How to get a child diagnosed with autism
Screening and Diagnosis of Autism Spectrum Disorder
Diagnosing autism spectrum disorder (ASD) can be difficult because there is no medical test, like a blood test, to diagnose the disorder. Doctors look at the child’s developmental history and behavior to make a diagnosis.
ASD can sometimes be detected at 18 months of age or younger. By age 2, a diagnosis by an experienced professional can be considered reliable [1]. However, many children do not receive a final diagnosis until much older. Some people are not diagnosed until they are adolescents or adults. This delay means that people with ASD might not get the early help they need.
Diagnosing children with ASD as early as possible is important to make sure children receive the services and supports they need to reach their full potential [2]. There are several steps in this process.
Developmental Monitoring
Developmental monitoring is an active, ongoing process of watching a child grow and encouraging conversations between parents and providers about a child’s skills and abilities. Developmental monitoring involves observing how your child grows and whether your child meets the typical developmental milestones, or skills that most children reach by a certain age, in playing, learning, speaking, behaving, and moving.
Parents, grandparents, early childhood education providers, and other caregivers can participate in developmental monitoring. CDC’s Learn the Signs. Act Early. program has developed free materials, including CDC’s Milestone Tracker app, to help parents and providers work together to monitor your child’s development and know when there might be a concern and if more screening is needed. You can use a brief checklist of milestones to see how your child is developing. If you notice that your child is not meeting milestones, talk with your doctor or nurse about your concerns and ask about developmental screening. Learn more about CDC Milestone Tracker app, milestone checklists, and other parent materials.
When you take your child to a well visit, your doctor or nurse will also do developmental monitoring. The doctor or nurse might ask you questions about your child’s development or will talk and play with your child to see if they are developing and meeting milestones.
The doctor or nurse might ask you questions about your child’s development or will talk and play with your child to see if they are developing and meeting milestones.
Your doctor or nurse may also ask about your child’s family history. Be sure to let your doctor or nurse know about any conditions that your child’s family members have, including ASD, learning disorders, intellectual disability, or attention deficit/hyperactivity disorder (ADHD).
Developmental Screening
Developmental screening takes a closer look at how your child is developing.
Developmental screening is more formal than developmental monitoring. It is a regular part of some well-child visits even if there is not a known concern.
The American Academy of Pediatrics (AAP) recommends developmental and behavioral screening for all children during regular well-child visits at these ages:
- 9 months
- 18 months
- 30 months
In addition, AAP recommends that all children be screened specifically for ASD during regular well-child visits at these ages:
- 18 months
- 24 months
Screening questionnaires and checklists are based on research that compares your child to other children of the same age.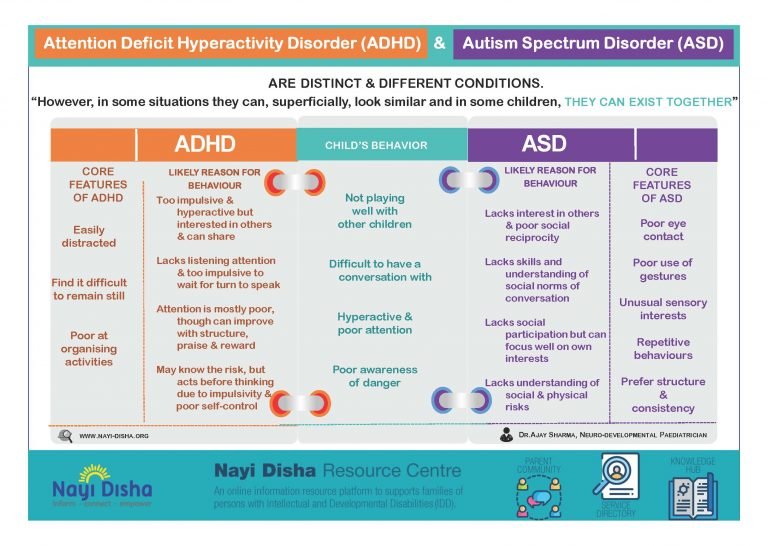 Questions may ask about language, movement, and thinking skills, as a well as behaviors and emotions. Developmental screening can be done by a doctor or nurse, or other professionals in healthcare, community, or school settings. Your doctor may ask you to complete a questionnaire as part of the screening process. Screening at times other than the recommended ages should be done if you or your doctor have a concern. Additional screening should also be done if a child is at high risk for ASD (for example, having a sibling or other family member with ASD) or if behaviors sometimes associated with ASD are present. If your child’s healthcare provider does not periodically check your child with a developmental screening test, you can ask that it be done.
Questions may ask about language, movement, and thinking skills, as a well as behaviors and emotions. Developmental screening can be done by a doctor or nurse, or other professionals in healthcare, community, or school settings. Your doctor may ask you to complete a questionnaire as part of the screening process. Screening at times other than the recommended ages should be done if you or your doctor have a concern. Additional screening should also be done if a child is at high risk for ASD (for example, having a sibling or other family member with ASD) or if behaviors sometimes associated with ASD are present. If your child’s healthcare provider does not periodically check your child with a developmental screening test, you can ask that it be done.
View and print a fact sheet on developmental monitoring and screening pdf icon[657 KB, 2 Pages, Print Only]
Developmental Diagnosis
A brief test using a screening tool does not provide a diagnosis, but it can indicate whether a child is on the right development track or if a specialist should take a closer look. If the screening tool identifies an area of concern, a formal developmental evaluation may be needed. This formal evaluation is a more in-depth look at a child’s development and is usually done by a trained specialist such as a developmental pediatrician, child psychologist, speech-language pathologist, occupational therapist, or other specialist. The specialist may observe the child give the child a structured test, ask the parents or caregivers questions, or ask them to fill out questionnaires. The results of this formal evaluation highlight your child’s strengths and challenges and can inform whether they meet criteria for a developmental diagnosis.
If the screening tool identifies an area of concern, a formal developmental evaluation may be needed. This formal evaluation is a more in-depth look at a child’s development and is usually done by a trained specialist such as a developmental pediatrician, child psychologist, speech-language pathologist, occupational therapist, or other specialist. The specialist may observe the child give the child a structured test, ask the parents or caregivers questions, or ask them to fill out questionnaires. The results of this formal evaluation highlight your child’s strengths and challenges and can inform whether they meet criteria for a developmental diagnosis.
A diagnosis of ASD now includes several conditions that used to be diagnosed separately; autistic disorder, pervasive developmental disorder not otherwise specified (PDD-NOS), and Asperger syndrome. Your doctor or other healthcare provider can help you understand and navigate the diagnostic process.
The results of a formal developmental evaluation can also inform whether your child needs early intervention services. In some cases, the specialist might recommend genetic counseling and testing for your child.
In some cases, the specialist might recommend genetic counseling and testing for your child.
References
- Lord C, Risi S, DiLavore PS, Shulman C, Thurm A, Pickles A. Autism from 2 to 9 years of age. Arch Gen Psychiatry. 2006 Jun;63(6):694-701.
- Hyman SL, Levey SE, Myers SM, Council on Children with Disabilities, Section on Developmental and Behavioral Pediatrics. Identification, Evaluation, and Management of Children With Autism Spectrum Disorder. Pediatrics. 2020 Jan;145(1).
I Think My Child May Have Autism: How to Get a Diagnosis
If you think your child has autism or your child is showing signs or symptoms of autism, it is important to have them screened. The sooner your child receives a diagnosis, the sooner they can begin needed services which can improve their outcome and quality of life.
This article will give you information about the screening and assessment processes, including:
- How to prepare for your appointment(s)
- What to do during your appointment(s)
- Answers to frequently asked questions, such as what to do if a doctor or school tells you to “wait and see”
For details about the diagnostic criteria for autism, click here.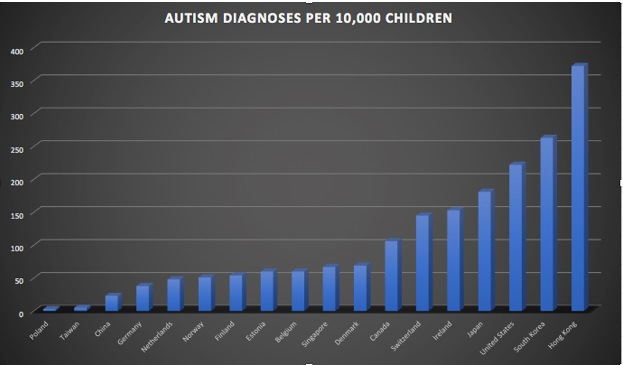
Screening vs. Assessment
Developmental Screenings
Developmental screenings are brief, informal evaluations to identify children who are at risk for developmental delays and need further evaluation. Doctors, nurses, or other professionals in healthcare, community, or school settings can perform developmental screenings.
During the screening process, your child will undergo a brief test while you complete a questionnaire. The results will help determine if your child needs to see a specialist for further evaluation.
Developmental Assessments
If areas of concern are identified in the screening process, your child will need a formal, in depth developmental assessment. Please note, developmental assessments are conducted by a trained specialist or a team of trained specialists, such as:
- Developmental Pediatricians
- Psychologists
- Psychiatrists
- Neurologists
- Occupational Therapists
- Speech-Language Pathologists
Many specialists have wait lists, so you will want to call and schedule an appointment for a developmental assessment immediately following your referral.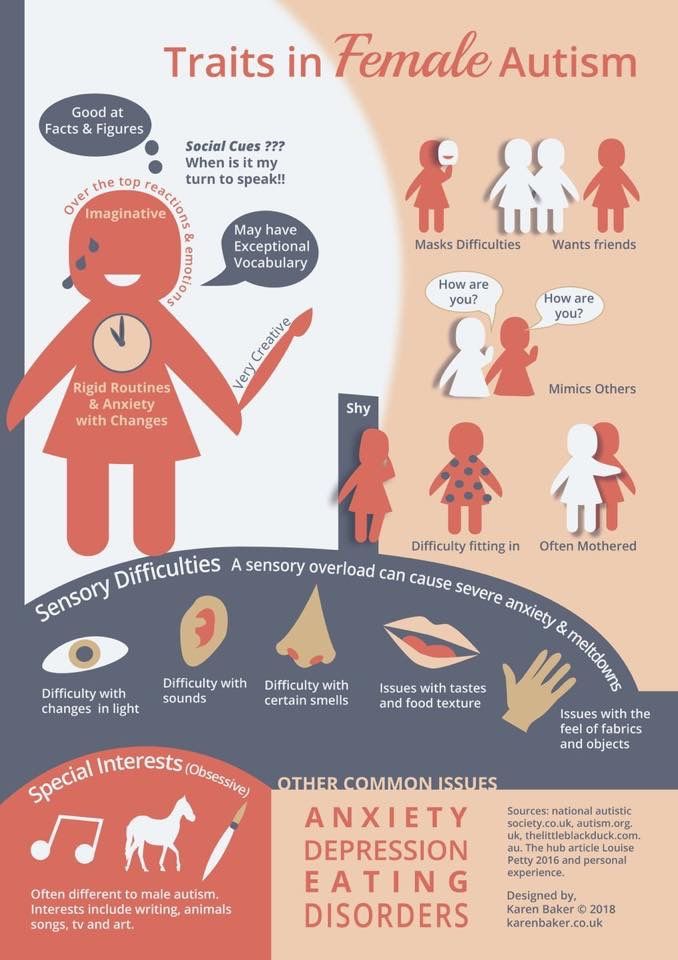
How To Get an Appointment for a Screening and/or Assessment
There are a number of ways to begin the evaluation process. One way is through your child’s pediatrician. Another way is through your state’s Early Childhood Intervention Program (ECI).
