or sting
- problems with your kidneys, liver or heart
- a blood clot
- an infection
Information:
Find out more about swollen ankles, feet and fingers in pregnancy
Check if you have oedema
Symptoms of oedema include:
Swollen or puffy ankles, feet or legs.Credit:
CaptureIt / Alamy Stock Photo https://www.alamy.com/stock-photo-swollen-puffy-feet-toes-and-ankles-of-adult-female-woman-after-an-16909905.html?pv=1&stamp=2&imageid=BDF21AF8-3C21-44B4-996A-B05115785B6B&p=61997&n=0&orientation=0&pn=1&searchtype=0&IsFromSearch=1&srch=foo%3Dbar%26st%3D0%26sortby%3D2%26qt%3DAXT1NP%26qt_raw%3DAXT1NP%26qn%3D%26lic%3D3%26edrf%3D1%26mr%3D0%26pr%3D0%26aoa%3D1%26creative%3D%26videos%3D%26nu%3D%26ccc%3D%26bespoke%3D%26apalib%3D%26ag%3D0%26hc%3D0%26et%3D0x000000000000000000000%26vp%3D0%26loc%3D0%26ot%3D0%26imgt%3D0%26dtfr%3D%26dtto%3D%26size%3D0xFF%26blackwhite%3D%26cutout%3D%26archive%3D1%26name%3D%26groupid%3D%26pseudoid%3D32846%26userid%3D%26id%3D%26a%3D%26xstx%3D0%26cbstore%3D1%26resultview%3DsortbyPopular%26lightbox%3D%26gname%3D%26gtype%3D%26apalic%3D%26tbar%3D1%26pc%3D%26simid%3D%26cap%3D1%26customgeoip%3D%26vd%3D0%26cid%3D%26pe%3D%26so%3D%26lb%3D%26pl%3D0%26plno%3D%26fi%3D0%26langcode%3Den%26upl%3D0%26cufr%3D%26cuto%3D%26howler%3D%26cvrem%3D0%26cvtype%3D0%26cvloc%3D0%26cl%3D0%26upfr%3D%26upto%3D%26primcat%3D%26seccat%3D%26cvcategory%3D*%26restriction%3D%26random%3D%26ispremium%3D1%26flip%3D0%26contributorqt%3D%26plgalleryno%3D%26plpublic%3D0%26viewaspublic%3D0%26isplcurate%3D0%26imageurl%3D%26saveQry%3D%26editorial%3D1%26t%3D0%26edoptin%3D
Shiny or stretched skin.
Credit:
SCIENCE PHOTO LIBRARY https://www.sciencephoto.com/media/260060/view
Changes in skin colour, discomfort, stiffness and dents when you press on the skin.How to ease swelling yourself
Swelling in your ankles, feet or legs should go away on its own, but there are some things you can try to help.
Do
-
raise your legs or the swollen area on a chair or pillows when you can
-
get some gentle exercise, like walking, to improve your blood flow
-
wear wide, comfortable shoes with a low heel and soft sole
-
wash, dry and moisturise your feet to avoid infections
Non-urgent advice: See a GP if:
1 or both of your ankles, foot or legs are swollen and:
- it has not improved after treating it at home for a few days
- it gets worse
Urgent advice: Ask for an urgent GP appointment or get help from NHS 111 if:
- you have swelling in 1 ankle, foot or leg and there's no obvious cause, such as an injury
- the swelling is severe, painful or starts very suddenly
- the swollen area is red or feels hot to the touch
- your temperature is very high, or you feel hot and shivery
- you have diabetes and your feet, ankles or legs are swollen
You can call 111 or get help from 111 online.
Immediate action required: Call 999 if:
- you feel short of breath or are struggling to breathe
- your chest feels tight, heavy or painful
- you're coughing up blood
You could have a blood clot in your lungs, which needs immediate treatment in hospital.
Treatment for swelling and oedema
Treatment for swelling or oedema that does not go away on its own will depend on the cause. Your GP can help you with the right treatment.
Speak to your GP about making, lifestyle changes, such as losing weight or going on a low-salt diet.
