How to soothe a coughing child
Coughs: Meds or Home Remedies?
Medicines (OTC)
Over-the-Counter (OTC) cough and cold medicines can cause side effects. These side effects can be serious in young children. The risks of using these medicines outweigh any benefits. The Food and Drug Administration (FDA) recommends these medicines never be used in young children. After age 6, the medicines are safe to use, if you follow the package instructions. But, it's easy to treat coughs and colds without these medicines.
Home Remedies:
A good home remedy is safe, cheap, and as helpful as OTC medicines. They are also found in nearly every home. Here are some simple but helpful home treatments.
1. Runny Nose: Just suction it or blow it. Teach your child how to blow the nose at age 2 or 3. When your child's nose runs like a faucet, it's getting rid of viruses. Allergy medicines (such as Benadryl) do not help the average cold. They are useful only if your child has nasal allergies (hay fever).
2. Blocked Nose: Use nasal saline.
- Use saline (salt water) nose drops or spray to loosen up the dried mucus. If you don't have saline, you can use a few drops of water. Use distilled water, bottled water or boiled tap water.
- Step 1: Put 3 drops in each nostril. If age under 1 year old, use 1 drop.
- Step 2: Blow (or suction) each nostril separately, while closing off the other nostril. Then do other side.
- Step 3: Repeat nose drops and blowing (or suctioning) until the discharge is clear.
- How Often: Do nasal saline rinses when your child can't breathe through the nose. Limit: If under 1 year old, no more than 4 times per day or before every feeding.
- Saline nose drops or spray can be bought in any drugstore. No prescription is needed.
- Reason for nose drops: Suction or blowing alone can't remove dried or sticky mucus. Also, babies can't nurse or drink from a bottle unless the nose is open.
- Other option: use a warm shower to loosen mucus.
 Breathe in the moist air, then blow (or suction) each nostril.
Breathe in the moist air, then blow (or suction) each nostril. - For young children, can also use a wet cotton swab to remove sticky mucus.
- Medicines. There are no drugs that can remove dried mucus from the nose.
3. Coughing: Use homemade cough medicines.
- Age 6 months to 1 year. Give warm clear fluids (such as apple juice or lemonade). Dose: 1-2 teaspoons (5-10 mL) four times per day when coughing. Under 3 months, see your child's doctor. Caution: Do not use honey until 1 year old.
- Age 1 year and older. Use Honey ½ to 1 teaspoon (2 to 5 mL) as needed. It thins the secretions and loosens the cough. If you don't have honey, you can use corn syrup. Research shows that honey works better than cough syrups to reduce nighttime coughing. Can also offer warm lemonade or herbal teas. Amount: a few ounces (30 mL) each time.
- Age 6 years and older. Use Cough Drops to decrease the tickle in the throat. If you don't have any, you can use hard candy.
 Avoid cough drops before 6 years. Reason: risk of choking.
Avoid cough drops before 6 years. Reason: risk of choking. - Coughing fits. The warm mist from a shower can help.
4. Fluids: Help your child drink lots of fluids. Staying well hydrated thins the body's secretions. That makes it easier to cough and blow the nose.
5. Humidity: If the air in your home is dry, use a humidifier. Moist air keeps the nose and airway from drying out. Run a warm shower for a while to help put moisture in the air.
Treatment is Not Always Needed:
- If symptoms aren't bothering your child, they don't need medicine or any treatment. Many children with a cough or cold are happy, play fine and sleep well.
- Only treat symptoms if they cause discomfort or wake your child up. Treat a cough if it's hacking and really bothers your child.
- Fevers are helpful. Only treat them if they slow your child down or cause some discomfort. That does not occur until 102° F (39° C) or higher.
 Acetaminophen (Tylenol) or ibuprofen (Motrin or Advil) can be given. Use to treat higher fever or pain. See Dose tables.
Acetaminophen (Tylenol) or ibuprofen (Motrin or Advil) can be given. Use to treat higher fever or pain. See Dose tables.
