Newborn scoring system
The Apgar Score | ACOG
Number 644 (Replaces Committee Opinion Number 333, May 2006. Reaffirmed 2021)
Committee on Obstetric Practice
American Academy of Pediatrics—Committee on Fetus and Newborn
This document reflects emerging clinical and scientific advances as of the date issued and is subject to change. The information should not be construed as dictating an exclusive course of treatment or procedure to be followed. This document reflects emerging concepts on patient safety and is subject to change. The information should not be construed as dictating an exclusive course of treatment or procedure to be followed.
ABSTRACT: The Apgar score provides an accepted and convenient method for reporting the status of the newborn infant immediately after birth and the response to resuscitation if needed. The Apgar score alone cannot be considered to be evidence of or a consequence of asphyxia, does not predict individual neonatal mortality or neurologic outcome, and should not be used for that purpose. An Apgar score assigned during a resuscitation is not equivalent to a score assigned to a spontaneously breathing infant. The American Academy of Pediatrics and the American College of Obstetricians and Gynecologists encourage use of an expanded Apgar score reporting form that accounts for concurrent resuscitative interventions.
Introduction
In 1952, Dr. Virginia Apgar devised a scoring system that was a rapid method of assessing the clinical status of the newborn infant at 1 minute of age and the need for prompt intervention to establish breathing 1. A second report evaluating a larger number of patients was published in 1958 2. This scoring system provided a standardized assessment for infants after delivery. The Apgar score comprises five components: 1) color, 2) heart rate, 3) reflexes, 4) muscle tone, and 5) respiration, each of which is given a score of 0, 1, or 2. Thus, the Apgar score quantitates clinical signs of neonatal depression such as cyanosis or pallor, bradycardia, depressed reflex response to stimulation, hypotonia, and apnea or gasping respirations. The score is reported at 1 minute and 5 minutes after birth for all infants, and at 5-minute intervals thereafter until 20 minutes for infants with a score less than 7 3. The Apgar score provides an accepted and convenient method for reporting the status of the newborn infant immediately after birth and the response to resuscitation if needed; however, it has been inappropriately used to predict individual adverse neurologic outcome. The purpose of this statement is to place the Apgar score in its proper perspective. This statement revises the 2006 College Committee Opinion and AAP Policy Statement to include updated guidance from Neonatal Encephalopathy and Neurologic Outcome, Second Edition, along with new guidance on neonatal resuscitation.
The score is reported at 1 minute and 5 minutes after birth for all infants, and at 5-minute intervals thereafter until 20 minutes for infants with a score less than 7 3. The Apgar score provides an accepted and convenient method for reporting the status of the newborn infant immediately after birth and the response to resuscitation if needed; however, it has been inappropriately used to predict individual adverse neurologic outcome. The purpose of this statement is to place the Apgar score in its proper perspective. This statement revises the 2006 College Committee Opinion and AAP Policy Statement to include updated guidance from Neonatal Encephalopathy and Neurologic Outcome, Second Edition, along with new guidance on neonatal resuscitation.
The Neonatal Resuscitation Program guidelines state that the Apgar score is
useful for conveying information about the newborn’s overall status and response to resuscitation. However, resuscitation must be initiated before the 1-minute score is assigned. Therefore, the Apgar score is not used to determine the need for initial resuscitation, what resuscitation steps are necessary, or when to use them 3.
Therefore, the Apgar score is not used to determine the need for initial resuscitation, what resuscitation steps are necessary, or when to use them 3.
An Apgar score that remains 0 beyond 10 minutes of age may, however, be useful in determining whether continued resuscitative efforts are indicated because very few infants with an Apgar score of 0 at 10 minutes have been reported to survive with a normal neurologic outcome 3 4 5. In line with this, the 2011 Neonatal Resuscitation Program guidelines state that “if you can confirm that no heart rate has been detectable for at least 10 minutes, discontinuation of resuscitative efforts may be appropriate” 3.
Neonatal Encephalopathy and Neurologic Outcome, Second Edition, published in 2014 by the College in collaboration with the AAP, defines a 5-minute Apgar score of 7–10 as reassuring, a score of 4–6 as moderately abnormal, and a score of 0–3 as low in the term infant and late-preterm infant 6. That document considers an Apgar score of 0–3 at 5 minutes or more as a nonspecific sign of illness, which “may be one of the first indications of encephalopathy” 6. However, a persistently low Apgar score alone is not a specific indicator for intrapartum compromise. Further, although the score is used widely in outcome studies, its inappropriate use has led to an erroneous definition of asphyxia. Asphyxia is defined as the marked impairment of gas exchange leading, if prolonged, to progressive hypoxemia, hypercapnia, and significant metabolic acidosis. The term asphyxia, which describes a process of varying severity and duration rather than an end point, should not be applied to birth events unless specific evidence of markedly impaired intrapartum or immediate postnatal gas exchange can be documented based on laboratory testing 6.
However, a persistently low Apgar score alone is not a specific indicator for intrapartum compromise. Further, although the score is used widely in outcome studies, its inappropriate use has led to an erroneous definition of asphyxia. Asphyxia is defined as the marked impairment of gas exchange leading, if prolonged, to progressive hypoxemia, hypercapnia, and significant metabolic acidosis. The term asphyxia, which describes a process of varying severity and duration rather than an end point, should not be applied to birth events unless specific evidence of markedly impaired intrapartum or immediate postnatal gas exchange can be documented based on laboratory testing 6.
