Body aches during early pregnancy
Body aches during pregnancy | BabyCenter
As your body changes during pregnancy, you'll feel new aches and pains. Body aches in early pregnancy may be due to hormonal changes. As pregnancy progresses, physical changes can lead to back pain, pelvic pain, round ligament pain, and sciatica. Applying heat or cold and staying physically active can help soothe and prevent pregnancy aches and pains – but sometimes they indicate a more serious issue.
Is pregnancy a literal pain in your back (and just about everywhere else)? Growing a brand-new person is hard work – and it can take a toll on your body, starting in the first weeks of pregnancy.
Here's how to get relief from your pregnancy aches and pains, as well as advice about when it's time to ask your healthcare provider for help.
What causes body aches in pregnancy?
Throughout your pregnancy, hormones relax your ligaments and joints to prepare your body for birth, which may result in body aches and pains.
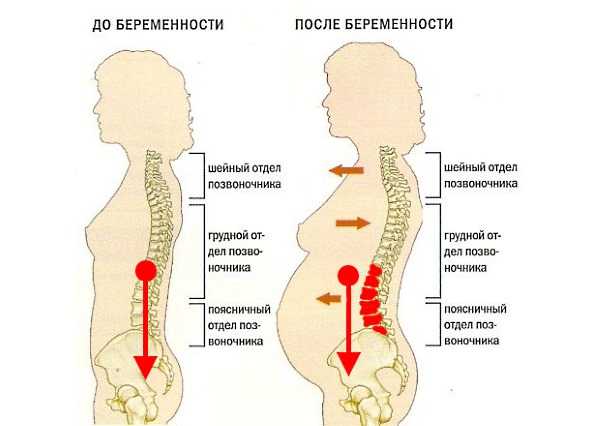
As pregnancy progresses – particularly from the second trimester on – you'll gain weight, which puts extra pressure on your joints. In addition, your growing belly pulls your center of gravity forward and stretches and weakens your abdominal muscles, which support your spine and back. As your body adjusts to these changes, it's very common to feel lower back pain, as well as pain in your pelvis, groin, legs, and buttocks.
In addition, beginning in the second trimester you may experience what's known as round ligament pain: a brief, sharp, stabbing pain or a longer-lasting dull ache in your lower belly or groin. This generally harmless condition happens when the attachments between your growing uterus and abdominal wall (The "round ligaments") are pulled or stretched.
You may also experience sciatica as pressure from the weight of your baby and uterus presses on your sciatic nerve, sending shooting pain from your buttocks down the back of your leg.
Is it normal to have body aches in early pregnancy?
Yes. You may experience early pregnancy body aches and muscle pains all over due to hormonal changes, especially toward the end of the first trimester.
Pelvic pain (technically known as pelvic girdle pain) and lower back pain are the most frequent complaints. These discomforts can pop up at any point in pregnancy, although they're more common beginning in week 14 (the start of the second trimester).
You may also experience mild uterine cramping in early pregnancy, similar to period pains, as your uterus begins to expand in size. You could also have stomach pains due to constipation or gas, both of which are common during pregnancy. Digestive problems are also linked to hormonal changes and start early in pregnancy.
Advertisement | page continues below
Relieving body aches in pregnancy
To relieve sore muscles and body aches in pregnancy, lie down, relax, and apply heat and/or cold to the affected areas. A cold pack can reduce inflammation and help to soothe muscle and back pain.
To apply heat, you can use an electric heating pad, hot water bottle, or microwaveable pad filled with flax or buckwheat. Don't apply heat to your abdomen for longer than ten minutes. You don't want to raise your internal temperature too much, as this can affect your developing baby.
Don't apply heat to your abdomen for longer than ten minutes. You don't want to raise your internal temperature too much, as this can affect your developing baby.
One of the best strategies to prevent and treat body aches in pregnancy is to stay physically active. While it may seem counterintuitive, exercise helps relieve all sorts of common pregnancy complaints, from back pain to constipation and gas. Pregnancy-safe exercise helps to keep pregnancy weight gain in check, strengthens and stretches your muscles, improves your posture, and supports your circulation.
To relieve back and pelvic pain specifically, sit in a supportive chair, sit down when getting dressed, use proper form to lift heavier objects, and try to avoid standing for long periods of time if possible.
If these tips don't help, talk to your provider about whether to take a pregnancy-safe pain reliever (usually acetaminophen). You can also ask your ob-gyn or midwife for a referral to a physical therapist. Working with a physical therapist can help to relieve your pain and increase your strength as pregnancy progresses.
Working with a physical therapist can help to relieve your pain and increase your strength as pregnancy progresses.
When to call your doctor or midwife
Sometimes, certain body aches and pains in pregnancy can be a sign of something more serious. Severe back pain may be a sign of a kidney infection; it's often accompanied by fever and a burning sensation when you urinate. Rarely, abdominal pain and cramping in the first trimester of pregnancy may be caused by ectopic pregnancy or miscarriage.
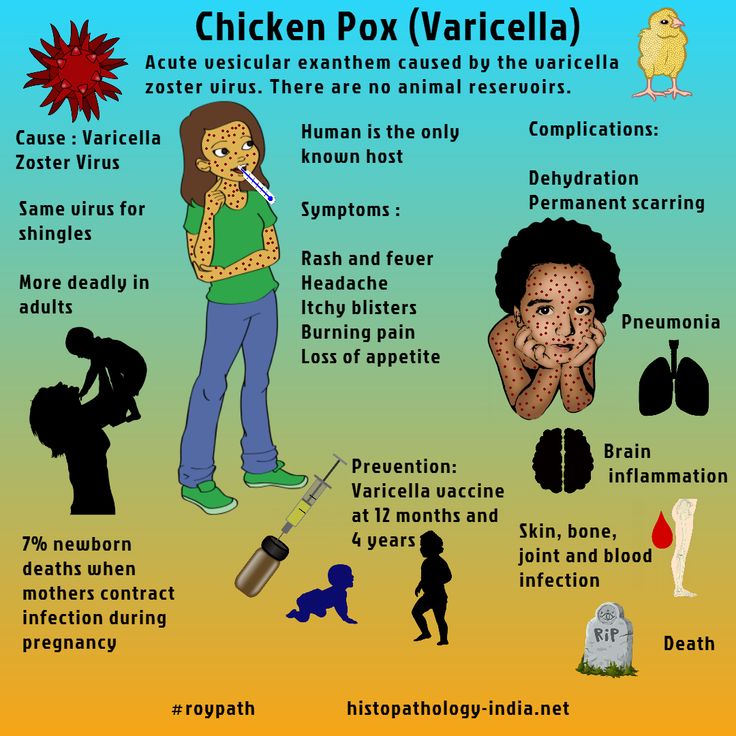
Generalized body aches along with fevers and/or upper respiratory symptoms can also be caused by flu or COVID-19. Pregnant women are more susceptible to complications with both of these infections.