Summary
If coughs or colds need treatment, home remedies may work better than medicines.
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Last Reviewed: 02/09/2023
Last Revised: 12/30/2022
Copyright 2000-2023 Schmitt Pediatric Guidelines LLC.
Home Remedies for Cough in Kids – Children's Health
Children’s Health Dec 5, 2018, 10:02:24 AM CST Jan 30, 2023, 5:47:15 PM CSTOver-the-counter cough and cold medicines are not recommended for young children. Learn how to soothe your child's symptoms naturally with these home cough remedies.
Share:
If your child seems to be coughing constantly, it can be concerning. Typically, a child's cough is nothing to worry about. Many times, it can be caused by a common cold or even by allergies.
Because over-the-counter cough and cold medicines are not recommended for children under the age of 6 years, it can be challenging to know how to help your child feel comfortable – especially if a cough is keeping them up at night. See seven ways you can treat your child's cough at home.
Home remedies to help soothe a child's cough
- Drink warm fluids: Encourage your child to drink plenty of fluids.
 Warm liquids such as caffeine-free tea, broth or hot water with lemon can help loosen up mucus and soothe a sore throat.
Warm liquids such as caffeine-free tea, broth or hot water with lemon can help loosen up mucus and soothe a sore throat. - Consider using a humidifier: Dry air can make a child's cough worse. Consider placing a cool-mist humidifier in your child's room, near where they sleep, to help ease their breathing.
- Breathe in warm water vapors: Let your child breathe in water vapors from a warm bath or shower. This can help loosen mucus and, as a bonus, calm your child before bed.
- Try icy treats: Give your child cold items like popsicles or ice cream to make a hurting throat feel better.
- Saline and suction: A saline solution, such as a nose spray or mist, can help loosen mucus in the nose. Have your child blow their nose frequently, or if they are young, use a suction bulb to prevent drainage.
- Give a spoonful of honey (over age 1): A teaspoon of honey can help combat coughing but should only be given to children over age 1.

- Get some zzz's: Encourage your to child get plenty of rest and sleep to promote healing. While coughing may seem aggravated at night, the above tips may help your child find relief.
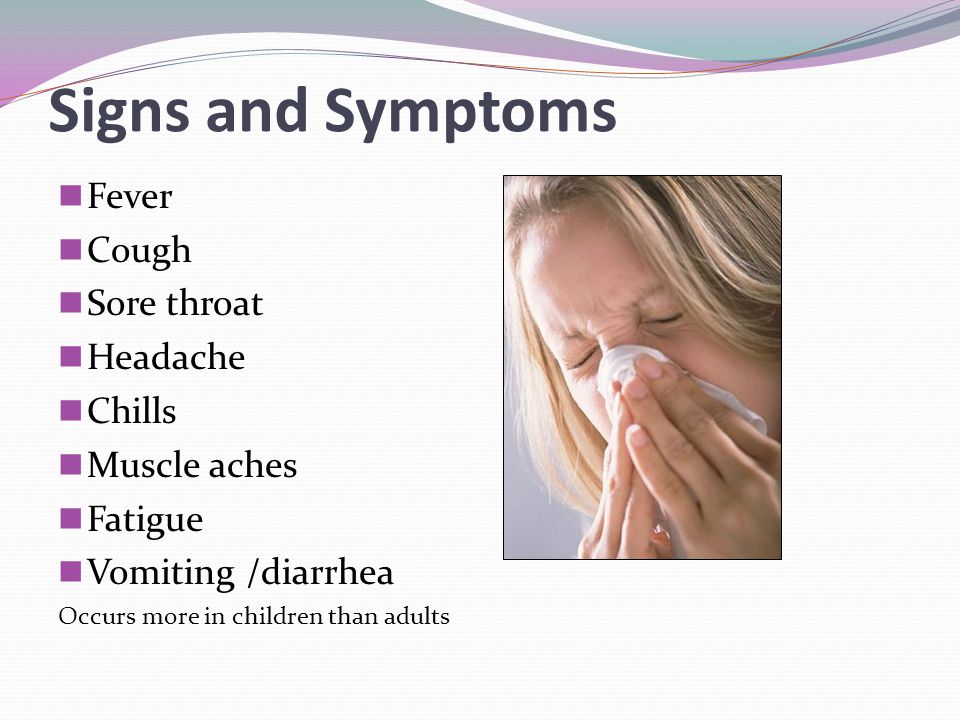
Remember, it can take a couple of weeks for a child to recover from a cold. However, if your child's cough continues to linger, is accompanied by symptoms such as a high fever or difficulty breathing, or you are concerned that it may be a sign of a more serious illness (see other common causes of coughs in children), contact your child's pediatrician as soon as possible.