Limitations of the Apgar Score
It is important to recognize the limitations of the Apgar score. The Apgar score is an expression of the infant’s physiologic condition at one point in time, which includes subjective components. There are numerous factors that can influence the Apgar score, including maternal sedation or anesthesia, congenital malformations, gestational age, trauma, and interobserver variability 6. In addition, the biochemical disturbance must be significant before the score is affected. Elements of the score such as tone, color, and reflex irritability can be subjective, and partially depend on the physiologic maturity of the infant. The score also may be affected by variations in normal transition. For example, lower initial oxygen saturations in the first few minutes need not prompt immediate supplemental oxygen administration; the Neonatal Resuscitation Program targets for oxygen saturation are 60–65% at 1 minute and 80–85% at 5 minutes 3. The healthy preterm infant with no evidence of asphyxia may receive a low score only because of immaturity 7 8. The incidence of low Apgar scores is inversely related to birth weight, and a low score cannot predict morbidity or mortality for any individual infant 8 9. As previously stated, it also is inappropriate to use an Apgar score alone to diagnose asphyxia.
In addition, the biochemical disturbance must be significant before the score is affected. Elements of the score such as tone, color, and reflex irritability can be subjective, and partially depend on the physiologic maturity of the infant. The score also may be affected by variations in normal transition. For example, lower initial oxygen saturations in the first few minutes need not prompt immediate supplemental oxygen administration; the Neonatal Resuscitation Program targets for oxygen saturation are 60–65% at 1 minute and 80–85% at 5 minutes 3. The healthy preterm infant with no evidence of asphyxia may receive a low score only because of immaturity 7 8. The incidence of low Apgar scores is inversely related to birth weight, and a low score cannot predict morbidity or mortality for any individual infant 8 9. As previously stated, it also is inappropriate to use an Apgar score alone to diagnose asphyxia.
Apgar Score and Resuscitation
The 5-minute Apgar score, and particularly a change in the score between 1 minute and 5 minutes, is a useful index of the response to resuscitation.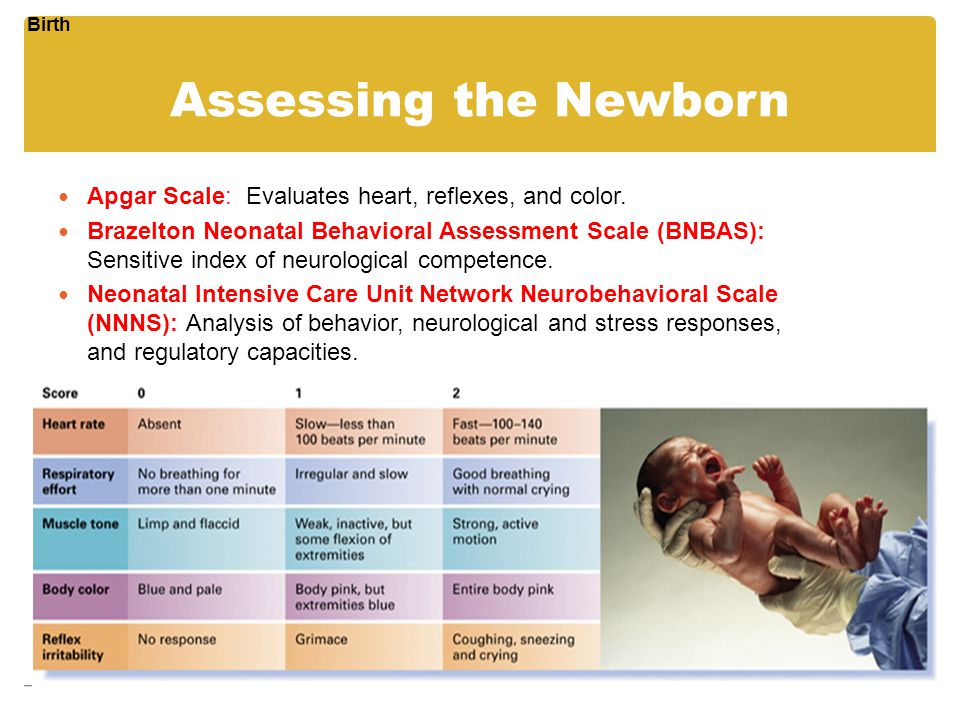 If the Apgar score is less than 7 at 5 minutes, the Neonatal Resuscitation Program guidelines state that the assessment should be repeated every 5 minutes for up to 20 minutes 3. However, an Apgar score assigned during a resuscitation is not equivalent to a score assigned to a spontaneously breathing infant 10. There is no accepted standard for reporting an Apgar score in infants undergoing resuscitation after birth because many of the elements contributing to the score are altered by resuscitation. The concept of an assisted score that accounts for resuscitative interventions has been suggested, but the predictive reliability has not been studied. In order to correctly describe such infants and provide accurate documentation and data collection, an expanded Apgar score report form is encouraged Figure 1. This expanded Apgar score also may prove to be useful in the setting of delayed cord clamping, where the time of birth (complete delivery of the infant), the time of cord clamping, and the time of initiation of resuscitation all can be recorded in the comments box.