Call your provider if body aches don't improve with the simple treatments above, or if you have:
- Severe and constant abdominal pain, especially if it doesn't go away within an hour given rest
- Vaginal bleeding or spotting
- Fever
- Unusual vaginal discharge
- Pain or burning when you pee
Common body aches in pregnancy
In addition to general body aches and muscle pain in pregnancy – especially in the back and pelvis – you may experience these other discomforts:
Headaches
Feeling a squeezing pain or a steady dull ache on both sides of your head could signal a tension headache. This usually harmless pregnancy symptom is especially common during the first trimester, linked to hormonal changes and increased blood flow. (If you're in your second or third trimester and have a severe headache that won't go away, call your healthcare provider just to be safe.)
This usually harmless pregnancy symptom is especially common during the first trimester, linked to hormonal changes and increased blood flow. (If you're in your second or third trimester and have a severe headache that won't go away, call your healthcare provider just to be safe.)
Find out more about headaches during pregnancy.
Hemorrhoids
Hemorrhoids are unusually swollen blood vessels in the rectal area that are usually linked to constipation and straining during bowel movements. They can be merely itchy or downright painful and can sometimes cause rectal bleeding, especially during a bowel movement. Some women get hemorrhoids for the first time while they're pregnant, but if you've had them before you got pregnant, you're very likely to have them again now.
Find out more about hemorrhoids during pregnancy.
Heartburn
If you feel a burning sensation in your chest after you eat, it's probably heartburn (also called acid indigestion or acid reflux). During pregnancy, hormones relax the lower esophageal sphincter, allowing stomach acid to climb back up and burn the esophagus. Later in pregnancy, your growing baby pushes up on the stomach and its contents, adding to the burn.
During pregnancy, hormones relax the lower esophageal sphincter, allowing stomach acid to climb back up and burn the esophagus. Later in pregnancy, your growing baby pushes up on the stomach and its contents, adding to the burn.
Find out more about heartburn during pregnancy.
Leg cramps
No one's really sure why spasms in the leg muscles are common during the second and third trimesters, but they could be from vitamin deficiencies, electrolyte imbalances, or changes in your activity level, among other reasons.
Find out more about leg cramps during pregnancy.
Carpal tunnel syndrome
If you feel tingling or numbness in your hands during pregnancy, it could be carpal tunnel syndrome. Extra fluid and swelling during pregnancy can press on the nerves that pass from the hand through the wrist to the forearm, causing these symptoms.
Find out more about carpal tunnel syndrome during pregnancy.
How to Deal with Body Aches During Pregnancy
You’re swollen, you’re tired and everything hurts. Oh, the joys of pregnancy! For many mamas-to-be, a day doesn’t seem to go by without pregnancy aches and pains. Whether it’s pain in a specific area (hello, pelvic pressure!) or more general discomfort, chances are you’ll experience some of this during your nine month journey to motherhood. The good news? Body aches in pregnancy are usually a completely normal reaction to the changes your body is going through. Read on to learn more about what could be causing your discomfort and how you can ease those body aches during pregnancy.
Oh, the joys of pregnancy! For many mamas-to-be, a day doesn’t seem to go by without pregnancy aches and pains. Whether it’s pain in a specific area (hello, pelvic pressure!) or more general discomfort, chances are you’ll experience some of this during your nine month journey to motherhood. The good news? Body aches in pregnancy are usually a completely normal reaction to the changes your body is going through. Read on to learn more about what could be causing your discomfort and how you can ease those body aches during pregnancy.
In this article:
Causes of body aches during pregnancy
How to ease body aches during pregnancy
When to call the doctor
Causes of Body Aches During Pregnancy
The cause of pregnancy aches and pains is usually two-fold: Your changing body, and all those pesky (but oh-so-important!) hormones. As your growing bump puts excess pressure on your muscles and skeleton, your hormones are also amping up and starting to relax your ligaments. “These factors change your posture and center of gravity to accommodate the growing fetus, while at the same time causing weakening of the abdominal walls and increasing strain on the muscles, which results in a combination of body aches and pains,” explains Talitha Bruney, MD, an ob-gyn at Montefiore Medical Center in New York City.
“These factors change your posture and center of gravity to accommodate the growing fetus, while at the same time causing weakening of the abdominal walls and increasing strain on the muscles, which results in a combination of body aches and pains,” explains Talitha Bruney, MD, an ob-gyn at Montefiore Medical Center in New York City.
When it comes to body aches in pregnancy, the most common complaint is definitely back pain, which a whooping 60 percent of pregnant women experience, according to Bruney. But many first-time moms will also experience abdominal aches and pains earlier on in pregnancy, explains Kecia Gaither, MD, an ob-gyn in New York City. “These abdominal pains, termed round ligament pain, are related to the uterus expanding out of the abdominal cavity, and typically resolve well into the second trimester,” she says.
Moms-to-be can also be on the lookout for possible leg, feet, hand, head and joint pain later on in pregnancy. Some of those discomforts may be caused by weight gain or swelling from fluid retention, which can put more pressure on your joints and nerves, Bruney explains.
“Symptoms vary from person to person and may be dependent on their activity level,” Bruney says. “Pregnancy body aches may be worse at the end of the day in a very active mom-to-be who has fatigued muscles, or may be worsened by certain positions, like moving from a sitting to standing position, sitting in an uncomfortable chair or being stationary for prolonged periods.” Aches and pains can occur at any point in pregnancy, but they’re often most bothersome during the third trimester, she adds, since baby is bigger at that stage of pregnancy.
How to Ease Body Aches During Pregnancy
The best way to prevent body aches in pregnancy is by staying active and keeping your pregnancy weight gain in check. (It’s recommended that women of normal BMI gain between 25 and 35 pounds in total.) But even if you’re already suffering from discomfort, moderate exercise like walking has been shown to help reduce pregnancy back pain, Bruney says. You can also take acetaminophen (Tylenol), or pick up a belly support belt. According to Bruney, “in patients with lower back pain and pelvic pain, providing better support to their abdominal wall and muscles can be helpful in relieving some of their symptoms.”
According to Bruney, “in patients with lower back pain and pelvic pain, providing better support to their abdominal wall and muscles can be helpful in relieving some of their symptoms.”