Get care now
We know that getting sick is never convenient. But now you can videoconference with a health care provider 24 hours a day, 7 days a week with Virtual Visit by Children's Health Virtual Care. Get treated right from your smartphone, tablet or computer for allergies, common colds and flu, cuts and more. Download the Virtual Visit app today.
Children’s Health Family Newsletter
Get health tips and parenting advice from Children’s Health experts sent straight to your inbox twice a month. Sign up now.
Sign up now.
breathing, cold and flu season, common cold, cough medicine, fever, respiratory, treatment, virus
Childrens Healththe pediatrician told how to help him - article on TSK
Night cough attacks deprive the child of sleep and do not allow the body to restore the forces needed to fight the disease. Of course, mothers are trying in every way to alleviate this unpleasant symptom. The problem is that this does not always work out, and the wrong actions can provoke an even more severe attack.
Pediatrician Yekaterina Volkova told how to understand the cause of a nighttime cough and provide a child of any age with the right help.
What the body defends against by coughing
Cough is not a disease. This is a symptom that indicates a problem, a natural reflex reaction that protects the body, helps the lungs get rid of the irritant and restore normal breathing. This means that we must fight with what irritates: a foreign body, mucus, dust, a pungent odor, and so on.
This means that we must fight with what irritates: a foreign body, mucus, dust, a pungent odor, and so on.
Main causes of coughing attacks in children:
- acute respiratory diseases (viral and bacterial),
- Allergic reactions,
- Dry Air,
- teeth teething,
- Bronchial asthma,
- A foreign body in the respiratory tract,
- Diseases and anomalies of the development of the gastrointestinal tract,
- heart disease,
- Available in the air of the harmful air. substances.
Increasing cough at night occurs because at this time the blood circulation of organs and tissues slows down, sputum dissolves slowly and accumulates in the respiratory tract. Also, attacks often occur in the morning, when the child takes an upright position and coughs up what has accumulated during the night.
How to relieve night coughing
The first thing parents should do if a child starts coughing at night is to try to understand what is the reason. Your task is to relieve the symptom and go to the doctor in the morning for advice or an appointment.
Your task is to relieve the symptom and go to the doctor in the morning for advice or an appointment.
If the baby is teething
The cough in this case is often caused by increased salivation. You can alleviate the symptom by changing the position of the child. Try elevating the mattress or crib on the side of your head (for example, by placing a couple of books under the legs). So the head will be higher, and the child will not choke on saliva.
Don't put babies on pillows: babies who haven't learned to roll over with confidence risk suffocating when they bury their nose in it. In principle, a child up to a year in a crib should not have anything other than a mattress and a sheet with an elastic band.
If the child is sick
The golden rule, relevant for almost all illnesses, is to drink plenty of warm liquids throughout the day. This will help soothe an irritated throat, reduce the thickness of blood and the viscosity of sputum. It will be easier for the child to cough.
Breastfed babies should be offered the breast more often if they are sick. This will also avoid overdrying of the throat mucosa.