If the Apgar score is less than 7 at 5 minutes, the Neonatal Resuscitation Program guidelines state that the assessment should be repeated every 5 minutes for up to 20 minutes 3. However, an Apgar score assigned during a resuscitation is not equivalent to a score assigned to a spontaneously breathing infant 10. There is no accepted standard for reporting an Apgar score in infants undergoing resuscitation after birth because many of the elements contributing to the score are altered by resuscitation. The concept of an assisted score that accounts for resuscitative interventions has been suggested, but the predictive reliability has not been studied. In order to correctly describe such infants and provide accurate documentation and data collection, an expanded Apgar score report form is encouraged Figure 1. This expanded Apgar score also may prove to be useful in the setting of delayed cord clamping, where the time of birth (complete delivery of the infant), the time of cord clamping, and the time of initiation of resuscitation all can be recorded in the comments box.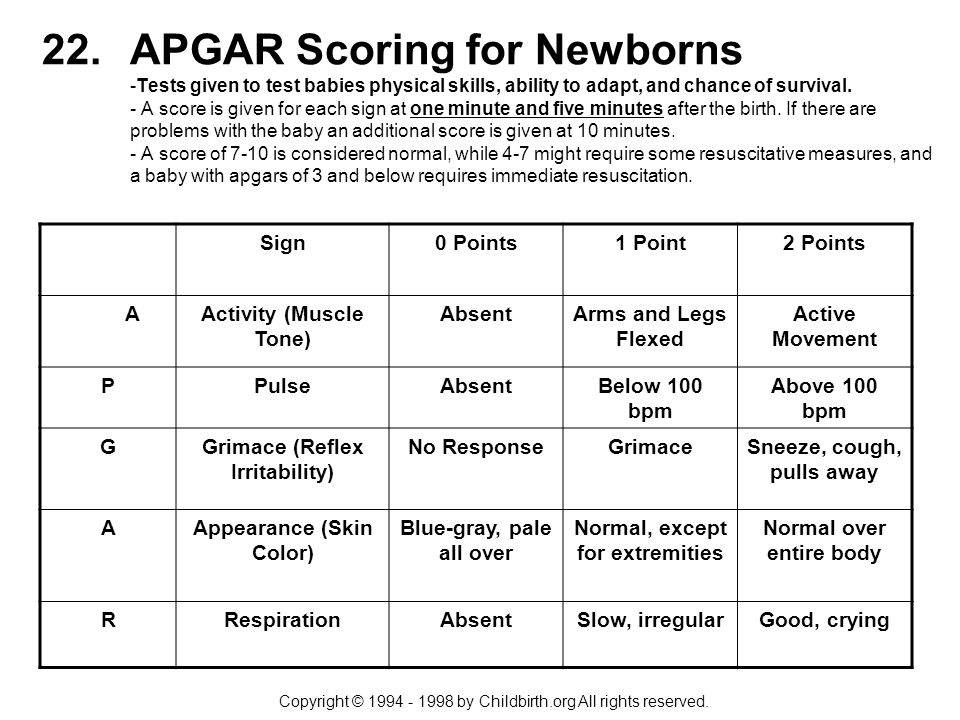
The Apgar score alone cannot be considered to be evidence of or a consequence of asphyxia. Many other factors, including nonreassuring fetal heart rate monitoring patterns and abnormalities in umbilical arterial blood gases, clinical cerebral function, neuroimaging studies, neonatal electroencephalography, placental pathology, hematologic studies, and multisystem organ dysfunction need to be considered in diagnosing an intrapartum hypoxic–ischemic event 5. When a Category I (normal) or Category II (indeterminate) fetal heart rate tracing is associated with Apgar scores of 7 or higher at 5 minutes, a normal umbilical cord arterial blood pH (± 1 standard deviation), or both, it is not consistent with an acute hypoxic–ischemic event 6.
Prediction of Outcome
A 1-minute Apgar score of 0–3 does not predict any individual infant’s outcome. A 5-minute Apgar score of 0–3 correlates with neonatal mortality in large populations 11 12, but does not predict individual future neurologic dysfunction. Population studies have uniformly reassured us that most infants with low Apgar scores will not develop cerebral palsy. However, a low 5-minute Apgar score clearly confers an increased relative risk of cerebral palsy, reported to be as high as 20-fold to 100-fold over that of infants with a 5-minute Apgar score of 7–10 9 13 14 15. Although individual risk varies, the population risk of poor neurologic outcomes also increases when the Apgar score is 3 or less at 10 minutes, 15 minutes, and 20 minutes 16. When a newborn has an Apgar score of 5 or less at 5 minutes, umbilical artery blood gas from a clamped section of the umbilical cord should be obtained, if possible 17. Submitting the placenta for pathologic examination may be valuable.
Population studies have uniformly reassured us that most infants with low Apgar scores will not develop cerebral palsy. However, a low 5-minute Apgar score clearly confers an increased relative risk of cerebral palsy, reported to be as high as 20-fold to 100-fold over that of infants with a 5-minute Apgar score of 7–10 9 13 14 15. Although individual risk varies, the population risk of poor neurologic outcomes also increases when the Apgar score is 3 or less at 10 minutes, 15 minutes, and 20 minutes 16. When a newborn has an Apgar score of 5 or less at 5 minutes, umbilical artery blood gas from a clamped section of the umbilical cord should be obtained, if possible 17. Submitting the placenta for pathologic examination may be valuable.
Other Applications
Monitoring of low Apgar scores from a delivery service can be useful. Individual case reviews can identify needs for focused educational programs and improvement in systems of perinatal care. Analyzing trends allows for the assessment of the effect of quality improvement interventions.