When to Call Your Doctor
Although body aches in pregnancy are considered normal, it’s still a good idea to chat with your doctor or midwife about them at your next appointment, Gaither suggests. (You’re always better safe than sorry, especially when pregnancy is concerned.) You’ll want to call your doctor right away if the aches are really severe, restrict your movement or include swelling or redness on your legs, Bruney adds, since those can be signs of a possible blood clot. Also know this: Pregnancy aches and pains usually affect a particular region in the body instead of all over, and they’re not typically associated with other symptoms (like fever, chills or cough)—so if you have any of those, you might be suffering from a cold or flu. In that case, give your primary care doctor a call.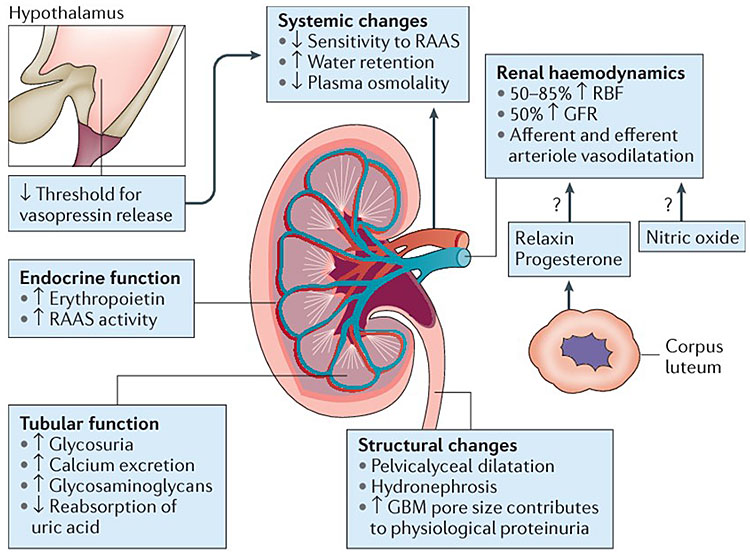
Updated February 2020
Expert bios:
Talitha Bruney, MD, is an ob-gyn and the medical director of the Comprehensive Family Care Center in the department of obstetrics and gynecology and women’s health at Montefiore Medical Center in New York City.
Kecia Gaither, MD, MPH, FACOG, is a double board-certified OB-GYN and maternal fetal medicine specialist in New York City with more than 20 years of experience. She serves as the director of perinatal services for NYC Health+Hospitals/Lincoln.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
How to Deal with Swelling During Pregnancy
How to Cope with Sciatica During Pregnancy
Over-the-Counter Medications You Can Take While Pregnant
Why pulls the stomach in the early stages of pregnancy?
Why does the stomach pull in the early stages of pregnancy? This question often worries expectant mothers, and at times leads to panic.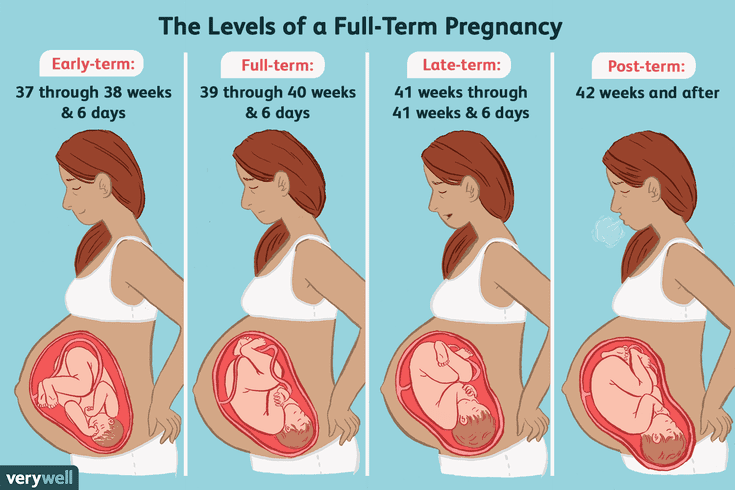 When is discomfort pathology, and when is it normal?
When is discomfort pathology, and when is it normal?
Pregnancy is a special time for a mother and her baby. After all, the connection between them is inextricable, and every negative influence or stress affects both of them.
Possible causes of pain
Every woman dreams of having an easy pregnancy and no cause for alarm. However, a very common complaint among pregnant women is pain in the lower abdomen of a pulling or aching nature.
Complaints are so common that it is necessary to clearly understand when pulling sensations during pregnancy are pathological and require immediate medical attention, and when they are completely physiological and require only general recommendations.
Of course, pain in the lower abdomen can appear at any stage of pregnancy, however, most often women notice their appearance in the early stages of pregnancy.
Painful sensations in the abdomen during pregnancy are very diverse both in subjective sensations and in their localization, in intensity of occurrence.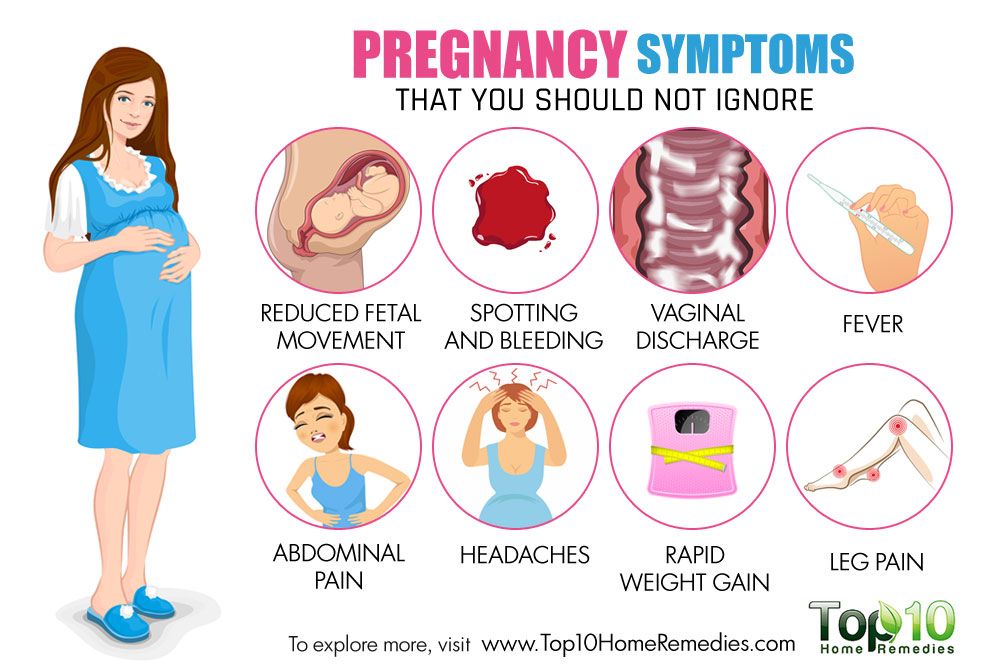 Pain can appear both at rest and after any physical activity. Unpleasant sensations can manifest themselves in one place, or radiate to other areas.
