Urine bacteria in pregnancy
Pregnancy and birth: What are the benefits of routinely screening for bacteria in the urine of pregnant women? - InformedHealth.org
Created: December 16, 2015; Last Update: March 22, 2018; Next update: 2021.
It’s not clear whether it’s a good idea to routinely screen for bacteria in the urine of pregnant women (bacteriuria screening). It’s also not possible to say whether antibiotics should be used if high levels of bacteria are detected in the urine but there are no noticeable urinary tract problems.
Routine screening tests are carried out during pregnancy to see whether the baby is developing normally and the mother is healthy. Screening tests in pregnancy include ultrasound scans and blood tests, as well as urine tests. In Germany, special guidelines (“Mutterschafts-Richtlinien”) specify what is to be tested in pregnancy, and what sorts of tests are used.
Urine tests during pregnancy
These guidelines specify that pregnant women should have routine urine tests. The urine is tested for proteins, sugar and bacteria. Routine testing for bacteria is also referred to as bacteriuria screening. If high levels of bacteria are detected in the urine, additional testing is done to confirm the results.
Laboratory results show that about 2 to 15 out of 100 pregnant women have above-average levels of bacteria in their urine, but the bacteria aren’t causing any symptoms. This is called “asymptomatic bacteriuria.”
Urinary tract infections and possible consequences
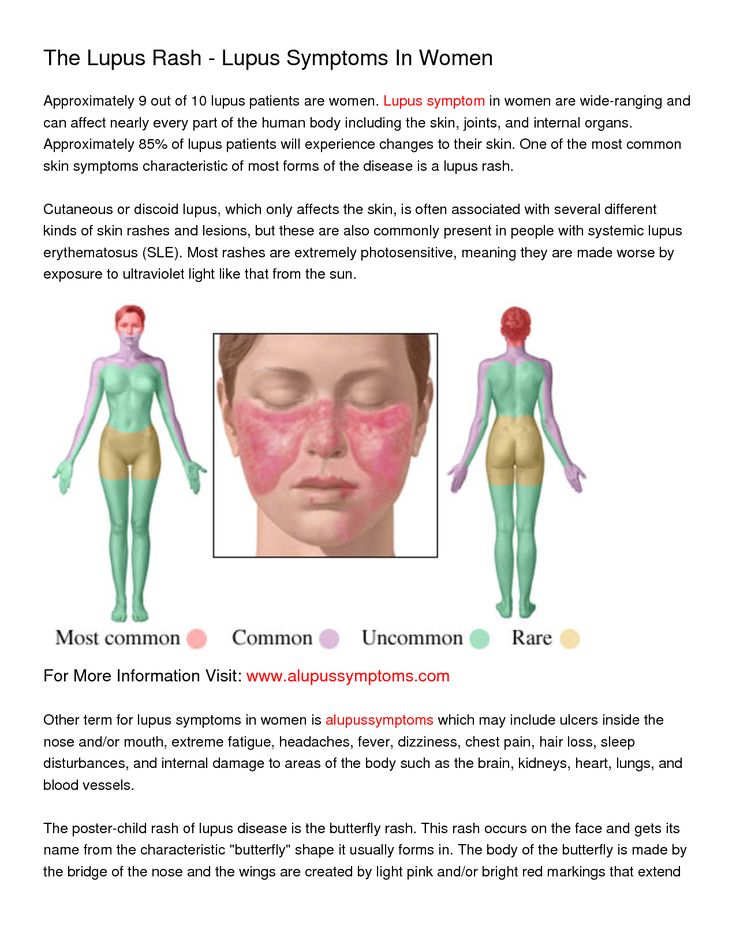
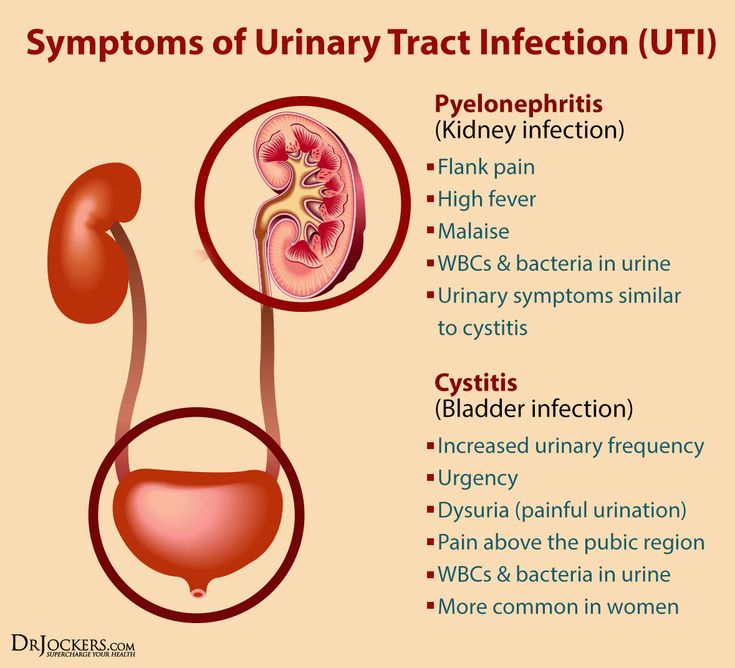
Having bacteria in your urine doesn’t often cause any problems. The bacteria usually just go away after a while. But women who have bacteria in their urine might go on to develop a urinary tract infection (UTI) such as cystitis.
Hormonal and physical changes make pregnant women more susceptible to urinary tract infections. These arise if bacteria infect the urethra (the tube that urine flows out of) and bladder. If the germs move upwards, they may also infect the ureters or kidneys.
Typical signs of a lower urinary tract infection include the following:
The following symptoms may also appear if the ureters or the renal pelvis are infected:
Fever
Pain around the kidneys (flank pain)
In some cases, nausea and vomiting
If you have at least one of these symptoms, it is important to see your doctor.
In rare cases, untreated urinary tract infections during pregnancy may lead to serious problems such as septicemia (blood poisoning). The presence of bacteria in urine is also associated with a higher risk of premature birth and low birth weight.
Pregnant women who have bacteria in their urine are usually given antibiotics to prevent possible complications – even if they don’t have any symptoms.
Research in this area
Researchers from the Institute for Quality and Efficiency in Health Care (IQWiG, Germany) wanted to find out whether routine testing for bacteria in urine during pregnancy actually has any benefits for the mother or the child. But the IQWiG researchers didn’t find any suitable studies on the benefits of these tests. So instead, they looked into the advantages and disadvantages of antibiotics in the treatment of asymptomatic bacteriuria: Do the antibiotics help to prevent complications in the mother and child if bacteria are found in urine but there are no symptoms of a urinary tract infection? They found three suitable studies on this topic. The women who participated in the studies either took antibiotics, a placebo medication (fake treatment) or didn’t have any treatment.
But the IQWiG researchers didn’t find any suitable studies on the benefits of these tests. So instead, they looked into the advantages and disadvantages of antibiotics in the treatment of asymptomatic bacteriuria: Do the antibiotics help to prevent complications in the mother and child if bacteria are found in urine but there are no symptoms of a urinary tract infection? They found three suitable studies on this topic. The women who participated in the studies either took antibiotics, a placebo medication (fake treatment) or didn’t have any treatment.
Not clear whether testing for bacteria in urine during pregnancy has benefits
But the researchers weren’t able to draw any conclusions about whether taking antibiotics to treat asymptomatic bacteriuria has any advantages or disadvantages. The studies didn’t provide important information about the study participants and the possible side effects of the antibiotics. Also, the medicines used in the studies are no longer used nowadays. The studies were done in the 1960s, and their results can’t be directly applied to the current health care situation for pregnant women.
The studies were done in the 1960s, and their results can’t be directly applied to the current health care situation for pregnant women.
So it’s still not clear whether it makes sense to routinely screen for bacteria in urine during pregnancy. It’s also not clear whether pregnant women should take antibiotics if bacteria are found in their urine but they don’t have any symptoms.
Sources
Institute for Quality and Efficiency in Health Care (IQWiG, Germany). Screening for asymptomatic bacteriuria within the framework of the German maternity guidelines, under special consideration of test methods: Final report; Commission S13-02. February 19, 2015 (IQWiG reports; Volume 279).
IQWiG health information is written with the aim of helping people understand the advantages and disadvantages of the main treatment options and health care services.
Because IQWiG is a German institute, some of the information provided here is specific to the German health care system.
 The suitability of any of the described options in an individual case can be determined by talking to a doctor. We do not offer individual consultations.
The suitability of any of the described options in an individual case can be determined by talking to a doctor. We do not offer individual consultations.Our information is based on the results of good-quality studies. It is written by a team of health care professionals, scientists and editors, and reviewed by external experts. You can find a detailed description of how our health information is produced and updated in our methods.
Urinary Tract Infection In Pregnancy - StatPearls
Patricia J. Habak; Robert P. Griggs, Jr.
Author Information and Affiliations
Last Update: July 5, 2022.
Continuing Education Activity
Urinary tract infections (UTIs) are frequently encountered in pregnant women. Pyelonephritis is the most common serious medical condition seen in pregnancy and may present similarly and may even result from inadequate treatment of urinary tract infections. Thus, it is crucial for providers to be able to distinguish normal versus abnormal findings of both the urinary tract and kidneys, evaluate abnormalities, and treat disease. Fortunately, urinary tract infections in pregnancy are usually easy to treat and respond well to treatment. This activity reviews the evaluation and management of urinary tract infection in pregnancy and highlights the role of interprofessional team members in collaborating to provide well-coordinated care and enhance outcomes for affected patients.