Conclusions
The Apgar score describes the condition of the newborn infant immediately after birth and, when properly applied, is a tool for standardized assessment 18. It also provides a mechanism to record fetal-to-neonatal transition. Apgar scores do not predict individual mortality or adverse neurologic outcome. However, based on population studies, Apgar scores of less than 5 at 5 minutes and 10 minutes clearly confer an increased relative risk of cerebral palsy, and the degree of abnormality correlates with the risk of cerebral palsy. Most infants with low Apgar scores, however, will not develop cerebral palsy. The Apgar score is affected by many factors, including gestational age, maternal medications, resuscitation, and cardiorespiratory and neurologic conditions. If the Apgar score at 5 minutes is 7 or greater, it is unlikely that peripartum hypoxia–ischemia caused neonatal encephalopathy.
Recommendations
The Apgar score does not predict individual neonatal mortality or neurologic outcome, and should not be used for that purpose.
It is inappropriate to use the Apgar score alone to establish the diagnosis of asphyxia. The term asphyxia, which describes a process of varying severity and duration rather than an end point, should not be applied to birth events unless specific evidence of markedly impaired intrapartum or immediate postnatal gas exchange can be can be documented.
When a newborn has an Apgar score of 5 or less at 5 minutes, umbilical artery blood gas from a clamped section of umbilical cord should be obtained. Submitting the placenta for pathologic examination may be valuable.
Perinatal health care professionals should be consistent in assigning an Apgar score during resuscitation; therefore, the American Academy of Pediatrics (AAP) and the American College of Obstetricians and Gynecologists (the College) encourage use of an expanded Apgar score reporting form that accounts for concurrent resuscitative interventions.
Full text document also published in Pediatrics.
Copyright October 2015 by the American College of Obstetricians and Gynecologists, 409 12th Street, SW, PO Box 96920, Washington, DC 20090-6920 and the American Academy of Pediatrics, 141 Northwest Point Boulevard, PO Box 927, Elk Grove Village, IL 60009-0927. All rights reserved.
ISSN 1074-861X
The Apgar score. Committee Opinion No. 644. American College of Obstetricians and Gynecologists. Obstet Gynecol 2015;126:e52–5.
Apgar score: MedlinePlus Medical Encyclopedia
URL of this page: //medlineplus.gov/ency/article/003402.htm
To use the sharing features on this page, please enable JavaScript.
Apgar is a quick test performed on a baby at 1 and 5 minutes after birth. The 1-minute score determines how well the baby tolerated the birthing process. The 5-minute score tells the health care provider how well the baby is doing outside the mother's womb.
In rare cases, the test will be done 10 minutes after birth.
Virginia Apgar, MD (1909-1974) introduced the Apgar score in 1952.
The Apgar test is done by a doctor, midwife, or nurse. The provider examines the baby's:
- Breathing effort
- Heart rate
- Muscle tone
- Reflexes
- Skin color
Each category is scored with 0, 1, or 2, depending on the observed condition.
Breathing effort:
- If the infant is not breathing, the respiratory score is 0.
- If the respirations are slow or irregular, the infant scores 1 for respiratory effort.
- If the infant cries well, the respiratory score is 2.
Heart rate is evaluated by stethoscope. This is the most important assessment:
- If there is no heartbeat, the infant scores 0 for heart rate.
- If heart rate is less than 100 beats per minute, the infant scores 1 for heart rate.
- If heart rate is greater than 100 beats per minute, the infant scores 2 for heart rate.
Muscle tone:
- If muscles are loose and floppy, the infant scores 0 for muscle tone.
- If there is some muscle tone, the infant scores 1.
- If there is active motion, the infant scores 2 for muscle tone.
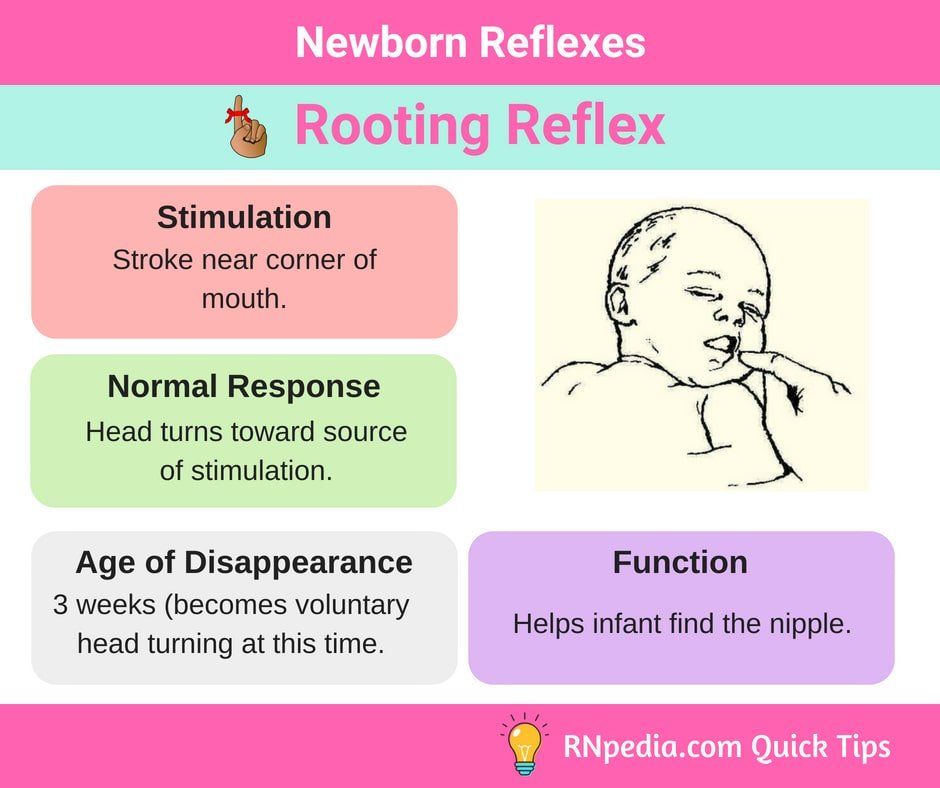
Grimace response or reflex irritability is a term describing response to stimulation, such as a mild pinch:
- If there is no reaction, the infant scores 0 for reflex irritability.