Page last reviewed: 18 January 2022
Next review due: 18 January 2025
Chronic Venous Insufficiency: Symptoms, Causes, Diagnosis, Treatment
Written by Teresa Dumain
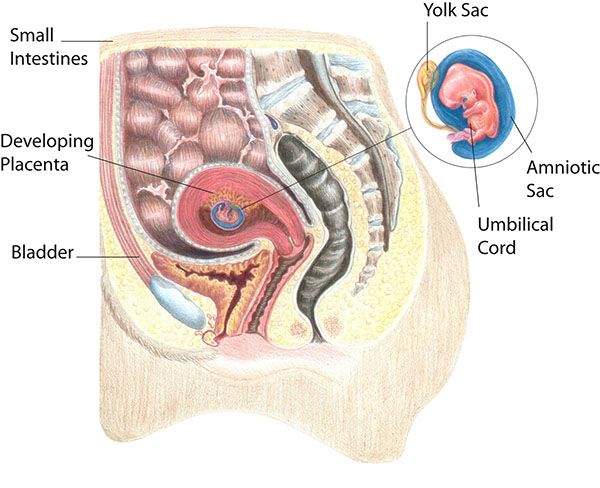
The veins in your legs carry blood back to your heart. They have one-way valves that keep blood from flowing backward. If you have chronic venous insufficiency (CVI), the valves don’t work like they should and some of the blood may go back down into your legs. That causes blood to pool or collect in the veins.
They have one-way valves that keep blood from flowing backward. If you have chronic venous insufficiency (CVI), the valves don’t work like they should and some of the blood may go back down into your legs. That causes blood to pool or collect in the veins.
Over time, CVI can cause pain, swelling, and skin changes in your legs. It may also lead to open sores called ulcers on your legs.
Causes
A blood clot in a deep vein in your leg (called deep vein thrombosis) can damage a valve. If you don’t exercise, that can cause CVI, too. So can sitting or standing for long stretches of time. That raises pressure in your veins and may weaken the valves.
Women are more likely than men to get CVI. Your chances also might be higher if you are:
- Obese
- Over age 50
- Pregnant or have been pregnant more than once
- From a family with a history of CVI
- Someone with history of blood clots
- A smoker
Symptoms
You may notice these in your legs:
- Swelling or heaviness, especially in the lower leg and ankle
- Pain
- Itchiness
- Varicose veins (twisted, enlarged veins close to the surface of the skin)
- Skin that looks like leather
Without treatment, the pressure and swelling will burst the tiny blood vessels in your legs called capillaries. That could turn your skin reddish-brown, especially near the ankles. This can lead to swelling and ulcers. These ulcers are tough to heal. They are also more likely to get infected, which can cause more problems.
That could turn your skin reddish-brown, especially near the ankles. This can lead to swelling and ulcers. These ulcers are tough to heal. They are also more likely to get infected, which can cause more problems.
If you have any of the symptoms of CVI, talk to your doctor. The sooner you treat it, the less likely you’ll get ulcers.
Diagnosis
Your doctor will take your medical history. They then will check the blood flow in your legs with a test called a vascular or duplex ultrasound. Your doctor will place a small device on your skin over the vein. Using sound waves, they can see the blood vessel and check how quickly and in what direction the blood flows.
Sometimes, you may need X-rays or specific scans to check for other causes of your leg swelling.
Treatment
The main goal is to stop swelling and prevent leg ulcers. Your doctor may suggest a combination of treatments based on your age, symptoms, and other things. Some options to help manage CVI include:
Lifestyle Changes
You can help blood flow better in your leg veins. Steps include:
Steps include:
Compression stockings. These elastic socks put pressure on your legs to help blood move. They come in different tightnesses, lengths, and styles. Your doctor can suggest which might work best for you.
Movement. Try not to sit or stand for a long time. If you have to sit for a while, stretch or wiggle your legs, feet, and ankles often to help your blood flow. If you stand a lot, take breaks to sit and put your feet up. This helps lower pressure in your leg veins.
Exercise. Working out helps pump your blood, too. Walking is a good, simple way to make your legs stronger and boost blood flow.