Pain can appear both at rest and after any physical activity. Unpleasant sensations can manifest themselves in one place, or radiate to other areas.
Unpleasant sensations in the lower abdomen are rarely avoided during pregnancy. These sensations can occur not only in pathology. During pregnancy, the uterus increases in size, there is a tension in its ligaments and muscles. In addition, there is a displacement of the pelvic organs. All this leads to the appearance of pulling or aching sensations in the abdomen. All these phenomena are manifestations of physiological changes that occur to a woman during pregnancy.
Of course, this state of fear does not cause and does not require any intervention on the part of the doctor. However, pulling pains in the lower abdomen are not always a physiological process. It happens that this indicates that the pregnancy proceeds with pathology and requires medical adjustment.
That is why, if there are pulling or aching pains in the lower abdomen, it is necessary to contact an obstetrician-gynecologist in order to accurately determine the cause of the pain.
Never self-medicate. Remember that you are responsible not only for yourself, but also for the little man that you carry under your heart.
Abdominal pain during pregnancy may be:
- obstetric;
- "non-obstetric".
Pain associated with pregnancy may be developmental:
- physiological changes during pregnancy;
- threatened miscarriage;
- missed pregnancy;
- ectopic pregnancy.
Pain not associated with pregnancy may occur with:
- inflammatory processes;
- pathologies of the digestive system;
- surgical diseases;
- diseases of other organs or systems.
Pain in the lower abdomen during pregnancy as a variant of the norm
Not all pain in the lower abdomen during pregnancy is a manifestation of pathology. Sometimes they can occur during the normal course of pregnancy.
As a physiological process, pain in the lower abdomen can occur in the following situations:
- sign of pregnancy;
- displacement of the pelvic organs by the growing uterus;
- stretching of the ligaments and muscles associated with the growth of the uterus.

Abdominal pain is a sign of pregnancy
Finding out that you are pregnant is now not a big deal, because there are pregnancy tests. In addition, a delay in menstruation can serve as evidence of pregnancy.
All this is good when menstruation is regular and delayed by at least 14 days. In this case, the pregnancy test may be positive. However, do not forget that not all tests are highly accurate, so it can show two cherished strips much later than we would like.
Therefore, it is necessary to pay close attention to the sensations of your body, because it signals the onset of pregnancy long before the manifestation of a delay in menstruation.
If you assume that pregnancy is possible, then listen carefully to your body: it can send you a signal in the form of pulling pains in the lower abdomen. At the same time, the pains will differ in their intensity: one woman will say that the pains are unbearable, the other will not notice them at all. Each woman is individual.
Each woman is individual.
If each menstruation is preceded by unpleasant pain in the lower abdomen or lower back, you may not understand that once again they are associated with the onset of pregnancy.
Pain in the lower abdomen during pregnancy may be associated with the implantation process. To do this, you need to remember the process of fertilization of the egg by the sperm. After their fusion in the fallopian tubes, the fertilized egg enters the uterus under the action of the movement of cilia in the fallopian tubes. The uterine endometrium is a loose mass where a fertilized egg is implanted.
The process of implantation is the insertion of a fertilized egg into the endometrium of the uterus. At this time, there is a violation of the integrity of the endometrium, which may be accompanied by unpleasant sensations in the lower abdomen. In addition, sometimes slight dark bloody discharge may appear from the genital tract, which can be perceived as the beginning of another menstruation.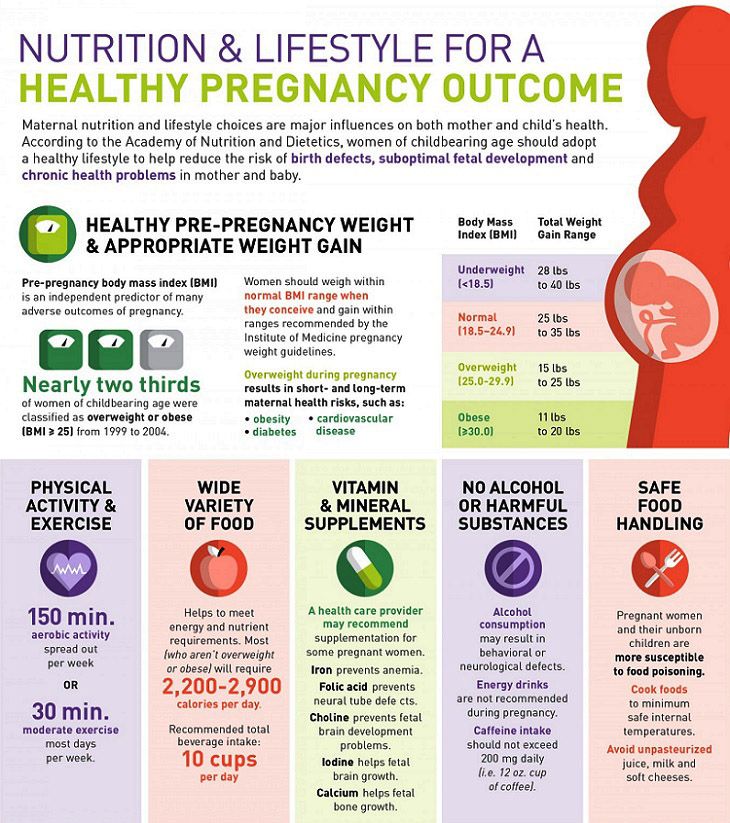
Threatened miscarriage
A fairly common cause of pain in the lower abdomen is a threatened miscarriage. This condition is individual and does not depend on physical exertion or complete rest, but on the condition of the woman and her unborn child.
Among the reasons that may cause a miscarriage may be:
- severe physical exertion;
- sexual contact;
- malnutrition of the ovum;
- genetic disorders and other causes.
Of course, this is not evidence that a miscarriage will not occur with complete rest. Miscarriage can occur due to genetic abnormalities, and due to stress. No woman is immune from the threat of pregnancy loss.
That is why attention and sensitivity to the state of your body is so necessary, which will in every possible way send signals that the pregnancy is not going the way you want.