Fortunately, urinary tract infections in pregnancy are usually easy to treat and respond well to treatment. This activity reviews the evaluation and management of urinary tract infection in pregnancy and highlights the role of interprofessional team members in collaborating to provide well-coordinated care and enhance outcomes for affected patients.
Objectives:
Identify the etiology of urinary tract infections pregnancy.
Explain how to diagnose urinary tract infections in pregnant patients.
Summarize the treatment options available for urinary tract infections in pregnant patients.
Review interprofessional team strategies for improving care and outcomes in pregnant patients with urinary tract infections.
Access free multiple choice questions on this topic.
Introduction
Urinary tract infections (UTIs) are frequently encountered in pregnant women. Pyelonephritis is the most common serious medical condition seen in pregnancy.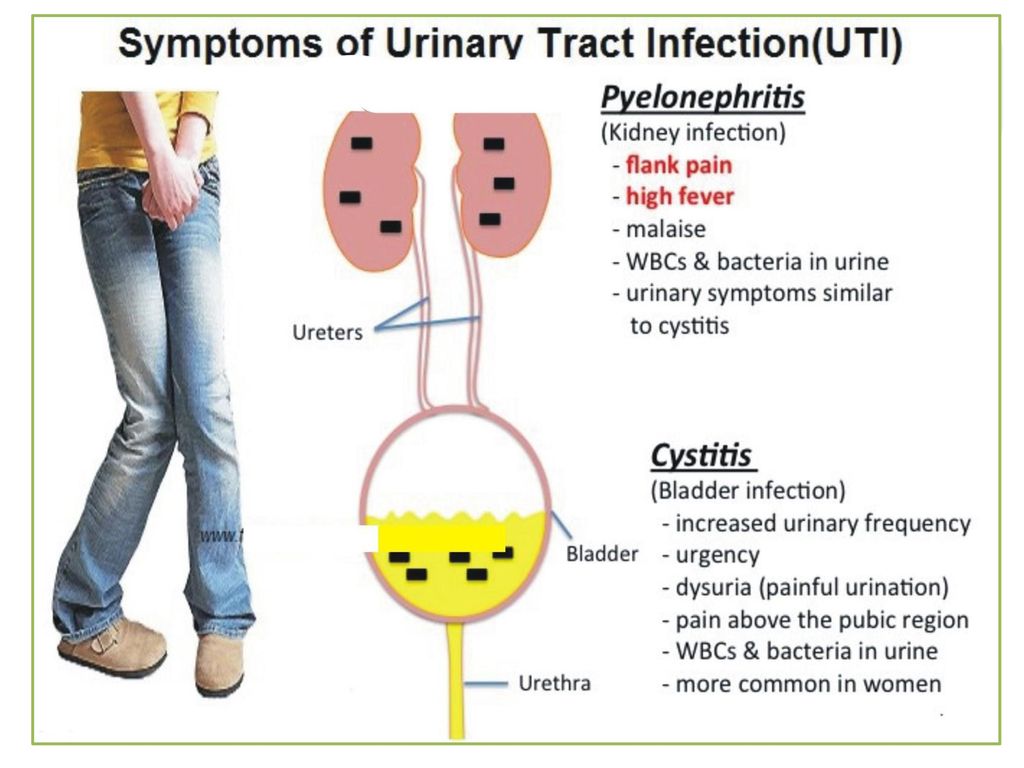 Thus, it is crucial for providers of obstetric care to be knowledgeable about normal findings of the urinary tract, evaluation of abnormalities, and treatment of disease. Fortunately, UTIs in pregnancy are most often easily treated with excellent outcomes. Rarely, pregnancies complicated by pyelonephritis will lead to significant maternal and fetal morbidity.
Thus, it is crucial for providers of obstetric care to be knowledgeable about normal findings of the urinary tract, evaluation of abnormalities, and treatment of disease. Fortunately, UTIs in pregnancy are most often easily treated with excellent outcomes. Rarely, pregnancies complicated by pyelonephritis will lead to significant maternal and fetal morbidity.
Changes of the urinary tract and immunologic changes of pregnancy predispose women to urinary tract infection. Physiologic changes of the urinary tract include dilation of the ureter and renal calyces; this occurs due to progesterone-related smooth muscle relaxation and ureteral compression from the gravid uterus. Ureteral dilation may be marked. Decreased bladder capacity commonly results in urinary frequency. Vesicoureteral reflux may be seen. These changes increase the risk of urinary tract infections.
Etiology
During pregnancy, urinary tract changes predispose women to infection. Ureteral dilation is seen due to compression of the ureters from the gravid uterus.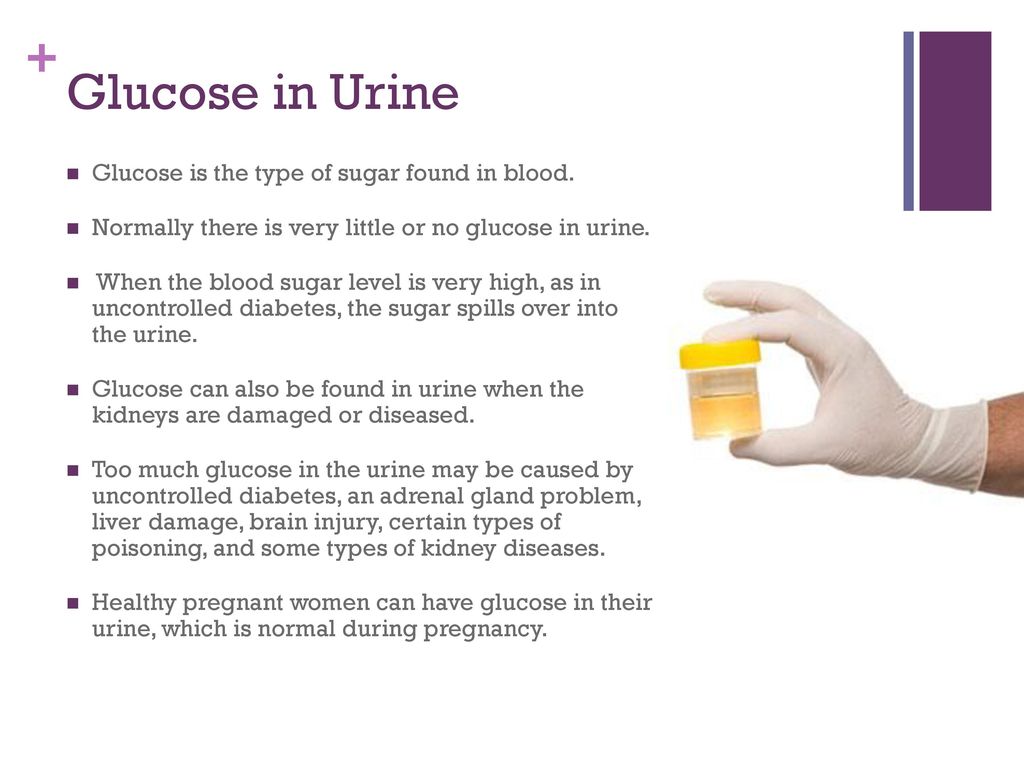 Hormonal effects of progesterone also may cause smooth muscle relaxation leading to dilation and urinary stasis, and vesicoureteral reflux increases. The organisms which cause UTI in pregnancy are the same uropathogens seen in non-pregnant individuals. As in non-pregnant patients, these uropathogens have proteins found on the cell-surface which enhance bacterial adhesion leading to increased virulence. Urinary catheterization, frequently performed during labor, may introduce bacteria leading to UTI. In the postpartum period, changes in bladder sensitivity and bladder overdistention may predispose to UTI.
Hormonal effects of progesterone also may cause smooth muscle relaxation leading to dilation and urinary stasis, and vesicoureteral reflux increases. The organisms which cause UTI in pregnancy are the same uropathogens seen in non-pregnant individuals. As in non-pregnant patients, these uropathogens have proteins found on the cell-surface which enhance bacterial adhesion leading to increased virulence. Urinary catheterization, frequently performed during labor, may introduce bacteria leading to UTI. In the postpartum period, changes in bladder sensitivity and bladder overdistention may predispose to UTI.
Pregnancy is a state of relative immunocompromise. This immunocompromise may be another cause for the increased frequency of UTIs seen in pregnancy.
Epidemiology
The most significant factor predisposing women to UTI in pregnancy is asymptomatic bacteriuria (ASB). ASB is defined as more than 100,000 organisms/mL on a clean catch urinalysis obtained from an asymptomatic patient. If asymptomatic bacteriuria is untreated in pregnancy, the rate of subsequent UTI is approximately 25%.[1] Due to both to the high rate and potential seriousness of pyelonephritis, it is recommended that all pregnant women be screened for ASB at the first prenatal visit. This is most often done with a clean catch urine culture. Treatment of ASB decreases the rate of clinical infection to 3% to 4%.
If asymptomatic bacteriuria is untreated in pregnancy, the rate of subsequent UTI is approximately 25%.[1] Due to both to the high rate and potential seriousness of pyelonephritis, it is recommended that all pregnant women be screened for ASB at the first prenatal visit. This is most often done with a clean catch urine culture. Treatment of ASB decreases the rate of clinical infection to 3% to 4%.