- If there is grimacing, the infant scores 1 for reflex irritability.
- If there is grimacing and a cough, sneeze, or vigorous cry, the infant scores 2 for reflex irritability.
Skin color:
- If the skin color is pale blue, the infant scores 0 for color.
- If the body is pink and the extremities are blue, the infant scores 1 for color.
- If the entire body is pink, the infant scores 2 for color.
This test is done to determine whether a newborn needs help breathing or is having heart trouble.
The Apgar score is based on a total score of 1 to 10. The higher the score, the better the baby is doing after birth.
The higher the score, the better the baby is doing after birth.
A score of 7, 8, or 9 is normal and is a sign that the newborn is in good health. A score of 10 is very unusual, since almost all newborns lose 1 point for blue hands and feet, which is normal for after birth.
Any score lower than 7 is a sign that the baby needs medical attention. The lower the score, the more help the baby needs to adjust outside the mother's womb.
Most of the time a low Apgar score is caused by:
- Difficult birth
- C-section
- Fluid in the baby's airway
A baby with a low Apgar score may need:
- Oxygen and clearing out the airway to help with breathing
- Physical stimulation to get the heart beating at a healthy rate
Most of the time, a low score at 1 minute is near-normal by 5 minutes.
A lower Apgar score does not mean a child will have serious or long-term health problems. The Apgar score is not designed to predict the future health of the child.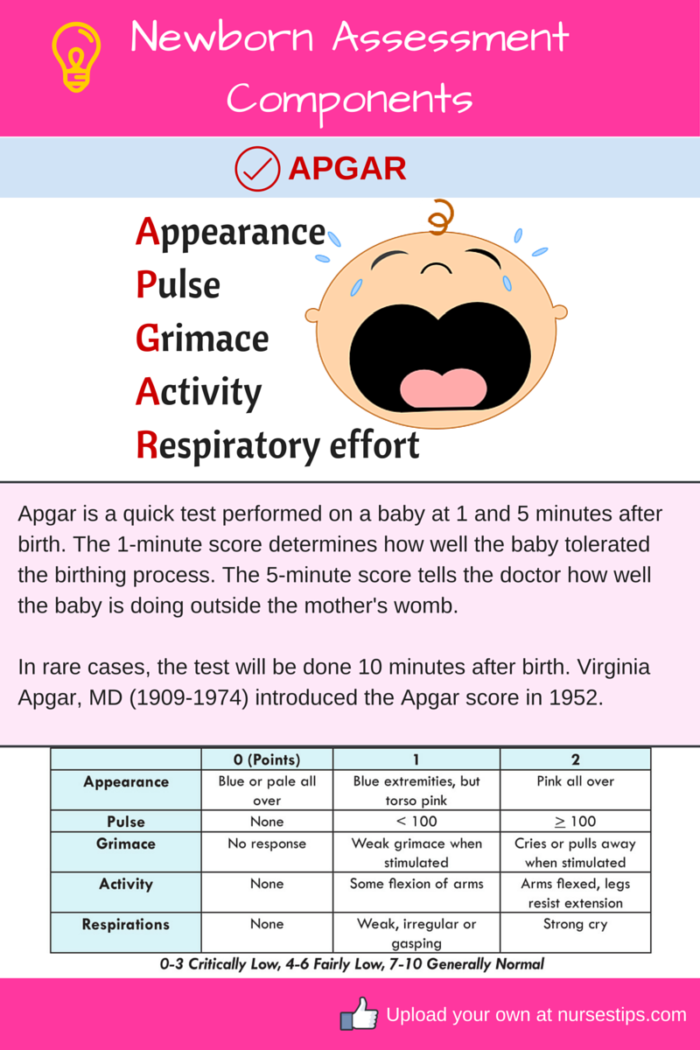
Newborn scoring; Delivery - Apgar
- Infant care following delivery
- Newborn test
Arulkumaran S. Fetal surveillance in labor. In: Arulkumaran SS, Robson MS, eds. Munro Kerr's Operative Obstetrics. 13th ed. Philadelphia, PA: Elsevier; 2020:chap 9.
Goyal NK. The newborn infant. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 113.