Threatened miscarriage is accompanied by:
- aching or pulling pains in the lower abdomen;
- aching or drawing pains in the small of the back or sacrum.
- bloody discharge from the genital tract.
If you have pain in the lower abdomen, you need to see a doctor, because a threatened miscarriage, if medical assistance is not provided, can turn into an abortion that has begun, the treatment of which is much more difficult, if not completely useless.
An ambulance should be called if:
- pain in the lower abdomen gets worse;
- pains begin to radiate to other areas;
- painful sensations do not go away for a long time;
- bloody discharge from the genital tract appeared.
Increased pain
If the pulling pains in the lower abdomen are weak, do not increase and do not radiate to other areas, then you can come to the antenatal clinic in the daytime on your own. This will not threaten serious complications of your condition.
If the pain becomes more intense, does not go away at rest, you should not self-medicate, take drugs without a doctor's prescription.
Do not put anything on the stomach. Both hot and cold application can contribute to the onset of a miscarriage. In addition, with the threat of termination of pregnancy, this manipulation will not remove the pain.
Localized pain
When a threatened miscarriage occurs, pain of a pulling or aching nature disturbs the pregnant woman in the lower abdomen.
If the pains have a clear localization in a certain place, most often on the right or left, then a mandatory consultation with a specialist is necessary, since an ectopic pregnancy or surgical pathology, such as appendicitis, may develop.
Bloody discharge from the genital tract
If bloody discharge from the genital tract has joined the pulling pain in the lower abdomen, urgent medical attention is needed. This phenomenon may indicate a miscarriage that has begun.
The discharge may be scanty, spotting or copious, dark or bright. In any case, you can not do without consulting an obstetrician-gynecologist.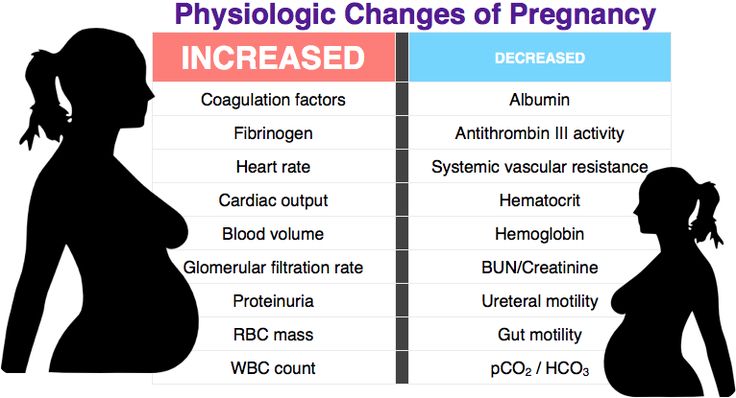
There are situations when there is no pain, but there is bloody discharge from the genital tract. This case also requires specialist advice.
Any bloody discharge from the genital tract may indicate a miscarriage. Only timely treatment can contribute to the preservation and prolongation of pregnancy.
In some cases, the appearance of bloody discharge from the genital tract may be a manifestation of a miscarriage, which requires immediate medical attention.
Miscarriage
The fertilized egg does not always develop correctly. In some cases, there is a cessation of its division and death. Most often, missed pregnancy occurs due to any mutations. At the same time, the woman does not suspect that the pregnancy has stopped.
However, the dead fetal egg begins to be rejected on its own. At the same time, there are pulling pains in the lower abdomen, which are soon joined by bloody discharge from the genital tract.
When a miscarriage is diagnosed, curettage of the uterine cavity may be indicated. Conservative management is also possible, but this can only be determined by a specialist after consultation.
Conservative management is also possible, but this can only be determined by a specialist after consultation.
Ectopic pregnancy
Ectopic pregnancy most often occurs as a tubal pregnancy, when the fertilized egg does not reach the uterus, and the implantation process occurs in the fallopian tube. At the same time, the development of the fetal egg can continue for a long time without any manifestations, up to 12 weeks of pregnancy. However, most often such a pregnancy is interrupted at 6 to 8 weeks.
The fertilized egg develops and grows, which causes pain in the right or left side of the lower abdomen. The pains are unilateral, are obsessive, tend to increase.
In addition to pain in the lower abdomen, bloody discharge from the genital tract appears, and the pain begins to radiate to the leg from the side of the pain. There may be unpleasant sensations of pressure on the rectum. Medical surgery is the only way to save a woman's life. Preservation of pregnancy is impossible.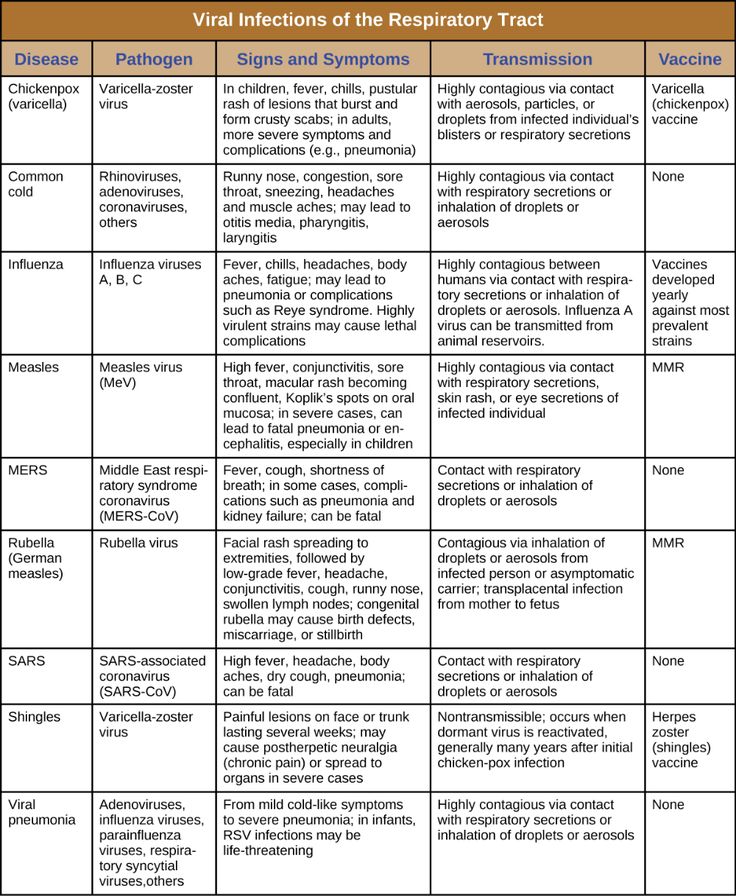
"Non-obstetric" causes of pain in the lower abdomen
Inflammatory processes
Among the "non-obstetric" causes of pain in the lower abdomen, the most common are inflammatory processes of the pelvic organs. If earlier it was believed that there could be no inflammation in pregnant women, now it has been proven that a decrease in the immunity of a pregnant woman awakens all pathological processes in her body.