The rate of asymptomatic bacteriuria in non-pregnant women is 5% to 6% which compares similarly to estimated rates in pregnancy of 2% to 7%. ASB is seen more frequently in parous women and women of low socioeconomic status. Women who are carriers for sickle cell trait also have a higher incidence of ASB.[1]
UTIs are a common cause of serious infection in pregnant women. In one study, 3.5% of antepartum admissions were due to UTI.[2] Pyelonephritis is the most common cause of septic shock in pregnant women. Risk factors for UTIs in pregnancy include low socioeconomic status, young age, and nulliparity.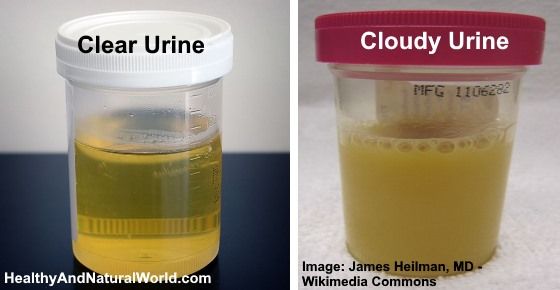 As with ASB some patients may be predisposed to infection and may report a history of having had ASB, cystitis or pyelonephritis in the past. Pyelonephritis is more often right-sided however may be bilateral in up to 25% of cases.
As with ASB some patients may be predisposed to infection and may report a history of having had ASB, cystitis or pyelonephritis in the past. Pyelonephritis is more often right-sided however may be bilateral in up to 25% of cases.
Pathophysiology
Organisms causing UTI in pregnancy are the same uropathogens which commonly cause UTI in non-pregnant patients. Escherichia coli is the most common organism isolated. An 18-year retrospective analysis found E. coli to be the causative agent in 82.5% of cases of pyelonephritis in pregnant patients.[3] Other bacteria which may be seen include Klebsiella pneumoniae, Staphylococcus, Streptococcus, Proteus, and Enterococcus species.
History and Physical
Patients with asymptomatic bacteriuria have no symptoms; thus, it is important to screen for the disease. These patients may have a history of frequent UTI or may have experienced ASB in a prior pregnancy.
Cystitis presents with the same symptoms seen in non-pregnant individuals.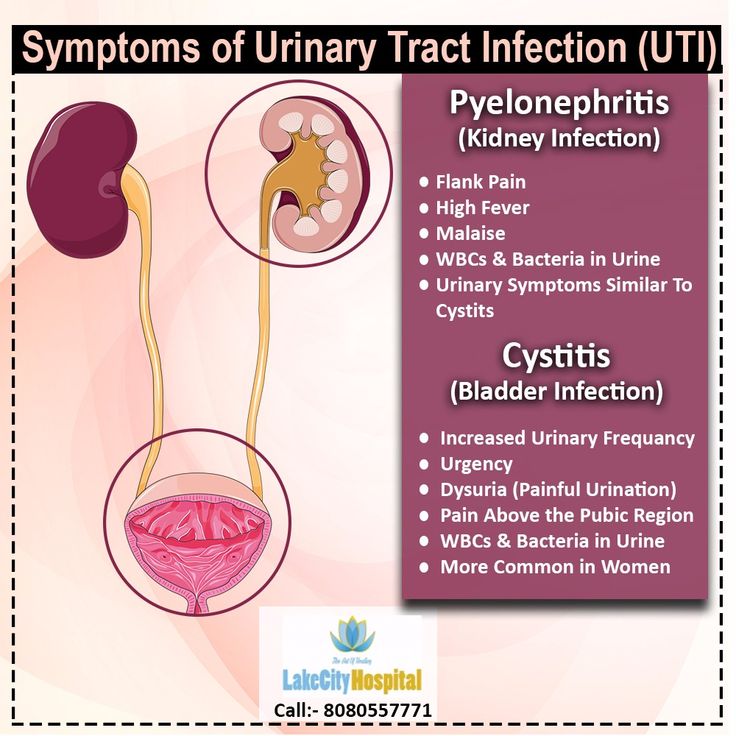 Symptoms may include pain or burning with urination (dysuria), urinary frequency or urinary urgency. Suprapubic pain and tenderness may be noted.
Symptoms may include pain or burning with urination (dysuria), urinary frequency or urinary urgency. Suprapubic pain and tenderness may be noted.
Likewise, patients with pyelonephritis exhibit symptoms seen in non-pregnant patients with the same disease. Symptoms may include flank pain, fever, and chills. Non-specific symptoms such as malaise, anorexia, nausea, and vomiting may be reported thus the differential diagnosis on initial presentation is often broad. Differential diagnosis includes acute intraabdominal processes such as appendicitis, cholecystitis, and pancreatitis as well as pregnancy complications including preterm labor and placental abruption. Patients may report contractions or contractions may be seen with uterine monitoring. This uterine activity often is due to smooth muscle irritability caused by infection. Patients should be assessed, and if cervical dilation is not found, treatment is typically not needed for preterm labor. Patients should be monitored closely however as preterm labor may develop.
Signs and symptoms of sepsis may be present. These include tachycardia and hypotension. Such patients require prompt evaluation and interventions.
A full physical examination should be performed with special attention to vital signs and exam of the heart and lungs. An abdominal exam may reveal tenderness, and costovertebral tenderness is usually able to be elicited. A genitourinary (GU) exam should be performed to assess for cervical infection and assess cervical dilation on admission. Even when pregnancy complications are not a concern initially, it is still reasonable to evaluate if contractions or other abnormalities occur during hospitalization.
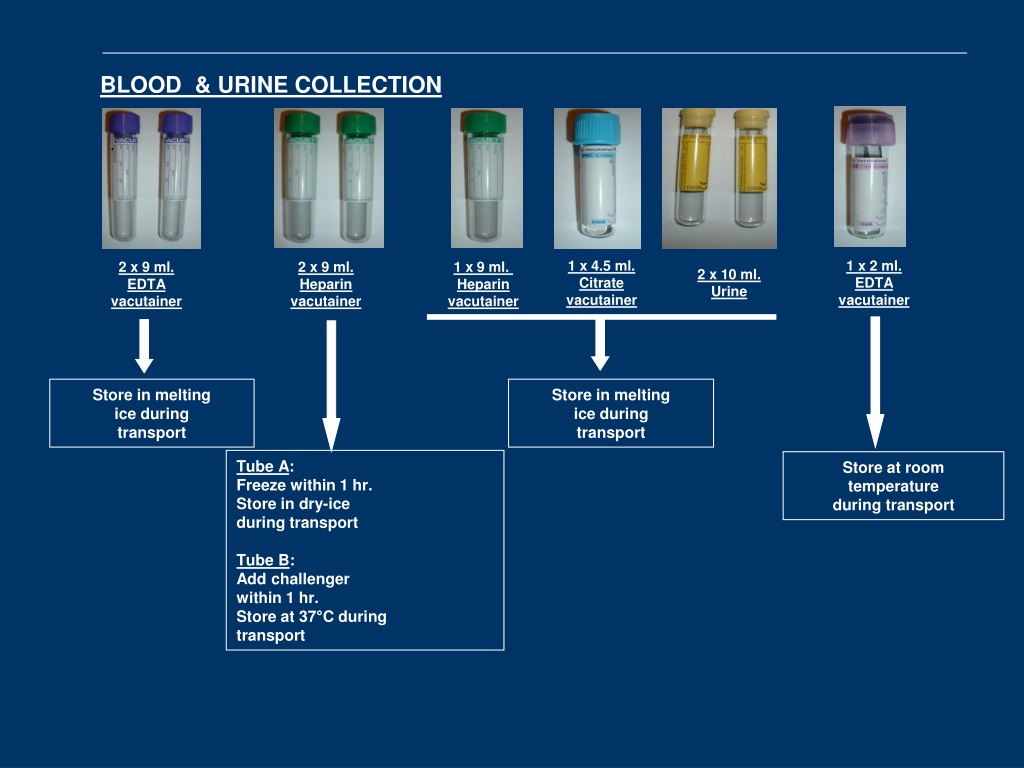
Evaluation
Evaluation will include urinalysis and clean catch urine culture. In the collection of urinary specimens in pregnancy a few considerations are noteworthy. Patients who are well hydrated may excrete dilute urine rendering some assessed parameters to be less accurate. Hematuria may be seen as a result of contamination, particularly when specimens are collected from laboring or postpartum patients. Due to reduced reabsorption of protein, small amounts of protein may normally be excreted. Contamination, as may occur with mucous discharge, may also contribute to the presence of proteinaceous material in the urine of pregnant women.
Due to reduced reabsorption of protein, small amounts of protein may normally be excreted. Contamination, as may occur with mucous discharge, may also contribute to the presence of proteinaceous material in the urine of pregnant women.
Laboratory analysis should include complete blood count (CBC), electrolytes and serum creatine. Tailored studies should be included as appropriate to exclude other causes of patient symptoms, for example, amylase and lipase if pancreatitis is being considered as a diagnosis. If there is a concern for sepsis lactic acid and blood cultures should be obtained. All cultures should be obtained as soon as possible and before starting antibiotic therapy.
When the fetus is viable, fetal heart rate and contraction monitoring should occur. Consideration should be given to obtaining cervical and GBS cultures on admission if pregnancy-related complications develop. Infrequently, renal ultrasound may be indicated to assess for a possible renal abscess.