Severe runny nose often provokes nocturnal coughs. Make sure that the child can breathe freely through the nose. Before going to bed, the sinuses must be washed out: for example, with a light saline solution or special means. Try offering your child a higher pillow: this measure also helps to reduce the frequency of coughing.
Circular stroking movements on the back in the area of the bronchi reduce discomfort and soothe the child, and at the same time improve blood circulation and relieve spasm. Warming ointments also have a similar property. The method should be used for children older than three years with the so-called residual cough.
Keep your child's feet warm. The warmer the feet, the more blood will flow to them, which means that the swelling in the lungs will decrease. However, be careful: woolen socks and heating pads are acceptable only if the child does not have a high fever.
All the methods described can only relieve the symptom for a short time. Adequate treatment, suitable drugs and dosage should be prescribed by a doctor.
If the cause of the nighttime cough is not obvious
Try changing the climate in the room. For comfortable breathing and cough relief, a temperature of +21 ° C and air humidity up to 50–60% are recommended. Turn on the ionizer or air humidifier, spread wet towels on the radiator, do wet cleaning - all this makes breathing easier. Do not be afraid to open a window or turn on the air conditioner: dry air is more dangerous for a coughing baby. If you're worried, put your child in pajamas and warm socks. However, do not overdo it: too cold air can backfire, and the baby will begin to cough due to spasm when inhaling.
Another non-obvious reason for coughing can be allergies. Perhaps you recently changed your laundry detergent or installed a room air freshener, put in a new pillow or toy with an untested filler. The smell does not have to be strong for the baby to react to it with a cough. Watery eyes and puffiness will tell you that the cough is due to an allergic reaction.
The smell does not have to be strong for the baby to react to it with a cough. Watery eyes and puffiness will tell you that the cough is due to an allergic reaction.
What not to do during a nocturnal cough
- If the cough is accompanied by severe rhinitis (runny nose), do not immediately before going to bed, and even more so at night, instill vasoconstrictor drops into the child's nose. They dry out the mucous membrane and can additionally provoke a cough. The procedure is best done an hour before bedtime.
- Expectorants should not be given to the child during attacks of dry cough. They will provoke new spasms, but the cough will not become “more productive”.
- With a wet cough, on the contrary, it is not necessary to prevent the child from coughing, squeezing the urge with antitussives.
- Inhalations and rubbing are not allowed for babies under six months.
- Never give children antibiotics without a doctor's prescription. Self-medication is dangerous and can cause serious complications.
The main thing to remember is that a doctor should treat a child. The task of parents is to notice the symptoms, provide first aid and carefully monitor all manifestations and reactions in order to describe them in detail to a specialist.
Good night to you and your children!
Etiquette or rules of conduct when coughing
Cough is a frequent and rather loud companion of colds.
It interferes with sleep, work...and not only for the person with a cold, but also for those around him.
Cough loudly draws attention to itself, breaking the silence in the cinema, theater, restaurant and other public places, wherever the person goes and whatever he does.
But besides the fact that a cough is an obvious manifestation of a cold, it also serves as a way to spread it. This is due to the fact that when coughing, as well as when sneezing, along with the air flow, the smallest droplets of saliva and sputum enter the surrounding space, inside which pathogenic microorganisms can also be found - pathogens of respiratory infectious diseases. Due to the fact that the cough is a strong forced expiration through the mouth, the range of spread of sputum and saliva particles can reach 2 meters at a speed of up to 800 km/h.
In poorly ventilated enclosed spaces, germs can survive for several hours. When breathing, they enter the body of a healthy person, contributing to infection and the risk of developing colds. This is how, mainly by airborne droplets, pathogens spread in acute respiratory viral infections, including influenza and SARS of a non-influenza nature. Through coughing and sneezing, the infection spreads very quickly.
To reduce the risk of further spread of infection, it is important to know, remember and follow a few simple yet important rules that make up the actual etiquette or cough hygiene.