Your Child’s Pediatrician
To go through your child’s pediatrician, contact them to inform them you are concerned about your child’s development, and need a developmental screening.
If your child’s pediatrician identifies areas of concern during the screening process, they should refer you to a trained specialist (developmental pediatrician, neurologist, psychiatrist, or psychologist) for further evaluation in an autism assessment.
Your State’s Child Find Program
Another option is to obtain an evaluation and diagnosis through your state’s Child Find program. Child Find is a provision under the Individuals with Disabilities Education Act (IDEA) that requires states to find and evaluate kids with disabilities at no extra cost to families.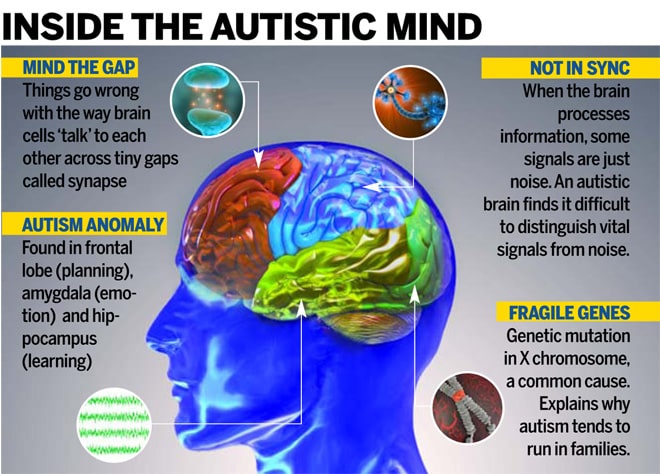
Your child’s age will determine how you go about scheduling an appointment for an evaluation through Child Find:
- Children Under 3:
- Contact your state’s Early Childhood Intervention (ECI) program
- Find your state’s ECI contact information here
- Contact your state’s Early Childhood Intervention (ECI) program
- Children Over 3:
- First, contact your local public school and ask where to send a request for evaluation
- Then, send a formal request for an evaluation via certified mail with a return receipt
- Provide details about why you feel your child needs an evaluation
- For example, “I am asking that you evaluate my child for autism because they are showing the following symptoms…”
- Give consent for evaluation in your formal request (the school cannot evaluate your child without your consent)
- Provide details about why you feel your child needs an evaluation
Before Your Appointment
Preparing for your appointment paves the way for effective advocacy for your child and helps ensure they receive a thorough evaluation.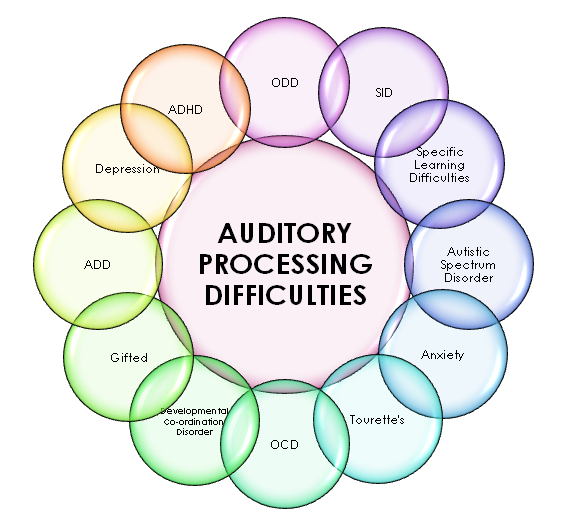 You can prepare for your appointment by:
You can prepare for your appointment by:
- Compiling a list of questions and concerns to discuss with your doctor or the person who will be evaluating your child
- Collecting video data of your child doing any concerning behaviors that you feel your child may not engage in during an assessment
- Completing a milestones checklist. Some free options include:
- The CDC’s “Learn the Signs. Act Early.” website has printable and digital trackers
- Modified Checklist for Autism in Toddlers (M-CHAT)
- Autism Treatment Evaluation Checklist (ATEC)
- Completing any surveys or questionnaires given to you by your child’s doctor or ECI office
- Be sure to do this 3-5 days before your appointment to allow for ample time for completion
- Calling your insurance company to verify coverage and any out-of-pocket expenses that you might incur
- Screenings and assessments through state’s ECI program should be free of charge (see above)
During Your Appointment
During the screening and assessment processes, your child will complete some simple tests that may look like play. As the parent, you will answer questions about your child’s development and behaviors.
As the parent, you will answer questions about your child’s development and behaviors.
During your appointment, go over your completed milestone checklists and/or M-CHAT with your doctor. Point out all of the missed or delayed milestones. Most importantly, accurately describe concerns and issues. Do not “sugar coat” or downplay any delays. Minimizing or downplaying answers will not help your child in the long run. Also, don’t be afraid to speak up. Your input is invaluable throughout this process!
Remember, screenings are brief, informal, and may look like a well-child visit. However, their informal nature doesn’t excuse the person conducting the screening from taking this process seriously. Your concerns should never be dismissed. If the person screening your child tells you to “wait and see” or suggests this a “just a stage” your child will grow out of, go and get a second opinion! Always listen to your intuition.
Developmental assessments, on the other hand, are more comprehensive and in-depth than screenings.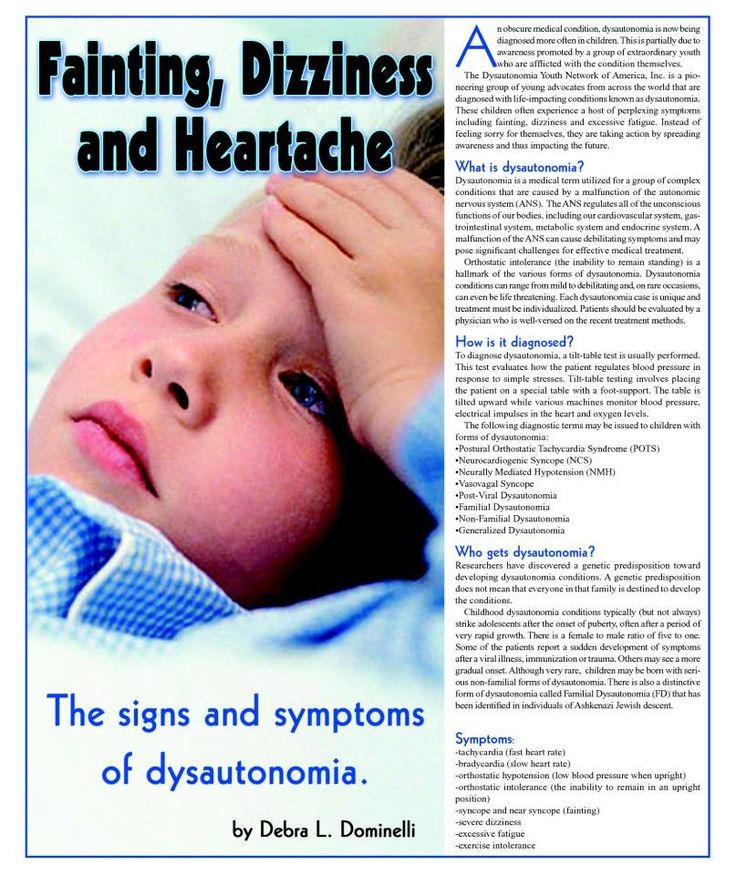 Because they can take a long time to complete, the professional or team of professionals assessing your child may break up the process into several different appointments.
Because they can take a long time to complete, the professional or team of professionals assessing your child may break up the process into several different appointments.
Please note, in order to ensure your child receives a comprehensive assessment, they need to be observed in a number of different settings. Doing so will help the professional(s) assessing your child obtain an understanding of how they behave in various environments. Depending on your child’s comfort level, you may be asked to be in the room with your child, view the from an observation room, or remain in the waiting room.
Frequently Asked Questions
Resources
- Signs and Symptoms of Autism (in both English and Spanish)
- How to contact your state’s Early Childhood Intervention Program
- Find additional information and tools (in both English and Spanish) for navigating the diagnostic process on the CDC’s website.
Myths about autism and things that can be done in time if you know / Habr
Hello, Habr! I am a neurologist and I often see patients with ASD or suspected ASD. As a pediatric neurologist, I work with children and adolescents. Perhaps, of the entire spectrum of my work, it is autism that is most subject to various fictions and myths both among patients and among specialists. In recent years, there have been many new scientific studies with good levels of confidence that are changing the idea of what can and cannot be done. And so let's take a look at the main myths.
As a pediatric neurologist, I work with children and adolescents. Perhaps, of the entire spectrum of my work, it is autism that is most subject to various fictions and myths both among patients and among specialists. In recent years, there have been many new scientific studies with good levels of confidence that are changing the idea of what can and cannot be done. And so let's take a look at the main myths.
First and foremost, early diagnosis up to two years can sometimes greatly compensate for possible consequences.
Second, people often think that ASD is a “loose” diagnosis. This has not been the case for a long time, and there are conditions in which the correct and timely help of specialists can help very well even in adulthood.