Treatment / Management
ASB and acute cystitis are treated with antibiotic therapy.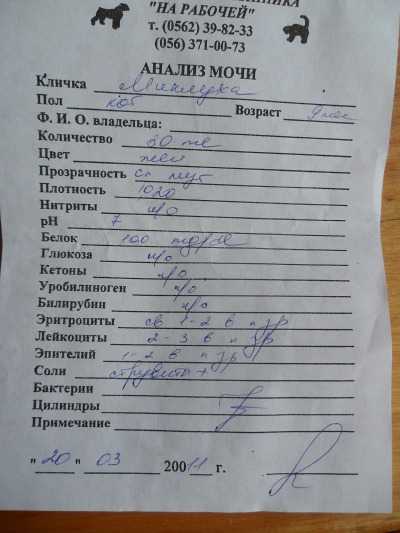 Antibiotic choice can be tailored based on organism sensitivities when available from urine culture results. One-day antibiotic courses are not recommended in pregnancy, although 3-day courses are effective.[4] Antibiotics commonly used include amoxicillin, ampicillin, cephalosporins, nitrofurantoin, and trimethoprim-sulfamethoxazole. Fluoroquinolones are not recommended as a first-line treatment in pregnancy due to conflicting studies regarding teratogenicity. Short courses are unlikely to be harmful to the fetus, and thus, it is reasonable to use this class of drugs with resistant or recurrent infections.
Antibiotic choice can be tailored based on organism sensitivities when available from urine culture results. One-day antibiotic courses are not recommended in pregnancy, although 3-day courses are effective.[4] Antibiotics commonly used include amoxicillin, ampicillin, cephalosporins, nitrofurantoin, and trimethoprim-sulfamethoxazole. Fluoroquinolones are not recommended as a first-line treatment in pregnancy due to conflicting studies regarding teratogenicity. Short courses are unlikely to be harmful to the fetus, and thus, it is reasonable to use this class of drugs with resistant or recurrent infections.
Recently evidence has developed suggesting a link between the use of sulfa derivatives and nitrofurantoin and congenital disabilities when these medications are prescribed in the first trimester. These studies have had limitations; however, it is currently recommended to avoid the use of these medications in the first trimester when alternatives are available.[5] Because the potential consequences of untreated UTI in pregnancy are significant, it is reasonable to use these medications when needed as the benefit strongly outweighs the risk of use. Additional cautions exist with respect to these 2 classes of antibiotics. Patients with G6P deficiency should not be prescribed sulfa derivatives or nitrofurantoin as these medications can precipitate hemolysis. In the late third trimester, trimethoprim-sulfamethoxazole should be avoided due to the potential risk for development of kernicterus in the infant following delivery.
Additional cautions exist with respect to these 2 classes of antibiotics. Patients with G6P deficiency should not be prescribed sulfa derivatives or nitrofurantoin as these medications can precipitate hemolysis. In the late third trimester, trimethoprim-sulfamethoxazole should be avoided due to the potential risk for development of kernicterus in the infant following delivery.
If Group B Streptococcus (GBS) is noted on urine culture, patients should receive intravenous (IV) antibiotic therapy at the time of delivery in addition to indicated treatment for ASB or UTI. This is to prevent the development of early-onset GBS sepsis which may occur in the infants of women who are colonized with GBS.
Pyelonephritis in pregnancy is a serious condition usually requiring hospitalization. Once an evaluation has been completed, treatment consists primarily of directed antibiotic therapy and IV fluids to maintain adequate urine output. Fever should be treated with a cooling blanket and acetaminophen as needed.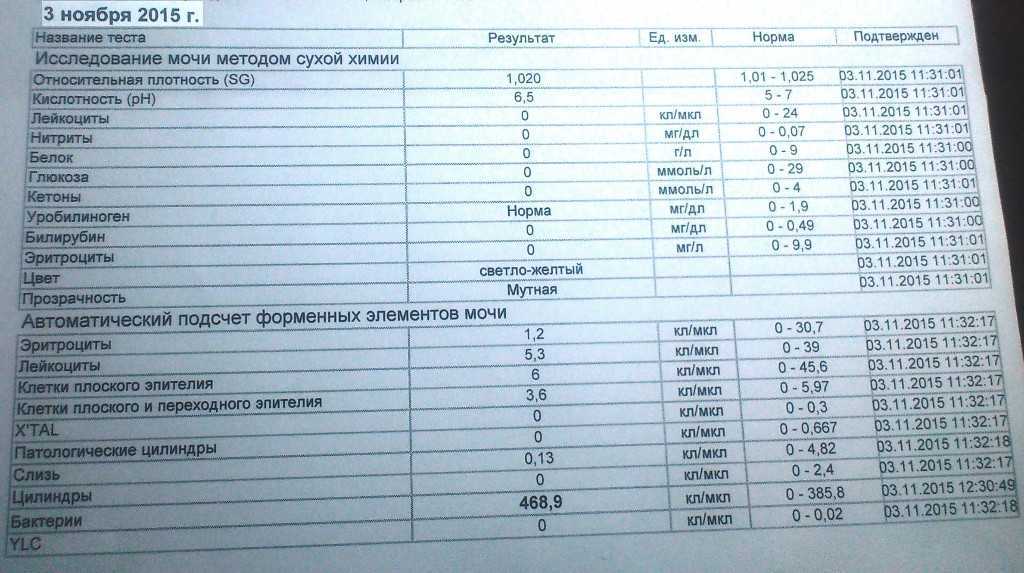 Commonly, second or third generation cephalosporins are used for initial treatment. Ampicillin and gentamicin or other broad-spectrum antibiotics are alternatives. Patients should be monitored closely for the development of worsening sepsis.
Commonly, second or third generation cephalosporins are used for initial treatment. Ampicillin and gentamicin or other broad-spectrum antibiotics are alternatives. Patients should be monitored closely for the development of worsening sepsis.
Differential Diagnosis
Differential diagnosis includes acute intraabdominal disease such as appendicitis, pancreatitis, or cholecystitis as well as pregnancy-related complications such as preterm labor, chorioamnionitis, or placental abruption.
Complications
Patients with pyelonephritis are at risk for several significant complications.
Sepsis may worsen resulting in hypotension, tachycardia, and decreased urine output. ICU admission may be required.
Pulmonary complications are not uncommon, occurring in up to 10% of pregnant patients undergoing treatment for pyelonephritis.[4] This is due to endotoxin-mediated alveolar damage and may manifest as pulmonary edema or acute respiratory distress syndrome (ARDS). Urine output and oxygen status should be monitored closely, and patients may require ICU admission for respiratory support.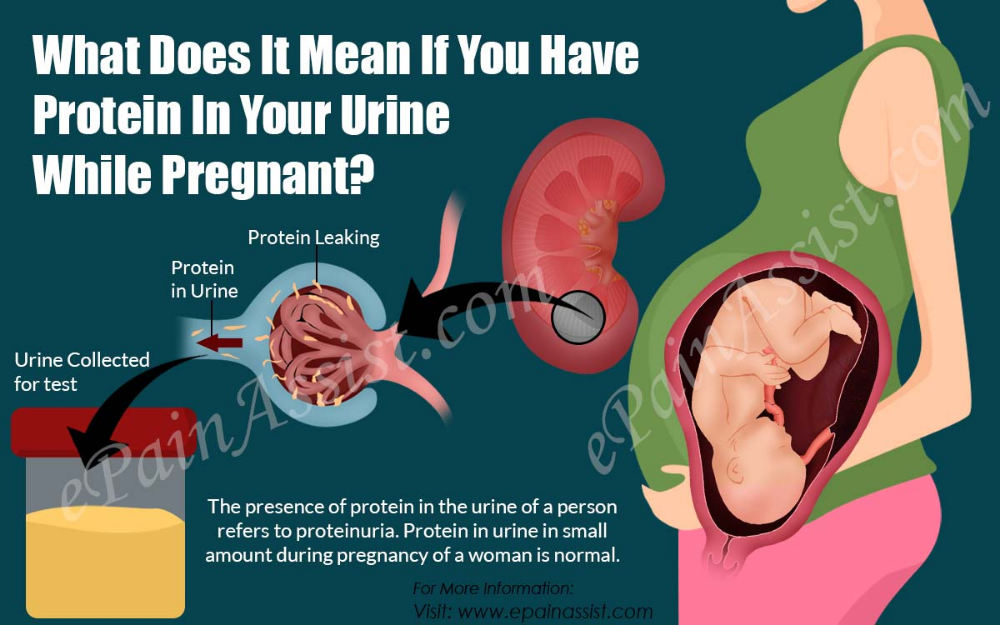
Endotoxin release may lead to anemia, this typically resolves spontaneously following treatment. This is the most common complication seen with pyelonephritis occurring in up to 25% of patients.[3]
Endotoxin release may also cause uterine contractions and patients should be monitored for preterm labor; patients should be treated for preterm labor when indicated. Caution should be exercised in use of tocolytic therapy as the risk of pulmonary edema is increased in the setting of UTI.
A small number of patients may experience persistent infection. In these cases, consideration should be given to urinary obstruction or renal abscess. Antibiotic choice should be re-evaluated and culture results reviewed.
Deterrence and Patient Education
After 2 to 4 weeks following completion of treatment, urine culture should be obtained to assure that reinfection has not occurred.
Suppressive antibiotic therapy, usually with nitrofurantoin once daily, is commonly recommended especially in cases where patients have had prior UTI. This is typically continued thru pregnancy and the early postpartum period.
This is typically continued thru pregnancy and the early postpartum period.
Enhancing Healthcare Team Outcomes
Interprofessional collaboration is crucial in the management of these ill patients. With the administration of antibiotics patients may show initial worsening due to the release of endotoxin, however, most patients improve within 72 hours. Long-term complications such as renal damage are rare.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Gilstrap LC, Ramin SM. Urinary tract infections during pregnancy. Obstet Gynecol Clin North Am. 2001 Sep;28(3):581-91. [PubMed: 11512502]
- 2.
Gazmararian JA, Petersen R, Jamieson DJ, Schild L, Adams MM, Deshpande AD, Franks AL. Hospitalizations during pregnancy among managed care enrollees. Obstet Gynecol. 2002 Jul;100(1):94-100. [PubMed: 12100809]
- 3.