Updated by: Neil K. Kaneshiro, MD, MHA, Clinical Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
A neonatologist from St. Petersburg State Pediatric Medical University explained how a newborn is assessed on the Apgar scale
What do the scores on the scale say and whether it is possible to judge the future development of the baby from them to the portal "Doctor Piter" Larisa Fedorova, associate professor of the department of neonatology of St.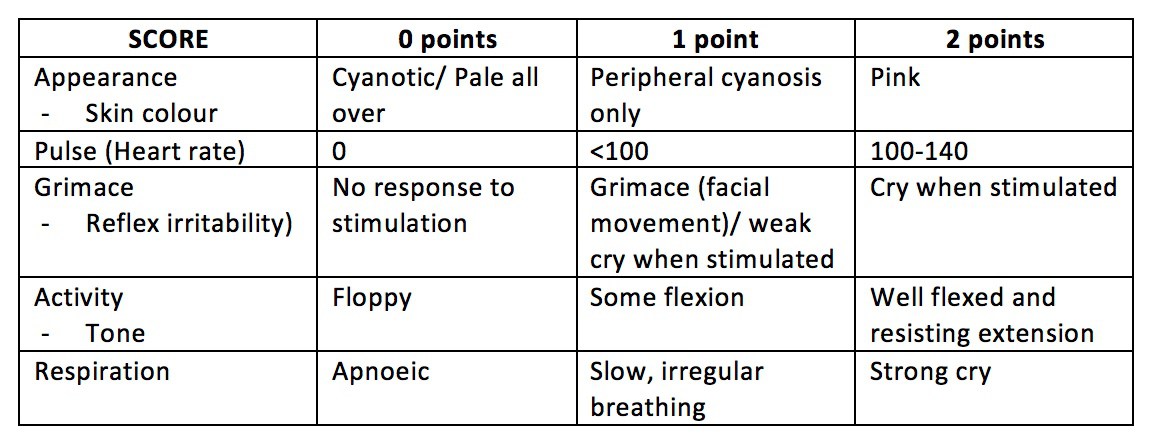 Petersburg State Pediatric Medical University 9002
Petersburg State Pediatric Medical University 9002
In essence, the Apgar scale shows whether a newly born baby needs medical help here and now. The peculiarity of such screening is that it does not require any special equipment - the assessment is given, as they say, "by eye", quickly and accurately.
The scale consists of 5 blocks:
- skin color
- heart rate
- reflex excitability (reaction to external stimuli)
- muscle tone
- breath
Doctors assess the child's condition twice - at the end of the first and fifth minutes of life, so the points obtained are written through a slash 6/7 or 8/9. According to Larisa Fedorova, a neonatologist at St. Petersburg State Pediatric Medical University, 7 points and more fall within the normal range. At the same time, it is desirable that the second assessment be higher than the first, because after birth, the child does not immediately adapt to a new world for himself. Positive dynamics is important.
Petersburg State Pediatric Medical University, 7 points and more fall within the normal range. At the same time, it is desirable that the second assessment be higher than the first, because after birth, the child does not immediately adapt to a new world for himself. Positive dynamics is important.
| — If one child got 7 points in the first minute of life, and the other 9 - this is absolutely no reason for parents to worry. The second mark - at the fifth minute - should be higher than the first one, but if it is 8/8, it's also not bad. The indicators are below 7 - it doesn’t matter if they are different or the same, they are already signaling that the child needs the help of doctors. In general, three degrees of the condition of the newborn are distinguished: normal (if the score at the 5th minute reaches 7-10 points), moderate (4-6 points) and severe (1-3 points), - explains the doctor. |
Why do doctors take into account the first 5 minutes of life, and not 7 or 10, when assessing the Apgar scale? According to the neonatologist, studies have shown that this time period is most informative in relation to the outcome: if, with an initially serious condition of the newborn, after 5 minutes it was not possible to improve the performance, complications or even death may develop. According to the doctor, the Apgar scale alone is not enough to fully assess the severity of the condition of the newborn.
| - The scale is good for quick screening. Of course, in the process of childbirth, neonatologists also focus on other indicators - we evaluate everything as a whole. For example, if necessary, we look at the gas composition of the blood - the level of oxygenation (oxygen saturation - ed. |
All material Read the link >>>
Date of publication: 23. 08.2021
9000APAGA specialists - Articles from the Clinic "Mother and Die"
baby's first assessments
As soon as a baby is born, doctors immediately evaluate his condition and physical development. But not only weight and height are measured for the baby, there are other characteristics by which one can judge how healthy the child is. To do this, use a special scale proposed by the anesthesiologist Virginia Apgar and named after her.
why
The Apgar score is used to determine which children need more attention. According to this scale, the health status of each newborn is assessed on five indicators: heart rate, respiration, muscle tone, reflexes and skin color of the baby.
The Apgar score, whether it be high or low, is not a diagnosis. This is a signal for the doctor about what measures are now needed or, conversely, the child does not need. Depending on the results of the assessment, an additional examination may be prescribed: blood tests, urine tests, a study for intrauterine infections, ultrasound, neurosonography. And after that, it is decided what to do next - to observe or treat the child.