In general, let me tell you what I often encounter in my work and try to explain how you can actually help patients with ASD. Below is a list of myths and an analysis of each of them.
"Autism is treated with severe antipsychotics"
This is only partly a myth: ASD is rarely an isolated diagnosis, it is often accompanied by other serious problems, for example, severe sleep disorders, behavioral disorders, epilepsy, and more.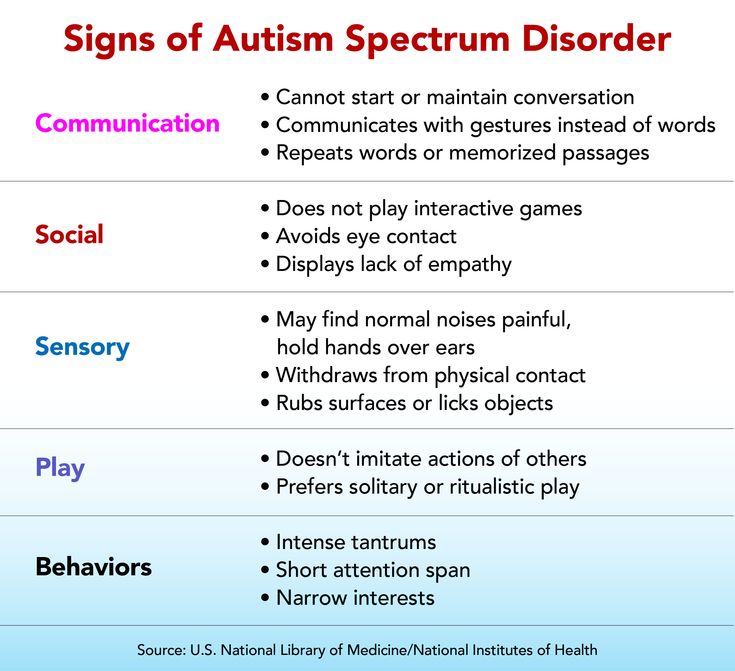 In such cases, doctors prescribe appropriate drug therapy: it can be antipsychotics, anticonvulsants, or something else. In this situation, pills in therapy will really be needed, but not for curing ASD, but for correcting concomitant disorders. If we are talking about those patients who can safely be in society for themselves and others, then pharmacotherapy, as a rule, is not used.
In such cases, doctors prescribe appropriate drug therapy: it can be antipsychotics, anticonvulsants, or something else. In this situation, pills in therapy will really be needed, but not for curing ASD, but for correcting concomitant disorders. If we are talking about those patients who can safely be in society for themselves and others, then pharmacotherapy, as a rule, is not used.
The results of scientific research (we will return to them below) show that the emphasis should be placed on psychological and pedagogical work. That is, it is possible and necessary to help such a patient with the help of certain exercises and techniques (for example, teaching game sessions), which are carried out by specially trained teachers and psychologists.
Total: The most common cases of ASD are treated with behavioral therapy.
"Vaccination Causes Autism"
This is probably the most persistent myth among parents.
This is the story.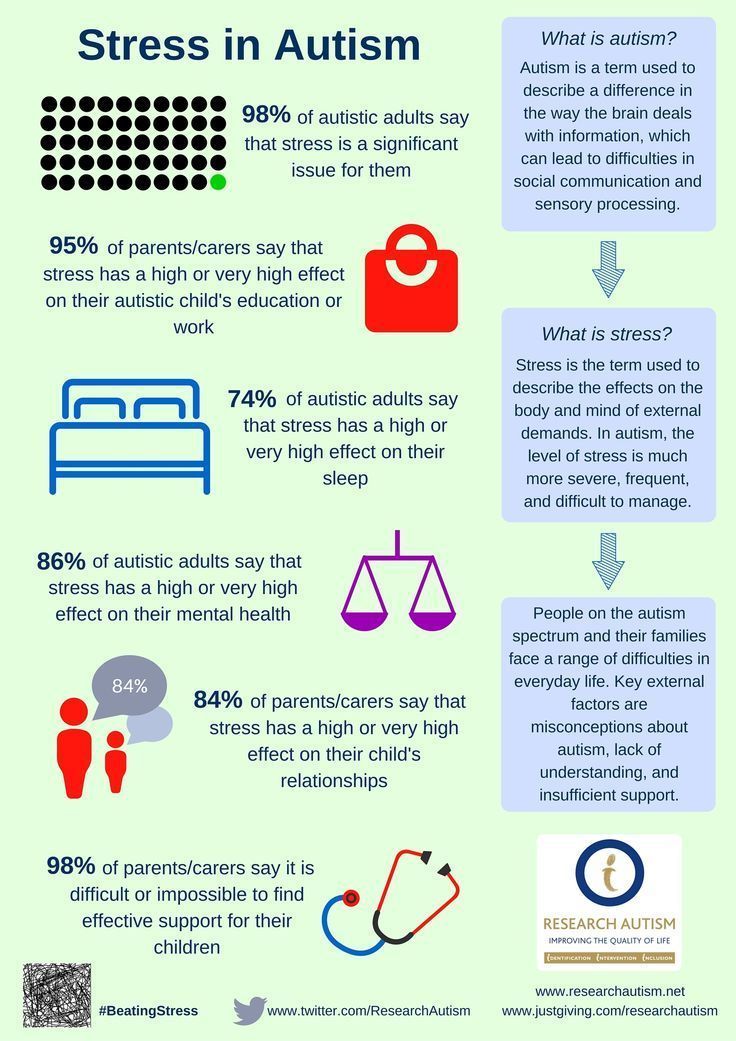
The most popular hypothesis about the association of vaccines with the development of autism appeared in 1998, when British researcher Andrew Wakefield published a paper in which he described several cases of autism in children who received vaccinations against measles, rubella and mumps. He was quickly caught tampering with the data: for example, in some children the symptoms of autism appeared even before vaccinations, for others, the timing of the onset of the disease indicated by Wakefield did not coincide with the data provided by the parents.
Inactivating substances were suspected as a harmful substrate: thiomersal (essentially a preservative) and an aluminum adjuvant. It was believed that they in inactivated vaccines can cause RAS. The conclusions were then based on individual observations, there were no systemic clinical studies. At the moment, a lot of work has been done, and the connection is not shown.
Of the important. Changes in the vaccination schedule and the withdrawal of some vaccines or their components did not affect the spread of ASD in any way.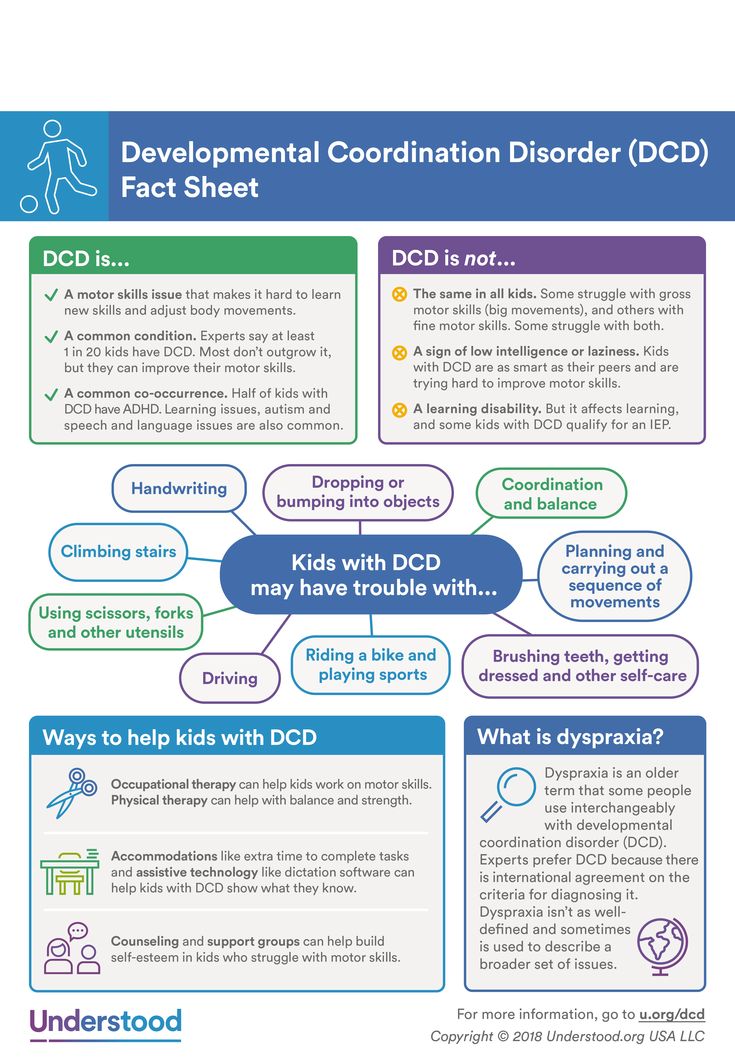 (DeStefano F. Thimerosal-containing vaccines: evidence versus public apprehension//Expert opinion on drug safety. – 2009. - T. 8. - No. 1. - S. 1-4 .; Madsen K. M. et al. A Population-based study of measles, mumps, and rubella vaccination and autism // New England Journal of Medicine. - 2002. - No. 19 (347). – P. 1477–1482.)
(DeStefano F. Thimerosal-containing vaccines: evidence versus public apprehension//Expert opinion on drug safety. – 2009. - T. 8. - No. 1. - S. 1-4 .; Madsen K. M. et al. A Population-based study of measles, mumps, and rubella vaccination and autism // New England Journal of Medicine. - 2002. - No. 19 (347). – P. 1477–1482.)
It is sad to realize that sometimes it is doctors who explain ASD in a child by vaccination. It must be understood that parents are confused and simply poorly informed about the actual state of affairs. My task as a doctor is not to argue with the opinion of the family, but to explain what is really happening with their child, how and with what to help him. It should be explained to parents that some stages of vaccination coincide with a sensitive period in the development of a child, when, with a certain predisposition, he may become vulnerable to stress factors, for example, an infectious or other disease or vaccination.