Wing DA, Fassett MJ, Getahun D.
 Acute pyelonephritis in pregnancy: an 18-year retrospective analysis. Am J Obstet Gynecol. 2014 Mar;210(3):219.e1-6. [PubMed: 24100227]
Acute pyelonephritis in pregnancy: an 18-year retrospective analysis. Am J Obstet Gynecol. 2014 Mar;210(3):219.e1-6. [PubMed: 24100227]- 4.
Sheffield JS, Cunningham FG. Urinary tract infection in women. Obstet Gynecol. 2005 Nov;106(5 Pt 1):1085-92. [PubMed: 16260529]
- 5.
Committee Opinion No. 717: Sulfonamides, Nitrofurantoin, and Risk of Birth Defects. Obstet Gynecol. 2017 Sep;130(3):e150-e152. [PubMed: 28832488]
Urinalysis during pregnancy - what to watch
- Why take a urine test during pregnancy
- How to properly pass urine for analysis
- What a urine test shows and how it is assessed
- Special urine tests
During pregnancy, a woman undergoes many different tests. The most frequent, and at the same time the simplest study is a urinalysis. It is taken regularly, before each visit to the doctor of the antenatal clinic, that is, at least 12 times during pregnancy.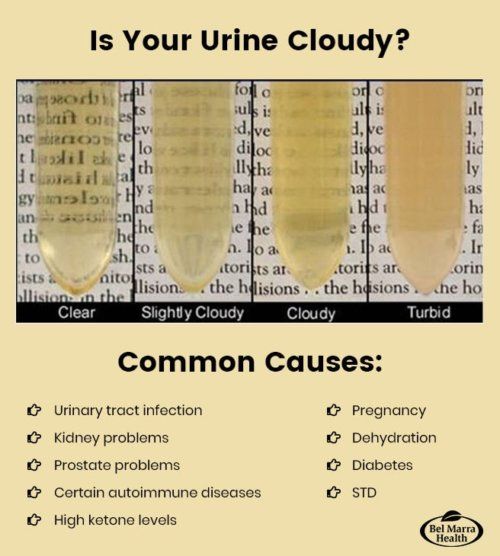
Why take a urine test during pregnancy
Urine is formed in the kidneys during blood filtration, with it the decay products formed during metabolism, salts, vitamins, hormones are excreted from the body. Based on this analysis, one can judge the work of the kidneys and other organs. The main component of urine is water (92-99%). Approximately 50-70 dry substances are removed from the body with urine every day, most of which are urea and sodium chloride. The composition of urine varies significantly even in healthy people, depending on the diet, drinking regimen and medication. During pregnancy, a regular study of a general urine test allows you to suspect in time the initial pathological processes in the body of a future mother, for example, the development of a urinary tract infection or toxicosis in the second half of pregnancy. For a correct assessment of the results of the analysis, urine must be collected correctly.
How to donate urine for analysis
On the eve of the test, it is recommended to refrain from intense physical activity, do not eat a lot of meat products, salty, sour and spicy foods, as well as coloring foods (beets, carrots, etc. ). This can lead to a distortion of the result - the appearance of protein and salts in the urine. For a general urinalysis, it is preferable to collect the morning portion of urine.
). This can lead to a distortion of the result - the appearance of protein and salts in the urine. For a general urinalysis, it is preferable to collect the morning portion of urine.
Preliminary thorough toileting of the external genitalia with warm water and soap. It is better to close the vagina with a cotton swab to prevent secretions from entering the urine sample. Urine is collected in a clean, dry container. For analysis, an average portion of urine is used, that is, for the first few seconds you need to urinate into the toilet, then into a jar, and the remains again into the toilet.
Urine must be delivered to the laboratory within two hours of collection and it is advisable to try not to subject it to strong shaking during transport. It is allowed to store urine in the refrigerator at a temperature of +2-+4 degrees, but not more than 1.5 hours. It is desirable that the amount of material collected for the study be at least 70 ml.
What a urinalysis shows and how it is evaluated
In a urinalysis, many parameters are evaluated.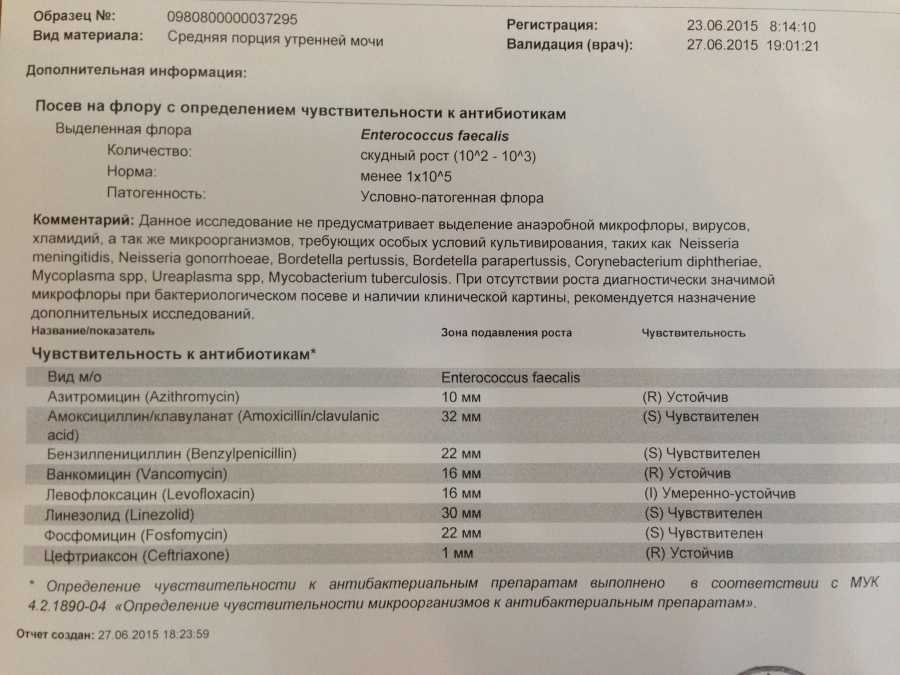
Color
Normal urine has a yellow color of various shades. The shade depends on the degree of saturation of urine with a special pigment - urochrome. A change in the color of urine can occur when taking certain medications (for example, vitamins can give a bright yellow color, aspirin - pink). However, much more often a change in the color of urine indicates the presence of any pathological processes in the body. When blood appears in the urine, which occurs in diseases of the kidneys and bladder, the urine becomes bright red (with renal colic, cystitis) or the so-called “color of meat slops” (with acute inflammatory kidney damage). With increased destruction of red blood cells (erythrocytes), urine acquires a reddish-brown hue. Yellow-brown (or beer-colored) urine occurs with liver diseases.
Transparency
Transparency should normally be complete. Turbidity of urine can be the result of the presence in the urine of erythrocytes, leukocytes, epithelium, bacteria, fat droplets, precipitation of salts.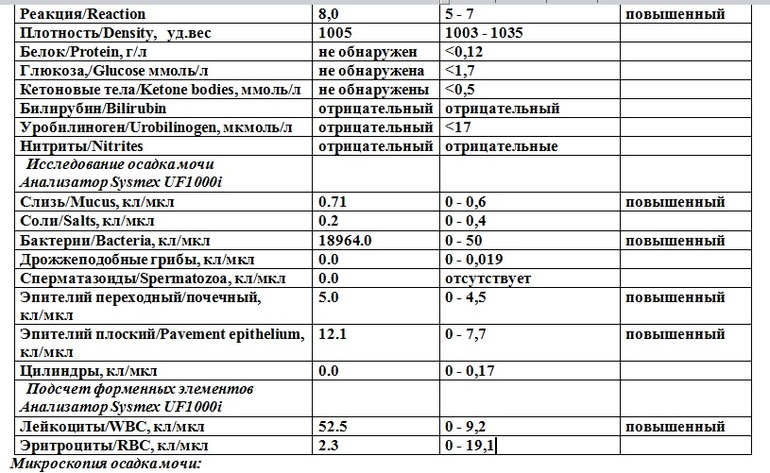
Relative density (specific gravity)
This is an indicator that characterizes the amount of trace elements, salts, various compounds. Normally, the specific gravity is 1003 - 1035 g / l. This indicator may decrease in the presence of glucose or protein in the urine, with toxicosis of the first half of pregnancy, dehydration. An increase in specific gravity occurs in chronic renal failure, diabetes insipidus, and heavy drinking.