Medications
Your doctor may prescribe an antibiotic to treat infections or leg ulcers. Sometimes, they’ll give you medicine to help prevent blood clots.
Medical Procedures
If your CVI is further along, you may need a nonsurgical treatment.
Sclerotherapy. Your doctor will inject a solution into the problem vein. It scars the vein, forcing blood to flow through healthier veins. Over time, your body absorbs the scarred vein.
It scars the vein, forcing blood to flow through healthier veins. Over time, your body absorbs the scarred vein.
Endovenous thermal ablation. This newer method uses high-frequency radio waves or a laser to heat and close the problem vein.
Surgery
Fewer than 1 in 10 people need surgery for CVI.
Here are your options:
Ligation. The vein is cut and tied off so blood can’t flow through. Your doctor may also remove a vein that is very damaged. You usually will go home on the same day.
Microincision/ambulatory phlebectomy. This technique uses much smaller incisions, punctures and small hooks to remove damaged veins.
Vein repair. Your doctor fixes the vein or the valves. This can be done through an open cut on your leg or through a smaller opening by using a long, hollow catheter or tube.
Vein transplant. Your doctor replaces the problem vein with a healthy one from somewhere else in your body.
Vein bypass. This is done on veins in the upper thigh and only in the most severe cases. Your doctor takes part of a healthy vein from another part of your body. They’ll use that to reroute blood around the affected vein. You’ll usually stay in the hospital for 2-5 days.
Swelling of the legs - the reasons why the legs swell
- Home
- Useful information
Only 10% of patients need a more intensive examination, including laboratory and imaging methods. Understanding the mechanism of edema development allows the doctor not only to make a correct diagnosis, but also to prescribe the correct treatment.
Treatment of chronic edema of the lower extremities pursues not so much cosmetic problems as ensuring the normal functioning of the skin and soft tissues.
 The fact is that oxygen and other nutrients enter the skin by penetrating through the vascular wall and further to the skin itself. In conditions of edema, this mechanism does not work. A decrease in metabolic processes leads to starvation of the skin, accumulation of metabolic products in them, deterioration of the barrier function of the skin and a decrease in its regenerative abilities.
The fact is that oxygen and other nutrients enter the skin by penetrating through the vascular wall and further to the skin itself. In conditions of edema, this mechanism does not work. A decrease in metabolic processes leads to starvation of the skin, accumulation of metabolic products in them, deterioration of the barrier function of the skin and a decrease in its regenerative abilities. Clinically, this is manifested by a violation of the color of the skin, it acquires a bluish tint, and also becomes more dense. In addition, the protein-rich edematous fluid serves as a good breeding ground for a variety of microorganisms that cause inflammation. Thus, this is a serious motivation to start treatment.
Causes of leg swelling
It is extremely difficult to single out any root cause. Basically, swelling of the legs occurs:
Leg edemaassociated with varicose veins can be on one or both legs. If varicose veins progress on one leg, the edema is usually asymmetric.
 Varicose edema is localized in the lower leg (below the knee). The foot usually does not swell. A typical sign of varicose edema is that it goes away or decreases significantly after a night's rest. With prolonged squeezing of the skin with a finger in the shin area (below the knee), characteristic dimples remain. Complaints can range from a simple feeling of heaviness from swelling to a feeling of dull arching pain. On examination, you can detect other manifestations of varicose veins: varicose veins and skin changes in the form of cyanosis, induration, etc.
Varicose edema is localized in the lower leg (below the knee). The foot usually does not swell. A typical sign of varicose edema is that it goes away or decreases significantly after a night's rest. With prolonged squeezing of the skin with a finger in the shin area (below the knee), characteristic dimples remain. Complaints can range from a simple feeling of heaviness from swelling to a feeling of dull arching pain. On examination, you can detect other manifestations of varicose veins: varicose veins and skin changes in the form of cyanosis, induration, etc. Lymphedema (Lymphostasis), in contrast to the pathology of the veins, is manifested by swelling of the foot and fingers. Edema of the rear of the foot is compared with a "pillow", and fingers - with "sausages". Lymphedema after a night's rest usually does not decrease. In the initial stages of the disease, pits remain on the skin of the lower leg from being squeezed by the fingers. Subsequently, as a result of the development of compaction of the skin, the soft tissues of the lower leg become dense like a shell.