“No ordinary healthy family will have a child with ASD”
There is an opinion among people that autism is more likely to develop in children whose parents suffer from drug, nicotine or alcohol addiction.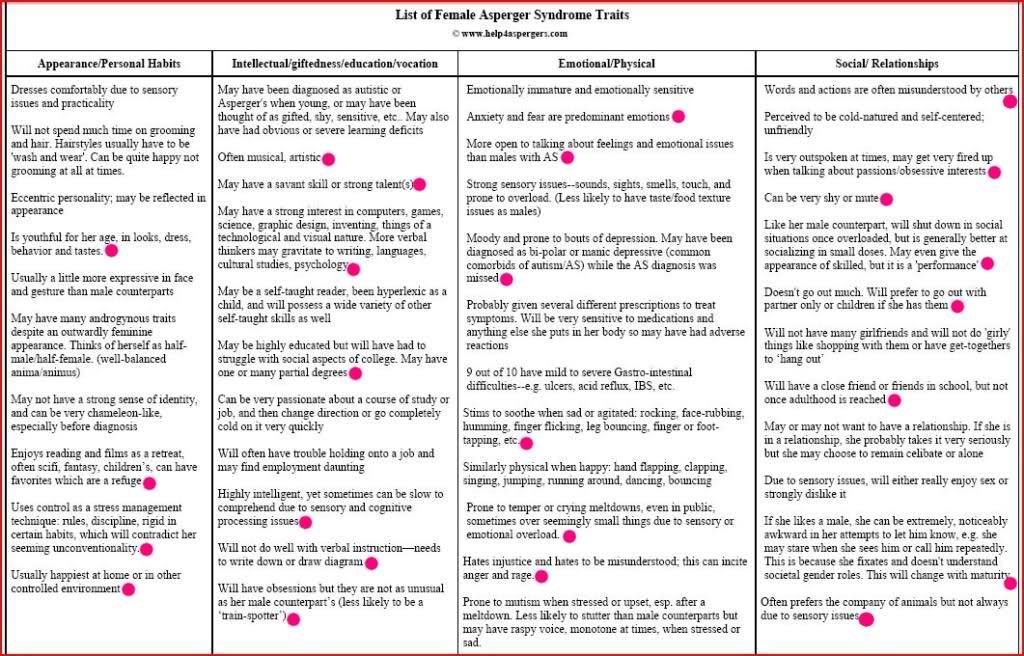 This, of course, is not at all the case. Conditionally healthy and highly educated people, adherents of a healthy lifestyle, can also have a child with a developmental disorder.
This, of course, is not at all the case. Conditionally healthy and highly educated people, adherents of a healthy lifestyle, can also have a child with a developmental disorder.
Today there is no single concept of the cause of autism. More than a hundred genes associated with ASD are already known. With the development of genetics, as well as the improvement in the quality of genetic tests, data on the number of genes that affect the likelihood of this disorder are increasing. Also, we doctors know that ASD can develop in some neurological and genetic syndromes, as well as in autoimmune diseases as part of them.
It is known that the risk of having a child with ASD increases with the age of the parents, which is associated, for example, with an increase in the number of mutations in spermatogenesis in older men.
So far, it is known that the sex of the child (given genetically) affects the likelihood of autism. The ratio of diagnosed boys to girls is 3:1.
Total: there is no unified theory of genesis yet, the leading role in the development of ASD belongs to genetic disorders.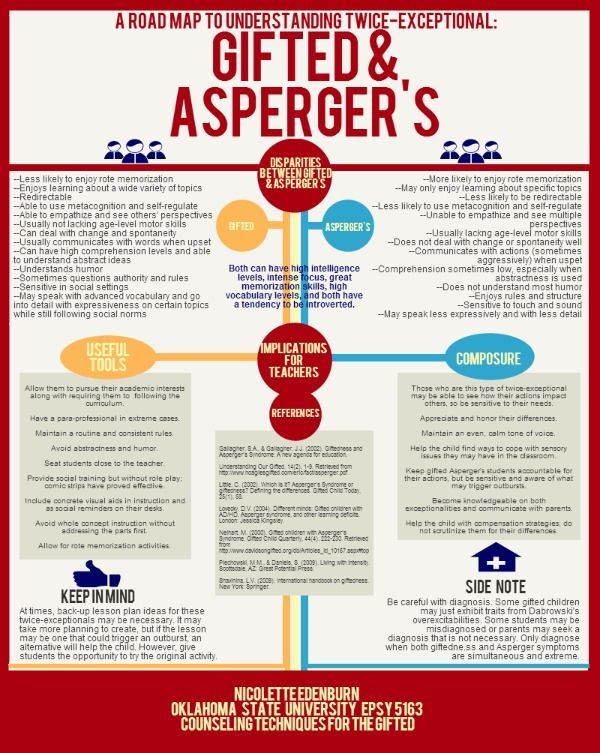 Vaccines do not cause the development of ASD.
Vaccines do not cause the development of ASD.
"We will ruin the future of the child if we confirm ASD with a psychiatrist"
The situation is this: in order to diagnose an autism spectrum disorder, you first need to get an appointment with a pediatrician or a neurologist who can recognize the signs of the disease and send the child for additional examination to a psychiatrist. The diagnosis is confirmed by a psychiatrist. If we are really talking about autism, it is important to get this confirmation as early as possible in order to continue to work successfully, while the child’s psyche and nervous system are sufficiently plastic.
In practice, it looks like this: in Moscow and a number of large cities, parents have access to a lot of information about autism, and they generally understand how a child should develop, what is normal and what is not. If it suddenly seems to them that something is not going according to plan, then they appear at my (pediatric neurologist) doorstep just to check if everything is fine.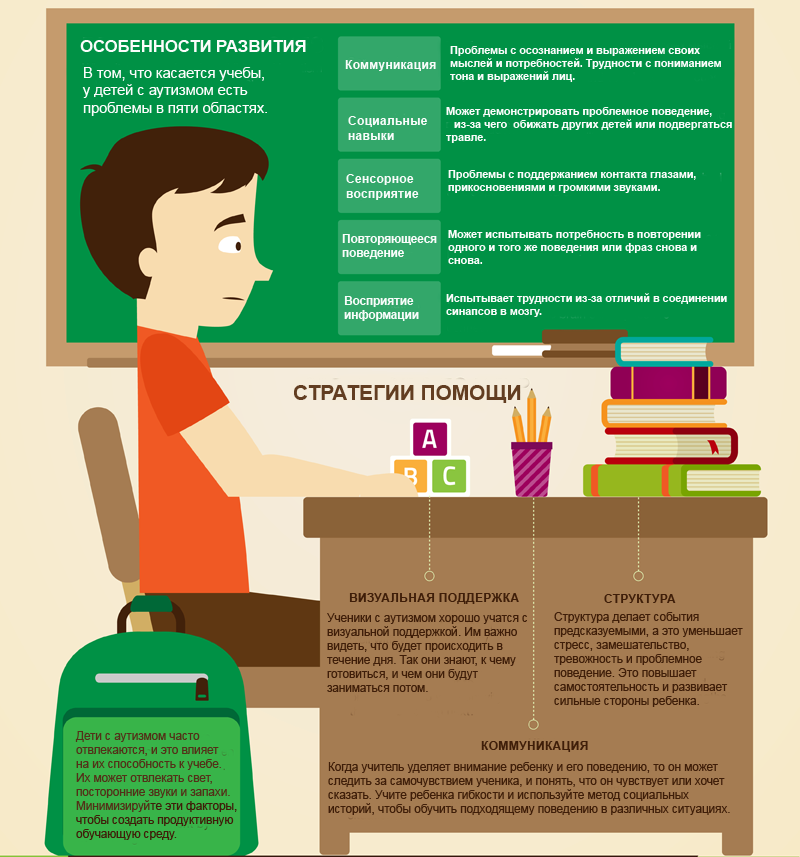 Or, at least, they know that it is possible to take a free online questionnaire on their own to decide whether to go to the doctor or not. The questionnaire, by the way, is here: test.autism.help. Highly recommend.
Or, at least, they know that it is possible to take a free online questionnaire on their own to decide whether to go to the doctor or not. The questionnaire, by the way, is here: test.autism.help. Highly recommend.
In the regions (I go to consult), unfortunately, the situation is often different: some doctors and psychologists pass off developmental disorders in a child as personality traits, and parents think that they should wait until the child grows up and this will pass. However, one cannot fail to say that there are very attentive and competent specialists who, in time, indicate the problem to the family and ways to solve it. Or there is an even more significant problem - the lack of specially trained teachers and psychologists.
Typical cases are described in the questionnaire: this is emotional scarcity. For example, a healthy child has a so-called “revitalization complex” when parents come to the crib, and he is happy with them and emotionally reacts to them with a smile and spreading his arms to the sides. Further, pre-speech moments are important, such as fairly frequent cooing and babble. Well, and the ability to follow the emotional reaction of parents, that is, to respond to their smiles or sadness, for example, to follow their reaction to any situation, copy it.
At an older age, one should look for the lack of speech and signs of rather monotonous and repetitive behavior. For example, the fact that a child plays the same game (and does not want to play others in principle), without modifying it, without adding something new to it, without complicating it. It is also important here that he does not allow you to make these changes, each time overreacting to your attempts. A very striking sign is sometimes described by parents: if you change the route from the kindergarten home, then the child each time reacts with loud crying, screaming and hysteria, which cannot be dealt with for a very long time.
Manifestations may vary. It is important to understand whether it is really a child's personality trait or a developmental disorder, including a case of ASD.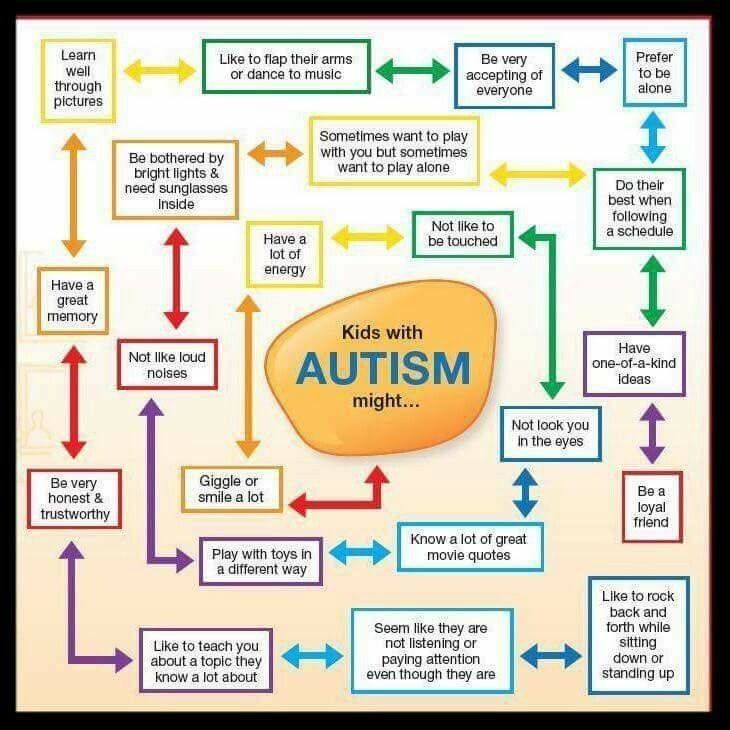 Why is it important - because I often encounter a situation where diagnoses like "mental retardation" or "motor alalia" are erroneously made without a proper diagnostic search, and the family loses a lot of time in vain. Why so - in the next myth.