Protein
Protein content in urine is one of the most important indicators of kidney function. Normally, it shouldn't be. A small amount of protein in the urine (physiological proteinuria) can also be found in healthy people, while the protein concentration does not exceed 0.033 g / l, in modern laboratories with more sensitive equipment - 0.14 g / l. The appearance of protein in the urine is noted in diseases of the kidneys, inflammatory diseases of the bladder and urinary tract. The presence of protein in the urine, combined with increased blood pressure and edema, is a sign of a serious complication of pregnancy - late preeclampsia, which can lead to seizures and even death of a pregnant woman and fetus.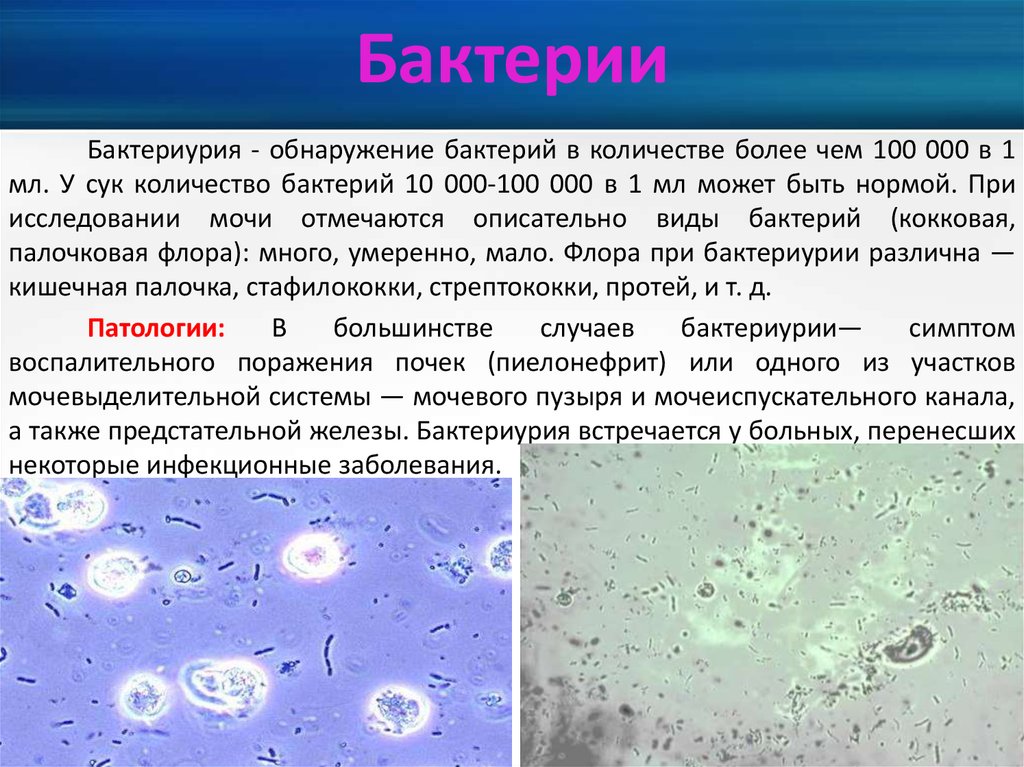
Glucose
Normally, there is no glucose in the general urine test. However, in the second half of pregnancy, the presence of glucose in the urine (glucosuria) can normally be detected. This is due to increased filtration of glucose in the kidneys. Since the appearance of glucose in the urine can be a sign of a serious illness - diabetes mellitus, acute inflammation of the pancreas, all patients with glucosuria need an additional examination - blood glucose control, sometimes even a glucose tolerance test with a sugar load - determination of blood glucose on an empty stomach and 2 hours after taking 75 grams of glucose.
Bilirubin
This is a blood pigment that is formed as a result of metabolic processes in the body and is excreted with bile into the gastrointestinal tract. With an increase in the concentration of bilirubin in the blood, it begins to be excreted by the kidneys and found in the urine. This occurs mainly with liver damage or mechanical obstruction of the outflow of bile.
Urobilinogen
This is a conversion product of bilirubin. Normally, it is excreted in the bile and practically does not enter the urine. The appearance of urobilinogen in the urine occurs in liver diseases, poisoning, increased decay of red blood cells - erythrocytes.
Ketone bodies
These are products formed during the breakdown of fatty acids in the body. Normally, there are no ketone bodies in the urine test. Determining them is very important in diagnosing the adequacy of diabetes therapy. The appearance of ketones can occur in the first trimester of pregnancy with early toxicosis and indicate dehydration.
Nitrites
These are salts of nitrous acid and are not normally found in urine. Their appearance indicates the presence of a urinary tract infection.
Leukocytes
These are white blood cells. Normally, in the general analysis of urine, leukocytes are found up to 5 in the field of view. If the number of leukocytes is increased, this indicates the presence of an inflammatory process in the kidneys, bladder or urethra, while the higher the number of leukocytes, the more pronounced the inflammation.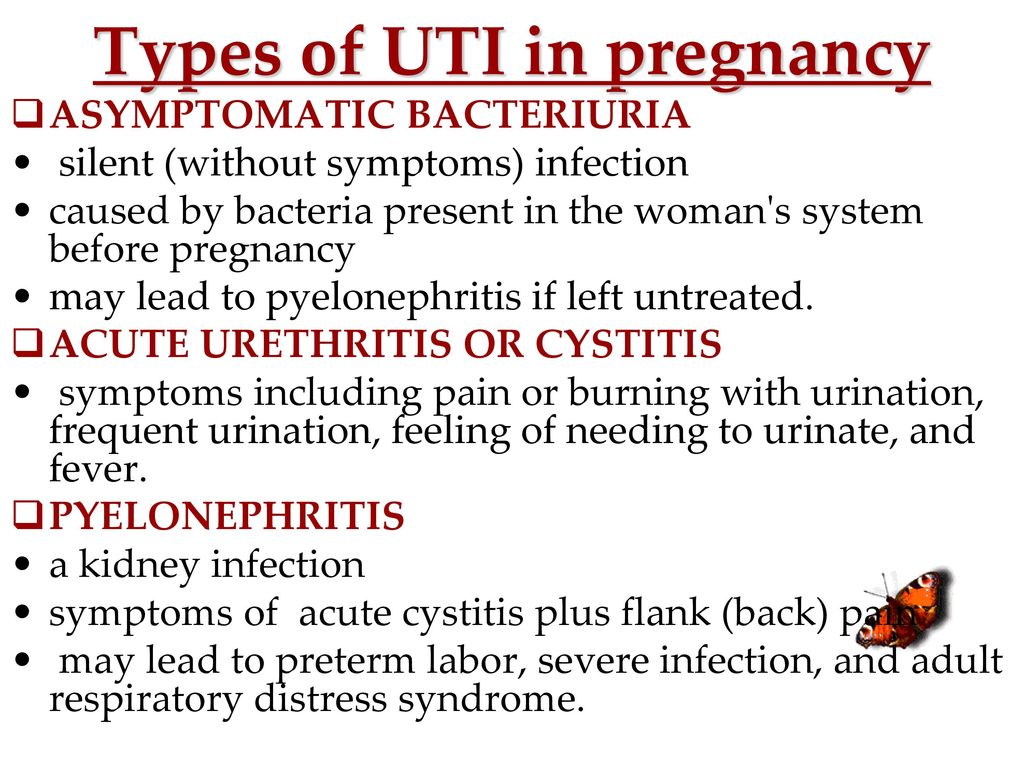 A slight increase in the number of leukocytes can be observed if vaginal discharge enters the urine with a poor toilet of the external genitalia.
A slight increase in the number of leukocytes can be observed if vaginal discharge enters the urine with a poor toilet of the external genitalia.
Erythrocytes
Red blood cells. Normally, in the general analysis of urine there should be no more than 2 erythrocytes in the field of view. An increase in their number occurs in the presence of stones in the kidneys or urinary tract, inflammation of the kidneys, injuries.
Cylinders
Cylindrical elements of urine sediment, consisting of protein or cells, may also contain various inclusions. Normally absent. They are found mainly in diseases of the kidneys.
Salts
These are inorganic substances which may precipitate on standing urine. Normally, there are no salts in the urine. The appearance of urates in the urine occurs with kidney diseases, as well as in the first trimester of pregnancy with vomiting of pregnant women.
Amorphous phosphates
Also found in vomiting of pregnant women, in inflammation of the bladder, and can occur normally with a predominance of vegetable and dairy foods in the diet.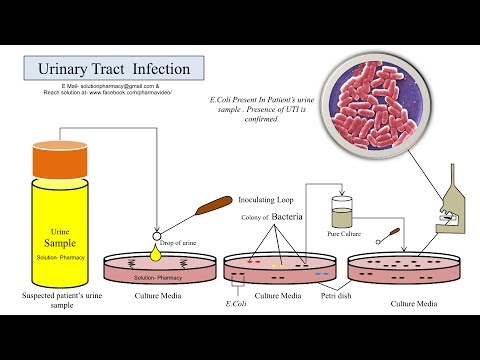
Oxalates
Occurs in inflammation of the kidneys, diabetes mellitus, as well as in the predominance of foods rich in oxalic acid in the diet (spinach, sorrel, tomatoes, asparagus).
Bacteria
Isolation of bacteria in the urine is of significant diagnostic value in pregnancy. The appearance of bacteria in the urine indicates the presence of an inflammatory process in the kidneys, bladder or urethra and requires mandatory treatment, even if the expectant mother is not worried about anything. Bacteria can also enter the urine from the vagina when the toilet of the external genitalia is poor. To determine the number of bacteria, their type and sensitivity to antibiotic therapy, an additional urine culture for flora is mandatory. To obtain the correct result of this analysis, after a thorough toilet of the external genital organs, close the vagina with a cotton swab, collect the middle portion of urine in a sterile container, tighten the lid tightly and deliver it to the laboratory within one and a half to two hours. Urine culture is prepared on average from 7 to 10 days and allows the doctor to decide whether it is necessary to carry out antibacterial treatment, and with what drugs.
Urine culture is prepared on average from 7 to 10 days and allows the doctor to decide whether it is necessary to carry out antibacterial treatment, and with what drugs.
Find out more about the services:
- Tests for pregnant women
Special urinalysis
Urine culture
Mandatory if bacteria are detected in the general urinalysis.
The purpose of the study. Performed to determine the number of bacteria, their type and sensitivity to antibacterial drugs.
Rules for collecting urine for analysis. To obtain a correct result from this test, urine must be collected after thorough toileting of the vulva, covering the vagina with a cotton swab. It is necessary to collect an average portion of urine in a sterile container, screw the lid tightly and deliver it to the laboratory within one and a half to two hours.