 With lymphedema, it is not possible to fold the skin on the back of the foot (back of the sole). Complaints are usually absent. Sometimes patients feel a feeling of heaviness in the calves. Lymphedema, more often, affects one lower limb.
With lymphedema, it is not possible to fold the skin on the back of the foot (back of the sole). Complaints are usually absent. Sometimes patients feel a feeling of heaviness in the calves. Lymphedema, more often, affects one lower limb. Diseases of the heart, kidneys, liver, endocrine system and long-term hormonal therapy cause systemic (central) edema that appears on both lower extremities and is localized on the lower leg. The edema is symmetrical and does not involve the rear of the foot and toes. When squeezing with a finger, pits that do not pass for a long time remain. Complaints of patients are associated with the underlying disease. Unpleasant sensations in the legs are minimal or completely absent.
Positional (hypodynamic, orthostatic) edema is difficult to distinguish from systemic. The main differential diagnostic sign in such cases is the limited mobility of patients. Positional leg edema often occurs in patients confined to wheelchairs. Externally, such edema aligns the conical profile of the lower leg and makes it look like a cylinder.
 There are no complaints from patients.
There are no complaints from patients. Edema of the legs associated with the use of pharmacological drugs is always bilateral and symmetrical. The intensity of swelling may decrease after a night's rest or lifting of the limbs, and as a rule, such swelling disappears quickly after discontinuation of drugs. Complaints are absent or minimal.
Also, an increase in the volume of the lower extremities may not be associated with edema, but with a non-standard distribution of adipose tissue. This condition is called lipedema.
Lipedema is inherited and appears already in adolescence. Such legs are often compared to the "trunk of a tree", noting the abnormally large thickness of the ankles. Feet remain completely normal. Night rest, prolonged compression and diuretic intake have no effect. The skin and subcutaneous tissue in lipedema, in contrast to true edema, have a loose texture. Complaints are minimal, sometimes patients note an increased sensitivity of the skin to touch.

Principles of treatment of venous and lymphatic edema
Of course, due to the variety of causes for the development of edema, there are a large number of treatment methods, but we will try to highlight the main directions. So, if the legs swell, it is necessary:
- Compression knitwear (allows you to act on swelling from the outside and help reduce it)
- Appointment of drugs that improve venous tone (due to increased tone of the veins, the outflow of fluid from the legs is faster).
- Changes in lifestyle and diet are important.
- Correction of the fluid level in the body (restriction of salt intake, intake of diuretics, etc.).
- Various physiotherapy procedures (lymphopress, lymphatic drainage massage, magnetotherapy, etc.)
4 photos
1 / 4
The results of our patients
Share
Back
Swelling of the legs - the reasons why the right or left leg, calves swell, swell, what should I do?
A fairly common symptom that occurs due to the accumulation of a large amount of fluid in the intercellular space of the tissues of the lower extremities.

Patients often come to our clinic with complaints of swelling of the lower extremities. It is not always a symptom of varicose veins. Consider the causes of its occurrence, as well as tests that will help identify lymphatic edema.
Causes and types of edema of the lower extremities
Edema is a symptom that may be associated with deep vein thrombosis or thrombophlebitis. There is chronic edema on the background of varicose veins, when we see that the veins in the legs are dilated and there is swelling of the legs, which manifests itself at the end of the day.
Edema of the legs is of two types: symmetrical - swelling of two limbs and asymmetric. The second occurs on one limb and is often accompanied by acute pain, may be associated with venous disease. It is caused by either deep vein thrombosis or thrombophlebitis. In advanced cases, chronic edema occurs against the background of varicose veins, when we see altered varicose veins and edema, which can appear as traces of a sock gum by the end of the day.
The main causes of swelling of the legs include:
- diseases of the veins of the lower extremities
- severe physical exertion;
- ➡️ prolonged standing or sitting position;
- ➡️ kidney disease;
- ➡️ hormonal fluctuations in women ;
- ➡️ diseases of the joints;
- ➡️ purulent processes;
- ➡️ thyroid dysfunction;
- ➡️ traumatic injuries;
- ➡️ heart problems.