Why is it important - because I often encounter a situation where diagnoses like "mental retardation" or "motor alalia" are erroneously made without a proper diagnostic search, and the family loses a lot of time in vain. Why so - in the next myth.
"THE NEUROLOGIST IN THE POLYCLINIC SHOULD NOTICE THIS!"
Unfortunately, it is difficult for a neurologist to notice the signs of ASD at a regular clinic appointment if they are not pronounced. OMS appointment is 12-15 minutes, of which five minutes the doctor fills in the medical history. If you have an experienced specialist in front of you and the child has time to demonstrate signs of behavior characteristic of ASD, then yes, this may alert the doctor.
Only a psychiatrist makes a final diagnosis. A neurologist or pediatrician can recognize the signs of autism and send the child for further examination to a psychiatrist. That is, the entry point is yes, a neurologist or a pediatrician.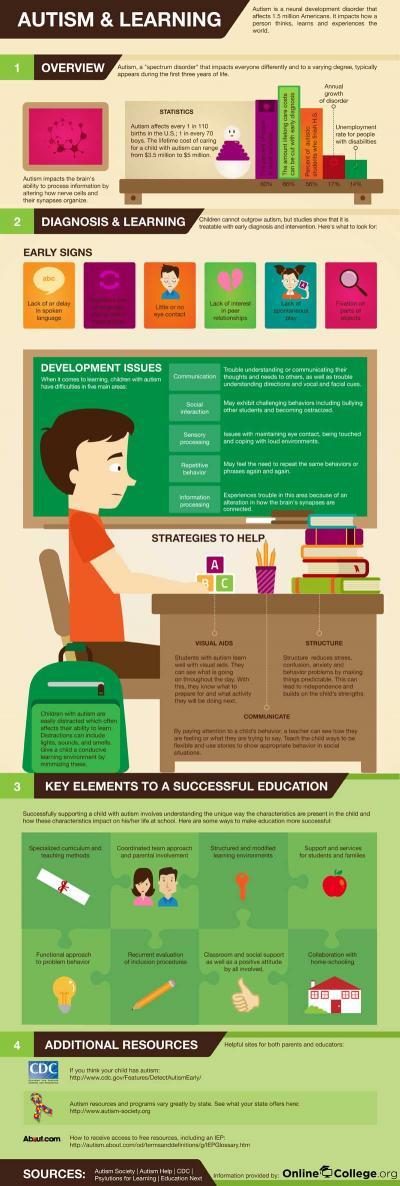 And it is better if it is a doctor who can devote enough time to your child.
And it is better if it is a doctor who can devote enough time to your child.
My appointment takes a total of 40 to 60 minutes, which is the minimum for a fairly accurate diagnosis. At my consultations, for the first 15–20 minutes, I only watch how the child behaves in the new office, how he gets used to me and reacts to the speech addressed to him, whether he allows me to approach him, how he is involved in communication, what he considers and so Further.
Sometimes it is incredibly difficult for me to refer a child to a psychiatrist, especially if the family lives in a small town or village, because parents very often not only do not trust doctors, but are also consciously afraid of them. In our society, there is still a stigmatization of patients, that is, if suddenly someone from the environment of the parents finds out that they took the child to a psychiatrist, then this is some kind of “shame”: mothers have repeatedly told how friends stopped communicating with them, and relatives accused, for example, the mother that she had given birth to a “sick” child.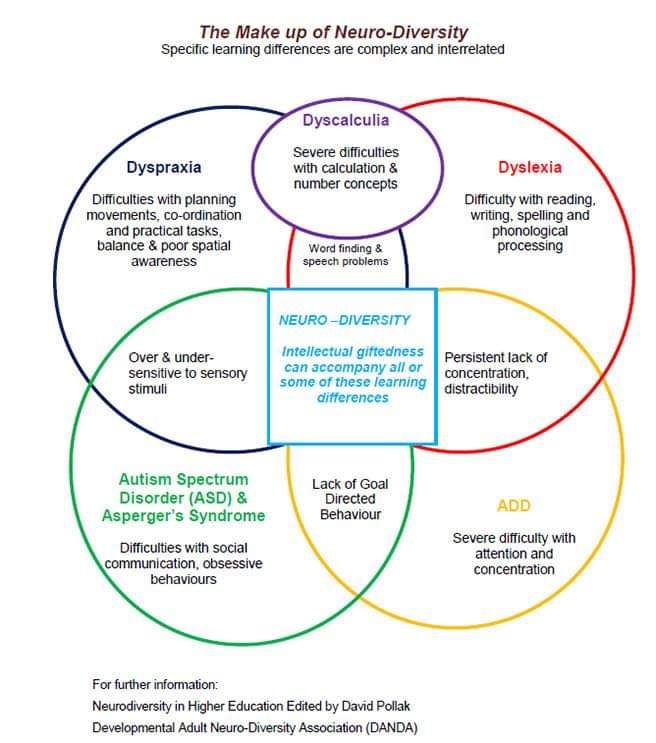 And in some cases, the threat of such a reaction in society is stronger than the motivation to make a correct diagnosis.
And in some cases, the threat of such a reaction in society is stronger than the motivation to make a correct diagnosis.
As a rule, parents agree to see a psychiatrist either after several months of observation with me, or in case of serious behavioral disorders, when it becomes obvious to them that this is not just attention deficit hyperactivity disorder, but something else. And these manifestations are just a mask of the main problem: RAS.
Well, then the question of trust in a psychiatrist arises.
Two psychiatrists = three opinions
A patient can see a psychiatrist in a variety of conditions, in a variety of moods and under a variety of circumstances. For example, he got used to the first two appointments with different psychiatrists, and the third psychiatrist may already seem familiar and safe to him, and he will contact him more actively. Perhaps, on the contrary, he will not make contact at all. Of course, all this should not affect the diagnosis.
ASD diagnosis should be consistent and comprehensive.
The diagnostic search looks like this:
- The M-CHAT-R symptom questionnaire, which you can fill out yourself at home before the consultation.
- Psychiatrist evaluation of clinical criteria for diagnosis.
- Multidisciplinary assessment (psychiatrist/psychologist, etc.).
- Of the instrumental methods for diagnosing ASD, the closest to the “gold standard” is the combined use of the ADOS-2 Autism Diagnostic Examination Plan and the Autism Diagnostic Interview, ADI-R (and each of the methods separately is also characterized by high rates sensitivity and specificity).
That is, ADOS-2 and ADI-R - this is what allows you to accurately assess what exactly is happening with the patient, scales in which the type and number of behavioral and emotional reactions are accurately described.
The reproducibility of the results is quite good.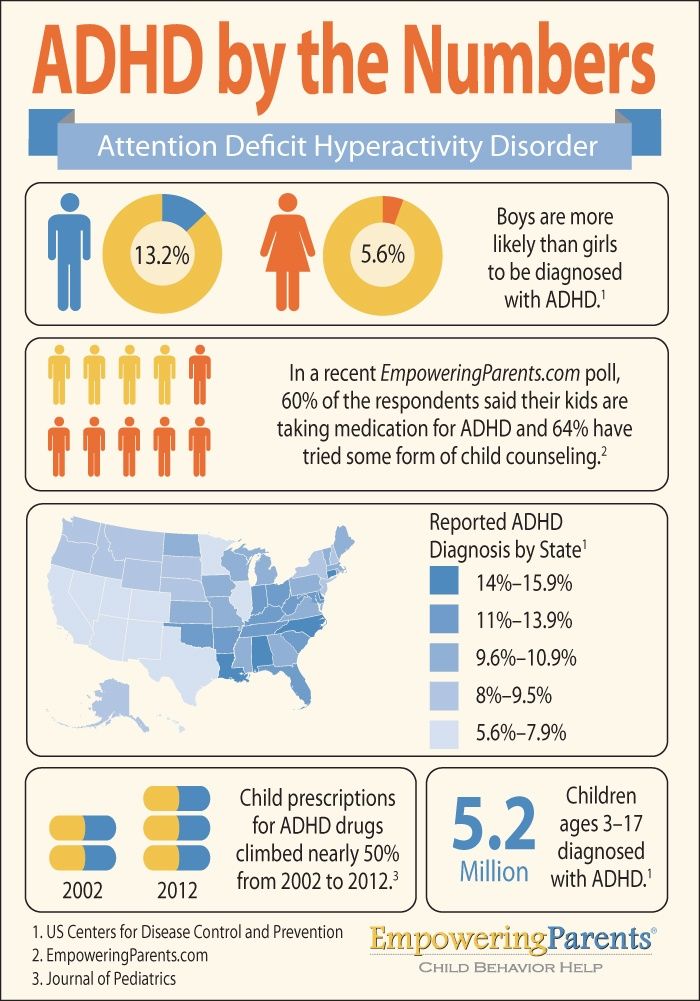 Naturally, this does not apply to situations where some spontaneous external circumstances change the child's behavior. For example, in my practice it was so that they dropped in on the way to the psychiatrist after the pediatrician, since they went to the clinic. The child had a temperature of 38.5, and, naturally, he did not demonstrate the complex of behavioral reactions that is normal for his age. Or, for example, before my consultation, the child was vaccinated, which he was very afraid of. All my reception goes to establishing communication with the baby.