how to test
During examination, each symptom (heart rate, respiration, muscle tone, reflexes, and skin color) is given 0, 1, or 2 points. A score of 2 points in the delivery room is considered the highest and means that the sign is pronounced, 1 point - weakly expressed, 0 points - the sign is absent.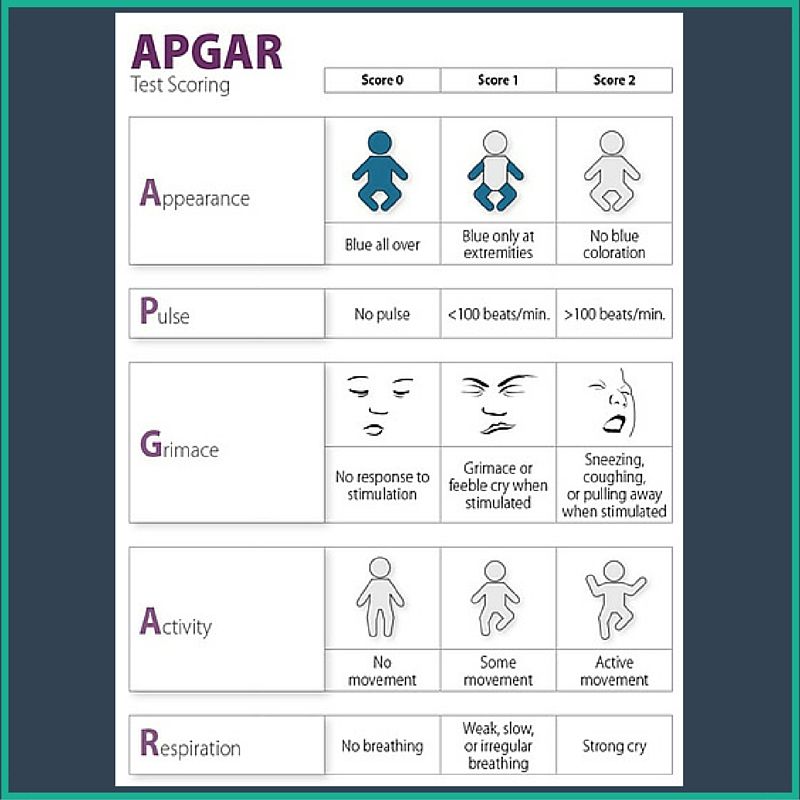 The child is evaluated on the Apgar scale at the 1st and 5th minutes of life, so there are always two scores, for example, 8/9 points or 9/10 points. Children rarely score the maximum 10 points in the first minute of life, and usually the first score is always lower than the second. But the second assessment can just be equal to 10 points.
The child is evaluated on the Apgar scale at the 1st and 5th minutes of life, so there are always two scores, for example, 8/9 points or 9/10 points. Children rarely score the maximum 10 points in the first minute of life, and usually the first score is always lower than the second. But the second assessment can just be equal to 10 points.
evaluation criteria
| 0 points | 1 point | 2 points | |
| Pulse | Missing | Less than 100 bpm | Over 100 bpm |
| Breathing | Missing | Slow, irregular | Good, cry |
| Muscle tone | Weak | Bends arms and legs | Actively moving |
| Reflexes | Missing | Weakly expressed | Called |
| Skin color | Blue, pale | Normal but bluish arms and legs | Normal throughout the body |
counting points
Children who score between 7 and 10 are considered to be in good condition and usually require only routine care. Those who score between 4 and 6 are in fair condition and may only need some resuscitation. Immediate life-saving assistance is needed for those who score below 4.
Those who score between 4 and 6 are in fair condition and may only need some resuscitation. Immediate life-saving assistance is needed for those who score below 4.
| Points | Result |
| 10–7 | Optimal, norm |
| 5-6 | Minor health problems |
| 3-4 | Average deviations in health status |
| 0–2 | Severe deviations in health |
let's be objective
In general, the Apgar score, although it is set according to objective criteria, still does not give an absolutely accurate forecast of the child's health in the future. It cannot be unequivocally said that a newborn who was given a 9or 10 Apgar scores, healthier than someone who got only 7 points. This only means that in the first case the baby breathes normally, he has pink skin and mucous membranes, he screams loudly enough, he has well-defined reflexes. And in the second case, one or two signs are less pronounced: for example, in the first minute the skin of the extremities is bluish, not pink, because the circulatory system takes about 5 minutes to get it working, or a healthy newborn loses points because he screams quietly in the first minutes life.
It cannot be unequivocally said that a newborn who was given a 9or 10 Apgar scores, healthier than someone who got only 7 points. This only means that in the first case the baby breathes normally, he has pink skin and mucous membranes, he screams loudly enough, he has well-defined reflexes. And in the second case, one or two signs are less pronounced: for example, in the first minute the skin of the extremities is bluish, not pink, because the circulatory system takes about 5 minutes to get it working, or a healthy newborn loses points because he screams quietly in the first minutes life.