Pain in inflammatory processes of the pelvic organs differ in their intensity. At the same time, they occur in the lower abdomen and most often have a pulling or aching character.
Pathology of the digestive system
Very often, pulling pains in the lower abdomen can occur in a pregnant woman due to problems with the digestive tract. During pregnancy, there is a decrease in intestinal contractility. In addition, there are significant changes in the hormonal background of a woman. Therefore, very often pregnancy is accompanied by constipation and bloating. To normalize digestion, a change in diet is recommended and mild laxatives can be taken.
To normalize digestion, a change in diet is recommended and mild laxatives can be taken.
Surgical pathology
Of the surgical pathologies that may be accompanied by pulling pains in the lower abdomen during pregnancy, acute appendicitis is the most common.
In the early stages of pregnancy, it is obligatory to differentiate obstetric and gynecological diseases from appendicitis, since it has similar symptoms. There are pains in the lower abdomen, which most often occur in the navel or stomach, and then descend to the right iliac region. Nausea, vomiting, fever joins. The only treatment is surgery. In this case, the pregnancy is preserved.
Diseases of other organs or systems
In addition to obstetric and surgical causes, which can cause pulling pains in the lower abdomen in early pregnancy, other body systems may also be involved in the pathological process. The most common lesion is the urinary tract.
Cystitis
Due to the anatomical features of a woman, cystitis can occur at any time and in any condition, so pregnant women are just as susceptible to it as non-pregnant women.
The bladder, located in the lower third of the abdomen, may give false symptoms of threatened miscarriage.
Cystitis, in addition to pulling or aching pains in the lower abdomen, is accompanied by pain during urination, pain at the end of the act of urination. In addition, with cystitis, the urine may be stained with blood, and it is difficult to distinguish this from bloody discharge during a miscarriage.
In any case, it is necessary to consult an obstetrician-gynecologist, pass a general urine test, and then consult a urologist and treat the infection. Any infection can adversely affect the condition of the fetus, so timely treatment is the key to the normal development of your child.
Make an appointment with a gynecologist
For more details, consult a qualified specialist at the Semeynaya clinic.
For prices for gynecological appointments or other questions, please follow the link below:
Early pregnancy | Shchelkovsky perinatal center
Pregnancy is a wonderful period! However, the changes taking place in the body at this time can greatly frighten you. The phenomena characteristic of pregnancy are different for all women, and will not necessarily be repeated during each subsequent gestation. Let's analyze the most common symptoms, their causes and possible methods of correction.
The phenomena characteristic of pregnancy are different for all women, and will not necessarily be repeated during each subsequent gestation. Let's analyze the most common symptoms, their causes and possible methods of correction.
1. Frequent urination.
Frequent, painless (!) urge to urinate is one of the signs of pregnancy. This is due to increased secretion of progesterone (pregnancy hormone), changes in metabolism and pressure from the growing uterus on the bladder.
Be sure to see a doctor if:
- painful urination (this may be a sign of an infection)
- urine of strange color (stained with blood, brown)
- the amount of urine excreted per day is much less than the liquid drunk per day
Life hack! Under no circumstances should fluid intake be restricted! To alleviate the condition and reduce the frequent urge to urinate, it is necessary to exclude products that have a diuretic effect: tea, coffee, zucchini, watermelon; as well as salty, spicy and fried foods.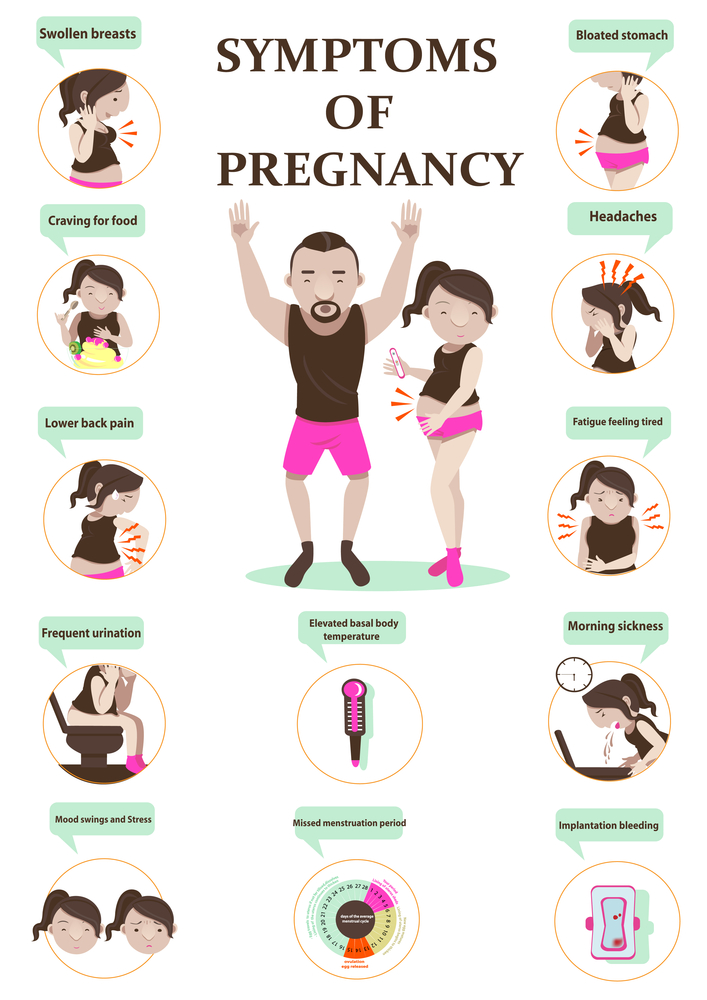 It is better to drink water or juice. Wear comfortable cotton underwear that does not squeeze the lower abdomen.
It is better to drink water or juice. Wear comfortable cotton underwear that does not squeeze the lower abdomen.
2. Nausea, vomiting, heartburn, increased susceptibility to odors.
Nausea is one of the common symptoms of early pregnancy. The range of issues related to nausea and vomiting during pregnancy is quite wide. From "it's good, I don't even feel sick" (with relief), "I don't feel sick, what's wrong with me?" (with anxiety) to "when will this nausea pass" (with hope). Indeed, these symptoms are not at all a mandatory accompaniment of gestation, they can manifest at 7-8 weeks and last up to 12-14 weeks. The duration of this condition can sometimes be delayed, but rarely persists throughout pregnancy.