Naturally, this does not apply to situations where some spontaneous external circumstances change the child's behavior. For example, in my practice it was so that they dropped in on the way to the psychiatrist after the pediatrician, since they went to the clinic. The child had a temperature of 38.5, and, naturally, he did not demonstrate the complex of behavioral reactions that is normal for his age. Or, for example, before my consultation, the child was vaccinated, which he was very afraid of. All my reception goes to establishing communication with the baby.
A typical mistake at the stage of making a diagnosis is to refuse it. Parents can ignore it, not admit that there is a problem. If another psychiatrist makes a diagnosis different from this one, they can gladly accept it. In such a situation, it is always a pity for the time of the child. One or two years of tremendously useful support and correction can be lost during those periods of a child's development when they would have given a greater result.
"Patients with ASD are not rehabilitated"
It's not even close. More precisely, the prognosis depends very much on what kind of ASD disorder it is. If we are talking about the Kanner option, then yes, the situation is complicated, it is disability and very difficult and constant rehabilitation, but even in this situation it is possible to improve the current state. Asperger's syndrome and non-severe variants of autism (meaning forms of ASD without severe concomitant disorders) are rehabilitated quite well, they change quite plastically. I have patients in my observation who are now studying in regular classes and do not experience any particular problems. Naturally, it is harder for them than for the rest, but not so much as to change their lifestyle drastically.
By the way, what are “atypical” variants of ASD.
This is when the diagnosis is made despite the fact that the patient does not seem to look like an autist.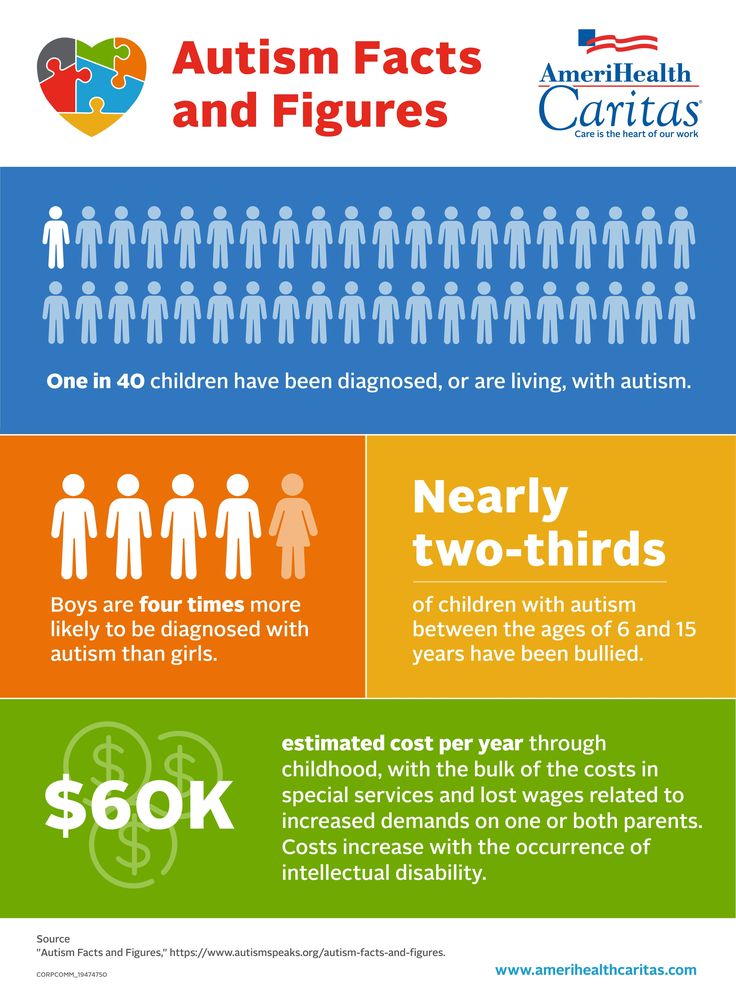 Such children, as a rule, are sociable, even warm in communication, they have speech (albeit with impairments). But at the same time, there may be a distortion of mental development without a decrease in intelligence or with a slight decrease in it, stereotypical behavior (repetitive actions, fixation on one type of game or the same book / topic) or an acute reaction to some stimuli when specific sounds or music provokes an acute negative reaction. I have patients under observation who react sharply to the sound of a hairdryer / certain music / someone's voice or smell, for example (and all this, as a rule, does not cause any inconvenience to others).
Such children, as a rule, are sociable, even warm in communication, they have speech (albeit with impairments). But at the same time, there may be a distortion of mental development without a decrease in intelligence or with a slight decrease in it, stereotypical behavior (repetitive actions, fixation on one type of game or the same book / topic) or an acute reaction to some stimuli when specific sounds or music provokes an acute negative reaction. I have patients under observation who react sharply to the sound of a hairdryer / certain music / someone's voice or smell, for example (and all this, as a rule, does not cause any inconvenience to others).
Parents often ask if it's okay for a child to love pirates and everything related to them. Normally, this is the usual game interest somewhere between dinosaurs and machines. The fact is that a child with ASD will line up his pirates in the same order without changing it. Or will play only one color of pirates. In my observation - a patient who fixed himself on plastic soldiers and lined them up strictly with alternation of two colors and nothing else. During the game, they always kept this order. It is important to ask parents about this, of course. Autonomous speech is also noticeable (the patient, during any activity, constantly says or whispers something under his breath without emotional coloring, and this speech does not correlate with what he is doing at that moment) and certain stereotypical gestures.
During the game, they always kept this order. It is important to ask parents about this, of course. Autonomous speech is also noticeable (the patient, during any activity, constantly says or whispers something under his breath without emotional coloring, and this speech does not correlate with what he is doing at that moment) and certain stereotypical gestures.
Weak prospects for socialization and adaptation are not true. Patients with ASD are very different, the spectrum itself includes a fairly large range of conditions and a fairly large spread of diagnoses in terms of socialization opportunities and intellectual potential.
In general, the main assistance is systematic psychological and pedagogical support, including applied behavioral analysis. It is often also known as ABA therapy because it was once the only implementation of the method. Several different frameworks are currently in use.
There are enough studies on PAP models. The level of persuasiveness of recommendations is A (level of evidence is 2). Most of the research has been done for the Lovaas model (UCLA or YAP). This is a program for children, which is based on the DTT technique (individual blocks), which involves individual lessons at home or with specialists in the center. That is, parents should work with the teacher, and a lot themselves. The main work is a meta-analysis by Reichow et al, as well as a meta-analysis by Makrygianni et al. Also recommended is the comprehensive Denver Early Intervention Model, aka ESDM for children aged 14 to 30 months, to help develop language skills.
The level of persuasiveness of recommendations is A (level of evidence is 2). Most of the research has been done for the Lovaas model (UCLA or YAP). This is a program for children, which is based on the DTT technique (individual blocks), which involves individual lessons at home or with specialists in the center. That is, parents should work with the teacher, and a lot themselves. The main work is a meta-analysis by Reichow et al, as well as a meta-analysis by Makrygianni et al. Also recommended is the comprehensive Denver Early Intervention Model, aka ESDM for children aged 14 to 30 months, to help develop language skills.
DIR/Floortime Grade A recommendation (Level of Evidence 2): This is a tool for preschool children. There are also studies with recommendation level B (level of evidence - 2).
Pair of quotes in English:
, 2011; Lal and Chhabria, 2013; Pajareya and Kopmaneejumruslers, 2011; Pajareya et al., 2019
…
Case studies have also been effective in supporting the use of DIRFloortime with children with autism.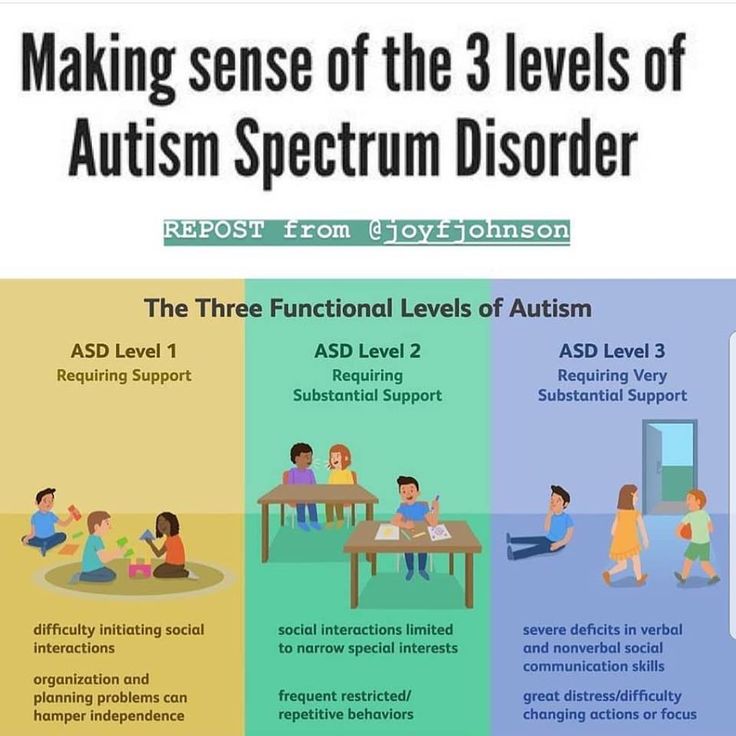 Dionne and Martini (2011) demonstrated a statistically significant improvement in communication between parent and child. Wieder and Greenspan (1997, 2005) did a comprehensive case study that spanned from 8-15 years. These studies supported the long-lasting results DIRFloortime had on individual child skills, as well as, the emotional connections the families were able to develop over time using this approach.”
Dionne and Martini (2011) demonstrated a statistically significant improvement in communication between parent and child. Wieder and Greenspan (1997, 2005) did a comprehensive case study that spanned from 8-15 years. These studies supported the long-lasting results DIRFloortime had on individual child skills, as well as, the emotional connections the families were able to develop over time using this approach.”
If you are interested in more details, then here are the studies:
- Reichow B. et al. Early intensive behavioral intervention (EIBI) for young children with
autism spectrum disorders (ASD) // Cochrane Database of Systematic Reviews. — 2018. - Rogers S. J. et al. A multisite randomized controlled two-phase trial of the early start.
- Denver model compared to treatment as usual // Journal of the American Academy of Child & Adolescent Psychiatry. — 2019. — No 9 (58). — C. 853–865.