Edema may occur regularly or periodically, accompanied by heaviness in the legs, fever of the whole body or the affected area. At the first symptoms, you should consult a doctor.
Lymphedema and tests to detect it
Lymphedema is characterized by persistent lymphatic swelling of the soft tissues of the affected area and most often occurs towards the end of the day. It is primary and secondary. There are several tests that will help identify such a disease:
- Measuring the circumference of the ankles before bedtime and in the morning.
 If the circumference changes, becomes larger in the evening, and disappears in the morning - this is the first signal for the development of lymphedema. If at the same time there are no visible varicose veins and the edema manifests itself symmetrically, then the lymphologist will deal with the problem.
If the circumference changes, becomes larger in the evening, and disappears in the morning - this is the first signal for the development of lymphedema. If at the same time there are no visible varicose veins and the edema manifests itself symmetrically, then the lymphologist will deal with the problem. - The second test - you need to examine the lower and upper limbs to detect local swelling of the ankle and wrist joints. The test is done in the morning and before bed. If the swelling does not subside overnight, then the disease is progressing.
- Finger pressure along the course is larger than the tibia. If the hole does not remain, and the leg is enlarged, then the leg is very swollen, lymphedema develops. If the fossa remains and does not pass for some time, then this is a cardiological edema, which is associated with poor functioning of the heart muscle.
It is recommended to keep a diary and write down the circumference of the right and left ankle at different times, as well as the circumstances in which the swelling occurred, such as hot weather.
 This will help to identify under what circumstances edema appeared and what it is connected with. The reason for the development of lymphedema can be a constant static load when a person is in a state of sitting or standing. At the slightest sign of the appearance of any edema, it is necessary to consult a phlebologist, lymphologist or therapist.
This will help to identify under what circumstances edema appeared and what it is connected with. The reason for the development of lymphedema can be a constant static load when a person is in a state of sitting or standing. At the slightest sign of the appearance of any edema, it is necessary to consult a phlebologist, lymphologist or therapist. IMPORTANT : Do not self-medicate.
We offer modern methods for diagnosing edema by the best specialists. The clinic uses high-tech equipment, we can perform laboratory tests, which allows us to form an optimal treatment plan.
Causes of swelling of the legs
Individual approach
Modern clinics
Experienced specialists
Operations without incisions
Before starting any procedure, it is necessary to consult a phlebologist
Initial consultation of a phlebologist surgeon + Ultrasound vein protocol + Treatment plan 1500 ₽
The clinic administrator will call you back within 15 minutes to agree on the date and time of the appointment, as well as learn more about your problem
By clicking on the button, you agree to the Policy privacy policy
FAQ
➡️ Is it possible to completely get rid of varicose veins?
The disease is chronic.
 Various methods and preparations help to remove its symptoms, however, if the patient already has venous "knots", then the vascular wall has been irreversibly changed and nothing can change them. In this case, surgical treatment is prescribed. The best that can be achieved is to contain the further development of the disorder and avoid the occurrence of complications (trophic ulcers, conditions that can lead to disability and even death). Today, such methods have become popular: sclerotherapy, laser, physiotherapy, hirudotherapy, drug treatment.
Various methods and preparations help to remove its symptoms, however, if the patient already has venous "knots", then the vascular wall has been irreversibly changed and nothing can change them. In this case, surgical treatment is prescribed. The best that can be achieved is to contain the further development of the disorder and avoid the occurrence of complications (trophic ulcers, conditions that can lead to disability and even death). Today, such methods have become popular: sclerotherapy, laser, physiotherapy, hirudotherapy, drug treatment. ➡️ What threatens varicose veins?
Varicose veins can lead to a number of complications and other diseases. Telangiectasia - swelling, burning, nocturnal cramps and loss of sensation. Thrombophlebitis is an acute inflammation of the walls of blood vessels, which can cause a violation of the structure of the blood and the speed of its circulation. Clots turn into solid blood clots, which can break away from the vessels and clog the lumen of the vein.