RULE #1
When coughing or sneezing, turn away from others by tilting your head down. Mouth and face must be covered with a handkerchief, which a cold person must have with him. The handkerchief itself does not need to be squeezed, wrinkled or crumple. It should be well straightened so that after it can be neatly rolled up. It is optimal if disposable paper napkins or handkerchiefs take over the function of the handkerchief. Today they can be bought everywhere, and after use it is not a pity to immediately throw them away.
The handkerchief itself does not need to be squeezed, wrinkled or crumple. It should be well straightened so that after it can be neatly rolled up. It is optimal if disposable paper napkins or handkerchiefs take over the function of the handkerchief. Today they can be bought everywhere, and after use it is not a pity to immediately throw them away.
RULE #2
In the absence of a handkerchief, do not cough into the palm or fist, especially the right hand. The traditional covering of the mouth with the palm of the hand only contributes to the further spread of the infection through the hands and household items. After all, most people greet with their right hand, take some objects, hold on to the handrails in transport, open doors and doors. When coughing, it is better to use the elbow or the back of the left hand.
RULE #3
When you have a wet cough, don't spit phlegm anywhere. Use only disposable handkerchiefs or paper napkins. In traditional fabric handkerchiefs, microbes are warm, damp and "cozy", they will live there for a long time, exposing them to the risk of re-infection. Do not scatter used handkerchiefs and napkins around the apartment or on the surface of the desktop. Throw them in the wastebasket immediately. If, out of habit, you can't refuse cloth handkerchiefs, put them in a plastic bag before putting them in your pocket or purse.
In traditional fabric handkerchiefs, microbes are warm, damp and "cozy", they will live there for a long time, exposing them to the risk of re-infection. Do not scatter used handkerchiefs and napkins around the apartment or on the surface of the desktop. Throw them in the wastebasket immediately. If, out of habit, you can't refuse cloth handkerchiefs, put them in a plastic bag before putting them in your pocket or purse.
RULE #4
If you catch a cold, cough or sneeze, limit contact with other people as much as possible. The most correct decision in this case from the point of view of etiquette is to take a sick leave. After all, your cold not only interferes with colleagues with constant coughing, sneezing or sniffing, but also poses a real threat of infection. If circumstances require your presence at the workplace, it is recommended to wear a medical mask in order not to spread the infection and reduce the risk of infecting others. It should be remembered that medical masks must be changed at least every 2 hours.
RULE #5
Wash your hands frequently and avoid touching your face, lips, nose and eyes. After coughing, regardless of whether you splashed your palm or not, it is recommended to immediately wash your hands. Wash your hands with warm water, use antibacterial soap, and use alcohol-based hand cleaners. Today, many people prefer to always have special gel “sanitizers” with them; you can buy them anywhere.
The above 5 rules form the basis of the etiquette of human behavior when coughing. Compliance with these simple rules will allow a cold to reduce the risk of infecting others. Compliance with these rules is especially important in public places (business centers, retail outlets, places of public entertainment of a closed type, etc.), where there is a large crowd of people, as well as in public transport, places of concentrated stay of children and adults - children's preschool and school organizations , educational, medical institutions, etc.
If someone is coughing near you, if possible, move to the side, turn away, and tilt your head slightly down. If you have a child with you, take him aside, turn away from the coughing one. Try not to stay long in a room where someone is coughing. Ventilate it more often, even arrange drafts. Feel free and remember to talk about cough hygiene with any coughing person.
And most importantly, don't start coughing! Seek help from experts in a timely manner. Do not allow the "lowering" of the cough in the lower parts of the respiratory tract and the development of complications. When choosing a cough remedy in a situation where you cannot consult a doctor, remember that each type of cough - dry and wet - requires its own differentiated approach to treatment. With a dry cough, it is important to stop the cough and alleviate the condition, with a wet cough, it is important to ensure that the sputum passes into a liquid state for better discharge. The use of cough blocking agents for wet cough with sputum carries a potential risk of complications.