In them, not only the texts themselves are important, but also references to other studies, each of which closes a specific question.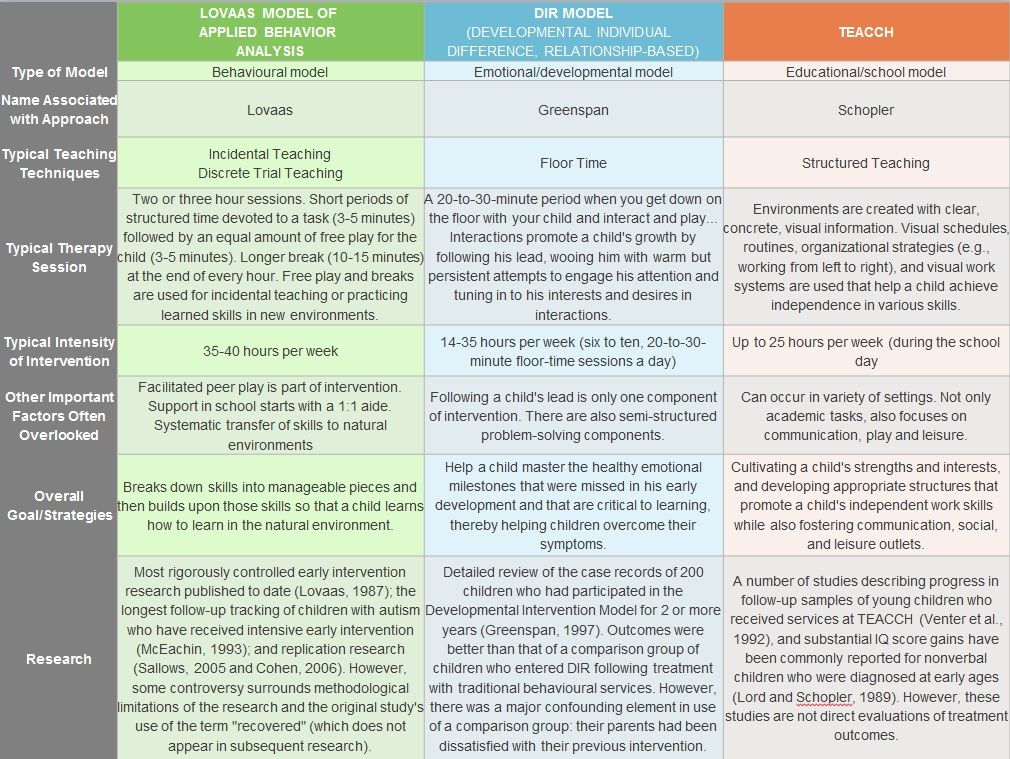
Bottom line: we have behavioral therapy tools with proven effectiveness. This is ABA therapy for children from 14 to 30 months, this is the Denver model of early intervention for preschoolers, this is the DIR / Floortime method and others. All of these models involve building an environment where children learn to communicate and develop social skills. This requires special psychologists with separate professional training. Alas, there are few such specialists in Russia, and those that do usually conduct courses in big cities. In addition, a very active participation of parents is needed.
We get very good results with DIR/Floortime in practice, but we need to adapt the methodology very much to the environment where the child grows up and to the people with whom he communicates. This requires effort from all participants in the process.
From the examples: there were two cases where the parents agreed to a psychiatrist only a few months after my diagnosis. But after the diagnoses were made (two different types of ASD in two children in the same family), they began working on the ABA method with psychologists. Were observed six months after the start of therapy, both patients made a strong breakthrough in speech and communication. At the first appointment, there was no speech at all. In the course of psychological work, they began to talk a little, establish stable visual contact, monitor the emotional reaction of the interlocutor, take an interest in objects, quickly felt the equipment of the office.
Were observed six months after the start of therapy, both patients made a strong breakthrough in speech and communication. At the first appointment, there was no speech at all. In the course of psychological work, they began to talk a little, establish stable visual contact, monitor the emotional reaction of the interlocutor, take an interest in objects, quickly felt the equipment of the office.
In general, a child with a mild case of ASD can recover fairly quickly if the diagnosis is made on time. In my observation, there are patients who were diagnosed with ASD late, but largely due to the correct psychological and pedagogical work, they study quite well at school according to the general education program. There are few of them with such great success, but they are!
"Take him to the dolphins!"
There are methods such as dog therapy (canistherapy), hippo and dolphin therapy. Evidence is currently insufficient for clinical use.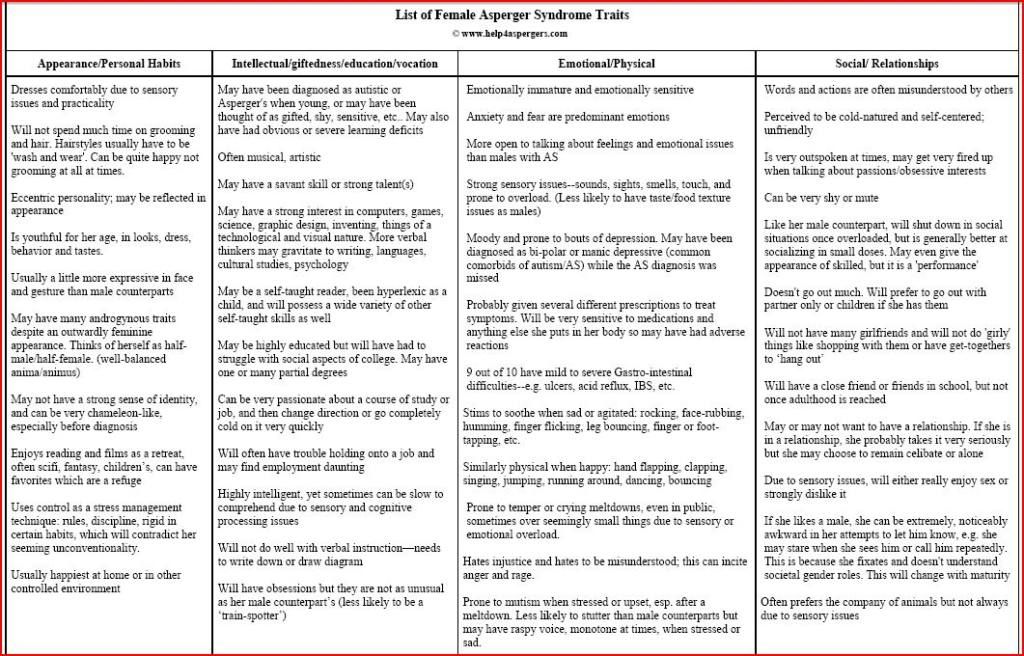 That is, if the child likes it, you can use it in addition to the existing methods and believe that they work, but, alas, there are no data, except for subjective value judgments and individual small observations.
That is, if the child likes it, you can use it in addition to the existing methods and believe that they work, but, alas, there are no data, except for subjective value judgments and individual small observations.
If methods based on communication with animals are generally safe and give an incomprehensible, but not dangerous result, then there are methods that can be called frankly charlatan, and those that are frankly harmful to children. For example, there is data on hyperbaric oxygen therapy: several cases of ear injuries are described instead of correcting the underlying disorder. There are microcurrents that offer to do instead of treatment. Similarly: there is no evidence of effectiveness, but there is a substitution of a proven technique.
Of the modern methods with insufficient evidence base, I would like to note the BFB (biofeedback) method, for which there is ambiguous evidence, and a database is now being accumulated. There is a method of cerebellar stimulation, according to which there are single data that have not yet been added to the system.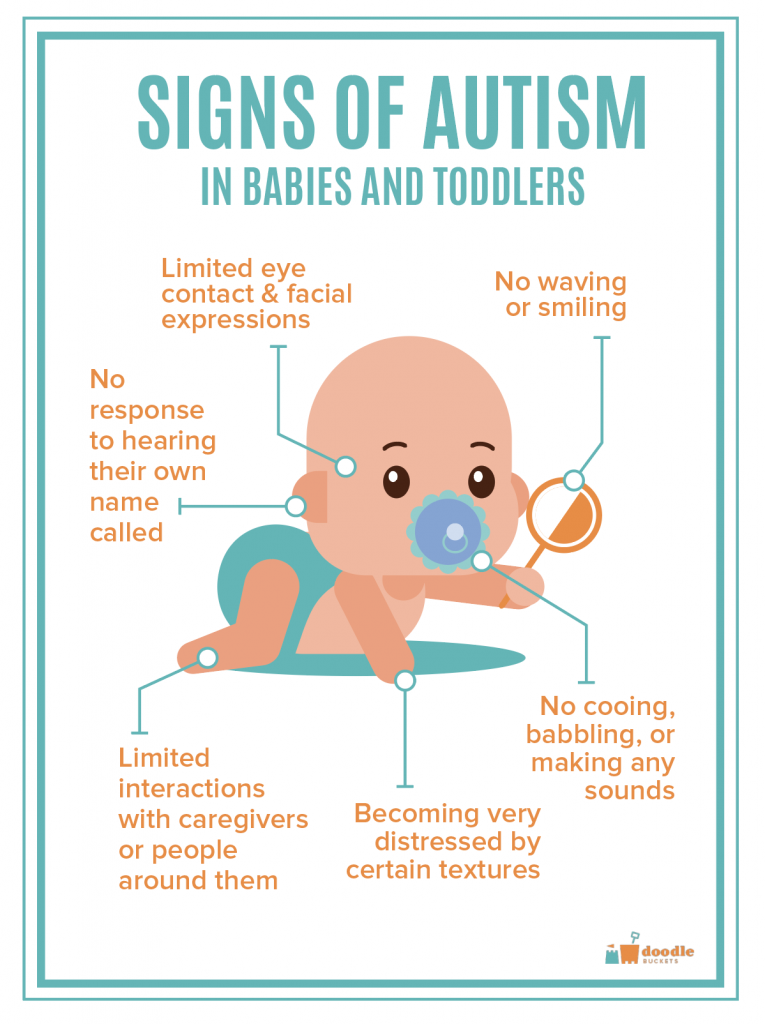 Some doctors sometimes include these methods in complex rehabilitation, and not only in Russia, but also abroad. The prospects and news of the possibilities of gene therapy are important, of course.
Some doctors sometimes include these methods in complex rehabilitation, and not only in Russia, but also abroad. The prospects and news of the possibilities of gene therapy are important, of course.