Life hack! For nausea, eat before feeling hungry. Solid, non-hot food and drinks at a cool temperature are best. With heartburn, you should eat small portions of food and often, and most importantly, sit, stand or walk for at least 30 minutes after eating, but do not lie down.
You should definitely consult a doctor if:
- vomiting occurs even after drinking water
- vomiting is exhausting, accompanied by dizziness, weakness
- dryness, jaundice and flaking of the skin appear
- Nausea and vomiting interfere with proper nutrition, accompanied by weight loss
To reduce nausea and vomiting in the morning, try eating something before you get out of bed. It can be a cracker, a cookie, a piece of hard cheese. And salty food is preferable to sweet. You can have a snack in the same way at night when you get up to go to the toilet. Do not lie down immediately after eating, this will only increase nausea. Vitamins for pregnant women with nausea should be taken in the evening after meals. Cool water with lemon, ginger, mint tea, or ginger or mint candies can alleviate the condition. It is necessary to exclude those foods, drinks and smells that are unpleasant to you. Brushing your teeth and rinsing your mouth often can also reduce nausea.
3. Pain or cramps in the lower abdomen, constipation, pain in the lumbar region.
The simplest and most easily controlled cause of pain is delayed and incomplete bowel movements. An increase in the concentration of progesterone relaxes the smooth muscles, which are located not only in the uterus, but also in other hollow organs. In this case, the correction of the diet and the restoration of the passage of feces will help. If the measures are ineffective, the doctor may prescribe safe drugs for you. A special type of pain that occurs during exclusivity in pregnant women is pain in the round ligament of the uterus. This acute, rather intense pain occurs, as a rule, on the one hand with a sharp change in body position (for example, when getting up from a chair or leaving a car). This pain occurs due to stretching, and then a sharp contraction, like a spring, of the round uterine ligaments. The pain quickly passes if you immediately take a comfortable position and does not require special treatment.
You should definitely consult a doctor if:
- pain is accompanied by spotting bloody discharge from the external genitalia
- increasing duration and intensity of pain
- abdominal pain accompanied by dizziness, fever, loss of consciousness
Life hack! To normalize bowel movements, eat more vegetables and fruits, drink water and move more during the day. Try to eat often and in small portions.
4. Enlargement and soreness of the mammary glands.
Hormonal restructuring of the body during gestation is accompanied, among other things, by an increase in the size of the mammary glands and an increase in their sensitivity. By the end of the first trimester, the soreness usually disappears, no additional methods of treatment are needed.
Life hack! Choose comfortable supportive underwear (it should not leave marks on the skin at the end of the day). You may need a larger size or a sports bra. Pain in the mammary glands is relieved by a warm shower at the end of the day.
You may need a larger size or a sports bra. Pain in the mammary glands is relieved by a warm shower at the end of the day.
You should definitely see a doctor if:
- the pain is severe
- mammary glands are very dense with redness and body temperature is increased
- discharge from the nipples appears (purulent, bloody)
5. Increased body temperature.
In early pregnancy, an increase in body temperature to 37.5 ° C is not necessary, but is possible due to the peculiarities of the action of progesterone. Because of this, it is difficult for pregnant women to endure stuffy, hot rooms. Self-medication is dangerous: an attempt to bring down the temperature even with a seemingly harmless folk method - tea with raspberries - can mask the true cause of hyperthermia and delay the diagnosis. Due to the increased body temperature, pregnant women should dress in layers and avoid stuffy and hot rooms and spaces so that they can always “adjust” their temperature on their own.
- temperature above 37.5 °C
- along with fever, any pain occurs
- runny nose, cough, body aches appear
6. Nasal congestion, difficulty in breathing, nosebleeds.
These symptoms can be explained by the individual reaction of the vascular system to the increase in blood volume that occurs during pregnancy. Another possible reason is dry air in the room, the operation of central heating batteries.
Life hack! The easiest way to deal with nasal congestion is to use a humidifier. If you don't have one, you can put a damp towel on the battery - less effective, but better than nothing. It is possible to use sprays with sea salt, but you need to carefully read the instructions and especially the "Indications" section, it should contain information about the safety of the product during pregnancy.
You should definitely see a doctor if:
- symptoms of a cold occur
- nasal congestion accompanied by ear congestion
- These symptoms appeared after exposure to the allergen known to you
7. Blood pressure fluctuations.
Blood pressure fluctuations.
An ideal option for the course of any pregnancy is the stability of the blood pressure throughout the gestation. However, this is extremely rare. A small (up to 10 units) increase in pressure from the usual reference may be due to an increase in the load on the cardiovascular system as a result of changes in body weight, hormonal changes, and uterine pressure on the vessels. Normal pressure: systolic below 130 mm Hg, diastolic no more than 85 mm Hg. Blood pressure in the range of 130-139/ 85–89 mm Hg considered high to be normal. High numbers are often observed in patients of older reproductive age, suffering from diabetes mellitus and kidney disease, obesity, etc. However, it is imperative to tell the doctor about all these concomitant pathological conditions at the first appointment and, if necessary, consult a neurologist, cardiologist, endocrinologist and other related specialists . Reasonable physical activity, adherence to sleep and wakefulness, a balanced diet, and the rejection of coffee and strong tea allow you to keep pressure within limits.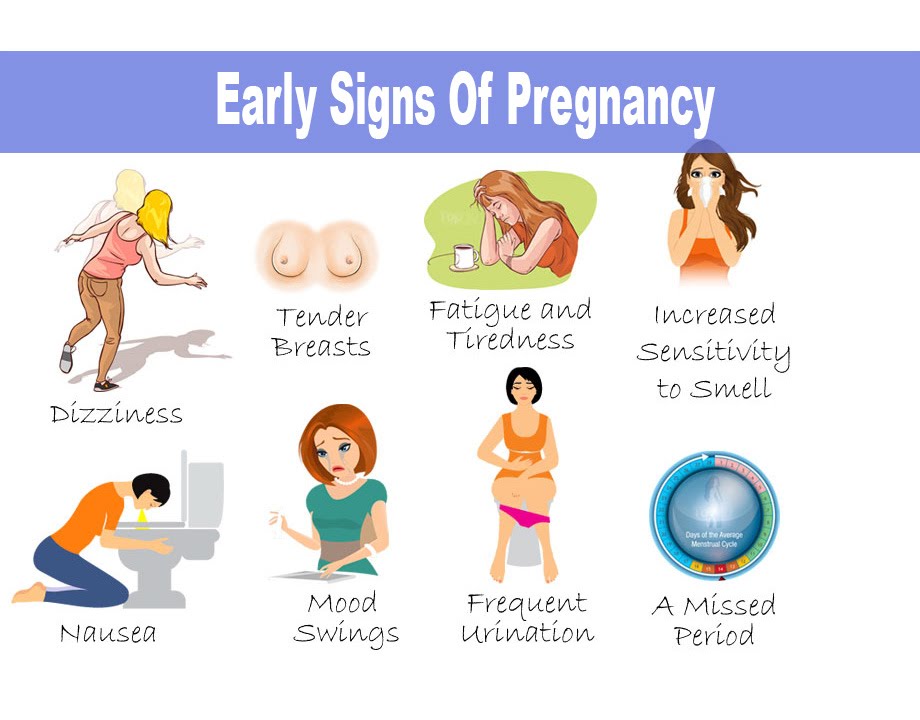 Of the completely exotic for our days, but no less significant - the prevention of stress.