Urine culture is prepared on average from 7 to 10 days and allows the doctor to decide whether to carry out antibacterial treatment and with what drugs. If there is a clinical picture of inflammation, before the results of the culture are obtained, antibacterial treatment with a broad-spectrum antibiotic (acts on a large range of bacteria) is carried out, and in case of asymptomatic course of the disease or mild inflammation, treatment is not carried out until the results of the analysis are obtained.
If there is a clinical picture of inflammation, before the results of the culture are obtained, antibacterial treatment with a broad-spectrum antibiotic (acts on a large range of bacteria) is carried out, and in case of asymptomatic course of the disease or mild inflammation, treatment is not carried out until the results of the analysis are obtained.
Urinalysis according to Nechiporenko
This is a special urine test that shows the content of erythrocytes, leukocytes and cylinders in 1 ml of urine.
The purpose of the study. This analysis is prescribed if there is a suspicion of an inflammatory process in the organs of the urinary system in a pregnant woman, if there are changes in the general analysis of urine. It gives more accurate results than a general urinalysis, and also allows you to control the ongoing treatment in dynamics.
Urine collection rules. Urine for analysis according to Nechiporenko is collected in the same way as for a general urine test.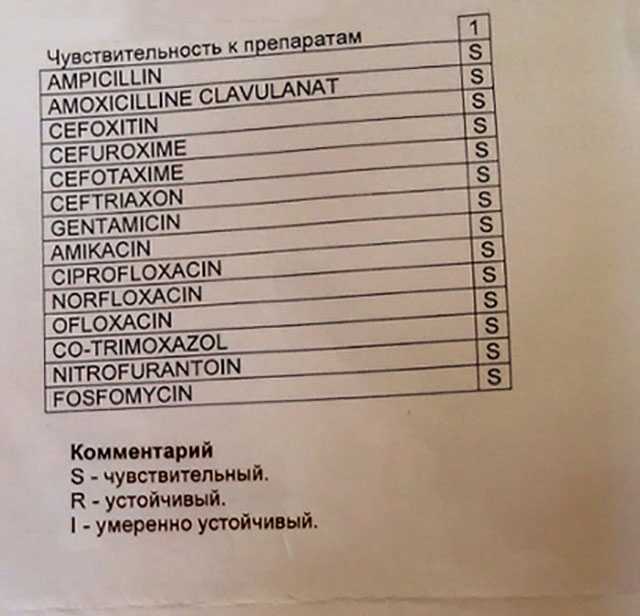
Parameters under investigation
- The number of leukocytes - normally they should be less than 2 thousand in 1 ml . An increase of in the number of leukocytes indicates the presence of pyelonephritis (an inflammatory disease of the pelvis and calices of the kidneys).
- The number of erythrocytes is normally less than 1 thousand per 1 ml. An increase in the number of red blood cells indicates the development of glomerulonephritis (inflammation of the renal glomeruli).
- The number of cylinders is normally less than 20 in 1 ml. The detection of an increased content of cylinders indicates arterial hypertension, diseases of the cardiovascular system, and can occur with early toxicosis of pregnant women.
Urinalysis according to Zimnitsky
Purpose of the study. This analysis is prescribed to clarify the ability of the kidneys to concentrate and dilute urine, to identify latent edema.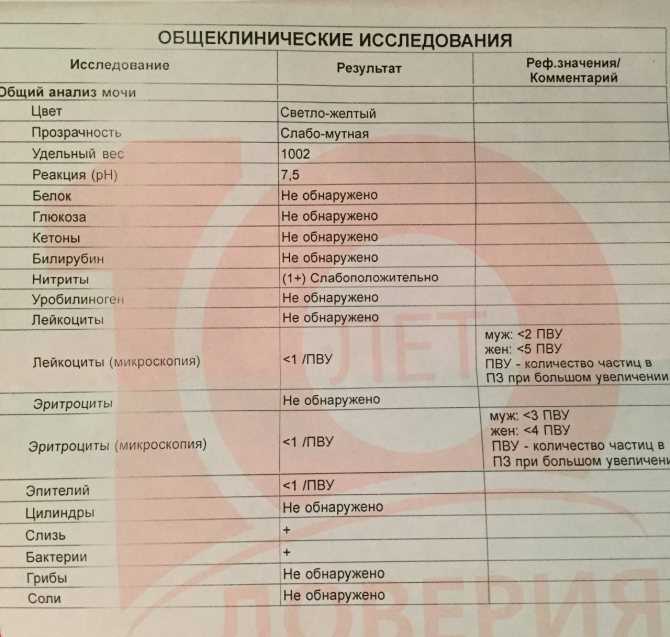 The study may be needed if you suspect the development of preeclampsia, renal failure, infections of the urinary system, as well as diabetes.
The study may be needed if you suspect the development of preeclampsia, renal failure, infections of the urinary system, as well as diabetes.
Urine collection rules. For urinalysis according to Zimnitsky, urine is collected during the day (24 hours) in 8 containers (jars), while the amount of liquid drunk is necessarily taken into account (the pregnant woman writes down how much liquid she drinks during the day, taking into account soups, fruits and vegetables). At 6 am, a woman urinates into the toilet, then all subsequent urine is collected in jars.
Total 8 servings:
- 1 serving - 6:00 a.m. to 9:00 a.m.,
- 2 portion - from 9-00 to 12-00 hours,
- 3 portion - from 12-00 to 15-00 hours,
- 4 portion - from 15-00 to 18-00 hours,
- 5 portion - from 18-00 to 21-00 hours,
- 6 portion - from 21-00 to 24-00 hours,
- 7 portion - from 24-00 to 3-00 hours,
- 8 portion - from 3-00 to 6-00 hours.

Jars are signed and delivered to the laboratory.
Test parameters. The amount and specific gravity of urine in each portion is estimated. Normal kidney function is characterized by:
- daily urine volume about 1.5 liters;
- predominance of daytime urination over nighttime;
- urinary excretion of approximately 70--80% of the liquid drunk per day;
- the specific gravity of urine in at least one of the portions is not lower than 1.020--1.022;
- significant fluctuations during the day the amount of urine in individual portions (from 50 to 400 ml) and the specific gravity of urine (from 1.003 to 1.028).
Deviations from these standards indicate a violation in the work of the kidneys.
Rehberg's test
Purpose of the study. This test is used to determine the ability of the kidneys to filter urine. It must be carried out for all pregnant women with preeclampsia, with urinary tract infections, with kidney diseases, and with diabetes.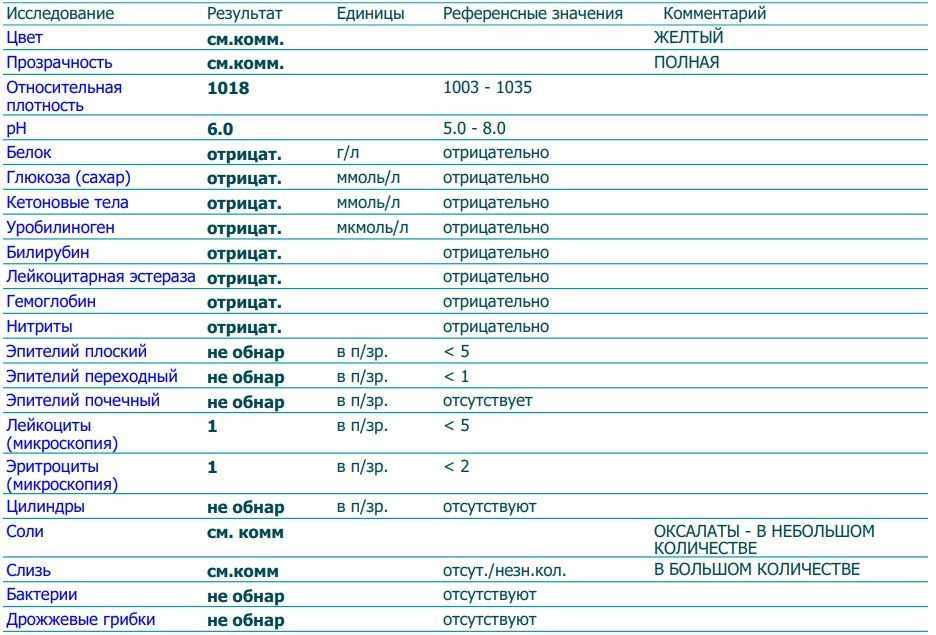
Urine collection rules. Before the test, intense physical activity, strong tea and coffee are excluded. Urine is collected during the day in one container, which is stored in the refrigerator during the entire collection time. After completing the collection of urine, measure the contents of the container, be sure to mix and immediately pour 70-100 ml into a special container or jar and deliver it to the laboratory, reporting the total volume of urine collected per day.
At the time of delivery of urine to the laboratory, blood is taken for creatinine from a vein.