what is important
As already mentioned, the first Apgar score is always lower than the second. In most newborns, the condition 1 minute after birth is estimated at 7-8 points on the Apgar scale, and after 5 minutes - at 8-10 points. And this suggests that the child was born in a satisfactory (normal) condition. If the Apgar score at the 1st minute is low, then the positive dynamics by the 5th minute will be important.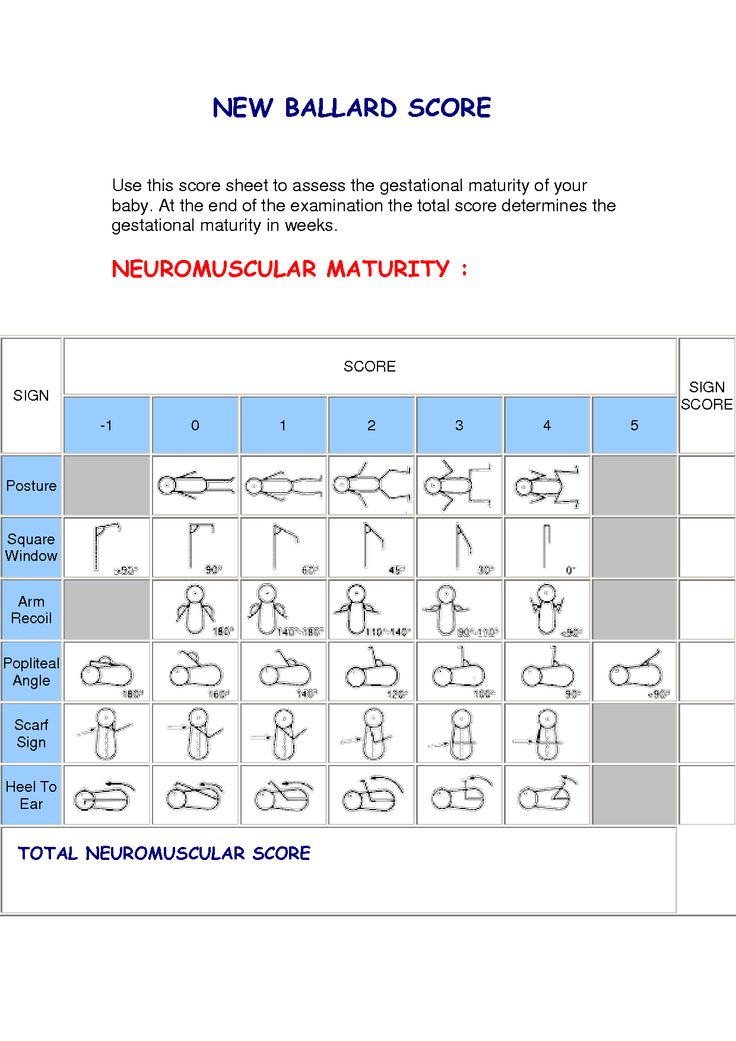 If the points increase by 2 or more by the 5th minute, then most likely the prognosis for health will be favorable. If, 5 minutes after birth, the Apgar score does not exceed 6 points, it will be necessary to conduct intensive therapy or continue resuscitation. So the main task of the Apgar scale is a quick assessment of whether a child needs medical help and how much.
If the points increase by 2 or more by the 5th minute, then most likely the prognosis for health will be favorable. If, 5 minutes after birth, the Apgar score does not exceed 6 points, it will be necessary to conduct intensive therapy or continue resuscitation. So the main task of the Apgar scale is a quick assessment of whether a child needs medical help and how much.
Whatever the Apgar score, the development of a child largely depends on love, care and upbringing in the family. So parental attention will always help the baby achieve the highest marks in life!
Children rarely score the maximum 10 points in the first minute of life, and usually the first score is always lower than the second. But the second score can just be equal to 10 points
With a low Apgar score at the 1st minute of a baby’s life, positive dynamics is extremely important - an increase of 2 or more points by the 5th minute of life
Most newborns have an Apgar score of 7–8 1 minute after birth and 8–10 Apgar scores 5 minutes later
Attention! Prices for services in different clinics may vary.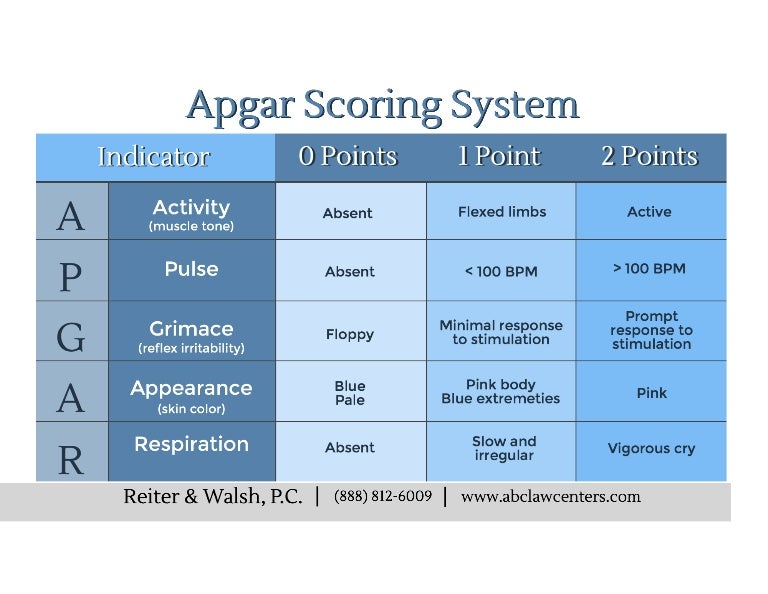 To clarify the current cost, select the clinic
To clarify the current cost, select the clinic
The administration of the clinic takes all measures to update the prices for programs in a timely manner, however, in order to avoid possible misunderstandings, we recommend that you check the cost of services by phone / with the managers of the clinic
Clinical Hospital MD GROUPClinical Hospital Lapino-1 "Mother and Child"Children's Clinic KG "Lapino" on New Riga (branch)Clinic "Mother and Child" KuntsevoClinic "Mother and Child" SavelovskayaClinic "Mother and Child" South-WestClinic "Mother and child" Novogireevo
All directionsKinesiotherapy for childrenSpecialist consultations (adults)Specialist consultations (children)Massage / manual therapy for childrenTherapeutic research
01.
Kinesiotherapy for children
02.
Consultations of specialists (adults)
03.
Consultations of specialists (children)
04.

 note), base deficiency and lactate level (a prognostic sign of neurological disorders after asphyxia suffered in utero or during childbirth - ed. note). The analysis is performed almost instantly, for this purpose in each maternity hospital there are special devices - gas analyzers, - explains specialist of the Pediatric University.
note), base deficiency and lactate level (a prognostic sign of neurological disorders after asphyxia suffered in utero or during childbirth - ed. note). The analysis is performed almost instantly, for this purpose in each maternity hospital there are special devices - gas analyzers, - explains specialist of the Pediatric University.