Of the completely exotic for our days, but no less significant - the prevention of stress.
Life hack! If you are experiencing high normal blood pressure for the first time, repeat the measurement after 15 minutes. If the pressure remains elevated, see a doctor.
Be sure to see a doctor if: NB! You should also pay attention to lowering blood pressure. Numbers less than 90/60 mmHg - an excuse to see a doctor. Life hack! Keep a blood pressure diary, especially if you have a tendency to hypertension. Show your diary to your doctor at every appointment. 8. Heaviness and pain in the legs. Heaviness and pain in the legs, especially in the evening, are frequent companions of pregnancy. Life hack! Ask your partner/husband to give you a foot massage, relax with your limbs elevated (not too much!) A therapeutic pedicure, dousing the legs with cool water, a contrast shower, a cream or gel for legs with cooling components (menthol, essential oils), as well as compression stockings or stockings of the lightest degree of compression will help. Be sure to see a doctor if: 9. Skin changes. During pregnancy, you may notice dark spots on your skin. Especially often such darkening (hyperpigmentation) is observed in the nipple area, along the white line of the abdomen. Stretch marks (stretch marks) may appear on the skin of the abdomen and thighs. Life hack! Oils and moisturizing creams to increase skin elasticity, contrast showers, massage with a hard brush will help reduce the likelihood of skin changes. You should definitely consult a doctor if: 10. Bleeding gums. Changes in the characteristics of blood circulation in the body of a pregnant woman can cause bleeding gums. You should definitely consult a doctor if: 11. Fatigue, mood instability. Tearfulness, lack of strength, forgetfulness, distraction, the whole palette of feelings "here and now"... The list can be continued, and there is only one explanation for this - pregnancy. The most common early symptom is severe fatigue. There is no universal recipe, just as there is no single picture of these states. The main recommendation for all pregnant women is to rest often, relax and even sleep during the day. Most importantly, you need to remember: pregnancy is not a disease, but a great time to prepare for motherhood.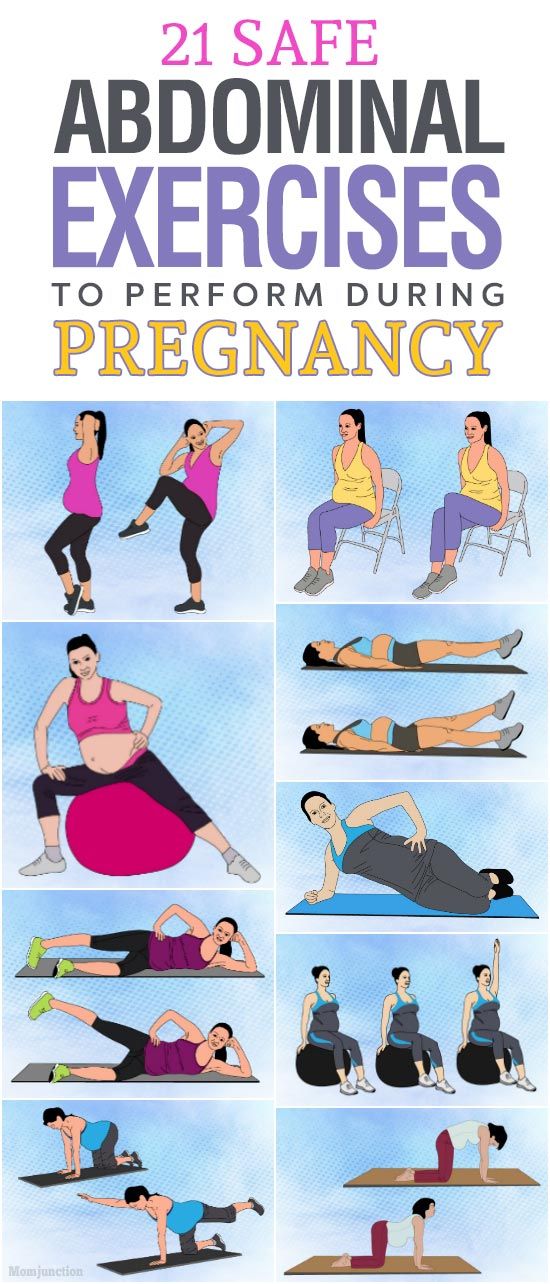 There is an explanation for the occurrence of symptoms: an increase in load due to growing weight and a shift in the center of gravity of the body.
There is an explanation for the occurrence of symptoms: an increase in load due to growing weight and a shift in the center of gravity of the body.
 These are normal signs and do not require any treatment. In most cases, skin color will return to normal after breastfeeding ends, and stretch marks will shrink and fade. Itching can be associated with stretching of the skin, especially in the abdomen and mammary glands. This symptom occurs infrequently and is usually successfully stopped by the use of special products to moisturize and soften the skin. By the way, these same remedies usually help in the fight against stretch marks.
These are normal signs and do not require any treatment. In most cases, skin color will return to normal after breastfeeding ends, and stretch marks will shrink and fade. Itching can be associated with stretching of the skin, especially in the abdomen and mammary glands. This symptom occurs infrequently and is usually successfully stopped by the use of special products to moisturize and soften the skin. By the way, these same remedies usually help in the fight against stretch marks.
 The appearance of minor blood impurities during brushing your teeth, when eating solid foods (for example, an apple) is acceptable. However, the key provision is "insignificant". If you find it difficult to assess your own condition, consult a specialist.
The appearance of minor blood impurities during brushing your teeth, when eating solid foods (for example, an apple) is acceptable. However, the key provision is "insignificant". If you find it difficult to assess your own condition, consult a specialist.