Test parameters. The method is based on the assessment of glomerular filtration by the rate of purification of blood plasma from creatinine, a special product of protein breakdown. This indicator can be determined if you know the concentration of creatinine in the blood, in the urine and the daily volume of urine. This indicator is calculated using a special formula and is called creatinine clearance.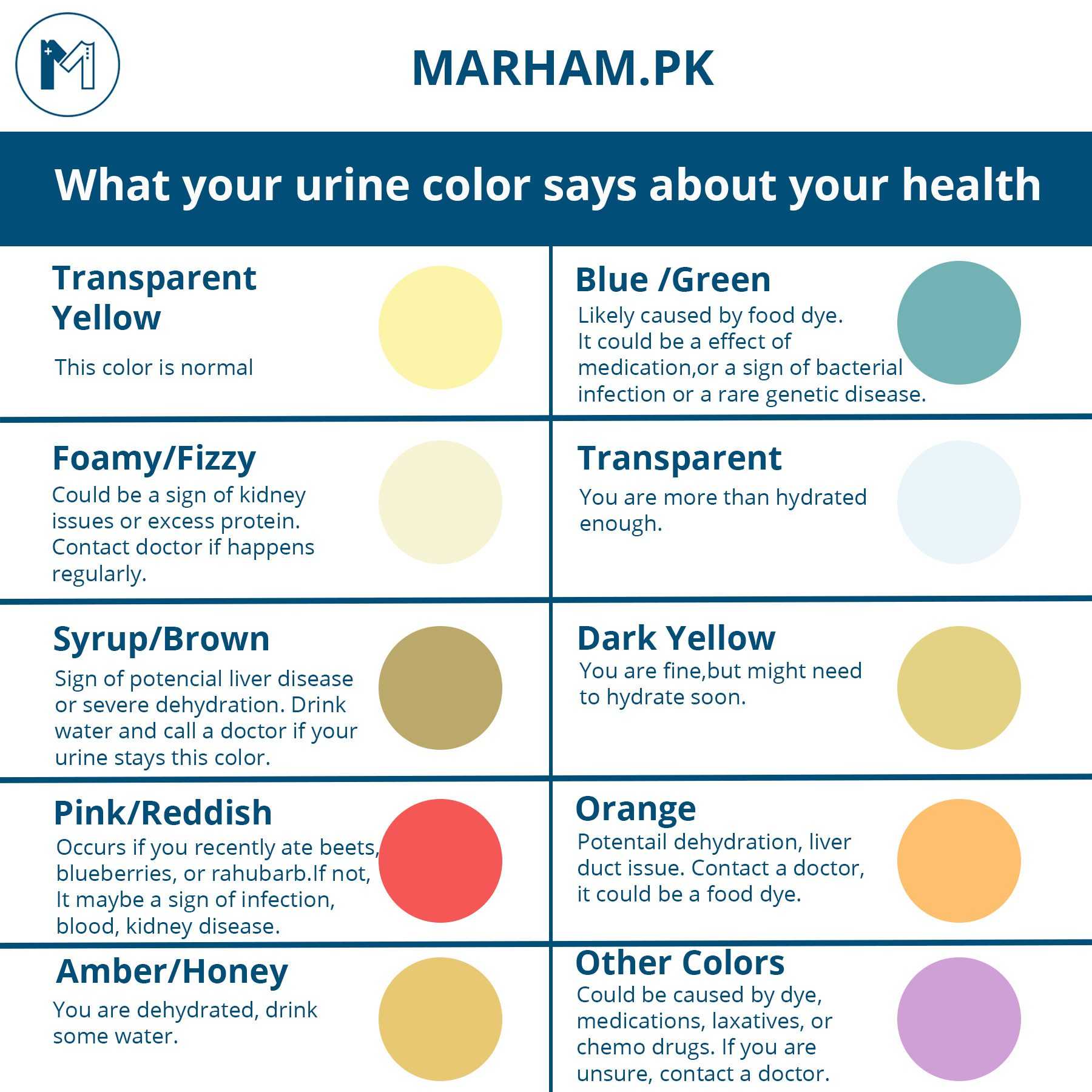 Normally, the value of this indicator ranges from 75 to 134 ml / min / 1.7 m2. A decrease in the level of renal filtration indicates kidney damage and occurs with severe complications of pregnancy - gestosis, kidney diseases (pyelonephritis, glomerulonephritis), diabetes mellitus, arterial hypertension, urolithiasis.
Normally, the value of this indicator ranges from 75 to 134 ml / min / 1.7 m2. A decrease in the level of renal filtration indicates kidney damage and occurs with severe complications of pregnancy - gestosis, kidney diseases (pyelonephritis, glomerulonephritis), diabetes mellitus, arterial hypertension, urolithiasis.
Urine for 17-KC
This test was previously widely prescribed to pregnant women to determine the hormones produced by the adrenal cortex. For analysis, urine was collected during the day, mixed, a small part of it was poured, which was delivered to the laboratory with an indication of the total amount of urine collected. An increase in the concentration of 17-ketosteroids in the urine indicated an excess production of hormones in the body of a pregnant woman, on the basis of which the doctor prescribed hormonal drugs. However, at present, the determination of these substances in urine is considered uninformative and is not used during pregnancy.
Urine tests are very easy to perform and very informative for the doctor, they allow you to timely detect the slightest changes in the body of the expectant mother and start treatment in a timely manner, which helps prevent serious complications from the pregnant woman and the unborn baby.
Asymptomatic bacteriuria - articles from the specialists of the clinic "Mother and Child"
Agranovskaya Anna Valerievna
Obstetrician-gynecologist
Lapino-1 Clinical Hospital "Mother and Child"
During pregnancy, this problem requires special attention!
It should be noted that the kidneys of a pregnant woman experience increased stress. The smooth muscle of the urinary system is affected by the hormone progesterone, which has a relaxing effect on it.
From the second trimester the gradually enlarging uterus begins to compress the abdominal organs, including the ureters, kidneys, and bladder. As a result, the pyelocaliceal system of the kidneys expands, which contributes to some stagnation of urine. Such urine is a favorable environment for the reproduction of bacteria.
During pregnancy, the presence of bacteria is found in urine tests, but the woman does not present any complaints, nothing bothers her.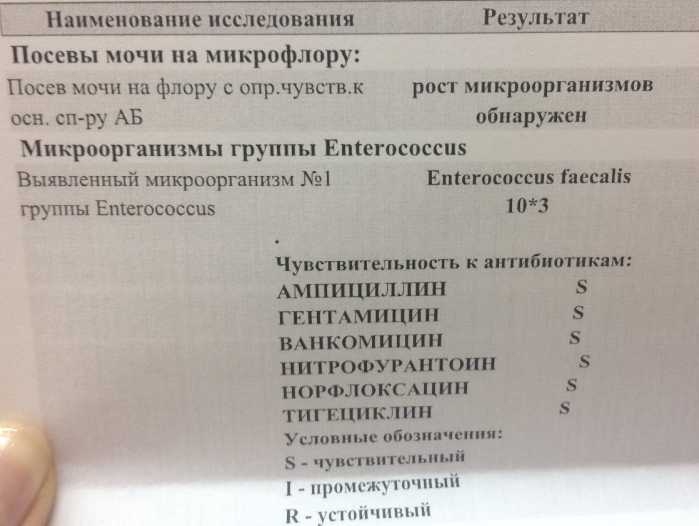 This is regarded as asymptomatic bacteriuria. A similar phenomenon occurs on average in 6% of cases.
This is regarded as asymptomatic bacteriuria. A similar phenomenon occurs on average in 6% of cases.
Asymptomatic bacteriuria in pregnant women significantly increases the risk of urinary tract infections - inflammation of the bladder / cystitis / and inflammation of the kidneys / pyelonephritis /. And urinary tract infections can cause a number of serious complications of pregnancy and childbirth - a decrease in hemoglobin, an increase in blood pressure, premature birth, the birth of children with a low body weight of less than 2500 g.
When bacteria are isolated in a general urinalysis, an additional examination is recommended - seeding for flora and sensitivity to antibiotics to identify bacteria and determine their sensitivity to antibacterial drugs.
Based on the results of sowing, the doctor prescribes an effective and safe treatment for a pregnant woman. The duration of the course of treatment depends on the severity of changes in the culture.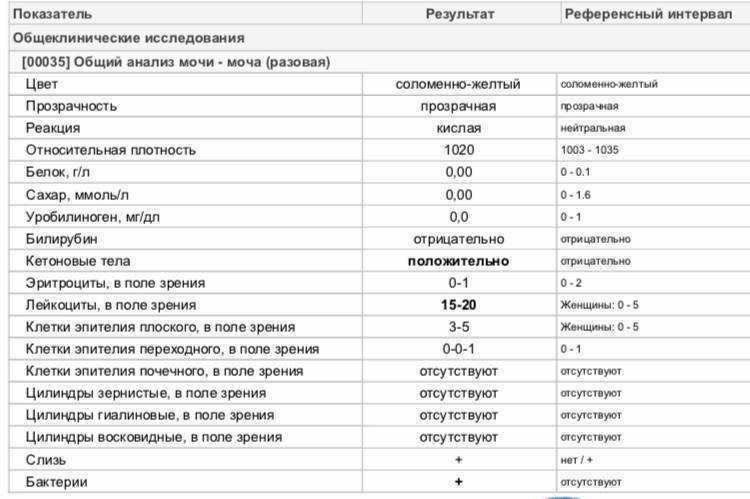 After treatment, urine culture control is prescribed, not earlier than 5 days after the end of treatment.
After treatment, urine culture control is prescribed, not earlier than 5 days after the end of treatment.
Prevention! In order to prevent exacerbations, it is necessary to follow the recommendations to ensure an improvement in the outflow of urine and prevent stagnation and reproduction of bacteria in the organs of the urinary system:
- diet with restriction of spicy, salty, smoked
- sweets should be limited - glucose is a favorable environment for the development of microorganisms
- drinking regime not less than 1.5–2.0 liters per day. A sufficient volume of liquid contributes to the free removal of waste substances and toxins from the body. Among drinks, preference should be given to mineral non-carbonated water, compotes, cranberry and lingonberry fruit drinks
- knee-elbow position for 5-10 minutes 3-5 times a day. In the knee-elbow position, the load is redistributed. The uterus, under the force of gravity, shifts forward and down, freeing the ureters, kidneys, and bladder from compression.