"The child should be placed in a special class"
It is not always necessary. In my practice, there are many cases when studying in regular school classes is possible. Yes, this is about non-severe variants of ASD, and for this you need to start active work on rehabilitation on time. Yes, this often requires basic training to be additionally accompanied by psychological or pedagogical work. But the adaptation is decent, and the family is so comfortable.
Weaknesses in children with ASD are often speech disorders, lack of understanding of the general meaning of the text, they retell what they read in memorized phrases or perceive oral speech in fragments, which can make it difficult to understand the conditions of the task, for example.
Program requirements are described in the Federal State Educational Standard for Primary General Education for Students with ASD. At the moment, there are four options for the educational program that children with ASD can study.
“There is nothing to read about this evidence”
This is true: for parents, most popular science works are not available because they are in English, and attention to these issues is often given in English-language blogs. But very good Russian-language resources on this topic have already begun to appear, compiled by psychiatrists, pediatricians, psychologists and speech therapists.
"No support"
There is support. There are charitable foundations that have support programs. That is, if parents do not have money for psychological and pedagogical work, then they can be helped with specific rehabilitation programs for free. To do this, you need to disclose data on your child for scientific research and fall under the criteria for these studies. That is, if your doctor roughly understands how these funds work, or if you are ready to read what programs they have, it is difficult to find support, but it is real. It’s worth starting with the websites of the Exit and Naked Heart foundations.
That is, if your doctor roughly understands how these funds work, or if you are ready to read what programs they have, it is difficult to find support, but it is real. It’s worth starting with the websites of the Exit and Naked Heart foundations.
“There is a special diet…”
It used to be thought that casein-free or gluten-free diets could help patients with ASD. At the moment, it is known that there is no such dependence on food. (Piwowarczyk A. et al. Gluten-and casein-free diet and autism spectrum disorders in children: a systematic review // European journal of nutrition. - 2018. - V. 57. - No. 2. - P. 433-440 .; Sathe N. et al. Nutritional and dietary interventions for autism spectrum disorder: a systematic review // Pediatrics. - 2017. - V. 139. – no. 6. – S. e20170346.; El-Rashidy O. et al. Ketogenic diet versus gluten free casein free diet in autistic children: a case-control study // Metabolic brain disease. - 2017. - T. 32. - No. 6. - S. 1935-1941.)
6. - S. 1935-1941.)
"There is autism - there will be no career"
If we are talking about those ASDs that are not accompanied by gross cognitive and mental impairments, then it is far from certain that this disorder will interfere with a professional career.
I know cases when teenagers with ASD were very good at drawing, entered specialized institutions and quite successfully graduated from them, became artists or architects. History knows cases of career-successful musicians, directors, dancers, actors and writers with ASD. Programmers and web designers. Well, yes.
That's all for now. If you have any questions “about a friend” for comments or in a personal, ask, I will try to answer within the framework of a neurological view.
P.S. If you get to our clinic - "Our Time", say that you are from Habr, there will be a small discount on services.
How is autism diagnosed | Cuprum
We use cookies
to improve our experience!
Good
I’m embarrassed to ask
Author: Vera Kurbatova
0003
6743 views
All people with autism spectrum disorder (ASD) are very different.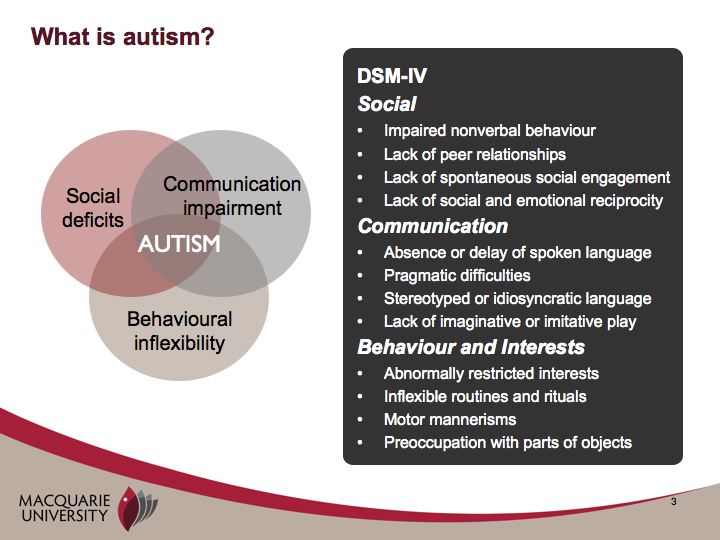 There are those who live with this feature and work, achieve great success, make families and friends, and there are those who need a long-term program of assistance and support. It is impossible to understand what kind of support a person needs without knowing his characteristics. Together with the Naked Heart Foundation and their nakedheart.online project, we have prepared a short article about methods and methods for diagnosing autism.
There are those who live with this feature and work, achieve great success, make families and friends, and there are those who need a long-term program of assistance and support. It is impossible to understand what kind of support a person needs without knowing his characteristics. Together with the Naked Heart Foundation and their nakedheart.online project, we have prepared a short article about methods and methods for diagnosing autism.
Naked Heart Foundation
Currently, there are no medical tests that confirm or deny the presence of autism in a child. Diagnostics is carried out in the form of interviews with parents and other people involved in child care. His behavior is being monitored. Structured diagnostic tests are used to evaluate behavior.
The most common screening in Russia is M-CHAT (Modified Checklist for Autism in Toddlers) - a modified version of the autism screening questionnaire. It consists of 20 questions that parents need to answer and allows you to determine the possible risk of autism in a child aged 1.5 - 2.5 years. The test questions take a few minutes to answer.
A more complex tool is CARS (Childhood Autism Rating Scale) - a rating scale for autism in a child. Typically, CARS is used by a specialist in combination with clinical observation, interaction with the child, and a structured interview with caring adults. In Russia, the translation of the previous version of CARS, available on the Internet, is widely used. This scale applies to children aged 2 to 4 years. An updated and improved version is available in English - CARS2. It has two versions: CARS2-ST for children under 6 years old and CARS2-HF for children over 6 years old with higher communication skills. The tool helps to assess the severity of impairments in different areas of a child's development and draw a conclusion about whether we really observe signs of ASD in a particular child. It should be noted that CARS is not a diagnostic tool either.
ADOS and ADI-R are the most reliable diagnostic tools for ASD and are often used together. These scales are available in Russian. They are used by professionals for the purpose of evaluation and diagnosis.
Turning to a specialist for a diagnosis, you must first make sure that he owns the modern diagnostic tools listed above. In our country, for the official statement of any diagnosis, ICD-10 is used - the International Classification of Diseases of the 10th revision. Its criteria and descriptive base also make it possible to diagnose ASD. Using all of the above tools makes this task easier, and the diagnosis more accurate and reliable.
Parents have the right to insist on a correct diagnosis. If the conclusion obtained is in doubt, it is necessary to seek the opinions of other specialists with sufficient clinical experience and professional qualifications for this.
Currently, the current criteria for diagnosing ASD are based on the DSM-5 classification. It is the most up-to-date guide for diagnosing autism among professionals around the world. These criteria will also be reflected in ICD-11 when it enters into force in 2022.
The DSM-5 provides the most up-to-date and comprehensive toolkit for understanding a child with autism's behavior, symptoms, and basic levels of severity for autism spectrum disorders.
In DSM-5, all components of autism spectrum disorders are divided into two main sections (“autism dyad”): (A) lack of social communication and social interaction and (B) limited, repetitive patterns of behavior, interests or activities.
The first part of the ASD dyad (A) consists of the following subsections:
- A1 - problems in starting and maintaining social interaction.
- A2 - problems with non-verbal communication.
- A3 - problems understanding social situations and social relationships.
The second part of the RAS dyad (B) consists of the following subsections:
- B1 - atypical speech, movements and play.
- B2 - rituals and resistance to change.
- B3 - excessive preoccupation with objects or interests.
- B4 Atypical sensory behavior.
At the same time, the diagnosis of "autism spectrum disorder" should be made only in cases where the manifestations of the "dyad of autism" affect everyday behavior. If a person finds it difficult to interact with relatives, peers and people, develop skills, including speech, be flexible and switch from one task to another. If there are no difficulties in everyday life, then there is no violation. The point of making a diagnosis should not be to put a label on a person, but to help him cope with the difficulties caused by the violation, help him realize his potential and live in society together with other people.
Most often, autism manifests itself in the form of difficulties with social communication and limited repetitive behavior. But, in addition to this, the child may have poorly developed speech and other cognitive impairments. Also, the main symptoms can be accompanied by completely different health problems. They make diagnosing autism even more difficult. For example, autism is often associated with disorders such as epilepsy, genetic syndromes, gastrointestinal disorders, ADHD. That is, they coexist side by side, but do not cause each other (in the scientific literature, this is called comorbidity).
Another important aspect is that behavioral disorders, manifestations of aggression, self-aggression and other forms of unwanted behavior are not related to the diagnostic criteria for ASD. In most cases, these manifestations are due to the insufficient development of the child's communication, as well as the peculiarities of his environment. Understanding children's communication needs and an appropriate assistance program will help reduce problem behaviors and help the child learn academic and social skills in a less restrictive environment.
Thus, problem behavior is not part of autism or other developmental disorders and not necessarily present symptoms, as previously thought.
It is also known that the risk of developing certain conditions (depression, anxiety disorders, obsessive-compulsive disorders, etc.) in adolescents and adults with autism is several times higher than in neurotypical people. We can effectively help these conditions and should not be confused with the diagnostic features of autism. Depression, anxiety disorders, and obsessive-compulsive disorders respond well to treatment in combination with psychotherapeutic help in many cases.
It is important to discuss with the child how the diagnosis will affect life and school. Ask your doctor to tell you more about this. Adults with autism spectrum disorders say that it is very important for them to know their diagnosis and reliable information about the characteristics of people with ASD.
Knowing about one's diagnosis helps a person to think more positively about himself (not to consider himself a loser or an ill-mannered person, to better understand himself and his characteristics). This helps to cope and adapt to difficulties and develop qualities that are important for success in society. For example, a person can learn ways to self-regulate, how to deal with anxiety, plan their day in advance, adapt to unexpected changes, maintain a dialogue, etc.
Information about a diagnosis for a person is a manifestation of respect for him and his features.